
 | Oncologie | 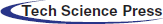 |
DOI: 10.32604/oncologie.2022.021347
CASE REPORT
Delayed Bilateral, Post-Traumatic Extra-Subdural Hematomas in a Patient with Meningioma
1Department of Neurosurgery, Cannizzaro Hospital, Trauma Center, Gamma Knife Center, Catania, Italy
2Department of Radiation Oncology, REM Radioterapia SRL, Viagrande, Italy
3Department of Neurosurgery, Neurosurgery Clinic, Birgunj, Nepal
4Department of Pathology, Stanford School of Medicine, Stanford University Medical Center, Palo Alto, USA
5Department of Pathological Anatomy, Cannizzaro Hospital, Catania, Italy
6Neurosurgery Unit, Highly Specialized Hospital and of National Importance “Garibaldi”, Catania, Italy
*Corresponding Author: Giuseppe Emmanuele Umana. Email: umana.nch@gmail.com
Received: 10 January 2022; Accepted: 23 March 2022
Abstract: Concomitant acute epidural hematoma (EDH) and subdural hematoma (SDH) is a rare finding, and its bilateral onset has not yet been reported in literature. We present the first report of a patient affected by post-traumatic concomitant EDH and SDH, with the contralateral, delayed onset of another, associated with meningioma previously treated with gamma knife. A 60-year-old female patient with a history of simple focal seizures with motor symptoms and well-controlled by drugs since childhood, arterial hypertension, and incidental diagnosis of multiple meningiomas was referred to our department after falling down the stairs. Initially, the patient was prescribed gamma knife treatment of the right frontal convexity meningioma. The patient was admitted to our emergency department with Glasgow Coma Scale (GCS) score of 7/15 and isochoric, myotic pupils. An immediate head CT scan revealed a small acute SDH in the right hemisphere and an acute blood collection in the left hemisphere, which exerted mass effect; furthermore, we discovered complex skull fractures across the superior sagittal sinus, and dislocated bone fragments. A left decompressive craniectomy was performed, and intraoperatively we observed a concomitant EDH/SDH. Due to the patient’s anisocoria, an urgent postoperative CT scan was performed, revealing a massive blood collection in the right hemisphere, which was discovered to be another concomitant EDH/SDH, during right trauma flap. Through this approach, we also removed the right frontal convexity meningioma. After 5 days in the intensive care unit (ICU), the patient died because she presented an acute heart failure. The development of a contralateral, delayed EDH/SDH must be considered in severe traumatic patients, especially if associated fractures across major dural sinuses are present. Intraoperative CT scan, if available, or immediate postoperative CT scan, is mandatory for adequate management of complex neurotrauma cases.
Keywords: Extradural hematoma; subdural; delayed; meningioma; gamma knife; radiosurgery
First described by Roy in 1884, post-traumatic acute extradural hematoma (EDH) is a life-threatening pathological entity, with a high risk of neurological sequelae and high mortality even after urgent surgical drainage [1,2]. It is usually unilateral, in only 2%–10% of cases it is bilateral [3]. Delayed EDHs are even rarer, and only a few reports can be found in literature [4,5]. Only one case of triple post-traumatic EDH had been reported [6].
Acute subdural hematoma (SDH) is a hemorrhage between the dura mater and arachnoid [7,8]. A bilateral subdural hematoma is a rare finding, usually associated with challenging surgical management and postoperative sequelae [7]. Concomitant acute EDH and SDH is also a rare entity [9–16], and a bilateral onset has not yet been reported in literature.
In managing patients affected by severe traumatic brain injury (TBI), the medical staff should consider the risk of the development of delayed hematomas, both acute and chronic [6,17–19].
We present the first report of a patient affected by post-traumatic concomitant EDH and SDH, with the contralateral, delayed onset of another, associated with meningioma previously treated with gamma knife.
A 60-year-old woman with a history of epilepsy since childhood, arterial hypertension, and incidental diagnosis of meningiomatosis was referred to our department after falling down the stairs. Four years before, the patient had undergone gamma knife treatment of the right frontal convexity meningioma (5.1 cm3) and a smaller falx meningioma (527.1 mm3) (12 Gy-40% and 14 Gy-50%, respectively) (Fig. 1).

Figure 1: Axial post-gadolinium enhancement T1-weighted MR images showing a right frontal convexity meningioma (A) and a right anterior parafalx meningioma (B)
The patient was admitted to our emergency department with a Glasgow Coma Scale (GCS) score of 7/15 and isochoric, myotic pupils. An immediate head CT scan revealed a small acute SDH in the right hemisphere and an acute blood collection in the left hemisphere, which exerted mass effect on the brain, with contralateral midline shift (Fig. 2).
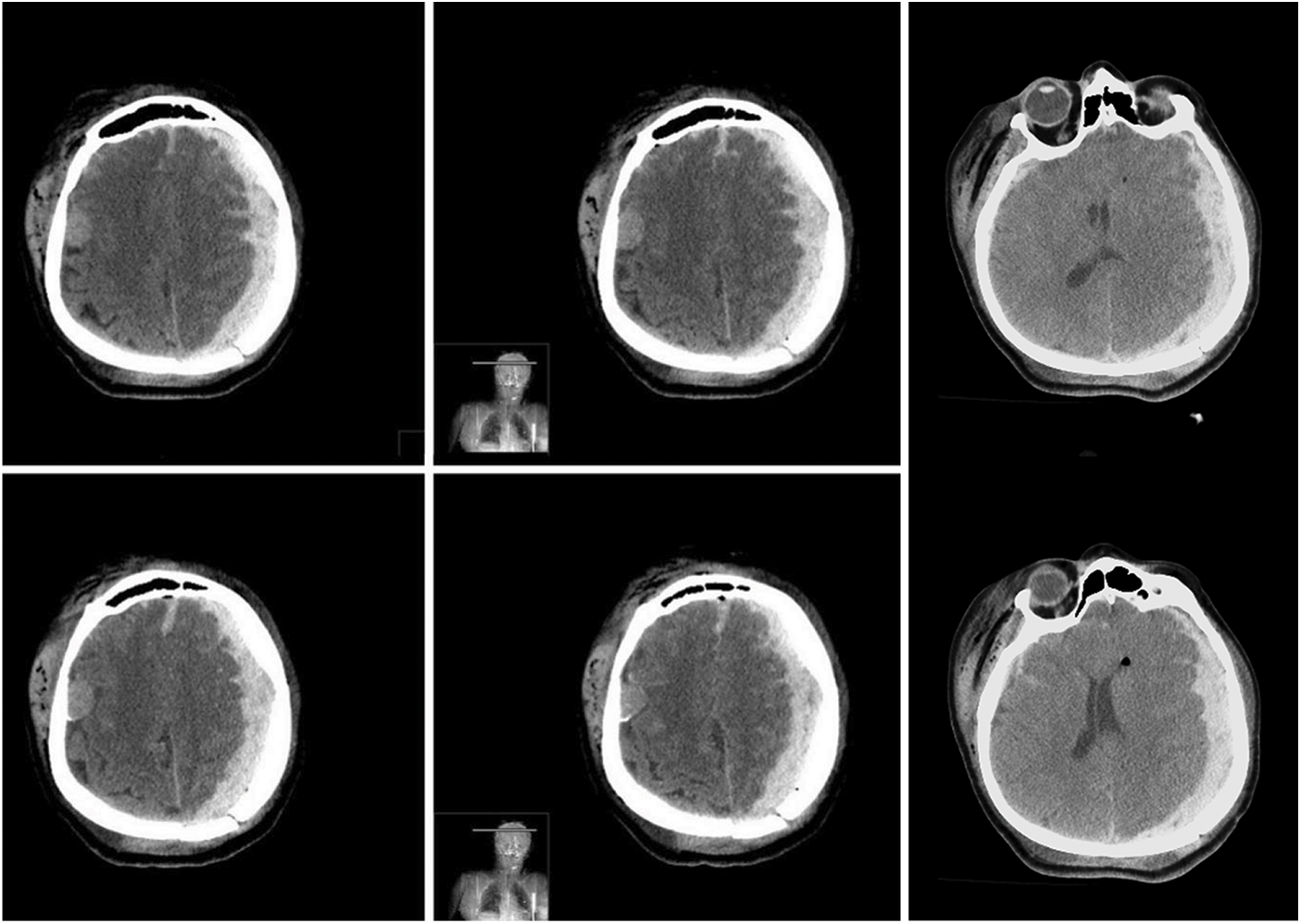
Figure 2: Pre-operative axial brain CT scan images in series showing a small right hemispheric acute subdural hematoma and a left hemispheric acute subdural hematoma (extradural blood component found intraoperatively), which exerted mass effect on the brain, with contralateral midline shift
Furthermore, we found a complex skull fracture across the superior sagittal sinus, the right frontal bone, and the left parieto-occipital bones with dislocation of fragments (Fig. 3).
Figure 3: Pre-operative brain CT scan with three-dimensional reconstruction showing a complex skull fracture across the superior sagittal sinus, the right frontal bone, and the left parieto-occipital bones with dislocation of fragments
A left decompressive craniectomy was performed, and a substantial epidural blood collection was removed. Once the dura mater was opened, a concomitant massive acute SDH was detected and removed. During surgery, the brain showed progressive swelling, which made replacing the bone flap impossible. We performed a duroplasty and skin closure, as usual, along with a subgaleal drain. Due to the patient’s right anisocoria, an urgent postoperative CT scan was needed, which revealed a massive blood collection in the right hemisphere, with left midline shift (Fig. 4).
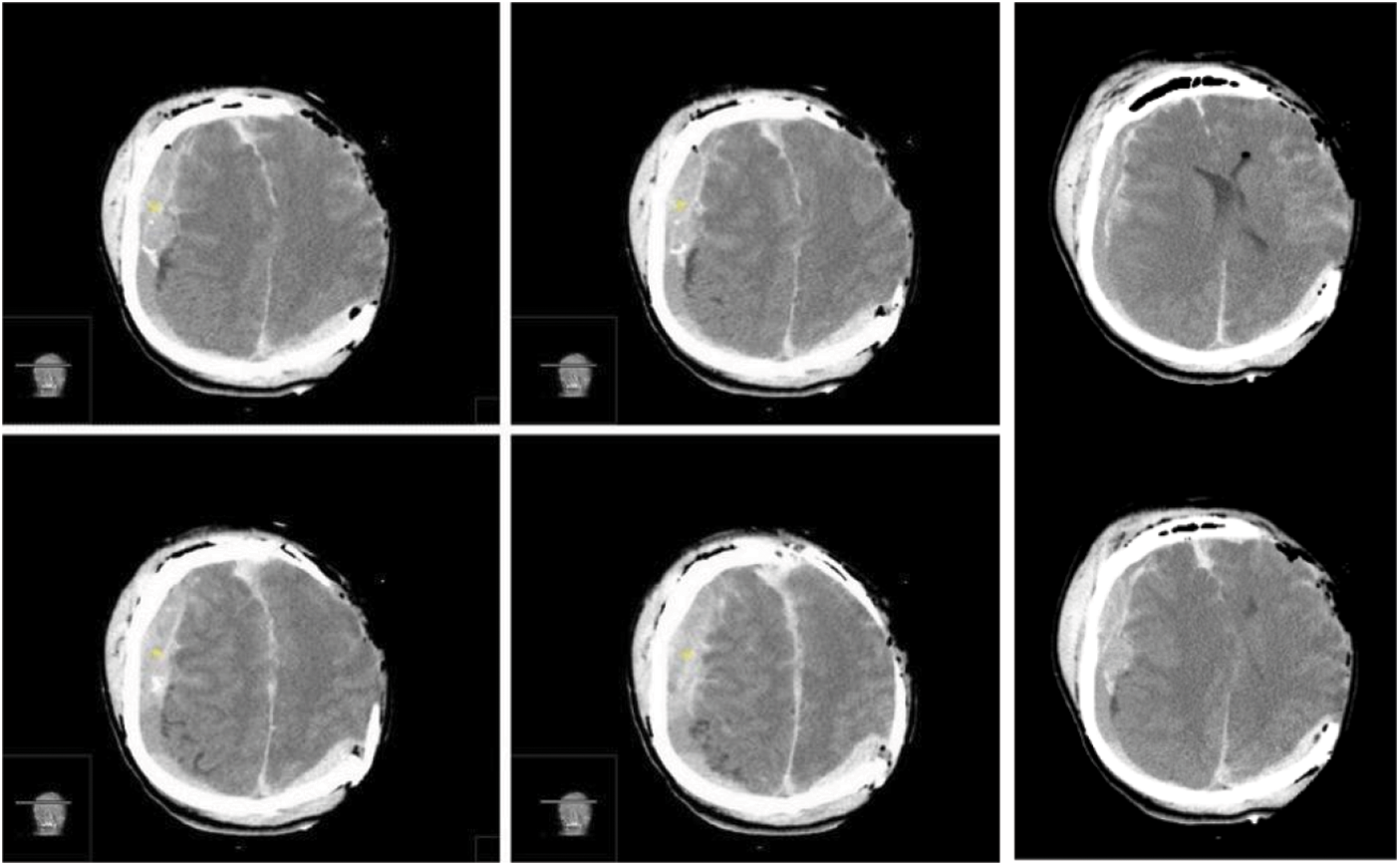
Figure 4: Immediate post-operative brain CT scan images in series revealing a massive concomitant right hemispheric acute extra-subdural hematoma, with left midline shift. In this case the “CT comma sign” and the detached dura are visible in the axial sequences (Yellow asterisks)
The patient underwent a second urgent surgery, during which we performed a right trauma flap, showing a concomitant acute EDH and SDH, which was removed. We also removed the right frontal convexity meningioma and its dural implant, sent for histological examination that documented a WHO Grade I psammomatous meningioma (Fig. 5).
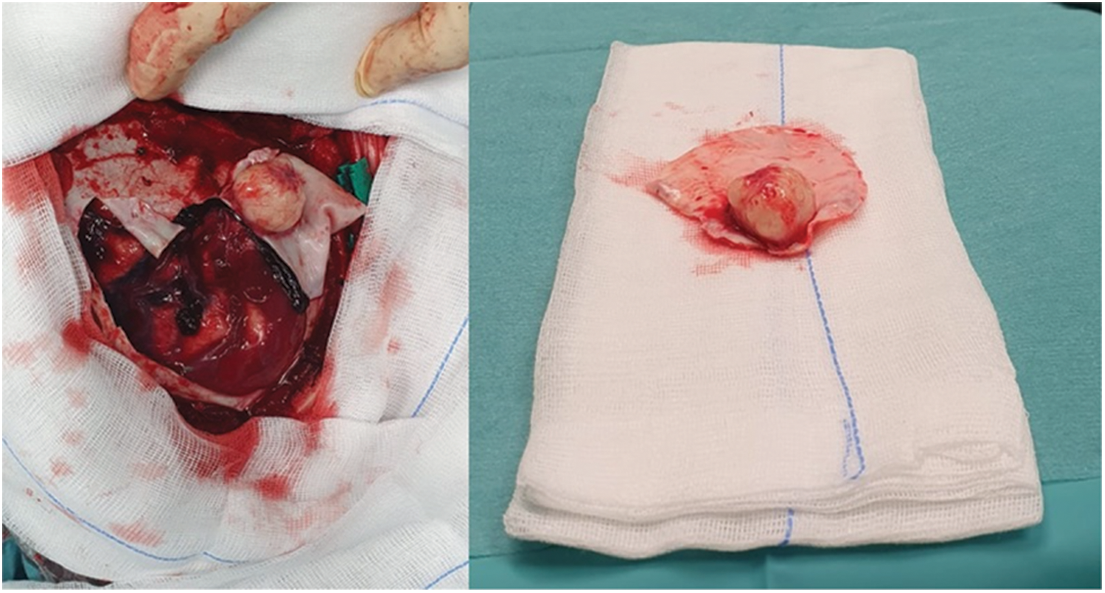
Figure 5: Intraoperative findings showing concomitant acute extradural and subdural hematoma and the small convexity meningioma without arachnoid adhesions, and excised en bloc with the surrounding dura
We completed the procedure with satisfying hemostasis, duroplasty, and repositioning of the bone flap; also in this case, a subgaleal drain was placed. After surgery, the patient was isochoric again, and a further postoperative CT scan revealed common postoperative findings and a proper brain decompression (Fig. 6).
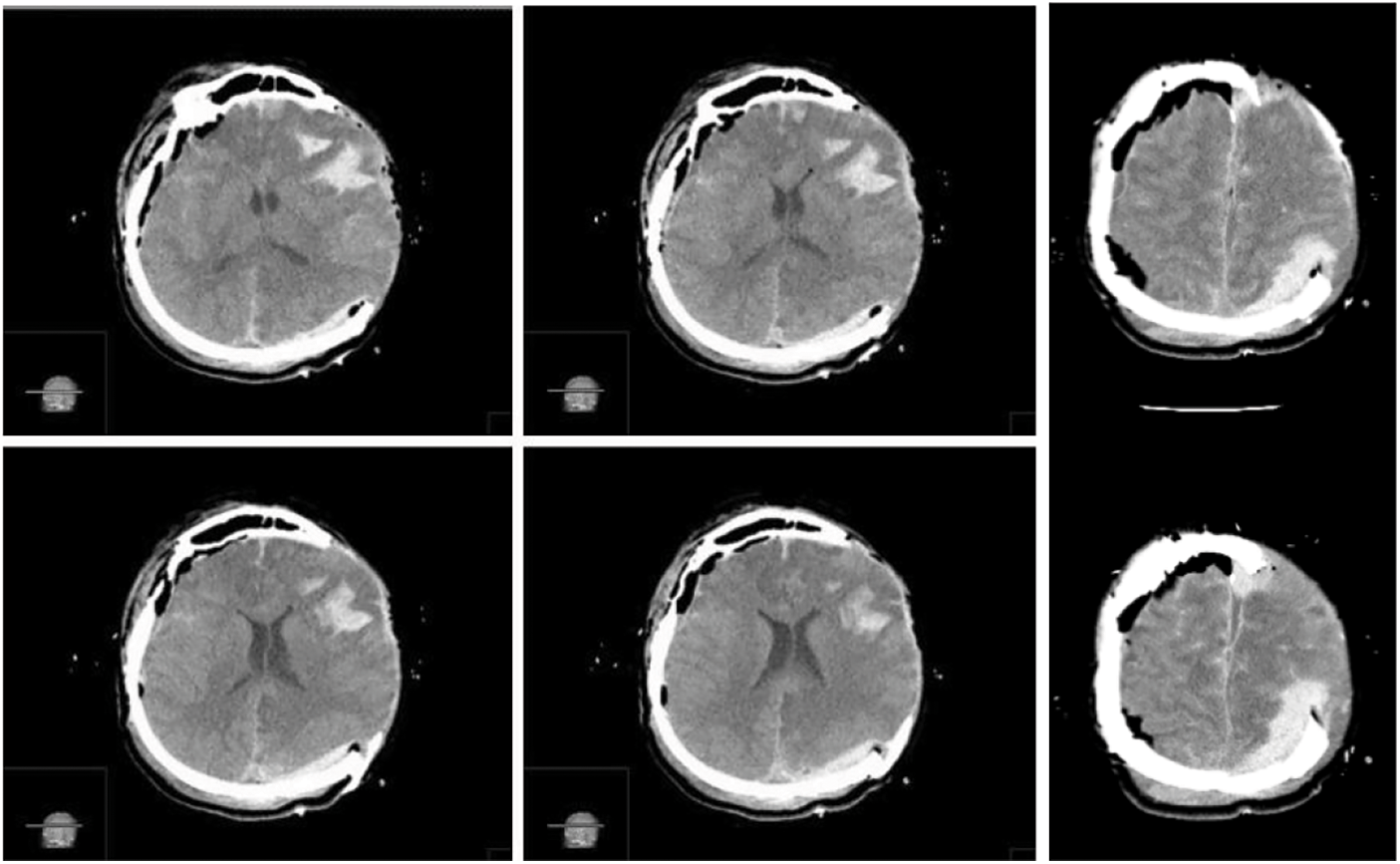
Figure 6: Postoperative CT scan images in series showing common postoperative findings and a bilateral proper brain decompression
After 5 days in the intensive care unit (ICU), the patient died because she presented an acute heart failure.
The development of an EDH due to the coup injury and an SDH as a contrecoup traumatism represents a common finding in brain traumatology [9–11,13,14,16]. Concomitant acute EDH and SDH is a rare finding [9–16], and, to our knowledge, this is the first bilateral case reported in literature. It is difficult to determine the coup-contrecoup in such concomitant cases even because there is an association with complex skull fractures and diffuse soft tissue damage. To demonstrate this, it was not possible, in our patient, to detect the concomitant EDH and SDH, which was an intraoperative finding. Moreover, we could not detect the characteristic “CT comma sign” [7,11,20], probably because of the diffuse brain and skull damage, with the hematoma also distributed in the interhemispheric fissure; the mechanism of blood distribution instead of collection was favored by unstable fracture fragments [10]. The current availability of CT scan, even in the intraoperative setting, allows to better detect known hematomas or the development of delayed hemorrhages, especially when radiological examination can be performed early after trauma and after surgery [6,21,22].
Interestingly, in our case, the delayed concomitant acute EDH/SDH caused severe neurological signs with right anisocoria, despite the decompressive craniotomy already performed in the contralateral side, configuring a worse neurological status that the initial hemorrhage. Thus, delayed hematoma must be strictly evaluated, expected, and managed carefully, especially when complex fractures across major dural sinuses are present.
As in every TBI patient, the clinical outcome is related to the initial neurological condition, the entity of the brain damage–including diffuse axonal injury (DAI) or contusions in eloquent areas–and the surgical timing [9–10,23,24]. Finally, an acute SDH caused by bleeding of a meningioma has been reported in literature, but we report the unique case in which the meningioma is not the cause of the bleeding, but a concomitant pathology, and the hematomas have a post-traumatic etiology.
In literature, acute SDHs have been associated with both spontaneous (i.e., caused by aneurysm, coagulation deficits) [25–27] and traumatic causes in patients affected by tumors, like meningioma, which bled after trauma [28]. Unlike those already reported, our case presented a massive acute EDH on the left and a small acute SDH on the right, clearly caused by trauma and brain decompression after the evacuation of the contralateral concomitant EDH/SDH, without bleeding from the meningioma itself. The upfront treatment of meningiomas with GK or other types of radio surgery is a daily practice, and the main goal is tumor growth control [29–31]. The present report may suggest a role of radio surgery, since the meningioma had been treated with gamma knife 4 years before, but the regressive events associated with radiosurgery makes bleeding from the meningioma less likely. Gk treatment appears to protect from meningioma’s bleeding, even after high energy trauma, thus confirming the safety of radiosurgery, that protect from tumor growth and for bleeding as well.
We report the first case of bilateral, concomitant, acute EDH and SDH treated with urgent surgery, with the occasional removal of a meningioma unrelated to the bleeding. The development of a contralateral delayed EDH/SDH must be considered in severe traumatic patients, especially if associated fractures across major dural sinuses are present. Intraoperative CT scan, if available, or immediate postoperative CT scan is mandatory for adequate management of complex neurotrauma cases. GK may reduce the risk of bleeding of meningiomas even after sever brain trauma.
Author’s Contributions: Conceptualization, G.E.U. and A.C.; methodology, G.E.U. and G.S.; software, G.S.; validation, L.C., D.F., M.F., F.G., G.F.N. and S.C.; formal analysis, G.F.; investigation, A.C. and G.S.; resources, G.F.; data curation, A.C., G.S. and M.G.T.; writing—original draft preparation, G.E.U., G.S. and A.C.; writing—review and editing, G.E.U. and G.S.; visualization, S.C., G.F.N.; supervision, B.C., V.C.; project administration, G.E.U.; funding acquisition, G.F. All authors have read and agreed to the published version of the manuscript.
Ethics Approval and Consent to Participate: Not applicable.
Consent for Publication: Written informed consent was obtained from the patient for publication of this case report and accompanying images.
Availability of Data and Material: Not applicable.
Funding Statement: The authors received no specific funding for this study.
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
1. Roy, G. C. (1884). Fracture of skull, extensive extravasation of blood on dura mater, producing compression of brain, trephining, partial relief of symptoms, death. Lancet, 2, 319. [Google Scholar]
2. Rosenthal, A. A., Solomon, R. J., Eyerly-Webb, S. A., Sanchez, R., Lee, S. K. et al. (2017). Traumatic epidural hematoma: Patient characteristics and management. The American Surgeon, 83(11), e438–e440. DOI 10.1177/000313481708301108. [Google Scholar] [CrossRef]
3. Dharker, S. R., Bhargava, N. (1991). Bilateral epidural haematoma. Acta Neurochirurgica, 110, 29–32. DOI 10.1007/BF01402044. [Google Scholar] [CrossRef]
4. Rochat, P., Johannesen, H. H., Poulsgård, L., Bøgeskov, L. (2002). Sequentially evolved bilateral epidural haematomas. Clinical, Neurology and Neurosurgery, 105(1), 39–41. DOI 10.1016/S0303-8467(02)00099-9. [Google Scholar] [CrossRef]
5. Eftekhar, B., Ketabchi, E., Ghodsi, M., Esmaeeli, B. (2003). Bilateral asynchronous acute epidural hematoma: A case report. BMC Emergency Medicine, 3(1), 1. DOI 10.1186/1471-227X-3-1. [Google Scholar] [CrossRef]
6. Fricia, M., Umana, G. E., Scalia, G., Raudino, G., Passanisi, M. et al. (2020). Posttraumatic triple acute epidural hematomas: First report of bilateral synchronous epidural hematoma and a third delayed. World Neurosurgery, 133, 212–215. DOI 10.1016/j.wneu.2019.10.009. [Google Scholar] [CrossRef]
7. Agrawal, A. (2010). Bilateral biconvex frontal chronic subdural hematoma mimicking extradural hematoma. Journal of Surgical Technique and Case Report, 2(2), 90–91. DOI 10.4103/2006-8808.73625. [Google Scholar] [CrossRef]
8. Mori, K., Maeda, M. (2001). Surgical treatment of chronic subdural hematoma in 500 consecutive cases: Clinical characteristics, surgical outcome, complications, and recurrence rate. Neurologia Medica Chirurgica, 41(8), 371–381. DOI 10.2176/nmc.41.371. [Google Scholar] [CrossRef]
9. Agrawal, A., Hegcde, K., Reddy, V. (2016). The “CT comma sign” in concurrent extradural and hyperacute subdural hematomas is revisited. West African Journal of Radiology, 23(1), 52–53. DOI 10.4103/1115-3474.155748. [Google Scholar] [CrossRef]
10. Gupta, R., Mohindra, S., Verma, S. K. (2008). Traumatic ipsilateral acute extradural and subdural hematoma. Indian Journal of Neurotrauma, 5(2), 113–114. DOI 10.1016/S0973-0508(08)80011-1. [Google Scholar] [CrossRef]
11. Monsalve, G. A. (2007). The “CT comma sign” in head trauma: Concurrent epidural and subdural acute intracranial hematomas. Journal of Trauma and Acute Care Surgery, 63(1), 195–196. DOI 10.1097/TA.0b013e318067e2c9. [Google Scholar] [CrossRef]
12. Baratham, G., Dennyson, W. G. (1972). Delayed traumatic intracere-bral haemorrhage. Journal of Neurology Neurosurgery and Psychiatry, 35(5), 698–706. DOI 10.1136/jnnp.35.5.698. [Google Scholar] [CrossRef]
13. Sharma, A. K., Diyora, B. D., Shah, S. G., Pandey, A. K., Mamidanna, R. (2005). An extradural and subdural hematoma in a neonate. Indian Journal Pediatry, 72(3), 269. [Google Scholar]
14. Ghosh, A., Barma, R., Sharma, T., Chakrobarty, M. (2017). Case report coexisting traumatic ipsilateral extra and subdural hematoma-is it really common? Open Access Journal of Neurology and Neurosurgery, 3, 555614. DOI 10.19080/OAJNN. [Google Scholar] [CrossRef]
15. Indira Devi, B., Arivazhagan, A., Sattur, M. G., Kolluri, S. V. R. (2007). Con-comitant post-traumatic craniospinal multicompartmental hematoma associated with posterior fossa extradural hematoma—Case report and review of literature. Indian Journal of Neurotrauma, 4(1), 55–57. DOI 10.1016/S0973-0508(07)80014-1. [Google Scholar] [CrossRef]
16. Madhugiri, V. S., Arimappamagan, A., Chandramouli, B. A. (2012). Trau-matic epidural and subdural hematomas and extensive brain infarcts in a patient with pial arteriovenous malformation: Mechanisms underlying clinical and radiological findings. Asian Journal of Neurosurgery, 7(4), 210–213. DOI 10.4103/1793-5482.106657. [Google Scholar] [CrossRef]
17. Umana, G. E., Cristaudo, C., Scalia, G., Passanisi, M., Corsale, G. et al. (2020). Chronic epidural hematoma caused by traumatic intracranial pseudoaneurysm of the middle meningeal artery: Review of the literature with a focus on this unique entity. World Neurosurgery, 136, 198–204. DOI 10.1016/j.wneu.2019.12.179. [Google Scholar] [CrossRef]
18. Umana, G. E., Chiriatti, S., Fricia, M., Alberio, N., Cicero, S. et al. (2020). Letter to the editor regarding “Twist drill procedure for chronic subdural hematoma evacuation-An analysis of predictors for treatment success”. World Neurosurgery, 139, 698. DOI 10.1016/j.wneu.2020.04.061. [Google Scholar] [CrossRef]
19. Umana, G. E., Chiriatti, S., Roca, E., Scaliac, G., Fricia, M. et al. (2020). New tools in percutaneous minimally invasive chronic subdural hematomas evacuation. Interdisciplinary Neurosurgery, 21, 100736. DOI 10.1016/j.inat.2020.100736. [Google Scholar] [CrossRef]
20. Agrawal, A., Kiran Kumar, V. A., Sai Kiran, N. A., Anil Kumar, V., Prithvi Raj, B. (2019). Concomitant overlapping acute extradural and subdural hematoma. Indian Journal of Neurotrauma, 16(1), 71–74. DOI 10.1055/s-0039-1696785. [Google Scholar] [CrossRef]
21. Chang, E. F., Meeker, M., Holland, M. C. (2006). Acute traumatic intraparenchymal hemorrhage: Risk factors for progression in the early post-injury period. Neurosurgery, 58(4), 647–656. DOI 10.1227/01.NEU.0000197101.68538.E6. [Google Scholar] [CrossRef]
22. Chen, H., Guo, Y., Chen, S. W., Wang, G., Cao, H. L. et al. (2012). Progressive epidural hematoma in patients with head trauma: Incidence, outcome, and risk factors. Emergency Medicine International, 2012, 134905. DOI 10.1155/2012/134905. [Google Scholar] [CrossRef]
23. Agrawal, A. (2011). Bilateral symmetrical parietal extradural hematoma. Journal of Surgical Technicque and Case Reports, 3(1), 34–36. DOI 10.4103/2006-8808.78469. [Google Scholar] [CrossRef]
24. Agrawal, A., Agrawal, C., Kumar, A., Adhikari, S. (2007). Outcome of traumatic extradural haematoma managed surgically: Ourexperience. Nigerian Journal of Orthopaedic Trauma, 6, 74–76. [Google Scholar]
25. Boujemâa, H., Góngora-Rivera, F., Barragán-Campos, H., Karachi, K., Chiras, J. et al. (2006). Bilateral acute subdural hematoma from ruptured posterior communicating artery aneurysm: A case report. Interventional Neuroradiology, 12(1), 37–40. DOI 10.1177/159101990601200107. [Google Scholar] [CrossRef]
26. Mansour, O., Hassen, T., Fathy, S. (2014). Acute aneurismal bilateral subdural haematoma without subarachnoid haemorrhage: A case report and review of the literature. Case Reports in Neurological Medicine, 2014, 260853. DOI 10.1155/2014/260853. [Google Scholar] [CrossRef]
27. Garbossa, D., Altieri, R., Specchia, F. M., Agnoletti, A., Pilloni, G. et al. (2014). Are acute subdural hematomas possible without head trauma? Asian Journal of Neurosurgery, 9(4), 218–222. DOI 10.4103/1793-5482.146612. [Google Scholar] [CrossRef]
28. Moriyama, E., Beck, H., Takayama, K., Okamoto, T. (1998). Acute traumatic subdural hematoma originating from a convexity meningioma--Case report. Neurologia Medico Chirurgica, 38(1), 20–23. DOI 10.2176/nmc.38.20. [Google Scholar] [CrossRef]
29. Barone, F., Inserra, F., Scalia, G., Ippolito, M., Cosentino, S. et al. (2021). 68Ga-DOTATOC PET/CT follow up after single or hypofractionated gamma knife ICON radiosurgery for meningioma patients. Brain Sciences, 11(3), 375. DOI 10.3390/brainsci11030375. [Google Scholar] [CrossRef]
30. Umana, G. E., Raudino, G., Alberio, N., Inserra, F., Giovinazzo, G. et al. (2020). Slit-like hypertensive hydrocephalus: Report of a late, complex, and multifactorial complication in an oncologic patient. Surgical Neurology International, 11, 219. DOI 10.25259/SNI_145_2020. [Google Scholar] [CrossRef]
31. Giammalva, G. R., Gagliardo, C., Marrone, S., Paolini, F., Gerardi, R. M. et al. (2021). Focused ultrasound in neuroscience. State of the art and future perspectives. Brain Sciences, 11(1), 84. DOI 10.3390/brainsci11010084. [Google Scholar] [CrossRef]
 | This work is licensed under a Creative Commons Attribution 4.0 International License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. |