
 | Oncologie |  |
DOI: 10.32604/Oncologie.2021.016420
ARTICLE
Effect of Cluster Nursing Mode Combined with Blood Pressure Regulation on Surgical Tolerance of Patients with Esophageal Cancer and Hypertension
1Department of Gastroenterology, Linyi Central Hospital, Linyi, 276400, China
2Department of Geriatrics, The Fifth People’s Hospital of Qingdao, Qingdao, 266002, China
*Corresponding Author: Hongyan Ai. Email: lxfahy@163.com
Received: 04 March 2021; Accepted: 18 May 2021
Abstract: Objective: To explore the effect of the cluster nursing mode combined with blood pressure regulation on the surgical tolerance of patients with esophageal cancer and hypertension. Methods: The clinical data of 86 patients with esophageal cancer and hypertension treated in our hospital (February 2016–February 2017) were retrospectively analyzed. The patients were randomly split into research group and reference group, with 43 cases in each group. The reference group received routine nursing, while the research group received cluster nursing combined with blood pressure regulation. The SBP, DBP and heart rates at D1 (at admission), D2 (2 h before surgery) and D3 (2 h after surgery) were compared between the two groups. In addition, the surgical tolerance, ESCA scores at 1 month after discharge, personality and behavior characteristics before and after intervention, and incidence of postoperative complications were also compared between the two groups. Results: With no obvious difference in SBP, DBP and heart rates at D1 between the two groups (P > 0.05), the SBP, DBP and heart rates at D2 and D3 in the research group were obviously lower compared with the reference group (P < 0.001). With no obvious difference in the number of patients with surgical tolerance of Grades I, II and III after intervention between two groups (P > 0.05), the number of patients with surgical tolerance of Grade IV in the research group was significantly higher than that in the reference group (P < 0.05). The scores of self-concept, self-care skills, self-care responsibility and health knowledge in the research group at 1 month after discharge were obviously higher compared with the reference group (P < 0.001). The scores of EPQ-L (lie), EPQ-P (psychoticism) and EPQ-N (neurosism) after intervention in both groups were obviously lower compared with those before intervention (P < 0.001), and the scores of EPQ-L, EPQ-P and EPQ-N after intervention in the research group were significantly lower than those in the reference group (P < 0.001). The total incidence of postoperative complications in the research group was significantly lower compared with the reference group (P < 0.05). Conclusion: Cluster nursing combined with blood pressure regulation can significantly improve the surgical tolerance of patients with esophageal cancer and hypertension and enhance the self-care ability after surgery, with obvious therapeutic effect, which is worthy of promotion and application.
Keywords: Cluster nursing; blood pressure regulation; esophageal cancer; hypertension; surgical tolerance
Esophageal cancer is a common malignant disease of esophageal epithelium [1]. Epidemiological studies have found that the prevalence of esophageal cancer in China is on the rise year by year, mostly in men aged 40–80 years old, with a higher incidence in urban areas than that in rural areas [2]. At present, the cause of esophageal cancer has not been found in the medical community, which may be related to nitrite, fungaltoxin, genetic factors, etc. Besides, local inflammation and stimulation caused by long-term consumption of too hot food is also one of the important risk factors for esophageal cancer [3–5]. With no significant symptoms in the early stage but choking when eating, this disease is characterized by dysphagia and obvious emaciation in the middle and late stages during which the esophageal cancer tissues will involve the whole esophagus of patients by penetrating the esophageal wall and invading adjacent organs [6–8]. Radical surgery for esophageal carcinoma is a common method to treat this disease, but a large number of data showed that most patients would have fear and tension before surgery and worry about the changes in physical function after surgery. In addition, their own hypertension also affects the surgery. Therefore, effective interventions in the perioperative period are of great significance to ensure the smooth implementation of the surgery, improve the treatment effect, and reduce postoperative complications [9–11]. Cluster nursing mode is a new nursing measure developing based on the concept of evidence-based medicine and focusing on the scientificity in clinical practice, which can effectively alleviate patients’ negative emotions, reduce the incidence of various complications, improve prognosis, and provide high-quality nursing services for inpatients. Since hypertension will increase systemic stress response and surgical risk, blood pressure control in patients with hypertension before surgery should be carried out to reduce surgical risk and improve safety [12]. Based on this, the study was aimed to further explore the effect of cluster nursing combined with blood pressure regulation on surgical tolerance of patients with esophageal cancer and hypertension, reported as follows.
The clinical data of 86 patients with esophageal cancer and hypertension treated in Linyi Central hospital (February 2016–February 2017) were retrospectively analyzed. The patients were randomly split into research group and reference group, with 43 cases in each group. The research group had 25 males and 18 females aged 43–71 years old with an average age of (49.33 ± 5.82) years old, including 16 cases of squamous-cell carcinomas, 14 cases of adenocarcinomas, 7 cases of adenosquamous carcinomas and 6 cases of mucoepidermoid carcinomas. As for TNM staging, 16 patients were in Stage I, 19 in Stage II and 8 in Stage III, with a hypertension course of 2–9 years and an average disease course of (5.38 ± 1.38) years. 14 patients had mild hypertension, 22 patients had moderate hypertension and 7 patients had severe hypertension. The reference group had 24 males and 19 females aged 45–73 years old with an average age of (49.38 ± 5.78) years old, including 14 cases of squamous-cell carcinomas, 13 cases of adenocarcinomas, 9 cases of adenosquamous carcinomas and 7 cases of mucoepidermoid carcinomas. As for TNM staging 15 patients were in Stage I, 20 in Stage II and 8 in Stage III, with a hypertension course of 3–11 years and an average disease course of (5.43 ± 1.35) years. 17 patients had mild hypertension, 20 patients had moderate hypertension and 6 patients had severe hypertension. There was no obvious difference in the general clinical data between two groups (P > 0.05), indicating comparability. The study obtained the approval of the Hospital Ethics Committee (No. 20160122), and the patients and their family members knew purpose and process of the study, and signed the informed consent.
(1) The patients met the diagnostic criteria for esophageal cancer and were diagnosed with different degrees of hypertension. (2) The expected survival time of patients was no less than 6 months. (3) The patients received radical surgery for esophageal carcinoma.
(1) The patients had surgical contraindication. (2) The patients had abnormal systemic coagulation. (3) The patients had organic lesions in brain, kidney and liver. (4) The patients had cognitive disorders or language communication barrier.
The reference group received routine nursing by informing the patients of the precautions during surgery, monitoring their vital signs after surgery, regular ward rounds, and formulation of scientific dietary plans with less salt intake. In addition, the patients were advised to take medicine on time, keep warm, and maintain adequate sleep [13–15].
The research group received cluster nursing combined with blood pressure regulation. A special cluster nursing group consisting of head nurses and senior nurses was established to provide perioperative nursing for patients, mainly including ward nursing, psychological nursing, dietary intervention, preoperative nursing, intraoperative nursing, etc. (1) Ward nursing. The nursing staff kept the patients’ ward environment clean and tidy, and maintained the room temperature and humidity to create a comfortable treatment environment for patients and eliminate their fear of surgery. (2) Psychological nursing. The patients were informed of surgery-related knowledge through brochures, videos and other means to change their incorrect cognition, increase the treatment confidence, and stabilize their preoperative moods. Additionally, the staff patiently informed the patients of preoperative precautions and communicated with them frequently to establish a good doctor-patient relationship. (3) Dietary intervention. Scientific dietary plans were formulated for the patients based on their various physical indicators and postoperative rehabilitation to maintain nutritional balance and accelerate physical recovery. (4) Preoperative nursing. The patients were advised to eat liquid food before surgery, and were forbidden to use shaving equipment in case of infection. Clinical health education was carried out to inform the patients of disease-related knowledge and postoperative precautions, teach them self-care skills, and increase the awareness and understanding of their own diseases. (5) Intraoperative nursing. During surgery, dynamic monitoring of various vital signs including oxygen status was maintained, with attention to keeping warm. Aseptic operation was implemented to prevent intraoperative infection.
Blood pressure regulation. Medication cards were made according to the patients’ blood pressure to mark the medication time, dosage and precautions for hypertension. The blood pressure was measured for 3 times a day and the drugs were timely adjusted according to the fluctuation of blood pressure [16].
Systolic pressure (SBP), diastolic pressure (DBP) and heart rates were detected at admission (D1), 2 h before surgery (D2) and 2 h after surgery (D3) in both groups.
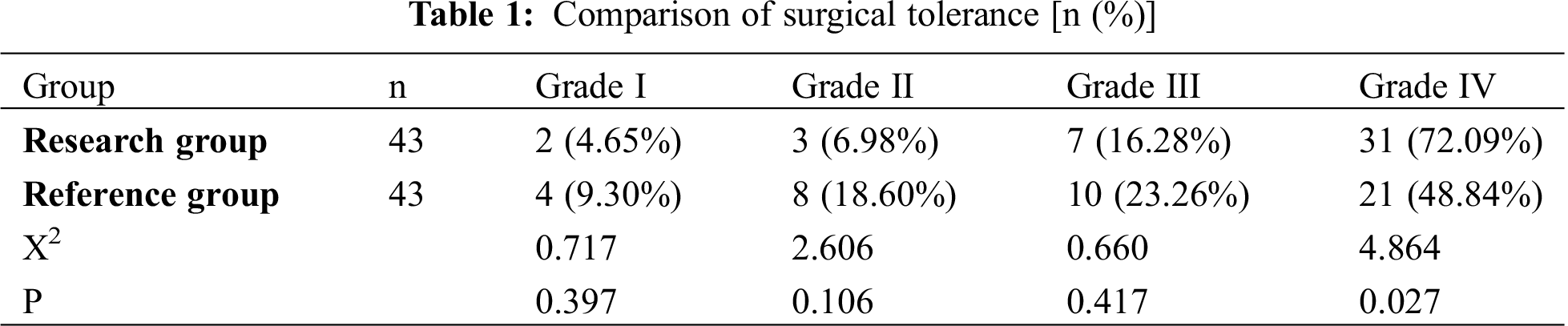
Referring to the criteria of literature [17], grade I referred to that the intolerance of the patients and strong physiological response led to the termination of the surgery; Grade II referred to that the patients could barely tolerate the surgery but the surgery could be implemented; Grade III was that the patients had slight discomfort and were basically tolerable to the surgery; and Grade IV was that patients were tolerable to the surgery.
The self-care ability of patients at 1 month after discharge was evaluated by the Exercise of Self-Care Agency (ESCA) [18], including four scoring aspects of self-concept, self-care skills, self-care responsibility and health knowledge, with each scoring 35 points. Higher scores indicated better self-care ability of patients.
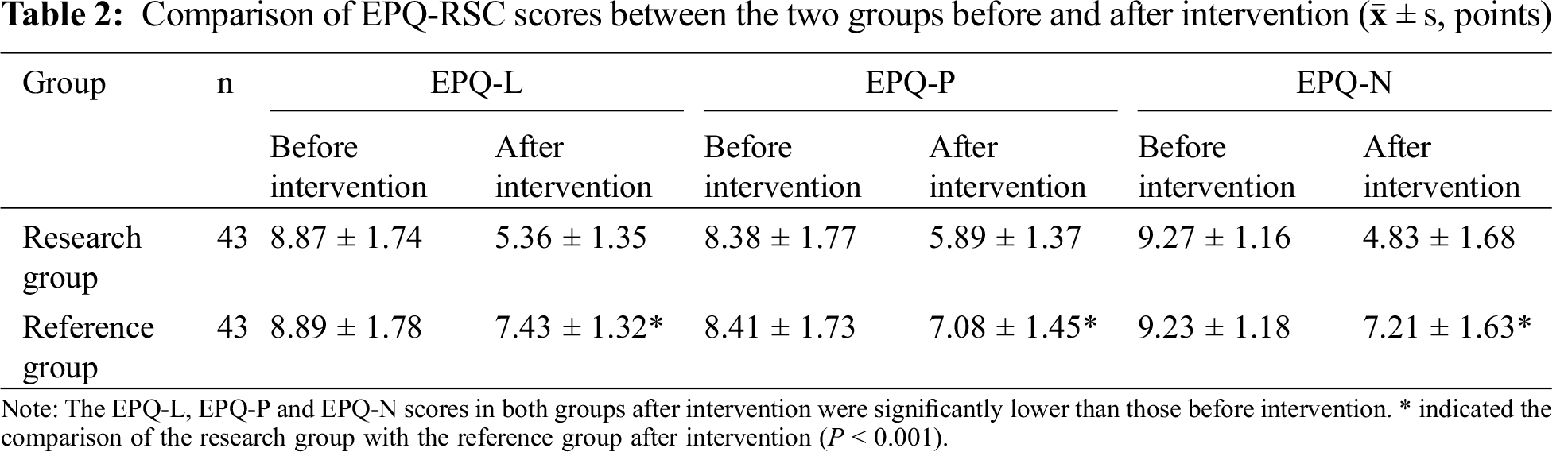
The EPQ-RSC [19] (Chinese version) was adopted to evaluate the personality and behavior characteristics before and after intervention, including three evaluation factors of EPQ-L (lie), EPQ-P (psychoticism) and EPQ-N (neurosism) with each scoring 12 points. Lower EPQ-N scores indicated more stable emotions, lower EPQ-P scores indicated more gentle moods and lower EPQ-L scores indicated weaker EPQ-L.
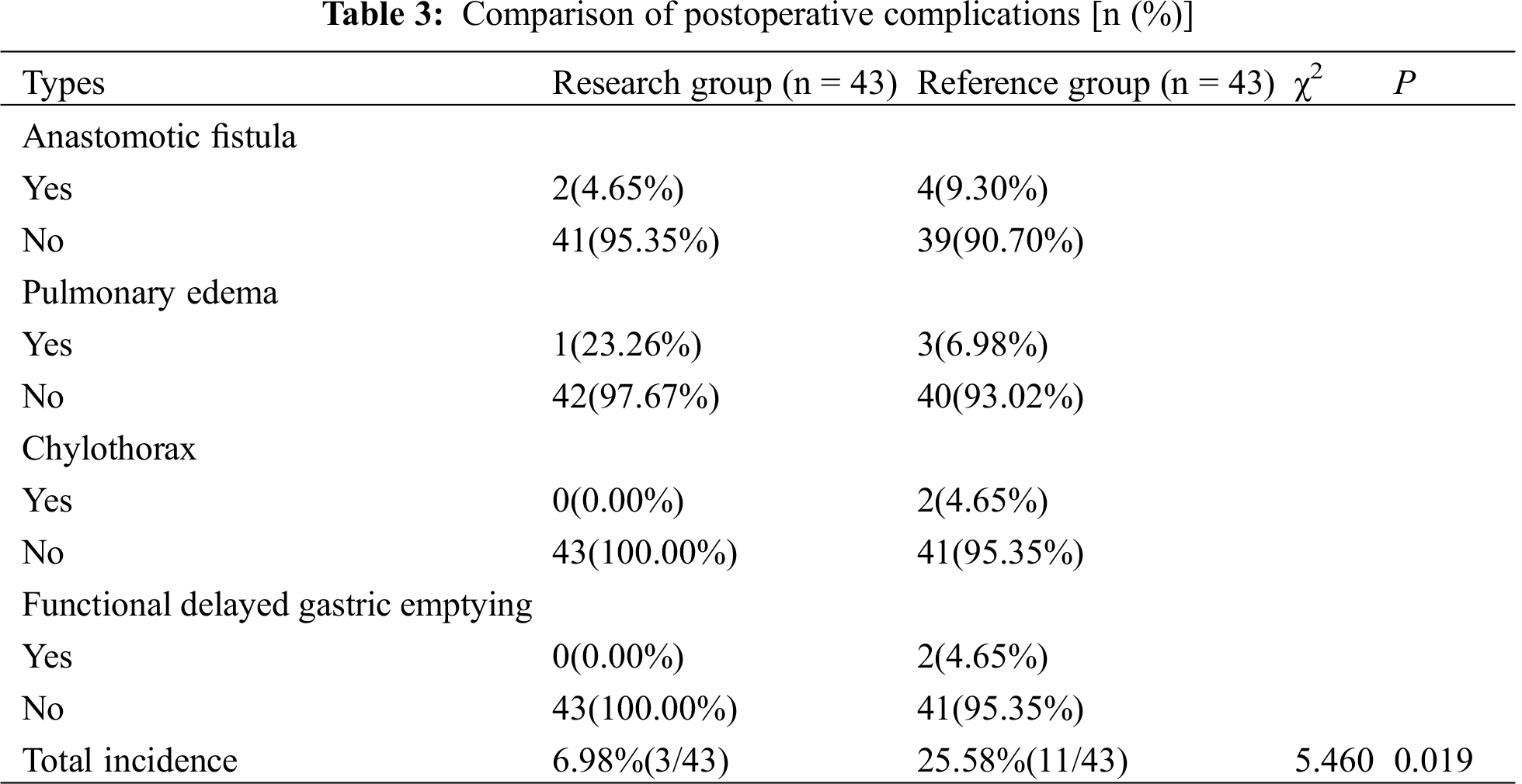
The postoperative complications were recorded and compared between the two groups.
SPSS21.0 software was adopted to analyze and process the data in the study. The measurement data were expressed by (
3.1 Comparison of SBP, DBP and Heart Rates
With no obvious difference in SBP, DBP and heart rates at D1 between two groups (P > 0.05), the SBP, DBP and heart rates at D2 and D3 in the research group were obviously lower compared with the reference group (P < 0.05), as shown in Figs. 1–3.
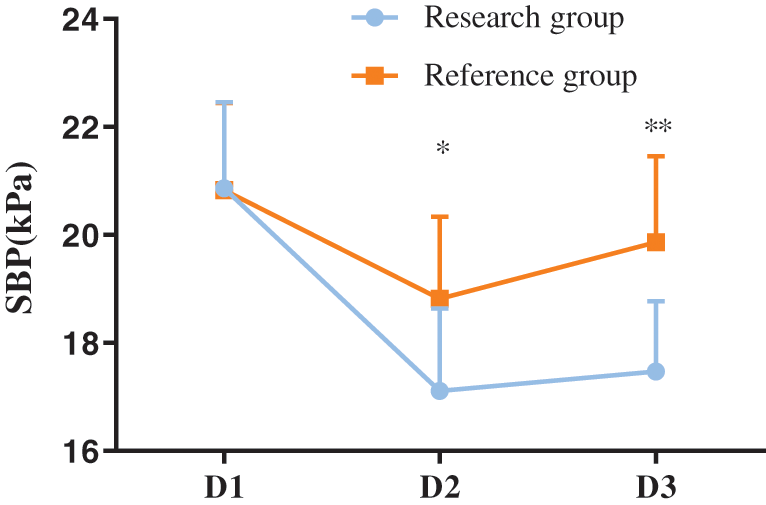
Figure 1: Comparison of SBP at different time points between the two groups (
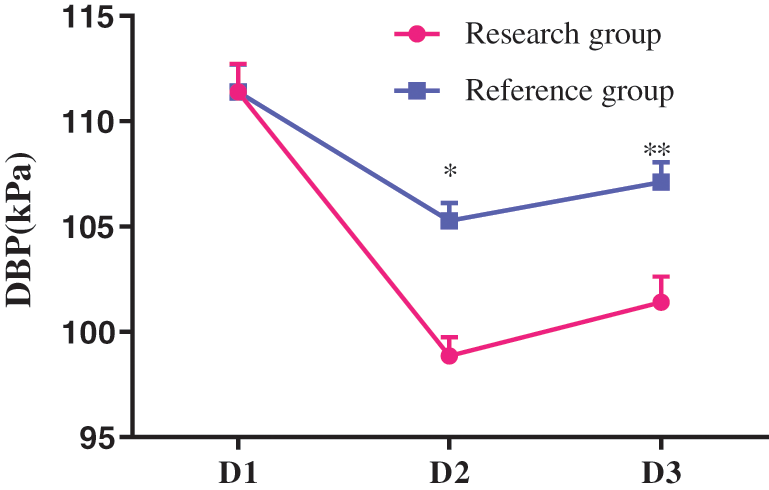
Figure 2: Comparison of DBP at different time points between the two groups (
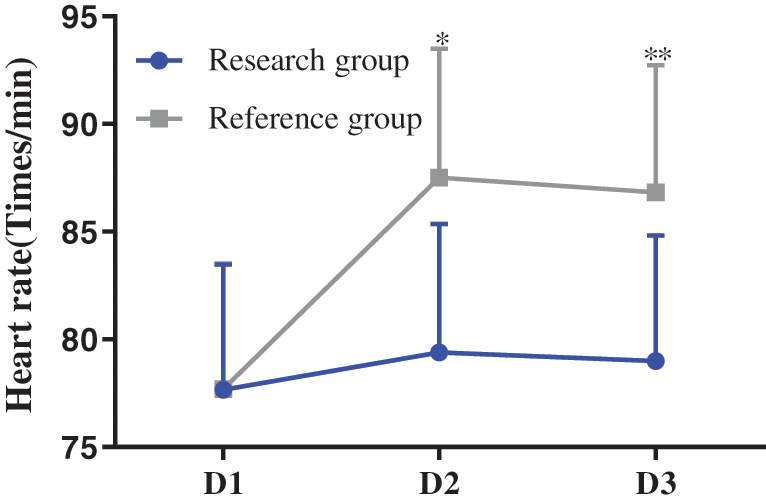
Figure 3: Comparison of heart rates at different time points between the two groups (
3.2 Comparison of Surgical Tolerance
With no obvious difference in the number of patients with Grades I, II and III between the two groups (P > 0.05), the number of patients with grade IV in the research group was obviously higher compared with the reference group (P < 0.05), as shown in Tab. 1.
3.3 Comparison of the ESCA Scores between the Two Groups at 1 Month after Discharge
The scores of self-concept, self-care skills, self-care responsibility and health knowledge in the research group at 1 month after discharge were obviously higher compared with the reference group (P < 0.05), as shown in Fig. 4.
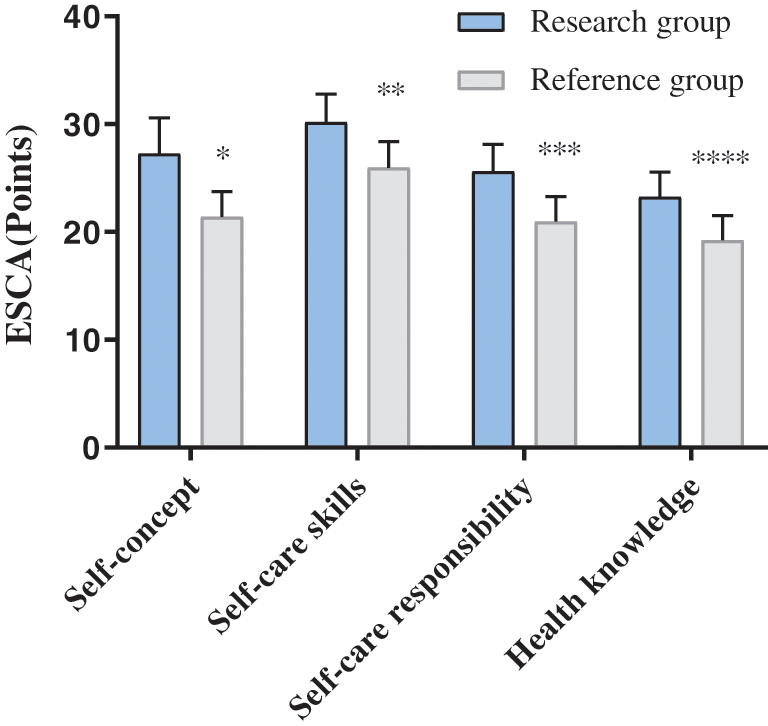
Figure 4: Comparison of ESCA scores between the two groups at 1 month after discharge (
3.4 Comparison of EPQ-RSC Scores between the Two Groups
The EPQ-L, EPQ-P and EPQ-N scores in both groups after intervention were obviously lower compared with those before intervention (P < 0.05), and the scores in the research group after intervention were obviously lower compared with those in the reference group (P < 0.05), as shown in Tab. 2.
3.5 Comparison of Postoperative Complications
The total incidence of postoperative complications in the research group was significantly lower than that in the reference group (P < 0.05), as shown in Tab. 3.
This study showed that the SBP, DBP and heart rates of patients were significantly improved after the implementation of the cluster nursing mode combined with blood pressure regulation. Leete et al. [20] have shown that hypertension can reduce the patients’ surgical tolerance which is also related with patients’ own emotions, psychological states, environment and other factors. Blood pressure regulation for patients before surgery can stabilize blood pressure, improve surgical tolerance, reduce stress response and ensure the surgical safety.
This study also demonstrated that the EPQ-L, EPQ-P and EPQ-N scores in the research group after intervention were obviously better than those in the reference group, suggesting that the cluster nursing mode combined with blood pressure regulation can significantly improve patients’ personality and behavior characteristics [21,22]. Psychologists believe that personality characteristics are a kind of psychological structure that can make people’s behavior disposition show stability, persistence and consistency, trigger and guide people’ behavior, and enable people to make the same response in the face of different types of stimulation. Therefore, patients with strong EPQ-L do not often communicate with others, are not good at expressing their emotions and are more likely to have adverse emotions when facing surgical stressors. Cluster nursing provides psychological counseling to patients with different personalities, masters their psychological changes through communication, listens carefully to their statements, and encourages them to release their negative emotions [23]. Huang et al. [24] have stated that cluster nursing intervention for patients with small cell carcinoma can improve their personality characteristics such as EPQ-L, EPQ-P and EPQ-N, thus improving their life quality after surgery. In this study, after the patients with esophageal cancer and hypertension received cluster nursing mode, the ESCA scores after intervention were significantly higher than those of patients with routine nursing (P < 0.001). This was because cluster nursing mode carried out preoperative clinical health education to inform the patients of their disease-related knowledge and enable them to learn self-care skills, increasing the understanding of their own diseases to some extent.
The study found that the surgical tolerance in the research group after intervention was significantly better than that in the reference group. Schutzenberger et al. [25] have pointed out in their study that after the implementation of cluster nursing combined with blood pressure regulation in the perioperative period of patients with colon cancer and hypertension, 27 patients with surgical tolerance of Grade IV in the research group were obviously more than 13 in the reference group, indicating that the intervention can significantly improve patients’ surgical tolerance and reduce their pain. Statistics and comparison of postoperative complications between the two groups showed that the total incidence of postoperative complications in the research group was significantly lower than that in the reference group (P < 0.05), possibly because cluster nursing mode started from many aspects of patients and reduced the risk of various factors affecting the surgical effect of patients through effective nursing intervention measures, so as to effectively control the occurrence of postoperative complications.
In conclusion, cluster nursing combined with blood pressure regulation in perioperative nursing of patients with esophageal cancer and hypertension can effectively improve their surgical tolerance and self-care ability after surgery, and reduce postoperative complications, which is worthy of popularization and application. This study also has some limitations such as the small number of selected cases, which may lead to bias in the research results. Therefore, the sample size should be further expanded to make the research results more objective and convincing.
Funding Statement: The authors received no specific funding for this study.
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
1. Men, K., Boimel, P., Janopaul-Naylor, J., Zhong, H., Huang, M. et al. (2018). Cascaded atrous convolution and spatial pyramid pooling for more accurate tumor target segmentation for rectal cancer radiotherapy. Physics in Medicine and Biology, 63(18), 185016. [Google Scholar]
2. Pittaka, M., Georgiou, C., Polyviou, P., Kountourakis, P., Loizou, P. et al. (2018). Fournier Gangrene in a patient receiving chemo-radiation for rectal cancer. Oxford Medical Case Reports, 2018(2), omx101. [Google Scholar]
3. Pan, H. D., Zhao, G., An, Q., Xiao, G. (2018). Pulmonary metastasis in rectal cancer: A retrospective study of clinicopathological characteristics of 404 patients in Chinese cohort. BMJ Open, 8(2), e019614. [Google Scholar]
4. Chapman, W. C., Choi, P., Hawkins, A. T., Hunt, S. R., Silviera, M. L. et al. (2018). Benchmarking rectal cancer care: institutional compliance with a longitudinal checklist. Journal of Surgical Research, 225, 142–147. [Google Scholar]
5. Mishra, N. (2018). Locally recurrent rectal cancer. Diseases of the Colon and Rectum, 61(6), 651–654. [Google Scholar]
6. Horvat, N., Petkovska, I., Gollub, M. J. (2018). MR imaging of rectal cancer. Radiologic Clinics of North America, 56(5), 751–774. [Google Scholar]
7. Westwood, D. A., Cuda, T. J., Hamilton, A. E. R., Clark, D., Stevenson, A. R. L. (2018). Transanal total mesorectal excision for rectal cancer: state of the art. Techniques in Coloprotology, 22, 649–655. [Google Scholar]
8. Chudner, A., Gachabayov, M., Bergamaschi, R. (2018). Transanal TME for rectal cancer. Diseases of the Colon & Rectum, 61(4), e31. [Google Scholar]
9. Gockel, I., Pommer, C., Langer, S., Jansen-Winkeln, B. (2018). Rezidivresektionen beim Rektumkarzinom (Resection of recurrent rectal cancer). Der Chirurg, 89, 647–660. [Google Scholar]
10. Leeds, I. L., Fang, S. H. (2018). Neoadjuvant therapy for rectal cancer. Diseases of the Colon & Rectum, 61(8), 883–886. [Google Scholar]
11. Luzietti, E., Pellino, G., Nikolaou, S., Qiu, S., Mills, S. et al. (2018). Comparison of guidelines for the management of rectal cancer. BJS Open, 2(6), 433–451. [Google Scholar]
12. Hida, K., Okamura, R., Sakai, Y., Konishi, T., Akagi, T. et al. (2018). Open versus laparoscopic surgery for advanced low rectal cancer. Annals of Surgery, 268(2), 318–324. [Google Scholar]
13. Frame, A. A., Carmichael, C. Y., Kuwabara, J. T., Cunningham, J. T., Wainford, R. D. (2019). Role of the afferent renal nerves in sodium homeostasis and blood pressure regulation in rats. Experimental Physiology, 104(8), 1306–1323. [Google Scholar]
14. Foco, L., Pattaro, C. (2019). Genetics of blood pressure regulation: Possible paths in the labyrinth. American Journal of Kidney Diseases, 74(3), 421–424. [Google Scholar]
15. Bata, A. M., Fondi, K., Witkowska, K. J., Werkmeister, R. M., Hommer, A. et al. (2019). Optic nerve head blood flow regulation during changes in arterial blood pressure in patients with primary open-angle glaucoma. Acta Ophthalmologica, 97(1), e36–e41. [Google Scholar]
16. Soriano, J. E., Scott, B. A., Rosentreter, R. E., Vaseghi, B. (2019). The sympathetic role of glutamatergic paraventricular nucleus neurons in blood pressure regulation. Journal of Physiology, 597(6), 1433–1434. [Google Scholar]
17. Hennings, J. C., Hübner, C. A. (2019). Disorders of renal NaCl transport and implications for blood pressure regulation. Medizinische Genetik, 31, 17. [Google Scholar]
18. Garten, R. S., Hogwood, A. C., Weggen, J., Decker, K., Darling, A. et al. (2019). Examining arm vascular function and blood flow regulation in row-trained males. Medicine and Science in Sports and Exercise, 51(10), 2058–2066. [Google Scholar]
19. Williams, N. D., Mehlsen, J., Tran, H. T., Olufsen, M. S. (2018). An optimal control approach for blood pressure regulation during head-up tilt. Biological Cybernetics, 113, 149–159. [Google Scholar]
20. Leete, J., Layton, A. T. (2019). Sex-specific long-term blood pressure regulation: Modeling and analysis. Computers in Biology and Medicine, 104, 139–148. [Google Scholar]
21. Donnelly, G. F. (2019). Blood pressure and dementia: Holistic interventions. Holistic Nursing Practice, 33(3), 129. [Google Scholar]
22. Tasoujian, S., Salavati, S., Franchek, M., Grigoriadis, K. (2019). Robust IMC-PID and parameter-varying control strategies for automated blood pressure regulation. International Journal of Control, Automation and Systems, 17, 1803–1813. [Google Scholar]
23. Alasia, D. D., Iyagba, A. M. (2019). The blood lead, blood pressure connection: An evaluation of apparently healthy lead exposed workers in Nigeria. Occupational Diseases and Environmental Medicine, 7(3), 75–90. [Google Scholar]
24. Huang, Z., Shi, L., Sun, N. (2019). Statistical analysis of homocysteine and folate on the regulation of blood pressure. Journal of Medical Imaging and Health Informatics, 9(8), 1563–1567. [Google Scholar]
25. Schutzenberger, K., Puchner, S., Grinner, L., Schmidl, D., Aschinger, G. C. et al. (2019). Regulation of retinal blood flow in response to an experimental increase in intraocular pressure. Investigative Ophthalmology & Visual Science, 60(9), 5732. [Google Scholar]
 | This work is licensed under a Creative Commons Attribution 4.0 International License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. |