
 | Molecular & Cellular Biomechanics |  |
DOI: 10.32604/mcb.2021.015993
ARTICLE
Surface Topography Assessments of Spine Shape Change within the Day in Healthy Male Adults
1College of Science & Technology, Ningbo University, Ningbo, 315300, China
2Auckland Bioengineering Institute, University of Auckland, Auckland, 1010, New Zealand
3Cardiff School of Sport & Health Sciences, Cardiff Metropolitan University, Cardiff, CF5 2YB, UK
*Corresponding Author: Jianming Lu. Email: davidlu88@sina.com
Received: 29 January 2021; Accepted: 12 May 2021
Abstract: Surface topography is a no-invasive, radiation-free method that can measure sufficient surface spine parameters by the structured back surface scan and a precise anatomical landmarks recognition. The purpose of the present study was to measure the spine shape parameter changes within the day via the DIERS Formetric 4D analysis system. Ten male healthy volunteers were recruited to participate in the experiment. All participants were sedentary people with the average sitting time during study or work t ≥ 8 h and without any back disease in the past six months. Data were analyzed by one-way ANOVA, which set time points within the day as variable and shape results as the dependent variable. The significant difference could be found for the trunk length VP-DM with a one-way ANOVA test of p = 0.011. There was a significant difference (p = 0.024) between time slots of 9 am and 7 pm with 95%CI (–15.83, –1.01) and MD –8.42. No significant difference statistically for the scoliosis angle and the p-value of the one-way ANOVA test is 0.715. There was no significant difference for trunk inclination VP-DM with a one-way ANOVA test of p = 0.284. Statistical analysis depicted no significant difference for the trunk imbalance VP-DM with a one-way ANOVA test of p = 0.730. Trunk length VP-DM was significantly decreased in the afternoon and evening. This may be a potential back pain risk for sedentary individuals. Regular physical activity and mild to moderate exercise are recommended to improve spinal stability and maintain spinal shape.
Keywords: Surface topography; DIERS Formetric 4D; spine shape; postural assessment
Abnormal spine posture may cause several symptoms, for instance low back pain, scoliosis, kyphosis and lordosis. Low back pain, as a common spine disorder, may affect around 70% of residents in the western world and has caused a fairly economic burden in the last decade [1]. According to the study by Negrini et al. [2], adolescent idiopathic scoliosis (AIS) is a common spinal disorder with an incidence of 2%–3%. Prior to any intervention or treatment is implemented, the anatomical situation of the spine must be assessed [3].
Surface topography is a no-invasive, radiation-free method that can measure sufficient surface spine parameters by the structured back surface scan and a precise anatomical landmarks recognition. Diagnostic investigation of the spine and trunk could be conducted by surface topography technique, which can three-dimensionally re-build the surface and vertebral column and stimulate spine shape [4]. It is cost-saving, convenient and can reduce ionizing radiation exposure, comparing to traditional radiograph methods [5].
DIERS 4D Formetric system based on moiré principle and reconstructs the anatomy of the spine virtually from the back surface with a frequency of up to 24 Hz [6,7]. The spine posture data measuring from it has shown high validity from previous studies [8–11]. However, it is argued that Formetric 4D raster stereography is validated but only reliable [12]. Bassani et al. [13] recommended that the rasterstereography method cannot be considered as a valid alternative to radiographic evaluation, but it can be utilized for early spine disorder screening and it is cost-benefit comparing to other traditional approaches.
The evidence has shown that the DIERS 4D Formetric system can quantify the deformity of AIS [14]. Lason et al. [7] found a significant difference between the angulations of the spine. Several studies have proven that spinal shape parameters are reliable in healthy participants and in adolescents with idiopathic scoliosis through within a day [15,16] and over several days [7,17,18] of data collection. Girdler et al. [5] illustrated that the DIERS formetric scanner can contribute to AIS diagnosis and monitor without radiation exposure. Through measuring spine posture difference, it was found that DIERS 4D Formetric system can evaluate the differences of trunk inclination and kyphotic angle between barefoot and shod runners [19]. Spine morphology is also a crucial index for acute and chronic low back pain evaluation [1].
Spine morphology presents a high degree of plasticity [20]. Postural changes contribute to the alternations of the intrinsic shape of the spine as well [21]. Low physical activity may reduce spine bone mineral density and muscle strength [22–24]. Thus, physical activities or sedentary behaviors may potentially influence spine shape. The purpose of the current study was to investigate the spine shape parameter changes within the day via the DIERS Formetric 4D analysis system. It was hypothesized that healthy participants from the sedentary cohort would demonstrate a deteriorated spine morphology reversibly within the day.
Recruitment information was spread through the internet and posters. Sample size was calculated in power analysis (pwr package, R) with significance level = 0.05, groups = 3, power = 0.8, effect size = 0.5. Fifteen symptom-free, healthy male volunteers (Age: 25.8 ± 2.06 years, Heights: 1.77 ± 0.06 m, Weight: 69.75 ± 6.95 kg, BMI: 22.21 ± 0.72 kg/m2) were recruited to participate in the experiment. All enrolled participants were sedentary people with the average sitting time during study or work t ≥ 8 h and without any back disease in the past six months. Participants with scars and tattoos on their back surface were excluded. Informed consent was obtained from all subjects who informed the study objective, requirements and experimental protocol. The procedure of this experiment was approved by the local Ethics Committee, which was in accordance with the Declaration of Helsinki.
2.2 Apparatus and Experience Protocol
The surface topography of the spine was scanned utilizing a video raster stereography, DIERS Formetric 4D (Formetric®-System, DIERS International Gmbh, Schlangenbad, Germany) (Fig. 1). Before the experiment, closing the curtains, lights and doors in the laboratory in order to avoid stripes covered by surrounding light. Each participant should take off their shirt and shoes, and remove jewelry if they wore. The sacrum point should be uncovered by the underpants. During the experiment, subjects were standing still, look slightly down and relaxing arms for 5–10 s, till the instructor told participants that scanning was finished.
Prior to scanning, the static 3D measure was chosen in DICAM 2.5.12 software (DIERS International Gmbh, Germany), and by adjusting the height of the camera to identify the angulus inferior of the scapula. Stripe projection needs appropriate reflection on the subject’s back during the scanning (Fig. 2). Manual landmark correction was adopted if dimple points (DL and DR) were not detected correctly [25].
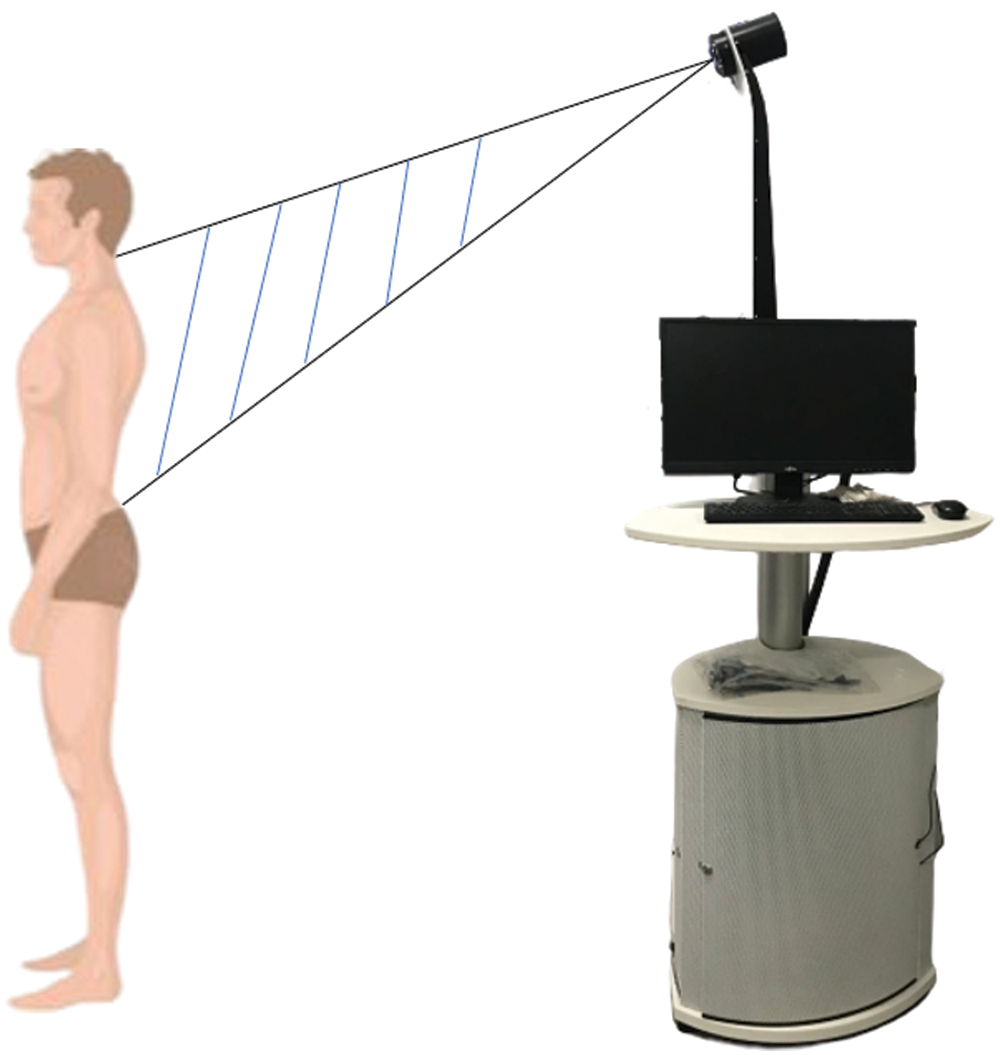
Figure 1: DIERS Formetric 4D system using in the experiment
Spine postural assessment within the day was measured including 3 time slots 9:00, 14:00, and 19:00. A three days test protocol was applied for all subjects. For each test, two trials were collected and each participant attends the experiment with a session of three days within a week. All data collection was conducted by the same instructor.
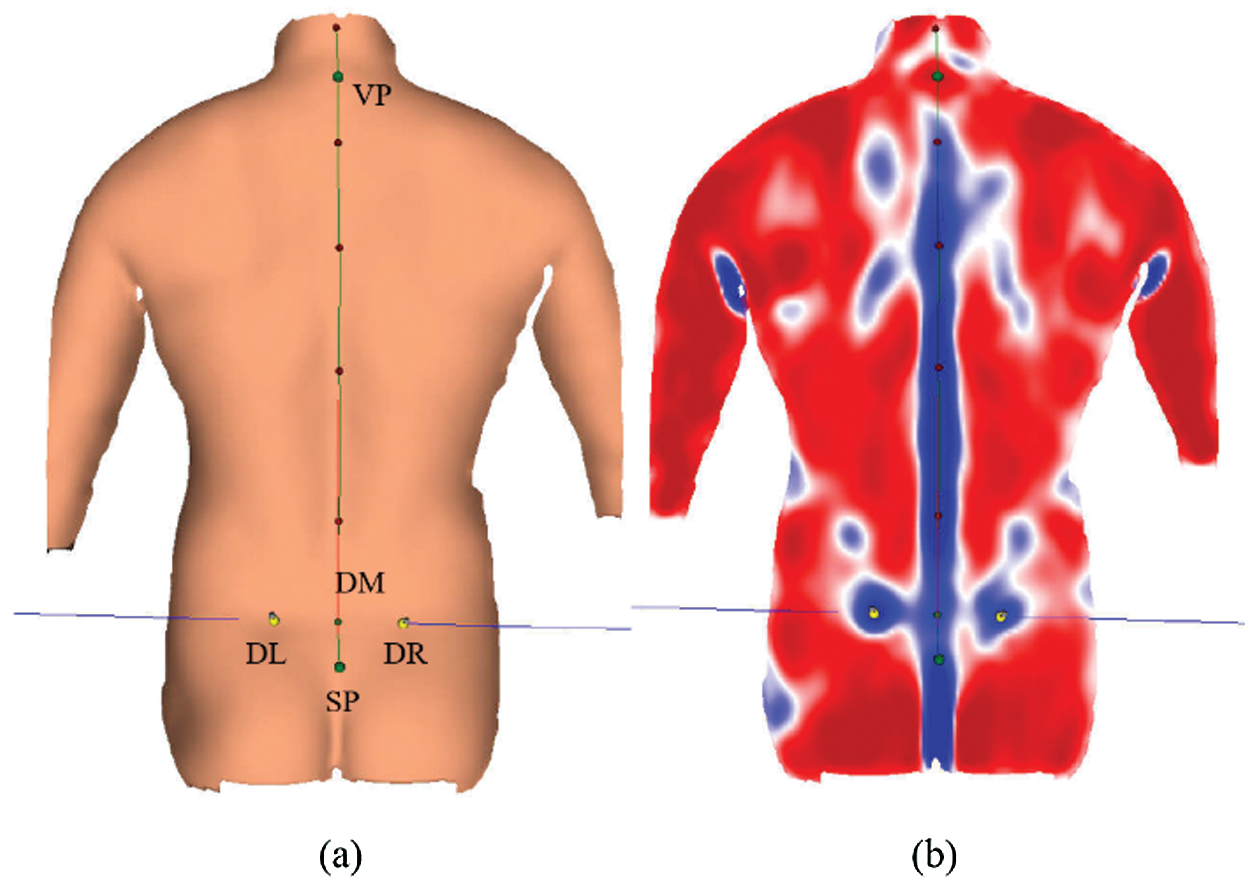
Figure 2: 3D modeling scanned from DIERS Formetric 4D system. Abbreviations: VP: vertebra prominent; DL: dimple left; DR: dimple right; DM: center between DL and DR (dimple middle); SP: sacrum point
2.3 Data Process and Statistical Analysis
Through system algorithms, a set of spine shape parameter values were obtained after scanning for postural assessment [26]. Surface topography data collected in this experiment including trunk length VP-DM, sagittal imbalance VP-DM (trunk inclination VP-DM), coronal imbalance VP-DM (trunk imbalance VP-DM), and scoliosis angle. Data were described as means ± SD, and normality distribution of data was examined and confirmed with the Shapiro-Wilk test. Homogeneity of variance was tested using Brown-Forsythe was used to test for homogeneity of variance for all vertebral column parameters prior to analysis of variance. The relevant data were analyzed by one-way ANOVA, which set time points within the day as variable and shape results as the dependent variable. Tukey HSD test was used for post-hoc analysis. All statistical tests were conducted in R (version 3.6.1). The significant threshold for all statistical tests was set at p < 0.05.
The spine shape parameters altered within the day (9 am in the morning, 2 pm in the afternoon and 7 pm in the evening) as shown in Tab. 1. The significant difference could be found for the trunk length VP-DM with a one-way ANOVA test of p = 0.011. The mean difference (MD) between 9 am and 2 pm was 8.04, 95%CI (0.63, 15.45) with a statistical difference of p = 0.032. The post hoc test of trunk length VP-DM between 2 pm and 7 pm showed a p value of 0.993. There was a significant difference (p = 0.024) between time slots of 9 am and 7 pm with 95%CI (–15.83, –1.01) and MD –8.42.
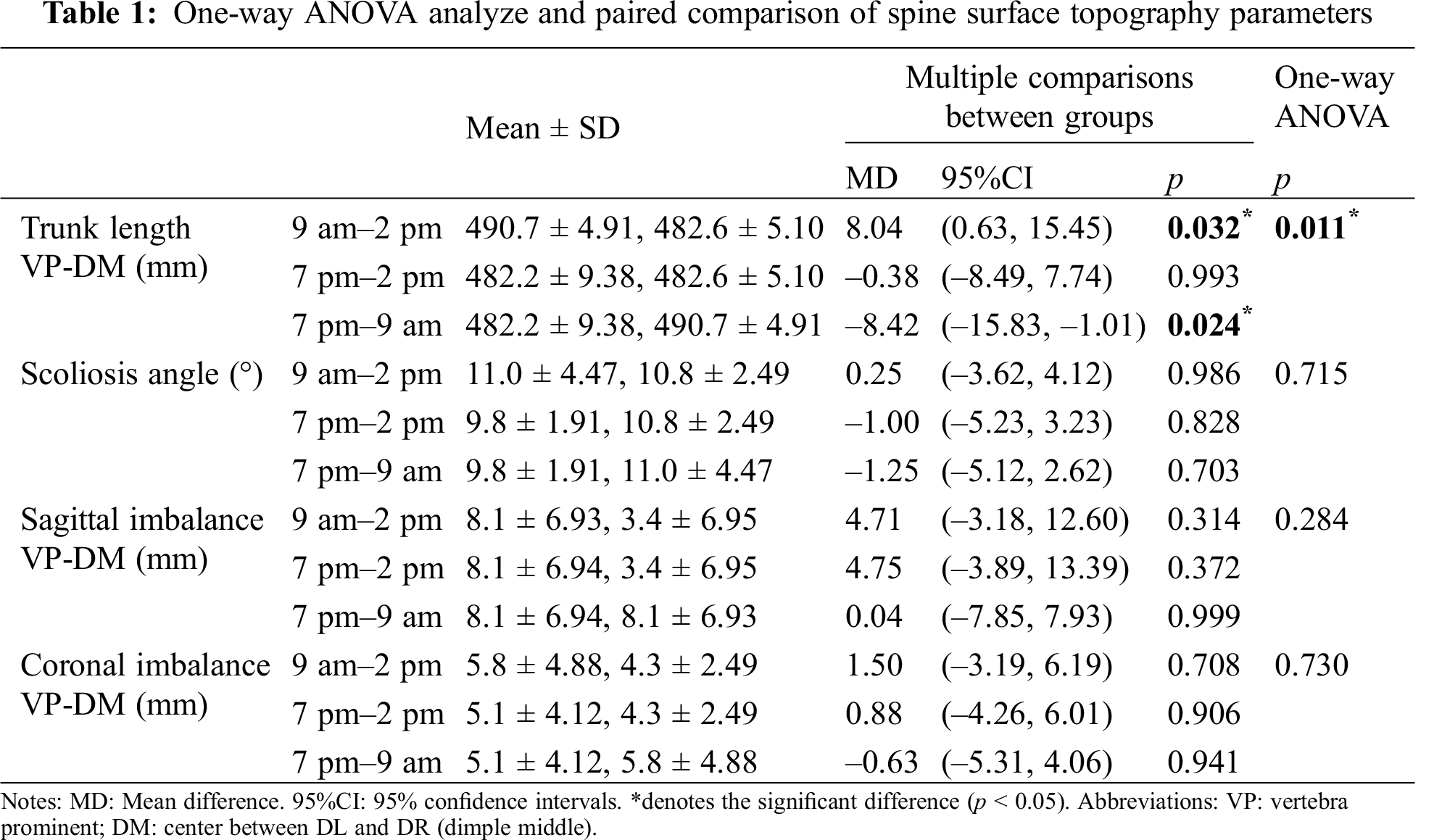
There was no significant difference statistically for the scoliosis angle with a one-way ANOVA test of p = 0.715. The mean difference (MD) between 9 am and 2 pm was 0.25, 95%CI (–3.62, 4.12) with p = 0.986. The post hoc test of the scoliosis angle showed a p value of 0.828 for the comparison of 2 pm and 7 pm. There was no significant difference (p = 0.703) between time slots of 9 am and 7 pm with 95%CI (–5.12, 2.62) and MD –1.25.
There was no significant difference for trunk inclination VP-DM with a one-way ANOVA test of p = 0.284. The mean difference (MD) between 9 am and 2 pm was 4.71, 95%CI (–3.18, 12.60) with p = 0.314. The post hoc test of sagittal imbalance CP-DM showed a p value of 0.372 for the comparison of 2 pm and 7 pm. There was no significant difference (p = 0.999) between time slots of 9 am and 7 pm with 95%CI (–7.85, 7.93) and MD 0.04.
Statistical analysis depicted no significant difference for the trunk imbalance VP-DM with a one-way ANOVA test of p = 0.730. The mean difference (MD) between 9 am and 2 pm was 1.50, 95%CI (–3.19, 6.19) with p = 0.708. The post hoc test of coronal imbalance VP-DM showed a p value of 0.906 for the comparison of 2 pm and 7 pm. There was no significant difference (p = 0.941) between time slots of 9 am and 7 pm with 95%CI (–5.31, 4.06) and MD –0.63.
The present study aimed to measure and evaluate spine shape parameters change, mainly trunk length VP-DM, trunk inclination VP-DM, trunk imbalance VP-DM, and scoliosis angle by surface topography method. The posture scan was conducted within the day (9 am, 2 pm and 7 pm) utilizing the DIERS Formetric 4D system. It was found trunk length VP-DM had a significant decrease in the afternoon and evening, comparing to the value in the morning.
The radiograph technique is used as the standard-of-care for disorder evaluation, but it contains shortages for instance inconvenient and safe-considering [27]. In recent years, surface topography technique has been widely used in the spine shape monitoring [13,28,29], and it has been proven for the data validity of the DIERS Formetric 4D spine scan [4,8].
Scoliosis angle, also known as the Cobby angle, is a key parameter for scoliosis evaluation. Cobb angle beyond 10° is defined as scoliosis, 10°–20° is mild scoliosis [30]. Through the correlation and principal component analysis, Manca et al. [29] found the spine parameters, surface rotation-rms and side deviation-rms, is significantly associated with scoliosis angle. The participants in our study have a risk of scoliosis, the reason may be that only the sedentary white-collar or postgraduate cohort was selected exploring spine shape parameters alteration within the day. However, contrary to our hypothesis, the scoliosis angle in the evening was slightly decreased, compared to data in the morning and afternoon. It implies that further investigation should be conducted in the future to illustrate this finding.
Consistent with our hypothesis, trunk length VP-DM was significantly decreased in the afternoon and evening. This may be a potential back pain risk for sedentary individuals. The spine shape may deteriorate in the future for the sedentary youngsters. Moderate exercise has showed crucial role in spine [31,32]. Regular physical activity and mild to moderate exercise are recommended to improve spinal stability and maintain spinal shape [33–35].
There is a deficiency in this work. No dynamic evaluation of spine morphology was performed. So, only stand still parameters were scanned and compared. Further study should explain the sedentary/physical inactivity effect for our spine within the day through investigating the dynamic vertebral column alter. In conclusion, this study conducted a prospective investigation into the spine shape alters within the day for sedentary individuals. The findings implicate that trunk length VP-DM was significantly decreased in the evening comparing to data in the morning, while the scoliosis angle demonstrated no statistical difference.
To sum up, this study measured the spine shape parameter changes of the sedentary cohort within the day via the DIERS Formetric 4D analysis system. Spine postural assessment within the day was measured including 3 time slots 9:00, 14:00, and 19:00. Spine shape parameter values were obtained after scanning for postural assessment. A significant difference could be found for the trunk length VP-DM between time slots of 9 am and 2 pm, and 9 am and 7 pm. This may be a potential back pain risk for sedentary individuals. Regular physical activity and mild to moderate exercise are recommended to improve spinal stability and maintain spinal shape.
Funding Statement: The authors received no specific funding for this study.
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
1. Roman, I., Luyten, M., Croonenborghs, H., Lason, G., Peeters, L. (2019). Relating the DIERS formetric measurements with the subjective severity of acute and chronic low back pain. Medical Hypotheses, 133, 109390. [Google Scholar]
2. Negrini, S., Donzelli, S., Aulisa, A. G., Czaprowski, D., Schreiber, S. (2018). 2016 SOSORT guidelines: Orthopaedic and rehabilitation treatment of idiopathic scoliosis during growth. Scoliosis and Spinal Disorders, 13(1), 3. [Google Scholar]
3. Peeters, L., Lason, G., Byttebier, G., Comhaire, F. (2015). Refining the reference values of DIERS 4D Formetric system and introducing a qualitative spine profile based on percentile ranking. Open Journal of Medical Imaging, 5(3), 150–158. [Google Scholar]
4. Navarro, I. J. R. L., da Rosa, B. N.,Candotti, C. T. (2019). Anatomical reference marks, evaluation parameters and reproducibility of surface topography for evaluating the adolescent idiopathic scoliosis: A systematic review with meta-analysis. Gait & Posture, 69, 112–120. [Google Scholar]
5. Girdler, S., Cho, B., Mikhail, C. M., Cheung, Z. B., Maza, N. et al. (2020). Emerging techniques in diagnostic imaging for idiopathic scoliosis in children and adolescents: A review of the literature. World Neurosurgery, 136, 128–135. [Google Scholar]
6. Diers, H., Mooshake, S., Heitmann, K. (2009). Dynamic 3D (4D) in objective classification of severe back deformities. Scoliosis, 4(2), 1. [Google Scholar]
7. Lason, G., Peeters, L., Vandenberghe, K., Byttebier, G., Comhaire, F. (2015). Reassessing the accuracy and reproducibility of DIERS Formetric measurements in healthy volunteers. International Journal of Osteopathic Medicine, 18(4), 247–254. [Google Scholar]
8. Degenhardt, B. F., Starks, Z., Bhatia, S. (2020). Reliability of the DIERS Formetric 4D spine shape parameters in adults without postural deformities. Scoliosis and Spinal Disorders, 2020(1), 1–10. [Google Scholar]
9. Abdel Raoof, N. A., Battecha, K. H., Elsayed, S. E. B., Soliman, E. S. (2017). The correlation between radiographic and surface topography assessments in three plane pelvic parameters. Journal of Back and Musculoskeletal Rehabilitation, 30(1), 175–181. [Google Scholar]
10. Humphries, T., Baker, M., Lee, L. B., Cole, A., Hughes-Lawson, C. et al. (2014). Correlation of rotation parameters in scoliosis between radiographs and DIERS Formetric scans. Orthopaedic Proceedings, 96(15), 18. [Google Scholar]
11. Kumar, V., Cole, A., Breakwell, L., Michael, A. L. R. (2016). Comparison of the DIERS Formetric 4D scanner and plain radiographs in terms of accuracy in idiopathic scoliosis patients. Global Spine Journal, 6(1), s-0036. [Google Scholar]
12. Padulo, J., Ardigò, L. P. (2014). Formetric 4D rasterstereography. BioMed Research International, 2014(1), 3–5. [Google Scholar]
13. Bassani, T., Stucovitz, E., Galbusera, F., Brayda-Bruno, M. (2019). Is rasterstereography a valid noninvasive method for the screening of juvenile and adolescent idiopathic scoliosis? European Spine Journal, 28(3), 526–535. [Google Scholar]
14. Lambert, A., Cole, A., Breakwell, L., Michael, A. L. R. (2016). The role of the DIERS 4D Formetric system in objectively quantifying the deformity seen in adolescent idiopathic scoliosis (AIS). Spine Journal, 16(4), 97–98. [Google Scholar]
15. Knott, P., Sturm, P., Lonner, B., Cahill, P., Betsch, M. (2016). Multicenter comparison of 3D spinal measurements using surface topography with those from conventional radiography. Spine Deformity, 4(2), 98–103. [Google Scholar]
16. Frerich, J. M., Hertzler, K., Knott, P., Mardjetko, S. (2012). Comparison of radiographic and surface topography measurements in adolescents with idiopathic scoliosis. Open Orthopaedics Journal, 6, 261. [Google Scholar]
17. Guidetti, L., Bonavolontà, V., Tito, A., Reis, V. M., Gallotta, M. C. et al. (2013). Intra-and interday reliability of spine rasterstereography. BioMed Research International, 2013, 1–5. [Google Scholar]
18. Tabard-Fougère, A., Bonnefoy-Mazure, A., Hanquinet, S., Lascombes, P., Armand, S. et al. (2017). Validity and reliability of spine rasterstereography in patients with adolescent idiopathic scoliosis. Spine, 42(2), 98–105. [Google Scholar]
19. Draus, C., Moravec, D., Kopiec, A., Knott, P. (2015). Comparison of barefoot vs. shod gait on spinal dynamics using DIERS Formetric 4D and DIERS pedoscan systems. Open Journal of Therapy and Rehabilitation, 3(3), 70. [Google Scholar]
20. Meakin, J. R., Gregory, J. S., Aspden, R. M., Smith, F. W., Gilbert, F. J. (2009). The intrinsic shape of the human lumbar spine in the supine, standing and sitting postures: Characterization using an active shape model. Journal of Anatomy, 215(2), 206–211. [Google Scholar]
21. Nikonenko, I., Jourdain, P., Alberi, S., Toni, N., Muller, D. (2002). Activity-induced changes of spine morphology. Hippocampus, 12(5), 585–591.22. [Google Scholar]
22. Heneghan, N. R., Baker, G., Thomas, K., Falla, D., Rushton, A. (2018). What is the effect of prolonged sitting and physical activity on thoracic spine mobility? An observational study of young adults in a UK university setting. BMJ Open, 8(5), e019371. [Google Scholar]
23. Porter, R. W., Adams, M. A., Hutton, W. C. (1989). Physical activity and the strength of the lumbar spine. Spine, 14(2), 201–203. [Google Scholar]
24. Tillmann, V., Darlington, A. S. E., Eiser, C., Bishop, N. J., Davies, H. A. (2002). Male sex and low physical activity are associated with reduced spine bone mineral density in survivors of childhood acute lymphoblastic leukemia. Journal of Bone and Mineral Research, 17(6), 1073–1080. [Google Scholar]
25. Knott, P., Mardjetko, S., Thompson, S. (2012). A comparison of authomatic vs. manual detection of anatomical landmarks during surface topography evaluation using the Formetric 4D system. Scoliosis, 7(1), 19. [Google Scholar]
26. Degenhardt, B., Starks, Z., Bhatia, S., Franklin, G. A. (2017). Appraisal of the DIERS method for calculating postural measurements: An observational study. Scoliosis Spinal Disord, 12(1), 1–11. [Google Scholar]
27. Knott, P., Mardjetko, S., Rollet, M., Baute, S., Riemenschneider, M. et al. (2010). Evaluation of the reproducibility of the Formetric 4D measurements for scoliosis. Scoliosis, 5(1), 1–3. [Google Scholar]
28. Gipsman, A., Rauschert, L., Daneshvar, M., Knott, P. (2014). Evaluating the reproducibility of motion analysis scanning of the spine during walking. Advances in Medicine, 2014(1), 1–9. [Google Scholar]
29. Manca, A., Monticone, M., Cugusi, L., Doria, C., Tranquilli-Leali, P. et al. (2018). Back surface measurements by rasterstereography for adolescent idiopathic scoliosis: From reproducibility to data reduction analyses. European Spine Journal, 27(9), 2130–2138. [Google Scholar]
30. Horng, M. H., Kuok, C. P., Fu, M. J., Lin, C. J., Sun, Y. N. (2019). Cobb angle measurement of spine from X-ray images using convolutional neural network. Computational and Mathematical Methods in Medicine, 2019, 1–18. [Google Scholar]
31. Gunter, K. B., Almstedt, H. C., Janz, K. F. (2012). Physical activity in childhood may be the key to optimizing lifespan skeletal health. Exercise and Sport Sciences Reviews, 40(1), 13. [Google Scholar]
32. Mobbs, R. J. (2020). Gait velocity (walking speed) is an indicator of spine health, and objective measure of pre and post intervention recovery for spine care providers. Journal of Spine Surgery, 6(2), 353. [Google Scholar]
33. Hrušová, D., Komestik, B. (2014). Effect of a modified pilates programme on flexion of spine at women with a sedentary job. Journal of Human Sport and Exercise, 9(1), 284–290. [Google Scholar]
34. Yaprak, Y. (2014). A comparison of spine ROM and physical fitness parameters in active females and sedentary females. Sports Medicine Journal, 10(4), 2462–2468. [Google Scholar]
35. Carter, J. M., Beam, W. C., McMahan, S. G. (2006). The effects of stability ball training on spinal stability in sedentary individuals. Journal of Strength & Conditioning Research, 20(2), 429–435. [Google Scholar]
 | This work is licensed under a Creative Commons Attribution 4.0 International License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. |