 Open Access
Open Access
ARTICLE
A Detailed Study on IoT Platform for ECG Monitoring Using Transfer Learning
School of Computer and Software, Nanjing University of Information Science and Technology, Nanjing, 210044, Jiangsu, China
* Corresponding Author: Md Saidul Islam. Email:
Journal on Internet of Things 2022, 4(3), 127-140. https://doi.org/10.32604/jiot.2022.037489
Received 05 November 2022; Accepted 07 March 2023; Issue published 12 June 2023
Abstract
Internet of Things (IoT) technologies used in health have the potential to address systemic difficulties by offering tools for cost reduction while improving diagnostic and treatment efficiency. Numerous works on this subject focus on clarifying the constructs and interfaces between various components of an IoT platform, such as knowledge generation via smart sensors collecting biosignals from the human body and processing them via data mining and, in recent times, deep neural networks offered to host on cloud computing architecture. These approaches are intended to assist healthcare professionals in their daily activities. In this comparative research, we discuss the construction of an IoT network for real-time management and monitoring of a network of biosensors and gateways and the utilization of a cloud-based deep neural network architecture with such categorization of ECG data into various cardiovascular diseases. The aim of this paper is to provide a quicker transmission of data at a cheaper rate.Keywords
Heart disease may be affected by many factors that are difficult to quantify and monitor. The electrocardiogram (ECG) is the primary instrument used in cardiac monitoring since it displays the heart status as a pattern of bio-electric potential. The growth of IoT technologies has the potential to address a number of the difficulties now confronting healthcare systems globally. The Internet of Things platforms, which refers to a complete system that connects intelligent devices to cloud computing, have spawned a new paradigm for the administration of healthcare services. These Internet-of-Things-based apps provide exciting alternatives to conventional health services, increasing the reach of healthcare outside hospital environments [1,2]. They primarily focus on early identification and prevention of patients’ health decline and enabling patients to live independently [3]. In the context of IoT, these systems may be customarily partitioned into three major tiers to enable health monitoring applications [4]. Fig. 1 illustrates the three layers. Health data is collected using a wireless body area network (WBAN), including wearable biosensors. In application scenarios, such data collecting is often conducted 24/7 through heterogeneous sensors, resulting in the generation of a vast amount of information (i.e., big data) over time [5–7]. Second, a gateway device is facilitated by continuous communication near the WBAN. Traditionally, the gateway device acts as a relay among the WBAN and the servers. However, additional functions might be assigned to the edge. Thirdly, a cloud server is in charge of continuous data analysis techniques, enabling real-time decision-making.

Figure 1: A three-tier of IoT-based health monitoring system [7]
In healthcare applications, various machine learning techniques [8–10] are used to make decisions [11,12]. However, as the volume of data grows over time and enormous quantities of data are created as big data, most conventional approaches, such as standard neural network models and k-nearest neighbors, become inapplicable [13]. On the other hand, deep learning approaches [14–17] provide potential options in this area since they use algorithms embedded in deep networks to build feature representation [18,19]. These approaches can manage vast volumes of data, and their performance improves as the number of training datasets increases. Convolutional neural networks (CNN) are one kind of deep learning technology examined for IoT-based health monitoring in this study.
Deep learning algorithms are well positioned on cloud storage to use high-end computers in such a cloud-based IoT ecosystem [20–22]. These computers provide an acceptable level of performance at a significantly reduced execution time. However, the system’s reaction time is highly dependent on the system’s quality and availability of Internet connection. These systems cannot satisfy latency-critical applications (e.g., health monitoring) since a latency in establishing a connection significantly affects patients in emergency scenarios. Recently, using intelligent gateways devices at the edge for health monitoring has been suggested [23–25]. In this respect, the gateway device’s duties are expanded to include data processing, which allows for local analysis of the gathered data [26] due to the restricted computing resources available on gateway devices. However, deep learning algorithms cannot be implemented entirely on edge devices due to their high computational cost.
With recent advancements in artificial intelligence and increased access to health data, deep neural networks have shown to be vital for regulating the intelligent healthcare system [27]. Traditional cloud-based medical analytics extensively explores ECG data analytics utilizing Machine Learning (ML) or Artificial Intelligence (AI) approaches, as well as time series ECG analysis employing nonlinear Delay Differential Equations (DDEs). However, the adoption of embedded smarts in ultra-edge devices has received little attention in the literature. A more efficient and compact analytics approach on-sensor is necessary to reduce communication time and bandwidth with the cloud and protect user data privacy by analyzing health data locally.
The contributions of this paper can be summarized below:
I) Proposing an efficient way in order to analysis the ECG data and provide faster and precise result.
II) Introducing a fine-tuned CNN model that can be further utilized for analyzing ECG data.
III) Proposing a proper procedure in order to detect heart disease at an earlier stage. Data can be sent through Cloud platforms. Doctors can analyze data and take necessary steps.
2 Study Overview and Methodology Analysis
2.1 Portable IoT Platform for ECG
An IoT platform for ECG analysis is depicted in Fig. 2, which includes an intelligent ECG sensor, a smartphone-based Web gateway, and a cloud server for monitoring and managing devices, all of which are connected to a deep neural network for signal classification. Using Bluetooth LE GATT notifications and WebSockets for the gateway and cloud server link, real-time capabilities are being implemented with a heavy focus on sensor nodes. This will allow us to transmit information in nearly real-time, but it will establish a communication channel to build an infrastructure for managing and controlling devices [28].
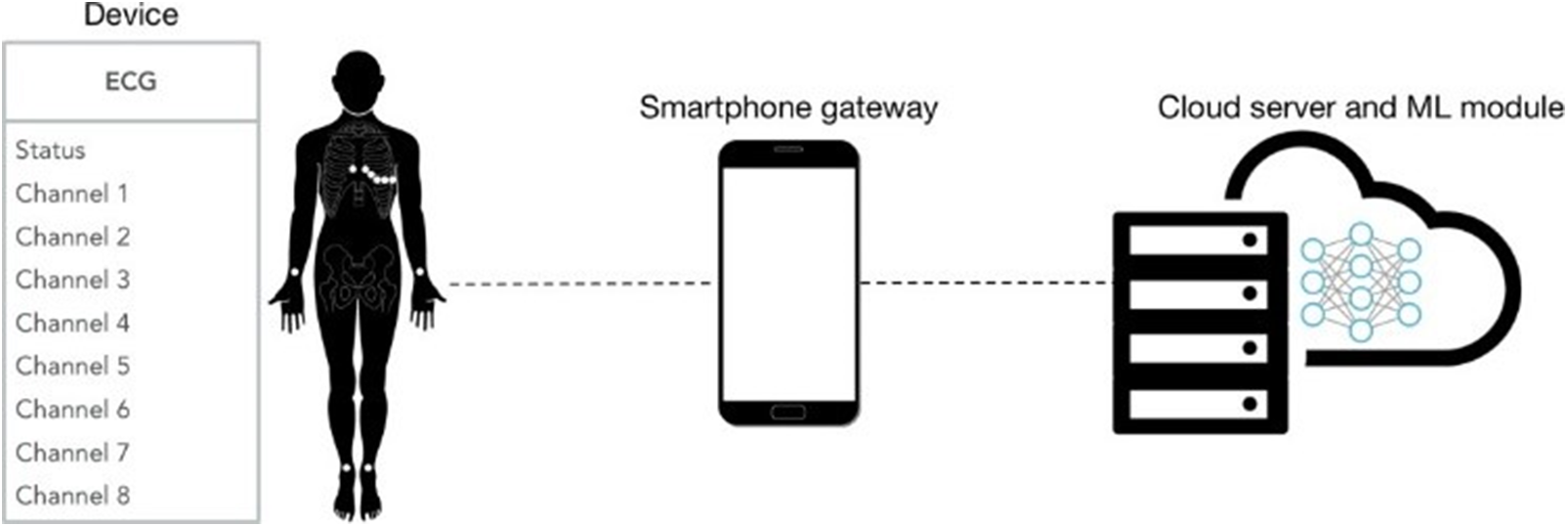
Figure 2: IoT platform for ECG [28]. A three-tier of IoT-based health monitoring system [7]
Residents can use self-adapting and optimized wireless sensor equipment (Fig. 3). A piece of ECG detection equipment is used. Users can choose from two innovative modes for -e wireless sensor equipment, which can be tailored to their specific needs. Detection accuracies vary depending on the user’s needs, and lead methods can be selected accordingly. Wearable ECG data is collected from a real human body and verified using the doctor’s Lenovo-SEU-DB dataset. The accuracies of different approaches in each functional module are evaluated. The three main steps in typical ECG diagnostic algorithms are pre-processing of the signal data, feature extraction from the data, and feature classification [29].
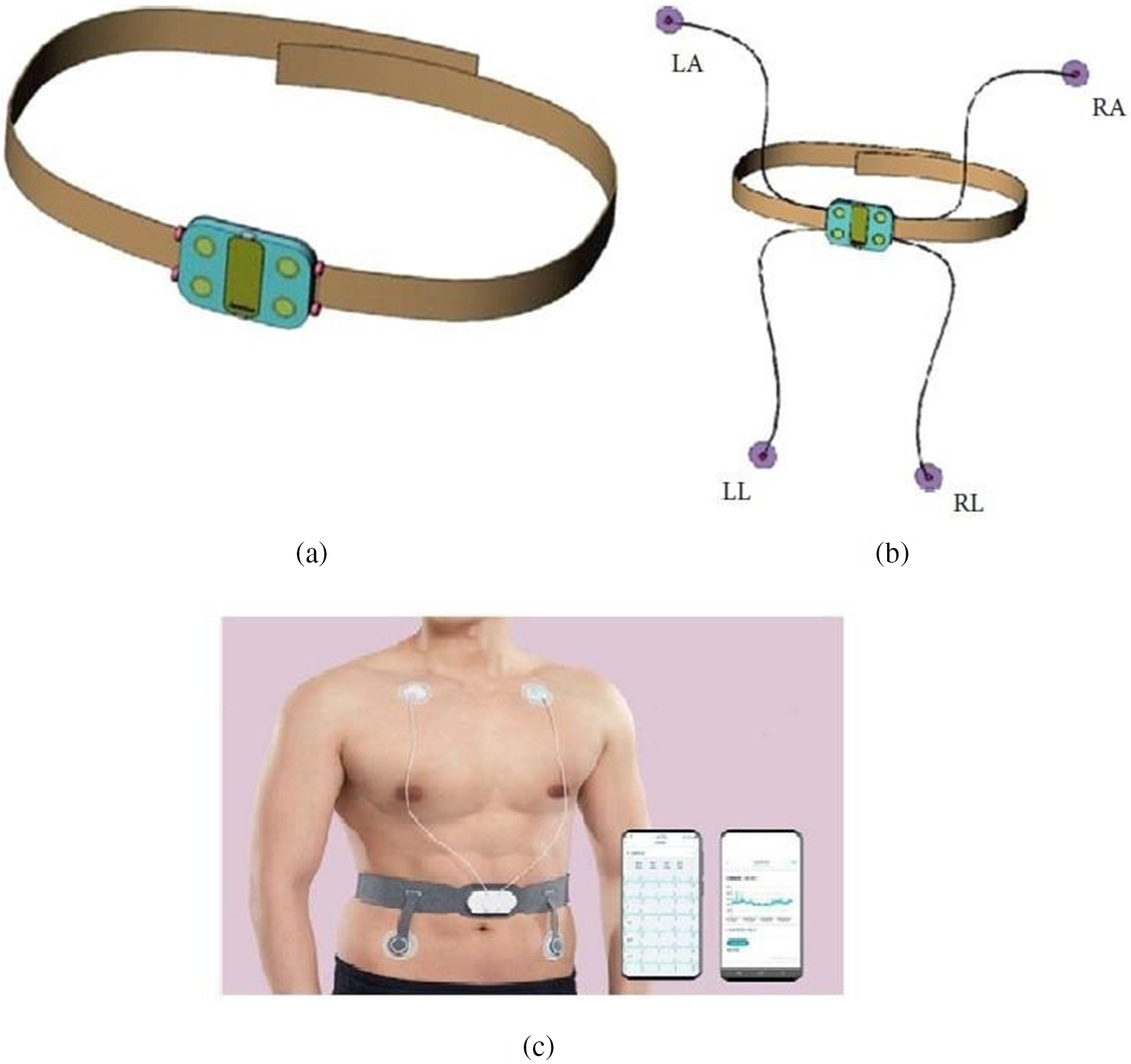
Figure 3: Wireless sensor equipment. LA: Left arm, LL: Left leg, RA: Right arm, and RL: Right leg [29]
As soon as the data is collected, it is sent to the central fog layer, processed, and forecasted in real-time. The ECG signal is captured and pre-processed in three layers. The ECG is captured in the first stage. To raise the heart signal’s amplitude from milli-volts (mV) to approximately 3.3 volts, the AD8232 differential amplifier is integrated into this step of the process. An analog-to-digital converter (ADS) ADS1115 is used to digitally transform the analog signal from the AD8232 [30]. How the hardware is deployed can be seen in Fig. 4.
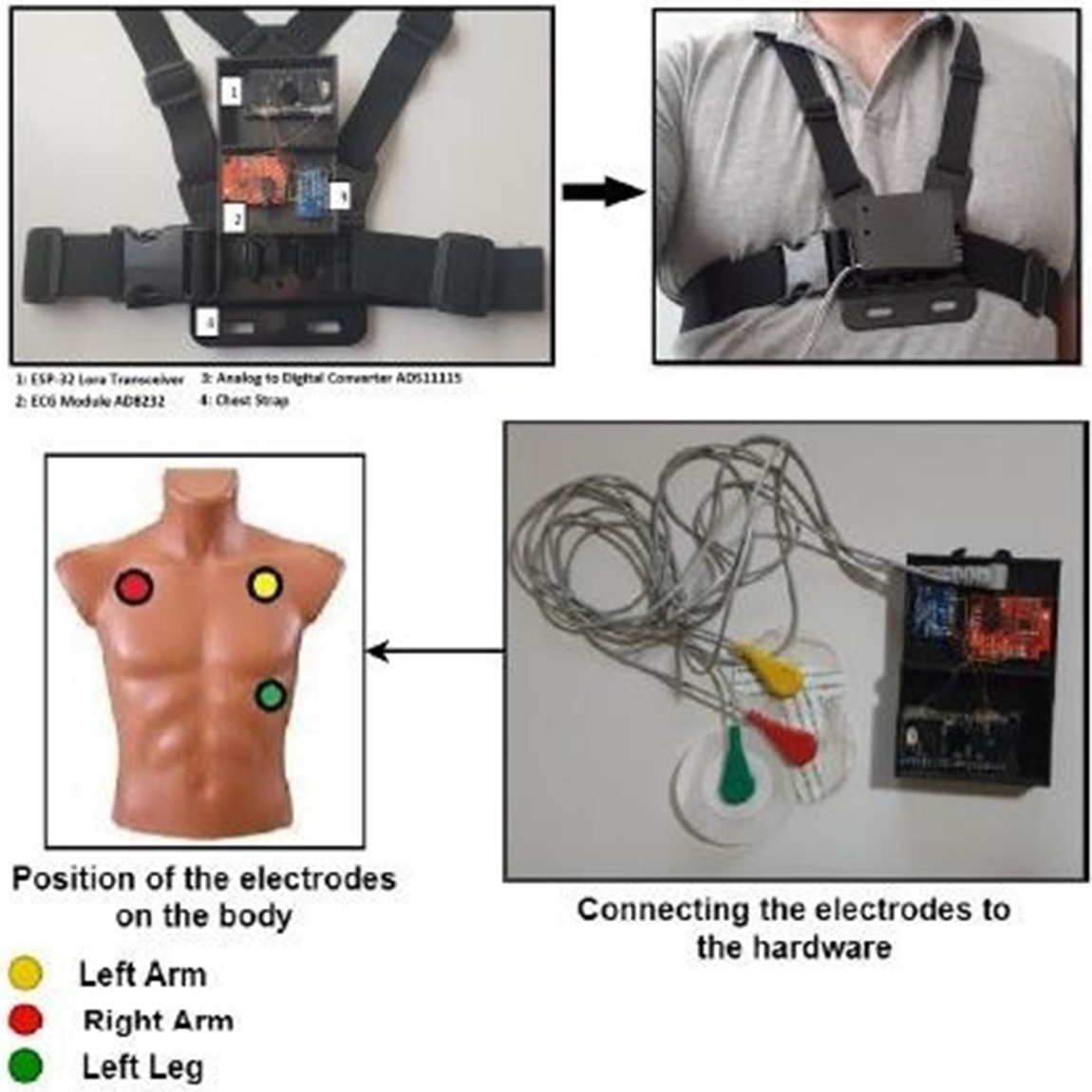
Figure 4: Hardware deployment of fog architecture [30]
2.4 Conventional ECG Heartbeat Classification
This technique may impair the security of ECG analysis for arrhythmia detection. To solve this issue, build an efficient, automated, and lightweight system with distributed intelligence that could be applied and coupled with logic-in-sensors for hyper IoT analytics. To create a portable ECG/arrhythmia monitoring system, we imagined an AI-assisted approach for identifying heartbeats using a bare single-lead ECG signal and comparing the suggested model to conventional machine learning techniques using the architecture represented in Fig. 2.
Four distinct heartbeat categories were created from the annotation files in each dataset following the Association for the Advancement of Medical Instrumentation (AAMI) EC57 standard. The hyperparameter tuning and training phases were carried out using the DS1 (MIT-BIH Supraventricular Arrhythmia Database). The model was evaluated using another three datasets during the running/inference stage (DS2, DS3, and DS4). Multiple datasets were used to assess the proposed model’s generalization ability. Although each dataset includes data for several ECG leads, the experiment only used lead II since the model only required single-lead ECG tracing [31].
2.5 Normalized Classification of ECG
The research approach begins with the acquisition of the ECG signal through the produced single-lead prototype and continues with the construction of the technique for automated ECG signal processing. Additionally, it locates the peak of each signal for a single full cycled signal trimming; the third step converts the cut signal to a single JPG picture and then classifies the signal category using a deep convolutional neural network. As a result, clinicians, such as emergency medical technicians, may use this gadget in crises as well (EMTs). Doctors may monitor a patient’s state in real-time during an emergency by using the remote ECG gadget. Additionally, when moving sick people to the operating room, anesthesiologists may simultaneously monitor and review patient’s real-time ECG data on mobile phones. This study employs an Arduino, a heart rate sensor, and a Raspberry Pi to create a prototype ECG signal analyzer capable of providing immediate ECG waveforms. Simultaneously, when paired with artificial intelligence technologies, the waveform type may be determined automatically. The following diagram depicts in Fig. 6. However, with the execution of the prototype idea, clinicians will be able to apply active methods in the treatment of patients that they have never used before. Doctors may monitor and discuss patients’ vital signs remotely with colleagues from various departments [32].
3 Results Overview and Analysis
3.1 Evaluating Portable IoT Platform for ECG Using CNN
The convolutional neural network learning module is able to classify incoming ECG signals and train the neural network using the TensorFlow version 1.3 library running on a GPU-accelerated machine. The TensorFlow engine has been implemented and connects to the RethinkDB database in order to query the original raw ECG signal data. Web-based annotation tools allow a heart technician to select waveform segments and label them according to different arrhythmia types as the network is trained. The application of live charts of sensor data is shown in Fig. 5. The network is trained using the selected signals. Once trained, the neural network takes the incoming live signal from the device and automatically classifies the ECG patterns into possible arrhythmias. The neural network is designed as successive convolutional, pooling, reshaping, fully connected, and dropout layers [28].
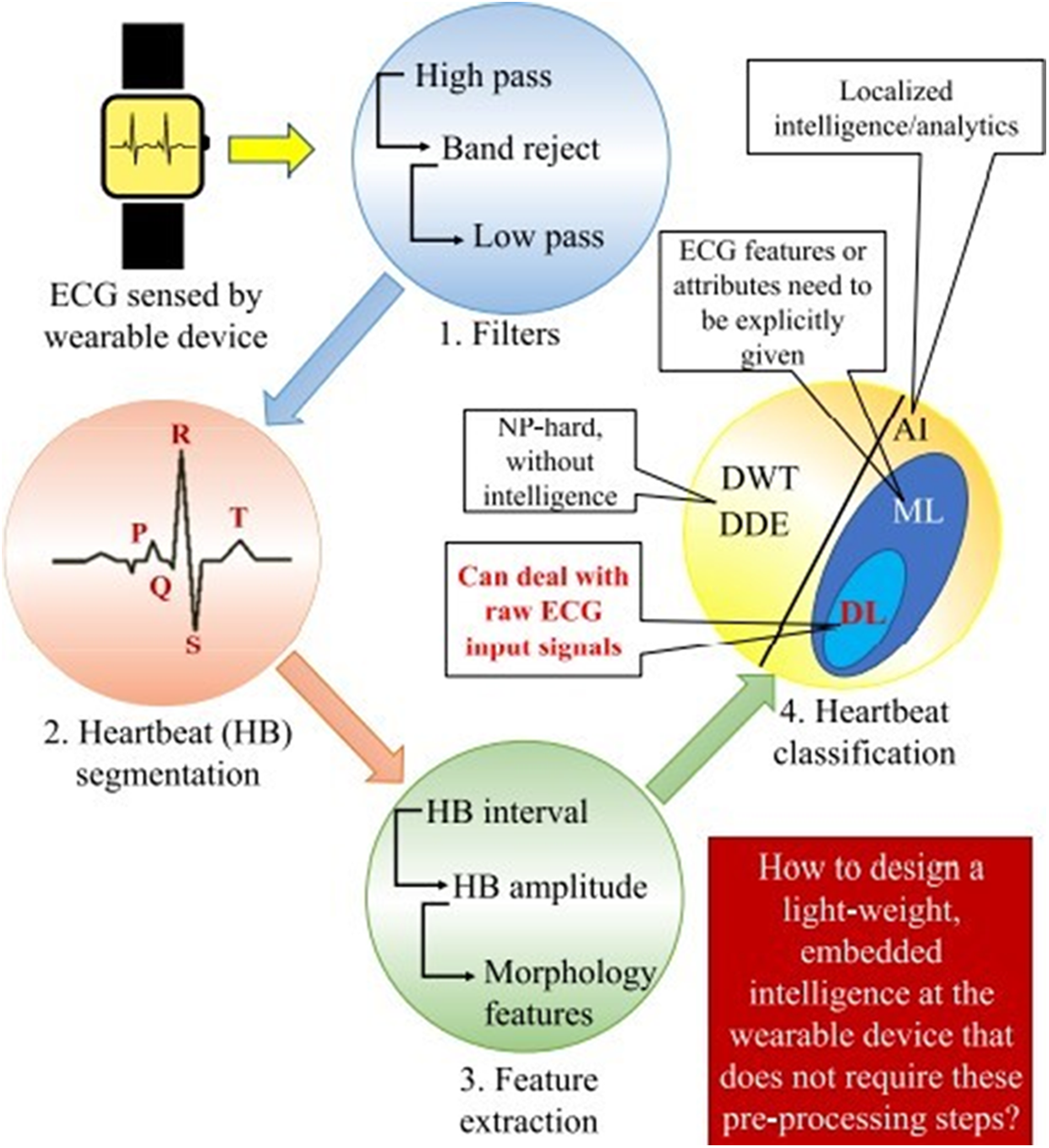
Figure 5: Classification of conventional ECG heartbeats in segments [31]
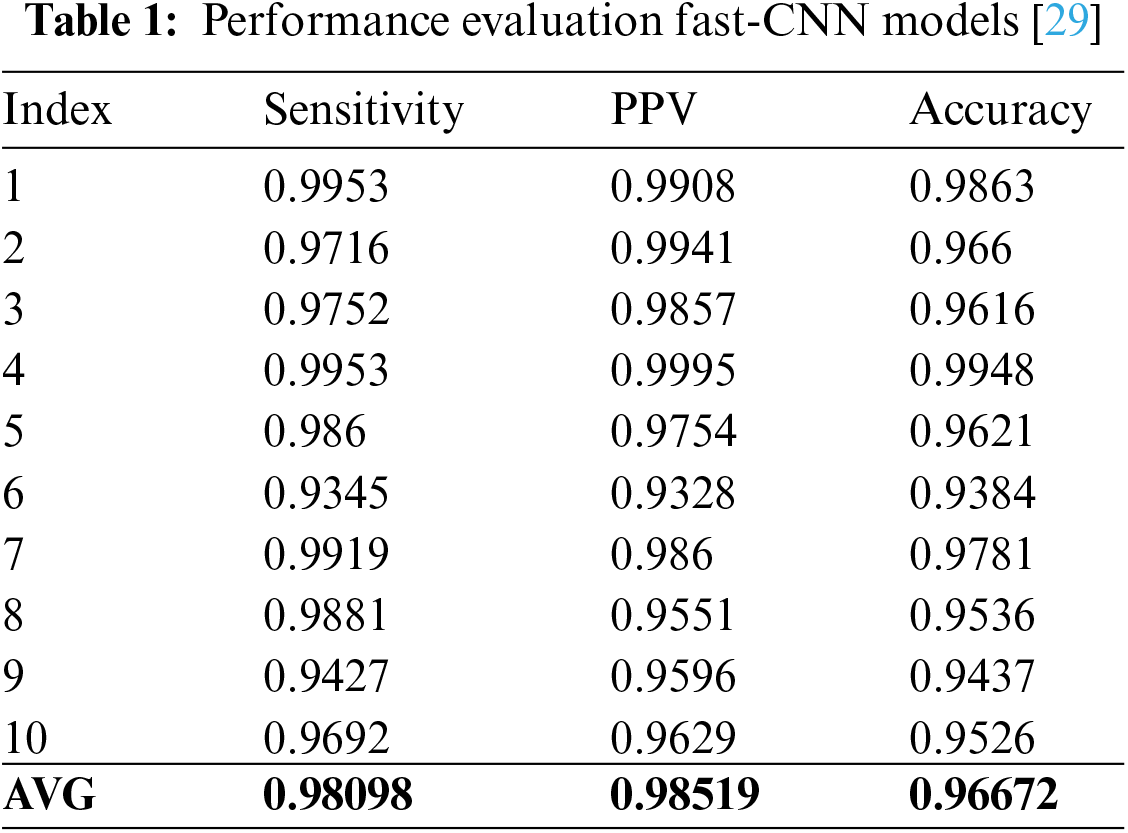
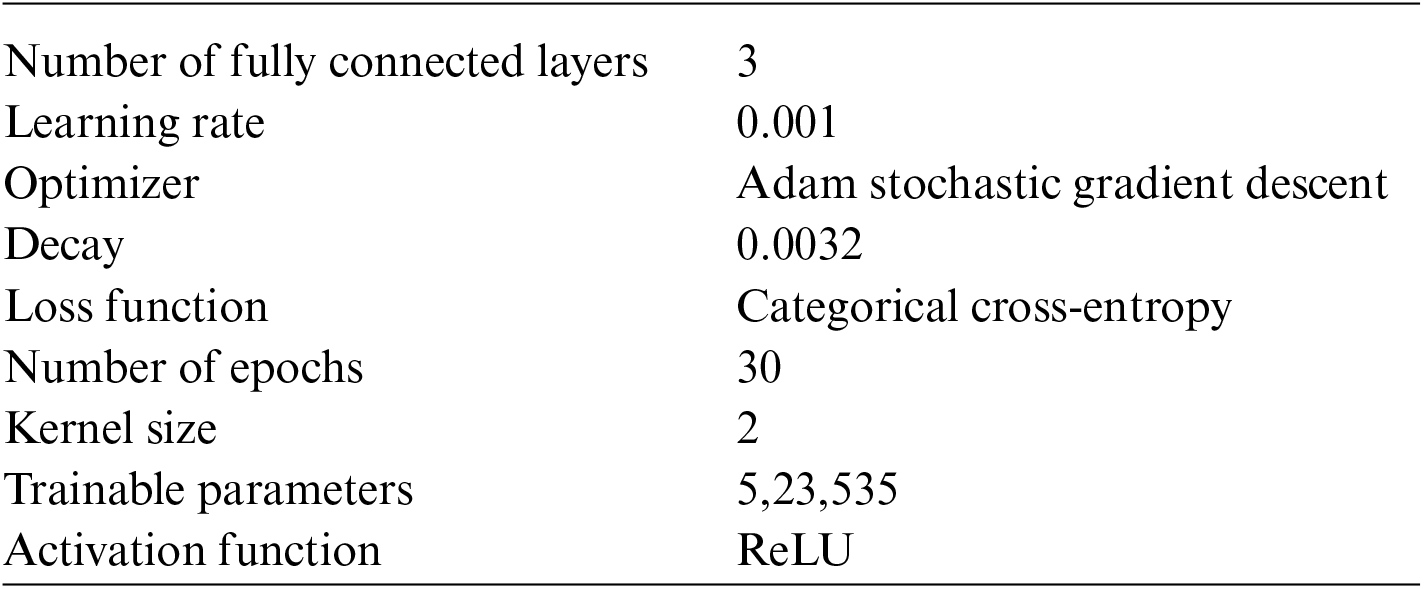
All the parameters for this model are fine-tuned. The desired result is achieved after applying 30 epochs. Table 1 shows the necessary fine-tuned parameters performed by the authors.
3.2 Evaluating Wearable ECG Kits Using Fast-CNN
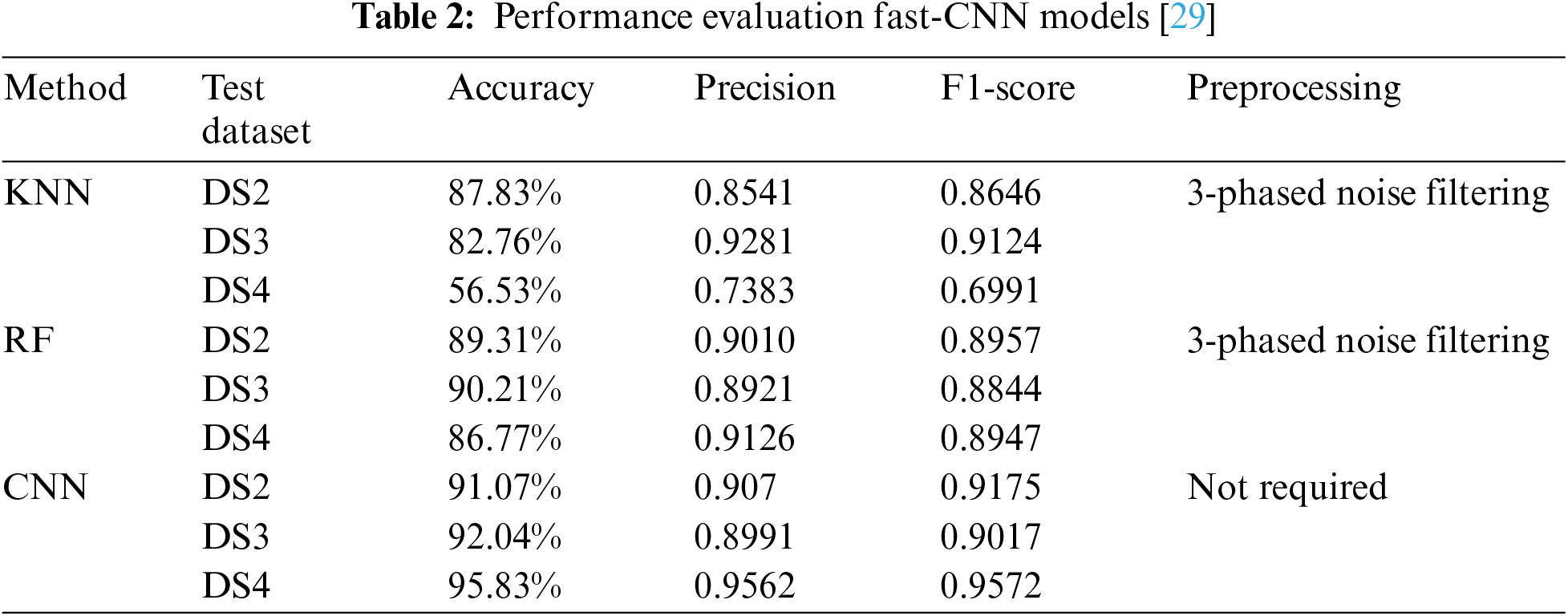
The fast-CNN algorithm used in this paper guarantees high accuracy and real-time detection of the CNN for QRS wave detection. The algorithm adopts a 32-layer convolution network structure, increasing detection sensitivity and accuracy for QRS detection and improving adaptability to worse Signal Noise Ratio (SNR) levels. As a result, it is more robust and adaptable to noise signals than the traditional ECG detection algorithm and has better detection accuracy. Tables 1 and 2 shows the performance using fast-CNN [29].
3.3 Evaluation of fog Architecture Using MobileNet
It was decided to convert the ECG signals into images in order to achieve this classification process. A series of image pre-processing steps were required to remove the axis from the image and crop it only to include the relevant portions of the image (see Figs. 6 and 7) [30].

Figure 6: Classification of conventional ECG heartbeats in segments [32]
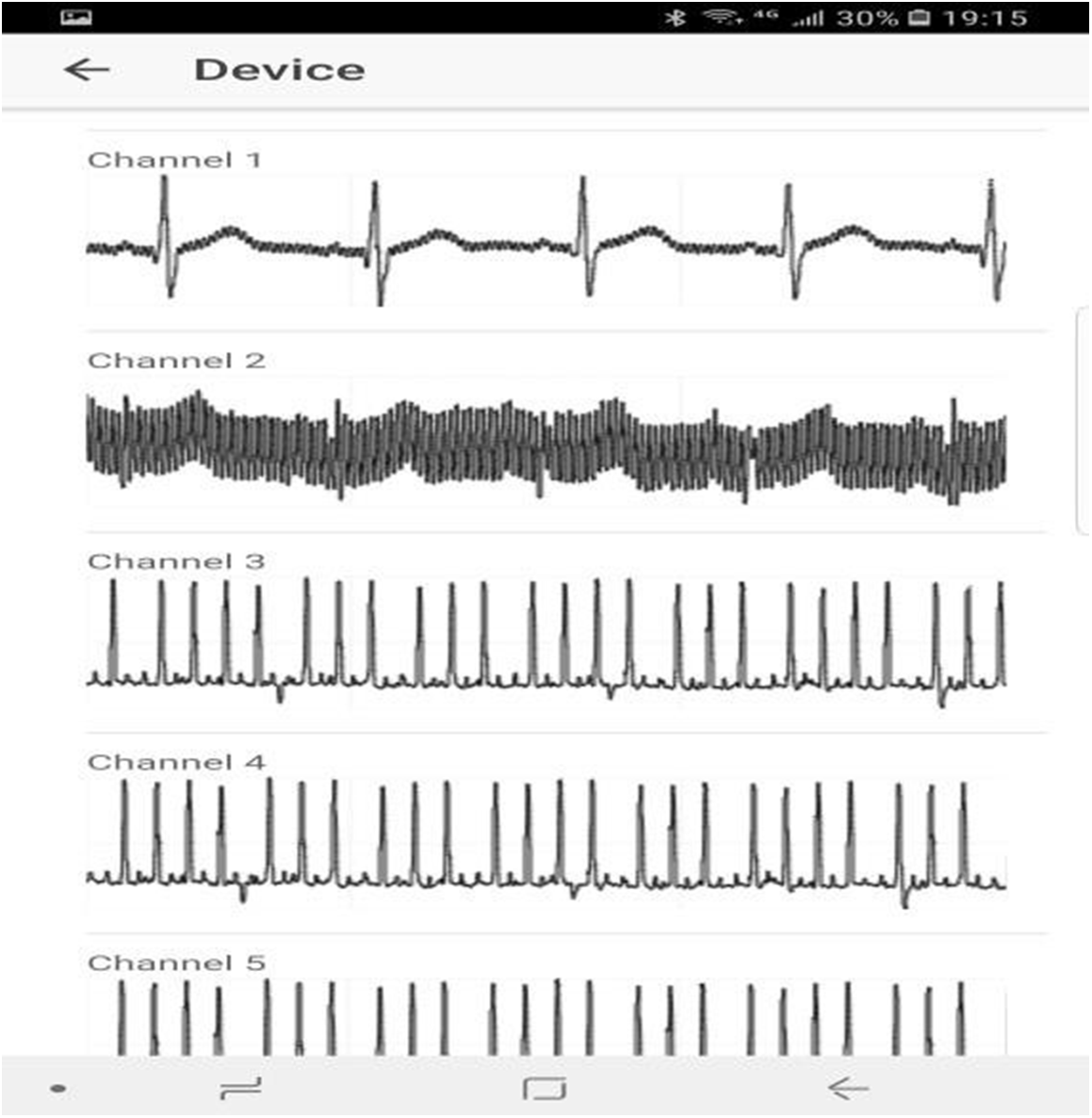
Figure 7: Multichannel sensor data [28]
To train the MobileNet, all images must be the same size, so they were resized from 1500 × 600 to 224 × 224 pixels. Hyperparameters of the MobileNet design are as follows: Learning rate: 0.01 per epoch; batch size: 512; 70 epochs. Due to the limited number of dataset samples, the test accuracy was around 0.6 during the training process. A confusion matrix (see Fig. 8) constructed from 100 unused images from the original dataset was used to validate the MobileNet.

Figure 8: Extraction of the area of interest from ECG image [30]
As shown in the confusion matrix, classification is generally accurate; however, it should be noted that 18% of the images in class Or were incorrectly labeled as Af. Class Af has an accuracy rate of 87%. Here Or refers to other rhythms, Nr refers to Normal sinus rhythm, No refers to Too noisy to classify, and Af refers to Atrial fibrillation.
3.4 Evaluating Conventional ECG Heartbeat Classification Using DS1 as the Training Dataset
Researchers used DS1 as the train set and DS2, DS3, and DS4 as the test datasets to evaluate the model’s performance. The suggested model outperformed established machine learning approaches in precision, accuracy, and F1-score in all three test datasets. The suggested CNN attained the accuracy of 94.07 percent, 92.04 percent, and 95.83 percent, respectively, using DS2, DS3, and DS4 as test datasets. The proposed custom CNN model outperforms existing machine learning approaches due to integrating convolution, sum- sampling, and normalization layers that automatically extract detailed characteristics from the ECG data. Additionally, the proposed model is more efficient at identifying important spots in the ECG due to the dynamic filter reduction in the deep convolution layers. The suggested technique avoids overfitting during training due to the inclusion of the regularization layer. However, even after considerable human pre-processing, existing approaches are incapable of automatically retrieving meaningful data from the ECG. While the proposed model models outperform conventional methods in terms of results, it is noteworthy that the proposed technique also achieves high accuracy with raw ECG signals without the need for noise filtering or manual feature extraction. The findings demonstrate that the proprietary CNN-based model is both resilient and lightweight in terms of identifying heartbeats with high accuracy, owing to the usage of raw single-lead ECG data [31].
3.5 ECG Classification by Deep Learning
For humans, the most intuitive type of information is visual. As a result, the scientific community has seen a rapid increase in the need for picture interpretation. It is necessary to have a machine with the intellectual ability to understand visual data. Image data has opened up several avenues and introduced us to the discipline of deep learning. Deep learning is the artificial intelligence functionality that simulates the human brain’s data processing and pattern generation processes [33,34]. Deep learning is a subfield of machine learning (AI) that utilizes networks capable of unsupervised learning from unstructured or unlabeled input. Additionally, it is referred to as deep neural networks or deep neural learning. Convolutional neural networks are indeed a subtype of deep neural networks that have garnered considerable interest in recent years due to their application to image recognition [35–40]. They are frequently used to extract characteristics and identify the immediate surroundings in order to construct a dense network. Because convolutional neural networks include additional convolution and pooling layers than typical neural networks, they can manage rotation, translation, and distortion and collect input for computation. Additionally, it maintains the shape and spatial information necessary for image processing. This has the benefit of being more convenient and quicker than conventional neural networks. Additionally, it may help to mitigate the danger of overfitting and neural train parameter overfitting [41]. Its capability for feature processing is critical in the disciplines of picture categorization and computer recognition.
The models used in this investigation were pre-trained AlexNet, ResNet, and SqueezeNet. Most of them are widely used in CNNs for images categorization. The input picture dimension in ResNet were 256 × 256. It comprises 53 convolution layers, one max-pooling layer, one fully linked layer, and a softmax output layer. The input picture dimension in AlexNet was 256 × 256. It consists of five convolutional layers, three max-pooling levels, seven ReLU layers, and two fully connected layers, all of which are preceded by a softmax output layer. The input picture dimension in SqueezeNet was 256 × 256. This image has twenty-six convolution layers, 3 max-pooling layers, and 26 ReLU layers. The findings indicated that the highest precision, accuracy, recall, F1-score, and kappa coefficient while employing the ResNet model were 0.97, 0.97, 0.97, and 0.96, respectively. The testing results between ResNet, AlexNet, and SqueezeNet demonstrated good accuracy and agreement when ResNet was used to classify the ECG’s 2D signal [32]. Figs. 9 and 10 depicts the results for ResNet, AlexNet, and SqueezeNet.
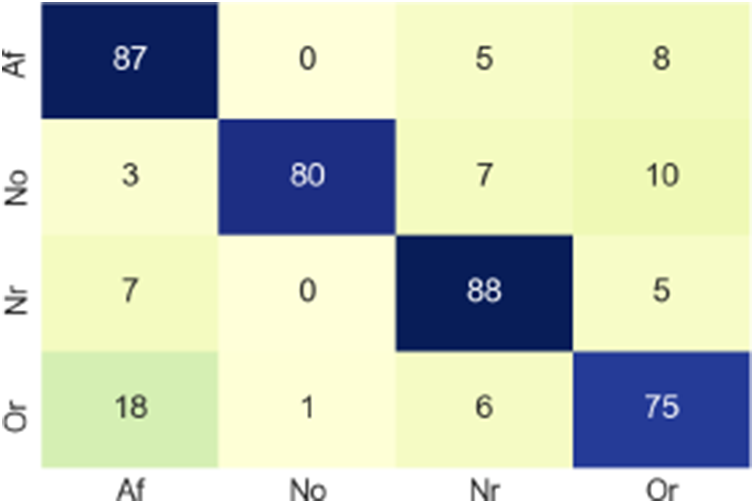
Figure 9: Confusion matrix [30]
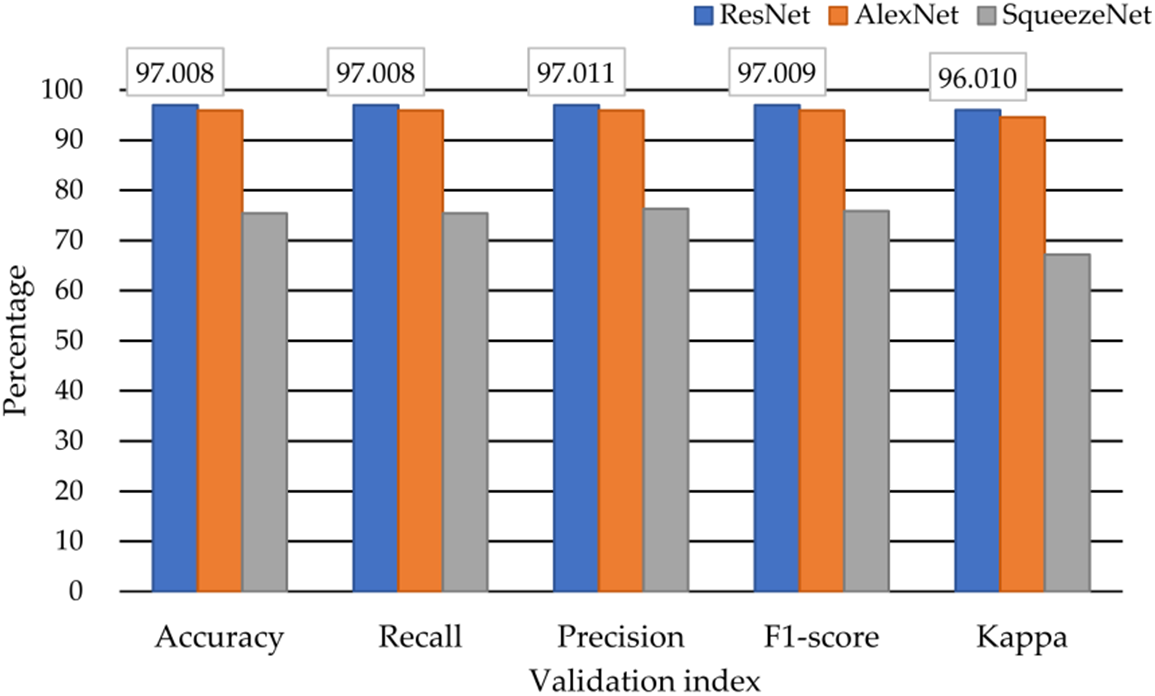
Figure 10: Classification results from several DNN models [32]
The reason behind limited processing power is that, the model requires significant amount of fine-tuning on other hyper-parameters along with number of trainable parameters should be reduced.
Health monitoring technologies powered by the Internet of Things allow at-risk sufferers to be tracked outside traditional healthcare settings. Such systems are required to provide a high level of service since a failure to do so might have grave repercussions for the patients. Deep learning may deliver adequate performance in terms of decision making since a large quantity of data can be supplied to the classification algorithm. These strategies can be applied entirely in cloud-based IoT systems. These technologies, however, are inadequate for time-sensitive health applications owing to the service’s reliance on the strength of the Internet connection. Other solutions include fully distributed edge-based systems, which are incapable of adopting deep learning algorithms due to their limited processing capability.
Funding Statement: The author received no specific funding for this study.
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
References
1. L. Atzori, “The internet of things: A survey,” Computer Networks, vol. 54, no. 15, pp. 2787–2805, 2010. [Google Scholar]
2. J. Gubbi, “Internet of things (IoTA vision, architectural elements, and future directions,” Future Generation Computer Systems, vol. 29, no. 7, pp. 1645–1660, 2013. [Google Scholar]
3. I. Azimi, “Internet of things for remote elderly monitoring: A study from user-centered perspective,” Journal of Ambient Intelligence and Humanized Computing, vol. 8, no. 2, pp. 273–289, 2017. [Google Scholar]
4. I. Azimi, “HiCH: Hierarchical fog-assisted computing architecture for healthcare IoT,” ACM Trans. Embed. Comput. Syst., vol. 16, no. 5s, pp. 174:1–174:20, 2017. [Google Scholar]
5. M. Beyer, “Gartner says solving ‘big data’ challenge involves more than just managing volumes of data,” 2017. www.gartner.com/newsroom/id/1731916 [Google Scholar]
6. D. Laney, “3D data management: Controlling data volume, velocity, and variety,” Technical Report. META Group Inc, 2001. [Google Scholar]
7. A. Rahmani, T. A. Gia, B. Negash, A. Anzanpour, I. Azimi et al., “Exploiting smart e-health gateways at the edge of healthcare internet-of-things: A fog computing approach,” Future Gener. Comput. Syst., vol. 78, pp. 641–658, 2018. [Google Scholar]
8. F. M. J. M. Shamrat, S. Chakraborty, M. M. Imran, J. N. Muna, M. M. Billah et al., “Sentiment analysis on Twitter tweets about COVID-19 vaccines using NLP and supervised KNN classification algorithm,” Indones. J. Electr. Eng. Comput. Sci., vol. 23, no. 1, pp. 463–470, 2021. [Google Scholar]
9. F. J. M. Shamrat, S. Chakraborty, M. M. Billah, M. Kabir, N. S. Shadin et al., “Bangla numerical sign language recognition using convolutional neural networks,” Indonesian Journal of Electrical Engineering and Computer Science, vol. 23, no. 1, pp. 405–413, 2021. [Google Scholar]
10. S. Afrin, F. J. M. Shamrat, T. I. Nibir, M. F. Muntasim, M. S. Moharram et al., “Supervised machine learning based liver disease prediction approach with LASSO feature selection,” Bulletin of Electrical Engineering and Informatics, vol. 10, no. 6, pp. 3369–3376, 2021. [Google Scholar]
11. G. Acampora, “A survey on ambient intelligence in healthcare,” Proceeding IEEE, vol. 101, no. 12, pp. 2470–2494, 2013. [Google Scholar]
12. K. P. Murphy, Machine Learning: A Probabilistic Perspective. Cambridge, Massachusetts London: The MIT Press, 2012. [Google Scholar]
13. O. Y. Al-Jarrah, “Efficient machine learning for big data: A review,” Big Data Research, vol. 2, no. 3, pp. 87–93, 2015. [Google Scholar]
14. M. O. Rahman, F. J. M. Shamrat, M. A. Kashem, M. F. Akter, S. Chakraborty et al., “Internet of things based electrocardiogram monitoring system using machine learning algorithm,” International Journal of Electrical and Computer Engineering (IJECE), vol. 12, no. 4, pp. 3739–3751, 2022. [Google Scholar]
15. F. J. M. Shamrat, S. Chakraborty, R. Ahammad, T. M. Shitab, M. A. Kazi et al., “Analysing most efficient deep learning model to detect COVID-19 from computer tomography images,” Indonesian Journal of Electrical Engineering and Computer Science, vol. 26, no. 1, pp. 462–471, 2022. [Google Scholar]
16. F. M. Shamrat, S. Azam, A. Karim, R. Islam, Z. Tasnim et al., “LungNet22: A fine-tuned model for multiclass classification and prediction of lung disease using X-ray images,” Journal of Personalized Medicine, vol. 12, no. 5, pp. 680, 2022. [Google Scholar] [PubMed]
17. S. Akter, F. M. Shamrat, S. Chakraborty, A. Karim and S. Azam, “COVID-19 detection using deep learning algorithm on chest X-ray images,” Biology, vol. 10, no. 11, pp. 1174, 2021. [Google Scholar] [PubMed]
18. J. Qiu, Q. Wu, G. Ding, Y. Xu and S. Feng, “A survey of machine learning for big data processing,” EURASIP Journal on Advances in Signal Processing, vol. 2016, pp. 1–67, 2016. [Google Scholar]
19. Q. Zhang, L. T. Yang, Z. Chen and P. Li, “A survey on deep learning for big data,” Information Fusion, vol. 42, no. 2018, pp. 146–157, 2018. [Google Scholar]
20. A. Dohr, R. Modre-Opsrian, M. Drobics, D. Hayn and G. Schreier, “The internet of things for ambient assisted living,” in 2010 Seventh Int. Conf. on Information Technology: New Generations, Las Vegas, NV, USA, pp. 804–809, 2010. https://doi.org/10.1109/ITNG.2010.104 [Google Scholar] [CrossRef]
21. M. Fazio, A. Celesti, F. G. Márquez, A. Glikson and M. Villari, “Exploiting the FIWARE cloud platform to develop a remote patient monitoring system,” in 2015 IEEE Symp. on Computers and Communication (ISCC), Larnaca, Cyprus, pp. 264–270, 2015. https://doi.org/10.1109/ISCC.2015.7405526 [Google Scholar] [CrossRef]
22. Association for the Advancement of Medical Instrumentation and American National Standards Institute, Testing and Reporting Performance Results of Cardiac Rhythm and ST-Segment Measurement Algorithms. The Association, Massachusetts, 1999. https://books.google.fi/books?id=gzPdtgAACAAJ [Google Scholar]
23. F. Bonomi, R. Milito, J. Zhu and S. Addepalli, “Fog computing and its role in the internet of things,” MCC, vol. 12, no. 2012, pp. 13–16, 2012. [Google Scholar]
24. A. M. Rahmani, P. Liljeberg, J. -S. Preden and A. Jantsch, Fog Computing in the Internet of Things Intelligence at the Edge. Germany: Springer, 2017. [Google Scholar]
25. A. M. Rahmani, T. N. Gia, B. Negash, A. Anzanpour, I. Azimi et al., “Exploiting smart e-health gateways at the edge of healthcare internet-of-things: A fog computing approach,” Future Generation Computer Systems, vol. 78, no. 2018, pp. 641–658, 2018. https://doi.org/10.1016/j.future.2017.02.014 [Google Scholar] [CrossRef]
26. D. Borthakur, H. Dubey, N. Constant, L. Mahler and K. Mankodiya, “Smart fog: Fog computing framework for unsupervised clustering analytics in wearable internet of things,” in 2017 IEEE Global Conf. on Signal and Information Processing (GlobalSIP), Montreal, QC, Canada, pp. 472–476, 2017. https://doi.org/10.1109/GlobalSIP.2017.8308687 [Google Scholar] [CrossRef]
27. Q. Yao, R. Wang, X. Fan, J. Liu and Y. Li, “Multi-class arrhythmia detection from 12-lead varied-length ECG using attention- based time-incremental convolutional neural network,” Inf. Fusion, vol. 53, pp. 174–182, 2020. https://doi.org/10.1016/j.inffus.2019.06.024 [Google Scholar] [CrossRef]
28. J. Granados, T. Westerlund, L. Zheng and Z. Zou, “IoT platform for real-time multichannel ECG monitoring and classification with neural networks,” in Int. Conf. on Research and Practical Issues of Enterprise Information Systems, Cham, Springer, October, pp. 181–191, 2017. [Google Scholar]
29. M. Yin, R. Tang, M. Liu, K. Han, X. Lv et al., “Influence of optimization design based on artificial intelligence and internet of things on the electrocardiogram monitoring system,” Journal of Healthcare Engineering, vol. 2020, pp. 1–8, 2020. [Google Scholar]
30. J. A. Rincon, S. Guerra-Ojeda, C. Carrascosa and V. Julian, “An IoT and fog computing-based monitoring system for cardiovascular patients with automatic ECG classification using deep neural networks,” Sensors, vol. 20, no. 24, pp. 7353, 2020. [Google Scholar] [PubMed]
31. S. Sakib, M. M. Fouda, Z. M. Fadlullah, N. Nasser and W. Alasmary, “A proof-of-concept of ultra-edge smart IoT sensor: A continuous and lightweight arrhythmia monitoring approach,” IEEE Access, vol. 9, pp. 26093–26106, 2021. [Google Scholar]
32. L. R. Yeh, W. C. Chen, H. Y. Chan, N. H. Lu, C. Y. Wang et al., “Integrating ECG monitoring and classification via IoT and deep neural networks,” Biosensors, vol. 11, no. 6, pp. 188, 2021. [Google Scholar] [PubMed]
33. J. Fan, L. Fang, J. Wu, Y. Guo and Q. Dai, “From brain science to artificial intelligence,” Engineering, vol. 6, pp. 248–252, 2020. [Google Scholar]
34. B. A. Richards, T. P. Lillicrap, P. Beaudoin, Y. Bengio, R. Bogacz et al., “A deep learning framework for neuroscience,” Nat. Neurosci., vol. 22, pp. 1761–1770, 2019. [Google Scholar] [PubMed]
35. F. M. J. M. Shamrat, S. K. Bhowmik, Z. Sultana, A. Hossain, M. Amina et al., “Comparative analysis to identify the best classifier for Parkinson prediction,” in 2021 2nd Int. Conf. on Smart Electronics and Communication (ICOSEC), Trichy, India, pp. 989–994, 2021. https://doi.org/10.1109/ICOSEC51865.2021.9591928 [Google Scholar] [CrossRef]
36. N. Ilyas, A. Shahzad and K. Kim, “Convolutional-neural network-based image crowd counting: Review, categorization, analysis, and performance evaluation,” Sensors, vol. 20, pp. 43, 2019. [Google Scholar] [PubMed]
37. S. Dodge and L. Karam, “A study and comparison of human and deep learning recognition performance under visual distortions,” in Proc. of the 2017 26th Int. Conf. on Computer Communication and Networks (ICCCN), Vancouver, BC, Canada, 31 July–3 August, pp. 1–7, 2017. [Google Scholar]
38. F. M. Javed Mehedi Shamrat, Z. Tasnim, T. R. Chowdhury, R. Shema, M. Uddin et al., “Multiple cascading algorithms to evaluate performance of face detection,” in Pervasive Computing and Social Networking, Singapore: Springer, pp. 89–102, 2022. [Google Scholar]
39. H. Zheng, J. Fu, T. Mei and J. Luo, “Learning multi-attention convolutional neural network for fine-grained image recognition,” in Proc. of the 2017 IEEE Int. Conf. on Computer Vision (ICCV), Venice, Italy, 22–29 October, pp. 5219–5227, 2017. [Google Scholar]
40. F. M. J. M. Shamrat, S. K. Bhowmik, M. F. Muntasim, T. I. Nibir, T. R. Chowdhury et al., “Comparative analysis of human face recognition using SURF and neural network methods,” in 2021 2nd Int. Conf. on Smart Electronics and Communication (ICOSEC), Trichy, India, pp. 984–988, 2021. https://doi.org/10.1109/ICOSEC51865.2021.9591722 [Google Scholar] [CrossRef]
41. N. Srivastava, G. Hinton, A. Krizhevsky, I. Sutskever and R. Salakhutdinov, “Dropout: A simple way to prevent neural networks from overfitting,” J. Mach. Learn. Res., vol. 15, pp. 1929–1958, 2014. [Google Scholar]
Cite This Article
 Copyright © 2022 The Author(s). Published by Tech Science Press.
Copyright © 2022 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.

 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools