DOI:10.32604/iasc.2022.027694
| Intelligent Automation & Soft Computing DOI:10.32604/iasc.2022.027694 |  |
| Article |
Influencing Factors Analysis of Rehabilitation for Patients with Spinal Cord Injury
1Rehabilitation Medicine Depart, Sichuan Academy of Medical Sciences, Sichuan Provincial People’s Hospital, Chengdu, 610072, China
2Nanjing University of Chinese Medicine, Nanjing, 210023, China
3Griffith University, Queensland, 4222, Australia
4Nanjing University of Information Science and Technology, Nanjing, 210044, China
*Corresponding Author: Yufeng Li. Email: liyufengchengdu@163.com
Received: 23 January 2022; Accepted: 01 March 2022
Abstract: The aim of spinal cord injury rehabilitation is to increase the independent ability of patients, so that patients can return to society and live a creative life. Regaining independence living is the primary goal of rehabilitation. Rehabilitation of patients with spinal cord injury is a long and lengthy process, which needs comprehensive dimensions support from medical workers, family members, and social support. At present, medical institutions and researchers mainly focus on the level of physical recovery and the treatment of complications in patients with spinal cord injury and pay less attention to social factors during the rehabilitation treatment of patients. Therefore, we collected data on patients with spinal cord injury, who hospitalized in the Rehabilitation Department of Sichuan Provincial People’s Hospital. And this paper uses a regression model to comprehensively analyze social and non-social factors that affect the rehabilitation after spinal cord injury, such as International Standards for Neurological Classification of Spinal Cord Injury from American Spinal Cord Injury Association, medical insurance, patient caregiver status, and so on. Moreover, systematic rehabilitation evaluation is carried out, and rehabilitation nursing goals are formulated to achieve precise rehabilitation. It promotes the self-care ability of patients with spinal cord injury, and makes patients integrate into the society as much as possible.
Keywords: Spinal cord injury; rehabilitation; influencing factors
Spinal cord injury (SCI) is a common and serious disease in spinal cord surgery. In recent years, with the development of transportation, construction and mining, the number of patients with spinal cord injury is increasing, and most of them are young adults [1–3]. Injury not only leads to limb paralysis, but is also accompanied by a variety of serious complications, which not only brings great pain and disability to patients, but also brings a great burden to the family and society. The treatment and functional rehabilitation of spinal cord injury has become an important topic of global concern [4–6].
The treatment of spinal cord injury needs multi-disciplinary coordination. The acute stage requires professional emergency treatment measures; while the chronic stage is often accompanied by long-term complications, requiring long-term rehabilitation treatment and nursing [7,8]. In the existing medical environment, it is necessary to understand the changes of spinal cord injury for rational allocation of medical resources, and development of targeted preventive and nursing measures [9–11].
Sichuan Provincial People’s Hospital is a tertiary first-class hospital. The Department of Rehabilitation Medicine currently has 300 rehabilitation beds and 5 rehabilitation wards, namely neurological rehabilitation, orthopedic rehabilitation, psychosomatic rehabilitation, pain rehabilitation, and traditional Chinese medicine rehabilitation. At the same time, it has multiple treatment areas, prosthetics and orthopedics centers, hyperbaric oxygen therapy centers, psychological workshops, and extended care centers. And it has large-scale evaluation and training equipment such as 3D gait analysis, electromyography, balance therapy device, core isokinetic trainer, virtual environment trainer, robot gait trainer, orthopedic prosthesis production and hyperbaric oxygen chamber. The medical staff have very rich experience in rehabilitation training and rehabilitation care after spinal cord injury [12–14].
This article collected 137 patients with spinal cord injury, who were treated in the rehabilitation department of Sichuan Provincial People’s Hospital from January 2015 to September 2021. Furthermore, this paper analyzed the social and non-social factors of patients, including the international standards for Neurological Classification of Spinal Cord Injury from American Spinal Cord Injury Association (ASIA), age and gender of patients, medical resources, family care, social insurance, etc [15–17].
The rest of the paper is organized as follows. Section 2 introduces the classification and rehabilitation stages of spinal cord injury respectively. Section 3 introduces the patient information and assessment content after spinal cord injury. Section 4 introduces the estaged rehabilitation treatment plan. Section 5 makes a final summary.
2.1 Classification of Spinal Cord Injury
The classification of spinal cord injury is complex. According to the cause, it can be divided into traumatic spinal cord injury and non-traumatic spinal cord injury. It can also be divided into the following types according to the degree of injury [18–20].
1. Anatomical transection of the spinal cord: the external force directly acts on the spinal cord, resulting in spinal cord penetration injury or vertebral body fracture fragments crushing the spinal cord, and the condition is serious [21].
2. Complete injury: manifested as complete loss of movement, sensation and function below the level of injury [22].
3. Incomplete injury: partial loss of conduction function, manifested as incomplete loss of motor, sensory, and sphincter functions below the level of injury, divided into hemisection syndrome, anterior cord syndrome, posterior cord syndrome, and central cord syndrome, cauda equina injury syndrome, conus injury syndrome and spinal cord concussion [23,24].
2.2 Rehabilitation Stages of Spinal Cord Injury
The rehabilitation of patients with spinal cord injury is divided into four major stages [25–27].
1. Acute stage: the acute stage is mainly based on rescue, including the treatment of hypotension, surgery, anti-infection, replenishment of body fluids, adjustment of electrolyte balance, etc. At this time, the rehabilitation treatment has been intervened, but to a limited extent.
2. Subacute stage: the clinical condition of the patient is basically stable, but not stable enough to be released from clinical treatment. And the patient needs to remain in the orthopaedic or neurology ward.
3. Stable stage: the patient’s condition is already stable, and there are not many clinical measures to be done. At this time, the patient is treated in a rehabilitation hospital.
4. Recovery stage: it means that problems that need to be dealt with in clinical medical treatment have ended, and the patient has entered a long-term functional recovery stage, which is theoretically in the community rehabilitation stage.
3 Patient Information and Assessment Content After Spinal Cord Injury
The research group collected clinical data. From January 2015 to September 2021, Sichuan Provincial People’s Hospital (SAMSPH) treated patients with spinal cord injury for a long time and selected 137 inpatients with complete data.
Inclusion Criteria: ① Spinal cord injury from any cause; ② The data in the original medical records are relatively complete, including the patient’s ASIA score.
Exclusion Criteria: Transfer or death due to serious complications or other related diseases during hospitalization [28–30].
Among the 137 patients from 11 provinces, the ages are from 6 to 86, including 4 patient sunder 18 years old (including 18 years old), 108 patients between 19 and 59 years old, and 25 patients over 60 years old. The distribution of the administrative regions (province, municipality, and autonomous region) of the 137 patients’ families is shown in Fig. 1.
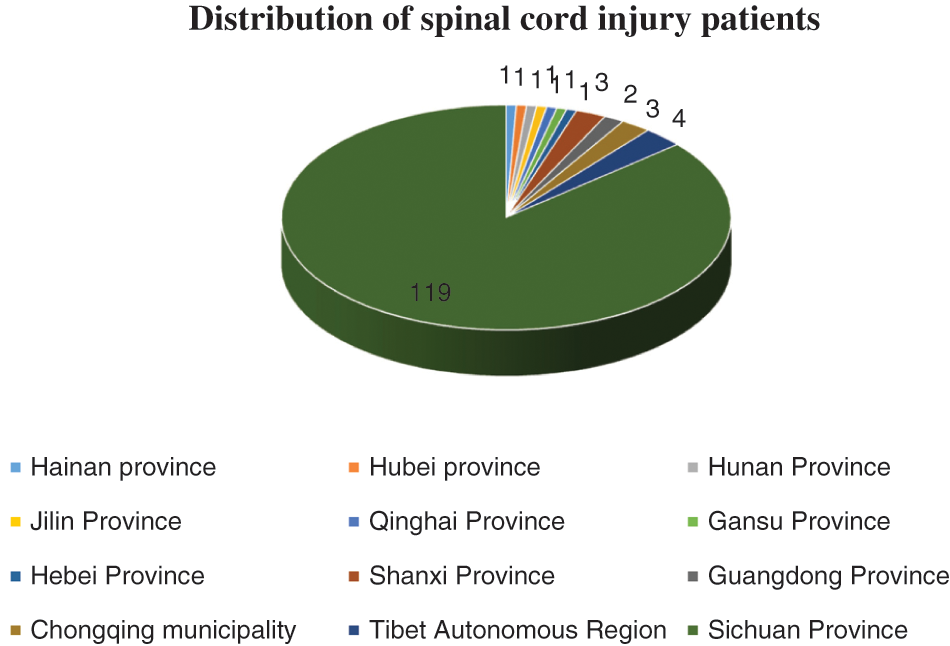
Figure 1: Distribution of the administrative regions of patients’ families
Among the 137 patients, there is 1 patient in Hainan Province, 1 patient in Hubei Province, 1 patient in Hunan Province, 1 patient in Jilin Province, 1 patient in Qinghai Province, 1 patient in Gansu Province, 1 patient in Hebei Province, 3 patients in Shanxi Province, 2 patients in Guangdong Province, 3 patients in Chongqing municipality, 4 patients in Tibet Autonomous Region, and 119 patients in Sichuan Province. The furthest patient is 3,200 kilometers away from the hospital.
Among the 137 patients, there are 93 males and 44 females. And 50 patients continued to receive treatment in the rehabilitation department of the hospital; 87 patients returned to the local or next-level hospital for treatment from our rehabilitation department. The distribution of the administrative regions (provinces, municipalities, and autonomous regions) of the 50 patients’ families is shown in Fig. 2.
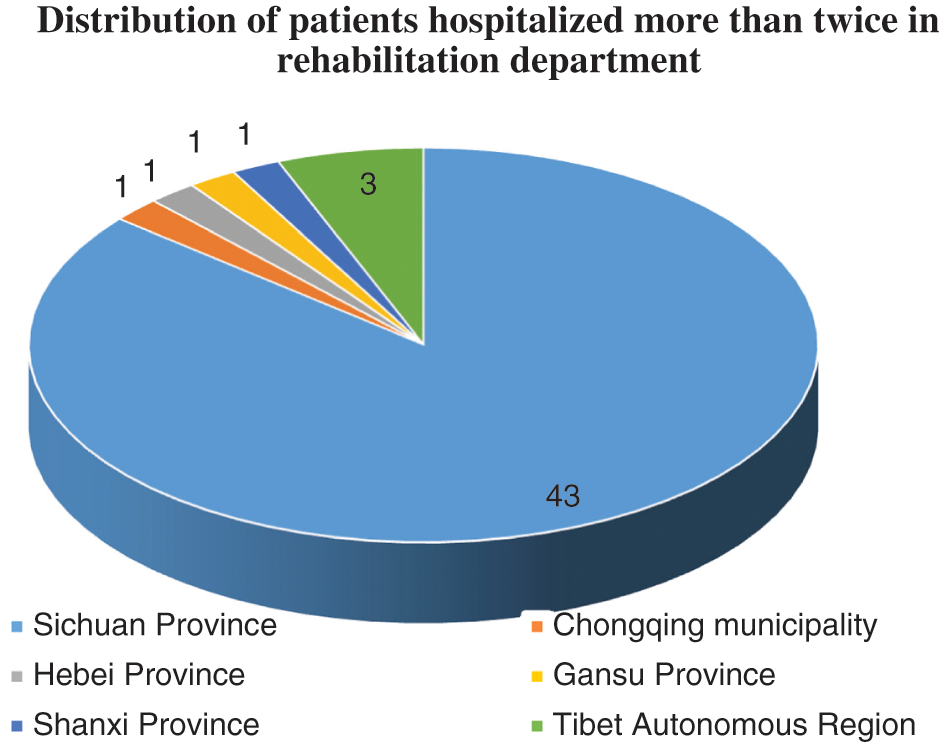
Figure 2: Distribution of patients hospitalized more than twice in rehabilitation department
Among the patients hospitalized for two or more times in the rehabilitation department, there are 43 patients in Sichuan Province, and 1 patient in Shanxi Province, 1 patient in Gansu Province, 1 patient in Hebei Province, 1 patient in Chongqing municipality, and 3 patients in Tibet Autonomous Region. The furthest patient is 2000 kilometers away from the hospital.
3.2 Admission Evaluation of Patients with Spinal Cord Injury
The initial assessment is carried out within 3 days after admission, the mid-term assessment is carried out in about 2 weeks according to the functional changes during the hospitalization, and the final assessment is carried out before discharge.
Evaluation items include the following.
1. General situation: including vital signs, urine and other basic conditions, to understand the overall treatment of patients.
2. Rehabilitation specialist assessment: injury degree classification, physical function classification, injury level and functional prognosis, nerve injury level assessment, pain assessment, circulatory function, respiratory function, swallowing function, bladder and bowel function assessment, psychological assessment, activities of daily living and occupational ability, social ability assessment.
3. Assessment of rehabilitation nursing: including venous thromboembolism (VTE) risk assessment scale, internal medicine thrombosis risk assessment scale (Padua assessment scale), Braden Pressure Ulcer Scale, Catheter Slipped Risk Assessment Scale, Fall Risk Assessment Scale, Pressure Ulcer Risk Assessment Scale, Early Warning Scoring Scale (MEWS), Barthel Index score.
The International Standard for Neurological Classification of Spinal Cord Injury (ISNCSCI, 2011 Revised) is issued by the American Spinal Cord Injury Association. And it is an internationally recognized spinal cord injury classification scale. At present, it is widely used in clinic and is of great significance to guide treatment and prevention. ASIA Impairment Scale is divided into five grades A, B, C, D and E. As shown in Tab. 1.

4 Staged Rehabilitation Treatment Plan
4.1 Staged Rehabilitation and Nursing Programs
After the patient is evaluated in hospital, rehabilitation physicians, rehabilitation nurses, and rehabilitation therapists formulate personalized rehabilitation treatment plans for patients at different times based on the patient’s physical condition and ASIA disability classification.
4.1.1 Acute Instability (Bed Rest Period)
Within about 2–4 weeks after acute spinal cord injury, the relative instability of the spine and the condition is the characteristic of this period. The patient needs bed rest and necessary braking, which is an important period for early recovery.
Respiratory function training and bladder function training are not only important for preventing early serious symptoms and stabilizing the condition, but also lay a good foundation for the gradual recovery process. When range of motion (ROM) training and muscle strengthening training are carried out, problems affecting the stability of the spine should be avoided, the range and intensity of physical activities should be controlled, and the progress should be made step by step. Physical therapist and occupational therapist should understand the condition, clearly know which training cannot be carried out, and should pay attention to the changes in the actual situation during the training process.
The clinical treatment and rehabilitation treatment in the acute instability should be carried out at the same time and cooperate with each other. Pulmonary infections are treated while respiratory function training is performed. The early survival rate of cervical high paraplegia is significantly improved, which is related to the rehabilitation of respiratory function. In the acute unstable period, rehabilitation training is 1–2 times a day, and the training intensity is not excessive. The main content of early training is as follows.
1. Range of Motion (ROM) training: Passive activities of the paralyzed limbs started on the first day of admission. Maintain joint mobility, prevent joint deformities, promote blood circulation in the limbs, and prevent muscle atrophy. It should be noted that patients with C6-C7 injuries should keep the fingers flexed when the wrist joint is stretched back, and the wrist must be flexed when the fingers are straightened.
2. Strength training: Under the principle of maintaining the stability of the spine, all active muscles should be exercised to avoid muscle atrophy or decrease in muscle strength.
3. Respiratory function training: Abdominal breathing training for thoracolumbar injuries. Appropriately compress the sternum twice a day to move the ribs to prevent adhesion of the costovertebral joints or the rib transverse joints.
4. Bladder function training: In the first aid phase, indwelling catheters should be used because it is difficult to control the infusion due to the need for infusion. After stopping the intravenous infusion, start intermittent catheterization and voluntary urination or reflex urination training.
4.1.2 Acute Stable Period (Wheelchair Period)
4-8 weeks after the end of the acute instability. The main clinical treatment in the acute stable period has basically ended, the patient’s spinal cord and condition have been stabilized, and rehabilitation has become the first task. The content and intensity of training should be individualized, and the content of rehabilitation training should be strengthened. Train for about 2 h a day, and monitor the changes in cardiopulmonary function during training. After the training of physical therapy (PT) and occupational therapy (OT) is completed in the training room, the patient can train by himself under the guidance of the nurse in the ward. Those who need a lower limb brace should be measured and prepared for training. Pay attention to the prevention and treatment of spine stability and orthostatic hypotension, support training on the mat, balance training, and transfer training on the bed or platform.
In wheelchair transfer training and wheelchair driving training, the habit of decompressing the sitting position is carried out every 30 minutes to prevent the occurrence of pressure sores. For patients who are likely to resume standing or walking, stand and walk training should be carried out with the corresponding lower extremity braces. Including standing and walking training inside the balance bar and using crutches. For patients who cannot resume walking, strengthen the residual muscle strength and overall endurance, and be proficient in wheelchair skills and training in daily life skills.
4.1.3 Early Stage (Wheelchair Activity Period) Mid-to-Late Stage Rehabilitation
Rehabilitation in the middle and late stages generally needs to start on the basis of early rehabilitation exercises 2–3 months after the injury. Strengthen the training of residual muscle strength and overall endurance, be proficient in wheelchair and life skills training, and carry out standing and walking training for patients who are likely to resume standing or walking. This post-rehabilitation treatment further strengthens physical training such as muscle strength training and balance training.
4.2 Variable Parameter Regression Model
At the same time of rehabilitation treatment, we searched for the relationship between patients’ social factors and non-social factors and the degree of spinal cord injury through variable parameter regression model.
The variable parameter regression model is a linear regression model with special features among the common regression models. Due to its own characteristics, the variable parameter regression model is different from the general regression model. In the variable parameter regression model, the parameter value corresponding to it can be generated by changing the value of each parameter in the regression model with the value of the independent variable. Usually for a single parameter variable
Among them,
The model (1) itself has no effect on the data to be analyzed, because for any set of observations
Local Weighted Fit
The local weighted regression algorithm makes the value of each parameter in the regression model change with the change of the value of the independent variable in the model, and then obtains the value generated in different changes, and selects different parameter values. That is, different parameter values correspond to different parameters, so that the estimated value of the corresponding regression function is given locally according to the difference of the independent variables. For different points
Weight Determination and Parameter Estimation
In the local weighted regression algorithm, each point of the independent variable needs to be assigned a corresponding weight, which is the W matrix. Among them, the points closer to x are given greater weight, because the closer to the sample point, the more consistent the same model. Correspondingly, some points that are far apart are given smaller weights, or even no weights. Therefore, you can specify a function
1. When
2. When
3. Other,
At present, the commonly used weight functions in the local weighted regression algorithm include the following two functions.
The cubic weight function is as follows.
Gauss weight function is as follows.
The local weighted linear regression method is applied to the model (1), that is, the corresponding
Thus, the following formula can be obtained.
The specific method assumes that the data to be tested is stored in the matrix X, and the regression coefficients are stored in the vector W. Therefore, for any given data
where T is the transpose of matrix X.
At this time, the regression coefficient W with the smallest error can be obtained by using the square error minimization, where the error refers to the difference between the estimated value and the actual value. So the square error can be written as the following formula.
The corresponding matrix expression is as follows.
Finally, the following formula can be solved.
where
Furthermore, weight
Among them,
Finally, the fitted value of x can be expressed as the following formula.
4.3 Analysis of Correlative Factors
4.3.1 ASIA Classification of Patients with Spinal Cord Injury
The ASIA impairment classification of patients with spinal cord injury, who are hospitalized once in the rehabilitation department, is shown in Tab. 2. The number of the patients is 87.

Fig. 3 shows the number of male and female patients in each ASIA grade. It can be seen that the proportion of male patient with spinal cord injury is higher than that of female from the data.
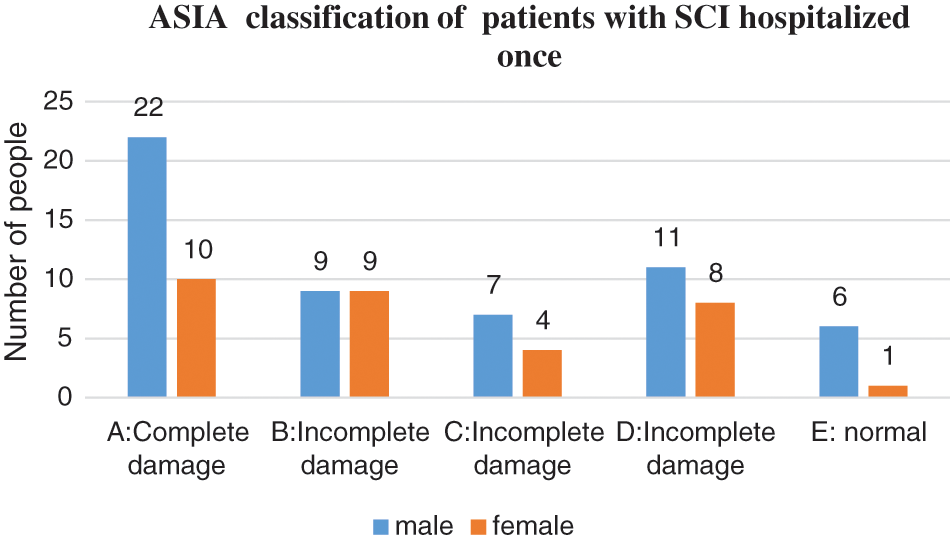
Figure 3: ASIA classification of patients with SCI hospitalized once
The ASIA impairment classification of patients with spinal cord injury, who are hospitalized in the rehabilitation department more than two times, is shown in Tab. 3. The number of the patients is 50.

Fig. 4 shows the number of male and female patients in each ASIA grade among the 50 patients. It can be seen that the proportion of male patient with spinal cord injury is higher than that of female from the data.
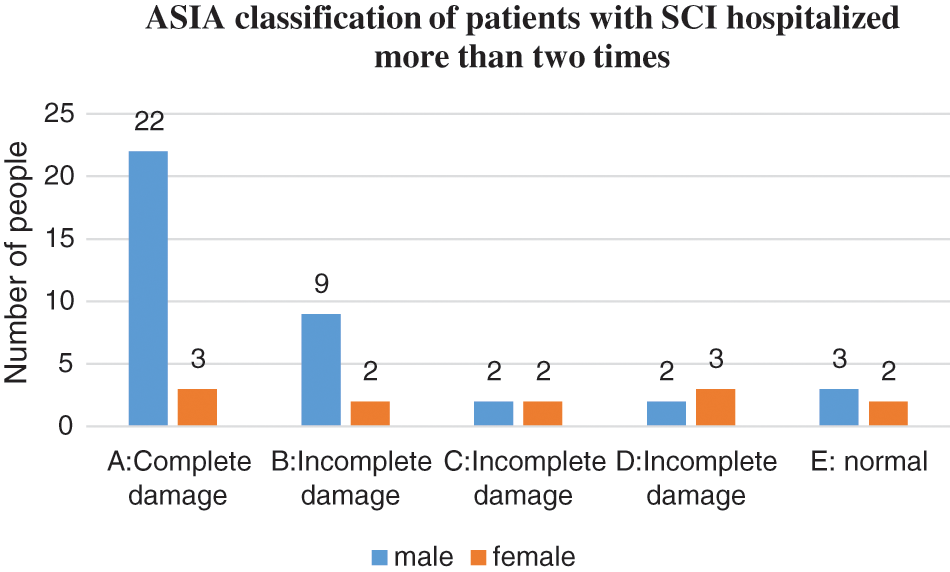
Figure 4: ASIA classification of patients with SCI hospitalized more than two times
ASIA impairment classification is not only convenient for clinical diagnosis, but also can be used to judge the prognosis of patients. Although grades B-D are incomplete injuries, the patients can be further graded according to functional movement and orientation. As can be seen from the above statistics, males account for a high proportion of spinal cord injury patients. The traumatic factors of patients are falling from heights, traffic accidents, and heavy objects, which may be related to the high proportion of men engaged in social activities.
The number of patients with spinal cord injury, who hospitalized once in the rehabilitation department of the hospital, was 46 with agricultural household registration, accounting for 52.9% of the total, and 41 patients with non-agricultural household registration, accounting for 47.1% of the total. The number of patients with spinal cord injury, who hospitalized for more than two times (including the two times) in the rehabilitation department of the hospital, was 26 with agricultural household registration, accounting for 52% of the total, and 24 patients with non-agricultural household registration, accounting for 48% of the total. As is shown in Fig. 5. Moreover, it is shown that China’s critical illness medical insurance system has played a positive role in recent years, enabling everyone to enjoy equal medical rights.
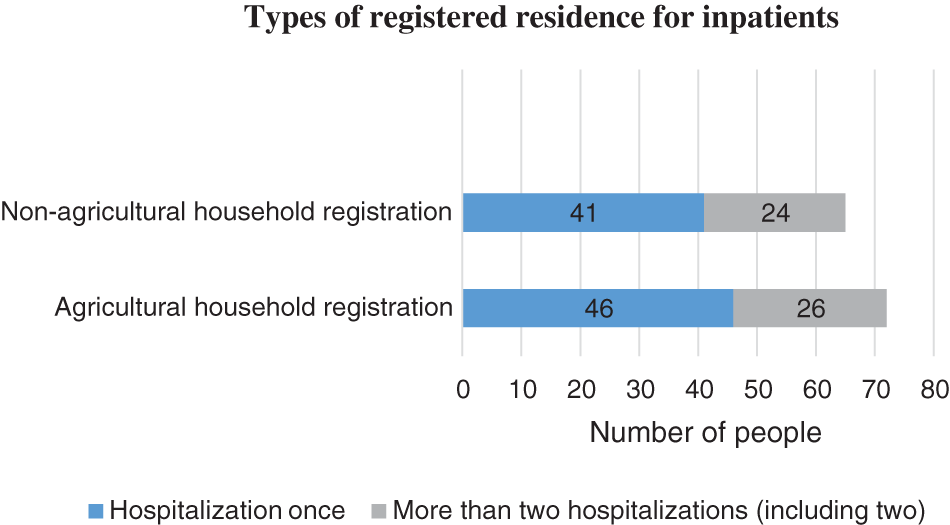
Figure 5: Types of registered residence for inpatients
The number of patients with spinal cord injury, who hospitalized once in the rehabilitation department of our hospital and lived more than 200 kilometers away from the hospital, was 48, accounting for 55.2% of the total; and 39 patients living within 200 kilometers of the hospital, accounting for 44.8% of the total. The number of patients with spinal cord injury, who hospitalized for more than two times (including the two times) in the rehabilitation department of the hospital and lived more than 200 kilometers away from the hospital, was 23, accounting for 46% of the total; and 27 patients living within 200 kilometers of the hospital, accounting for 54% of the total. As is shown in Fig. 6. This shows that after maximizing the benefits of medical information, patients and their families should fully consider the importance of the distance between the places of residence.
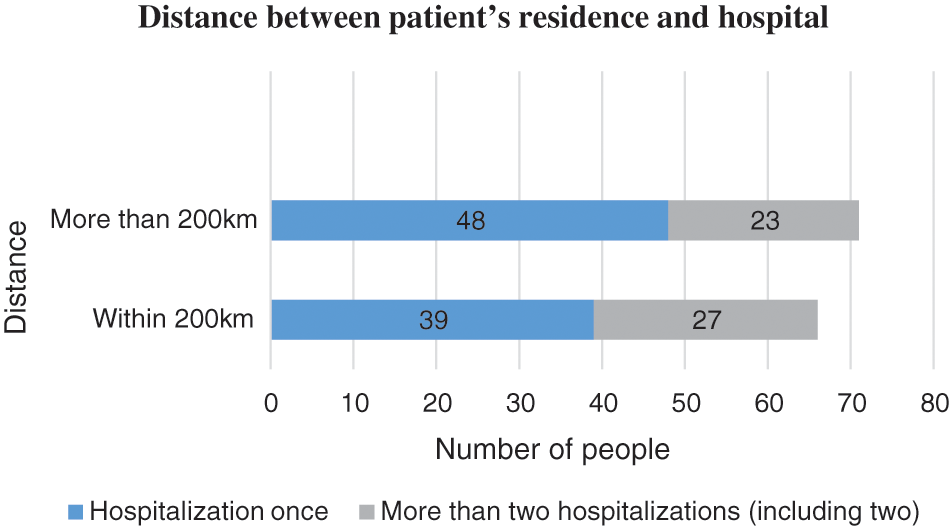
Figure 6: Distance between patient’s residence and hospital
The purpose of spinal cord injury rehabilitation is to increase patients’ ability to take care of themselves, so that patients can integrate into the society as much as possible and cultivate the ability to live independently. While considering the degree of the patient’s condition and the level of damage, medical staff should fully consider the optimization and balance of medical resources. It is very important for caregivers of patients with spinal cord injury, including the cognitive ability of the caregiver. And the time spent with them also needs to be fully evaluated. Psychological rehabilitation of patients with spinal cord injury is also very important. Professional psychological support needs to be provided at each rehabilitation stage. Not only the family members of the patients, but also professional psychotherapists are required to participate.
Overall, the rehabilitation of spinal cord injury is a long-term process. Medical staff and community must fully consider the social and non-social factors that affect rehabilitation after spinal cord injury, conduct systematic rehabilitation evaluation, and formulate rehabilitation nursing goals, so as to achieve precise rehabilitation.
Funding Statement: This work is supported by Health Research Project for Cadres of Sichuan Province (No. 2020-214). Min Rao received the grant and the URLs to sponsors’ websites is http://wsjkw.sc.gov.cn/scwsjkw/index.shtml.
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
1. Y. J. Ren, Y. Leng, J. Qi, K. S. Pradip, J. Wang et al., “Multiple cloud storage mechanism based on blockchain in smart homes,” Future Generation Computer Systems, vol. 115, pp. 304–313, 2021. [Google Scholar]
2. A. Richard-Denis, M. Beauséjour, C. Thompson, B. H. Nguyen and J. M. Mac-Thiong, “Early predictors of global functional outcome after traumatic spinal cord injury: A systematic review,” Journal of Neurotrauma, vol. 35, no. 15, pp. 1705–1725, 2018. [Google Scholar]
3. C. P. Ge, Z. Liu, J. Y. Xia and L. M. Fang, “Revocable identity-based broadcast proxy re-encryption for data sharing in clouds,” IEEE Transactions on Dependable and Secure Computing, vol. 18, no. 3, pp. 1214–1226, 2021. [Google Scholar]
4. J. Wang, C. Y. Jin, Q. Tang, N. X. Xiong and G. Srivastava, “Intelligent ubiquitous network accessibility for wireless-powered MEC in UAV-assisted B5G,” IEEE Transactions on Network Science and Engineering, vol. 8, no. 4, pp. 2801–2813, 2021. [Google Scholar]
5. E. Bourassa-Moreau, J. M. Mac-Thiong, A. Li, D. Ehrmann Feldman, D. H. Gagnon et al., “Do patients with complete spinal cord injury benefit from early surgical decompression? Analysis of neurological improvement in a prospective cohort study,” Journal of Neurotrauma, vol. 33, no. 3, pp. 301–306, 2016. [Google Scholar]
6. T. Li, N. P. Li, Q. Qian, W. Xu, Y. Ren et al., “Inversion of temperature and humidity profile of microwave radiometer based on bp network,” Intelligent Automation & Soft Computing, vol. 29, no. 3, pp. 741–755, 2021. [Google Scholar]
7. Y. J. Ren, F. Zhu, J. Wang, P. Sharma and U. Ghosh, “Novel vote scheme for decision-making feedback based on blockchain in internet of vehicles,” IEEE Transactions on Intelligent Transportation Systems, vol. 23, no. 2, pp. 1639–1648, 2022. [Google Scholar]
8. X. R. Zhang, X. Sun, X. M. Sun, W. Sun and S. K. Jha, “Robust reversible audio watermarking scheme for telemedicine and privacy protection,” Computers, Materials & Continua, vol. 71, no. 2, pp. 3035–3050, 2022. [Google Scholar]
9. C. P. Ge, W. Susilo, J. Baek, Z. Liu, J. Y. Xia et al., “Revocable attribute-based encryption with data integrity in clouds,” IEEE Transactions on Dependable and Secure Computing, vol. 21, no. 5, pp. 1–12, 2021. [Google Scholar]
10. K. Stephan, S. Huber, S. Häberle, K. G. Kanz, V. Bühren et al., “Spinal cord injury incidence, prognosis, and outcome: An analysis of the Trauma Register DGU,” The Spine Journal, vol. 15, no. 9, pp. 1994–2001, 2015. [Google Scholar]
11. L. Ren, J. Hu, M. Li, L. Zhang and J. Xia, “Structured graded lung rehabilitation for children with mechanical ventilation,” Computer Systems Science & Engineering, vol. 40, no. 1, pp. 139–150, 2022. [Google Scholar]
12. Y. J. Ren, J. Qi, Y. P. Liu, J. Wang and G. Kim, “Integrity verification mechanism of sensor data based on bilinear map accumulator,” ACM Transactions on Internet Technology, vol. 21, no. 1, pp. 1–20, 2021. [Google Scholar]
13. L. M. Fang, M. H. Li, Z. Liu, C. T. Lin, S. L. Ji et al., “A secure and authenticated mobile payment protocol against off-site attack strategy,” IEEE Transactions on Dependable and Secure Computing, vol. 21, no. 10, pp. 1–12, 2021. [Google Scholar]
14. M. Nott, I. Baguley, R. Heriseanu, G. Weber, J. Middleton et al., “Effects of concomitant spinal cord injury and brain injury on medical and functional outcomes and community participation,” Topics in Spinal Cord Injury Rehabilitation, vol. 20, no. 3, pp. 225–235, 2014. [Google Scholar]
15. C. P. Ge, W. Susilo, J. Baek, Z. Liu, J. Y. Xia et al., “A verifiable and fair attribute-based proxy re-encryption scheme for data sharing in clouds,” IEEE Transactions on Dependable and Secure Computing, vol. 21, no. 7, pp. 1–12, 2021. [Google Scholar]
16. J. Wang, H. Han, H. Li, S. M. He, P. K. Sharma et al., “Multiple strategies differential privacy on sparse tensor factorization for network traffic analysis in 5G,” IEEE Transactions on Industrial Informatics, vol. 18, no. 3, pp. 1939–1948, 2022. [Google Scholar]
17. Y. J. Ren, F. J. Zhu, S. P. Kumar, T. Wang, J. Wang et al., “Data query mechanism based on hash computing power of blockchain in Internet of Things,” Sensors, vol. 20, no. 1, pp. 1–22, 2020. [Google Scholar]
18. B. Sharma, C. Bradbury, D. Mikulis and R. Green, “Missed diagnosis of traumatic brain injury in patients with traumatic spinal cord injury,” Journal of Rehabilitation Medicine, vol. 46, no. 4, pp. 370–373, 2014. [Google Scholar]
19. C. B. Liu, K. L. Li, K. Q. Li and R. Buyya, “A new service mechanism for profit optimizations of a cloud provider and its users,” IEEE Transactions on Cloud Computing, vol. 17, no. 3, pp. 845–858, 2017. [Google Scholar]
20. C. P. Ge, W. Susilo, Z. Liu, J. Y. Xia, L. M. Fang et al., “Secure keyword search and data sharing mechanism for cloud computing,” IEEE Transactions on Dependable and Secure Computing, vol. 18, no. 6, pp. 2787–2800, 2021. [Google Scholar]
21. J. H. Piatt, “Pediatric spinal injury in the US: Epidemiology and disparities,” Journal of Neurosurgery: Pediatrics, vol. 16, no. 4, pp. 463–471, 2015. [Google Scholar]
22. Y. J. Ren, K. Zhu, Y. Q. Gao, J. Y. Xia, S. Zhou et al., “Long-term preservation of electronic record based on digital continuity in smart cities,” Computers Materials & Continua, vol. 66, no. 3, pp. 3271–3287, 2021. [Google Scholar]
23. X. R. Zhang, W. F. Zhang, W. Sun, X. M. Sun and S. K. Jha, “A robust 3-D medical watermarking based on wavelet transform for data protection,” Computer Systems Science & Engineering, vol. 41, no. 3, pp. 1043–1056, 2022. [Google Scholar]
24. J. Y. Hu, K. L. Li, C. B. Liu and K. Q. Li, “A game-based price bidding algorithm for multi-attribute cloud resource provision,” IEEE Transactions on Services Computing, vol. 21, no. 2, pp. 1–12, 2021. [Google Scholar]
25. A. Richard-Denis, D. Feldman, C. Thompson and J. M. Mac-Thiong, “Prediction of functional recovery six months following traumatic spinal cord injury during acute care hospitalization,” The Journal of Spinal Cord Medicine, vol. 41, no. 3, pp. 309–317, 2018. [Google Scholar]
26. Y. J. Ren, J. Qi, Y. P. Cheng, J. Wang and O. Alfarraj, “Digital continuity guarantee approach of electronic record based on data quality theory,” Computers Materials & Continua, vol. 63, no. 3, pp. 1471–1483, 2020. [Google Scholar]
27. X. Zhou, K. L. Li, Y. T. Zhou and K. Q. Li, “Adaptive processing for distributed Skyline queries over uncertain data,” IEEE Transactions on Knowledge & Data Engineering, vol. 28, no. 2, pp. 371–384, 2016. [Google Scholar]
28. M. Haldrup, S. Dyrskog, M. M. Thygesen, H. Kirkegaard, H. Kasch et al., “Initial blood pressure is important for long term outcome after traumatic spinal cord injury,” Journal of Neurosurgery: Spine, vol. 33, no. 2, pp. 256–260, 2020. [Google Scholar]
29. M. Haldrup, O. S. Schwartz, H. Kasch and M. M. Rasmussen, “Early decompressive surgery in patients with traumatic spinal cord injury improves neurological outcome,” Acta Neurochirurgica, vol. 161, no. 10, pp. 2223–2228, 2019. [Google Scholar]
30. Y. J. Ren, Y. Leng, Y. P. Cheng and J. Wang, “Secure data storage based on blockchain and coding in edge computing,” Mathematical Biosciences and Engineering, vol. 16, no. 4, pp. 1874–1892, 2019. [Google Scholar]
 | This work is licensed under a Creative Commons Attribution 4.0 International License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. |