 Open Access
Open Access
ARTICLE
IOT Assisted Biomedical Monitoring Sensors for Healthcare in Human
1 Department of ECE, Ramco Institute of Technology, Rajapalayam, 626117, India
2 Department of CSE, Sona College of Technology, Salem, 636005, India
3 Department of Mathematics, Ramco Institute of Technology, Rajapalayam, India
4 Government College of Engineering, Dharmapuri, India
* Corresponding Author: V. Nandini. Email:
Computer Systems Science and Engineering 2023, 45(3), 2853-2868. https://doi.org/10.32604/csse.2023.030538
Received 28 March 2022; Accepted 30 April 2022; Issue published 21 December 2022
Abstract
The Internet of Things (IoT) is a concept that refers to the deployment of Internet Protocol (IP) address sensors in health care systems to monitor patients’ health. It has the ability to access the Internet and collect data from sensors. Automated decisions are made after evaluating the information of illness people records. Patients’ health and well-being can be monitored through IoT medical devices. It is possible to trace the origins of biological, medical equipment and processes. Human reliability is a major concern in user activity and fitness trackers in day-to-day activities. The fundamental challenge is to measure the efficiency of the human system accurately. Aim to maintain tabs on the well-being of humans; this paper recommends the use of wireless body area networks (WBANs) and artificial neural networks (ANN) to create an IoT-based healthcare framework for hospital information systems (IoT-HF-HIS). Our evaluation system uses a server to estimate how much computing power is needed for modeling, and simulations of the framework have been done using data rate and latency requirements are implementing the energy-aware technology presented in this paper. The proposed framework implements several hospital information system case studies by building a time-saving simulation environment. As the world’s population ages, more and more people suffer from physical and emotional ailments. Using the recommended strategy regularly has been proven user-friendly, reliable, and cost-effective, with an overall performance of 95.2%.Keywords
Using an idea behind the Internet of Things, everyday objects and gadgets are given the ability to hear, sense, and communicate by exchanging data and communicating with one another [1]. The Internet of Things uses embedded systems, modulation schemes, sensor or access technologies, and applications to transform these standard things into smart ones [2]. IoT-based systems with worldwide connections may gather, manage, and share healthcare-related information, such as treatment, diagnostics, recovery, inventories, and medicine [3]. Healthcare services based on the Internet of Things contain wireless terminals and broadband connections that allow mobility [4]. Wi-Fi, 3G/4G/5G, Bluetooth, an indexing scheme, and other data analysis systems are all examples of IoT-enabled devices that could be found in an IoT-enabled environment [5]. Other examples include a smartphone, a computer, and a tablet device [6]. People or items can be identified, authorized, monitored, or sensed using IoT technology in the healthcare sector [7].
Internet of Things refers to a wide range of devices with low resources, such as implanted and transportable clothing, which boosts daily life effectiveness [8]. IoT health systems with processing speeds and sophisticated communication between physicians and patients are blamed for this high waiting period [9]. A doctor can monitor a patient’s health, how the biological device operates, and how it is handled using an IoT medical gadget [10]. Wireless body area networks are an essential part of the Internet of Things in healthcare [11]. Sensor networks and a proxy server are part of a WBAN [12]. Sensor nodes are equipment needs that may collect and transmit data from the human body [13], such as electrocardiograms (ECG), temperature, oxygen saturation, hypertension, and others through a wireless component to an internet connection [14].
Before being sent to the health-monitoring center, the data must be compressed, processed, or retrieved by the access point, which is indeed referred to as the central coordinator at this point [15]. Secure procedures for devices with poor battery life, limited processor power, and minimal storage capabilities are difficult to implement [16]. Medical IoT systems with device-to-device interaction necessitate this section’s investigation of security concerns [17]. WBANs for biological devices, where data throughput and transmission delay are critical quality of service (QoS) parameters, face substantial design challenges [18]. Inaccurate data may be gathered from patients’ physiological measurements if the QoS standards for certain measures are not met [19]. ECG, or any electrical impulses produced by the human body, are used in this process [20]. Instrumentation in the field of biomedical engineering assists doctors in diagnosing and treating patients [21]. This equipment combines engineering with medicine to benefit the general public’s health and well-being [22]. Knowledge and abilities are developed and applied to biomedical science [23]. Instrumentation in the field of biomedical engineering assists doctors in diagnosing as well as treating patients. Circuits and measurement methodologies are required to analyze biological signals and develop a medical gadget [24].
The major contribution of this paper is given as,
• It has been proposed to use WBAN to integrate all medical data into a single healthcare system hub.
• Developing an ANN-based model using data rate and latency requirements is presented in this paper.
• IoT-HF-HIS implement real-time predictions of the data acquired.
The structure of the paper is as follows: Section 2 literature studies involved in biomedical sensors in human health. Sections 3 and 4 of the proposed framework (IoT-HF-HIS) describe the performance evaluation of the WBAN and ANN components, respectively. Section 5 concludes the paper with a few last thoughts.
2 Background Researches Involved in Biomedical Sensors
The Internet of Things is a term for electronic connections that have the infrastructure with electronic sensors, and IoT healthcare may be created using a wide range of inexpensive sensors. It is worth noting the vulnerability of medical gadgets with low resources and unprotected Internet access. Thus, this area focuses on the investigation of secure authentication methods, the development of protocols, and the improvement of the confidentiality of communications of medical equipment.
Families of children with autism spectrum disorder based biomedical sensor (ASD-BMS) face a variety of barriers to timely diagnosis and care, according to Woo [25]. Three independent coders were present at the focus group sessions that transcribed the audio and reviewed it verbatim for accuracy and completeness. Several common themes were found regarding early diagnosis, and care challenges with focus group transcripts for researchers’ discoveries of ASD have implications for practice and future research.
Prior to surgery, Al-Turjman [26] deployed a fog-assisted healthcare architecture to reduce latency (FAHA-RL). Using this approach, patients can receive therapy at the right time and place. Doctors can give medical services via telesurgery in a variety of ways. A tele-use surgery of artificial intelligence, tactile Internet, and 5G technology reduces resource scheduling issues. Low-cost ECG health surveillance and automated review and warning system (ARWS) is reliable remote management, according to Brown Manikandan et al. [27]. Sensor nodes and a fog layer powered by IoT are part of the device, and data from the sensor nodes are transmitted to an intelligent door that the appropriate attendants can open. As a result of the device’s capabilities, users can receive real-time warnings, information acquired automatically, and other useful resources.
A systematic treatment enhancement program for bipolar disorder (STEP-BD) was proposed by Das et al. [28] to build an externally relevant public health strategy model for the treatment quality problems connected with bipolar disorder therapy. When it comes to selecting and certifying clinical care centers, this standard’s criteria for clinical management and sequential treatment techniques were examined in this paper. Diabetic patients can be cared for in an end-to-end safe manner using the healthcare model (ESMEHM) proposed by Fang et al. [29]. It includes wearable for monitoring the patient’s diabetic condition and anticipating its condition based on various indicators. A medical box is used to set the correct dosage and remind consumers to take their prescription on time. Insulin dosage will be maintained and continuously monitored by the gadget if it is kept cool enough. The hypothesis for the research is formulated as a consequence of the thorough literature review. Thus, IoT-HF-HIS has been presented to represent all medical data to a single-centre, addressing the existing model issues in ASD-BMS, FAHA-RL, ARWS, STEP-BD, ESMEHM; thus, IoT-HF-HIS has been proposed. It has been suggested that IoT-HF-HIS can improve accuracy ratio, prediction ratio, execution time, decision table, memory occupying, time taken for data transfer, and efficiency ratio by employing IoT.
3 IoT-Based Healthcare Framework for Hospital Information Systems (IoT-HF-HIS)
Health care comprises protecting or increasing health via the treatment, diagnosis, therapy, cure of sickness, illness, impairment, and other individual physical as well as psychological limitations. Health providers or allied healthcare sectors provide health care. The health sector comprises surgery, medicine, pediatrics, counselling, various treatments, sports, and other medical professions. Basic, intermediate, and quaternary care, as well as public health care, is all included in this. Existing data infrastructure can be leveraged to implement the many IoT-based models that have been mentioned.
IoT-HF-HIS framework is shown in Fig. 1. Proximity information is collected using wireless networks and sent to a server via the mobile data network using an ANN technique. These hardware solutions can transmit real-time data using the wireless sensor principle. Each piece of information gathered by medical sensors and biosensors is combined. IoT-HF-HIS design captures behavioural and physiological data from the patient quantitatively and qualitatively. People in generally good health have been shown to have decreased immunity levels in studies. Furthermore, those with chronic health conditions have a greater sensitivity. The IoT-HF-HIS architecture and the various datasets described in Tab. 1 must continuously monitor these patients. Data mining is used to gather all IoT-HF-HIS as the first stage in a decision-making framework. Data mining is the process of extracting useful information from large amounts of relevant information from IoT data providers in real-time. In other words, the research depends on a time-based examination of diverse IoT data. Because patient well-being is a time-sensitive characteristic, data mining relies on pure sequential mining methods. Using time series models (TSMs) and sequential mining, data can be gathered and analyzed in new ways. It is possible to derive time series models theoretically.
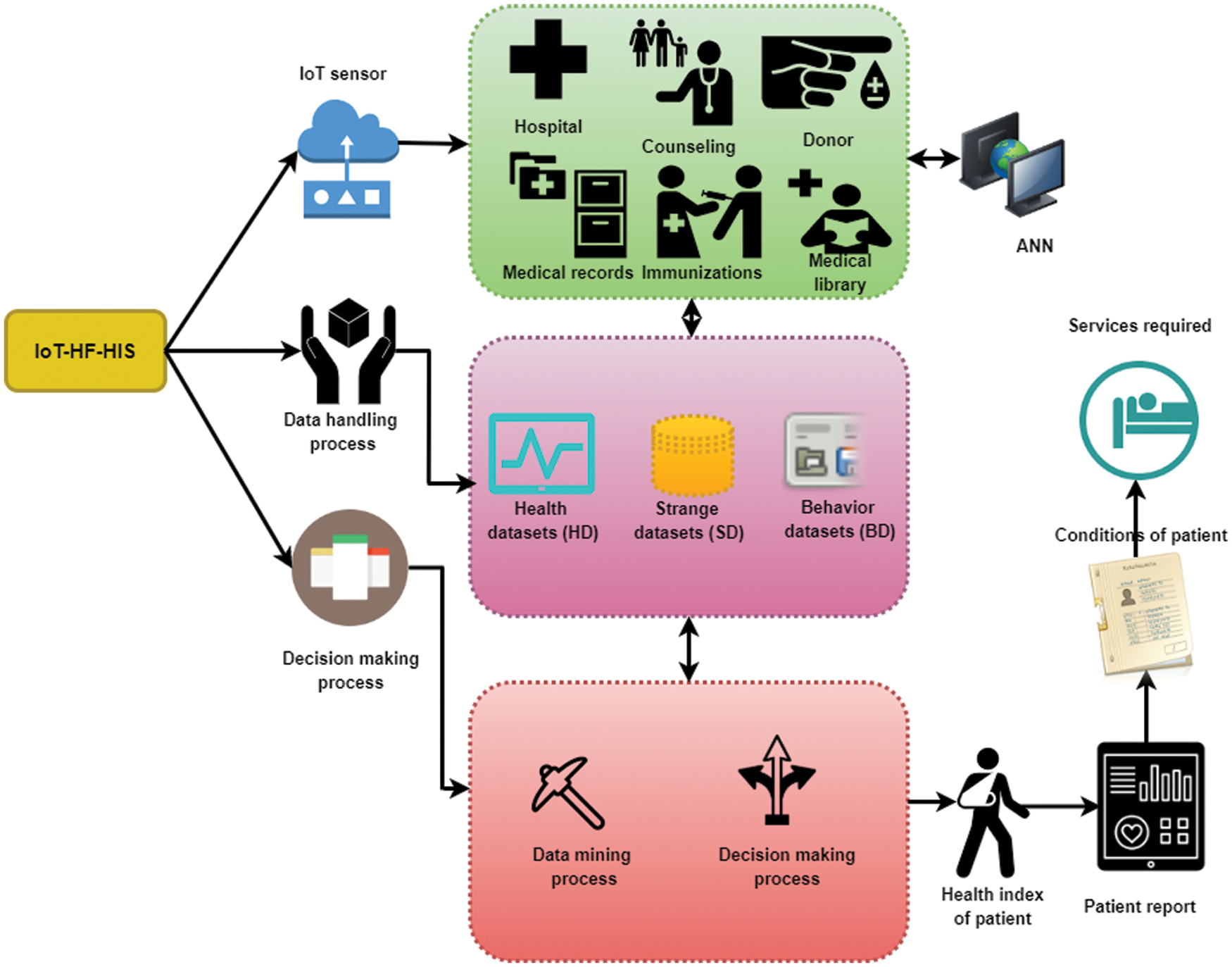
Figure 1: IoT-HF-HIS process framework

In this case, the data processing framework immediately process the hospital’s degree of impact (DOI) surpasses a certain threshold, the ECG is sent to the Internet for extensive analysis specified threshold can be derived as,
whereas
Shifting window techniques
Patients with a lower patient value
Values in the health dataset have a direct impact on healthcare and well-being. A patient’s bodily sensor network provides these values. To monitor the patient’s health, sensors are employed, illustrated in Tab. 1. It is evident from numerous researches that patients’ health is more closely tied to their surroundings than previously thought. Strange dataset collects and preserves data that is useful to the environment. Surrounding air quality, noise, temperature, and other factors are covered. Sensors placed in various parts of a room collect this information. For this purpose, sensors are placed throughout the space at various locations. Bed rest is recommended for patients with regular health difficulties. Patients will experience soreness, stress, and restlessness due to prolonged bed rest. The bed and the patient’s body are both fitted with sensors to collect data on the patients’ behavior.
An electrophysiological method is used to treat behavioral disorders using ECG and electromagnetic generator (EMG) sensors. There are trillions of data points in the ECG signals that have yet to be examined on a data management system.
IoT in biomedical
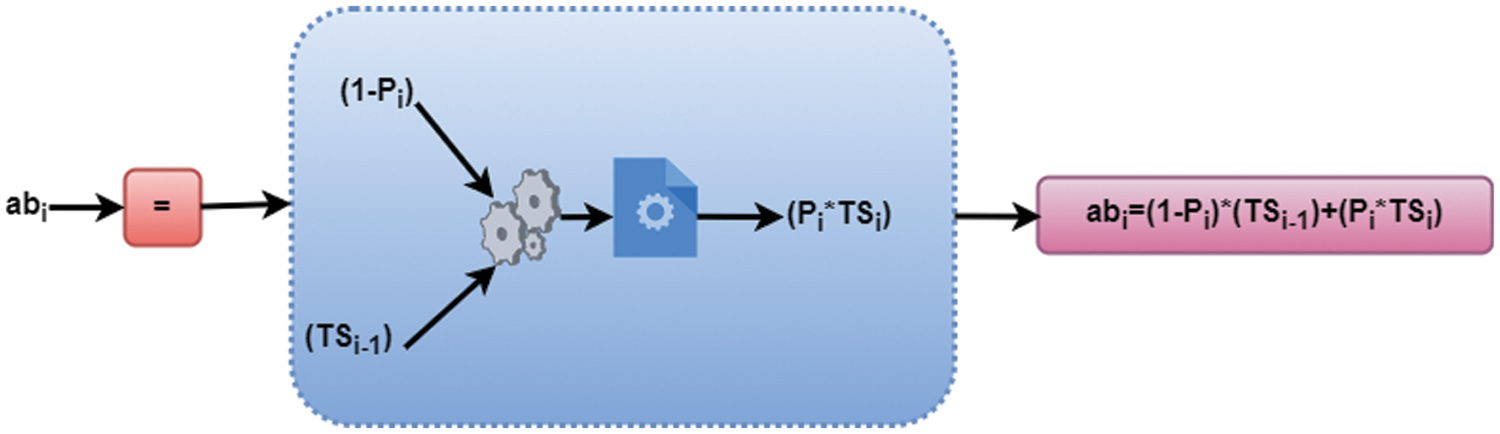
Figure 2: Representation of WBANs validation process
Superframe duration
They focused on abnormality identification
Fig. 3 depicts how artificial neural networks can be used in healthcare. It is an apprentice model built on the structure of a biological neural network, and it is an algorithm based on the human visual/auditory brain. The genuine mental processes in this incredible image can be achieved using an IoT gateway for a million light-years away. Layers “input,” “intermediate,” and “output” makes up a neural network’s overall structure. Consequently, how many neurons per layer and how many total layers there are largely dependent on the complexity of the system. The best network architecture must be determined. The three-layer structure of current ANN architecture is the most common design choice using IoT gateway.
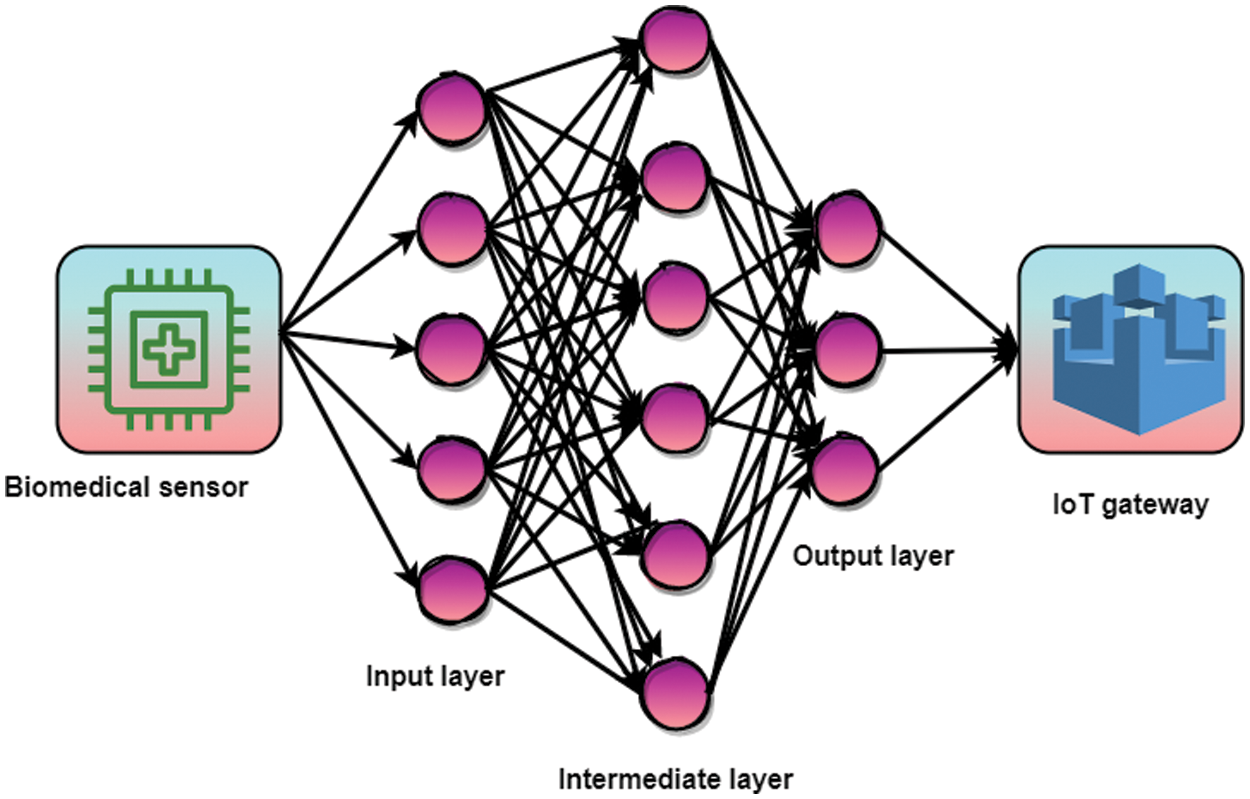
Figure 3: Biomedical sensor using IoT gateway in ANN process
An artificial neural network (ANN) models the human brain’s activities in a computer simulation. An ANN is a processing unit that has inputs and outputs. This layer’s neurons receive the information from the input layer and then pass it along via weighted ties to the neurons in the top-most layer. Mathematically, the data is saved and transmitted to the next layer of neurons. The neurons in the last layer that provide the network’s output are described below equations,
The hidden layer
As shown in Eq. (8),
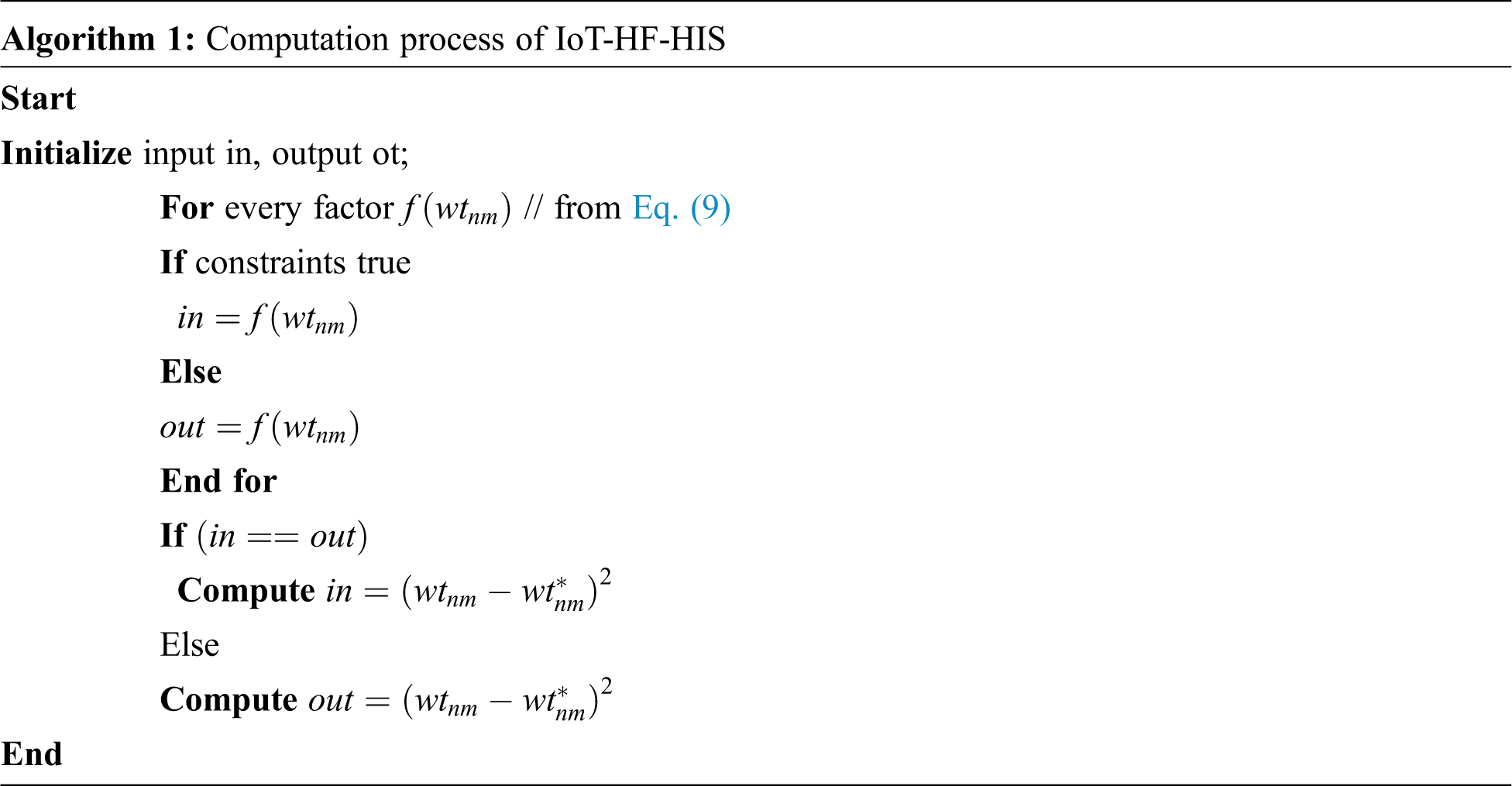
There are three identifiers in Eq. (9) that are utilized to generate weight values
In Eqs. (10) and (11), the parameter
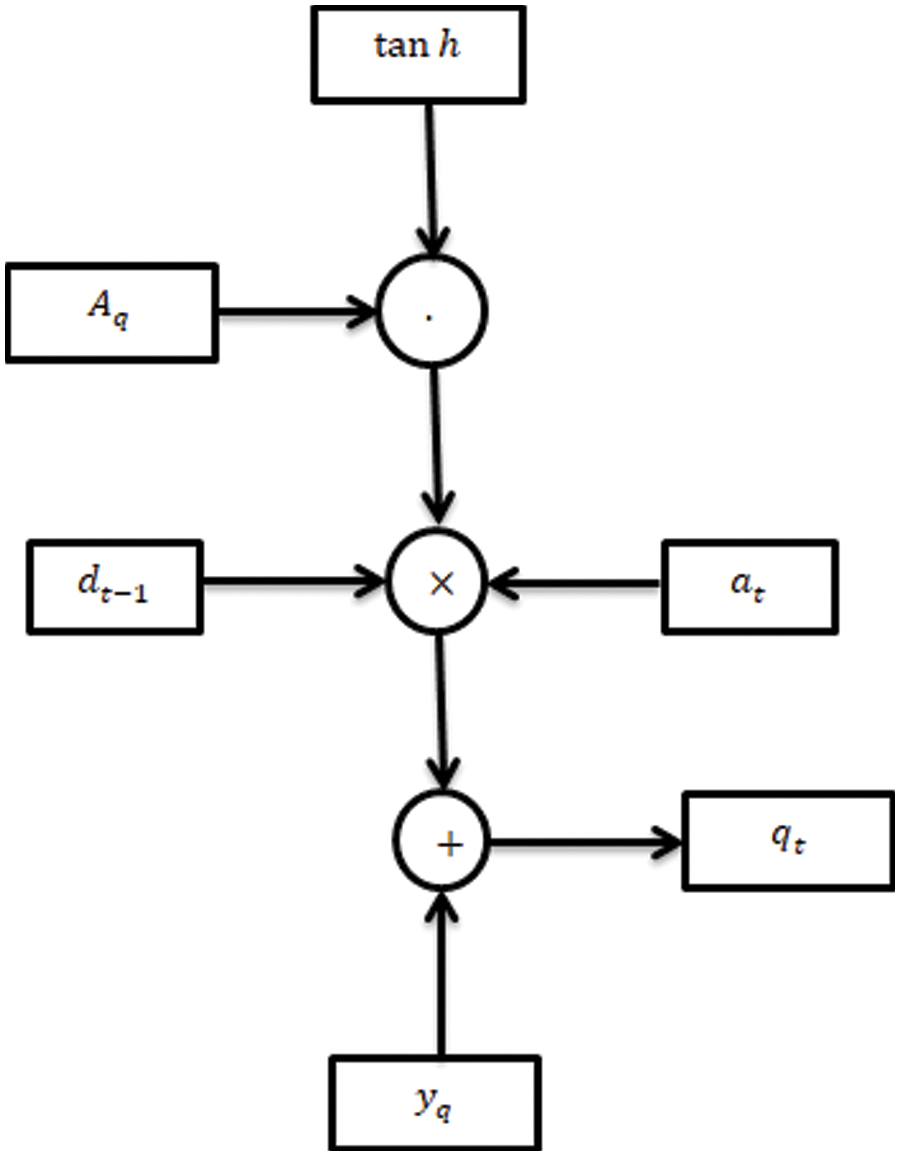
Figure 4: Biomedical sensor process using ANN
Researchers are concerned that artificial neural networks, which differ from the human brain, cannot forecast the speed at which simple machines calculate. The artificial neural network model is nearly wiped out in the IoT-HF-HIS system. Naturally, this version is about the machine’s output’s key relevance because the more hidden layers there are, the more unsettled the learning issue becomes. There are various data points processed by artificial neural networks (ANNs).
The biological sensor that deploys the data status and normal and problematic conditions detects the data. In this IoT-HF-HIS strategy, the sensor nodes are deployed in the IoT, and the algorithm is used to evaluate the healthcare situation. The system’s robustness is required during implementation in terms of equality and accountability. In the course of implementing IoT devices, the following issues have arisen. Numerous image centers and biomedical sensor models for images of a single domain spanning multiple photos have been widely predicted in practical healthcare situations
As Eq. (12)
As Eq. (13)
As Eq. (14) this Eq. describes how probable it is that health data
The sensor collects various biometric and medical data based on the data type. If the data is biometric, it includes another patient’s fingerprints, retinal, and body recognition state. Sensor hubs in biomedical are connected to various devices like ECG, and other patient data are the focus of healthcare observation data, on the other hand, are illustrated in Fig. 5. A biometric and medial observation combination defines the data and provides it to the database server on time. The patient’s state is detected, and the collected data are determined by equating the Eq. above (6). The Internet uses the devices’ data to classify the data into normal and emergency data. There are both standard and emergency datasets available for data detection. Medical and biometric data are then separated and archived for future use after being detected through the gateway. The biomedical sensor data identifies the current status and offers relevant responses such as a biomedical interpreter, sensor library, sensor detection, and mapping. An abnormality is recognized by analyzing the data from the multiple sensors at different intervals. Our approach improves service delivery rates by delivering a notice before an emergency situation develops. The difference between the patient’s normal and emergency states is calculated in the following sessions through the above algorithm.
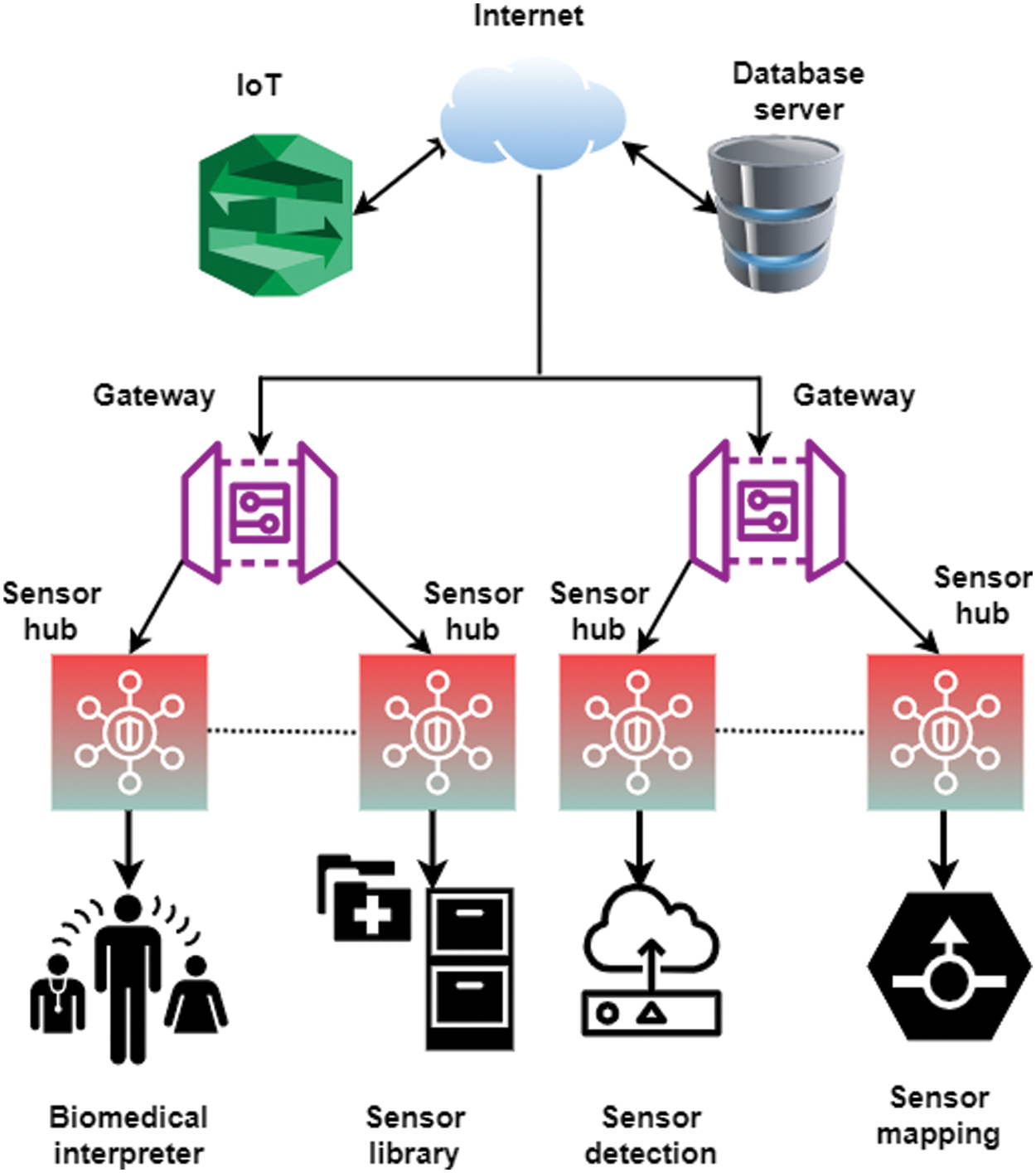
Figure 5: Biomedical sensors in IoT platform
However, key challenges include managing WBNs and routine work, medication adherence, inefficient medical diagnostics, other essential diseases; ineffective cost-effectiveness; and solving ANN ethics problems in medical practice. The proposed IoT-HF-HIS achieves accuracy, prediction, execution time, and decision-making using IoT and efficiency ratios.
The OPNET simulations used to assess the proposed IoT-HF-HIS performance are discussed in this section. There are 16 user devices and 90 sensor nodes in this simulation. Fig. 1 depicts the network’s model, which uses a centralized server as a data analyst. The existing 15-interval response recommendation is incorporated into this system. The server provides 1TB of storage and a speed of processing of 2.4 GHz. Data consumption, accuracy, delivering services ratio, and reaction time are used to measure performance. In addition to assessing the suggested method’s consistency, other methods will be compared with other traditional methods.
The feedback mechanism is employed in this project’s suggestion model. The feedback is based on the improved processing and the efficient mapping of similar data. These resources are put to use by evaluating how well they can mirror the previous state. As part of the matching process, a suggestion model is utilized, and the feedback is sent out immediately. Results and discoveries from Tab. 2 are summarized above from Eq. (4). Numerous minor medical diagnoses have been made where IoT uses are first reported.

Because of the widespread use of digital communications in healthcare, unauthorized individuals may alter or introduce inaccurate information. Classifying data as normal or abnormal is done using IoT mentioned in above Fig. 6a is obtained with an overall 91.3%. Patients can be warned using the IoT layer if two critical metrics fall outside their acceptable range. Use data to predict sensor readings from Eq. (8). To improve patient assistance and patient care, among other things, this project will investigate the healthcare sector are calculated from Fig. 6b with an achievement of 91.7%. Patient aid processes are less effective since the traditional patient assistance system cannot accurately predict healthcare data and demand. Wearable and remote healthcare data can accurately anticipate patient data using the IoT-HF-HIS system.
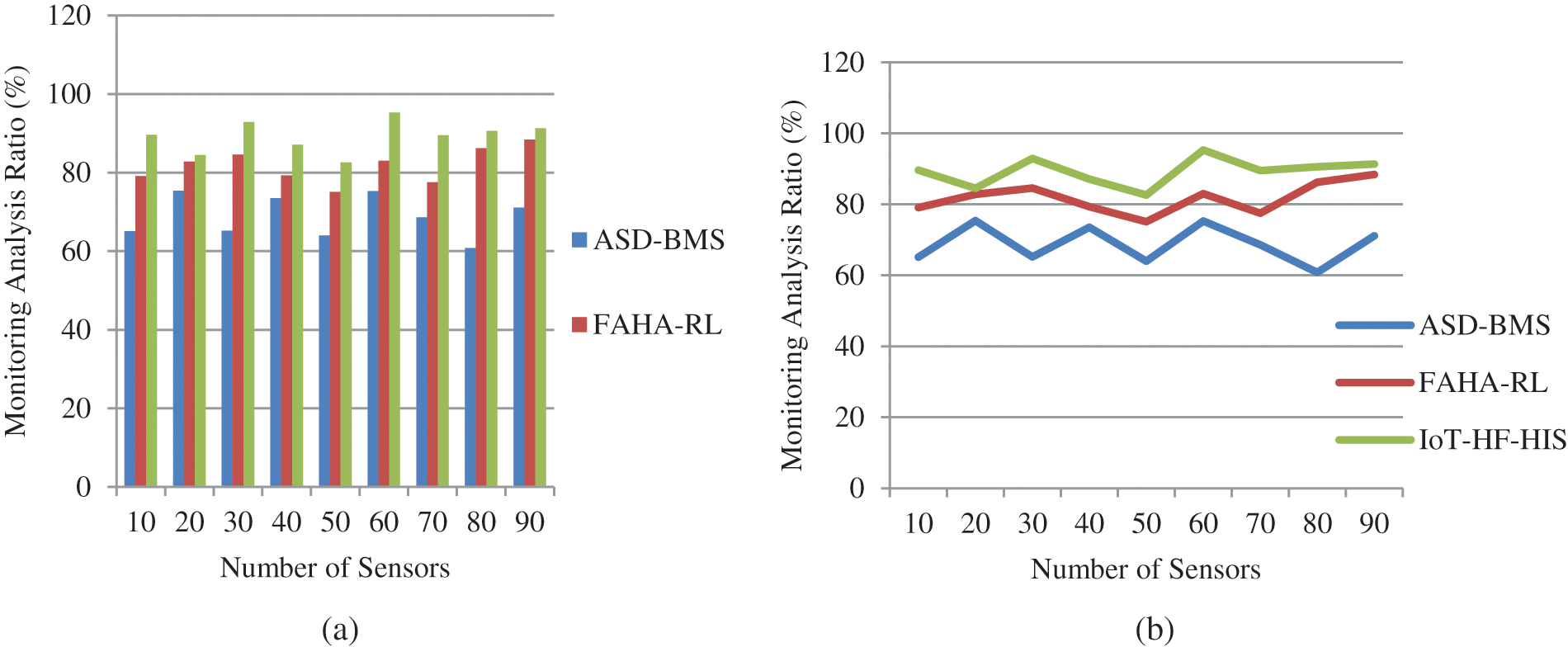
Figure 6: (a) and (b) Monitoring ratio analysis
The aged, severely disabled, and hospitalized patients can all get care in the comfort of their own homes thanks to the advancements in healthcare monitoring technology shown in Fig. 7a and achieved a latency rate of 93.4%. IoT-based remote monitoring of physiological parameters in an environment other than a health centre can be accomplished by a patient’s home, residential, and medical facility using data and communications technology from Eq. (5), Healthcare monitoring allows patients to remain in their homes while receiving adequate care, which is less expensive and more complex than traditional hospitalization. Patient monitoring has many benefits, such as earlier discharge from the hospital and better care in the hospital and elsewhere, shown in Fig. 7b by a numerical result of 94.1%. Healthcare providers are increasingly using IoT-HF-HIS to monitor and analyze patient data.
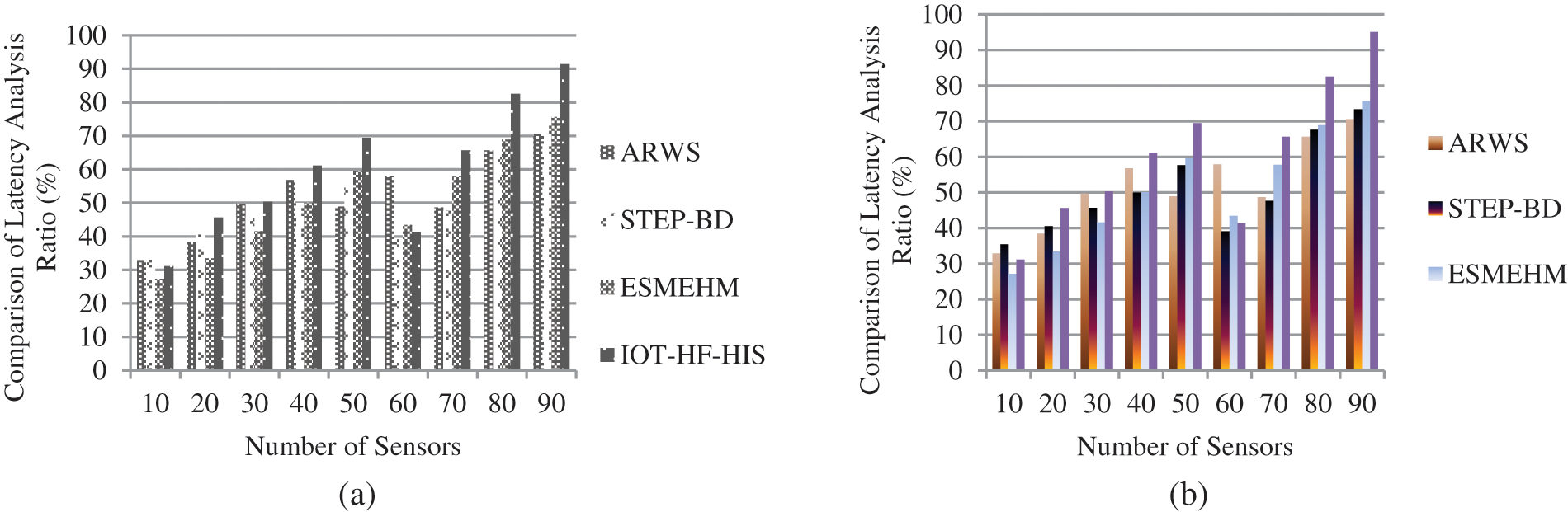
Figure 7: (a) and (b) Comparison of latency ratio
From the above Tab. 3 prediction ratio analysis is illustrated for the sensors with a patient in an intensive care unit (ICU). General ward decline can be predicted using predictive medical analytics that can identify high-risk patients in their homes and discourage readmission to the hospital. For the suggested IoT-HF-HIS, the greatest prediction ratio of 93.1% is observed with the sensors of 90 based on Eq. (10). With access to a wealth of information, doctors and organizations can make more accurate diagnoses and deliver better care promptly. At the same time, researchers can learn more about the mechanisms behind diseases to better forecast illness. In predictive analytics, various data analysis, predictive modeling, and deep learning technologies are used to forecast future or unforeseeable events by analyzing real and historical evidence.

Several benefits come from having access to information, including improved diagnosis and timely treatment, and enhanced insight into the causes of disease using sensors are defined in Fig. 8a. Real-time and population-based IoT with a large number of patients have the same issue: long execution times, whereas our proposed system executed faster when compared to other methods with 90.1% and Fig. 8b shows the graph of execution time for WBAN with an enhancement of 91.1%. When analyzing increasingly large sensor sizes in content measurement categories in Eq. (12) in ANN, it is necessary to phase in the system’s adoption. With smaller sensors, the method scales well using larger sizes, the average completion time per patient in each measurement group reduces significantly.
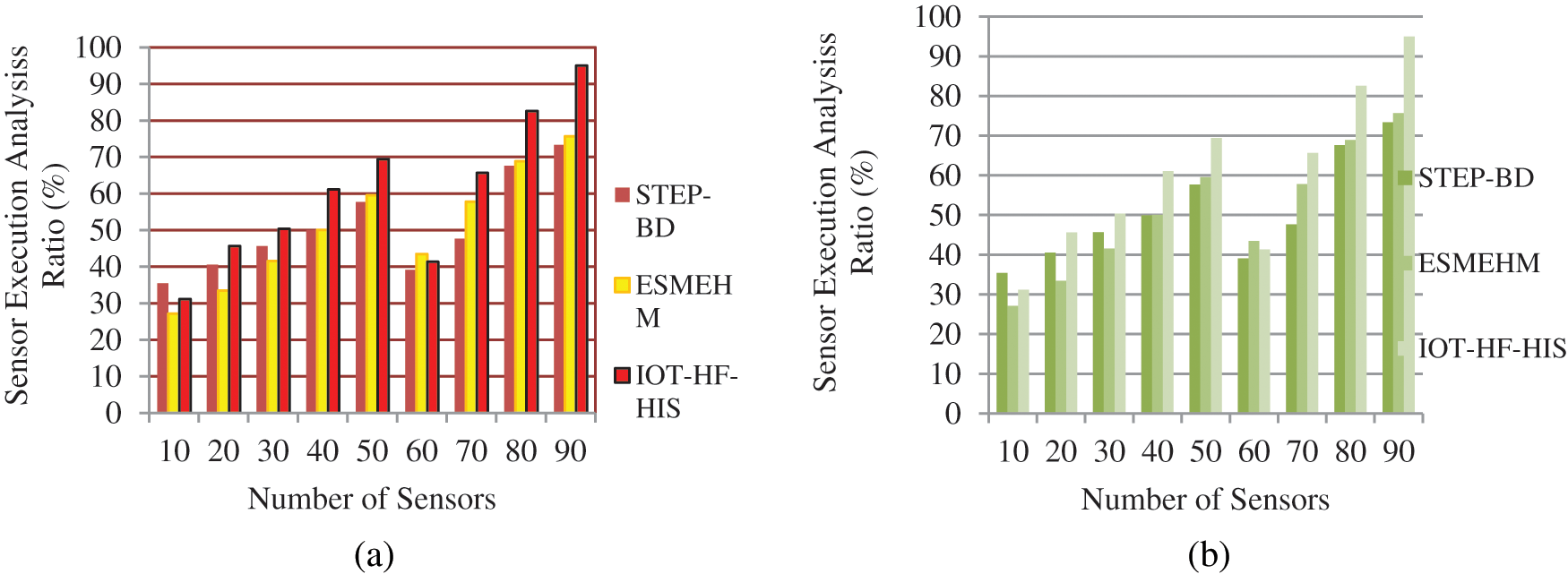
Figure 8: (a) and (b) Sensors execution time ratio
Sensors for individuals with persistent lung diseases, universal health care standard of living, and cardiovascular issues focus less on fall tracking and regular identification activities in smart environments and healthcare monitoring, according to Fig. 9a with the readiness of 95.2% in WBAN and Eq. (13). Smart healthcare surveillance systems based on the Internet of Things (IoT) can better handle circumstances or activities specified by the smart environment as 95.7% mentioned in Fig. 9b using ANN. A rough estimate of how long it will take to fulfill the customer’s request. Using an IoT sensor node, cloud computing is used to store medical records. It is possible to identify the IoT nodes connected to other nodes using the points on the planes.
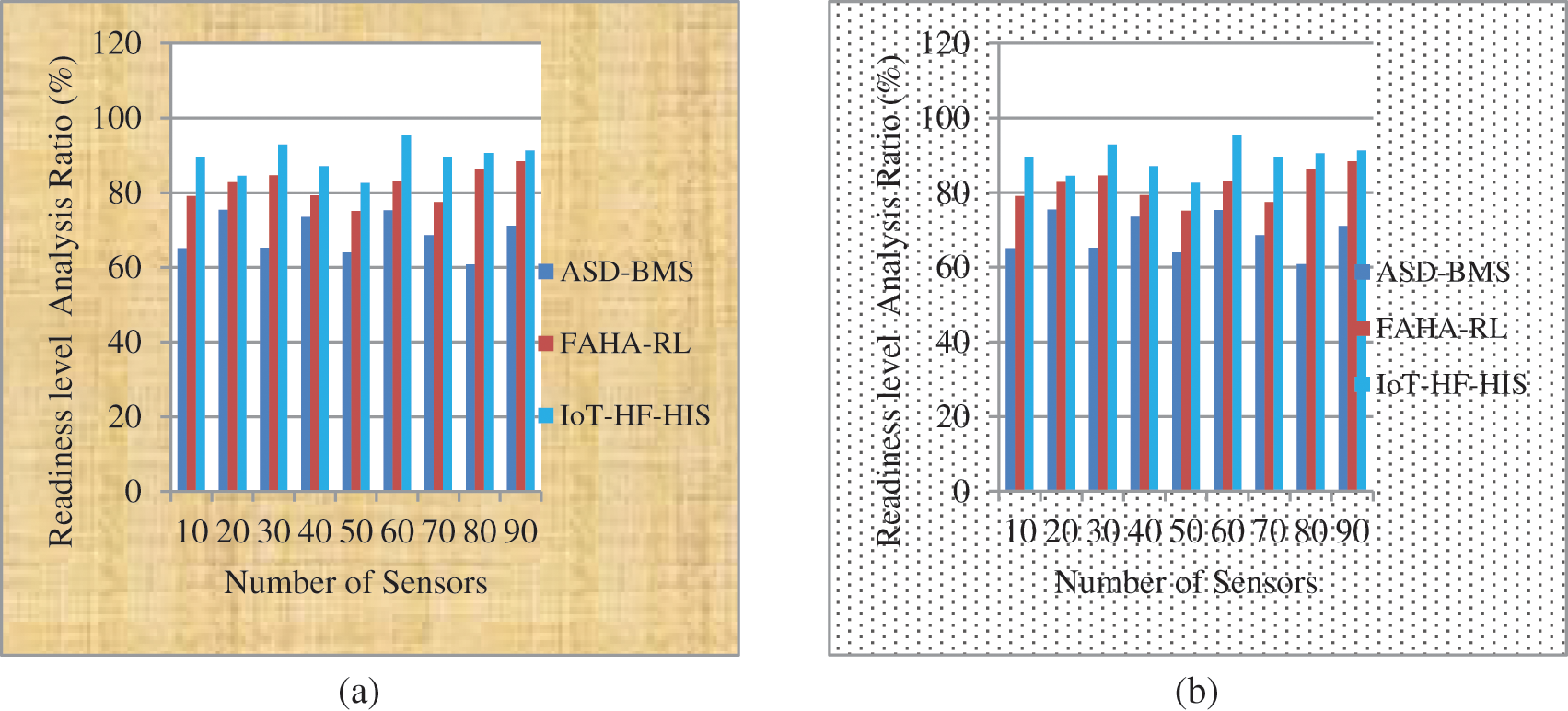
Figure 9: (a) and (b) IoT-HF-HIS framework level of preparation for a smart environment
Regarding physical health monitoring systems, the IoT-HF-HIS approach outperforms the others in terms of standardization and effectiveness compared to the WBANs method. Compared to other conventional methods, IoT-based physical sensor-based health monitoring systems are better at assuring standards and efficacy across the amount of iterations estimated using Eq. (7), as shown in Fig. 10a. Continuous and discontinuous biometric and medical data are used to create the response space and heuristic information for the data points by ANN shown in Fig. 10b.
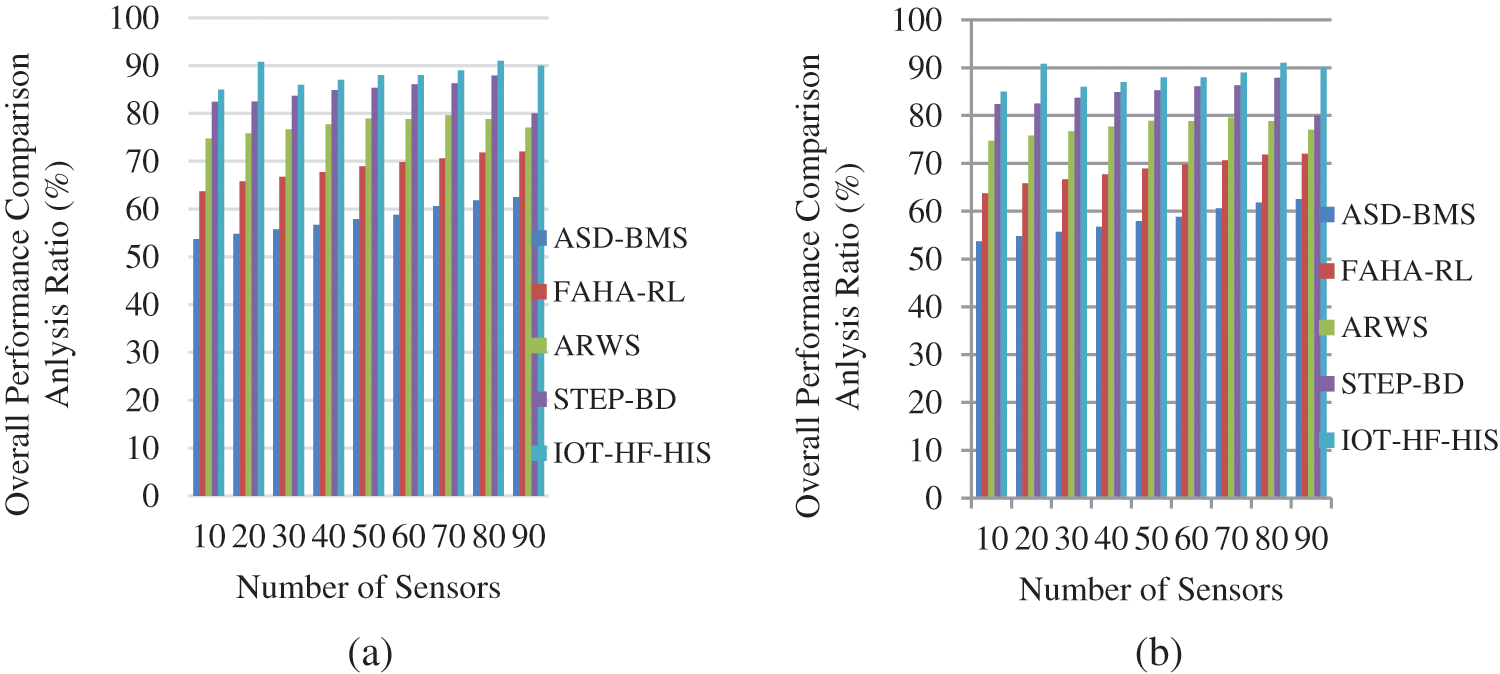
Figure 10: (a) and (b) Overall performance of IoT-HF-HIS framework
The proposed method IoT-HF-HIS achieves an enhancement in monitoring ratio, latency ratio, predicting behavior ratio, execution time analysis, readiness in a smart environment when compared with other traditional approaches ASD-BMS, FAHA-RL, ARWS, STEP-BD, and ESMEHM are analyzed.
IoT-based patient health reports are demonstrated in this system. The IoT-HF-HIS framework for health monitoring system enhancement gateway has been applied in this research (IoT-HF-HIS), allowing for quick treatment with little delay. In an effort to expand the ratio of the delivery service of mobility healthcare and remote surveillance systems, this paper presented an IoT-assisted multidimensional intelligent surveillance system. Wearable sensor information is used in the suggested method to provide quick service answers. The delivery of traditional healthcare services will be altered by deploying IoT technology in the hospital. In fact, for these models to be successfully implemented in clinical settings, several privacy and safety concerns must be addressed. For WBAN aided clinical diagnostic applications, however, a large-scale and comprehensive review is required through various organizations. ANN clinical implementations of medical diagnostic help are essential conditions for further medical technology expansion. IoT-HF-HIS improves accuracy predictability, execution time by less than two hours, and decision tables utilizing machine learning and efficiency as shown by numerical results with an efficiency of 95.2%. Deep learning-based models are expected to be implemented in the future for this high-quality healthcare network.
Funding Statement: The authors received no specific funding for this study.
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
References
1. S. Rani, S. H. Ahmed and R. Rastogi, “Dynamic clustering approach based on wireless sensor networks genetic algorithm for IoT applications,” Wireless Networks, vol. 9, pp. 1154–1172, 2019. [Google Scholar]
2. P. A. Catherwood, D. Steele, M. Little, S. McComb and J. A. McLaughlin, “A Community-based iot personalized wireless healthcare solution trial,” IEEE Journal of Translational Engineering in Health and Medicine, vol. 6, pp. 1–3, 2021. [Google Scholar]
3. H. Liao, Z. Zhou, X. Zhao, L. Zhang, S. Mumtaz et al., “Learning-based context-aware resource allocation for edge-computing-empowered industrial IOT,” IEEE Internet of Things Journal, vol. 7, no. 5, pp. 4260–4277, 2019. [Google Scholar]
4. S. Chakraborty, V. Bhatt and T. Chakravorty, “Impact of IOT adoption on agility and flexibility of healthcare organization,” International Journal of Innovative Technology and Exploring Engineering, vol. 10, pp. 2673–2681, 2019. [Google Scholar]
5. X. Chen, M. Ma and A. Liu, “Dynamic power management and adaptive packet size selection for IoT in e-healthcare,” Computers & Electrical Engineering, vol. 65, pp. 357–375, 2019. [Google Scholar]
6. A. Choi and H. Shin, “Longitudinal healthcare data management platform of healthcare IoT devices for personalized services,” Journal of UCS, vol. 24, No. no. 9, pp. 1153–1169, 2019. [Google Scholar]
7. M. M. Dhanvijay and S. C. Patil, “Internet of things: A survey of enabling technologies in healthcare and its applications,” Computer Networks, vol. 153, pp. 113–131, 2019. [Google Scholar]
8. O. I. Khalaf, G. M. Abdulsahib and N. A. Zghair, “IOT fire detection system using sensor with arduino,” AUS, vol. 26, pp. 74–80, 2019. [Google Scholar]
9. B. Farahani, F. Firouzi, V. Chang, M. Badaroglu and K. Mankodiya, “Towards fog-driven iotehealth: Promises and challenges of IoT in medicine and healthcare,” Future Generation Computer Systems, vol. 78, pp. 659–676, 2021. [Google Scholar]
10. P. A. Gaona García, S. Sánchez Alonso, and C. Montenegro Marin, “Visualization of information: A proposal to improve the search and access to digital resources in repositories,” Ingeniería e Investigación, vol. 34, no. 1, pp. 83–90, 2021. [Google Scholar]
11. M. M. Islam, A. Rahaman and M. Islam, “Development of smart healthcare monitoring system in IoT environment,” SN Computer Science, vol. 1, no. 3, pp. 267–281, 2020. [Google Scholar]
12. C. Shin and Y. Cho, “Efficient energy consumption prediction model for a data analytic-enabled industry building in a smart city,” Building Research & Information, vol. 5, pp. 1–7, 2020. [Google Scholar]
13. Y. S. Jeong and S. S. Shin, “An IoT healthcare service model of a vehicle using implantable devices,” Cluster Computing, vol. 21, no. 1, pp. 1059–1068, 2016. [Google Scholar]
14. W. Li, C. Jung and J. Park, “IoT healthcare communication system for IEEE 11073 PhD and IHE PCD-01 integration using coap,” KSII Transactions on Internet & Information Systems, vol. 12, no. 4, pp. 567–581, 2021. [Google Scholar]
15. H. Malik, M. M. Alam, Y. Moullec and A. Kuusik, “Narrowband-IoT performance analysis for healthcare applications,” Procedia Computer Science, vol. 130, pp. 1077–1083, 2021. [Google Scholar]
16. F. Al-Turjman and S. Alturjman, “5G/IoT-enabled UAVs for multimedia delivery in industry-oriented applications,” Multimedia Tools and Applications, vol. 79, no. 13, pp. 8627–8648, 2020. [Google Scholar]
17. A. A. Mutlag, M. K. AbdGhani, N. A. Arunkumar, M. A. Mohammed and O. Mohd, “Enabling technologies for fog computing in healthcare IoT systems,” Future Generation Computer Systems, vol. 90, pp. 62–78, 2019. [Google Scholar]
18. S. Palanimurugan, M. Chinnadurai and S. Manikandan, “Tour planning design for mobile robots using pruned adaptive resonance theory networks,” Computers, Materials & Continua, vol. 70, no. 1, pp. 181–194, 2022. [Google Scholar]
19. S. Sharma, K. Chen and A. Sheth, “Toward practical privacy-preserving analytics for iot and cloud-based healthcare systems,” IEEE Internet Computing, vol. 22, no. 2, pp. 42–51, 2021. [Google Scholar]
20. A. H. Sodhro, S. Pirbhulal and Z. Luo, “Towards an optimal resource management for IoT-based green and sustainable smart cities,” Journal of Cleaner Production, vol. 220, pp. 1167–1179, 2019. [Google Scholar]
21. V. Soni, V. Dineshkumar and F. Soni, “IOT connected with e-learning,” International Journal on Integrated Education, vol. 2, no. 5, pp. 273–277, 2019. [Google Scholar]
22. A. F. Subahi, “Edge-based IoT medical record system: Requirements, recommendations, and conceptual design,” IEEE Access, vol. 7, pp. 94150–94159, 2019. [Google Scholar]
23. T. Tekeste, H. Saleh, B. Mohammad and M. Ismail, “Ultra-low power QRS detection and ECG compression architecture for IoT healthcare devices,” IEEE Transactions on Circuits and Systems I: Regular Papers, vol. 66, no. 2, pp. 669–679, 2021. [Google Scholar]
24. H. Wang, “IoT-Based clinical sensor data management and transfer using blockchain technology,” Journal of ISMAC, vol. 2, no. 3, pp. 154–159, 2020. [Google Scholar]
25. M. W. Woo, J. Lee and K. Park, “A reliable IoT system for personal healthcare devices,” Future Generation Computer Systems, vol. 78, pp. 626–640, 2021. [Google Scholar]
26. F. Al-Turjman, “5G-enabled devices and smart-spaces in social-IoT: An overview,” Future Generation Computer Systems, vol. 92, pp. 732–744, 2019. [Google Scholar]
27. S. Manikandan, P. Dhanalakshmi, K. C. Rajeswari and A. Delphin Carolina Rani, “Deep sentiment learning for measuring similarity recommendations in twitter data,” Intelligent Automation & Soft Computing, vol. 34, no. 1, pp. 183–192, 2022. [Google Scholar]
28. A. Das, P. Rad, K. Choo and J. Martel, “Distributed machine learning cloud teleophthalmology IoT for predicting AMD disease progression,” Future Generation Computer Systems, vol. 93, pp. 486–498, 2019. [Google Scholar]
29. L. Fang, C. Yin, J. Zhu and C. Ge, “Privacy protection for medical data sharing in smart healthcare,” ACM Transactions on Multimedia Computing, Communications, and Applications (TOMM), vol. 16, no. 3, pp. 1–18, 2020. [Google Scholar]
Cite This Article
 Copyright © 2023 The Author(s). Published by Tech Science Press.
Copyright © 2023 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools