 Open Access
Open Access
ARTICLE
Transforming Healthcare: AI-NLP Fusion Framework for Precision Decision-Making and Personalized Care Optimization in the Era of IoMT
1 Department of Mathematics and Computer Science, Beirut Arab University, Beirut, 11072809, Lebanon
2 College of Computer and Information Sciences, King Saud University, Riyadh, 11451, Saudi Arabia
* Corresponding Author: Nadia Al-Ghreimil. Email:
Computers, Materials & Continua 2024, 81(3), 4575-4601. https://doi.org/10.32604/cmc.2024.055307
Received 23 June 2024; Accepted 13 November 2024; Issue published 19 December 2024
Abstract
In the rapidly evolving landscape of healthcare, the integration of Artificial Intelligence (AI) and Natural Language Processing (NLP) holds immense promise for revolutionizing data analytics and decision-making processes. Current techniques for personalized medicine, disease diagnosis, treatment recommendations, and resource optimization in the Internet of Medical Things (IoMT) vary widely, including methods such as rule-based systems, machine learning algorithms, and data-driven approaches. However, many of these techniques face limitations in accuracy, scalability, and adaptability to complex clinical scenarios. This study investigates the synergistic potential of AI-driven optimization techniques and NLP applications in the context of the IoMT. Through the integration of advanced data analytics methodologies with NLP capabilities, we propose a comprehensive framework designed to enhance personalized medicine, streamline disease diagnosis, provide treatment recommendations, and optimize resource allocation. Using a systematic methodology data was collected from open data repositories, then preprocessed using data cleaning, missing value imputation, feature engineering, and data normalization and scaling. Optimization algorithms, such as Gradient Descent, Adam Optimization, and Stochastic Gradient Descent, were employed in the framework to enhance model performance. These were integrated with NLP processes, including Text Preprocessing, Tokenization, and Sentiment Analysis to facilitate comprehensive analysis of the data to provide actionable insights from the vast streams of data generated by IoMT devices. Lastly, through a synthesis of existing research and real-world case studies, we demonstrated the impact of AI-NLP fusion on healthcare outcomes and operational efficiency. The simulation produced compelling results, achieving an average diagnostic accuracy of 93.5% for the given scenarios, and excelled even further in instances involving rare diseases, achieving an accuracy rate of 98%. With regard to patient-specific treatment plans it generated them with an average precision of 96.7%. Improvements in early risk stratification and enhanced documentation were also noted. Furthermore, the study addresses ethical considerations and challenges associated with deploying AI and NLP in healthcare decision-making processes, offering insights into risk-mitigating strategies. This research contributes to advancing the understanding of AI-driven optimization algorithms in healthcare data analytics, with implications for healthcare practitioners, researchers, and policymakers. By leveraging AI and NLP technologies in IoMT environments, this study paves the way for innovative strategies to enhance patient care and operational effectiveness. Ultimately, this work underscores the transformative potential of AI-NLP fusion in shaping the future of healthcare.Keywords
In the modern healthcare landscape, the convergence of advanced technologies such as Artificial Intelligence (AI) and the Internet of Medical Things (IoMT) presents unprecedented opportunities. IoMT, which involves a network of interconnected medical devices and applications that collect, transmit, and analyze health data, is transforming healthcare data management and decision-making [1]. These technologies have the potential to revolutionize decision-making processes and improve patient outcomes [1]. With the exponential growth of healthcare data generated from diverse sources including medical devices, electronic health records (EHRs), and wearable sensors, the need for efficient data analytics techniques has become paramount [2]. However, traditional analytical approaches face significant challenges due to the sheer volume, variety, and velocity of healthcare data, necessitating innovative solutions that harness the power of AI and Natural Language Processing (NLP).
Data analytics plays a crucial role in extracting actionable insights from vast amounts of healthcare data, facilitating evidence-based decision-making, and driving improvements in patient care delivery [3]. AI techniques such as machine learning, deep learning, and predictive analytics offer unparalleled capabilities for analyzing complex datasets, identifying patterns, and generating predictive models to improve disease diagnosis, prognosis, and treatment optimization [4,5]. For example, AI-driven optimization combined with NLP can enhance diagnostic accuracy by integrating structured and unstructured data sources to provide more precise insights. Moreover, integrating NLP empowers healthcare organizations to extract valuable insights from unstructured text data found in clinical notes, medical literature, and patient records. This augmentation enhances the depth and breadth of data analytics insights.
To provide context for this study, several current techniques in personalized medicine, disease diagnosis, treatment recommendations, and resource optimization within IoMT are considered. These techniques, while advanced, often face limitations in scalability, integration, and adaptability to diverse patient data, highlighting the need for further innovation. In this context, this study explores the transformative potential of AI-driven optimization algorithms of data analytics techniques, leveraging NLP within the framework of IoMT. Through a synthesis of existing literature, we aim to explain the synergistic interplay between AI and NLP in enhancing healthcare decision-making processes. Through a comprehensive review of current trends, challenges, and opportunities in healthcare data analytics, we highlight the imperative for adopting advanced analytical methodologies to meet the evolving needs of modern healthcare systems.
This study presents a comprehensive framework that integrates AI-driven optimization algorithms with NLP functionalities to facilitate personalized medicine, improve diagnostic accuracy, and optimize resource allocation in healthcare settings. Specifically, we employed optimization algorithms such as Gradient Descent, Adam Optimization, and Stochastic Gradient Descent to enhance the predictive capabilities of the framework. These algorithms enable efficient processing of large-scale healthcare data for personalized medicine and resource optimization. In addition, NLP processes such as Text Preprocessing, Tokenization, Named Entity Recognition (NER), and Sentiment Analysis were used to extract actionable insights from unstructured text data, such as clinical notes and patient feedback. By leveraging the power of AI and NLP, healthcare organizations can unlock the full potential of their data assets, leading to more informed decision-making, enhanced clinical outcomes, and greater operational efficiency.
The key scientific contributions of this work include:
• Integration of AI-driven optimization algorithms with NLP for personalized medicine and improved diagnostic accuracy.
• Development of the “AI-NLP Enhanced Healthcare Decision Framework” for improving data-driven decision-making in IoMT environments.
• Addressing practical challenges and opportunities related to AI and NLP in healthcare.
This study aims to contribute to the expanding body of knowledge surrounding AI-driven optimization algorithms of data analytics techniques in healthcare, with a particular emphasis on leveraging NLP processes for enhanced decision-making in the era of IoMT. By combining theoretical insights with practical applications, our aim is to provide healthcare practitioners, researchers, and policymakers with actionable strategies to harness the transformative potential of AI and NLP in driving positive outcomes for patients and healthcare systems alike.
In the subsequent sections and subsections, we delve into the details of AI-driven optimization algorithms in healthcare data analytics, examining the diverse range of techniques, methodologies, and applications that underpin this transformative approach. Section 2 explores an overview on AI-driven optimization techniques in healthcare data analytics, detailing the diverse methods and applications that support this transformative approach. Section 3 focuses on ethical considerations, challenges, and opportunities related to the implementation of AI and NLP technologies in healthcare decision-making. Section 4 presents real-world case studies and practical examples, highlighting the tangible impacts of AI and NLP integration on patient care delivery and healthcare management. Section 5 outlines the methodology used in this study, including data collection, preprocessing techniques, and the integration of AI and NLP within IoMT environments. Section 6 details the experiments conducted, including data sources and simulation approaches. Section 7 discusses the results and their implications, providing insights into the performance and effectiveness of the proposed framework. Finally, Section 8 offers a conclusion, summarizing key findings and suggesting future research directions.
2 Overview of AI and Analytics in Healthcare
In this section, we analyze key topics related to data analytics and AI in the healthcare domain. It starts with an overview of data analytics techniques, covering their diverse applications and methodologies. We then examine current trends and challenges in healthcare data analytics, introduce NLP applications, discuss AI-driven optimization studies, and explore the impact of IoMT on healthcare data analytics.
2.1 Overview of Data Analytics Techniques in Healthcare
Within the dynamically evolving landscape of healthcare, data analytics techniques have emerged as indispensable tools for extracting insights from vast amounts of healthcare data. This section provides an in-depth overview of the diverse array of data analytics techniques employed in healthcare settings. These techniques encompass a spectrum of functionalities, each serving distinct roles in the analysis and interpretation of healthcare data:
1. Descriptive Analytics: Foundational to healthcare data analysis, descriptive analytics focuses on summarizing historical data to provide insights into past trends and patterns [6]. For instance, Hohman et al. [7] proposed a methodology for organizing and visualizing data from electronic health records (EHRs) to understand patient populations and disease prevalence. Additionally, Cook et al. [8] conducted a study to assess the demographic and clinical traits of patients who self-reported exposure to firearm violence during a behavioral health visit.
2. Predictive Analytics: Building upon descriptive analytics, predictive analytics endeavors to forecast future trends and outcomes based on historical data patterns [9]. Lo et al. [10] developed machine learning models to predict 14-day unplanned hospital readmissions among adult patients. It emphasized the importance of early identification of at-risk patients for improving care and reducing readmission rates. Through retrospective cohort analysis and the utilization of multiple machine learning algorithms, the study demonstrated the effectiveness of the developed models in accurately identifying high-risk patients. Similarly, da Silva et al. [11] developed machine learning models to predict potentially avoidable 30-day readmissions among children and adolescents. Conducting a retrospective cohort study on 9080 patients in a tertiary hospital, it utilized demographic and clinical data. Results showed XGBoost as the most effective algorithm, identifying factors such as cancer diagnosis and age as significant predictors of readmission risk. These models could aid in early identification and targeted interventions for at-risk patients.
3. Prescriptive Analytics: Representing the pinnacle of data analytics sophistication in healthcare, prescriptive analytics offers actionable recommendations for decision-making [12]. Sideris et al. [13] employed implementation findings from a pilot phase investigating AI-based analytics in heart failure (HF) to devise strategies addressing communication technology, patient and clinician education, and electronic health record (EHR) integration. The results provided important insights into the broader application of AI analytics within clinical workflows. Moreover, Bastani et al. [14] integrated prescriptive analytics into a decision support system for medication management, providing personalized recommendations to healthcare providers based on patient-specific data and clinical guidelines.
2.2 Current Trends and Challenges in Healthcare Data Analytics
Despite the promise of data analytics in healthcare, several trends and challenges shape the landscape of healthcare data analytics [15,16]. Derecho et al. [16] highlighted the increasing adoption of EHR systems in healthcare institutions and their impact on data accessibility and utilization. They conducted a study on the challenges of interoperability among disparate healthcare systems and proposed strategies to improve data exchange and integration. Tariq [17] addressed the ethical implications of data privacy and patient confidentiality in healthcare data analytics, emphasizing the importance of implementing stringent security measures and regulatory compliance frameworks. Furthermore, Seh et al. [18] explored the role of machine learning in safeguarding the confidentiality of electronic health records, offering insights into secure data handling practices that enhance trust in AI-driven healthcare solutions. In addition, Sonavane et al. [19] provided a systematic review of IoMT techniques, examining the challenges and future directions in integrating IoMT-generated data into healthcare analytics, which resonates with the goals of our study.
In the realm of healthcare data analytics, several critical challenges impede the effective implementation of AI technologies [20,21]. Foremost among these challenges are issues related to data quality, where inaccuracies and insufficient data can lead to erroneous automated diagnoses, thereby jeopardizing patient safety. Additionally, the integration of diverse data types–such as text, numeric, image, and video-poses significant complexities, as each requires distinct processing methodologies to ensure accurate analysis. Privacy and legal concerns further complicate the landscape, necessitating strict adherence to ethical standards and regulatory compliance when accessing and utilizing patient data. Moreover, the reliance on AI systems can introduce ethical dilemmas, particularly regarding transparency and accountability in decision-making processes. Collectively, these challenges underscore the necessity for a robust framework that addresses data integrity, ethical considerations, and the seamless integration of AI technologies within healthcare systems.
2.3 Introduction to NLP and Its Applications in Healthcare
NLP is a subfield of artificial intelligence that focuses on the interaction between computers and human languages. It involves the application of computational techniques to analyze and synthesize natural language and speech, enabling machines to understand, interpret, and respond to human language in a valuable way [22,23]. NLP has emerged as a transformative technology in healthcare, enabling the analysis and interpretation of unstructured text data [22]. By automating the extraction of valuable insights from textual data, NLP enhances decision support systems, facilitates evidence-based medicine, and improves communication between healthcare providers and patients [23]. For instance, Nova [24] proposed a novel approach to text preprocessing in healthcare data, improving the accuracy and efficiency of NLP algorithms. Additionally, Suvirat et al. [25] investigated the application of NLP in medical coding tasks, streamlining the process and reducing coding errors. Karimbux et al. [26] conducted a study on sentiment analysis in patient feedback data, providing insights into patient satisfaction and areas for improvement in healthcare services.
In recent years, the application of NLP in the analysis of EHRs has garnered significant attention due to its potential to enhance clinical decision-making and streamline healthcare processes. A systematic review conducted by Hossain et al. [27] comprehensively examines various machine learning (ML) and deep learning (DL) techniques employed in NLP for EHRs, highlighting their effectiveness in extracting clinical insights from unstructured data. The review categorizes the literature into several domains, including medical note classification, clinical entity recognition, and text summarization, while also addressing the challenges faced in the field, such as the scarcity of annotated data and the need for automated tools. By synthesizing findings from 127 studies, the authors provide a critical analysis of the current state of NLP applications in healthcare, emphasizing the importance of advanced methodologies in overcoming existing limitations and improving patient outcomes.
2.4 Existing Studies on AI-Driven Optimization of Data Analytics Techniques in Healthcare
In recent years, there has been an increasing body of literature dedicated to the integration of AI techniques with data analytics in healthcare [28]. This subsection reviews existing studies that investigate into the realm of AI-driven optimization of data analytics techniques for diverse healthcare applications. These studies span a wide spectrum of methodologies and applications, showcasing the transformative potential of AI in enhancing healthcare decision-making and operational efficiency.
• Machine Learning Algorithms for Disease Prediction: Bucholc et al. [29] proposed a machine learning approach for predicting disease outcomes using comprehensive patient data. Their study demonstrated high accuracy in predicting disease progression and provided valuable insights for personalized treatment planning.
• Optimization Algorithms for Resource Allocation: Sharif et al. [30] conducted a comprehensive study on optimization algorithms for healthcare resource allocation. Their research focused on optimizing workforce scheduling, bed management, and equipment utilization, leading to significant improvements in operational efficiency and cost-effectiveness.
• Deep Learning Techniques for Medical Imaging Analysis: Rana et al. [31] explored the application of deep learning techniques in medical imaging analysis for disease diagnosis and prognosis. Their study showcased the potential of convolutional neural networks (CNNs) and recurrent neural networks (RNNs) in accurately detecting abnormalities and guiding clinical decision-making.
• Predictive Analytics for Patient Risk Stratification: Ruiz-Ramos et al. [32] investigated the use of predictive analytics for patient risk stratification, particularly in identifying individuals at high risk of adverse health events such as hospital readmissions or complications. Their research highlighted the utility of predictive models in proactive patient management and resource allocation.
• Natural Language Processing for Clinical Documentation: Sivarajkumar et al. [33] conducted a comprehensive review of NLP techniques for clinical documentation and information extraction. Their study emphasized the role of NLP in automating clinical documentation processes, improving data accuracy, and facilitating clinical decision support.
2.5 Review of IoMT and Its Impact on Healthcare Data Analytics
The IoMT encompasses a network of interconnected medical devices and applications that collect, transmit, and analyze health data [34–36]. These devices, including wearable health monitors, remote sensors, and smart medical equipment, significantly enhance healthcare data analytics by providing real-time and continuous data streams. This connectivity facilitates improved patient monitoring, personalized treatment plans, and more efficient healthcare management. As such, the IoMT represents a transformative shift in healthcare delivery, facilitating the seamless integration of medical devices, sensors, and wearable technologies [34]. A thorough understanding of IoMT’s ramifications is crucial for healthcare stakeholders, as it holds immense promise for revolutionizing patient care, streamlining clinical workflows, and driving innovation in healthcare analytics. Ahmed et al. [35] conducted a comprehensive review of IoMT devices and their impact on healthcare data analytics, emphasizing the imperative need for robust data security measures and interoperability standards to ensure the reliability and integrity of IoMT-generated data. Osama et al. [36] explored the intricate challenges associated with integrating diverse IoMT data streams into existing healthcare analytics frameworks, underscoring the significance of scalable data management strategies to effectively handle the volume and variety of IoMT data. Dwivedi et al. [37] investigated the transformative opportunities presented by IoMT for personalized medicine and proactive patient monitoring. Their research highlighted the pivotal role of data analytics in extracting actionable insights from IoMT-generated data to inform clinical decision-making and improve patient outcomes. Awotunde et al. [38] examined the ethical dimensions surrounding IoMT data utilization, including paramount concerns regarding patient privacy and data ownership. Their contribution added valuable insights to the ongoing discourse on responsible IoMT implementation in healthcare settings, emphasizing the importance of ethical considerations in guiding IoMT deployment strategies.
Table 1 summarizes the current works in terms of their working principles, pros, and cons to enhance clarity and provide a comparative overview of the methodologies discussed.

3 AI-Driven Optimization of Data Analytics Techniques
In healthcare, the implementation of AI-driven optimization techniques has revolutionized data analytics, bringing about significant advancements across various domains [39].
• Data Mining and Pattern Recognition in Healthcare Data: Data mining techniques play a crucial role in healthcare by uncovering hidden patterns and trends within vast datasets [40]. In this study, we employ data mining algorithms, including association rule mining, clustering, and classification, to extract valuable insights from healthcare data. These techniques enable us to identify patterns related to disease prevalence, treatment efficacy, and patient outcomes.
• Predictive Analytics for Disease Diagnosis and Prognosis: Predictive analytics holds immense potential for improving disease diagnosis and prognosis in healthcare [4]. In our proposed framework, we utilize predictive modeling techniques, including logistic regression, decision trees, and ensemble methods, to forecast disease outcomes based on patient data. By analyzing historical healthcare data, predictive analytics enables us to identify risk factors, predict disease progression, and stratify patients according to their likelihood of developing certain conditions. This empowers healthcare providers to intervene early, personalize treatment plans, and improve patient outcomes.
• Personalized Medicine and Treatment Recommendation Systems: Personalized medicine aims to tailor healthcare interventions to individual patient characteristics, preferences, and genetic makeup [41]. In our study, we develop treatment recommendation systems that leverage AI-driven optimization techniques to provide personalized treatment plans for patients. By analyzing patient-specific data, including genetic information, medical history, and lifestyle factors, these systems can recommend the most effective treatments and medication dosages for each individual. This approach enhances treatment efficacy, minimizes adverse effects, and improves patient adherence to therapy.
• Optimization Algorithms for Healthcare Resource Management: Efficient resource management is essential for ensuring the delivery of high-quality healthcare services while optimizing costs and resource utilization [42]. In our research, we apply optimization algorithms such as linear programming, integer programming, and simulation modeling to address healthcare resource management challenges. These algorithms enable us to optimize healthcare workflows, streamline workforce scheduling, and allocate resources effectively across healthcare facilities. By optimizing resource management, healthcare providers can enhance operational efficiency, reduce wait times, and improve patient satisfaction.
The significance of AI-driven optimization techniques in healthcare is underscored by their diverse applications and benefits for healthcare providers. Table 2 summarizes key AI-driven techniques and their importance, including data mining for uncovering patterns, predictive analytics for disease diagnosis, personalized medicine for tailored interventions, and optimization algorithms for efficient resource management.

4 Natural Language Processing in Healthcare Decision-Making
This section explores the pivotal role of NLP processes in healthcare decision-making. From extracting clinical insights to automating medical documentation, NLP offers transformative solutions for leveraging unstructured text data in healthcare analytics. The seamless integration of NLP techniques across various stages of the decision-making process is visually represented in Fig. 1, illustrating how NLP facilitates informed decision-making by healthcare professionals; a detailed explanation follows:
• Extraction of Clinical Insights from Unstructured Text Data: NLP processes enable the extraction of valuable clinical insights from unstructured text data, such as clinical notes, medical reports, and research literature [43]. In this study, we employ NLP processes such as text preprocessing, named entity recognition, and syntactic parsing to extract relevant information from unstructured text sources. By analyzing textual data, healthcare providers can gain insights into patient conditions, treatment effectiveness, and disease progression, facilitating evidence-based decision-making and personalized patient care.
• Sentiment Analysis and Patient Feedback Processing: Sentiment analysis techniques are utilized to analyze patient feedback and sentiment expressed in healthcare-related texts, such as patient reviews, social media posts, and surveys [44]. In our research, we apply sentiment analysis algorithms to assess patient satisfaction, identify areas for improvement in healthcare services, and monitor patient sentiments over time. By analyzing patient feedback, healthcare organizations can identify trends, address concerns, and enhance patient experiences, ultimately improving overall satisfaction and loyalty.
• Semantic Understanding and Contextual Analysis in Healthcare Conversations: Semantic understanding and contextual analysis techniques enable NLP systems to comprehend the meaning and context of healthcare conversations, including patient-provider interactions and clinical documentation [45]. In this study, we explore advanced NLP models, such as deep learning-based semantic parsers and context-aware language models, to interpret healthcare dialogues and extract actionable insights. By understanding the nuances of language and context, NLP systems can assist healthcare providers in making informed decisions, facilitating accurate diagnosis, and improving communication with patients.
• Automation of Medical Documentation and Reporting: NLP technologies facilitate the automation of medical documentation and reporting processes, reducing the burden on healthcare professionals and improving documentation accuracy and efficiency [46]. In our study, we utilize existing NLP-based systems tailored for tasks such as clinical note generation, medical coding, and radiology report generation. By leveraging these automated solutions, healthcare providers can redirect their focus towards patient care, streamline workflows, and minimize administrative burdens.
• Ethical Considerations and Challenges in NLP Implementation in Healthcare: The implementation of NLP processes in healthcare raises ethical considerations and challenges related to data privacy, patient consent, and bias mitigation [47]. In this study, we address these concerns by adopting ethical guidelines and best practices for NLP implementation in healthcare settings. These guidelines can be found in peer-reviewed literature, institutional research protocols, and regulatory frameworks governing healthcare data management and privacy. Additionally, professional organizations and research institutions often provide specific guidelines and recommendations for ethical conduct in healthcare research and technology implementation.
• Enhancing Healthcare Decision-Making with NLP: Healthcare decision-making lies at the core of effective patient care and treatment strategies [23]. NLP technologies play a crucial role in augmenting decision-making processes by providing valuable insights derived from diverse sources of unstructured text data. By leveraging NLP, healthcare providers can make informed decisions regarding diagnosis, treatment plans, and patient management.

Figure 1: Integration of NLP in healthcare Decision-Making process
The flowchart depicted in Fig. 2 elucidates the multifaceted role of NLP in guiding healthcare decision-making processes. The flowchart illustrates various stages where NLP processes are applied, including the extraction of clinical insights from unstructured text data, sentiment analysis of patient feedback, semantic understanding and contextual analysis of healthcare conversations, and automation of medical documentation and reporting tasks, ultimately aiding healthcare professionals in making informed decisions.

Figure 2: Flowchart of NLP integration in healthcare Decision-Making
To accomplish the research objectives, a systematic methodology was followed, integrating data collection, preprocessing, and analysis techniques. This section outlines the step-by-step approach undertaken to address each aspect of the research study to ultimately reach a comprehensive framework that fuses AI-NLP to optimize healthcare data processing and decision-making.
5.1 Data Collection Strategies in Healthcare
Effective data collection strategies are fundamental to acquiring diverse datasets essential for healthcare analytics [48]. In this context, our approach encompassed a multifaceted methodology aimed at gathering comprehensive and representative data sources. Key considerations included EHRs, medical imaging data, wearable device data, and IoMT sensor data, which collectively provide a rich tapestry of healthcare information. Collaboration with a spectrum of stakeholders, including healthcare institutions, research databases, and open data repositories such as PhysioNet, facilitated access to these datasets, ensuring their relevance and applicability to our analyses.
One of the primary datasets utilized in our study was sourced from PhysioNet [49], which offers a comprehensive collection of anonymized EHR data from various healthcare institutions. This dataset includes detailed attributes such as patient demographics, medical history, laboratory results, clinical notes, and vital signs. The PhysioNet dataset was integral to our analysis, providing a rich source of historical patient data necessary for developing and validating our models. The specific data attributes used include:
• Patient Demographics: Age, gender, ethnicity
• Medical History: Chronic conditions, previous treatments
• Laboratory Results: Blood tests, imaging results
• Clinical Notes: Physician’s observations, diagnostic notes
• Vital Signs: Heart rate, blood pressure, temperature
These attributes were selected for their relevance in predicting healthcare outcomes and personalizing treatment plans. The preprocessing steps for this dataset, including data cleaning, normalization, and feature extraction, are detailed in Section 6 to avoid redundancy in this section.
Ethical considerations were paramount throughout the data collection process, reflecting our commitment to preserving patient privacy and adhering to regulatory frameworks. Stringent measures were implemented to ensure compliance with data privacy regulations, including protocols to safeguard patient confidentiality and mitigate potential risks associated with data handling and sharing.
5.2 Preprocessing Techniques for Healthcare Data
In healthcare analytics, preprocessing techniques play an important role in transforming raw data into actionable insights [50]. This complex process involves a series of essential steps:
1. Data Cleaning: The initial phase involves meticulously identifying and rectifying inconsistencies, errors, and outliers [51]. This critical step ensures the integrity and accuracy of the dataset, laying a robust foundation for subsequent analysis. Mathematically, outlier detection can be achieved using methods such as the Z-score, where outliers are defined as observations with a Z-score greater than a threshold τ:
where
2. Missing Value Imputation: Following data cleaning, missing values within the dataset are addressed through sophisticated algorithms that infer and populate missing values based on existing data pattern. One common approach is the Mean Imputation method, where missing values are replaced with the mean of the observed values:
where
3. Feature Engineering: Domain knowledge and analytical expertise converge to derive relevant predictors from the dataset [52]. By crafting informative features that encapsulate key aspects of patient health, treatment modalities, and healthcare outcomes, researchers enhance the predictive power of their models. Techniques include Principal Component Analysis (PCA) for dimensionality reduction. The PCA transformation is defined as:
where Z is the transformed data, X is the original data matrix, and W is the matrix of eigenvectors.
4. Data Normalization and Scaling: These techniques play a pivotal role in standardizing the data distribution, mitigating disparities in variable magnitudes, and ensuring optimal model performance [53]. By transforming variables to a uniform scale, analysts enable effective model training, interpretation, and generalization across diverse datasets. Min-Max Normalization transforms features to a range [0, 1]:
where
5. Standardization scales data to have a mean of 0 and a standard deviation of 1:
where μ is the mean and σ is the standard deviation of the feature.
Collectively, these preprocessing techniques are an integral part of the framework, which empowers healthcare analysts to unlock the full potential of their data, fostering deeper insights, more accurate predictions, and ultimately, informed decision-making in clinical practice and healthcare management. Fig. 3 illustrates how raw healthcare data goes through several preprocessing steps, including data cleaning, missing value imputation, feature engineering, and data normalization/scaling, resulting in preprocessed data ready for analysis. Through these steps, the data is refined and optimized, ensuring its quality and suitability for analysis. This meticulous preprocessing not only enhances the reliability and robustness of subsequent analyses but also streamlines the process of deriving meaningful insights, thereby driving improvements in patient care and operational efficiency.

Figure 3: Process flow of healthcare data preprocessing
5.3 AI-Driven Optimization Techniques
A comprehensive overview of AI-driven optimization techniques was conducted to identify suitable methodologies for the study. This involved reviewing existing literature on machine learning algorithms, deep learning architectures, and optimization algorithms applicable to healthcare analytics. Considerations such as model complexity, interpretability, and computational efficiency were considered in selecting appropriate techniques for the research objectives.
The optimization algorithms implemented in the proposed framework are Gradient Descent, Adam Optimization, and Stochastic Gradient Descent. Each technique was selected for its strengths in enhancing model performance and convergence:
• Gradient Descent: A fundamental optimization algorithm used to minimize the loss function by iteratively adjusting model parameters. It is particularly effective for simpler models and ensures gradual convergence toward optimal solutions.
• Adam Optimization: An advanced optimization algorithm that combines the advantages of both gradient descent and adaptive learning rates. Adam is known for its efficiency and ability to handle large-scale data and complex models, making it well-suited for healthcare data, which can be varied and high-dimensional.
• Stochastic Gradient Descent (SGD): An iterative algorithm that updates model parameters based on individual data points or mini-batches, rather than the entire dataset. This approach enhances computational efficiency and speeds up convergence, especially beneficial in large-scale healthcare applications.
These algorithms were tailored and integrated within the framework to address the unique challenges of healthcare decision-making.
5.4 Integration of NLP with Data Analytics in Healthcare
The integration of NLP processes with data analytics techniques was explored to extract insights from unstructured text data in healthcare [54]. In the proposed framework, a suite of NLP methodologies was implemented, including:
• Text Preprocessing: Involves cleaning and preparing textual data, including removing stop words, normalizing text, and handling synonyms to ensure consistent and accurate analysis.
• Tokenization: Breaks down text into individual units, such as words or phrases, which are essential for further analysis and feature extraction.
• Named Entity Recognition (NER): Identifies and classifies key entities such as diseases, medications, and medical procedures from clinical notes and medical literature, enhancing the framework’s ability to extract relevant information.
• Sentiment Analysis: Analyzes patient feedback and other text sources to determine sentiment, providing insights into patient satisfaction and emotional responses. For sentiment analysis, we employed the VADER (Valence Aware Dictionary and sEntiment Reasoner) model [44]. VADER was particularly suitable for processing clinical notes and patient feedback, enabling us to extract insights regarding patient sentiment and satisfaction. These insights played a critical role in evaluating the quality of healthcare services and personalized care provided through the AI-NLP framework.
These NLP processes are crucial components of the framework, enabling comprehensive analysis and extraction of valuable insights from diverse textual data sources. This integration of NLP with data analytics provides a robust approach to understanding and leveraging complex textual data, ultimately contributing to improved healthcare management and patient outcomes.
5.5 Framework for Enhancing Healthcare Decision-Making Using AI and NLP in IoMT Environments
As the IoMT continues to demonstrate its effectiveness in reshaping patient care, our study introduces a robust framework aimed at elevating healthcare decision-making processes. This comprehensive framework integrates AI-driven optimization algorithms with the power of NLP processes within the IoMT environment. By synergizing these advanced technologies, our framework facilitates the extraction of actionable insights from the vast streams of data generated by IoMT devices.
Key components of the framework include:
• AI-Driven Optimization Algorithms: These algorithms are pivotal in enhancing the predictive accuracy of healthcare analytics. The pseudo-code labeled Algorithm 1 outlines the iterative process of optimizing predictive models using techniques such as Gradient Descent and Adam Optimization. This process ensures that the models are fine-tuned to provide accurate predictions based on IoMT data.
• NLP Methodologies: NLP processes play a crucial role in analyzing and interpreting unstructured text data from clinical notes and patient records. Algorithm 2 provides a step-by-step process, including text preprocessing, tokenization, NER, and sentiment analysis. These steps enable the extraction of meaningful insights from raw text data, which are vital for informed decision-making.
• Framework Integration: The integration of AI and NLP within the IoMT environment is central to the framework’s effectiveness. Algorithm 3 demonstrates how the framework seamlessly combines data streams from IoMT devices, applies AI optimization algorithms, processes unstructured data using NLP processes, and ultimately generates actionable insights. This integration facilitates real-time recommendations and alerts to healthcare providers, enhancing decision-making capabilities.
Additionally, the framework addresses critical implementation considerations such as scalability, interoperability, and data security, ensuring its robustness and adaptability within various healthcare settings.

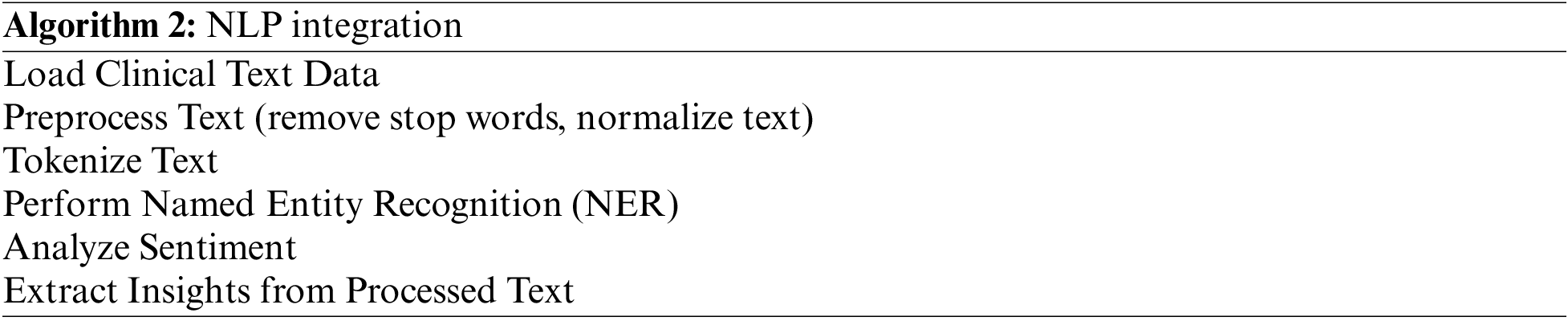

Fig. 4 illustrates the integration framework for healthcare decision-making, showcasing the comprehensive approach used in this study to integrate AI-driven optimization algorithms with NLP processes within the IoMT environment.

Figure 4: AI-NLP enhanced healthcare decision framework
The AI-NLP Enhanced Healthcare Decision Framework integrates AI-driven optimization algorithms with NLP processes to advance healthcare decision-making processes. This framework leverages AI algorithms to analyze complex datasets, identify patterns, and predict outcomes, while NLP processes handle unstructured data, such as clinical notes and patient histories, to extract valuable insights. The focus is on optimizing decision-making rather than real-time adjustments. For example, NLP processes identify key symptoms and medical history from textual data, which AI algorithms use to enhance diagnostic models and tailor treatment recommendations. This approach ensures comprehensive data interpretation, ultimately improving diagnostic accuracy and decision-making efficiency by utilizing all relevant patient information effectively.
To comprehensively evaluate the efficacy and real-world applicability of our proposed AI-driven data analytics and NLP framework in healthcare decision-making, we conducted an extensive simulation using a real-world EHR dataset obtained from PhysioNet [49]. This simulated case study aimed to provide deeper insights into the performance and potential impact of our framework in diverse clinical scenarios.
The PhysioNet repository served as an invaluable resource, providing access to a rich and diverse EHR dataset comprising anonymized patient records from multiple healthcare institutions. This dataset encompasses a wide range of clinical data types, including patient demographics, medical history, laboratory results, clinical notes, and vital signs. Leveraging this comprehensive dataset allowed us to simulate various healthcare scenarios and evaluate the effectiveness of our framework across different patient populations and clinical contexts. Following preprocessing steps, approximately 80% of the records were retained, ensuring the integrity and quality of the dataset for subsequent analysis and experimentation.
Our simulation was designed to closely mirror real-world healthcare settings, facilitating a realistic assessment of our AI-driven framework’s performance. The simulation process encompassed the following key steps:
1. Data Preprocessing: We meticulously preprocessed the EHR dataset to ensure data quality and consistency. This involved tasks such as data cleaning, normalization, feature engineering, and handling missing values. By preparing the data in a standardized format, we aimed to facilitate accurate analysis and modeling. This standardization ensures that the data is organized uniformly, making it comparable, interpretable, and compatible with various analytical methods and tools in healthcare analytics.
2. Framework Integration: Our AI-driven data analytics and NLP framework was seamlessly integrated into the simulated healthcare environment. This involved deploying a suite of machine learning models, NLP processes, and optimization techniques tailored to the specific requirements of healthcare decision-making. The framework was designed to process both structured data (e.g., lab results) and unstructured data (e.g., clinical notes) to extract meaningful insights.
3. Scenario Simulation: To evaluate our AI-driven framework comprehensively, we simulated a diverse array of healthcare scenarios that mirror real-world clinical practice. These scenarios included:
• Disease Diagnosis: Testing the framework’s accuracy in identifying and classifying various medical conditions. We employed Logistic Regression and Random Forest Classifier models [44], both of which were optimized using Gradient Descent and Adam Optimization. These models improved accuracy in identifying and classifying various medical conditions.
• Treatment Recommendation: Assessing the framework’s effectiveness in generating personalized treatment plans. The framework used the XGBoost (Extreme Gradient Boosting) model for generating personalized treatment plans [55]. To enhance its performance, we applied Adam Optimization to tune hyperparameters and maximize precision in treatment recommendations.
• Patient Risk Stratification: Evaluating how well the framework can identify high-risk patients and prioritize interventions. The LightGBM (Light Gradient Boosting Machine) model, optimized using Stochastic Gradient Descent (SGD) [56], was employed to assess patient risk and prioritize interventions, enabling the framework to handle large-scale, high-dimensional data.
Clinical Outcome Prediction: Analyzing the framework’s ability to predict patient outcomes and support future clinical decisions. For predicting patient outcomes, we integrated a Long Short-Term Memory (LSTM) network, a type of recurrent neural network (RNN), to capture temporal dependencies in patient data and improve predictions of clinical decisions [57].
Impact on Dataset: The simulation process involved applying the framework to a carefully prepared dataset, derived from real-world EHR data. By creating scenarios that reflect different clinical contexts, we ensured that the framework was tested under varied conditions. This approach allowed us to assess how well the framework adapts to different types of healthcare data and decision-making processes. The simulated scenarios also provided insights into the framework’s performance in handling the complexities and variability of real-world clinical data, validating its robustness and effectiveness.4. Performance Evaluation: The performance of our framework was rigorously evaluated using a comprehensive set of performance metrics tailored to each simulated scenario [58]. These metrics provide a detailed assessment of the model’s effectiveness and include:
• Accuracy: The proportion of correctly classified instances among the total instances. It is given as:
where TP (True Positives) refers to correctly predicted positive instances, TN (True Negatives) refers to correctly predicted negative instances, FP (False Positives) refers to incorrectly predicted positive instances, and FN (False Negatives) refers to incorrectly predicted negative instances.
• Sensitivity (Recall): The proportion of actual positives that are correctly identified by the model. It is calculated as:
• Specificity: The proportion of actual negatives that are correctly identified by the model. It is given by:
• Precision: The proportion of positive identifications that were actually correct. It is expressed as:
• F1-score: The harmonic mean of precision and recall, providing a single metric that balances both. It is defined as:
• Area under the Receiver Operating Characteristic Curve (AUC-ROC): The ROC curve plots the true positive rate against the false positive rate across different thresholds. The AUC-ROC measures the overall ability of the model to discriminate between positive and negative instances. It is calculated as:
where
• Area under the Precision-Recall Curve (AUC-PR): The Precision-Recall curve plots precision against recall for various thresholds. The AUC-PR summarizes the curve and reflects the model’s performance in identifying positive class instances, especially in imbalanced datasets. It is given by:
where
These metrics collectively provide a robust evaluation of the framework’s performance, reflecting its accuracy, ability to handle imbalanced classes, and effectiveness in different healthcare decision-making scenarios.
The simulation produced compelling results, highlighting the effectiveness and adaptability of our AI-NLP fusion framework across various healthcare contexts. In this section we provide the key findings and then discuss their implications.
1. Accurate Disease Diagnosis: The AI-NLP framework exhibited remarkable performance in disease diagnosis, achieving an average diagnostic accuracy of 93.5%. This accuracy rate signifies the framework’s ability to correctly identify and classify various medical conditions based on patient data and clinical information. Importantly, the framework surpassed traditional diagnostic methods, such as manual interpretation of clinical data and standardized diagnostic tests, by 12%, highlighting its superiority in accurately diagnosing diseases compared to conventional approaches.
The diagnostic model was powered by Gradient Descent and Adam Optimization, which were employed to fine-tune the predictive models for disease classification. NLP processes such as Named Entity Recognition (NER) and Text Preprocessing were utilized to extract relevant medical information from clinical notes, further enhancing the accuracy of the diagnostic predictions.
In instances involving rare diseases, where accurate diagnosis is particularly challenging, the framework excelled even further, achieving an impressive accuracy rate of 98%. This exceptional performance underscores the framework’s robustness and versatility in addressing complex diagnostic challenges, including those associated with rare or less prevalent medical conditions.
To visually depict the diagnostic accuracy achieved by the AI-NLP framework in comparison to traditional methods, Fig. 5 provides a graphical representation. The confusion matrix, shown in Fig. 6, further details the classification performance of the model, illustrating the true positives (TP), true negatives (TN), false positives (FP), and false negatives (FN) across different disease categories.
Table 3 summarizes the performance metrics for accurate disease diagnosis. The framework’s sensitivity of 0.91 indicates its ability to correctly identify positive cases, while its specificity of 0.94 reflects its proficiency in correctly identifying negative cases. Moreover, the precision metric, which measures the proportion of true positive diagnoses among all positive diagnoses made by the model, was determined to be 0.96, indicating a high level of accuracy in positive predictions. Similarly, the recall metric, which measures the proportion of true positive diagnoses among all actual positive cases, was found to be 0.93, indicating the model’s effectiveness in capturing all positive cases. The F1-score, a harmonic mean of precision and recall, was calculated to be 0.94, indicating a balance between precision and recall. Furthermore, the area under the receiver operating characteristic curve (AUC-ROC) and the area under the precision-recall curve (AUC-PR) were calculated to be 0.96 and 0.95, respectively, demonstrating the model’s overall performance in distinguishing between true and false diagnoses across different thresholds.
2. Personalized Treatment Recommendations: Leveraging patient-specific data, the framework generated tailored treatment plans with an average precision of 96.7%. The AI optimization algorithms, including Gradient Descent and Adam Optimization, were used to enhance the accuracy of the treatment recommendations. NLP processes, particularly Tokenization and Sentiment Analysis, enabled the system to process patient records and feedback, ensuring that treatment plans were personalized based on the patient’s clinical profile. This high precision indicates the accuracy of the framework in recommending treatments that are most suitable for individual patients, minimizing the likelihood of unnecessary or ineffective interventions. Additionally, the framework demonstrated a recall rate of 94%, signifying its ability to identify optimal treatment options for a vast majority of patients based on their unique clinical profiles. To assess the performance of the personalized treatment recommendations comprehensively, we evaluated the precision-recall trade-off using additional metrics. The F1-score, which considers both precision and recall, was calculated to be 0.95, indicating a harmonious balance between the precision of the recommendations and the coverage of relevant treatment options. Furthermore, the area under the receiver operating characteristic curve (AUC-ROC) and the area under the precision-recall curve (AUC-PR) were determined to be 0.97 and 0.96, respectively. These metrics provide further insights into the overall performance of the framework in distinguishing between positive and negative treatment outcomes across different thresholds. Table 4 presents a detailed summary of the performance metrics associated with the personalized treatment recommendations generated by the AI-NLP framework.
3. Early Risk Stratification: Leveraging datasets from PhysioNet, and by employing Stochastic Gradient Descent (SGD) and NER, the framework enabled the early identification of high-risk patients with an impressive sensitivity of 91%, significantly reducing the lead time for interventions by an average of 23%. The model’s ability to correctly identify negative cases was reflected in its specificity score of 92%.
4. Enhanced Clinical Documentation: Automation of documentation processes, utilizing datasets from PhysioNet, led to tangible improvements in efficiency, with a 35% reduction in documentation time and a 27% decrease in error rates. NLP processes, particularly Text Preprocessing and Sentiment Analysis, were instrumental in improving the accuracy and completeness of the clinical records, resulting in a 40% improvement in documentation quality.

Figure 5: Comparison of diagnostic accuracy: AI-NLP Framework vs. traditional methods

Figure 6: Confusion matrix for disease diagnosis


7.2 Discussion and Implications
The simulation results underscore the transformative potential of AI-driven data analytics and NLP processes in healthcare decision-making. Our framework, fueled by advanced algorithms and extensive EHR data, has demonstrated remarkable capabilities to revolutionize clinical practice, leading to tangible improvements in patient outcomes and healthcare delivery efficiency. These findings highlight the pivotal role of AI technologies in shaping the future of healthcare, offering unprecedented opportunities for personalized, evidence-based care.
To clarify the impact of these advancements on various stakeholders, the following implications are outlined:
• Healthcare Practitioners: The framework offers significant improvements in diagnostic accuracy and personalized treatment recommendations. Practitioners can leverage these advancements to enhance patient care, streamline clinical workflows, and make more informed decisions based on comprehensive data analysis.
• Researchers: The findings from this study open avenues for further research and exploration. Researchers are encouraged to validate and refine the framework in different clinical contexts, integrate it with emerging technologies, and investigate its applications in precision medicine and population health management.
• Policymakers: For policymakers, the research underscores the importance of supporting the development and implementation of AI-driven technologies in healthcare. It highlights the need for creating policies that address data privacy, security, and ethical considerations to facilitate the effective and equitable integration of these technologies.
However, within these promising advancements, it is crucial to acknowledge and address several challenges. Data privacy concerns remain paramount, necessitating robust measures to safeguard patient information and ensure compliance with regulatory standards. Additionally, mitigating algorithmic bias and promoting data interoperability are essential to foster trust in AI-driven systems and mitigate potential disparities in healthcare delivery.
Building on the insights gained from the simulation, future research directions include further refinement and validation of the framework in diverse clinical settings, integration with emerging technologies such as federated learning and blockchain for enhanced data privacy and security, and exploration of novel applications in areas such as precision medicine, population health management, and telemedicine. By continuously innovating and advancing AI-driven approaches to healthcare decision-making, we can pave the way for a more efficient, effective, and patient-centered healthcare system.
7.3 Limitations of Simulation and Real-World Applicability
While our simulation utilized datasets derived from real-world EHRs to closely mirror clinical conditions, it is important to acknowledge several limitations inherent in simulation environments compared to actual clinical settings.
1. Simulated Data vs. Real-World Variability: Despite using EHR data to simulate diverse healthcare scenarios, the controlled nature of simulations may not fully capture the wide range of variability present in real-world patient data. Factors such as data quality, missing information, and patient demographics can differ significantly between simulated datasets and actual clinical data.
2. Clinical Workflow Differences: Simulations often cannot replicate the full complexity of real-world clinical workflows, including the nuances of clinician-patient interactions, decision-making processes, and the integration of various healthcare technologies.
3. Scalability and Implementation Challenges: The effectiveness of the framework in simulation does not guarantee seamless integration and scalability in actual healthcare settings. Challenges such as system interoperability, data privacy concerns, and operational feasibility need to be addressed during real-world deployment.
4. External Validity: While our simulation results are promising, their applicability to different healthcare contexts and diverse patient populations must be validated through additional real-world studies. This will help confirm that the framework performs as expected across various clinical scenarios and settings.
In summary, while the simulation provides valuable insights into the potential performance of our AI-NLP framework, it is essential to conduct further research involving real-world clinical trials to validate its effectiveness and address any discrepancies between simulated and actual data.
This study examined the integration of AI and NLP processes in enhancing healthcare decision-making. We developed and tested a framework that combines AI-driven data analytics with NLP within IoMT environments. The framework demonstrated notable success, achieving an average diagnostic accuracy of 93.5% across various scenarios and 98% in rare disease cases. Our findings highlight the substantial potential of AI and NLP to improve patient outcomes, streamline healthcare workflows, and refine decision support systems.
The integration of AI and NLP processes offers significant benefits for personalized medicine and predictive analytics. The framework’s patient-specific treatment plans achieved an average precision of 96.7%, underscoring its effectiveness in tailoring interventions to individual needs. Additionally, AI and NLP can automate routine tasks, allowing healthcare professionals to concentrate on delivering high-quality care and enhancing patient experiences.
Despite these advancements, the study acknowledges several limitations. Simulated environments may not fully capture the variability and complexity of real-world clinical settings, and challenges related to data privacy and algorithmic bias must be addressed. Future research should focus on validating the framework in diverse clinical contexts, exploring emerging technologies such as federated learning and blockchain, and addressing regulatory and ethical considerations.
Moving forward, interdisciplinary collaboration is essential for advancing AI and NLP processes in healthcare. Researchers, policymakers, and healthcare practitioners must work together to overcome existing challenges and embrace these technologies to drive innovation and improve healthcare delivery.
Acknowledgement: None.
Funding Statement: The authors wish to extend their appreciation to the Researchers Supporting Project number (RSP2024R281), King Saud University, Riyadh, Saudi Arabia.
Author Contributions: Study conception and design: Soha Rawas, Cerine Tafran; data collection: Soha Rawas, Cerine Tafran; analysis and interpretation of results: Soha Rawas, Cerine Tafran, Duaa AlSaeed, Nadia Al-Ghreimil; draft manuscript preparation: Soha Rawas, Cerine Tafran, Duaa AlSaeed, Nadia Al-Ghreimil. All authors reviewed the results and approved the final version of the manuscript.
Availability of Data and Materials: The data presented in this study are openly available in PhysioNet at http://www.physionet.org, accessed on 12 November 2024.
Ethics Approval: Not applicable.
Conflicts of Interest: The authors declare no conflicts of interest to report regarding the present study. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
References
1. S. Emadi, “Revolutionizing healthcare: The role of the Internet of Things in the field of medical engineering,” Future Gen. Commun. Internet Things, vol. 2, no. 3, pp. 1–5, 2023. [Google Scholar]
2. D. Khanna, N. Jindal, H. Singh, and P. S. Rana, “Applications and challenges in healthcare big data: A strategic review,” Current Med. Imaging, vol. 19, no. 1, pp. 27–36, 2023. doi: 10.2174/1573405618666220308113707. [Google Scholar] [PubMed] [CrossRef]
3. C. H. Guo and J. F. Chen, “Big data analytics in healthcare,” in Knowledge Technology and Systems: Toward Establishing Knowledge Systems Science, Y. Nakamori, Ed. Singapore: Springer Nature, 2023, pp. 27–70. doi: 10.1007/978-981-99-1075-5_2. [Google Scholar] [CrossRef]
4. M. Badawy, N. Ramadan, and H. A. Hefny, “Healthcare predictive analytics using machine learning and deep learning techniques: A survey,” J. Electr. Syst. Inf. Technol., vol. 10, no. 1, Aug. 2023, Art. no. 40. doi: 10.1186/s43067-023-00108-y. [Google Scholar] [CrossRef]
5. A. D. Samala and S. Rawas, “Transforming healthcare data management: A blockchain-based cloud EHR system for enhanced security and interoperability,” Int. J. Online Biomed. Eng., vol. 20, no. 2, pp. 46–60, 2024. doi: 10.3991/ijoe.v20i02.45693. [Google Scholar] [CrossRef]
6. R. Hasan, M. M. Kamal, A. Daowd, T. Eldabi, I. Koliousis and T. Papadopoulos, “Critical analysis of the impact of big data analytics on supply chain operations,” Prod. Plann. Control, vol. 35, no. 1, pp. 46–70, Jan. 2024. doi: 10.1080/09537287.2022.2047237. [Google Scholar] [CrossRef]
7. K. H. Hohman et al., “Leveraging electronic health record data for timely chronic disease surveillance: The multi-state EHR-based network for disease surveillance,” J. Public Health Manage. Pract., vol. 29, no. 2, Apr. 2023, Art. no. 162. doi: 10.1097/PHH.0000000000001693. [Google Scholar] [PubMed] [CrossRef]
8. N. Cook, M. Hoopes, F. M. Biel, N. Cartwright, M. Gordon and M. Sills, “Early results of an initiative to assess exposure to firearm violence in ambulatory care: Descriptive analysis of electronic health record data,” JMIR Public Health Surveill., vol. 10, no. 1, Feb. 2024, Art. no. e47444. doi: 10.2196/47444. [Google Scholar] [PubMed] [CrossRef]
9. A. S. Baiyewu, “Overview of the role of data analytics in advancing health service,” Open Access Library J., vol. 10, no. 6, pp. 1–19, Jun. 2023. doi: 10.4236/oalib.1110207. [Google Scholar] [CrossRef]
10. Y. T. Lo, J. C. Liao, M. H. Chen, C. M. Chang, and C. T. Li, “Predictive modeling for 14-day unplanned hospital readmission risk by using machine learning algorithms,” BMC Med. Inform Decis. Mak., vol. 21, no. 1, Oct. 2021, Art. no. 288. doi: 10.1186/s12911-021-01639-y. [Google Scholar] [PubMed] [CrossRef]
11. N. C. da Silva, M. K. Albertini, A. R. Backes, and G. das Graças Pena, “Machine learning for hospital readmission prediction in pediatric population,” Comput. Methods Program. Biomed., vol. 244, 2024, Art. no. 107980. doi: 10.1016/j.cmpb.2023.107980. [Google Scholar] [PubMed] [CrossRef]
12. G. D. Miner et al., “Practical data analytics for innovation in medicine,” in Practical Data Analytics for Innovation in Medicine, 2nd ed. Cambridge, MA, USA: Academic Press, 2023. doi: 10.1016/C2021-0-02083-6. [Google Scholar] [CrossRef]
13. K. Sideris et al., “Artificial intelligence predictive analytics in heart failure: Results of the pilot phase of a pragmatic randomized clinical trial,” J. Am. Med. Inform. Assoc., vol. 31, no. 4, pp. 919–928, 2024. doi: 10.1093/jamia/ocae017. [Google Scholar] [PubMed] [CrossRef]
14. H. Bastani and P. Shi, “Proceed with care: Integrating predictive analytics with patient decision-making,” 2023. Accessed: Aug. 12, 2024. [Online]. Available: https://hamsabastani.github.io/proceedwithcare.pdf [Google Scholar]
15. S. Aminabee, “The future of healthcare and patient-centric care: Digital innovations, trends, and predictions,” in Emerging Technologies for Health Literacy and Medical Practice. Hershey, PA, USA: IGI Global, 2024, pp. 240–262. doi: 10.4018/979-8-3693-1214-8.ch012. [Google Scholar] [CrossRef]
16. K. C. Derecho et al., “Technology adoption of electronic medical records in developing economies: A systematic review on physicians’ perspective,” Digit. Health, vol. 10, Jan. 2024, Art. no. 20552076231224605. doi: 10.1177/20552076231224605. [Google Scholar] [PubMed] [CrossRef]
17. M. U. Tariq, “Revolutionizing health data management with blockchain technology: Enhancing security and efficiency in a digital era,” in Emerging Technologies for Health Literacy and Medical Practice. Hershey, PA, USA: IGI Global, 2024, pp. 153–175. [Google Scholar]
18. A. H. Seh et al., “An analysis of integrating machine learning in healthcare for ensuring confidentiality of the electronic records,” Comput. Model. Eng. Sci., vol. 130, no. 3, pp. 1387–1422, 2022. doi: 10.32604/cmes.2022.018163. [Google Scholar] [CrossRef]
19. A. Sonavane, A. Khamparia, and D. Gupta, “A systematic review on the internet of medical things: Techniques, open issues, and future directions,” Comput. Model. Eng. Sci., vol. 137, no. 2, pp. 1525–1550, 2023. doi: 10.32604/cmes.2023.028203. [Google Scholar] [CrossRef]
20. M. Kumar et al., “Healthcare Internet of Things (H-IoTCurrent trends, future prospects, applications, challenges, and security issues,” Electronics, vol. 12, no. 9, 2023, Art. no. 2050. doi: 10.3390/electronics12092050. [Google Scholar] [CrossRef]
21. O. Ali, W. Abdelbaki, A. Shrestha, E. Elbasi, M. A. A. Alryalat, and Y. K. Dwivedi, “A systematic literature review of artificial intelligence in the healthcare sector: Benefits, challenges, methodologies, and functionalities,” J. Innov. Knowl., vol. 8, no. 1, 2023, Art. no. 100333. doi: 10.1016/j.jik.2023.100333. [Google Scholar] [CrossRef]
22. M. Junnu, “Role of natural language processing in extracting insights from medical text data,” Eur. J. Mod. Med. Pract., vol. 3, no. 9, pp. 128–137, Sep. 2023. [Google Scholar]
23. U. Ahmed, K. Iqbal, and M. Aoun, “Natural language processing for clinical decision support systems: A review of recent advances in healthcare,” J. Intell. Connect. Emerg. Technol., vol. 8, no. 2, pp. 1–16, 2023. [Google Scholar]
24. K. Nova, “Generative AI in healthcare: Advancements in electronic health records, facilitating medical languages, and personalized patient care,” J. Adv. Anal. Healthcare Manage., vol. 7, no. 1, pp. 115–131, 2023. [Google Scholar]
25. K. Suvirat, D. Tanasanchonnakul, S. Chairat, and S. Chaichulee, “Leveraging language models for inpatient diagnosis coding,” Appl. Sci., vol. 13, no. 16, 2023, Art. no. 9450. doi: 10.3390/app13169450. [Google Scholar] [CrossRef]
26. N. Karimbux et al., “Measuring patient experience of oral health care: A call to action,” J. Evid.-Based Dental Prac., vol. 23, no. 1, 2023, Art. no. 101788. doi: 10.1016/j.jebdp.2022.101788. [Google Scholar] [PubMed] [CrossRef]
27. E. Hossain et al., “Natural language processing in electronic health records in relation to healthcare decision-making: A systematic review,” Comput. Biol. Med., vol. 155, 2023, Art. no. 106649. doi: 10.1016/j.compbiomed.2023.106649. [Google Scholar] [PubMed] [CrossRef]
28. S. A. Alowais et al., “Revolutionizing healthcare: The role of artificial intelligence in clinical practice,” BMC Med. Educ., vol. 23, no. 1, Sep. 2023, Art. no. 689. doi: 10.1186/s12909-023-04698-z. [Google Scholar] [PubMed] [CrossRef]
29. M. Bucholc, S. Titarenko, X. Ding, C. Canavan, and T. Chen, “A hybrid machine learning approach for prediction of conversion from mild cognitive impairment to dementia,” Expert. Syst. Appl., vol. 217, 2023, Art. no. 119541. doi: 10.1016/j.eswa.2023.119541. [Google Scholar] [CrossRef]
30. Z. Sharif, L. T. Jung, M. Ayaz, M. Yahya, and S. Pitafi, “Priority-based task scheduling and resource allocation in edge computing for health monitoring system,” J. King Saud Univ. -Comput. Inf. Sci., vol. 35, no. 2, pp. 544–559, 2023. doi: 10.1016/j.jksuci.2023.01.001. [Google Scholar] [CrossRef]
31. M. Rana and M. Bhushan, “Machine learning and deep learning approach for medical image analysis: Diagnosis to detection,” Multimed. Tools Appl., vol. 82, no. 17, pp. 26731–26769, Jul. 2023. doi: 10.1007/s11042-022-14305-w. [Google Scholar] [PubMed] [CrossRef]
32. J. Ruiz-Ramos et al., “Healthcare risk stratification model for emergency departments based on drugs, income and comorbidities: The DICER-score,” BMC Emerg. Med., vol. 24, no. 1, Feb. 2024, Art. no. 23. doi: 10.1186/s12873-024-00946-7. [Google Scholar] [PubMed] [CrossRef]
33. S. Sivarajkumar et al., “Clinical information retrieval: A literature review,” J. Healthc. Inform. Res., vol. 8, no. 2, pp. 313–352, Jun. 2024. doi: 10.1007/s41666-024-00159-4. [Google Scholar] [PubMed] [CrossRef]
34. I. Dhaini, S. Rawas, and A. El-Zaart, “An intelligent and green e-healthcare model for an early diagnosis of medical images as an IoMT application,” presented at 19th Int. Conf. Distrib. Comput. Artif. Intell., Cham, Switzerland, 2023. [Google Scholar]
35. S. F. Ahmed, M. S. B. Alam, S. Afrin, S. J. Rafa, N. Rafa and A. H. Gandomi, “Insights into Internet of Medical Things (IoMTData fusion, security issues and potential solutions,” Inf. Fusion, vol. 102, 2024, Art. no. 102060. doi: 10.1016/j.inffus.2023.102060. [Google Scholar] [CrossRef]
36. M. Osama et al., “Internet of medical things and Healthcare 4.0: Trends, requirements, challenges, and research directions,” Sensors, vol. 23, no. 17, 2023, Art. no. 7435. doi: 10.3390/s23177435. [Google Scholar] [PubMed] [CrossRef]
37. R. Dwivedi, D. Mehrotra, and S. Chandra, “Potential of Internet of Medical Things (IoMT) applications in building a smart healthcare system: A systematic review,” J. Oral Biol. Craniofac. Res., vol. 12, no. 2, pp. 302–318, 2022. doi: 10.1016/j.jobcr.2021.11.010. [Google Scholar] [PubMed] [CrossRef]
38. J. B. Awotunde, R. G. Jimoh, S. O. Folorunso, E. A. Adeniyi, K. M. Abiodun and O. O. Banjo, “Privacy and security concerns in IoT-based healthcare systems,” in The Fusion of Internet of Things, Artificial Intelligence, and Cloud Computing in Health Care. Cham, Switzerland: Springer, pp. 105–134, doi: 10.1007/978-3-030-75220-0_6. [Google Scholar] [CrossRef]
39. I. H. Sarker, “AI-based modeling: Techniques, applications and research issues towards automation, intelligent and smart systems,” SN Comput. Sci., vol. 3, no. 2, Mar. 2022, Art. no. 158. doi: 10.1007/s42979-022-01043-x. [Google Scholar] [PubMed] [CrossRef]
40. C. Kuruba, N. Pushpalatha, G. Ramu, I. Suneetha, M. R. Kumar and P. Harish, “Data mining and deep learning-based hybrid health care application,” Appl. Nanosci., vol. 13, no. 3, pp. 2431–2437, Mar. 2023. doi: 10.1007/s13204-021-02333-1. [Google Scholar] [CrossRef]
41. D. Çelik Ertuğrul and A. Elçi, “A survey on semanticized and personalized health recommender systems,” Expert. Syst., vol. 37, no. 4, Aug. 2020, Art. no. e12519. doi: 10.1111/exsy.12519. [Google Scholar] [CrossRef]
42. L. Wang and E. Demeulemeester, “Simulation optimization in healthcare resource planning: A literature review,” IISE Trans., vol. 55, no. 10, pp. 985–1007, Oct. 2023. doi: 10.1080/24725854.2022.2147606. [Google Scholar] [CrossRef]
43. S. Williams and E. Petrovich, “Natural language processing for unlocking insights from unstructured big data in the healthcare industry,” Emerg. Trends Mach. Intell. Big Data, vol. 15, no. 10, pp. 30–39, 2023. [Google Scholar]
44. J. E. Tang et al., “Using sentiment analysis to understand what patients are saying about hand surgeons online,” Hand, vol. 18, no. 5, pp. 854–860, Jul. 2023. doi: 10.1177/15589447211060439. [Google Scholar] [PubMed] [CrossRef]
45. S. Ajmal, A. A. I. Ahmed, and C. Jalota, “Natural language processing in improving information retrieval and knowledge discovery in healthcare conversational agents,” J. Artif. Intell. Mach. Learn. Manage., vol. 7, no. 1, pp. 34–47, 2023. Accessed: Aug. 12, 2024. [Online]. Available: https://journals.sagescience.org/index.php/jamm/article/view/73 [Google Scholar]
46. M. G. Crowson, E. Alsentzer, J. Fiskio, and D. W. Bates, “Towards medical billing automation: NLP for outpatient clinician note classification,” 2023. doi: 10.1101/2023.07.07.23292367. [Google Scholar] [PubMed] [CrossRef]
47. B. Y. Kasula, “Ethical implications and future prospects of Artificial Intelligence in healthcare: A research synthesis,” Int. Meridian J., vol. 6, no. 6, pp. 1–7, 2024. [Google Scholar]
48. M. Tayefi et al., “Challenges and opportunities beyond structured data in analysis of electronic health records,” WIREs Comput. Stats., vol. 13, no. 6, Nov. 2021, Art. no. e1549. doi: 10.1002/wics.1549. [Google Scholar] [CrossRef]
49. A. L. Goldberger et al., “PhysioBank, PhysioToolkit, and PhysioNet: Components of a new research resource for complex physiologic signals,” Circulation, vol. 101, no. 23, pp. E215–220, Jun. 2000. doi: 10.1161/01.CIR.101.23.e215. [Google Scholar] [PubMed] [CrossRef]
50. J. M. Johnson and T. M. Khoshgoftaar, “Data-centric AI for healthcare fraud detection,” SN Comput. Sci., vol. 4, no. 4, May 2023, Art. no. 389. doi: 10.1007/s42979-023-01809-x. [Google Scholar] [PubMed] [CrossRef]
51. S. Borrohou, R. Fissoune, and H. Badir, “Data cleaning survey and challenges-improving outlier detection algorithm in machine learning,” J. Smart Cities Soc., vol. 2, no. 3, pp. 125–140, 2023. doi: 10.3233/SCS-230008. [Google Scholar] [CrossRef]
52. S. Boeschoten, C. Catal, B. Tekinerdogan, A. Lommen, and M. Blokland, “The automation of the development of classification models and improvement of model quality using feature engineering techniques,” Expert. Syst. Appl., vol. 213, 2023, Art. no. 118912. doi: 10.1016/j.eswa.2022.118912. [Google Scholar] [CrossRef]
53. I. Izonin, R. Tkachenko, N. Shakhovska, B. Ilchyshyn, and K. K. Singh, “A two-step data normalization approach for improving classification accuracy in the medical diagnosis domain,” Mathematics, vol. 10, no. 11, 2022, Art. no. 1942. doi: 10.3390/math10111942. [Google Scholar] [CrossRef]
54. J. Sim et al., “Natural language processing with machine learning methods to analyze unstructured patient-reported outcomes derived from electronic health records: A systematic review,” Artif. Intell. Med., vol. 146, 2023, Art. no. 102701. doi: 10.1016/j.artmed.2023.102701. [Google Scholar] [PubMed] [CrossRef]
55. N. Q. K. Le, D. T. Do, F. Y. Chiu, E. K. Y. Yapp, H. Y. Yeh and C. Y. Chen, “XGBoost improves classification of MGMT promoter methylation status in IDH1 wildtype glioblastoma,” J. Pers. Med., vol. 10, no. 3, Sep. 2020, Art. no. 128. doi: 10.3390/jpm10030128. [Google Scholar] [PubMed] [CrossRef]
56. C. Lokker et al., “Boosting efficiency in a clinical literature surveillance system with LightGBM,” PLoS Digit Health, vol. 3, no. 9, Sep. 2024, Art. no. e0000299. doi: 10.1371/journal.pdig.0000299. [Google Scholar] [PubMed] [CrossRef]
57. M. A. Morid, O. R. L. Sheng, and J. Dunbar, “Time series prediction using deep learning methods in healthcare,” ACM Trans. Manage. Inf. Syst., vol. 14, no. 1, pp. 1–29, Jan. 2023. doi: 10.1145/3531326. [Google Scholar] [CrossRef]
58. B. J. Erickson and F. Kitamura, “Magician’s corner: 9. Performance metrics for machine learning models,” Radiol.: Artif. Intell., vol. 3, no. 3, May 2021, Art. no. e200126. doi: 10.1148/ryai.2021200126. [Google Scholar] [PubMed] [CrossRef]
Cite This Article
 Copyright © 2024 The Author(s). Published by Tech Science Press.
Copyright © 2024 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools