 Open Access
Open Access
ARTICLE
Harnessing Blockchain to Address Plasma Donation Network Challenges
1 Department of Computer Science and Engineering, SRM University, Delhi-NCR, 1310029, India
2 Department of Computer Science and Information, Taibah University, Medina, 42353, Saudi Arabia
3 Department of Computer Science and Engineering, KIET Group of Institutions, Delhi-NCR, Ghaziabad, 201206, India
4 College of Computer Science and Engineering, Taibah University, Madinah, Saudi Arabia
5 College of Computer Science and Engineering, Taibah University, Yanbu, Madinah, Saudi Arabia
6 Department of Computer Science and Engineering, Banasthali Vidyapith, Rajasthan, 304022, India
7 Department of Computer Science and Engineering, Graphic Era (Deemed to Be University), Dehradun, 248002, India
* Corresponding Author: Mohammad Zubair Khan. Email:
Computers, Materials & Continua 2023, 76(1), 631-646. https://doi.org/10.32604/cmc.2023.039241
Received 17 January 2023; Accepted 18 April 2023; Issue published 08 June 2023
Abstract
Plasma therapy is an extensively used treatment for critically unwell patients. For this procedure, a legitimate plasma donor who can continue to supply plasma after healing is needed. However, significant dangers are associated with supply management, such as the ambiguous provenance of plasma and the spread of infected or subpar blood into medicinal fabrication. Also, from an ideological standpoint, less powerful people may be exploited throughout the contribution process. Moreover, there is a danger to the logistics system because there are now just some plasma shippers. This research intends to investigate the blockchain-based solution for blood plasma to facilitate authentic plasma transfer. Blockchain parameters, including electronic identification, chain code, and certified ledgers, have the potential to exert a substantial, profound influence on the distribution and implementation process of blood banks. To understand the practical ramifications of blockchain, the current study provides a proof of concept approach that aims to simulate the procedural code of modern plasma distribution ecosystems using a blockchain-based architecture. The agent-based modeling used in the testing and evaluation mimics the supply chain to assess the blockchain’s feasibility, advantages, and constraints for the plasma.Keywords
Therapeutic items containing plasma proteins extracted from blood are called plasma compounds [1]. The industry for plasma, which provides medicines for conditions including immune deficiency diseases, is expected to grow exponentially and US$15.5 billion by next year [2]. Elevated fatality rates might be one of the worst effects of scarcely available plasma [3]. Plasma can be obtained by plasmapheresis, which involves returning the blood’s cellular components to the contributor, or as a separate process in the blood collection cycle.
The plasma supply network involves blood and plasma collection from volunteers and examining, processing, and distributing plasma. Three fundamental problems hinder the plasma supply network: unpredictability in supply and demand spots, plasma waste in therapies, and plasma scarcity in healthcare. The basic difficulty in the plasma supply network is constant access to persistent volunteers for improved supply administration and reducing plasma wastage in the treatment sector. The present plasma supply industry entails a variety of concerns, including ethical, contamination, falsification, and supply chain [1]. Paying donors can encourage those from lower socioeconomic classes, such as the impoverished and drug users, to donate plasma regularly, even if the consequences for their health are unclear, which raises an ethical issue. The contaminated blood posed a significant concern; in the late 1980s, infected blood infiltrated the supply chain, sparking an HIV outbreak [4]. Also, falsification, such as misrepresenting the plasma source or forging test results, is a big concern.
Furthermore, relying too much on a single basis uncovers the supply chain to severe dangers. Plasma accumulation needs to be improved to reduce supply chain concerns [5]. The plasma supply chain network must ensure the following:
■ Enhance transparency and tracking: Real-time visibility in the plasma supply chain must be offered when the plasma moves from the donor to the recipient. This should resolve any issues during transfer, handling, or transit.
■ Improve confidentiality and security: The plasma supply network must safeguard sensitive patient information against data breaches and guarantee that personal information is preserved.
■ Promote accountability and develop trust: To strengthen accountability and mitigate the likelihood of corruption, wastage, and misuse in the plasma supply chain, an auditable log of every activity must be kept.
■ Improve cooperation and coordination: The plasma supply chain’s participants, including donors, health centers, physicians, and authorities, must cooperate and coordinate to make sure that plasma is delivered to the areas where it is most necessary and utilized securely.
1.2 Why Blockchain Over Centralized Database?
Blockchain offers the plasma industry data integrity, traceability (without sacrificing anonymity), and commodity validation automation. This provides blood banks with more cross-matches, improved system trust (owing to a decreased risk of tainted blood clearing certification), and connectivity scaling. A typical database is impractical for the plasma sector. The first factor is related to trustworthiness. The primary advantage we have offered is a communication pathway that allows interoperability for all concerned stakeholders. In this situation, it is possible to exchange data using a normal database, but all parties involved must have confidence in the security and dependability of the central database version. Since this type of confidence has yet to exist, it is not viable.
On the contrary, blockchain protects this confidence by duplicating the ledger and requiring event approval from all contemporaries before allowing any party to change the ledger. Further, transparency is an area where conventional databases lag. The private group dialogue makes it feasible for the advantage suggested via the message channel to be realized. This kind of communication preserves network consistency by isolating a ledger between authorized participants and encrypting all data, permits, and executable code. Additionally, the feature of chain code allows for manipulating this information.
In comparison to a database, the blockchain offers a protection system that is far more adaptable. Because of the size of the plasma supply network, this flexibility is required. A database does not preserve records for each data item and would need a centralized controller to administer rights for all relevant stakeholders. Because of this, a database may give identical data to two stakeholders; however, it does not reveal how the data has changed over time. Conversely, a blockchain keeps track of all the metadata and background information for each item on the ledger. Indeed, these features demonstrate that blockchain is the best option for overcoming the problem of linear and efficient communication time. As a result, blockchain offers conventional databases a more adaptable and scalable solution for meeting the confidentiality and transparency requirements of the plasma supply network.
This study developed a distributed network for plasma matching and donor identification leveraging blockchain technology to expedite the postoperative plasma therapy procedure. Chain codes identify the plasma of the relevant blood group for critically ill patients. It will assist in keeping track of the contributions and subsequent activities. The proposed proof of concept model aims to address plasma donation network challenges, as highlighted below.
■ Facilitating plasma donation tracking and discouraging overly recurring donations with a decentralized donor registry. Thus, preventing unscrupulous tendencies wherein abusers or other vulnerable people would be taken advantage of by recurrent contributions that would endanger their health.
■ Enabling contributors to take ownership of their records, donations, and associated economic rewards through incentive-based models and a reduction in the industry intermediary’s role.
■ Verifying the plasma’s origin and ensuring it originated from a reliable one with appropriate testing and sterilization procedures.
■ Establishing a plasma donation supply-chain network with acceptable latency and throughput performance in a real-life scenario.
■ Designed and deployed chain codes to control and automate transactions involving plasma donations and inventories on a private blockchain network, improving the effectiveness and dependability of the plasma supply chain management system.
■ Making use of blockchain technology, which offers a verifiable and traceable history of all transactions and operations, increases transparency and confidence in the plasma donation process.
■ Offering a safe and effective system that allows direct interaction and data exchange between clinics, blood banks, and donors.
■ Increasing the overall efficacy and efficiency of the plasma donation procedure may help save lives and enhance the prognosis for patients who are severely sick.
The manuscript is further divided into sections. Section 2 explores the existing literature. Section 3 introduces the architectural design and implementation details of the proposed model. Section 4 presents the evaluation results achieved from the proposed model concerning latency and throughput. Section 5 finally concludes this research.
Among the most transformative advanced technologies is blockchain. Using a distributed ledger system, it stores and transmits transparent, reliable, manageable, and fault-tolerant content. Numerous blockchain solutions have been discussed in the literature throughout the years. Three categories, i.e., Public, Private, and Consortium, could be used to characterize these blockchain solutions [6].
MedRec, a decentralized distributed ledger platform built on blockchain that enables sharing and maintaining patient health information, is presented in [7]. It is a bitcoin-based approach designed to address problems with fragmentation, poor medical information accessibility, and interoperability. MedRec is a service that enables smart contracts and uses proof-of-concept as its primary agreement method [8]. The smart contract uses a cryptographic hash method to preserve the confidentiality and integrity of healthcare data.
The author addressed the difficulties with the present medical blockchains in [9]. According to the research, the medical supply chain is one of the most important industries that need monitoring. According to the WHO, fraudulent, pirated, and subpar medications are sold on the marketplace each year for over $200 billion [10]. To protect the medical supply chain, many blockchain healthcare systems have been developed, including block verify [9], chronicled [11], and farm trust [12].
A blockchain-based startup called MedicoHealth [13] aims to streamline the disjointed healthcare industry. The MedicoHealth platform enables completely private and secure customer interaction with top doctors around the globe.
Investigation into the blood supply chain has concentrated on ensuring blood supplies during emergencies and reducing travel times. Dusseljee-Peute et al. [14] proposed a technique for selecting the appropriate blood registration locations and the optimum locations for blood offerings. A system for data management for the blood supply chain that utilized Radio-Frequency identification (RFID) was proposed in [15,16]. The main drawback of this approach is confidentiality since data may be altered.
Baek et al. [17] created a high-level framework for a blockchain-based blood supply chain utilizing the concept of a shared ledger. The approach does not control blood wastage, encourage donor compatibility, or maintain track of donor data. KanChain [18], a permission blood delivery system based on Ethereum, has been proposed in recent research. The concept offers monitoring participant transactions of KanCoins to trace the blood path. Peltoniemi et al. conducted an exploratory study on the potential use of a blockchain-based supply chain for plasma [19]. The idea of compensating potential participants to encourage more consensual donations is further clarified in [20].
Lakshminarayanan et al. [21] aim to create a combination model that manages and monitors supplied blood utilizing new blockchain technology’s potential, allowing for better photography, peer-to-peer tracing, and reliability.
To prevent data manipulation and deformation, Arsyad et al. suggested the blockchain-based Encapsulating Block Mesh (EBM) [22]. This allows data to be tracked securely and transparently. To decrease installation and implementation delay as well as mean reaction latency in the real-time smart healthcare system, Raj et al. developed blockchain-based identity management for a health surveillance system to decrease installation and implementation delay and mean reaction latency in the real-time smart healthcare system [23]. Using a blockchain network, Gupta et al. suggested a very effective attribute-based searchable encryption strategy for cloud-based cyber-physical medical systems [24]. For devices in the internet of things, Lu et al. developed a unique blockchain-based cloud storage system that can achieve safe data exchange with minimal computational burden [25]. Access management was made simpler for the Internet of Things in 2019 by Ding et al. revolutionary attribute-based access control approach [26]. A distributed blockchain cloud architecture paradigm that efficiently offloads data to the cloud was developed by Sharma et al. [27]. Yuan et al. [28] describe the overall structure of partitioned observers and collective signatures across the NTRU lattice to further enhance the efficiency of the blockchain. His plan offers a blockchain network for locations with limited resources.
Current research pioneers the field of blockchain-based plasma supply chain. By adopting real-time data recording, the proposed strategy protects the integrity of plasma data governance. Considering this, the suggested approach has the benefit of clarifying blood classifications, origins, and quality. This system can handle various plasma demands without distinguishing between supply and demand for plasma. This study broadens the research on the medical industry, particularly in the supply chain for plasma, which blockchain technology has yet to reclaim.
Plasmapheresis is the most widely used type of donation management [29]. This eliminates the requirement for whole blood donations and concentrates only on gathering plasma. However, this does not supply additional elements like red blood cells. Due to its extensive dispersion, our solution uses the conventional blood-to-plasma governance model.
Current research utilizes Hyperledger concepts as they are made to give consumers greater autonomy over blockchain-based operations’ privacy, secrecy, and performance (features that are crucial for many corporate applications). A few blockchain-based platforms, like Ethereum, are built with decentralization above control and are intended for more widespread use cases. Decentralization can be good, but it can also mean longer execution times for transactions and much less control over confidentiality and anonymity. As a result, the decision to implement a Hyperledger-based solution may be influenced by the application’s particular requirements, such as the level of anonymity and secrecy control, the required transaction processing rates, as well as the associated scenario. Using the Hyperledger Fabric framework; this research introduces and builds a plasma donation network. This approach addresses the issues with various plasma donation supply chains, including plasma source or integrity. The overall architecture of the proposed model is presented in Fig. 1. The participants of the proposed system are
■ Donors: Anyone who wishes to contribute can donate, provided they are eligible.
■ Collection Point (CP): A place responsible for verifying and registering blood/plasma donors is termed CP. It is the central point for communication among participants and other CPs belonging to regions.
■ Refining Facility (RF): It takes the overall responsibility of validating the quality of blood, extraction of plasma, and storage of plasma.
■ Medical Facility (MF): A patient approaches an MF for its treatment, and if there is a need for plasma, MF contacts the nearest CP with a request.
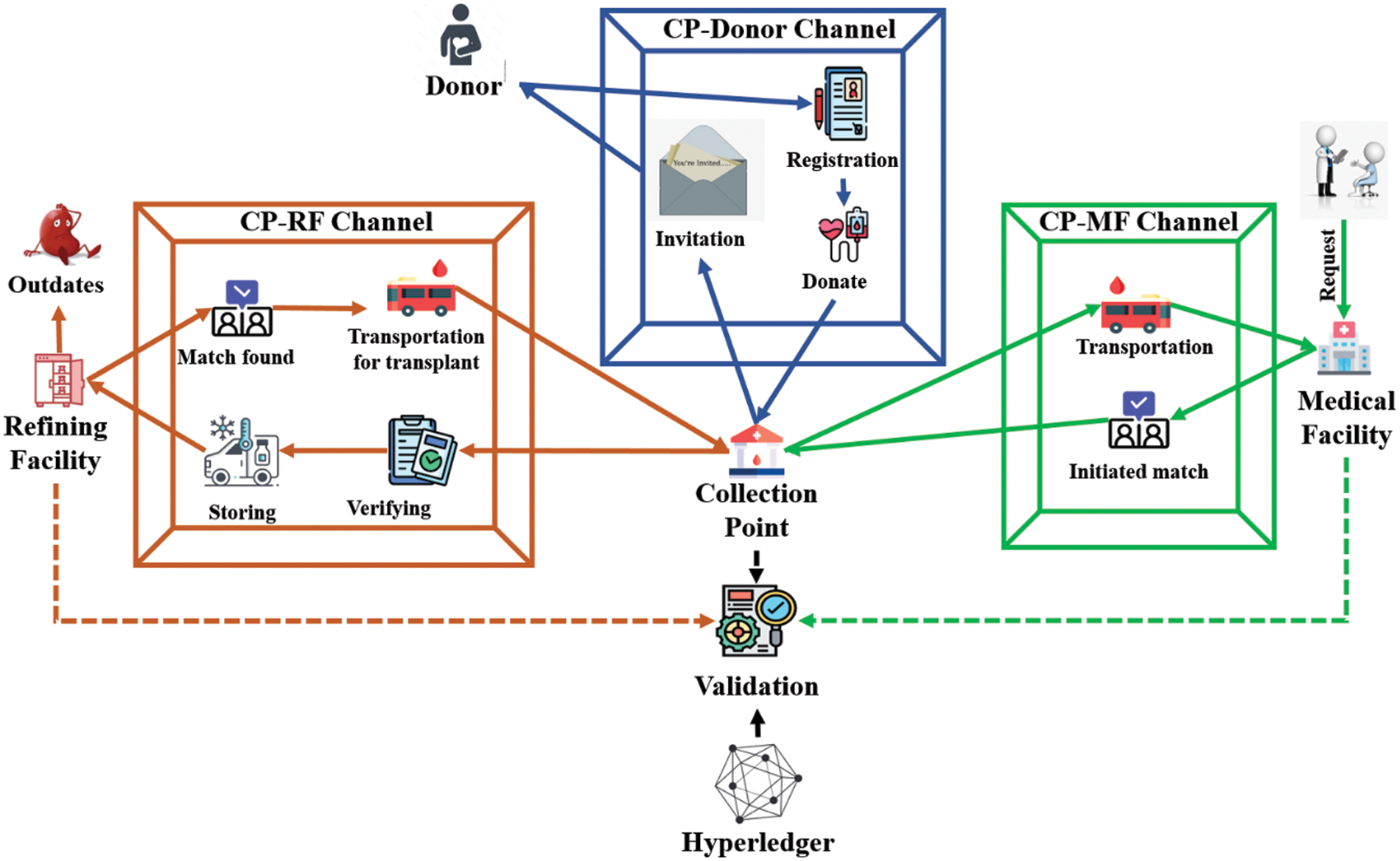
Figure 1: Architecture of proposed model
Depending upon the level of accessibility, different parties communicate with the blockchain ledger using apps. HTTP requests interact with databases and blockchain ledgers via a Rest API. It can begin a transaction, search, or check the status of a collection of actions. Also, the data is kept in MongoDB to do prospective data analyses for commercial objectives, if any, supplementary to the blockchain ledger.
The Hyperledger Fabric concept has a feature called a channel that enables secure interaction between two or more authorized entities. Every entity in the suggested model corresponds to the existing regional institutions. The proposed network consists of an ecosystem with four channels, i.e., CP-Donar, CP-RF, CP-MF, and CP-CP. A solitary CP is in charge of a territory and is linked to the CPs of other zones. All of them share the ledger, so they may access plasma information kept in their areas and available upon request. The processes done by each channel in the plasma donation network are well-explained through algorithms in the next subsections. Various algorithms defined in subsequent subsections make use of some user-defined functions that are detailed in Table 1.

The donor either volunteers to donate or has received an invitation to contribute at the closest CP. If the donor is not registered, they are registered at CP following Algorithm 1.
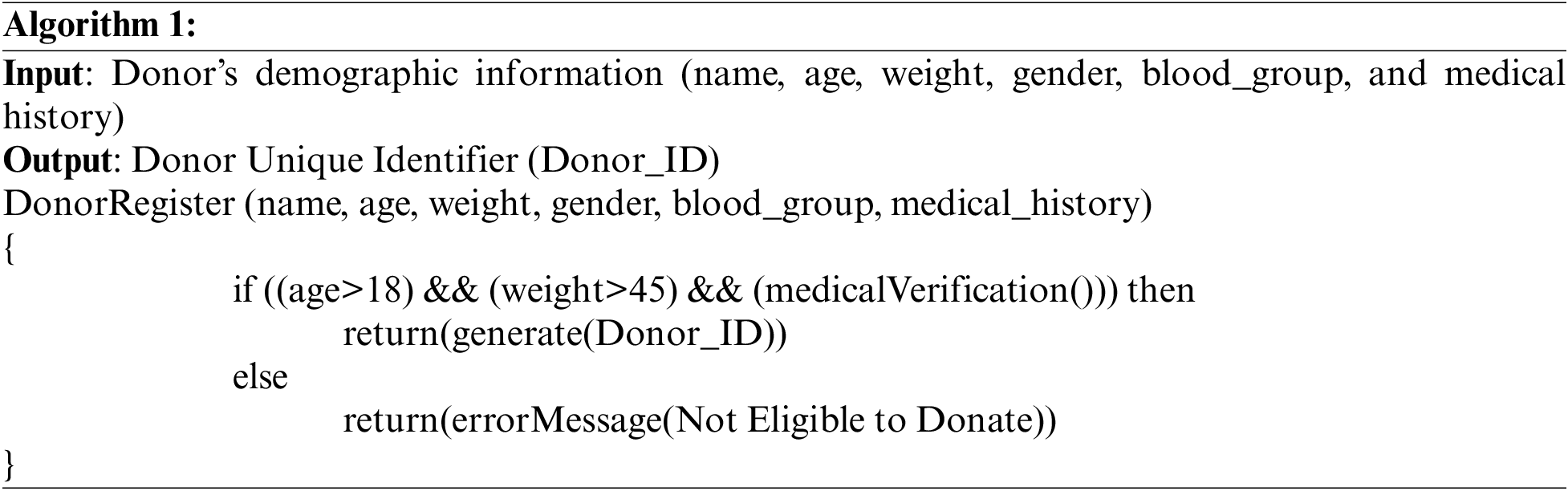
Donors can provide blood at a CP, i.e., a blood bank or a donation camp. The primary objective of a CP is to serve as a multifunctional organization in the plasma supply chain for streamlining transactions among various medical centers [30]. At a specific moment and place, the CP must solicit donations. Following the donation, the blood unit is divided into batches depending on the date of the donation. This batch is then tested to confirm the accuracy of the donor state and the blood’s purity. Certain blood-related information (such as quantity and uniformity) is collected following testing. In addition to the blood type, maturity date, and supporting documentation, this data is labeled to the constituent container. To ensure the quality, every container holding donated blood is monitored with at least three sensors, usually one for each zone. When any deviation from the threshold range of −1°C to 10°C [31] occurs, the sensors that monitor the blood units trigger the alerts. They are given a unique identifier to store samples [32,33]. Data is included in the ledger following validation.
The unprocessed units of blood are classified into separate constituents at the RF. If any commodities have corrupted during shipment from CP to RF, they are instantly eliminated as they approach the RFs (the outdates). The average proportion of loss attributed to the testing procedure, as per Nagurney, is 1.7% [34]. The proposed model exhibits the same purpose and sequence of behavior, and the validation process is carried out automatically thanks to the usage of chain code on the Hyperledger ecosystem. The first step when the items reach the RF is to validate the plasma information. Items are, therefore, carefully stored in cold storage. Every plasma is associated with a unique plasma identifier through Algorithm 2.

To maintain constituent quality and durability, each constituent is preserved according to its specific requirements [31]. Therefore, processing raw blood from CP, separating the blood into constituents, and carefully preserving and disseminating the segregated units are the roles of the RF. After that, the parts are returned to the CP for preservation and distribution. It is crucial to understand that the CP and the RF are standalone systems for some zones, a more advanced but uncommon strategic approach used to conserve effort and resources further [31].
The MFs in the area submit requests to the CP for the patient-specific supplies needed at a particular moment. Multiple facilities may submit demands; thus, the CP must choose who gets a specific request through a well-defined strategy [31]. Several variables determine this approach, and each CP may have its exclusive formula in the current research. Inside the priority queue, requests are ranked according to their transit time and distance. The plasma is transported to the CP, which sends the request to RF as specified in Algorithm 3 once the request has been matched. CP sends a request for plasma across the RF-CP link. A single CP can submit a priority queue of requests to the Chain code. The service propagates over each accessible asset and, for each asset, iterates through each request before serving the ones with the greatest priority. The CP receives the matched requests and selects whether to proceed with the matches at hand or reserve them for a later iteration.
It has been established that forwarding all demands to a centralized aggregation authority, or at the collection point, is the most effective approach to accomplish a medical facility’s primary job, enabling patients’ blood transfusions [35]. The MF starts the practice of seeking a match after receiving a request. Only a minimum of information is shared between MF and the CP throughout the transit process. This involves data verification but excludes specifics like the patient ID and MF name [31,36].
If the specified plasma type is available, it requests the closest CP. The MFs in its territory submit requests to the CPs for separate components required for a patient at a certain moment. The CPs are sent a distinct message of request affirmation along with the number of units sought whenever a request from the MF is received. The CPs also have access to a data view of the demands received by the MF. Other MF may have published a data view of its demands with the same CPs at the same time, which likewise sends a message to the CPs about the request’s existence. This is handled by bundling the queries. The CP will prioritize the requests after bundling them in a manner that reflects its allocation strategy. The bundled requests are kept in a priority queue to determine which request should be sent first.
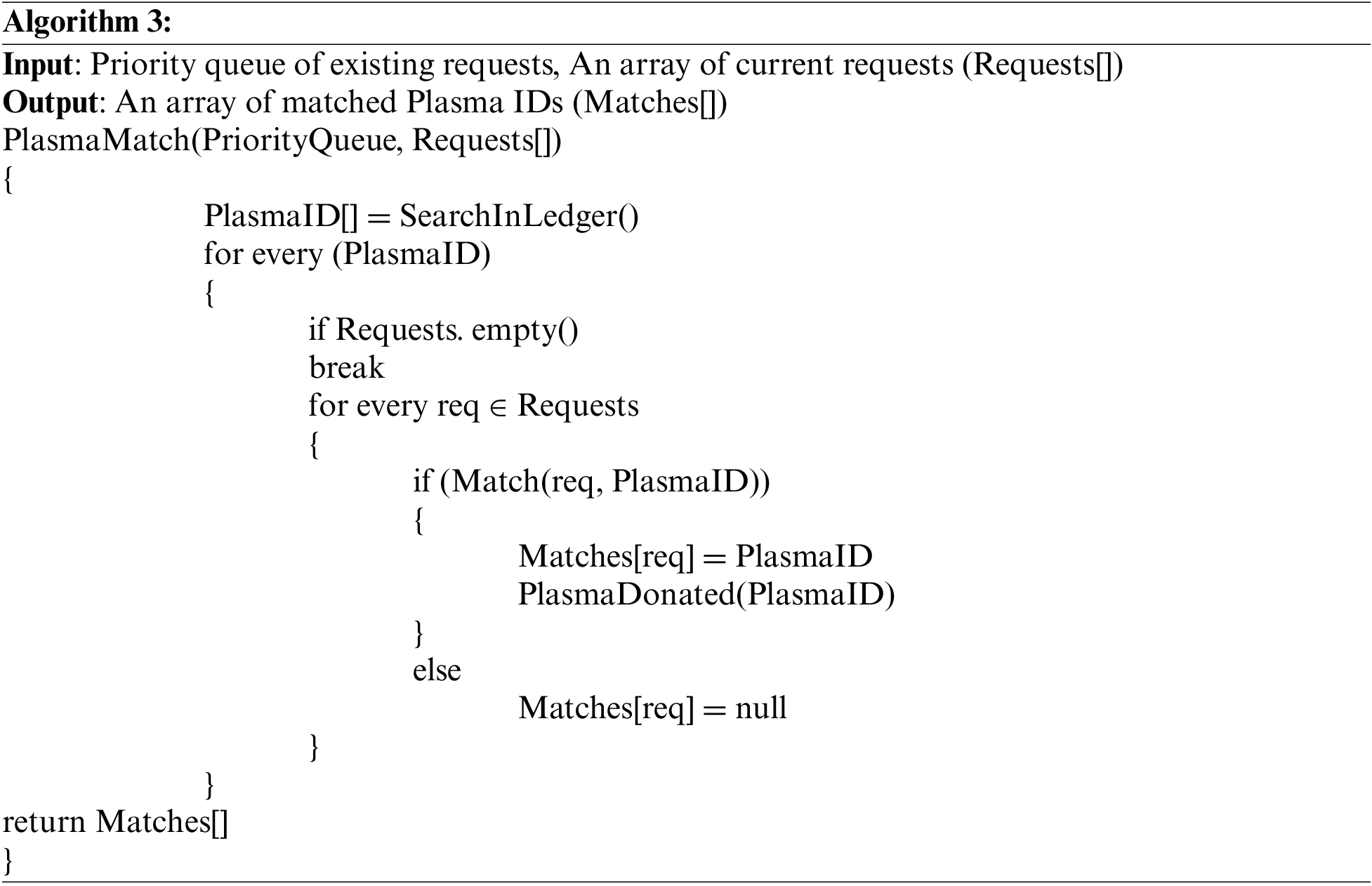
After receiving the request from MF, further communication to RF is initiated by CP to facilitate the MF with the desired plasma. Each CP will have a strategy for allocating plasma to MF in its region. Every day, plasma is checked for out-of-date units and quality evaluations, converted into changes for the CPs database as required.
Unit matching is verified once more before being issued. Other stakeholders need to be given access to the cross-matching and allocation regulations. Once the allocation has been decided, the unit is transported to the MFs for transfusion, and if not required anymore, it is eventually returned.
The CP is responsible for meeting the demands of its territory by effectively distributing its assets through trade and greater integration. However, an organization must control the allocation scheme because it has the widest dataset for identifying cross-matches and can guarantee that assets are transferred securely and confidentially. These needs are met via chain code and channel connectivity, eliminating the supervisory position’s necessity. The CP handles all management. As a result, the commodities are kept in the ledger for particular CPs and the ledger for message channels.
4 Experimental Setup and Results
An agent-based modeling controller (Python, Mesa) has been employed to stimulate the system evaluation to assess the model’s performance under concurrent connections in the blood plasma business at any moment. Statistically generated random data by following the data ranges specified by [36] is adopted in current research. For clarity, a situation with two collection points, two refining facilities, and ten medical facilities nearby within a five-kilometer range has been investigated. The blockchain was launched using the genesis blocks, including those for Blood and Donor. Ten transactions per block size were used for setting up the system. One hundred plasma demands have been generated to evaluate the suggested method’s effectiveness. Each transaction generates a new block linked to the preceding block, as seen in Fig. 2. Many organizations, such as CP, MF, and RF, participating in the plasma supply chains might play the miner’s position. They would be in charge of tracing the transit of plasma supplies, confirming their legitimacy, and adding pertinent information to the blockchain ledger.
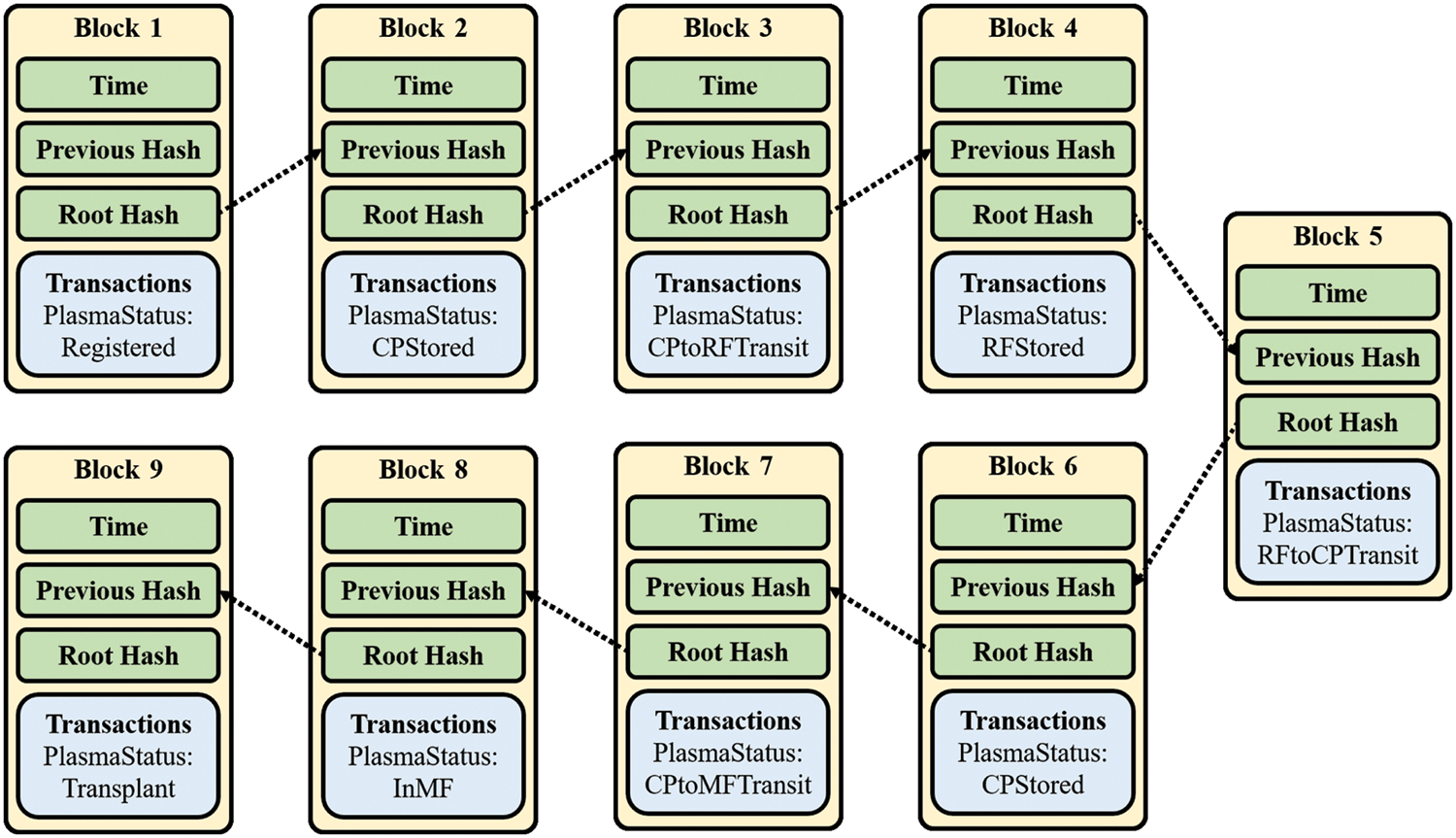
Figure 2: Chain of blocks generated
The network nodes would keep up with the blockchain by inserting empty blocks into it, which would not include any transaction information when there are no transactions. On the contrary, when blocks generate excessively often, it may lead to a scenario where several blocks are generated quickly, clogging the network and increasing the likelihood of block forks. One can resolve this problem by altering the block creation interval according to the current network load to preserve a stable state and prevent congestion. The proposed system is evaluated on below-listed four dimensions.
■ Latency of data initialization
■ Latency of database query
■ Latency of data update
■ Transaction throughput
For evaluation purposes, the number of queries (requests) varied between 1000 and 9000.
4.1 Latency of Data Initialization
The authors assess and analyze the latency associated with the data initialization to demonstrate the system’s efficacy. It displays the latency that occurs while registering plasma samples. The results observed corresponding to the latency of data initialization are presented in Fig. 3. Owing to congestion in queries; there may be a surge in processing times in several systems, delaying the handling of incoming transactions. However, the average and minimum processing time for requests is observed at an approximately constant level of 130.16 s/request and 0.64 s/request, respectively.
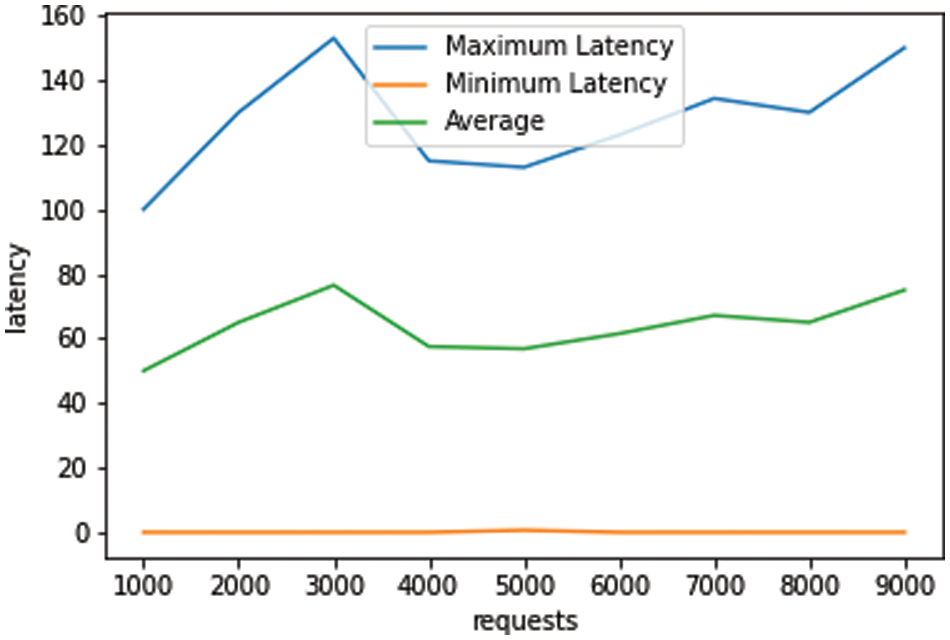
Figure 3: Results for latency observed corresponding to data initialization
The latency of the database query corresponds to the latency in the database searching when a search query is posted to search for a particular plasma sample among all that is preserved. The maximum latency index (of a database query) for the proposed model is observed to be varied between 1.0 and 1.4 s per request (as depicted in Fig. 4). Further, the average and minimum computation latency for requests is maintained at a constant level of 1.23 s/request, and 0.01–0.02 s/request, respectively. The maximum duration for the total request is recorded to be 1.45 s under a simulation where ten users simultaneously sent 2000 queries to the system.
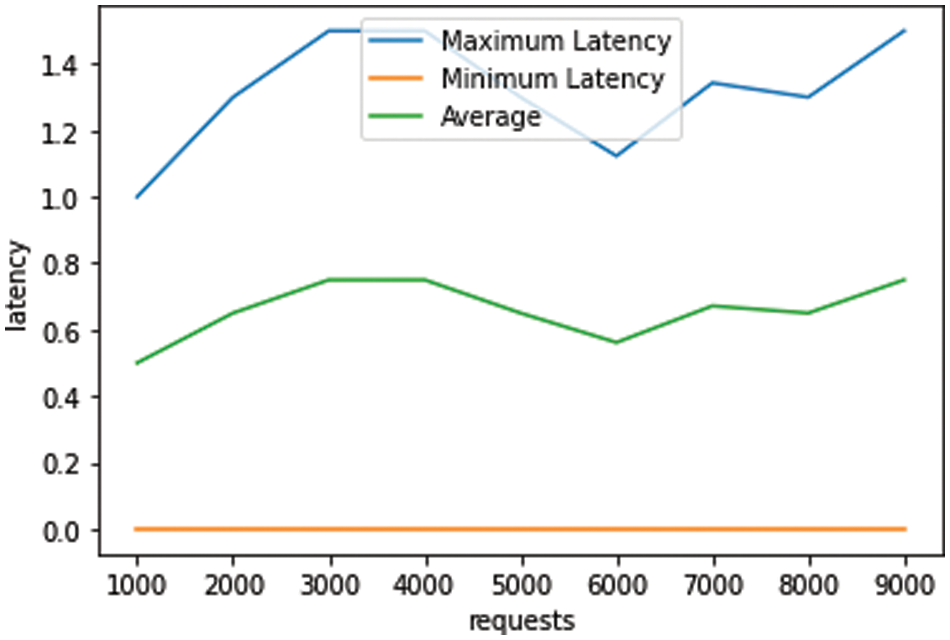
Figure 4: Results for latency observed corresponding to database query
This type of latency is recorded to observe the delay behavior of the proposed system while updating the plasma samples’ data. It has been observed (as presented in Fig. 5) that as the number of queries rises from 1000 to 9000, the latency of the requests remains constant. When the system begins searching the data and modifies the required attributes, the computation time is at its highest level compared to queries for initialization and searching data.
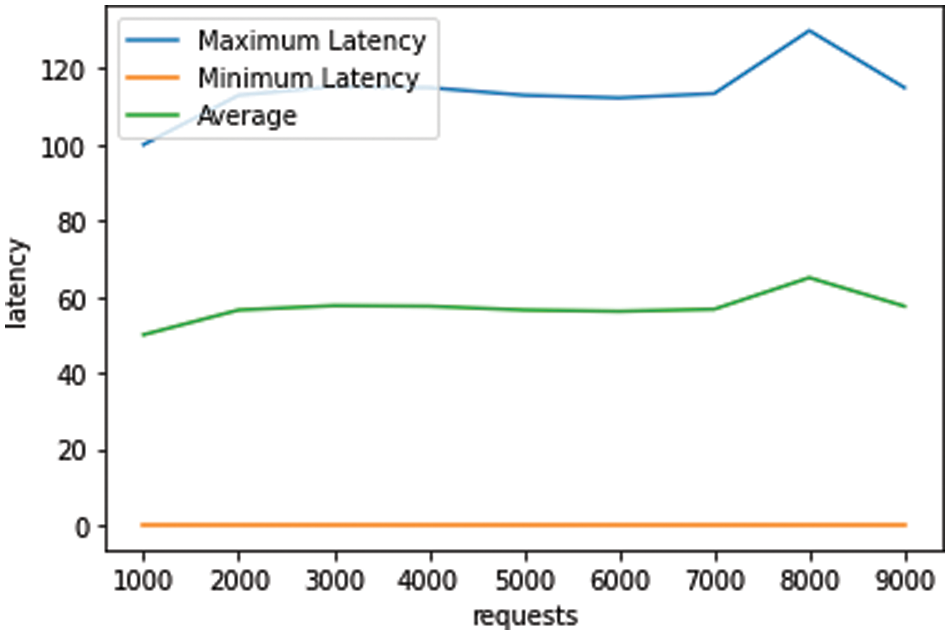
Figure 5: Results for latency observed corresponding to data update
The blockchain commits valid transactions to create a chain of blocks. The transaction change is denoted by the change in plasma status (i.e., Registered, CPStored, CPtoRFTransit, RFStored, RFtoCPTransit, CPStored, CPtoMFTransit, inMF, and Transplant). The transaction throughput is calculated as the number of committed transactions per second as presented in Eq. (1)
The observed throughput results for every type of plasma status is presented in Fig. 6. The average of all transaction throughput was discovered to be 132.8 transactions per second. It is evident that, on average, fewer RFtoCPTransit blocks are created than the rest of the blocks due to the high time complexity behavior of the PlasmaMatch() algorithm.

Figure 6: Results for transaction throughput achieved
Extensive testing will be necessary with more incoming requests and heavier loads. Since the system is based on Hyperledger Fabric, the plasma trails (transaction results) are recorded in Key-Value Store. The recommended technique ensures that provided blood is traced from the point of the donation until it is consumed. It also has a mechanism for keeping track of a donor’s suitability for donations based on their fitness, well-being, and timeframe since their previous contribution.
The method effectively confirms blood quality checks while transferring blood across regions to build trust. Blood is provided fairly and honestly, owing to the blood-matching system. The proposed system may be used as a peer-to-peer blood trial surveillance method to boost the effectiveness of blood usage and minimize malpractices.
We examined the computational efficiency of two well-known blockchain systems, Ethereum and Hyperledger Fabric, with identical experimental setups and data sets. The findings indicated that although Ethereum had a throughput of fewer than 15 transactions per second, Hyperledger Fabric had an average throughput of about 33 transactions per second. This shows that Hyperledger Fabric would be a superior option for situations like the blood plasma supply chain that demand high throughput and reduced latency.
Ethereum’s slow transaction computing power is a drawback when used in a decentralized plasma donation and transfusion system. Ethereum can perform about 15 transactions per second, which is insufficient for generating traffic for plasma donations and transplants quickly and effectively.
Contrarily, a Hyperledger-based system, like Hyperledger Fabric, can manage a lot more transactions every second; in fact, some studies claim that with the right setup, it can process up to 20,000 transactions every second. Because of the speedier transaction processing, calls for plasma donations and transplants may be handled more quickly and effectively, eventually benefiting patients.
Furthermore, the permission design of Hyperledger Fabric enables fine-grained governance over who has rights to and may edit data on the blockchain. This is crucial in a delicate and strictly regulated industry like plasma donation and transfusion, where confidentiality and data safety are major considerations. It is feasible to guarantee that all activities are auditable and identifiable and that only authorized parties have exposure to the pertinent data with a permission framework. Contrarily, it is harder to impose data privacy and security systems due to Ethereum’s permissionless design.
The existing management strategy of the plasma fractionation market needs to be more sustainable and challenging for all concerned stakeholders due to the constantly expanding global population and changing legislation controlling the healthcare system. This superfluous conversation would therefore be sped up by deploying a distributed ledger to efficiently convey the inventory and demand of blood plasma amongst various agencies. To achieve several objectives, including reliable plasma information visibility and guaranteeing the plasma quality for both recipients and donors, this paper intended, established, and analyzed a plasma supply chain network that manages a plasma donation system utilizing a private blockchain. When blood is donated, the accompanying plasma is removed, labeled, and logged in distributed ledgers, facilitating the effective governance of plasma. This is accomplished by the legitimate capturing and exchange of information. The other parties involved in the same transaction have access to the stakeholders’ information. Using relevant information, the suggested approach makes it simple for stakeholders to trace the origin of blood quality. A complete assessment of the proposed model is made to demonstrate the viability of the suggested system. However, to implement the blockchain network suggested by current research, the alignment of goals among plasma chain network entities, as well as architectural, political, administrative, and technological concerns, should be taken into account.
Funding Statement: The authors received no specific funding for this study.
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
References
1. T. Peltoniemi and J. Ihalainen, “Evaluating blockchain for the governance of the plasma derivatives supply chain: How distributed ledger technology can mitigate plasma supply chain risks,” Blockchain in Healthcare Today, vol. 2, pp. 1–13, 2019. [Google Scholar]
2. J. Prevot and S. Jolles, “Global immunoglobulin supply: Steaming towards the iceberg?” Current Opinion in Allergy and Clinical Immunology, vol. 20, no. 6, pp. 557, 2020. [Google Scholar] [PubMed]
3. J. Beliën and H. Forcé, “Supply chain management of blood products: A literature review,” European Journal of Operational Research, vol. 217, no. 1, pp. 1–16, 2012. [Google Scholar]
4. A. Farrugia, “Safety issues of plasma-derived products for treatment of inherited bleeding disorders,” Seminars in Thrombosis and Hemostasis, vol. 42, no. 5, pp. 583–588, 2016. [Google Scholar] [PubMed]
5. P. Tiberghien, “Increasing unpaid plasma collection by blood establishments to ensure availability of plasma–derived medicinal products and blood components in Europe,” Transfusion Clinique et Biologique, vol. 28, no. 4, pp. 331–333, 2021. [Google Scholar] [PubMed]
6. M. Pilkington, “Blockchain technology: Principles and applications,” in Research Handbook on Digital Transformations, Cheltenham, UK: Edward Elgar Publishing, pp. 225–253, 2016. [Google Scholar]
7. A. Ekblaw, A. Azaria, J. D. Halamka and A. Lippman, “A case study for blockchain in healthcare: “MedRec” prototype for electronic health records and medical research data,” in Proc. of IEEE Open & Big Data Conf., Vienna, Austria, pp. 13, 2016. [Google Scholar]
8. A. Azaria, A. Ekblaw, T. Vieira and A. M. Lippman, “Using blockchain for medical data access and permission management,” in 2nd Int. Conf. on Open and Big Data (OBD), Vienna, Austria, pp. 25–30, 2016. [Google Scholar]
9. Hulseapple, C. Block Verify Uses Blockchains to End Counterfeiting and ‘Make World More Honest, 2015. [Online]. Available: https://cointelegraph.com/news/block-verify-uses-blockchains-to-end-counterfeiting-and-make-world-more-honest. [Accessed 22 November 2022]. [Google Scholar]
10. E. A. Blackstone, J. P. Fuhr Jr and S. Pociask, “The health and economic effects of counterfeit drugs,” American Health & Drug Benefits, vol. 7, no. 4, pp. 216, 2016. [Google Scholar]
11. J. H. Tseng, Y. C. Liao, B. Chong and S. W. Liao, “Governance on the drug supply chain via gcoin blockchain,” International Journal of Environmental Research and Public Health, vol. 15, no. 6, pp. 1055, 2018. [Google Scholar] [PubMed]
12. Farmatrust. Fake Drugs: Real Problem, 2017. [Online]. Available: https://www.farmatrust.com/news/fake-drugs-real-problem/. [Accessed 23 May 2019]. [Google Scholar]
13. MedicoHealth. MedicoHealth, MedicoHealth Whitepaper, 2018. [Online]. Available: https://medicohealth.io/supporters/documents/wp_beta.pdf. [Accessed 15 April 2022]. [Google Scholar]
14. L. W. Dusseljee-Peute, R. Van der Togt, B. Jansen and M. W. Jaspers, “The value of radio frequency identification in quality management of the blood transfusion chain in an academic hospital setting,” JMIR Medical Informatics, vol. 7, no. 3, pp. e9510, 2019. [Google Scholar] [PubMed]
15. A. Jabbarzadeh, B. Fahimnia and S. Seuring, “Dynamic supply chain network design for the supply of blood in disasters: A robust model with real world application,” Transportation Research Part E: Logistics and Transportation Review, vol. 70, pp. 225–244, 2014. [Google Scholar]
16. R. Davis, B. Geiger, A. Gutierrez, J. Heaser and D. Veeramani, “Tracking blood products in blood centres using radio frequency identification: A comprehensive assessment,” Vox Sanguinis, vol. 97, no. 1, pp. 50–60, 2009. [Google Scholar] [PubMed]
17. E. J. Baek, H. O. Kim, S. Kim, Q. E. Park and D. J. Oh, “The trends for nationwide blood collection and the supply of blood in Korea during 2002∼2006,” the Korean Journal of Blood Transfusion, vol. 19, no. 2, pp. 83–90, 2008. [Google Scholar]
18. Hyperledger composer–Hyperledger foundation, 2021. [Online]. Available: https://www.hyperledger.org/use/composer. [Accessed 19 June 2022]. [Google Scholar]
19. Membership Service Providers (MSP)—hyperledger-fabricdocs master documentation, 2019. [Online]. Available: https://hyperledger-fabric.readthedocs.io/en/release-1.4/msp.html. [Accessed 19 June 2022]. [Google Scholar]
20. H. T. Le, T. T. L. Nguyen, T. A. Nguyen, X. S. Ha and N. Duong-Trung, “BloodChain: A blood donation network managed by blockchain technologies,” Network, vol. 2, no. 1, pp. 21–35, 2022. [Google Scholar]
21. S. Lakshminarayanan, P. N. Kumar and N. M. Dhanya, “Implementation of blockchain-based blood donation framework,” in Int. Conf. on Computational Intelligence in Data Science, Chennai, India, pp. 276–290, 2020. [Google Scholar]
22. A. A. Arsyad, I. W. Widayat and M. Köppen, “Supporting farming smart documentation system by modular blockchain solutions,” Decision Making: Applications in Management and Engineering, vol. 5, no. 1, pp. 1–26, 2022. [Google Scholar]
23. A. Raj and S. Prakash, “A Privacy-preserving authentic healthcare monitoring system using blockchain,” International Journal of Software Science and Computational Intelligence (IJSSCI), vol. 14, no. 1, pp. 1–23, 2022. [Google Scholar]
24. B. B. Gupta, K. C. Li, V. C. Leung, K. E. Psannis and S. Yamaguchi, “Blockchain-assisted secure fine-grained searchable encryption for a cloud-based healthcare cyber-physical system,” IEEE/CAA Journal of Automatica Sinica, vol. 8, no. 12, pp. 1877–1890, 2021. [Google Scholar]
25. J. Lu, J. Shen, P. Vijayakumar and B. B. Gupta, “Blockchain-based secure data storage protocol for sensors in the industrial internet of things,” IEEE Transactions on Industrial Informatics, vol. 18, no. 8, pp. 5422–5431, 2021. [Google Scholar]
26. S. Ding, J. Cao, C. Li, K. Fan and H. Li, “A novel attribute-based access control scheme using blockchain for IoT,” IEEE Access, vol. 7, pp. 38431–38441, 2019. [Google Scholar]
27. P. K. Sharma, M. Y. Chen and J. H. Park, “A software defined fog node based distributed blockchain cloud architecture for IoT,” IEEE Access, vol. 6, pp. 115–124, 2017. [Google Scholar]
28. B. Yuan, F. Wu and Z. Zheng, “Post quantum blockchain architecture for internet of things over NTRU lattice,” PLoS One, vol. 18, no. 2, pp. e0279429, 2023. [Google Scholar] [PubMed]
29. V. Sirelson and E. Brodheim, “A computer planning model for blood platelet production and distribution,” Computer Methods and Programs in Biomedicine, vol. 35, no. 4, pp. 279–291, 1991. [Google Scholar] [PubMed]
30. W. P. Pierskalla, “Supply chain management of blood banks,” in Operations Research and Health Care, vol. 70. Boston, MA: Springer, pp. 103–145, 2005. [Google Scholar]
31. J. C. Fratantoni, The Management and Logistics of Blood Banking: Conference Proceedings, Department of Health, Education, and Welfare, Public Health Service, National Institutes of Health, National Heart, Lung, and Blood Institute, Division of Blood Diseases and Resources, 1978. [Online]. Available: https://books.google.co.in/books/about/The_Management_and_Logistics_of_Blood_Ba.html?id=1efp53C1dbUC&redir_esc=y [Google Scholar]
32. Z. Vasickova, M. Penhaker and M. Darebnikova, “The functionality control of horizontal agitators for blood bags,” in XII Mediterranean Conf. on Medical and Biological Engineering and Computing 2010, Chalkidiki, Greece, pp. 859–862, 2010. [Google Scholar]
33. J. Hardwick, “Blood storage and transportation,” ISBT Science Series, vol. 3, no. 2, pp. 177–196, 2008. [Google Scholar]
34. A. Nagurney and A. H. Masoumi, “Supply chain network design of a sustainable blood banking system,” in Sustainable Supply Chains: Models, Methods, and Public Policy Implications, vol. 174. New York, NY: Springer, pp. 49–72, 2012. [Google Scholar]
35. S. Vallabhaneni, D. Boscovic and J. Kellso, Leveraging blockchain for plasma fractionation supply chains. 2020. [Online]. Available: https://keep.lib.asu.edu/items/131600 [Google Scholar]
36. H. H. S. Office for Civil Rights, “Standards for privacy of individually identifiable health information. Final rule,”Federal Register, vol. 67, no. 157, pp. 53181–53273, 2002. [Google Scholar]
Cite This Article
 Copyright © 2023 The Author(s). Published by Tech Science Press.
Copyright © 2023 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools