| Computers, Materials & Continua DOI:10.32604/cmc.2022.031879 |  |
| Article |
Bio-Inspired Modelling of Disease Through Delayed Strategies
1Baqai Medical University, Karachi, 75340, Pakistan
2Shalamar Medical and Dental College, Lahore, 54000, Pakistan
3Department of Mathematics, Cankaya University, Balgat, Ankara, 06530, Turkey
4Department of Medical Research, China Medical University, Taichung, 40402, Taiwan
5Institute of Space Sciences, Magurele-Bucharest, 077125, Romania
6Department of Mathematics, Govt. Maulana Zafar Ali Khan Graduate College Wazirabad, Punjab Higher Education Department (PHED), Lahore, 54000, Pakistan
7Department of Biochemistry, University of Sialkot, Sialkot, 51310, Pakistan
8Department of Mathematics and Statistics, The University of Lahore, Lahore, 54590, Pakistan
9Department of Mathematics, Faculty of Sciences, University of Central Punjab, Lahore, 54000, Pakistan
10Department of Mathematics, University of Gujrat, Gujrat, 52000, Pakistan
*Corresponding Author: Ali Raza. Email: alimustasamcheema@gmail.com
Received: 29 April 2022; Accepted: 07 June 2022
Abstract: In 2020, the reported cases were 0.12 million in the six regions to the official report of the World Health Organization (WHO). For most children infected with leprosy, 0.008629 million cases were detected under fifteen. The total infected ratio of the children population is approximately 4.4 million. Due to the COVID-19 pandemic, the awareness programs implementation has been disturbed. Leprosy disease still has a threat and puts people in danger. Nonlinear delayed modeling is critical in various allied sciences, including computational biology, computational chemistry, computational physics, and computational economics, to name a few. The time delay effect in treating leprosy delayed epidemic model is investigated. The whole population is divided into four groups: those who are susceptible, those who have been exposed, those who have been infected, and those who have been vaccinated. The local and global stability of well-known conclusions like the Routh Hurwitz criterion and the Lyapunov function has been proven. The parameters’ sensitivity is also examined. The analytical analysis is supported by computer results that are presented in a variety of ways. The proposed approach in this paper preserves equilibrium points and their stabilities, the existence and uniqueness of solutions, and the computational ease of implementation.
Keywords: Leprosy disease; delayed model; stability analysis; computer results
Leprosy is an infectious disease generated by a bacillus known as Mycobacterium leprae and lepromatosis. The morphology character of Mycobacterium leprae is an acid-fast, intracellular bacterium that is aerobic and rod-shaped. This long-term infection is also called Hansen’s disease. Tuberculiod, Lepromatous and Borderline is the types of leprosy. There is also some simple classification of leprosy disease, known as Multibacillary and Paucibacillary leprosy. It is mostly found in poverty where there is poor nutrition. This infection is mostly prevented in thronged areas and infects those whose immune system is weak enough to fight such disease. This murderous infectious harms an infected person’s nerves, respiratory, tract, skin, and eyes. As a result, nerve damage deprives the infected individual of the ability to feel pain, resulting in the loss of limbs owing to reoccurring traumas or infection from undiscovered wounds. Loss of eyesight and weakness of muscles is an aching part of this disease. Its symptoms may vary from person to person. Its first symptoms may occur within a year, and for others, it can take 20 years to exhibit any symptom. Primarily, this disease shows paler patches on the skin and sometimes nodules on the skin. It can be complex due to diagnosing it, and other times the patient remains misdiagnosed for years. The most common or usual symptoms of leprosy include a runny nose, muscle and eyesight weakness, dry scalp, skin lesions, loss of sensation in some body parts, especially fingers and toes, nasal cartilage destruction, and speech phonation and resonation of sound. These symptoms vary from person to person. The symptoms of this disease are categorized according to their stages. The incubation period is five years. The infected person may notice pale or pinkish skin patches that may lead to pain or sometimes temperature or insensitive. The next stage of leprosy can result in tissue loss, and it will affect fingers and toes to become insensitive to any pain. The immunological response of an individual varies according to the type of leprosy. Nerve damage is also a fatal symptom as it may cause loss of muscle function that may lead to paralysis and numbness. if treated early, this disease can be curable but become perpetual if delayed for months. Early discovery of the disease is significant, as it will present physical and neurological damage. The WHO recommends that those in close contact with someone who has leprosy receive preventive treatment. A single dosage of rifampicin (SDR) is suggested for adults and children who do not have leprosy or tuberculosis. This precaution treatment reduces infection up to 51% within 02 years and 30% within 06 years. The Bacillus Calmette-Guerin (BCG) is considered a great weapon against leprosy. According to WHO estimates, this vaccine (BCG) at birth reduces the cases of leprosy, and it should be recommended in countries that have repeated frequent leprosy cases. A 3–drug regimen of rifampicin, dapsone, and clofazimine is suggested to cure leprosy. On the other hand, multidrug therapy (MDT) has shown efficacy, and individuals are no longer infectious following the first monthly dose. According to the estimate of WHO in the year 2018, approximately 208. Six hundred nineteen cases were reported in different countries of the world. According to a report, in 2003, Pakistan had 20,000 leprosy cases, and its ratio decreased from 2009 to 2018. The leprosy rate is highly associated with India, the African region is considered the second most highly affected, and Brazil is third [1]. In 2004, Meima et al. investigated the effects of the current strategy to overcome leprosy, and the scenario presented that the following strategy will help reduce transmission. However, it may be slow in the process [2]. In 2004, Haanpa et al. discussed the possible dynamics, challenges in treatment, and needs in neuropathic pain, which required research work [3]. In 2006, Scollarod et al. explained the advanced research of Mycobacterium leparo [4]. In 2009, Bakker et al. discussed GIS to reduce the leprosy disease rate. GIS was a powerful tool in disease [5]. In 2010, Fischer et al. approached the comprehensive data of cluster leprosy within the household [6]. In 2012, Mushayabasa et al. presented the result of different strategies aiming to overcome leprosy disease by targeting infected and susceptible people [7]. In 2014, Barreto et al. discussed spatial analysis to explain the temporal pattern of leprosy disease in the Brazilian Amazon region. Through spatial analysis, the leprosy rate in early childhood gives a better understating [8]. In 2014, Lastoria et al. updated leprosy aspects like dermatologists on epidemiological etiopathogenic, and clinical [9]. In 2014, Martinez et al. evaluated PCR-based techniques for diagnosing leprosy disease [10]. In 2015, white et al. suggested some areas that play an important role for future research in leprosy disease and some challenges in which leprosy patients survive and the physician is facing in the treatment of Hansen’s disease [11]. In 2015, Blok et al. discussed that the eradication of leprosy is reached at the national level by 2020, but it remains in some specific regions [12]. Oli et al., 2017, investigated the dynamic of leprosy and its impact on the host population [13]. In 2018, Block et al. discussed the result of a diagnostic test to find the subclinical leprosy rate [14]. Le et al., in 2018, presented Southwest China the epidemiological characteristics of leprosy and presented the current situation of antigen-specific serum antibodies in humans who are suffering from leprosy and have different types of clinical [15]. In 2018, de Souza et al. examined the relationship link between the social degree of vulnerability and the intensity of leprosy [16]. In 2018, Mawardi et al. Leprosy morbidity reports played an important role in epidemiology because its result was authentic [17]. Using a mathematical model, Giraldo et al. described the involvement of multibacillary and paucibacillary leprosy. Some mathematical simulations are taken to analyze different stages of leprosy disease [18]. Lietman et al. estimated that the spread of leprosy in different areas of India was explained using geometric stability [19]. In 2018, Geluk et al. discussed strategies to identify leprosy reactions based on correlations that would be useful in leprosy [20]. In 2020, Gunawan et al. presented that testicular atrophy has many frequencies. The testicular function should be considered normal for leprosy patients [21]. Similar research on leprosy has been discussed in [22,23]. Numerical techniques with spatio temporal analysis of models are discussed [24,25]. In [26–36], researchers have recently focused on computer simulations of the epidemic model with various delay tactics. The following work studied the related models [37,38].
Delay models play a key role in real-life objects in the mathematical epidemiological field. Delay tactics are a control strategy near nature. As a result, we strive for a highly effective leprosy cure through delay tactics. Our scenario for the paper is as follows: Section 1 introduces leprosy as a model of delay. Section 2 discusses the leprosy model’s equilibria. Section 3 leprosy impairs model stability on a local and global scale. Section 4, to support theoretical analysis, some numerical results are discussed in the model and future discussions.
In this section, we have studied leprosy delayed epidemic model. At any time

Figure 1: Flow diagram of leprosy delayed epidemic model
The parameters of the leprosy delayed model are described as follows:
The initial conditions are as follows:
2.1 Positivity and Boundedness of Model
The delayed Leprosy epidemic model must maintain positivity and boundedness for practical analysis. All the state variables of the model
For this purpose, we will investigate the following results.
Theorem: The solutions (
Proof: It is clear from the system (1–4) as follows:
As desired.
Theorem [25]: The solutions (
Proof: Consider the function as follows:
We obtain this disparity as a result of Gronwall’s inequality.
This demonstrates that the solution to system (1–4) is constrained and falls within the feasible region
In this section, the equilibrium points of the model are presented as follows:
Leprosy trivial equilibrium (LTE-
Leprosy free equilibrium (LFE-
Leprosy existing equilibrium (LEE-
Where the values of
The reproduction rate of the leprosy delayed epidemic model is described in this section. It is an essential component of the model denoted by
where
By the next-generation matrix method, the largest eigenvalue represents the reproduction number given by
2.4 Sensitivity Analysis of Parameters
The parameters employed in the leprosy delayed epidemic model are critical to the disease’s dynamics. The effects of small changes in parameters change the entire dynamic. We have addressed the sensitivity analysis of the parameters in this part. For this, we proceed as follows:
From the above analysis, it can be seen that
This section discusses the local stability of leprosy delayed epidemic model at three equilibrium locations (LTE-
Theorem: Leprosy trivial equilibrium points, the system (1–4) is locally asymptotically stable at (LTE-
Proof: The Jacobian matrix
At leprosy trivial equilibrium (LTE-
Now,
Theorem: The system (1–4) is locally asymptotical stable at leprosy free equilibrium (LFE-
Proof: The Jacobian matrix calculated at leprosy free equilibrium point (LFE-
By computing
Where,
By evaluating the above determinant, we have the following polynomial
By Routh-Hurwitz Criterion for 3rd-degree polynomial, we have
Therefore, the leprosy existence equilibria (LEE-
Theorem: The system (1–4) is locally asymptotical stable at leprosy existence equilibrium (LEE-
Proof: The Jacobian matrix calculated at leprosy existence equilibrium point (LEE-
where,
Now evaluating
where,
By Routh-Hurwitz Criterion for 4th-degree polynomial, we have
Hence, the leprosy existence equilibria (LEE-
The global stability of the leprosy delayed epidemic model is examined using the following data.
Theorem: The system (1–4) is globally asymptotical stable at leprosy trivial equilibrium (LTE-
Proof: Define the Volterra Lyapunov function
Since,
Theorem: The system (1–4) is globally asymptotically stable at leprosy free equilibrium (LFE-
Proof: Consider the Volterra Lyapunov function
It can easily be observed that
Theorem: The system (1–4) is globally asymptotical stable at leprosy existence equilibrium (LEE-
Proof: Consider the Volterra Lyapunov function
As
So, (LEE-
The numerical treatment of the leprosy delay delayed epidemic model from the parameter value is presented. The parameter values and their data analysis is presented in Fig. 2.

Figure 2: Data analysis behavior of the disease
Example 1: (Without delay, simulation at leprosy-free equilibrium (PFE-P 1).
Fig. 3a through Fig. 3d illustrate the solution of the system (1–4) at the leprosy-free equilibrium (PFE

Figure 3: Plots of time for the system (1–4) at the model’s leprosy-free equilibrium
Example 2: (Simulation at leprosy existing equilibrium (LEE
Figs. 4a to 4d illustrate the solution of the system (1–4), at leprosy existing equilibrium (LEE

Figure 4: Plots of time for the system (1–4) at the model’s Leprosy existing equilibrium
Example 3: (Simulations at the state of leprosy with a temporal delay effect).
In this section, we have taken the effect of the system (1–4) at leprosy existing equilibrium of the model with effective use of artificial delay tactics. Figs. 5a to 5e, we can observe the susceptibility of humans increases with the help of delay tactics. On the other hand, we can keep the infectivity of leprosy patients decreasing and even converging to zero.

Figure 5: Time graphs of the system (1–4) in its leprosy-free state with successful employment of delay tactics
Example 6: (Effectiveness of delaying techniques on the model’s reproduction rate).
Let

Figure 6: Comparison graph showing the model’s reproduction rate and artificial delay duration
Example 5: (Replication of the delay term’s effect on the infectious class).
The varying values of

Figure 7: The influence of the delay term on the model’s infectious class is visualized
Example 6: 2 phase plots with delay effects.
Using artificial delay techniques, we plotted the model’s two-dimensional behavior. However, these simulations are based on the interaction between the model’s susceptible class and the rest of the model’s compartments. Figs. 8a–8c shows that the human immune system is dominant over the immune system of infected individuals, as intended.
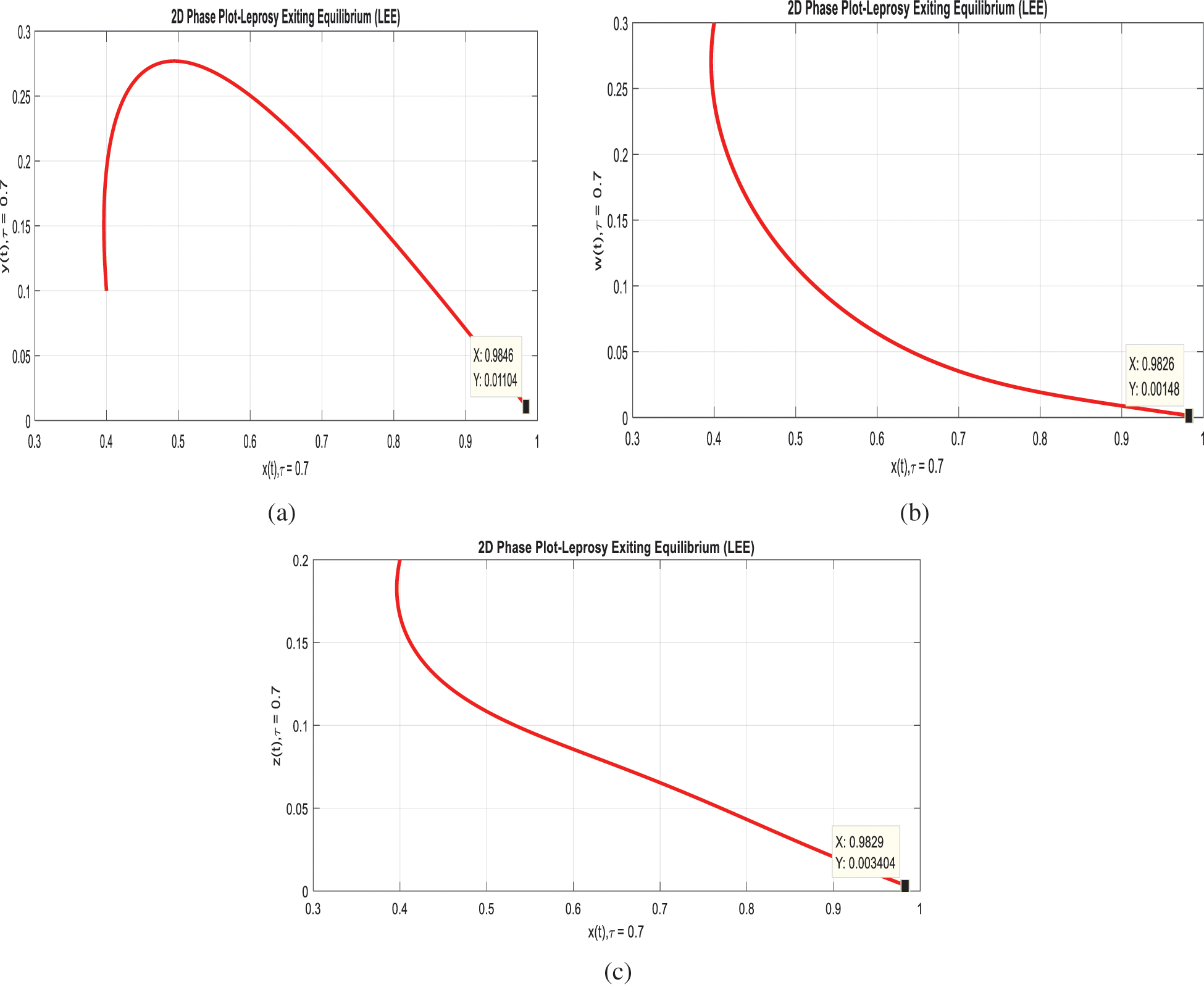
Figure 8: The system’s two-dimensional phases (1–4) with a delay effect
However, in delayed differential equations (DDEs), the past determines the system’s evolution at a specific time instant. The introduction of such time delays significantly increases the complexity of a differential model. Therefore, stability and bifurcation analysis of these models are essential for studying their qualitative behavior. These models haven’t been appropriately investigated for parameter identifiability or sensitivity analysis. The application of DDEs with state-dependent delays is a very recent topic in mathematics that might result in significant advances. This article examined the dynamics of leprosy disease through the successful use of delay techniques. As a group, we split the whole population into three groups:
• People who were susceptible to the virus.
• People are exposed to the virus.
• People who had been infected or had been vaccinated.
The reproduction number for the leprosy delayed epidemic model and sensitivity analysis on the reproduction number-related parameters are examined. Additionally, using well-known mathematical results, the demonstration of the model’s local and global stabilities at its equilibrium states, namely leprosy-free and leprosy-existing equilibrium. It is concluded that the desired research can control the dynamic of leprosy by positively using different effective delay techniques like treating infected people, keeping distance from the infected people, by immediate and annual examinations for a minimum of five years after the last meeting with an infected person.
Acknowledgement: Thanks to our families and colleagues who supported us morally. Also, The Govt. of Pakistan.
Funding Statement: The authors received no specific funding for this study.
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
References
1. A. Raza, J. Awrejcewicz, M. Rafiq, N. Ahmed, M. S. Ahsan et al., “Dynamical analysis and design of computational methods for nonlinear stochastic leprosy epidemic model,” Alexandria Engineering Journal, vol. 61, no. 10, pp. 8097–8111, 2022. [Google Scholar]
2. K. M. Owolabi and A. Atangana, “Mathematical analysis and computational experiments for an epidemic system with nonlocal and nonsingular derivatives,” Chaos, Solitons & Fractals, vol. 126, no. 1, pp. 41–49, 2019. [Google Scholar]
3. S. A. Plotkin, A. Lebrun and H. Koprowski, “Vaccination with the CHAT strain of type 1 attenuated leprosymyelitis virus in leopoldville, belgian congo. 2,” Studies of the Safety and Efficacy of Vaccination Bull World Health Organ, vol. 22, no. 1, pp. 215–234, 1960. [Google Scholar]
4. T. J. John and P. Jayabal, “Oral leprosy vaccination of children in the tropics-I. the poor seroconversion rates and the absence of viral interference,” American Journal of Epidemiology, vol. 96, no. 4, pp. 263–269, 1972. [Google Scholar]
5. D. M. Emperador, D. E. Velasquez, C. F. Estivariz, B. Lopman, B. Jiang et al., “Interference of monovalent, bivalent, and trivalent oral leprosyvirus vaccines on monovalent rotavirus vaccine immunogenicity in rural Bangladesh,” Clinical Infectious Diseases, vol. 62, no. 2, pp. 150–156, 2016. [Google Scholar]
6. R. Haque, C. Snider, Y. Liu, J. Z. Ma, L. Liu et al., “Oral leprosy vaccine response in breastfed infants with malnutrition and diarrhea,” Vaccine, vol. 32, no. 4, pp. 478–482, 2014. [Google Scholar]
7. M. Taniuchi, J. A. P. Mills, S. Begum, M. J. Uddin, S. U. Sobuz et al., “Impact of enterovirus and other enteric pathogens on oral leprosy and rotavirus vaccine performance in Bangladeshi infants,” Vaccine, vol. 34, no. 27, pp. 3068–3075, 2016. [Google Scholar]
8. K. Zhao, J. Jorba, J. Shaw, J. Iber, Q. Chen et al., “Are circulating type 2 vaccine-derived leprosyviruses (VDPVs) genetically distinguishable from immunodeficiency-associated VDPVs,” Computational and Structural Biotechnology Journal, vol. 15, no. 1, pp. 456–462, 2017. [Google Scholar]
9. M. T. Yeh, E. Bujaki, P. T. Dolan, M. Smith, R. Wahid et al., “Engineering the live-attenuated leprosy vaccine to prevent reversion to virulence,” Cell Host & Microbe, vol. 1, no. 1, pp. 01–18, 2020. [Google Scholar]
10. H. Manukyan, T. Zagorodnyaya, R. Ruttimann, Y. Manor, A. Bandyopadhyay et al., “Quantitative multiplex one-step RT-PCR assay for identification and quantitation of sabin strains of leprosyvirus in clinical and environmental specimens,” Journal of Virological Methods, vol. 259, no. 1, pp. 74–80, 2018. [Google Scholar]
11. M. Taniuchi, M. Famulare, K. Zaman, M. J. Uddin, A. M. U. Brown et al., “Community transmission of type 2 leprosyvirus after cessation of trivalent oral leprosy vaccine in Bangladesh: An open-label cluster-randomised trial and modelling study,” The Lancet Infectious Diseases, vol. 17, no. 10, pp. 1069–1079, 2017. [Google Scholar]
12. J. Suvisaari, J. Haukka, A. Tanskanen, T. Hovi and J. Lönnqvist, “Association between prenatal exposure to leprosyvirus infection and adult schizophrenia,” American Journal of Psychiatry, vol. 156, no. 7, pp. 1100–1102, 1999. [Google Scholar]
13. K. M. Thompson and D. A. Kalkowska, “Review of leprosyvirus modeling performed from 2000 to 2019 to support global leprosy eradication,” Expert Review of Vaccines, vol. 19, no. 7, pp. 661–686, 2020. [Google Scholar]
14. A. A. Hemedan, M. A. Elaziz, P. Jiao, A. H. Alavi, M. Bahgat et al., “Prediction of the vaccine-derived leprosyvirus outbreak incidence: A hybrid machine learning approach,” Scientific Reports, vol. 10, no. 1, pp. 01–12, 2020. [Google Scholar]
15. G. R. Macklin, K. M. Oreilly, N. C. Grassly, W. J. Edmunds, O. Mach et al., “Evolving epidemiology of leprosyvirus serotype 2 following withdrawal of the serotype 2 oral leprosyvirus vaccine,” Science, vol. 368, no. 6489, pp. 401–405, 2020. [Google Scholar]
16. R. J. D. Tebbens, L. M. Hampton, S. G. Wassilak, M. A. Pallansch, S. L. Cochi et al., “Maintenance and intensification of bivalent oral leprosyvirus vaccine use prior to its coordinated global cessation,” Journal of Vaccines & Vaccination, vol. 7, no. 5, pp. 01–16, 2016. [Google Scholar]
17. K. M. Thompson and R. J. D. Tebbens, “Current leprosy global eradication and control policy options: Perspectives from modeling and prerequisites for oral leprosyvirus vaccine cessation,” Expert Review of Vaccines, vol. 11, no. 4, pp. 449–459, 2012. [Google Scholar]
18. R. J. D. Tebbens and K. M. Thompson, “Leprosy endgame risks and the possibility of restarting the use of oral leprosyvirus vaccine,” Expert Review of Vaccines, vol. 17, no. 8, pp. 739–751, 2018. [Google Scholar]
19. M. Famulare, W. Wong, R. Haque, J. A. P. Mills, P. Saha et al., “Community structure mediates sabin 2 leprosy vaccine virus transmission,” MedRxiv, vol. 2, no. 1, pp. 01–20, 2020. [Google Scholar]
20. D. A. Kalkowska, M. A. Pallansch, A. Wilkinson, A. S. Bandyopadhyay, J. L. K. Anstadt et al., “Updated characterization of outbreak response strategies for 2019–2029: Impacts of using a novel type 2 oral leprosyvirus vaccine strain,” Risk Analysis, vol. 3, no. 1, pp. 01–25, 2020. [Google Scholar]
21. R. J. Duintjer Tebbens and K. M. Thompson, “Leprosyvirus vaccination during the endgame: Insights from integrated modeling,” Expert Review of Vaccines, vol. 16, no. 6, pp. 577–586, 2017. [Google Scholar]
22. R. D. Tebbens and K. M. Thompson, “Comprehensive screening for immunodeficiency-associated vaccine-derived leprosyvirus: An essential oral leprosyvirus vaccine cessation risk management strategy,” Epidemiology & Infection, vol. 145, no. 2, pp. 217–226, 2017. [Google Scholar]
23. N. C. Grassly, C. Fraser, J. Wenger, J. M. Deshpande, R. W. Sutter et al., “New strategies for the elimination of leprosy from India,” Science, vol. 314, no. 5802, pp. 1150–1153, 2006. [Google Scholar]
24. N. Ahmed, M. Rafiq, M. A. Rehman, M. S. Iqbal and M. Ali, “Numerical modelling of three dimensional brusselator reaction-diffusion system,” AIP Advances, vol. 9, no. 2, pp. 15205–15225, 2019. [Google Scholar]
25. N. Ahmed, T. Shaikh, M. Imran, M. Rafiq, M. A. Rehman et al., “Numerical analysis of auto-catalytic glycolysis model,” AIP Advances, vol. 9, no. 1, pp. 85213–85230, 2019. [Google Scholar]
26. M. Naveed, D. Baleanu, A. Raza, M. Rafiq and A. H. Soori, “Treatment of polio delayed epidemic model via computer simulations,” Computers, Materials & Continua, vol. 70, no. 2, pp. 3415–3431, 2022. [Google Scholar]
27. A. Raza, A. Ahmadian, M. Rafiq, S. Salashour, M. Naveed et al., “Modeling the effect of delay strategy on transmission dynamics of HIV/AIDS disease,” Advances in Difference Equations, vol. 663, no. 1, pp. 01–19, 2020. [Google Scholar]
28. A. Raza, A. Ahmadian, M. Rafiq, S. Salahshour and I. R. Laganà, “An analysis of a nonlinear susceptible-exposed-infected-quarantine-recovered pandemic model of a novel coronavirus with delay effect,” Results in Physics, vol. 21, no. 1, pp. 01–07, 2021. [Google Scholar]
29. W. Shatanawi, A. Raza, M. S. Arif, M. Rafiq, M. Bibi et al., “Essential features preserving dynamics of stochastic dengue model,” Computer Modeling in Engineering and Sciences, vol. 126, no. 1, pp. 201–215, 2021. [Google Scholar]
30. A. Raza, M. S. Arif, M. Rafiq, M. Bibi, M. Naveed et al., “Numerical treatment for stochastic computer virus model,” Computer Modeling in Engineering and Sciences, vol. 120, no. 2, pp. 445–465, 2019. [Google Scholar]
31. M. S. Arif, A. Raza, K. Abodayeh, M. Rafiq and A. Nazeer, “A numerical efficient technique for the solution of susceptible infected recovered epidemic model,” Computer Modeling in Engineering and Sciences, vol. 124, no. 2, pp. 477–491, 2020. [Google Scholar]
32. A. Raza “Mathematical modelling of rotavirus disease through efficient methods,” Computers, Materials and Continua, vol. 72, no. 3, pp. 4727–4740, 2022. [Google Scholar]
33. M. A. Noor, A. Raza, M. S. Arif, M. Rafiq, K. S. Nisar et al., “Non-standard computational analysis of the stochastic COVID-19 pandemic model: An application of computational biology,” Alexandria Engineering Journal, vol. 61, no. 1, pp. 619–630, 2021. [Google Scholar]
34. K. Abodayeh, A. Raza, M. S. Arif, M. Rafiq, M. Bibi et al., “Numerical analysis of stochastic vector-borne plant disease model,” Computers, Materials and Continua, vol. 63, no. 1, pp. 65–83, 2020. [Google Scholar]
35. A. Raza, M. Rafiq, J. Awrejcewicz, N. Ahmed and M. Mohsin, “Dynamical analysis of coronavirus disease with crowding effect and vaccination: A study of third strain,” Nonlinear Dynamics, vol. 107, no. 1, pp. 3963–3982, 2022. [Google Scholar]
36. A. Raza, J. Awrejcewicz, M. Rafiq and M. Mohsin, “Breakdown of a nonlinear stochastic nipah virus epidemic model through efficient numerical methods,” Entropy, vol. 23, no. 12, pp. 01–20, 2021. [Google Scholar]
37. K. Abodayeh, A. Raza, M. S. Arif, M. Rafiq, M. Bibi et al., “Stochastic numerical analysis for impact of heavy alcohol consumption on transmission dynamics of gonorrhoea epidemic,” Computers, Materials and Continua, vol. 62, no. 3, pp. 1125–1142, 2020. [Google Scholar]
38. A. Raza and M. Rafiq, “Modeling and transmission dynamics of leprosy disease via numerical methods,” Iranian Journal of Science and Technology, Transactions A: Science, vol. 46, no. 1, pp. 279–290, 2022. [Google Scholar]
 | This work is licensed under a Creative Commons Attribution 4.0 International License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. |