DOI:10.32604/cmc.2022.025049

| Computers, Materials & Continua DOI:10.32604/cmc.2022.025049 |  |
| Article |
Technologically Advanced Reusable 3D Face Shield for Health Workers Confronting COVID19
1Chitkara University Institute of Engineering and Technology, Chitkara University, 140401, Punjab, India
2Department of Computer Science, College of Computers and Information Technology, Taif University, Taif, 21944, Saudi Arabia
3Higher Polytechnic School, Universidad Europea del Atlántico, C/Isabel Torres 21, 39011, Santander, Spain
4Department of Project Management, Universidad Internacional Iberoamericana, Campeche, 24560, Mexico
5National Institute of Technology, Kurukshetra, 136119, Haryana, India
*Corresponding Author: Shikha Rani. Email: er.shikha2@gmail.com
Received: 09 November 2021; Accepted: 24 January 2022
Abstract: The probability of medical staff to get affected from COVID19 is much higher due to their working environment which is more exposed to infectious diseases. So, as a preventive measure the body temperature monitoring of medical staff at regular intervals is highly recommended. Infrared temperature sensing guns have proved its effectiveness and therefore such devices are used to monitor the body temperature. These devices are either used on hands or forehead. As a result, there are many issues in monitoring the temperature of frontline healthcare professionals. Firstly, these healthcare professionals keep wearing PPE (Personal Protective Equipment) kits during working hours and as a result it would be very difficult to monitor their body temperature. Secondly, these healthcare professionals also wear face shields and in such cases monitoring temperature by exposing forehead needs removal of face shield. Doing so after regular intervals is surely uncomfortable for healthcare professionals. To avoid such issues, this paper is disclosing a technologically advanced face shield equipped with sensors capable of monitoring body temperature instantly without the hassle of removing the face shield. This face shield is integrated with a built-in infrared temperature sensor. A total of 10 such face shields were printed and assembled within the university lab and then handed over to a group of ten members including faculty and students of nursing and health science department. This sequence was repeated four times and as a result 40 healthcare workers participated in the study. Thereafter, feedback analysis was conducted on questionnaire data and found a significant overall mean score of 4.59 out of 5 which indicates that the product is effective and worthy in every facet. Stress analysis is also performed in the simulated environment and found that the device can easily withstand the typically applied forces. The limitations of this product are difficulty in cleaning the product and comparatively high cost due to the deployment of electronic equipment.
Keywords: Temperature sensing face shield; electronic 3D face shield; IoT enabled face-shield
Healthcare professionals are more exposed to harmful infectious pathogens on a daily basis. This pathogenic nanoparticle is of about 120 nm (nanometer) and spreads abruptly. It is still unknown how persistent they are in the environment and the effective way to cure patients from them. This deadly disease spreads primarily through oral and nasal emission as these regions have very thin and penetrable membranes. Due to this fact the oral and nasal protection of paramedical staff is utmost essential. Moreover, additional preventive measures must be taken to protect medical staff from flying contaminants and particulates.
The human race has hugely damaged without any discrimination due to community transfer of this pandemic disease. This invisible enemy has not spared any of the country. The frontline health workers are playing a major role in saving communities to protect themselves from this deadly disease. Doctors and supporting healthcare professionals are working day and night tirelessly to protect people and to control the community transfer of this disease. Several educational and research institutes are in the process of discovery of vaccines to curb the pandemic. Due to pandemic spread, face shields are recommended as a safety measure. All face shields are not supposed to be effective. In fact, face shields must meet several requirements which are vital to protect people effectively. These face shields must be designed carefully to meet requirements like easy to wear, easy to remove, light weight, adequately cover the nasal and mouth area, must not obstruct the vision, support ample ventilation, avoid fogging and it should avoid accumulation of moisture.
Due to this pandemic, there have been many fears of shortages in protective equipment like masks, face shields and other medical devices. As a result, rapid manufacturing was required and 3D printed face shields came into existence [1]. In addition, the supply chain framework also confronted outrageous disturbance because of the regular and serious lockdowns across the globe. In such a circumstance, additive manufacturing turns into a supplementary manufacturing process to fulfill the touchy needs and to facilitate the wellbeing around the world. Additive manufacturing is also known as 3D printing or rapid prototyping. In contrast to conventional manufacturing processes, additive manufacturing fabricates objects by adding materials as required to obtain the desired shapes. In fact, precise geometric shapes can directly be printed from a computer-aided-design model. This technology offers a simplified way of fabricating complex objects with a lower manufacturing cost [2].
The body temperature monitoring of healthcare staff at regular intervals is vital as this preventive measure can serve as a first wall of defense and help avoid community transfer. Infrared temperature sensing guns have proved its effectiveness and therefore such devices are used to monitor the body temperature. These devices are either used on hands or forehead. As a result, there are many issues in monitoring temperature of frontline healthcare professionals at regular intervals. Firstly, these healthcare professionals keep wearing PPE kits during working hours and it would be very difficult to monitor their body temperature. Secondly, these healthcare professionals also wear face shields during working hours and in such cases monitoring temperature by exposing forehead needs removal of face shield. Doing so after regular intervals is surely uncomfortable for healthcare professionals. To avoid such issues, this paper is disclosing a technologically advanced face shield equipped with sensors capable of monitoring body temperature instantly without the hassle of removing the face shield.
The present state of art suggests that existing face shields are not rich in functionalities and suffer from lack of key features. Therefore, there is a need in the industry to provide technologically advanced face shields that can measure the user temperature instantly whenever required without removing the face shield. This research work is disclosing an in-house development of innovative face shield equipped with IoT enabled microcontroller and sensors for frontline health workers or paramedical staff.
The use of a face shield is a protective measure and has also proved its effectiveness. Even international organizations like WHO (World Health Organization) also recommended the use of face shields [3]. In fact, face shields can protect health workers by reducing inhalation exposure by 96% and surface contamination of a respirator by 97% instantly after a cough at a distance of 45.7 cm [4]. The past studies have also reported in the favor of face shields to protect from hazardous infections [4,5]. The radiologists also need protection from droplet transmissions and in one of the studies a face shield manufactured through 3D printing technique found effective to avoid this kind of transmission from coronavirus during the clinical trial [6]. Such 3D printed face shields have also been designed and manufactured for anesthesia providers as they have more risk due to close patient contact [7].
Likewise, an ergonomic and inexpensive 3D face shield made of PVC (Polyvinyl Chloride) having 0.3 mm (milimetre) thickness has also been offered as a preventive measure [8]. Special face shields have also been designed and manufactured for the patients undergoing endoscopy to reduce the aerosol contamination [9]. Indian Institute of Technology, Madras manufactured a face shield from 3D printers from generally accessible materials and provided the additional facility of replacing transparent sheets as and when required [10]. The researchers in [11] used 3D printing of face shields to protect oral and maxillofacial surgeons. This product was manufactured with Polylactic Acid Filaments (PLA) and could be reused after disinfecting with super Sani-Cloth-Germicidal-Disposable-Wipes.
A group of teachers and students form a team and named it Charlotte MEDI (Medical Emergency Device Innovation) at Charlotte Latin School to design and manufacture face shields to overcome the issue of shortage of face shields due to the pandemic. They started this novel work to provide basic lifesaving equipment like face shields to healthcare professionals. This team made an innovative design and used a 3D printing technique for rapid manufacturing. As a result, within a few days dozens of face shields were manufactured and handed over to medical staff at local hospitals. They delivered 15000 face shields per week using a community network of 3D printers and local manufacturing companies. They made this product from PETG (Polyethylene Terephthalate Glycol) and PLA filament [12]. In another research, locally fabricated face shield composed of PLA into general use in a rapid but well controlled manner was introduced [13]. Unlike other face shields, this product was designed to be reusable. The product reusability was ensured through standard disinfectants. Tab. 1 is disclosing comprehensive details of 3D printed face shields.

Few other small and large scale companies also utilized 3D printing techniques to fulfill the demands of face shields using different materials like premium PLA profilament [15], PETG, photopolymer resin medical grade nylon and ABS-42 filament (Acrylonitrile Butadiene Styrene) [2]. The related literature depicts that the majority of the innovations in the field of manufacturing face shields to protect healthcare workers were merely restricted to 3D printing and lacking in technology intervention.
This research work is offering a unique design and development procedure to develop a face shield capable of examining body temperature of doctors and paramedical staff without the hassle of removing gloves, PPE kit and face shield. The design, material and procedure are explained below.
While designing and choosing the material for this prototype the focus was on achieving enough flexibility without losing the strength. The CAD (Computer Aided Design) model was prepared and simulated under the normal loading conditions to meet the above said criteria. Thus, the study used PETG printed sheets with fill density of 25% and 38 MPa (Mega Pascal) tensile strength as this material has already been validated previously and has been found effective [16]. The tensile strength of 5.5 MPa was used for silicon (Latex-Free) to make the forehead strap. The length of the shield along the longitudinal direction of the nose of the subject was kept as 165 mm. The head length (distance from forehead to rear portion of head) of the subject was kept as 186.13 mm in normal un-stretched mode.
The head width (distance from left ear to right ear) of the subject was kept as 151 mm in normal un-stretched mode. These dimensions were chosen carefully after considering average anthropometric dimensions of the head size of an Indian adult. Anthropometric dimensions refer to human body part measurements which further assist to design the products. Tab. 2 summarizes the anthropometric dimensions [17]. Figs. 1 and 2 depicts the face-shield in different views where key components are labelled.

This face shield comprises three main modules specifically forehead strap which is also called forehead band, shield frame and a transparent shield. Fig. 3 exhibits various 3D components of the face shield.

Figure 1: Face shield (front view)

Figure 2: Face shield (rear view)

Figure 3: Key components of face shield
This IoT enabled face shield is technologically functional due to incorporation of infrared temperature sensor, mini speaker, display unit and microcontroller powered by a lithium polymer battery. The detailed configuration of these items is disclosed in the Tab. 3. The face shield assembly consists of three major components namely forehead strap, shield frame and a transparent shield. The material, volume and computed mass is disclosed in the Tab. 4. The tensile strength and density of the key components according to the material chosen is depicted in Fig. 4. Both transparent shield and shield frame were made of PETG material having tensile strength 38 MPa and density 1.38 ρ g/cm³ (gram per cubic centimetre) whereas the strap was made of silicon material having tensile strength of 5.5 MPa and density 1.2 ρ g/cm³.
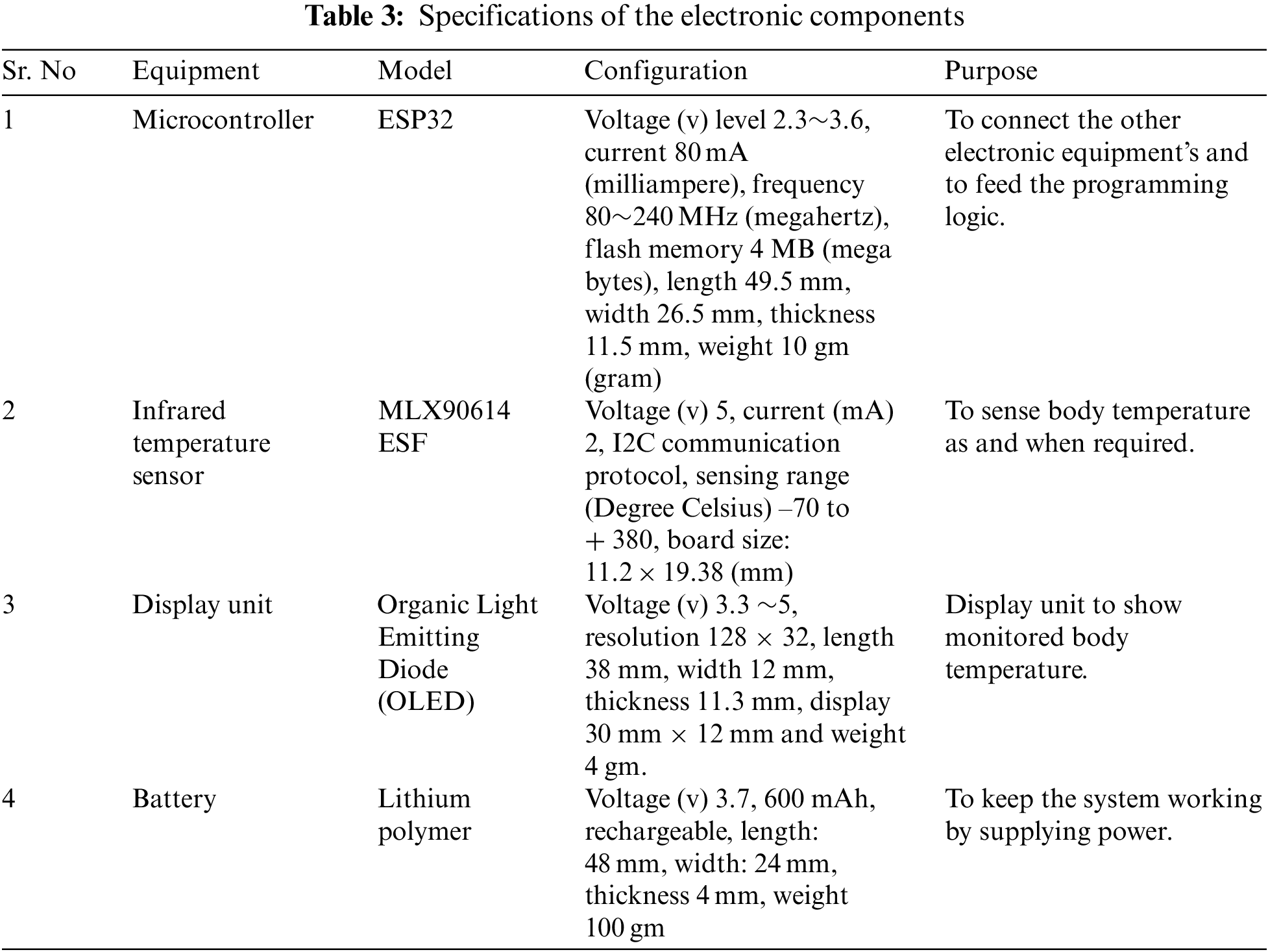


Figure 4: Face shield component material, tensile strength and density
The face shield components were printed using an in-house 3D printer. The printer has the capability of printing objects of 450 mm × 500 mm × 500 mm. It has a nozzle size of 0.4 mm and printing speed can be adjusted between 30 to 180 mm/s (millimeter per second). It also consists of an aluminium heat bed to provide the constant heat throughout the printing process. This face shield is capable of connecting with Wi-Fi because it is using an ESP32 microcontroller which has a built-in Wi-Fi board. As a result, it is capable of transmitting monitored body temperature remotely and can make a timestamp based log.
The prototype was developed in a few stages. Initially, the team reviewed the existing face shields and found that the technology was absent which needs to be incorporated [18,19]. Thereafter, technological ideas were generated and an idea to integrate an infrared sensor within the face shield was finalized. In the next stages, 3D design was made followed by 3D printing and fitting electronic components into it. Fig. 5 depicts all the stages in a chronological order.

Figure 5: Chronological order of prototype development stages
This face shield can be adjusted on any head easily as it is designed by considering anthropometric dimensions of Indian adults. It is equipped with an infrared sensor that will be activated only when the button is pressed. As soon as the button is pressed, the infrared sensor will instantly sense the body temperature and display it on the OLED screen and in parallel will also inform the wearer of face shield through audio description. This way, the wearer will get informed about his/her body temperature without removing the face shield and the person standing in front will also get informed through the OLED screen. As a result, it is serving two purposes i.e., monitoring body temperature instantly and protecting health workers by reducing inhalation exposure. Once fully charged, the system will last for approximately 5 h.
The temperature sensing process starts by pressing an activation switch placed at the right side of the face shield. Thereafter, the infrared sensor (MLX90614 ESF) monitors the body temperature and displays it immediately on the OLED screen mounted on the forehead of the face shield. The temperature sensing gun stops immediately after sensing the temperature and waits for the next input. The complete algorithm is shown below.

Initially, 10 face shields were designed and manufactured within the university lab and then handed over to a group of ten members including both teachers and students of the nursing and health science department. This arrangement was followed four times and as a result 40 healthcare workers contributed to the study. A short training was also given before distributing the face shields. The assembly and disassembly of the product was taught during the training. The participants were also educated to use Isopropyl alcohol to maintain the cleanliness of the face shield before reusing. After one week, a short questionnaire was shared with these participants to get the feedback of the product. A five point Likert scale was utilized (1 being the lowest and 5 being the highest) to measure the feedback responses. IBM SPSS tool was used to measure the feedback responses.
The cumulative mean score of 4.59 out of 5 signifies that the face shield is worthy in every aspect. Moreover, at present there is no other face shield which is equally technologically advanced. The participants only faced a few issues while cleaning the product. The Fig. 6 shows the mean scores and corresponding standard deviations in response to every question asked in the questionnaire. Seven questions were asked in the questionnaire which are disclosed in the Tab. 5.

Figure 6: Feedback responses

Due to the pandemic, the hospitals and healthcare workers faced shortage of medical equipment like face masks and face shields. As a result, the concept of additive manufacturing which is also known as rapid manufacturing came into existence. This research work made an effort to extend the idea of additive manufacturing through 3D printing technique by introducing technology by means of electronic sensors. This deadly disease spreads primarily through oral and nasal emissions; these regions have very thin and penetrable membranes. Due to this fact there is a high probability of healthcare staff getting affected from this disease. So, as a preventive measure the body temperature monitoring of medical staff at regular intervals is highly recommended. This preventive measure can help avoid community transfer through medical staff.
These days, infrared temperature sensing guns are used to monitor the temperature. This gun is either used on hands or forehead. As a result, there are many issues in monitoring the temperature of frontline healthcare professionals at regular intervals. Firstly, these healthcare professionals keep wearing gloves during working hours and it would be very uncomfortable for them to remove gloves at regular intervals to monitor body temperature. Secondly, these healthcare professionals also wear face shields during working hours and in such cases monitoring temperature by exposing forehead needs removal of face shield. Doing so after regular intervals is surely uncomfortable for healthcare professionals. To avoid such issues, this paper is disclosing a technologically advanced face shield which can monitor temperature instantly without removing it. The major challenge while designing this face-shield was to make a precise 3D design keeping in mind the dimensions of electronic equipment as they need to be placed inside it. Therefore, the team first collected the measurements of these electronic items before making the actual design. These measurements are disclosed in the Tab. 3.
Arduino programming language is used to interface electronic equipment. The most significant feature of this face shield design is inclusion of anthropometric dimensions of Indian male and female.
The feedback analysis was accomplished with the IBM SPSS tool. Fig. 6 exhibits the descriptive statistics of feedback responses. The feedback responses indicate that this product is worthy in every facet except one. The mean score of 3.93 in response to the question “How easy is it to clean and reuse this product?” shows that the participants faced little difficulty in cleaning the product as the cleaning process requires assembly and disassembly of a few key components of the face shield.
This seems a temporary issue as the feedback was taken only after one week. The long term usage and more training on cleaning the product may resolve this issue. The standard deviations and variances in responses to every question are depicted in the Fig. 7 to indicate the variability in the distribution and variability was found normal. This study also performed stress analysis of the forehead band only as this component has to be more resilient to any static stress deformation. The design has been simulated and tested for maximum deflection and induced stress. The simulation express module of 3D design application of Solidworks (Dassault Systems) has been utilized for the same. The deformation test has been carried out to obtain the results. It is assumed that in extreme conditions, a maximum of 3 Kgs of force acts on both sides of the forehead band. This force is equivalent to 29.43 Newton. The Eq. (1) is used for converting force in kilograms into newton units.

Figure 7: Variability of feedback responses
Considering mass as 3 kilograms and standard value of m/s2 as 9.81 the computed force in newton comes out to be 29.43. The total surface area of the forehead band is 10215.98 mm2 out of which the area considered under force is 1392 mm2. Thus, the force applied per unit was computed as below.
Force per unit area = (29.43/1392) N/mm2 = 0.0211 N/mm2 = 21100 N/m2
Tab. 6 shows mesh settings for stress analysis and simulation results are shown in the Fig. 8, where it can be clearly seen that there is no appearance of red zones in the figure hence indicating that the device can easily withstand the typically applied forces, in a very effective manner.
As per the Von Mises stress criteria, the maximum value of induced stress is


Figure 8: Simulation results for stress analysis
This innovative and technologically advanced face shield is unique as it is equipped with built-in sensors that can make doctors life safe and easy due to the facility of instant body temperature monitoring that too without the hassle of removing PPE kits, gloves or face shield. Monitoring doctors and other supporting staff body temperature is the first preventive measure to avoid community transfer of this deadly disease as an affected doctor may contribute to community transfer. The feedback analysis also found a significant cumulative mean score of 4.59 out of 5 which indicates that the product is effective and usable. The feedback analysis found that end users faced difficulty while cleaning the face shield and it is expected that this issue can be resolved through more intensive training sessions. Similar existing face shields are merely manufactured with different materials like PVC, PLA and PETG which are surely cheap but do not support instant body temperature monitoring. The face shield designed and developed in this research work is costly due to the involvement of electronic sensors but offers a highly safe environment. This face shield is armed with an IoT enabled microcontroller which in future may help in real time monitoring of body temperature. One possible use case of IoT enabled face shield is that it can be used to remotely monitor body temperature of health workers as well as patients.
Acknowledgement: This research was supported by Taif University Researchers Supporting Project number (TURSP-2020/347), Taif University, Taif, Saudi Arabia.
Funding Statement: This research was funded by Taif University Researchers Supporting Project Number (TURSP-2020/347), Taif University, Taif, Saudi Arabia.
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
1. R. C. Advincula, J. R. C. Dizon, Q. Chen, I. Niu and J. Chung, “Additive manufacturing for COVID-19: Devices, materials, prospects, and challenges,” MRS Communications, vol. 10, no. 3, pp. 413–427, 2020. [Google Scholar]
2. M. S. Tareq, T. Rahman, M. Hossain and P. Dorrington, “Additive manufacturing and the COVID-19 challenges: An in-depth study,” Journal of Manufacturing Systems, vol. 60, pp. 787–798, 2021. [Google Scholar]
3. T. M. Cook, “Personal protective equipment during the coronavirus disease (COVID) 2019 pandemic–A narrative review,” Anaesthesia, vol. 75, no. 7, pp. 920–927, 2020. [Google Scholar]
4. W. G. Lindsley, J. D. Noti, F. M. Blachere, J. V. Szalajda and D. H. Beezhold, “Efficacy of face shields against cough aerosol droplets from a cough simulator,” Journal of Occupational and Environmental Hygiene, vol. 11, no. 8, pp. 509–518, 2014. [Google Scholar]
5. S. Shoham, C. Acuna-Villaorduna, M. Cotton and M. Hardwick, “Comparison of protection against ocular contamination with disposable eyewear products,” 2020 Available at Wholesale Strengthen Porcelain Coffee Tea Ceramic Cup and Saucer (accessed on July 16, 2015). [Google Scholar]
6. M. Sapoval, A. L. Gaultier, C. D. Giudice, O. Pellerin, N. Kassis-Chikhani et al., “3D-printed face protective shield in interventional radiology: Evaluation of an immediate solution in the era of COVID-19 pandemic,” Diagnostic and Interventional Imaging, vol. 101, no. 6, pp. 413–415, 2020. [Google Scholar]
7. P. R. Armijo, N. W. Markin, S. Nguyen, D. H. Ho, T. S. Horseman et al., “3D printing of face shields to meet the immediate need for PPE in an anesthesiology department during the COVID-19 pandemic,” American Journal of Infection Control, vol. 49, no. 3, pp. 302–308, 2021. [Google Scholar]
8. V. Lemarteleur, V. Fouquet, S. Le Goff, L. Tapie, P. Morenton et al., “3D-printed protected face shields for health care workers in covid-19 pandemic,” American Journal of Infection Control, vol. 49, no. 3, pp. 389–391, 2021. [Google Scholar]
9. D. M. A. Martín, C. Corso, C. Fuentes, M. V. A. Aparicio and L. C. Sabbagh, “Use of a new face shield for patients of the endoscopy unit to avoid aerosol exchange in the COVID-19 era,” VideoGIE, vol. 5, no. 11, pp. 522, 2020. [Google Scholar]
10. P. Patel and P. Gohil, “Role of additive manufacturing in medical application COVID-19 scenario: India case study,” Journal of Manufacturing Systems, vol. 60, pp. 811–822, 2020. [Google Scholar]
11. D. Amin, N. Nguyen, S. M. Roser and S. Abramowicz, “3D printing of face shields during COVID-19 pandemic: A technical note,” Journal of Oral and Maxillofacial Surgery, vol. 78, no. 8, pp. 1275, 2020. [Google Scholar]
12. “Homepage–Charlotte MEDI.” https://www.charlottemedi.org/ (accessed Dec. 11, 2021). [Google Scholar]
13. A. Mostaghimi, M. J. Antonini, D. Plana, P. D. Anderson, B. Beller et al., “Regulatory and safety considerations in deploying a locally fabricated, reusable face shield in a hospital responding to the COVID-19 pandemic,” Med, vol. 1, no. 1, pp. 139–151, 2020. [Google Scholar]
14. A. Skamnelos, A. Murino, N. Lazaridis, L. Cunado and E. J. Despott, “Endoscopy during the COVID-19 pandemic: Simple construction of a single-use, disposable face shield using inexpensive and readily available materials,” VideoGIE, vol. 5, no. 9, pp. 399–401, 2020. [Google Scholar]
15. “What is PLA plastic material and how to use it for 3D printing.” https://www.sculpteo.com/en/materials/fdm-material/pla-material/ (accessed Dec. 11, 2021). [Google Scholar]
16. K. S. Kumar, R. Soundararajan, G. Shanthosh, P. Saravana kumar and M. Ratteesh, “Augmenting effect of infill density and annealing on mechanical properties of PETG and CFPETG composites fabricated by FDM,” Materials Today: Proceedings, vol. 45, pp. 2186–2191, 2021. [Google Scholar]
17. P. B. Shah, Y. Luximon, F. Fu and V. Makwana, “Anthropometric investigation of head measurements for Indian adults,” in Proc. of 9th Int. Conf. and Exhibition on 3D Body Scanning and Processing Technologies, Lugano, Switzerland, pp. 114–119, 2018. [Google Scholar]
18. J. Viera-Artiles and J. J. Valdiande, “3D-printable headlight face shield adapter. Personal protective equipment in the COVID-19 era,” American Journal of Otolaryngology, vol. 41, no. 5, pp. 102576, 2020. [Google Scholar]
19. C. Studders, I. Fraser, J. W. Giles and S. M. Willerth, “Evaluation of 3D-printer settings for producing personal protective equipment,” Journal of 3D Printing in Medicine, vol. 5, no. 3, pp. 133–144, 2021. [Google Scholar]
 | This work is licensed under a Creative Commons Attribution 4.0 International License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. |