DOI:10.32604/cmc.2021.015140

| Computers, Materials & Continua DOI:10.32604/cmc.2021.015140 |  |
| Article |
Prediction Models for COVID-19 Integrating Age Groups, Gender, and Underlying Conditions
1Department of Information and Communication Engineering, Yeungnam University, Gyeongsan-si, 38541, Korea
2Department of Computer Science, King Saud University, Riyadh, Saudi Arabia
3School of Intelligent Mechatronics Engineering, Sejong University, Korea
4Department of Computing and Mathematics, Manchester Metropolitan University, Manchester, United Kingdom
*Corresponding Author: Yousaf Bin Zikria. Email: yousafbinzikria@ynu.ac.kr
Received: 08 November 2020; Accepted: 19 December 2020
Abstract: The COVID-19 pandemic has caused hundreds of thousands of deaths, millions of infections worldwide, and the loss of trillions of dollars for many large economies. It poses a grave threat to the human population with an excessive number of patients constituting an unprecedented challenge with which health systems have to cope. Researchers from many domains have devised diverse approaches for the timely diagnosis of COVID-19 to facilitate medical responses. In the same vein, a wide variety of research studies have investigated underlying medical conditions for indicators suggesting the severity and mortality of, and role of age groups and gender on, the probability of COVID-19 infection. This study aimed to review, analyze, and critically appraise published works that report on various factors to explain their relationship with COVID-19. Such studies span a wide range, including descriptive analyses, ratio analyses, cohort, prospective and retrospective studies. Various studies that describe indicators to determine the probability of infection among the general population, as well as the risk factors associated with severe illness and mortality, are critically analyzed and these findings are discussed in detail. A comprehensive analysis was conducted on research studies that investigated the perceived differences in vulnerability of different age groups and genders to severe outcomes of COVID-19. Studies incorporating important demographic, health, and socioeconomic characteristics are highlighted to emphasize their importance. Predominantly, the lack of an appropriated dataset that contains demographic, personal health, and socioeconomic information implicates the efficacy and efficiency of the discussed methods. Results are overstated on the part of both exclusion of quarantined and patients with mild symptoms and inclusion of the data from hospitals where the majority of the cases are potentially ill.
Keywords: COVID-19; age & gender vulnerability for COVID-19; machine learning-based prognosis; COVID-19 vulnerability; psychological factors; prediction of COVID-19
The last two decades have witnessed several pandemics that challenged the capacity of our health system and destroyed the so-called claim of medical advancement. Pandemics such as severe acute respiratory syndrome (SARS), Ebola, Middle East respiratory syndrome (MERS) caused thousands of deaths and altered human living conditions and daily activities. The term “pandemic” refers to the outbreak of an infectious disease that endangers millions of lives distributed over large geographical areas while epidemics are restricted to a specific location, city, or country [1]. In December 2019, another severe disease, called coronavirus disease 2019 (COVID-19), emerged in Wuhan, Hubei Province, China, and began to spread rapidly. Within the next few weeks, it became a global outbreak and was declared a pandemic by the World Health Organization (WHO). COVID-19 is caused by SARS Coronavirus 2 (SARS-CoV-2) and attacks the respiratory system, leading to high mortality in critically ill patients and people with preexisting respiratory problems [2]. By the end of September 2020, 33.72 million people had been diagnosed with COVID-19, and worldwide 1.009 million were dead [3]. COVID-19 has caused the loss of trillions of dollars and widespread unemployment in many large economies. For example, the US had only 1% of the population receiving unemployment benefits before COVID-19 that increased to 18% by early May 2020 [4]. Besides financial upheaval and social tumult, COVID-19 is reshaping the working and living conditions and the patterns of our social interactions.
The medical community has responded promptly to COVID-19, and a broad range of techniques in multifarious domains such as medical prognosis, diagnosis, prevention, and treatment have been proposed. Such studies have helped diagnose COVID-19 patients readily and led to the clinical trials of many potential medicines for Ebola and SARS. The research community investigated many machine learning and deep learning models to help medical professionals diagnose COVID-19 patients to tackle the burden of the fast-paced spread of COVID-19. The research covers many aspects of COVID-19 patients such as clinical symptoms, the impact of age group on mortality, and the use of imaging technology to identify potential COVID-19 patients, and are broadly categorized into nine groups as shown in Fig. 1.
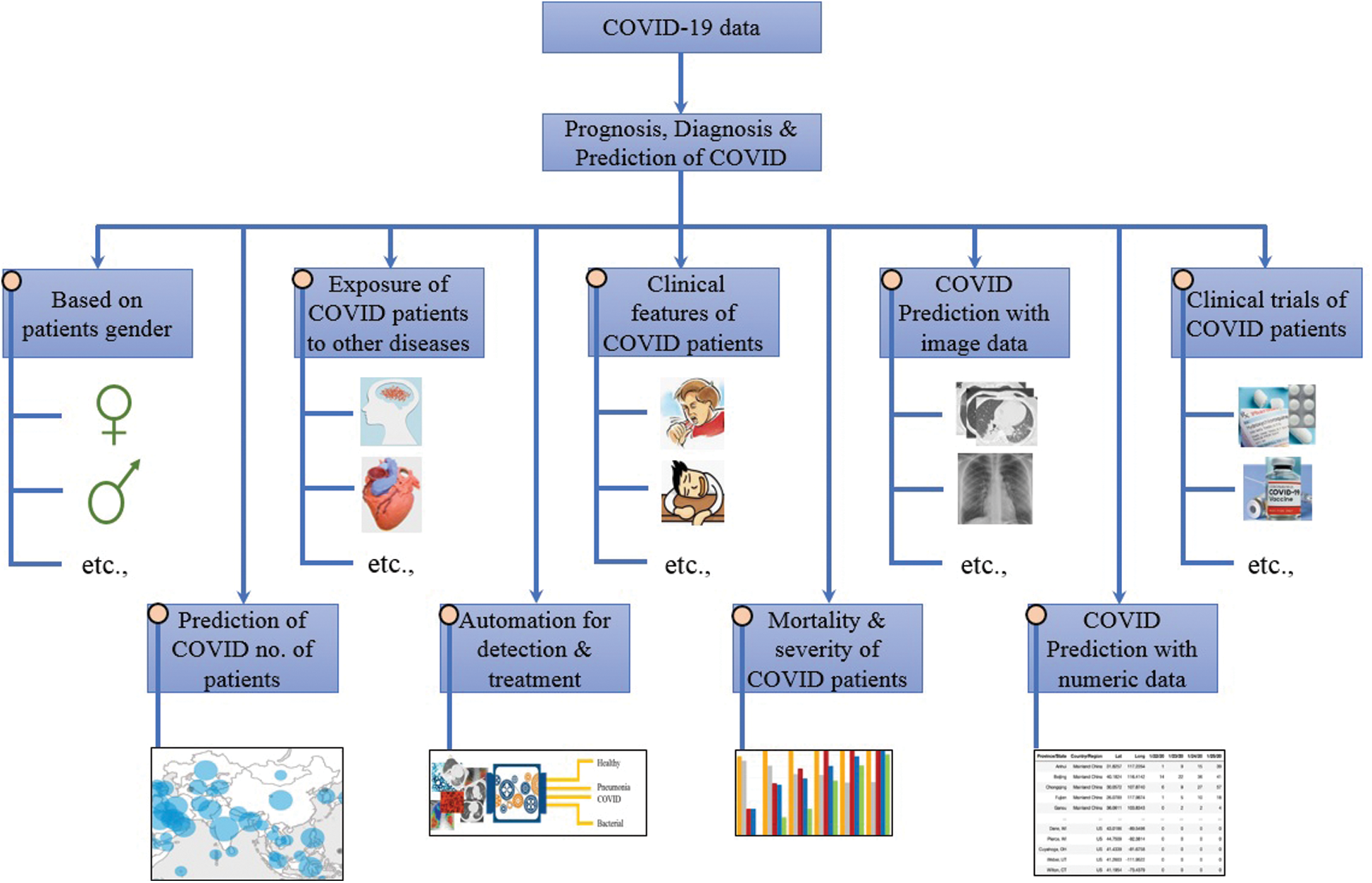
Figure 1: Classification of COVID-19 research works
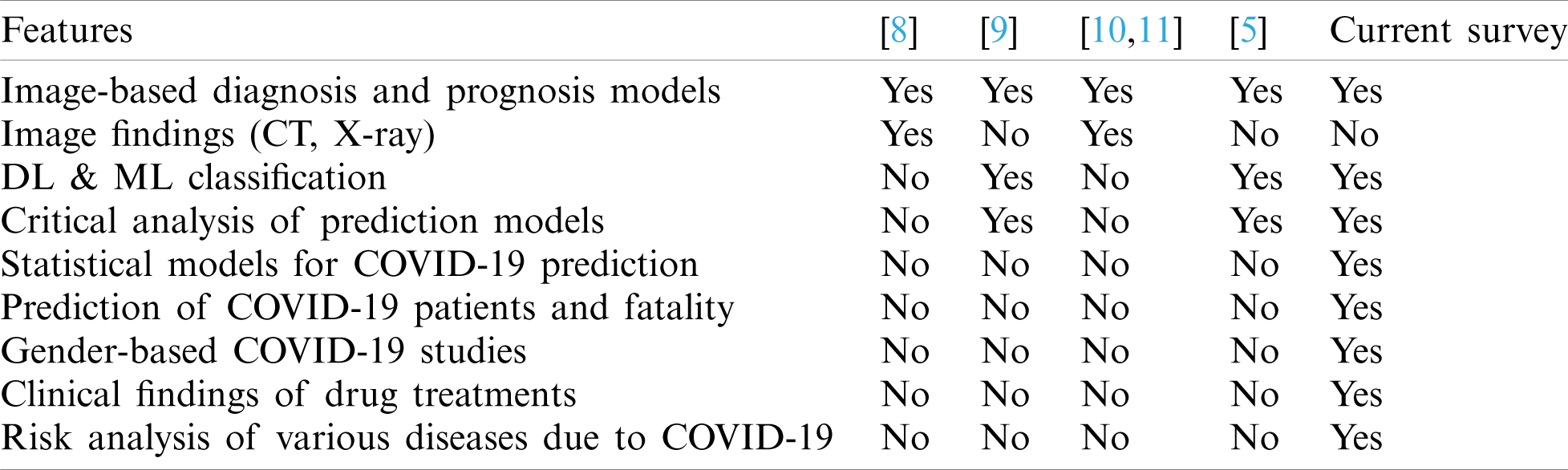
Several reviews of the research in the aforementioned categories have been available. For example, [5] provides an overview of the machine and deep learning approaches to the diagnosis of COVID-19. It critically analyzes artificial intelligence algorithms used for the prediction and diagnosis of COVID-19 patients. Nucleic acid testing and protein testing are laboratory tests for COVID-19 patients, and many kits have been designed for this purpose [6]. Such techniques require random-access, integrated devices with scalable capacities to facilitate the rapid diagnosis of COVID-19 patients [7]. Laboratory techniques require specialized equipment and are time-consuming. Conversely, computed tomography (CT), and X-ray (or radiography) images are utilized to assist and facilitate medical professionals for the initial and rapid prediction of COVID-19 patients. Consequently, prognostic and diagnostic studies are predominantly based on imaging techniques. Therefore, many review papers cover imaging-based machine and deep learning approaches presented to diagnose COVID-19 patients. For example, [8] presents an exploration of the role of imaging in detecting COVID-19 patients and discovering the symptoms of the disease from images. These characteristics are revealed using CT, X-ray, and ultrasound images of COVID-19 patients. Such characteristics/symptoms are discussed during different phases of the disease, that is, diagnosis, treatment and follow-up. Reference [9] presents a critical appraisal of various diagnostic and prognostic models presented for COVID-19. The models are discussed regarding the sample size, number of predictors, type of adopted validation, and risk of bias in each model. Similarly, [10,11] detail investigations of the approaches based on chest CT, X-ray, and ultrasound images and outlined the important findings identified by these approaches. The differential diagnosis of COVID-19 patients is also characterized, along with the complications of COVID-19. Despite the elaborate discussions in the above-cited works, the majority of the review papers focus mainly on the diagnostic models based on imaging technology. Thus, they neglect many important categories such as statistical models to predict the probable number of patients in a city or country, prediction of mortality or severity, and how gender is related to COVID-19 vulnerability? Tab. 1 shows a comparison of the topics covered by the research works discussed and highlights the contribution of the current study.
Table 1: Summary of the contributions of the current study
This study mainly focused on models that predict mortality or the severity of illness among COVID-19 patients, statistical models for COVID-19, and how gender groups are affected in the wake of the pandemic. Additionally, the impact of preexisting medical conditions, such as diabetes, hypertension, and heart disease, and the exposure of COVID-19 patients to other diseases are analyzed. Because many review papers have covered machine and deep learning research on imaging technology, this paper discusses only the most recent works in this regard. In summary, this study makes the following contributions:
• Contrary to previous studies that focused on studying diagnosis and prognosis models, the current study analyzed the models proposed to predict the number of patients in a locality, county, or country.
• Machine learning and deep learning approaches used to predict the severity of illness or probability of death are discussed and analyzed comprehensively.
• Studies that investigated the vulnerability to COVID-19 by gender are discussed along with the outcomes.
• Studies suggesting the risk of COVID-19 leading to various psychological and physiological disorders are given special consideration in the current study.
• The risk of death or complicated medical conditions associated with preexisting diseases, such as heart problems, diabetes, and hypertension, is discussed.
The rest of the paper is organized as follows. Section 2 discusses the models that predict the number of patients for various cities and countries. Extant studies concerning the exposure and vulnerability of COVID-19 patients to other diseases are discussed in Section 3. Section 4 describes research that analyzes the complications affecting COVID-19 patients with preexisting medical conditions. In contrast, Section 5 analyzes research that, by gender, highlights the impact of COVID-19 on patients. Research that emphasizes the mortality or severity prediction of COVID-19 is reviewed in Section 6. Future research directions are discussed in Section 7, and the conclusion is presented in Section 8.
2 Prediction Methodologies for Number of Patients of COVID-19
Owing to the rapid and widespread outbreak of the COVID-19, governments face difficulty in devising appropriate and prompt policies to adopt preventive measures. The derivation of models with the capability to predict the probable number of patients in a particular area provides advantages for planning appropriate policies to fight the disease. For this reason, researchers have modeled diverse algorithms that can predict high-risk areas and the number of people who are likely to be affected by the pandemic.
2.1 Machine and Deep Learning Models
A mathematical model is presented in [12] that can predict the number of patients in a specific country given the previous number of patients. The logistic model is modified to make it integrable and produce results with the measured data from different countries. The data from three countries—China, Austria, and France—are used to evaluate the performance of the proposed model. Various generalizations of the model have been proposed to deal with areas with various space distributions and low- and high-mortality cases. The model cannot incorporate important parameters such as quarantine and large distributions of COVID-19 patients. Similarly, it cannot be applied to each country. The data are used from Austria and China, where the infected population’s spatial distribution is most localized and does not apply to countries such as the United States and India where the cases are highly scattered in each state.
Accurate forecasting of the outbreak has significant importance in mitigating the impact of the disease as it enables the governments to plan beforehand. Reference [13] presents an analysis of the capability of various time-series models for outbreak prediction in various countries. Six models were tested, namely, autoregressive-integrated moving-average (ARIMA) model [14], Holt-Winters additive (HWA) model [15], trigonometric Box-Cox autoregressive-moving-average (ARMA) trend (TBAT) model [16], Facebook’s Prophet [17], DeepAR [18,19], and neural basis expansion analysis for interpretable time series (N-BEATS) [20]. The study revealed that a one-size-fits-all approach does not apply to COVID-19 case prediction. However, statistical methods such as ARMA and TBAT are superior to their counterpart deep learning approaches such as DeepAR and N-BEATS to predict patient numbers seven days ahead. The performance analysis is based on the root mean square error (RMSE) and Friedman’s test to rank the algorithms. Despite the significant performance superiority of TBAT over Prophet, DeepAR, and N-BEATS, the inter-country performance cannot be explained because of climatic, population, testing, disease duration, and other similar characteristics related to the spread prevention of COVID-19.
A hybrid machine learning approach was proposed in [21] to predict the number of COVID-19 patients in Hungary. The proposed model is based on an adaptive network-based fuzzy inference system (ANFIS) and a multilayered perceptron-imperialist competitive algorithm (MLP-ICA). The training was performed on the data acquired from 4 March to 19 April, while the testing was performed on the data acquired from 20 April to 28 April to predict the infected population and mortality rate. Three member functions, namely, triangular, trapezoidal, and Gaussian functions, are analyzed for their performance with ANFIS. Accuracy is established through the determination coefficient, mean absolute percentage error (MAPE), and RMSE. MLP-ICA is evaluated based on the number of neurons for the generation of empires. The results indicate that the machine learning models show superior performance compared to susceptible-infected-recovered (SIR)-based models to predict the infected patient numbers and mortality for COVID-19. However, the proposed approach is tested on Hungary’s data, and it is not clear whether it is adequate for different population densities and sizes.
A Gauss model was studied in [22] to predict the number of active cases and deaths per day for 25 countries. The quadratic function is found to be suitable for predicting fatalities for each country separately. The model can predict mortality per country, with additional aspects of the peak number of deaths per day, date of peak deaths, and the period during which the deaths occur. The adoption of the bell-shaped Gauss model demonstrates such models’ potential to predict COVID-19 cases; however, they may not be appropriate for all countries, as the results show large errors in the fitted curves. Asymptomatic patients also make it difficult to estimate the true case fatality ratio (CFR) for the COVID-19 pandemic. Reference [23] presents an investigation of a crude CFR model to predict COVID-19 cases and fatalities in Korea using the Monte Carlo Markov-Chain method with the Bayesian framework. It reports that the CFR for Korea is higher than that of China. Early CFR values were low, indicating a delay in reporting confirmed cases or increasing ascertainment bias. In the initial phase of an epidemic, the true CFR is underestimated in current and previous studies.
Reference [24] presents a deterministic and stochastic modeling approach to predict Kuwait’s confirmed COVID-19 cases. Owing to the unavailability of a detailed dataset, which is necessary for ABMs (agent-based models), the SIR approach is followed. The SIR approach and logistic regression are adopted to predict the epidemic size and its probable ending phase. Changes in the susceptible patients numbers are modeled using the individual contact model (ICM) model with various reproduction number values. Reference [25] presents the use of a logistic model to predict the number of infected people in India. For this purpose, the logistic-growth curve model is used for active cases, while SIR models are used for the maximum number of active cases and peak time. Additionally, the impact of lockdown and other similar restrictions is taken into account for the time interrupted regression (TIR) model. The predictions follow the patterns for short-term cases. However, to predict long-term cases and incorporate additional government interventions, the approach needs to be remodeled. An exploratory time-series analysis was adopted in [26] for predicting COVID-19 cases in Greece. A regression spline model was adopted to analyze the evolution of COVID-19 cases by first determining the spline knot vector using a complex-network-based approach. The results demonstrate that the complex-network spline demonstrates superior performance compared to the cubic and regression models. The approach was tested on Greece’s data only and may require remodeling or parameter tuning for other countries. Other parameters, such as isolation, quarantine, and social distancing, are not incorporated in this study.
Incorporating the government’s interventions in a prediction model may potentially make it highly useful for accurate predictions. For example, [27] considered intervention measures to analyze the evolution of COVID-19 in European countries. The data from Spain, Italy, UK, Germany, and France were used to fit the model for predicting infections and the infections-to-deaths rates. Analysis confirms other studies’ findings that government restrictions, including social distancing, quarantine, and isolation, can potentially slow down the spread of infection. However, the model using the probability distributions based on the historical data of infections to the probability distributions based on the historical data of China’s infection-to-death ratios. Changing such data for other countries will change the probability distributions and output of the model. Additionally, the R value in the regression model varies over time and takes different values for each country. The R value was assumed to be constant in this study.
2.2 Susceptible-Infected-Recovered Models
A SIR model was used in [28] to fit the data related to COVID-19 patients for New Jersey (NJ) and New York (NY) states in the US. The presented model was a classical SIR model with a non-autonomous approach in which the rate of susceptible people and deaths are adjusted to fit the available data. The following two assumptions were made to the model for data fitting: many infected people are not tested positive, and lockdown policies reduce the transmission and infection rates. The model predicts disease waves in NY followed by NJ and the exponential increase, peak, and decrease of the pandemic. A different approach was adopted in [29], wherein the empirical data from South Korea and Italy were used to forecast long-run cases in Utah State, USA. A log-logistic model was used to align the start of the pandemic in Utah. The model involves the following four parameters: The initial infected population size (c), final infected population size (d), inflection point of the logistic curve (e), and scaling factor (b) representing the slope parameter. The model indicated a pandemic level similar to that of South Korea. The model can make short-run predictions with fair accuracy, while the long-run forecast is neither robust nor accurate
COVID-19 cases were predicted for Pakistan using a model called the exponential inverse exponential exponential (EMIEE), which is based on the exponential M (EM) family of continuous distributions [30]. Model parameters were estimated using the maximum likelihood method. The proposed model is used to estimate the number of infected people in Pakistan and peak time, and to compare the number of cases with other countries. Performance analysis with other models showed promising results. Two models were adopted in [31] to realize a real-time prediction of the COVID-19 outbreak for Saudi Arabia based on empirical data from 2 March to 15 May 2020. The logistic-growth and SIR models were used to predict the number of infected people across the country. The modeling timescale was assumed to be short with no vital dynamics, and a constant host population size was considered for the SIR model. The infection was predicted concerning the peak, transition, and decrease phases. The logistic model showed better performance than the SIR model. Similarly, a SIR model was leveraged to predict the COVID-19 peak duration in Malaysia [32]. Initially, a genetic algorithm was used to estimate the infection rate, and the adaptive neuro-fuzzy inference system model provided an estimate of short-term infected cases. The impact of government constraints was also considered to delay the peak time of the epidemic. Additionally, the prediction showed that intervention can reduce the infection rate, and longer intervention periods would reduce the epidemic’s scale during the peak.
The epidemic peak for COVID-19 was predicted for Japan by [33] using the susceptible-exposed-infectious-removed (SEIR) compartmental model. The reproduction number was estimated with the help of the lease-square-based method with Poisson noise. The impact of government intervention was assumed to slow down the infection rate. The peak was predicted to be in July. Research indicates that interventions over a longer period positively reduce the scale of the final epidemic. Additionally, the epidemic size would be less likely to be impacted by the actual infective population. The number of patients was predicted in [34] using a rolling gray Verhulst model. Six models were used on 7, 8, and 9-day data for predicting confirmed cases of COVID-19. The MAPE was used to evaluate the performances of the models during the training phase. Only the data from 20 January to 20 February 2020, for COVID patients from China, were used for the models; therefore, the results cannot be generalized. Many important parameters, such as imposed restrictions, lockdown, and environmental conditions, were not considered.
Reference [35] presents the use of a multiple ensemble neural network model with fuzzy response aggregation to predict COVID-19 cases in Mexico. Multiple neural networks were trained for prediction, and the final output was generated using fuzzy logic, which considers uncertainty. Short-term data were used for prediction with an increasing trend, making it simple but unsuitable for data with multiple trends. Similarly, a deep learning approach was used in [36] to predict the trend of COVID-19. Various long short-term memory (LSTM) adaptations such as vanilla, stacked, multilayer, and bidirectional LSTM were analyzed for their efficacy in predicting the number of infected people. Correlation analysis was also performed considering factors such as temperature, rainfall, sunshine, population, infected cases, death, and population density. The study concluded that COVID-19 has no dependence on the weather, such as sunshine, temperature, precipitation, while social distancing is vital to reduce the spread.
2.3 Use of Social Media Search Index
Contrary to traditional methods that utilize empirical time-series data for prediction, [37] predicted suspected cases from the social media search indexes (SMSIs) for various symptoms of COVID-19, such as dry cough, fever, chest distress, and pneumonia. Lagged series were used to predict suspected cases. Subset selection, forward selection, lasso regression, ridge regression, and elastic net are used as coefficients to avoid overfitting. The study demonstrated the significance of using SMSI data by indicating that suspected cases can be detected 6–9 days earlier. While using SMSI, the correlation with suspected case numbers differs for each day considered, showing that although SMSI can sense an outbreak, it is not a tool to predict confirmed COVID-19 cases conclusively. Reference [38] presents a space and time correlation approach to predict the community outbreak for COVID-19 in the USA. Proxy datasets were generated from publicly available news articles. Then, spatial analysis can provide insights into space–time patterns of COVID-19. The analysis findings indicate the need for strict social distancing during the disease’s initial spread to slow down its impact.
2.4 Critical Analysis of Methods
The use of forecasting models to predict the number of COVID-19 infected people can be grouped into the following three categories: Machine learning models, SIR models, and deep learning models. Machine learning models include both classical machine learning algorithms and other models such as logistic, correlation, and Verhulst models. Although a subset of machine learning, deep learning models are categorized according to their operational processes, such as feature extraction, parameter tuning, and processing capabilities.
SIR models are epidemiological algorithms used to predict the number of infections based on suspected, infected, and recovered patients’ empirical data. A challenge to devising a model for long-term prediction is the lack of essential data to analyze its performance. Additionally, the uncertainty in data restricts the higher accuracy of epidemiological models. Machine learning models show promising results in the research works discussed when experimented on with limited data. The data are limited in terms of locality or time. Most studies analyze the models’ performance on data from a single country and a limited time. The limitation of such models is that each would perform differently because of the underlying assumptions. Similarly, differences in population density, environmental conditions, health system capacity, government control over the people to enforce interventions, and socioeconomic conditions would affect a model’s results. Deep learning models are data-intensive and can behave differently because of the data provided for training. Additionally, the prediction and analysis using deep learning-based models are conducted under simple or ideal conditions and do not consider the complex scenarios with a large number of variables that pertain in real conditions. This can adversely affect the prediction of such models. In addition, deep learning models require large amounts of data to support parametrization. Lack of sufficient data may significantly vary the prediction results. In addition, such models require extensive hyperparameter tuning related to the number of hidden layers used in a model that increase their complexity. Currently, there is uncertainty about the transparency of various governments in reporting the actual number of COVID-19 patients. It would be possible to miss a significant number of confirmed cases that may influence a given model’s accuracy. One advantage of a model is the distribution of the number of infected cases given a similar feature set, such as population, climate, health system, and sanitary conditions, which are missing in the proposed models.
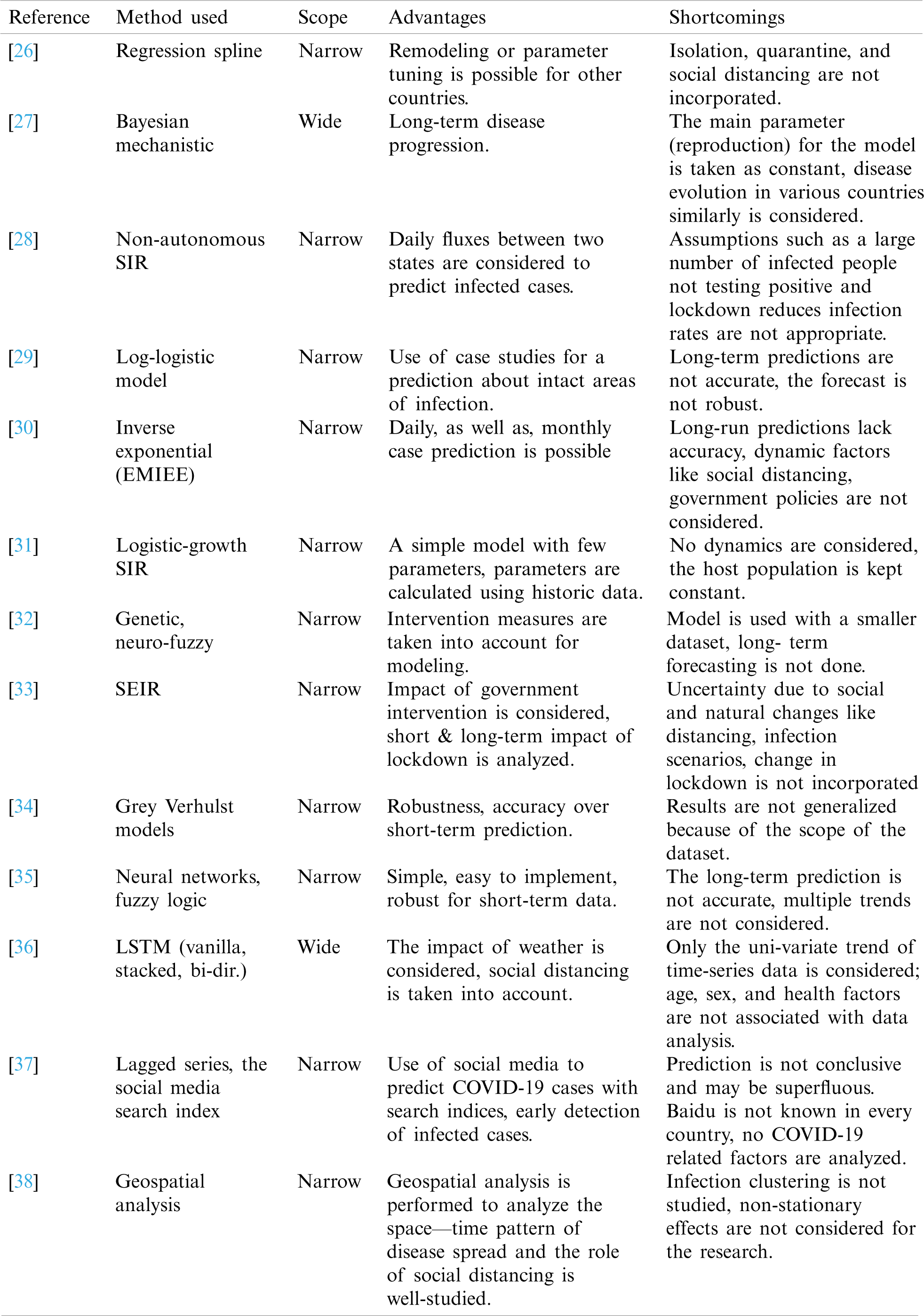
Tab. 2 presents a summary of the methods used to predict the number of patients with COVID-19. Three types of models are used to predict the total number of COVID-19 patients for various cities, countries, and continents, namely, machine learning models, SIR models, and deep learning models. A major challenge for prediction with such models is the availability of a suitable dataset that carries the patients’ geographical, medical, and personal details. Many issues related to data uncertainty, such as incomplete records, an increased or decreased number of patients reported, and nature of symptoms (symptomatic/asymptomatic), restrict the utilization of a model’s full potential. For example, without the aforementioned data, the SIR model cannot perform a long-run prediction. Although machine and deep learning approaches show promising results for accurate predictions, in the same vein, their performance is not generalized. Owing to the uncertainty in data used for training and testing, the performance of such models may vary significantly. The data is often limited by time and space, and changes in the data may cause very different results. Typically, many important factors are not considered, such as environmental conditions, population density, health and medical conditions of a society, government interruptions, and socioeconomic conditions, which have a direct or indirect impact on the spread of the pandemic. The lack of transparency of various governments in reporting the number of infected people is also an issue in estimating the number of infections with adequate accuracy.
Table 2: Summary and critique of the research that predicts the number of COVID-19 patients
3 Exposure of COVID-19 Patients to Other Diseases
Viral infections, such as those by rhinovirus, respiratory syncytial virus, influenza virus, human parainfluenza virus, and metapneumovirus, are regarded as triggers for many other diseases [39–41]. In light of such findings, it would be highly appropriate to investigate the impact of the COVID-19 virus in exposing infected people to other diseases. Consequently, numerous studies that analyze COVID-19 patients for its impact, both positive and negative, on the vulnerability/resistance of the patients to other diseases.
The authors performed a Mann–Whitney U and chi-square test in [42] to study the impact of COVID-19 on asthma in a population of 376 confirmed patients. In contrast, the effect of medications used to treat asthma was analyzed in COVID-19 patients. The study indicated that asthma prevalence in patients with COVID-19 is low and not associated with asthma exacerbation. It was also suggested, as did other studies [43,44], that inhaled corticosteroids with or without bronchodilators can inhibit coronavirus replication.
Possible cardiac complications were studied in [45] using magnetic resonance imaging (MRI) images from 26 recovered COVID-19 patients who reported cardiac symptoms. Tests were performed using various models such as Shapiro–Wilk, Student’s t-test, analysis of variance (ANOVA), Mann–Whitney U test, and Kruskal–Wallis test. Various symptoms were found in recovered patients, such as abnormal MRI in 58% of patients, myocardial edema in 54%, and late gadolinium enhancement (LGE) in 31% of patients. Cardiac involvement was found in many of the examined patients with MRI manifestations involving myocardial edema, fibrosis, and impaired right ventricular (RV) function. Another study [46] investigated the correlation between cardiovascular disease (CVD) and COVID-19 and suggested that the patients have a prevalence of CVD. This prevalence is significantly higher in critically ill patients than in those with relatively mild disease.
Information on mental health problems in adults resulting from the COVID-19 pandemic was examined using a survey [47]. Studies indicate that the pandemic’s perceived negative impact has a significant effect on mental health problems, including sleeplessness, depression, and post-traumatic symptoms in the general population. Cognitive and prosocial coping behaviors can help relieve such problems; therefore, cognitive-behavioral treatments should be engineered. The authors performed a study to examine COVID-19 related stress among people in Iran [48]. The survey contains 54 items about demographic characteristics, past medical history, stress levels, and awareness of COVID-19 symptoms. The mean age of the 3787 participants was 34.9 years, 66.6% were without chronic disease, and 67.4% were female. The stress score was weighted between 1 and 5, from very low to very high, and the average stress score among the participants was 3.33. A higher stress score is associated with females aged between 30 and 39 years with chronic disease.
A structured questionnaire was used in [49] to assess the mental health of people in Hong Kong. The questionnaire was completed by 500 randomly recruited participants. The questionnaire contained structured questions about health, anxiety disorder level, rating of change scale, and COVID-19 related items. Multiple logistic regression indicated that 19% and 14% of the participants had high depression and anxiety, respectively, while an additional 25.4% faced mental health deterioration. Poor mental health problems are caused by the fear of getting infected with COVID-19, unavailability of enough masks, and inability to work from home.
3.4 Sleep Disorder, Hypertension, Stress, and Psychological Problems
In [50], the authors included stress, physical activity, alcohol intake, and cigarette smoking in addition to depression, anxiety, and sleep in an online survey conducted for Australians. The survey results, completed by 1491 adults, show that COVID-19 affected people’s lives negatively by 48.9% for physical activity, 40.7% for a sleep disorder, 26.6% for alcohol use, and 6.9% for smoking. Such negative changes are highly associated with females and single people with low incomes aged between and 18–45 years.
Similarly, the reference [51] presents a study on COVID-19 related psychological responses of health workers and physicians. The online survey covered three aspects, namely, sociodemographic (age, gender, marital status, etc.), working conditions, and the Depression Anxiety and Stress scale (DAS)-21. The analysis was performed using Student’s t-test, ANOVA test, and multiple linear regression analyses on the data collected from 442 participants. Depression, anxiety, and stress were found in 64.7%, 51.6%, and 41.2% of participants, respectively. A high score is associated with being female, young, single, having low work experience, or being a frontline worker, while this score is relatively low for workers having children. A higher score in DAS-21 is caused by increased working hours, a higher number of COVID-19 patients, lower-level peer support, lower logistic support, and feelings of lower competence.
In a similar study [52], the authors analyzed the impact of lockdown on mental health and sleep disturbance in Italy. The questionnaire contained sociodemographic characteristics, people behaviors and healthcare, and patient health questionnaire-2 and generalized anxiety disorder-2. Sleep disorder was analyzed using the insomnia severity index with a population size of 1515. Group differences were defined using the chi-square and Mann–Whitney U tests. Univariable and multivariable logistic regression was used to determine the influence of individual variables. Results showed that 24.7% and 23.2% of the participants had depression and anxiety, while 42.2% faced sleep disturbances, of which 17.4% experienced insomnia.
The authors studied the factors associated with suicide in India during COVID-19 in [53]. The data were collected using a web search for suicide news in Indian and international English newspapers, which resulted in 34 completed suicides during the period from January 25 to April 18, 2020. The majority of the victims (52.94%) were young adults between 18 and 36 years old. The reasons associated with suicide are fear of infection, misinterpretation of fever as COVID-19, depression, loneliness, and perceived stigma of COVID-19 infection.
Reference [54] presents a study on human behavior and habits in Austria, Switzerland, and Germany during COVID-19 lockdown. A total of 435 tests were obtained by individuals of high socioeconomic status and high educational level to assess the quality and quantity of sleep, the mid-sleep difference between working and free days, and life satisfaction. Advanced non-parametric analysis revealed that the mismatch between social and biological sleep—wake timing was reduced during the lockdown resulting from accomplishing more work from home. Sleep quality was reduced by 0.25 points (0–25 scale); the subjective burden increased accordingly while mental and physical wellbeing decreased. Sleep quality reduction was associated with social sleep reduction and working hours.
Reference [55] reports on the analysis of psychological states. The data were collected using an online survey containing questions related to sociodemographic conditions, contact with COVID-19, and emergency conditions due to COVID-19. The results indicate that psychopathological symptoms such as anxiety, mood alternations, and PTSD symptoms were found in 31.38%, 37.19%, and 27.72% of the participants, respectively. The causative factors include being female under 50 years of age, having direct contact with COVID-19 infected patients, and uncertainty about the risk of COVID-19.
Factors associated with coronavirus anxiety were studied in [56] using an online survey in Germany. A total of 1615 participants (79.8% female and 19.8% male) completed the questionnaire between March 15 and 22, 2020 for trait health anxiety, cyberchondria severity scale, emotion regulation, and questions about the COVID-19 pandemic. The repeated ANOVA (rANOVA), Spearman’s correlation coefficients, and rANCOVA (repeated measures analyses of covariance) were used for analyses. The results indicated significantly high anxiety due to COVID-19 in individuals with heightened trait health anxiety. Cyberchondria indicated a correlation with anxiety, while adaptive emotion regulation serves as a moderator to reduce anxiety.
Reference [57] investigated the impact of COVID-19 on sleep disturbance and suicidal thoughts using a Facebook survey in Taiwan. Several COVID-related factors were collected from the participants, including anxiety level, social interaction patterns, study-related interference, social support to combat the disease, and physical health. The majority of the participants (55.8%) reported sleep disturbance, while a smaller portion (10.8%) admitted suicidal ideation. Factors such as increased worry, changes in social interaction, impaired social support, severe academic interruption, and poor physical health care are responsible for sleep distress problems. In addition, suicidal thoughts are associated with less handwashing, lower social support, lower COVID-19 related support, poor physical health, and youthfulness.
Health factors related to psychological distress during COVID-19 in Spain were studied in [58]. Bivariate analysis, chi-squared test, and Student’s t-test were used on the data collected from 4180 people containing general health questionnaire-12. Psychological disorders were found in 72% of the participants, with a higher percentage in women and lower middle-aged people. The younger population lacks the resilience to face adversity and is more exposed to distress. Similarly, people living with children experience high distress and psychological vulnerability. In addition, the mental health of Chinese children and adolescents was analyzed in [59] during the COVID-19 outbreak. The questionnaire contained a Spence Child Anxiety Scale, Child Depression Inventory, and Coping Style Scale, and 359 children and 3254 adolescents completed the questionnaire online. Analysis indicated that 22.28% of the participants suffered from depression symptoms. Anxiety was associated with being female, resident in urban regions, and an emotion-focused coping style. Depression was linked with smartphone addiction, internet addiction, and residents in Hubei province. Reference [60] presents a study that analyzed COVID-19 patients’ data for anxiety and depression. Among the 1642 respondents in the survey, 23.1% experienced moderate-severe anxiety, while 41% faced mild anxiety. Moderate depression was found in 48%, while 9.2% faced moderate-severe depression. Students and the unemployed experienced higher anxiety than non-students and the employed, respectively. Similarly, those with a preexisting psychiatric history faced higher anxiety and depression.
The factors associated with sleep disorders include stress, less physical activity, alcohol intake, cigarette smoking, age, marital status, depression, coronavirus anxiety, mood alterations, and female sex.
3.5 Evaluation of the Discussed Methods
Numerous research studies have investigated the physical and psychological damage caused by COVID-19 in general population as well as health workers and physicians. The results indicate asthma, heart disease, suicidal ideation, and sleep irregularities. Predominantly, most of these studies relate to mental health problems such as sleep disorders, stress, anxiety, and depression. Sleep and anxiety disorders are most commonly reported among those surveyed. However, the percentage of victims varies by country and study because of the use of various analysis techniques. Stress analysis and mental health problems were studied using surveys that omitted many considerations. For example, these studies cover a single community, city, or country and are limited because of regional differences, including demographic and socioeconomic conditions, awareness, education level, and health system. Therefore, a survey designed for a specific country may not be suitable for other countries with different prevailing conditions. Questions answered in surveys unintentionally may be biased or incorrectly answered because of a lack of knowledge or understanding. Surveys involving children and adolescents are limited by the possibility that the results and conclusions were influenced by participants who required assistance from their guardians and the degree of understanding of the questions. In addition, the questions added in the surveys and questionnaires were selected concerning their quantitative importance for statistical analysis and restricted the participants from expressing their subjective views. In several studies, the sample size was too small for the results to be generalized. Similarly, changing the analysis technique might produce different results on the same data.
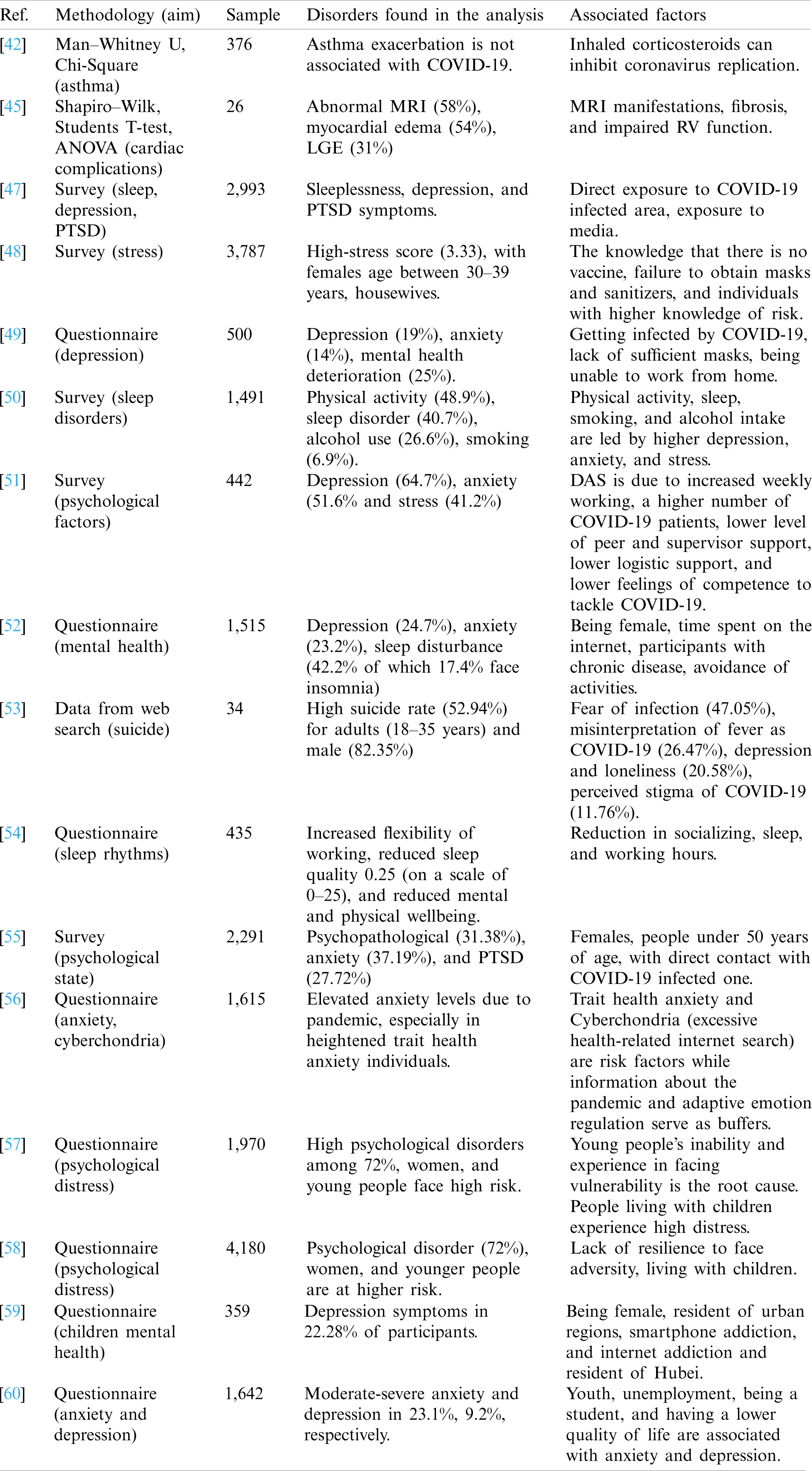
Tab. 3 provides a summary of the research works investigating the resulting problems from COVID-19. Several previous studies suggest that viral infections are associated with a high risk of exposure to other diseases such as anxiety, heart disease, lung disease, and mental disorders [39–41]. Subsequently, many studies have focused on analyzing the impact of COVID-19 on physical and mental health in infected areas. The findings of these studies suggest that asthma, cardiac complications, and several mental health problems such as stress, anxiety, depression, sleep disorder, and suicidal thoughts, are prevalent in people facing COVID-19, lockdown, and other social interaction restrictions. Predominantly, such studies investigate mental health problems such as sleep irregularities, anxiety, and depression, using surveys and questionnaires that are lacking in several aspects. For the most part, these studies are designed for a single community, city, or country. They do not apply to other countries owing to differences in demographics, socioeconomic status, education, and health conditions. Moreover, the participants were hired to complete surveys and questionnaires, and answers may be biased, incorrectly answered owing to a lack of understanding, or by intention. Similarly, surveys requiring children’s response may not be transparent because of guardian or parental influence, apart from the degree of a child’s understanding. Additionally, the surveys and questionnaires were selected because of their quantitative importance for statistical analysis, and participants’ subjective views were not recorded. Similarly, the sample size for such surveys is too small for their results to be generalized.
Table 3: Summary of works studying the exposure of COVID-19 patients to other diseases
4 Impact of Various Diseases on COVID-19 Infection Level
Several observational and retrospective studies that analyze the impact of viral infection suggest the prevalence of various underlying conditions such as asthma, diabetes, and heart disease and confirm severe outcomes and complicated medical conditions [40,61]. As a result, it is highly desirable to investigate the role of preexisting medical conditions in the severity and fatality of COVID-19 patients. Multitudinous works that focus on analyzing the impact of underlying medical conditions on the outcome of COVID-19 patients can be found in the literature.
The impact of high cholesterol on the infectivity of COVID-19 was analyzed in [62]. Analyses revealed that COVID-19 patients with CVD, hypertension, and obesity seem to have severe clinical conditions. Similarly, the authors in [63] suggested that patients with CVD disease are highly prone to COVID-19 infection, especially with CVD originating from atherosclerosis. Another research work [64] investigated the connection between COVID-19 and cholesterol metabolism. Analysis indicated that triglycerides (TGs) and high-density lipoprotein cholesterol (HDL-C) levels were lower in patients with severe COVID-19 illness. Along the same lines, research [65] states that lower free cholesterol (FC), high-density lipoprotein (HDL), and low-density lipoprotein (LDL) are associated with COVID-19 patients than those those not infected.
A summary of the health records of 72,314 COVID-19 patients from China was analyzed in [66]. It has been reported that the fatality rate is higher for COVID-19 infected cases with preexisting medical conditions such as CVD, diabetes, and respiratory disease. Patients with CVD are at higher risk, with a fatality rate of 10.5%, followed by diabetes, chronic respiratory disease, hypertension, and cancer with a fatality rate of 7.3%, 6.3%, and 5.6%, respectively. Similarly, the authors investigated 187 patients with COVID-19 [67] for the impact of underlying CVD and myocardial injury on the fatal outcome. Analyses indicate that the fatality rate is higher (13.33%) for COVID-19 patients with CVD than for those without CVD (7.62%). CVD is associated with fatal outcomes in COVID-19 patients; however, myocardial injury has a significant association with fatality compared to CVD without myocardial injury.
Other studies [68,69] suggest that patients with a high prevalence of CVD are more severely ill when infected with COVID-19 than those with mild CVD disease. Similarly, non-surviving COVID-19 patients had critical CVD compared to survivors at the hospital in China during the start of the outbreak [70]. Two similar studies [71,72] that investigated clinical features in COVID-19 patients with the data of 150 and 191 COVID-19 admitted patients indicate that the fatality rate is high for patients with coronary heart disease. Similarly, Italian COVID-19 patients’ data show that three or more preexisting chronic CVDs are present in approximately 60% of the deaths [73,74]. Such conditions include hypertension, coronary artery disease, and diabetes.
4.3 Hypertension, Diabetes, and Kidney Disease
The authors studied the clinical profiles of 204 elderly patients admitted with confirmed COVID-19 in [75]. The results indicate that besides age, hypertension is highly associated with an increased risk of death. Other disease conditions that contribute to the elevated risk of mortality are CVD, diabetes, COPD, malignant tumors, and kidney disease. Patients with lung, heart, and kidney disease are highly vulnerable to COVID-19. Similarly, the data for 87 elderly people were collected from a nursing home to study the characteristics of COVID-19 in [76]. It was found that the probability of COVID-19 infection is 100% for people younger than 90 years with dyspnea and falls, people older than 90 with anorexia, and people older than 90 without anorexia but with altered dementia. Similarly, [77] analyzed the data of 2968 patients from Iran to analyze the impact of underlying diseases on the outcome of COVID-19 patients. Findings indicate that a higher age group is at a higher risk of COVID-19 infection. Older people with preexisting diabetes, chronic respiratory diseases, hypertension, CVD, chronic kidney diseases, and cancer have a higher associated risk of complicated COVID-19 infection and mortality. In the same vein, the authors performed analyses on 14,712 patients with 43.7% females and 56.3% males in [78]. Statistics suggest that male patients are older ( ). A high prevalence of hypertension, diabetes, coronary disease, obstructive pulmonary disease, nicotine dependence, and heart failure is found in COVID-19 victims.
). A high prevalence of hypertension, diabetes, coronary disease, obstructive pulmonary disease, nicotine dependence, and heart failure is found in COVID-19 victims.
The analyses of 1591 confirmed patients with COVID-19 in [79] revealed that 31.99% of the patients had hypertension. Hypertension is found in a higher number of older patients than younger people. Similarly, the authors analyzed the data of 2634 patients (out of 5700 admitted) who died or were discharged during the COVID-19 outbreak in [80]. Evidence shows that diabetics are more likely to require mechanical ventilation. The death rates for patients requiring mechanical ventilation in the age groups 18–65 and older than 65, respectively were 76.4% and 97.2%. Similarly, the influence of diabetes leads to acute kidney injury compared to patients without diabetes. The most common comorbidities found in COVID-19 patients were hypertension, obesity, and diabetes, with 56.6%, 41.7%, and 33.8%, respectively. Similarly, a study [81] conducted on 161 COVID-19 confirmed patients in China investigated underlying comorbidities. Analysis indicated that hypertension was found in 23.0% of the patients, while 8.0% had diabetes. Another 5.3% had coronary heart disease, while 7.1% of the patients were current smokers. Exposure to patients with the confirmed disease is likely to increase the infection rate. Prolonged treatment is associated with preexisting hypertension.
The data for 2634 patients who died or were discharged showed that 12.2% required mechanical ventilation, of which 76.4% and 97.2% died for 18–65 years and older than 65 years, respectively. The mortality rate for those who did not receive mechanical ventilation was 1.98%, 26.6% for 18–65 years, and older than 65 years of age groups. The study revealed that older men are highly exposed to COVID-19, similar to those with preexisting hypertension and diabetes.
Several studies have investigated the impact of preexisting kidney disease on severe illness and mortality in COVID-19 patients. For example, the author studied kidney abnormalities in 701 confirmed patients with COVID-19 [82]. Approximately half of the admitted patients (42.6%) had one or more comorbidities such as chronic kidney disease, chronic obstructive pulmonary disease, hypertension, diabetes, and tumor, of which kidney patients constituted 2.0%. High serum creatinine was reported in 14.4% of the admitted patients, who were predominantly male, older, and seriously ill than those with normal serum creatinine. Similarly, another study that explored the clinical characteristics of 155 patients in China revealed that 45.8% of the patients had at least one preexisting disease, such as hypertension (23.9%), kidney disease, diabetes (9.7%), and CVD (9.7%) [83]. The authors state that obesity significantly increases the risk of complicated respiratory disease and COVID-19 infection [84]. Analysis performed on 214 patients with confirmed COVID-19 suggests that patients having MAFLD (Metabolic Associated Fatty Liver Disease) have metabolic risk factors and may lead to severe respiratory disease. Of the patients with severe COVID-19, 89.5% were more obese than those with mild disease. A six-fold increased risk of critical illness was associated with COVID-19 patients with MAFLD.
The findings of the above-discussed studies indicate that COVID-19 patients with preexisting CVD are at high risk of developing a critical illness or death. Despite this, there is no single CV factor responsible for such complications. Moreover, the data findings are from two or three countries and may not apply to other countries with different age groups and living and health conditions, such as South Korea. Many of the studies are retrospective and are limited by selection bias, health conditions, and care-seeking behaviors. The mortality rate found in many of the studies was higher than that of the average mortality rate for COVID-19, suggesting that a large percentage of the included data is from hospitalized patients and those quarantined with mild symptoms are not taken into account. Studies indicate that patients with CVD should be placed under special consideration to avoid severe illness.
Multiple studies suggest that the prevalence of preexisting medical conditions, such as asthma, diabetes, and hypertension, complicates the illness and the probability of death for COVID-19 patients. As a result, numerous researchers have studied the impact of various medical conditions on the severity and fatality of infected patients. Results indicate that patients with preexisting CVD are at an elevated risk of severe illness and death. Similarly, underlying kidney disease leads to higher chances of mechanical ventilation. Hypertension is another medical condition associated with a higher risk of death. Diabetes, malignant liver disease, and cancer patients are prone to grave danger from complicated medical conditions and death if infected by COVID-19. Though such studies’ findings are helpful for medical experts and policymakers to consider when making plans to tackle the COVID-19 outbreak, they are restricted by a few limitations. In most instances, research findings are from two or three countries. Many important elements such as health conditions, living conditions, demographics, and personal information, are not considered for analysis, limiting their wider application. Similarly, studies that are retrospective by nature may be biased because of selection, health conditions, and care-seeking behaviors. Fatality rates are calculated without considering the outputs of all admitted patients and may be exaggerated. People in quarantine, being asymptomatic, and with mild conditions are not included thus limiting the scope of the analysis.
High cholesterol, preexisting CVD, hypertension, diabetes, and kidney disease are associated with a higher risk of severe illness and fatality in COVID-19 patients. Such indicators can potentially be used to measure the level of illness and the probability of death.
5 Disparity of COVID-19 Cases for Different Age Groups and Gender
Emerging evidence suggests that the risk of developing COVID-19 infection varies by age group and gender. Consequently, studies across a broad spectrum were conducted to evaluate these hypotheses. Such studies may be broken down into three broad categories: studies that investigate the impact of age on COVID-19 risk, studies that analyze the vulnerability to COVID-19 by gender, and studies investigating other factors that may explain the probability of getting COVID-19, such as pregnancy and age peer group. In the following sections, the research works and their findings are discussed for each category.
5.1 Impact of Age to Combat COVID-19
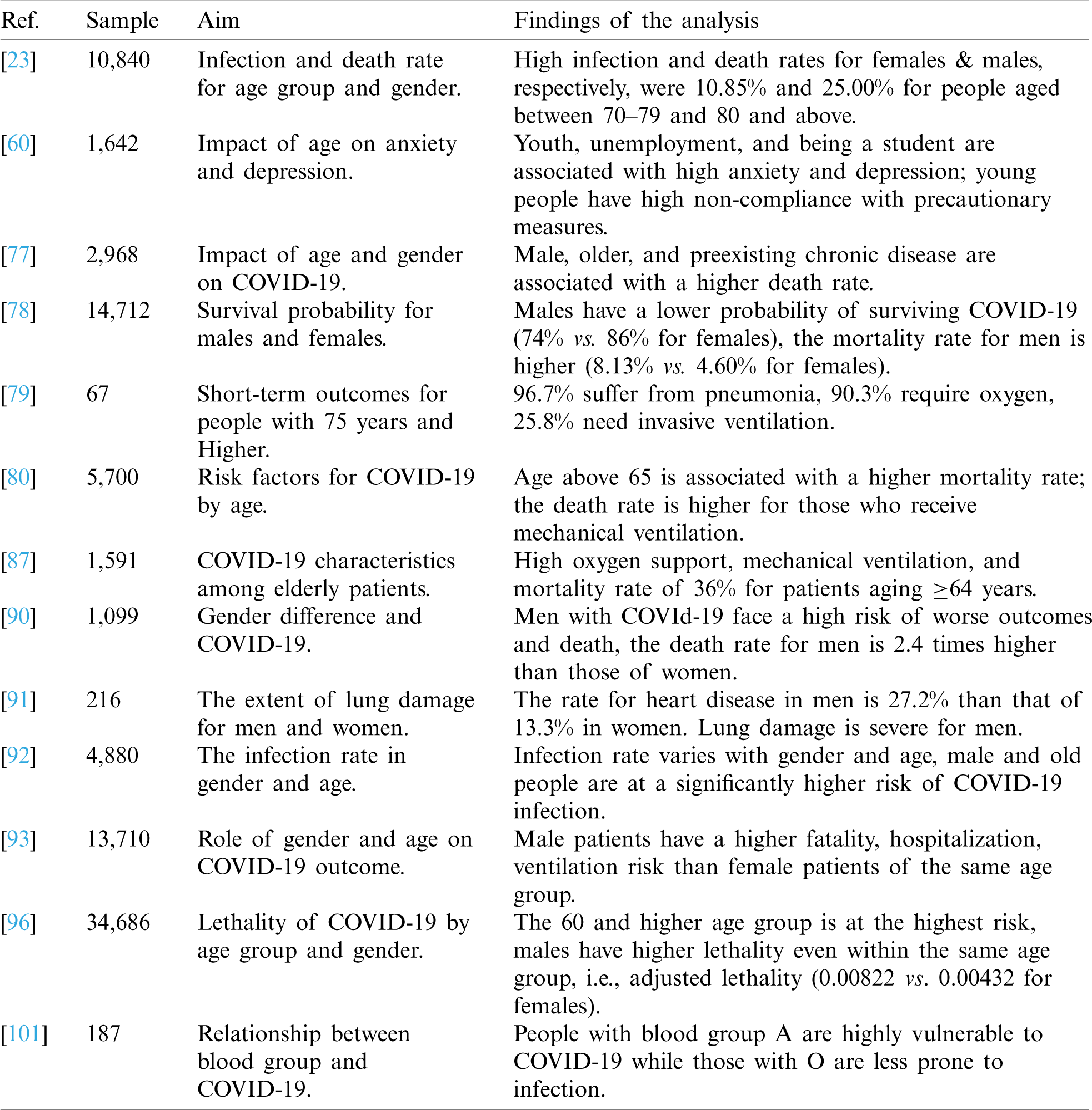
A scoping study [23] of 10,840 patients from South Korea points out the impact of age and gender on the death rate from COVID-19. The female infection rate was higher (59.35%) than that of males (40.65%); however, the fatality rate is higher for male patients, that is, 3.02% vs. 1.91% for females. Similarly, the death rate is higher for people aged 80 years or older (25.00%), followed by those aged 70–79 years (10.85%). The authors analyzed the data of 5700 patients with COVID-19 from the US for preexisting conditions resulting in complicated illness [80]. The data for 2634 patients who died or were discharged showed that 12.2% received mechanical ventilation, of which respectively 76.4% and 97.2% in the 18–65 cohort, and the older than 65 cohort, died. The mortality rates for those who did not receive mechanical ventilation were 1.98%, 26.6% for the 18–65, and older than 65 age groups.
Age plays a vital role in combating COVID-19 infection, and [75] studies the impact of greater age on the outcome of COVID-19 patients, where a sample of 204 confirmed patients was analyzed. The age of all patients was above 60, with a median age of 68. Upon initial admission, 64.7% of the cases were mild. Analysis results show that age and underlying diseases are associated with high fatality risk. Despite the lower mortality rate of COVID-19, a higher fatality rate of 37.3% is associated with patients aged ¿ 60 years. Another study in the same direction was [85], in which the characteristics of greater age were investigated in COVID-19 patients. The data for 339 patients aged between 60 and 80 years admitted to a hospital were analyzed. The results revealed that the fatality rate for elderly COVID-19 patients is high, and 19.2% of the sample size died after a short stay in the hospital. The factors associated with a high fatality rate are symptoms of dyspnea, CVD, chronic obstructive pulmonary disease, and acute respiratory distress syndrome.
The authors performed COVID-19 screening and study characteristics in [76] for a nursing home with 87 older people and 92 staff members. The results show that the residents and staff have different attack rates of 47% and 24%, respectively. The mortality rate for older people studied in the research was 15%, which is higher than the average reported rate (2%–3%). Reference [60] also presents an analysis of COVID-19 patients’ data for exploring the impact of age and gender. The Mann–Whitney test shows that women have higher anxiety and patient health questionnaire-9 scores than men. The Kruskal–Wallis H test indicates that younger people (18 to 29 years) face the highest anxiety and depression. Students and unemployed experience higher anxiety than those of non-students and employed, respectively. Similarly, people with a preexisting psychiatric history face higher anxiety and depression. Younger people prove to be less compliant with precautionary measures.
The data of 17,305 patients were analyzed in [86] to find the correlation between the age group and its impact on the recovery and fatality rates for COVID-19. The results show that clustering related ages is more explanatory than by country. The cluster with higher infections belongs to the 30–40 years range. Similarly, it was found that recovery rates are higher in the Asian, EU, and UK groups. Additionally, higher fatality rates are found for the Middle East and North American groups, and females have lower fatality rates than males in Asia, the EU, and the UK. Another work [79] reviewed the data of 67 confirmed patients with COVID-19 who were aged 75 years to study short-term outcomes of being discharged, not discharged, and death. Statistics revealed that 96.7% of the patients suffered from pneumonia, 90.3% required oxygen supplements, and 25.8% underwent invasive ventilation. A total of six deaths occurred among 67 patients because of acute respiratory distress syndrome worsened by septic shock and heart injury. Results showed that patients aged  65 years had severe outcomes.
65 years had severe outcomes.
The data for 1591 confirmed patients of COVID-19 were analyzed in [87] for Italy to investigate the important characteristics of the patients. The majority of the patients were 56 to 70 years old, and males constituted 82% of the total patients. Respiratory support was provided to approximately 99% of patients with 88% mechanical ventilation and 11% with noninvasive ventilation. Older patients aged  64 years have a higher mortality rate of 36% than those aged
64 years have a higher mortality rate of 36% than those aged  63 with a mortality rate of 15%.
63 with a mortality rate of 15%.
5.2 Vulnerability of Gender Group for COVID-19
Apart from age, the outcome of COVID-19 by gender has been investigated in many analytic studies. For example, the authors perform a comprehensive analysis of the available data from various databases, online news, and published articles on how gender is related to COVID-19 in [88]. The results indicate that South America, NY, and Asian countries experience higher COVID-19 cases associated with males, except for South Korea. In global Europe, the infection rates for males and females are comparable. Another study [89] investigating symptomatic and asymptomatic cases for the initial outbreak in China showed that the infection rate is higher for females. The male infection rate was 42.6%, while 57.4% of females were infected with COVID-19. However, males tend to be highly asymptomatic (54.5%), while females experience symptomatic features when infected with COVID-19.
The study [90] investigated the influence of gender on COVID-19 outcomes using data from multiple sources such as hospital patients (43), public datasets (37), and the dataset of surviving patients from China (1019). The analysis revealed that greater age and multiple comorbidities proved to be fatal for COVID-19 patients. Even though men and women are prone to COVID-19, men are at a higher risk for worse outcomes, with a fatality rate of 2.4 times that of women. Along the same lines, the authors performed an analysis to assess the extent of lung injury in men and women with COVID-19 [91]. Results show that heart disease is more prevalent among men, with a rate of 27.2% against 13.3% in women. CT findings showed a higher severity score for men than for women. The study corroborates that men are at a higher risk of death than women.
The role of sex and gender on the outcome of COVID-19 was studied in [92] for 4880 patients with respiratory symptoms or close contact with COVID-19 confirmed patients in Wuhan, China. A total of 38.42% of these people tested positive for COVID-19. The analysis shows that higher infection rates are associated with gender and age; among the suspected cases older males had a significantly higher risk of developing COVID-19 infection. Similarly, gender disparity was analyzed in [93] for COVID-19 patients. The study considered age and sex to analyze the outcome for COVID-19 patients. Results indicate that a higher mortality risk is associated with males. Similarly, the risk of hospitalization and mechanical ventilation is higher for male victims. The risk of death and comorbidities is higher in male patients than in female patients, even for the same age group. The gender-based risk of fatality is higher in men of higher age. Additionally, a higher risk of ICU admission is associated with male patients than female COVID-19 patients [94].
On a similar note, a cohort study is presented in [77] on the data of 2968 patients in Iran. The results suggest that male patients are at higher risk of death than female patients with COVID-19. Being male, of greater age (60 and higher), and having underlying diseases are associated with a higher probability of mortality. In the same way, the research [95] indicates that although both men and women are victims of COVID-19, the difference lies in mortality and vulnerability to the disease. Results suggest that the male fatality rate is higher than the female, potentially based on immunological or gendered differences.
Reference [78] presents a study on the role of gender in surviving COVID-19, wherein the data of 14,712 patients were analyzed. A higher number of older men were found among patients with various preexisting diseases. Evidence indicates that the mortality rate among males is 8.8% and females (4.3%). Additionally, the probability of survival for males is significantly lower than that for females, at 74% and 86%, respectively. In the same vein, the authors assess the data of patients from Mexico in [96]. The concept of adjusted lethality is used to describe the probability of death for various age groups, for males and females, separately. Statistics show that the highest risk of mortality is for the age group 60 or higher for both males and females. Additionally, lethality among males is approximately 100% higher than for females, even within the same age group.
Besides males and females, homosexuals also have associated risk factors, mental problems, and special needs amidst the COVID-19 crisis. Reference [97] indicates that because of social barriers based on binary gender norms, transgender people face an increased risk of illness and mortality during COVID-19. Additionally, transgender adults already face underlying medical problems that increase their vulnerability to COVID-19 and may lead to severe illness or death [98]. In the US alone, a total of 319,800 transgender adults face one or more diseases, such as asthma, diabetes, heart disease, and HIV. Another study [99] investigated physical and mental problems in lesbian, gay, bisexual, and transgender (LGBT) community showed that 45.7% of LGBT college students confused about their identity and almost 60% of LGBT college students face psychological distress, anxiety, and depression during COVID-19.
5.3 Vulnerability of Various Blood Groups to COVID-19
Besides age and gender, two additional study lines are the vulnerability of various blood groups and the probability of COVID-19 in children born from COVID-19 infected mothers. Therefore, the impact of COVID-19 on newborns was analyzed in [100] using the medical data of 755 pregnant women and 598 infants. The authors state that there is no evidence of vertical transmission based on the findings of the study. Among the 493 infants tested for COVID-19, only 2% were found to have the disease. The influence of a specific blood group is important to tackle COVID-19; therefore, the authors studied the relationship between blood group and COVID-19 patients’ characteristics in [101]. The study identified that among 187 patients selected for analysis, type A blood patients were significantly higher (36.90%). People with type A blood have the highest risk of infection. Conversely, those with O blood groups have a lower associated risk of being infected with COVID-19.
5.4 Critical Appraisal of Discussed Works
The data selected for COVID-19 patients were predominantly obtained from hospitals. The proportion of severely and critically ill patients may be higher than those of other hospitals in different countries with different living and health conditions. The fatality rate may differ from that of the entire infected population in a country. Similarly, the data collected from various nursing homes and other similar institutions may not be fully representative of the general population. The residents isolated in such institutions do not suffer from the same cognitive disorders as the common population.
Tab. 4 imparts a critical appraisal of the research works that study the role of age groups and gender in combating the COVID-19 pandemic. The impact of age groups and gender is an important factor that may indicate the susceptibility of COVID-19 infection. A broad spectrum of research focuses on the relationship between age groups and gender and their vulnerability to COVID-19 infection and death. Evidence and findings of these studies suggest multifarious views about the vulnerability of males to severe illness and death. Many studies have revealed that males have a higher associated risk of COVID-19 infection. Additionally, the mortality rate is higher for male patients admitted with COVID-19. The likelihood of fatality is higher when the age is 60 years or higher among both males and females; however, males are at higher associated risk. When greater age is associated with preexisting medical conditions such as diabetes, CVD, hypertension, and lung disease, the probability of a severe outcome is even higher. Various blood groups have different vulnerability levels to COVID-19, where blood group A patients are at a significantly elevated risk of death. Despite the findings of these studies, several factors undermine their importance. The data used for analysis are often collected from hospitals and clinics caring for severely ill and critical patients. Such inclusion of the data may be potentially higher than those with mild symptoms and quarantined patients, resulting in overstating the fatality rate. The data collected from hospitals may not reflect the general population, and the results may vary significantly if the data for all those infected are considered. Similarly, data from a different country with different health and social conditions may change the results dramatically.
Table 4: Summary of findings of works that study the influence of gender on COVID-19
Greater age is associated with an elevated risk of COVID-19 infection and fatality. Various age groups have different risk factors for COVID-19. Females are found to be less vulnerable than males to COVID-19 infection. Similarly, transgender adults have a higher associated risk concerning their preexisting medical conditions.
6 Prediction of Mortality and Severity of COVID-19
Coping with the accelerated pace of fast-spreading COVID-19 requires analyzing the risk of deterioration, assessing the underlying comorbidities, predicting the probability of death or critically ill patients, and stratifying patients to manage them accordingly. By analyzing the clinical characteristics of COVID-19 patients to identify predictors of critical care admission and death is an important task that can facilitate the task of health professionals and save lives. Mortality or critical condition prediction involves analyzing several factors such as age, gender, comorbidities, respiratory capability, and oxygenation. Several studies can be found in the literature on the role of such indicators in predicting mortality and critical care admission for COVID-19 patients.
There are several types of studies that focus on COVID-19 severity of illness and mortality. Among the most widely conducted investigations is the analysis of factors associated with aggravated illness and elevated mortality and analysis of CFR and infection fatality rate (IFR) comparison among various countries. The following discussions are categorized under the groups mentioned above.
6.1 Risk Indicators to Predict Fatality and Severity of Illness
The authors performed the analysis on 1,157 confirmed COVID-19 patients in [102] to predict patients at high risk of critical care or death. The risk score for death or severe condition was calculated by incorporating 12 factors such as age > 40, male, non-white, oxygenation < 93%, radiological severity score > 3, neuropathic count > 8.0109/L, CRP > 40 mg/L, albumin < 34 g/L, creatinine > 100 mmol/L, diabetes, hypertension, and chronic lung disease. A risk score of 4 indicates a 40.7% risk of death higher than the 12.4% for patients with a risk score of less than 4. A higher risk score is associated with critical care admission of a longer duration. Similarly, the authors performed a detailed chart overview in [103] for 355 patients who died of COVID-19 in Italy. The majority of the fatalities were older with a median age of 79.5 years and male (70%). The high-risk factor identified during the analysis was underlying co morbidity and greater age. COVID-19 patients with diabetes have a higher association with death, with a rate of 35.5%, followed by active cancer, CVD, atrial fibrillation, stroke, and dementia with death rates of 30.0%, 24.5%, 20.3%, 9.6%, and 6.8%, respectively. Of the patients who died, 25.1%, 25.6%, and 48.5% had one, two, and three or more underlying diseases, respectively. An additional supporting study [104] suggests that a higher fatality rate is found in COVID-19 patients aged 60 years or older. A study of 1560 cases indicated that 31.5% of total deaths result from cancer, other underlying diseases, or severe infections. It was also stated that the fatality rate is higher for patients with mixed bacterial infection and basic disease.
Sardinia, an Italian island, was selected for epidemiological studies owing to its geographical characteristics and genetic homogeneity [105]. A sample of 1223 COVID-19 patients was selected to study potential risk factors for the disease’s final outcome. Approximately 98.9% of the deceased patients carry underlying health conditions. Elderly people are at higher risk of death, as the analysis indicates that 83.5% of the deaths are aged 70 or more. The CFR for men is almost double that of women, that is, 10.4% vs. 6.2%, respectively. The high-risk factor is associated with COVID-19 patients with underlying diseases such as CVD, chronic neurological diseases, chronic lung diseases, and diabetes mellitus. Similarly, it was pointed out in [106] that hypertension, diabetes, and chronic kidney disease have an elevated risk of death in COVID-19 patients. Additionally, the analysis of 5,152 patients suggests that other comorbidities such as asthma, HIV, and cancer lead to severe illness and critical care is required for recovery. Other parameters that are useful to determine the risk of death for COVID-19 patients are age, sex, respiratory rate, oxygen saturation level, systolic blood pressure, and maximum temperature.
In the same vein, the demographic and clinical characteristics of 417 patients were studied in [107] to build a model for predicting the severity of COVID-19 illness. The findings indicate that of the patients who took more than 20 days to recover, the majority were in the 50 or older age group. Four risk factors were identified, namely, age, body mass index (BMI), CD4 T lymphocytes, and IL-6 levels. Severe illness occurred in patients with age > 55 with BMI > 27 kg/m2, IL-6 > 20 pg/mL, and CD4 T cells > 400 mL. A lower platelet count requires a longer recovery time. Similarly, underlying chronic liver disease, hypertension, diabetes, and CVD medical conditions were found in 8.4%, 7.6%, 4.8%, and 2.8% of the patients, respectively. In a similar study [108], which focused on the severity and CFR of COVID-19 patients, the data of 2547 patients in India were studied for underlying risk factors that lead to severe illness or death. Disease fatality rates (DFRs) were used to analyze the lethality of particular underlying diseases for COVID-19 patients. The analysis indicated that diabetes in COVID-19 Indian patients is associated with a death rate of 39.4%, followed by CVD, hypertension, respiratory problems, kidney disorders, and liver ailments with rates of 33.3%, 25.8%, 15.2%, 10.6%, and 3.0%, respectively.
A study incorporating longer-term baseline mortality was presented in [109], where the underlying health conditions were integrated to estimate 1-year mortality with different infection rate scenarios. By considering the data of 3,862,012 people, the study suggests that 20% of the total population is at high risk of catching COVID-19 in the UK. People older than 70 and having at least one co morbidities are at higher risk of death from COVID-19. In a mitigation scenario where the suppression rate is 10%, 73,498 additional deaths are expected with a relative risk of 3.0.
6.2 Analysis of Infection and Case Fatality Rates
An analysis of the case fatality rate was performed in [110] to compare the mortality of COVID-19 between Turkey and European countries to understand epidemiological patterns. Fifteen days of data were selected from Turkey, and regression analysis was carried out to compare CFR between Turkey and Italy, Spain, the UK, France, Germany, Switzerland, Belgium, Austria, Netherlands, and Portugal. Analysis indicates that Turkey faces a similar CFR (1.85) as France (1.979). However, increasing the data for two more weeks suggests that other selected countries have a subsequent increase in CFR. A total of 40,835 confirmed patients and 1,620 deaths were analyzed in [111] to investigate the IFR and crude fatality rate (CrFR) for 134 US counties. CrFR varies from 1.7% to 33.3%, while the IFR rate varies between 0.5% and 3.6% for various counties. Variations in CrFR and IFR are a result of several demographic factors like age, gender, as well as, levels of population health, and provision of health care. Risk mitigation factors, such as social distancing and self-quarantining, have been reported to decrease IFR. In the absence of these strategies and because of the lack of health care supplies, the US is expected to experience 500,000 deaths this year from COVID-19. Similarly, the authors performed a mechanistic-statistical approach to infer the IFR from the data of infected cases in France [112]. Data from 10,612 confirmed cases and 1015 deaths were used for analysis. The IFR for hospital-counted deaths is 0.5%, while the CFR is 2% for the number of deaths which is higher than the diagnosed cases. Considering the number of deaths in nursing homes, the IFR would rise to 0.8%. Based on the analysis results, if 80% of the French population is infected with COVID-19, a death toll of 336,000 is expected from the general population, that is, without considering the number of deaths occurring in nursing homes.
6.3 Critical Evaluation of the Discussed Works
Many studies assume that the identified cases are symptomatic. However, substantial numbers of infected persons are reported to be asymptomatic [113]. As a result, the reported infection or death rate may be overstated. Similarly, the reported infection rate and CFR are not adjusted for age groups and comorbidity as the data for comorbidity profiles are not available. Similarly, the analysis of patients’ data whose outcomes are not available yet potentially varies from precise estimates when all the cases are available. Moreover, CFR is a poor measure to indicate the fatality risk of COVID-19 because of several important factors, such as demographic and health conditions. For example, a high CFR for a country with low population density means lower expected deaths and this may not be alarming for a small country. On the contrary, even a lower CFR for countries with high population density, such as China and India, indicate a higher mortality risk for such countries.
Predominantly, the models used for analyzing the risk factors are based on death over a short period for example, the number of fatalities over days, the majority of whom report underlying diseases. Such models neither integrate factors indicating high-risk conditions nor consider long-term mortality. Researchers lack complex models that consider various categories such as asymptomatic cases, unobserved symptomatic cases, observed symptomatic infectious, and infectious diseases without any link to confirmed cases. The application of such models would make it possible to predict the fraction of severity and fatality cases for COVID-19.
Getting to grips with COVID-19 involves the analysis of preexisting comorbidities and predicting the chances of critical illness and death so that it would be possible to stratify the patients who require intensive care and treatment. For this purpose, studies bring to light important indicators that can determine the probability of complicated medical conditions and death for medical experts to act accordingly to save lives. Such studies follow two plans of action: analyzing various factors among COVID-19 patients associated with illness and death and studying case fatality and infection fatality rates to establish a link between infection and fatality. In this process, various analytical approaches such as descriptive analysis, ratio analysis, and cohort study are used to analyze the clinical and demographic characteristics of COVID-19 patients. Many proposed models perform well for predicting the fatality of COVID-19, but they have several limitations. For example, the data used for the analyses were not adjusted for various age groups and comorbidities and proved to be less informative. The reported CFR and IFR may be excessive because of the exclusion of asymptomatic patients from the analysis. Matrices like CFR and IFR are not appropriate without considering demographic and health conditions such as population density and population age profiles. Using short-term data is yet another limitation, where the majority of the dead victims have preexisting medical complications. High-risk conditions and long-term mortality are not incorporated in such models. Similarly, simple models do not integrate various categories such as asymptomatic cases, infection scenarios, government interventions, and social interaction policies. Without the inclusion of such parameters, the results of these studies prove to be inadequate with insufficient information. Tab. 5 discusses the risk factors found in the works mentioned above and elaborates on their findings.
Table 5: Findings of works analyzing the risk of death and critical care admission for COVID-19
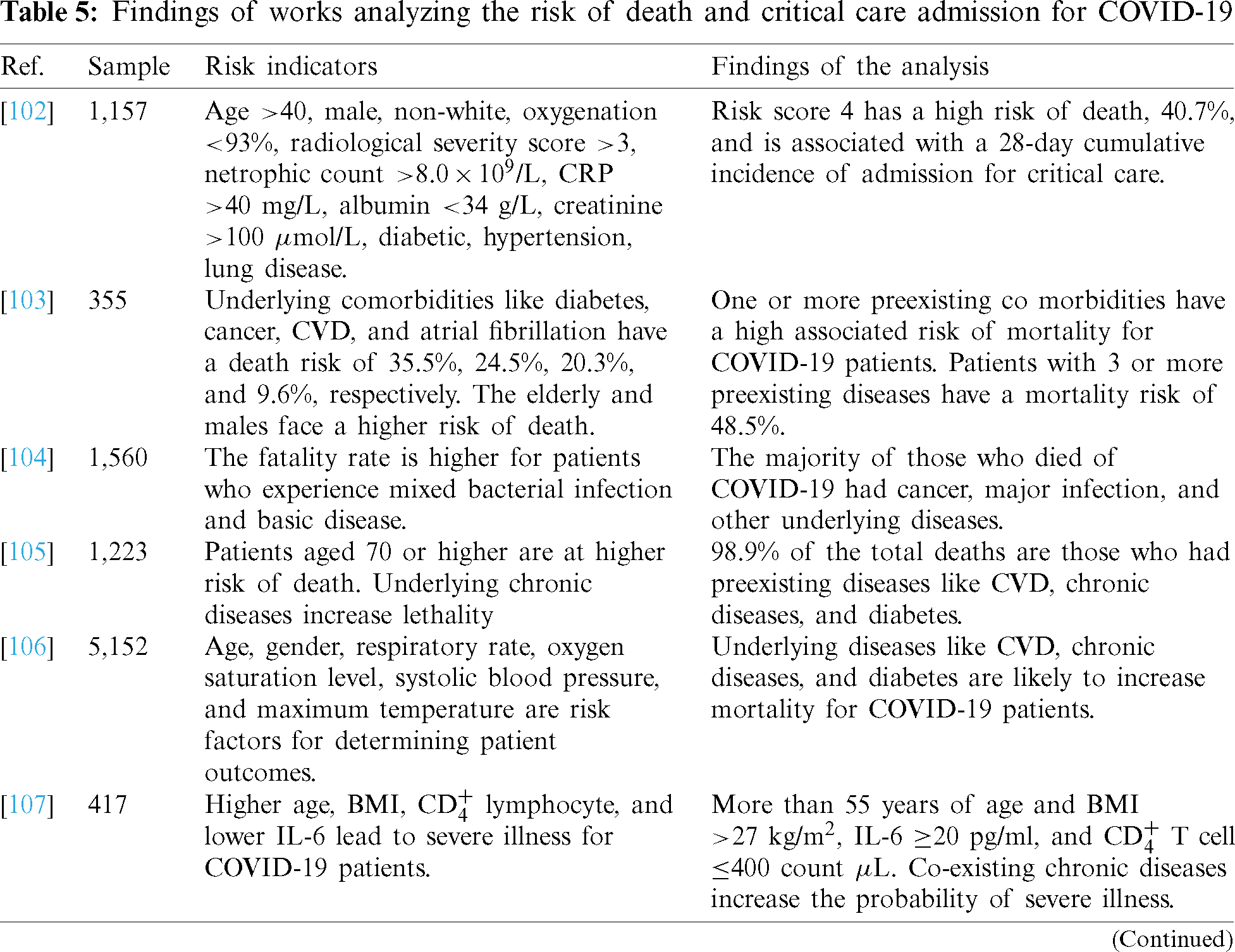
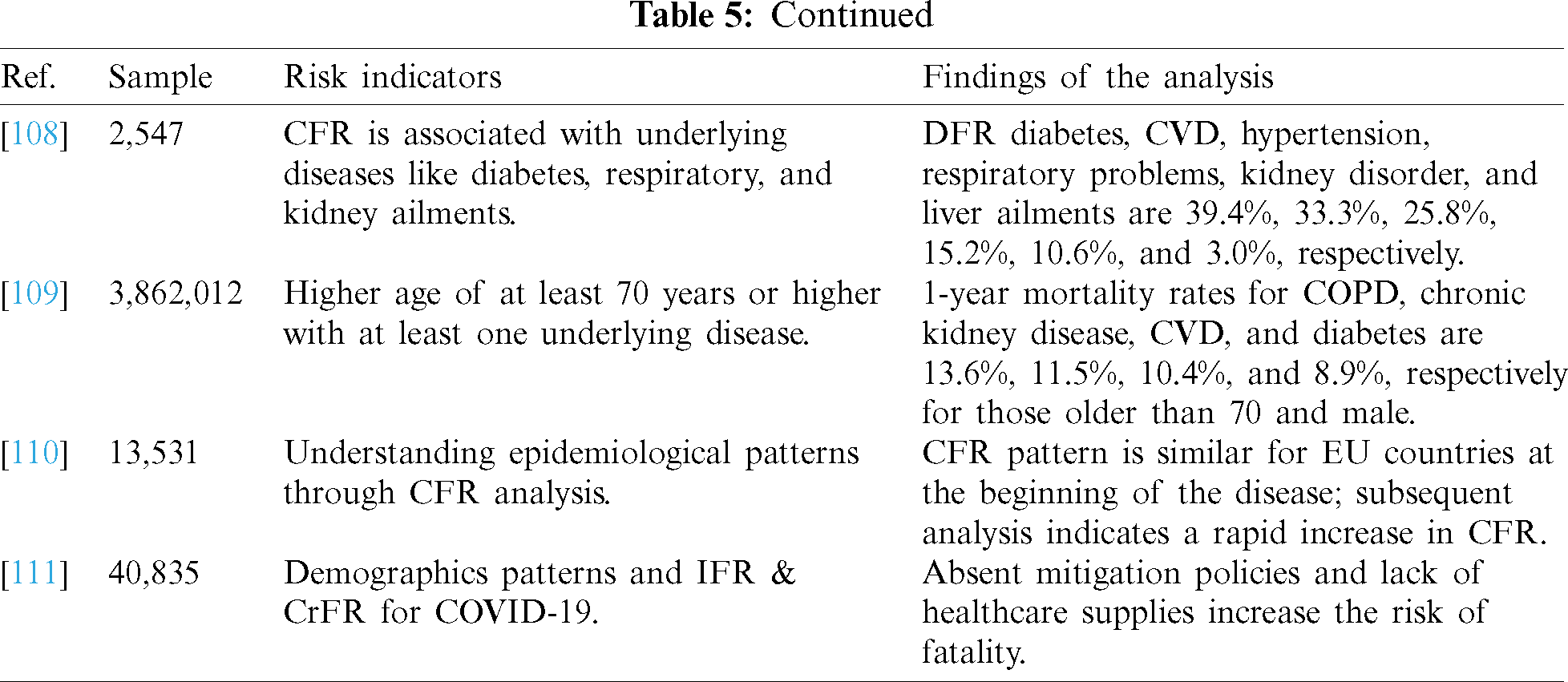
Studies that predict the fatality rate and level of illness focus on two aspects of COVID-19 patients: risk indicators that are useful for prediction and predicting the number of infected patients and fatality rates. Risk indicators include age, ethnicity, and preexisting medical conditions such as diabetes, hypertension, and chronic lung disease. The risk of death increases with an extended duration of critical care and the presence of multiple medical conditions. The CFR varies between 1.7% and 2, while CFR ranges between 1.7% and 33.3% from one country to another.
Despite government intervention policies to ensure directed social interaction behaviors and preventive measures taken at either the collective level, the pace of COVID-19 spread is not reducing, as expected. In such scenarios, modeling approaches, paradigms, and algorithms that can help research both positive and negative factors related to COVID-19 transmission and prevention are of great importance. Future work directions are critical to reduce substantially the spread of COVID-19 and hasten the recovery of those infected. Fig. 2 illustrates important areas that necessitate research contributions from various research communities to enhance the efficacy and efficiency of prediction and analysis approaches for COVID-19.
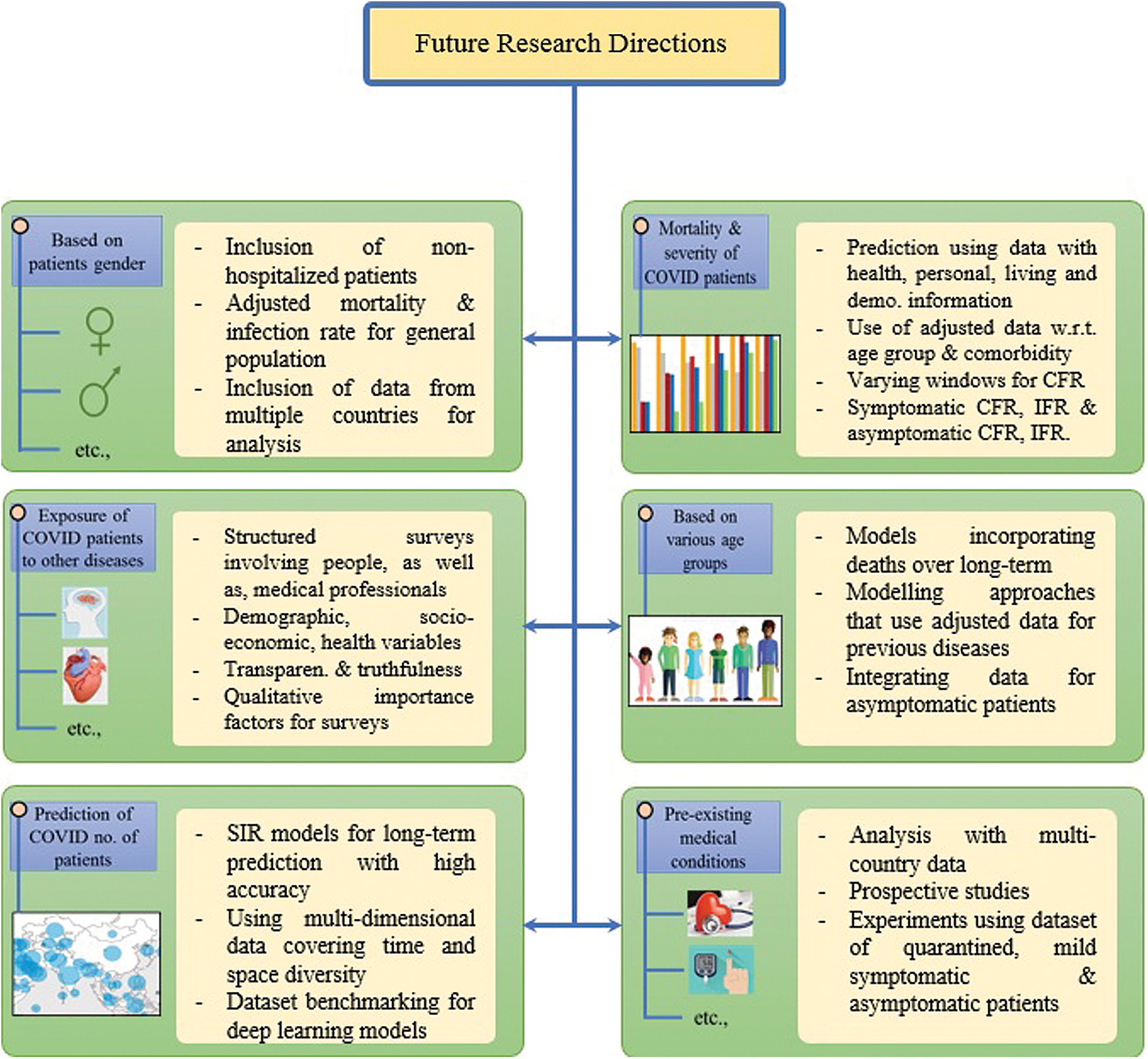
Figure 2: The future research directions in COVID-19 diagnostic & prognosis models
7.1 Models Prediction Number of Patients of COVID-19
Current SIR models used for predicting COVID-19 patients are used for a specific city or country, and the forecasts are short-term predictions spanning only a week or a month. Although few studies use SIR models for long-term predictions their accuracy is minimal. Moreover, multi-dimensional data reflecting spatio-temporal diversity are not used for prediction. Dataset benchmarking is another important line of action that can facilitate research to improve the models’ efficacy.
7.2 Exposure of COVID-19 Patients to Other Disease
An appropriate policy can be formulated based on the findings of the approaches that illustrate the exposure of COVID-19 patients to other diseases such as hypertension, sleep disturbances, suicidal thoughts, and similar problems. Current surveys and questionnaire-based studies are not well structured and lack the involvement of an appropriate population sample size. Well-integrated surveys incorporating demographic, socioeconomic, and health variables should be performed involving both civilians and medical professionals to unravel the psychological and physiological ailments.
7.3 Preexisting Medical Conditions and COVID-19
Analysis of COVID-19 data to study the influence of preexisting diseases such as CVD, diabetes, and lung diseases is mainly based on the data from one or two countries and is not generalized. Predominantly, retrospective studies are conducted, which necessitates prospective studies from multi-country data. A dataset comprising symptomatic as well as asymptomatic patients is urgently required.
7.4 Disparity of COVID-19 Cases for Various Genders
Studies that analyze gender-based vulnerabilty utilize the data of hospitalized patients where most are in a severe condition. The data for non-hospitalized patients, both self-quarantined, and with mild symptoms is desirable to explore the function of gender in combating COVID-19. Analysis should be done with the dataset adjusted for ethnicity, country, and age groups.
7.5 Role of Age Group to Combat COVID-19
Innovative complex models that can incorporate fatalities over a longer period are needed. The results from models trained on short-term death data are overrated and exaggerated. Data containing information of patients in hospital and quarantined, both symptomatic infectious and asymptomatic infectious is necessary to determine the relationship between various age groups and their vulnerability to severe illness and mortality for COVID-19.
7.6 Prediction of Mortality and Severity of COVID-19
Diversified data are required for integrating personal information, living conditions, health systems, and demographic information to make appropriate predictions. Metrics such as CFR and IFR alone can be misleading to represent the mortality of COVID-19 [114,115]. Additional metrics such as symptomatic CFR, asymptomatic CFR, and IFR should be used. Using a dataset adjusted for age group, demographics, and co morbidity can portray people’s general outcomes.
7.7 Impact of Adjusted Datasets on Prediction Models
Predominantly, the prediction models that currently are used either apply smaller datasets from single/multiple countries or the datasets are not adjusted to accommodate asymptomatic and self-quarantined individuals. This may result in the overstatement and exaggeration of infection and fatality rates. Adjusted datasets are essential to present balanced and more realistic CFR and IFR results.
Pandemics pose a huge threat to human existence as they spread worldwide, impacting physical and mental health. Apart from many deaths, widespread, long-term consequences influence national and international health policies and contingency plans. With the rapid spread of COVID-19, the general public and, particularly, governments face the challenging task of coping with many patients, ensuring medical and food supplies, and investigating the probable causes of the outbreak. Many medical researchers, data analysts, and biotechnologists have initiated research focusing on finding solutions for robust diagnosis, prediction of the approximate number of patients in cities and countries, and factors that may have a positive or negative impact on the spread and recovery from COVID-19. The current study groups such works under nine categories for age, gender, the outcome of the disease, method used for prediction, and role of underlying medical conditions. However, the emphasis is on models that predict mortality or the severity of COVID-19 in patients, the role of age and sex, impact of preexisting medical conditions, and exposure of COVID-19 patients to other diseases because the studies that resort under other groups have previously been discussed in several review papers.
The prediction models largely use simple datasets without adjusting for age group, comorbidities, and demographic information, which would produce different results if such parameters were incorporated. Complex models capable of integrating such parameters are required to provide efficient and reliable predictions. Approaches that consider government policies regarding the prevention of COVID-19, social distancing, self-seclusion, and quarantine are not accommodated in these models, which substantially reduces their efficacy. Conversely, datasets used for predictive and analytical models are gathered from hospitals and exclude patients with mild symptoms or who are asymptomatic. Therefore, the results can be somewhat overstated and exaggerated. Predominantly, the data are not adjusted for ethnicity, gender, age group, and preexisting medical complications, which is critical for analysis as the infection and case fatality rates vary by location and from nation to nation. CFR and IFR are most widely used to estimate the probability of severe illness and mortality, which, when used alone, can be misleading indicators to represent COVID-19 mortality. In summary, complex models with multiple parameters and diversified datasets containing detailed information of patients (such as demographic, personal, and health information) should be focused on in future investigations.
Finally, despite the critiques and deficiencies of the studies discussed herein, psychological and physiological analyses performed in such studies unravel many important factors and indicators to understand their impact and role in dealing with the widely spread COVID-19. Medical conditions that aggravate illness help medical experts to plan appropriately to cope efficiently with the influx of patients. Conversely, psychological problems found among COVID-19 patients of various communities are indicators that can help other communities define remedial policies in advance.
Funding Statement: This research was supported by the Researchers Supporting Project Number (RSP-2020/250), King Saud University, Riyadh, Saudi Arabia.
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
1. J. N. Hays. (2005). Epidemics and Pandemics: Their Impacts on Human History, 1 ed. Santa Barbara, CA, USA: Abc-clio. [Google Scholar]
2. X. Yang, Y. Yu, J. Xu, H. Shu, H. Liu et al. (2020). , “Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: A single-centered, retrospective, observational study,” Lancet Respiratory Medicine, vol. 8, no. 5, pp. 475–481. [Google Scholar]
3. W.H. Organization. (2019). “Coronavirus disease (COVID-19) dashboard,” , [Online]. Available: https://covid19.who.int/ (Accessed 21 November 2019). [Google Scholar]
4. R. Lea. (2020). “Coronavirus crisis: Unemployment and redundancies begin to rise,” Arbuthnot Banking Group, vol. 21, pp. 1–20. [Google Scholar]
5. H. Swapnarekha, S. B. Janmen, J. Nayakb and B. Naik. (2020). “Role of intelligent computing in COVID-19 prognosis: A state-of-the-art review,” Chaos Solitons & Fractals, vol. 138, pp. 109947. [Google Scholar]
6. B. Udugama, P. Kadhiresan, H. N. Kozlowski, A. Malekjahani, M. Osborne et al. (2020). , “Diagnosing COVID-19: The disease and tools for detection,” ACS Nano, vol. 14, no. 4, pp. 3822–3835. [Google Scholar]
7. Y. W. Tang, E. J. E. Schmitz, H. P. David and W. S. Charles. (2020). “Laboratory diagnosis of COVID-19: Current issues and challenges,” Journal of Clinical Microbiology, vol. 58, no. 6, pp. 3822–3835. [Google Scholar]
8. D. Dong, Z. Tang, S. Wang, H. Hui, L. Gong et al. (2020). , “The role of imaging in the detection and management of COVID-19: A review,” IEEE Reviews in Biomedical Engineering, . https://doi.org/10.1109/RBME.2020.2990959. [Google Scholar]
9. L. Wynants, B. V. Claster, G. S. Collins, R. D. Riley, G. Heinz et al. (2020). , “Prediction models for diagnosis and prognosis of COVID-19: Systematic review and critical appraisal,” BMJ, vol. 369, pp. m1328. [Google Scholar]
10. A. Jajodia, E. Lukas, H. Benedikt, C. Arvind and P. Helmut. (2020). “Imaging in corona virus disease 2019 (COVID-19)—A scoping review,” European Journal of Radiology Open, vol. 7, pp. 100237. [Google Scholar]
11. S. Salehi, A. Aidin, B. Sudheer and G. Ali. (2020). “Coronavirus disease 2019 (COVID-19A systematic review of imaging findings in 919 patients,” American Journal of Roentgenology, vol. 215, no. 1, pp. 87–94. [Google Scholar]
12. R. Cherniha and E. Vasyl. (2020). “A mathematical model for the COVID-19 outbreak and its applications,” Symmetry, vol. 12, no. 6, pp. 990. [Google Scholar]
13. V. Papastefanopoulos, L. Pantelis and K. Sotiris. (2020). “COVID-19: A comparison of time series methods to forecast percentage of active cases per population,” Applied Sciences, vol. 10, no. 11, pp. 3880. [Google Scholar]
14. G. E. P. Box, G. M. Jenkins, G. C. Reinsel and M. L. G. M. Lung. (2015). Time Series Analysis: Forecasting and Control. Hoboken, NJ, USA: John Wiley & Sons. [Google Scholar]
15. C. Chatfield. (1978). “The Holt-winters forecasting procedure,” Journal of the Royal Statistical Society: Series C (Applied Statistics), vol. 27, no. 3, pp. 264–279. [Google Scholar]
16. A. M. De Livera, J. H. Rob and D. S. Ralph. (2011). “Forecasting time series with complex seasonal patterns using exponential smoothing,” Journal of the American Statistical Association, vol. 106, no. 496, pp. 1513–1527. [Google Scholar]
17. S. J. Taylor and B. Letham. (2018). “Forecasting at scale,” American Statistician, vol. 72, no. 1, pp. 37–45. [Google Scholar]
18. D. Salinas, V. Flunkert, J. Gasthaus and T. Januschowski. (2020). “DeepAR: Probabilistic forecasting with autoregressive recurrent networks,” International Journal of Forecasting, vol. 36, no. 3, pp. 1181–1191. [Google Scholar]
19. A. Alexandrov, K. Benidis, M. Bohlke-Schneider, V. Flunkert, J. Gasthaus et al. (2019). , “Gluonts: Probabilistic time series models in python,” arXiv preprint arXiv:1906.05264. [Google Scholar]
20. B. N. Oreshkin, C. Dmitri, C. Nicolas and B. Yoshua. (2019). “N-BEATS: Neural basis expansion analysis for interpretable time series forecasting,” arXiv preprint arXiv:1905.10437. [Google Scholar]
21. G. Pinter, I. Felde, A. Mosavi, P. Ghamisi and R. Gloaguen. (2020). “COVID-19 pandemic prediction for Hungary: A hybrid machine learning approach,” Mathematics, vol. 8, no. 6, pp. 890. [Google Scholar]
22. J. Schüttler, R. Schlickeiser, F. Schlickeiser and M. Kröger. (2020). “Covid-19 predictions using a Gauss model, based on data from April 2,” Physics, vol. 2, no. 2, pp. 197–212. [Google Scholar]
23. E. Shim, M. Kenji, C. Wongyeong and C. Gerardo. (2020). “Estimating the risk of COVID-19 death during the course of the outbreak in Korea, February–May 2020,” Journal of Clinical Medicine, vol. 9, no. 6, pp. 1641. [Google Scholar]
24. A. M. Almeshal, I. A. Abdulla, R. A. Mohammad and N. A. Saleh. (2020). “Forecasting the spread of COVID-19 in Kuwait using compartmental and logistic regression models,” Applied Sciences, vol. 10, no. 10, pp. 3402. [Google Scholar]
25. B. Malavika, S. Marimuthu, M. Joy, A. Nadaraj, E. S. Asirvatham et al. (2021). , “Forecasting COVID-19 epidemic in India and high incidence states using SIR and logistic growth models,” Clinical Epidemiology and Global Health, vol. 9, pp. 26–33. [Google Scholar]
26. K. Demertzis, T. Dimitrios and M. Lykourgos. (2020). “Modeling and forecasting the COVID-19 temporal spread in Greece: An exploratory approach based on complex network defined splines,” Int. J. Environ. Res. Public Health, vol. 17, pp. 4693. [Google Scholar]
27. J. Fernandez-Recio. (2020). “Modelling the evolution of COVID-19 in high-incidence European countries and regions: Estimated number of infections and impact of past and future intervention measures,” Journal of Clinical Medicine, vol. 9, no. 6, pp. 1825. [Google Scholar]
28. B. Ambrosio and M. A. Aziz-Alaoui. (2020). “On a coupled time-dependent SIR models fitting with New York and New-Jersey states COVID-19 data,” Biology, vol. 9, pp. 135. [Google Scholar]
29. F. Qeadan, T. Honda, L. H. Grem, J. Dailey-Provost, L. S. Bensos et al. (2020). , “Naive forecast for COVID-19 in Utah based on the South Korea and Italy models-the fluctuation between two extremes,” International Journal of Environmental Research and Public Health, vol. 17, no. 8, pp. 2750. [Google Scholar]
30. R. A. R. Bantan, C. Chesneau, F. Jamal and M. Elgarhy. (2020). “On the analysis of new COVID-19 cases in Pakistan using an exponentiated version of the M family of distributions,” Mathematics, vol. 8, no. 6, pp. 953. [Google Scholar]
31. D. Alboaneen, P. Bernardi, A. Dhahi, A. Nourah and A. Raja. (2020). “Predicting the epidemiological outbreak of the Coronavirus disease 2019 (COVID-19) in Saudi Arabia,” International Journal of Environmental Research and Public Health, vol. 17, no. 12, pp. 4568. [Google Scholar]
32. A. Alsayed, S. Hayder, K. Raja and S. Hasan. (2020). “Prediction of epidemic peak and infected cases for COVID-19 disease in Malaysia,” 2020 International Journal of Environmental Research and Public Health, vol. 17, no. 11, pp. 4076. [Google Scholar]
33. T. Kuniya. (2020). “Prediction of the epidemic peak of coronavirus disease in Japan,” 2020 Journal of Clinical Medicine, vol. 9, no. 3, pp. 789. [Google Scholar]
34. Y. F. Zhao, M. H. Shou and Z. X. Wang. (2020). “Prediction of the number of patients infected with COVID-19 based on rolling grey verhulst models,” International Journal of Environmental Research and Public Health, vol. 17, no. 12, pp. 4582. [Google Scholar]
35. P. Melin, J. C. Monica, D. Sanchez and O. Castillo. (2020). “Multiple ensemble neural network models with fuzzy response aggregation for predicting COVID-19 time series: The case of Mexico,” Healthcare, vol. 8, no. 2, pp. 181. [Google Scholar]
36. A. Chatterjee, M. W. Gerdes and S. G. Martinez. (2020). “Statistical explorations and univariate timeseries analysis on COVID-19 datasets to understand the trend of disease spreading and death,” Sensors, vol. 20, no. 11, pp. 3089. [Google Scholar]
37. L. Qin, Q. Sun, Y. Wang, K. F. Wu, M. Chen et al. (2020). , “Prediction of number of cases of 2019 novel coronavirus (COVID-19) using social media search index,” International Journal of Environmental Research and Public Health, vol. 17, no. 7, pp. 2365. [Google Scholar]
38. V. Thakar. (2020). “Unfolding events in space and time: Geospatial insights into COVID-19 diffusion in Washington state during the initial stage of the outbreak,” ISPRS International Journal of Geo-Information, vol. 9, no. 6, pp. 382. [Google Scholar]
39. B. G. G. Oliver, P. Robinson, M. Peters and J. Black. (2014). “Viral infections and asthma: An inflammatory interface?,” State of the Art Infections and Asthma, vol. 44, no. 6, pp. 1666–1681. [Google Scholar]
40. J. J. Feddema and E. Claassen. (2020). “Prevalence of viral respiratory infections amongst asthmatics: Results of a meta-regression analysis,” Respiratory Medicine, vol. 173, pp. 106020. [Google Scholar]
41. A. Jha, J. Dunning, T. Tunstall, R. S. Thwaites, L. T. Hoang et al. (2019). , “Patterns of systemic and local inflammation in patients with asthma hospitalised with influenza,” European Respiratory Journal, vol. 54, no. 4, pp. 1900949. [Google Scholar]
42. E. Garcia-Pachon, L. Zamora-Molina, M. J. Soler-Sempere, C. Baeza-Martinez, J. Grau-Delgado et al. (2020). , “Asthma prevalence in patients with SARS-CoV-2 infection detected by RT-PCR not requiring hospitalization,” Respiratory Medicine, vol. 171, pp. 106084. [Google Scholar]
43. D. M. G. Halpin, R. Faner, O. Sibila, J. R. Badia and A. Agusti. (2020). “Do chronic respiratory diseases or their treatment affect the risk of SARS-CoV-2 infection?,” Lancet Respiratory Medicine, vol. 8, no. 5, pp. 436–438. [Google Scholar]
44. M. Yamaya, H. Nishimura, X. Deng, M. Sugawara, O. Watanabe et al. (2020). , “Inhibitory effects of glycopyrronium, formoterol, and budesonide on coronavirus HCoV-229E replication and cytokine production by primary cultures of human nasal and tracheal epithelial cells,” Respiratory Investigation, vol. 58, no. 3, pp. 155–168. [Google Scholar]
45. L. Huang. (2020). “Cardiac involvement in patients recovered from COVID-2019 identified using magnetic resonance imaging. JACC Cardiovasc,” Imaging, vol. 13, no. 11, pp. 2330–2339. [Google Scholar]
46. V. Russo, R. Bottino, A. Carbone, A. Rago, A. A. Papa et al. (2020). , “Covid-19 and heart: From clinical features to pharmacological implications,” Journal of Clinical Medicine, vol. 9, no. 6, pp. 1944. [Google Scholar]
47. J. Guo, X. L. Feng, X. H. Wang and M. H. van IJzendoorn. (2020). “Coping with COVID-19: Exposure to COVID-19 and negative impact on livelihood predict elevated mental health problems in Chinese adults,” International Journal of Environmental Research and Public Health, vol. 17, no. 11, pp. 3857. [Google Scholar]
48. M. Maarefvand, S. Hosseinzadeh, O. Farmani, A. Safarabadi Farahani and J. Khubchandani. (2020). “Coronavirus outbreak and stress in Iranians,” International Journal of Environmental Research and Public Health, vol. 17, no. 12, pp. 4441. [Google Scholar]
49. E. P. H. Choi, B. P. H. Hui and E. Y. F. Wan. (2020). “Depression and anxiety in Hong Kong during COVID-19,” International Journal of Environmental Research and Public Health, vol. 17, no. 10, pp. 3740. [Google Scholar]
50. R. Stanton, Q. G. To, S. Khalesi, S. L. Williams, S. J. Alley et al. (2020). , “Depression, anxiety and stress during COVID-19: Associations with changes in physical activity, sleep, tobacco and alcohol use in Australian adults,” International Journal of Environmental Research and Public Health, vol. 17, no. 11, pp. 4065. [Google Scholar]
51. R. Y. Elbay, K. Ayşe, A. Selim and K. Emrah. (2020). “Depression, anxiety, stress levels of physicians and associated factors in Covid-19 pandemics,” Psychiatry Research, vol. 290, pp. 113130. [Google Scholar]
52. M. R. Gualano, L. M. Giuseppina, V. Gianluca, B. Fabrizio and S. Roberta. (2020). “Effects of Covid-19 lockdown on mental health and sleep disturbances in Italy,” International Journal of Environmental Research and Public Health, vol. 17, no. 13, pp. 4779. [Google Scholar]
53. S. Shoib, N. Sachin, G. Omityah, R. Sajjadur and R. Ramdas. (2020). “Factors associated with COVID-19 outbreak-related suicides in India,” Asian Journal of Psychiatry, vol. 53, pp. 102223. [Google Scholar]
54. C. Blume, H. S. Marlene and C. Christian. (2020). “Effects of the COVID-19 lockdown on human sleep and rest-activity rhythms,” Current Biology, vol. 30, no. 14, pp. 795–797. [Google Scholar]
55. G. Forte, F. Favieri, R. Tambelli and M. Casagrande. (2020). “The enemy which sealed the world: Effects of COVID-19 diffusion on the psychological state of the Italian population,” Journal of Clinical Medicine, vol. 9, no. 6, pp. 1802. [Google Scholar]
56. S. M. Jungmann and W. Michael. (2020). “Health anxiety, cyberchondria, and coping in the current COVID-19 pandemic: Which factors are related to coronavirus anxiety?,” Journal of Anxiety Disorders, vol. 73, pp. 102239. [Google Scholar]
57. D. J. Li, K. Nai-Ying, C. Yi-Lung, W. Peng-Wei, C. Yu-Ping et al. (2020). , “COVID-19-related factors associated with sleep disturbance and suicidal thoughts among the Taiwanese public: A Facebook survey,” International Journal of Environmental Research and Public Health, vol. 17, no. 12, pp. 4479. [Google Scholar]
58. J. Gómez-Salgado, A. V. Montserrat, D. S. Sara, D. M. Diego and R. F. Carlos. (2020). “Related health factors of psychological distress during the COVID-19 pandemic in Spain,” International Journal of Environmental Research and Public Health, vol. 17, no. 11, pp. 3947. [Google Scholar]
59. L. Duan, X. Shao, Y. Wang, Y. Huang, J. Miao et al. (2020). , “An investigation of mental health status of children and adolescents in china during the outbreak of COVID-19,” Journal of Affective Disorders, vol. 275, pp. 112–118. [Google Scholar]
60. I. Solomou and C. Fofi. (2020). “Prevalence and predictors of anxiety and depression symptoms during the COVID-19 pandemic and compliance with precautionary measures: Age and sex matter,” International Journal of Environmental Research and Public Health, vol. 17, no. 14, pp. 4924. [Google Scholar]
61. D. C. Knockaert. (2007). “Cardiac involvement in systemic inflammatory diseases,” European Heart Journal, vol. 28, no. 15, pp. 1797–1804. [Google Scholar]
62. D. Radenkovic, S. Chawla, M. Pirro, A. Sahebkar and M. Banach. (2020). “Cholesterol in relation to COVID-19: Should we care about it?,” Journal of Clinical Medicine, vol. 9, no. 6, pp. 1909. [Google Scholar]
63. N. Katsiki, M. Banach and D. Mikhailidis. (2020). “Lipid-lowering therapy and renin-angiotensin-aldosterone system inhibitors in the era of the COVID-19 pandemic,” Archives of Medical Science, vol. 16, no. 3, pp. 485–489. [Google Scholar]
64. Y. Wang, Y. Zong, F. Yin, X. Yang, H. Zhong et al. (2020). , “Cholesterol metabolism—Impacts on SARS-CoV-2 infection prognosis,” medRxiv, . Preprint, https://doi.org/10.1101/2020.04.16.20068528. [Google Scholar]
65. N. Zaki, H. Alashwal and S. Ibrahim. (2020). “Association of hypertension, diabetes, stroke, cancer, kidney disease, and high-cholesterol with COVID-19 disease severity and fatality: A systematic review,” Diabetes & Metabolic Syndrome: Clinical Research & Reviews, vol. 14, no. 5, pp. 1133–1142. [Google Scholar]
66. Z. Wu and M. M. Jennifer. (2020). “Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: Summary of a report of 72 314 cases from the Chinese center for disease control and prevention,” JAMA, vol. 323, no. 13, pp. 1239–1242. [Google Scholar]
67. T. Guo, Y. Fan, M. Chen, X. Wu, L. Zhang et al. (2020). , “Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19),” JAMA Cardiology, vol. 5, no. 7, pp. 811–818. [Google Scholar]
68. N. Chen, M. Zhou, X. Dong, J. Qu, F. Gong et al. (2020). , “Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: A descriptive study,” Lancet, vol. 395, no. 10223, pp. 507–513. [Google Scholar]
69. D. Wang, B. Hu, C. Hu, F. Zhu, X. Liu et al. (2020). , “Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, Chinaa,” JAMA, vol. 323, no. 11, pp. 1061–1069. [Google Scholar]
70. Q. Ruan, K. Yang, W. Wang, L. Jiang and J. Song. (2020). “Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China,” Intensive Care Medicine, vol. 46, no. 5, pp. 846–848. [Google Scholar]
71. C. Chen, J. T. Yan, N. Zhou, J. P. Zhao and D. W. Wang. (2020). “Analysis of myocardial injury in patients with COVID-19 and association between concomitant cardiovascular diseases and severity of COVID-19,” Chinese Journal of Cardiovascular Disease, vol. 48, pp. 567–571. [Google Scholar]
72. F. Zhou, T. Yu, R. Du, G. Fan, Y. Liu et al. (2020). , “Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study,” Lancet, vol. 395, no. 10229, pp. 1054–1062. [Google Scholar]
73. Lazzerini M. and Putoto G. (2020). “COVID-19 in Italy: Momentous decisions and many uncertainties,” Lancet Global Health, vol. 8, no. 5, pp. 641–642. [Google Scholar]
74. L. Fratino, P. Giuseppe, D. M. Massimo, C. Saverio, L. Silvana et al. (2020). , “Coronavirus: Older persons with cancer in Italy in the COVID-19 pandemic,” Frontiers in Oncology, vol. 10, pp. 648. [Google Scholar]
75. P. Li, L. Chen, Z. Liu, J. Pan, D. Zhou et al. (2020). , “Clinical features and short-term outcomes of elderly patients with COVID-19,” International Journal of Infectious Diseases, vol. 97, pp. 245–250. [Google Scholar]
76. G. Sacco, F. Gonzague, B. Olivier and A. Cédric. (2020). “COVID-19 in seniors: Findings and lessons from mass screening in a nursing home,” Maturitas, vol. 141, pp. 46–52. [Google Scholar]
77. M. Nikpouraghdam, A. J. Farahani, G. Alishiri, S. Heydari, M. Ebrahimnia et al. (2020). , “Epidemiological characteristics of coronavirus disease 2019 (COVID-19) patients in IRAN: A single center study,” Journal of Clinical Virology, vol. 127, pp. 104378. [Google Scholar]
78. M. Alkhouli, A. Nanjundappa, F. Annie, M. C. Bates and D. L. Bhatt. (2020). “Sex differences in COVID-19 case fatality rate: Insights from a multinational registry,” Mayo Clinic Proceedings, vol. 95, no. 8, pp. 1613–1620. [Google Scholar]
79. G. Bruno, S. Perelli, C. Fabrizio and G. B. Buccoliero. (2020). “Short-term outcomes in individuals aged 75 or older with severe coronavirus disease (COVID-19First observations from an infectious diseases unit in Southern Italy,” Journal of Infection, vol. 81, no. 2, pp. 86–88. [Google Scholar]
80. S. Richardson, J. S. Hirsch, M. Narasimhan, M. J. Crawford, T. McGinn et al. (2020). , “Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York city area,” JAMA, vol. 323, no. 20, pp. 2052–2059. [Google Scholar]
81. K. Xu, Y. Chen, J. Yuan, P. Yi, C. Ding et al. (2020). , “Factors associated with prolonged viral RNA shedding in patients with COVID-19,” Clinical Infectious Diseases, vol. 71, no. 15, pp. 799–806. [Google Scholar]
82. Y. Cheng, R. Luo, K. Wang, M. Zhang, W. Wang et al. (2020). , “Kidney disease is associated with in-hospital death of patients with COVID-19,” Kidney International, vol. 97, no. 5, pp. 829–838. [Google Scholar]
83. P. Mo, Y. Xing, Y. Xiao, L. Deng, Q. Zhao et al. (2020). , “Clinical characteristics of refractory COVID-19 pneumonia in Wuhan, China,” Clinical Infectious Diseases, . Ahead of print, https://doi.org/10.1093/cid/ciaa270. [Google Scholar]
84. K. I. Zheng, F. Gao, X. B. Wang, Q. F. Sun, K. H. Pan et al. (2020). , “Obesity as a risk factor for greater severity of COVID-19 in patients with metabolic associated fatty liver disease,” Metabolism-clinical and Experimental, vol. 108, pp. 154244. [Google Scholar]
85. L. Wang, W. He, X. Yu, D. Hu, M. Bao et al. (2020). , “Coronavirus disease 2019 in elderly patients: Characteristics and prognostic factors based on 4-week follow-up,” Journal of Infection, vol. 80, no. 6, pp. 639–645. [Google Scholar]
86. S. Ahmad. (2020). “Potential of age distribution profiles for the prediction of COVID-19 infection origin in a patient group,” Informatics in Medicine Unlocked, vol. 20, pp. 100364. [Google Scholar]
87. G. Grasselli, Z. Zangrillo, A. Zanella, M. Antonelli, L. Cabrini et al. (2020). , “Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy region, Italy,” JAMA, vol. 323, no. 16, pp. 1574–1581. [Google Scholar]
88. S. Rozenberg, J. Vandromme and C. Martin. (2020). “Are we equal in adversity? Does Covid-19 affect women and men differently?,” Maturitas, vol. 138, pp. 62–68. [Google Scholar]
89. Y. Ma, Q. N. Xu, F. L. Wang, W. M. Ma, X. Y. Wang et al. (2020). , “Characteristics of asymptomatic patients with SARS-CoV-2 infection in Jinan, China,” Microbes and Infection, vol. 22, no. 4–5, pp. 212–217. [Google Scholar]
90. J. M. Jin, P. Bai, W. He, F. Wu, X. F. Liu et al. (2020). , “Gender differences in patients with COVID-19: Focus on severity and mortality,” Frontiers in Public Health, vol. 8, pp. 152. [Google Scholar]
91. A. Dangis, N. D. Brucker, A. Heremans, M. Gillis, J. Frans et al. (2020). , “Impact of gender on extent of lung injury in COVID-19,” Clinical Radiology, vol. 75, no. 7, pp. 554–556. [Google Scholar]
92. R. Liu, H. Han, F. Liu, Z. Lv, K. Wu et al. (2020). , “Positive rate of RT-PCR detection of SARS-CoV-2 infection in 4880 cases from one hospital in Wuhan, China, from Jan to Feb 2020,” Clinica Chimica Acta, vol. 505, pp. 172–175. [Google Scholar]
93. S. Singh, C. Monica, C. Arka and K. Ahmad. (2020). “Gender-based disparities in COVID-19: Clinical characteristics and propensity-matched analysis of outcomes,” medRxiv, . Preprint, https://doi.org/10.1101/2020.04.24.20. [Google Scholar]
94. P. K. Bhatraju, B. J. Ghassemieh, M. Nichols, R. Kim, K. R. Jerome et al. (2020). , “COVID-19 in critically ill patients in the Seattle region—Case series,” New England Journal of Medicine, vol. 382, no. 21, pp. 2012–2022. [Google Scholar]
95. C. Wenham, J. Smith and R. Morgan. (2020). “COVID-19: The gendered impacts of the outbreak,” Lancet, vol. 395, no. 10227, pp. 846–848. [Google Scholar]
96. S. Hernandez, M. Carlos and M. Z. Efren. (2020). “Statistics associated with the lethality of COVID-19 by age group and gender in Mexico,” medRxiv, . Preprint, https://doi.org/10.1101/2020.06.28.20142117. [Google Scholar]
97. Y. Wang, B. Pan, Y. Liu, A. Wilson, J. Ou et al. (2020). , “Health care and mental health challenges for transgender individuals during the COVID-19 pandemic,” Lancet Diabetes & Endocrinology, vol. 8, no. 7, pp. 564–565. [Google Scholar]
98. J. L. Herman and K. O’Neill. (2020). “Vulnerabilities to COVID-19 among transgender adults in the US,” . [Online]. Available: https://escholarship.org/content/qt55t297mc/qt55t297mc.pdf. [Google Scholar]
99. G. Gonzales, E. L. de Mola, K. A. Gavulic, T. McKay and C. Purcell. (2020). “Mental health needs among lesbian, gay, bisexual, and transgender college students during the COVID-19 pandemic,” Journal of Adolescent Health, vol. 67, no. 5, pp. 645–648. [Google Scholar]
100. A. F. Lopes de Sousa, H. E. F. D. Carvalho, L. B. D. Oliveira, G. Schneider, E. L. S. Camargo et al. (2020). , “Effects of COVID-19 infection during pregnancy and neonatal prognosis: What is the evidence?,” International Journal of Environmental Research and Public Health, vol. 17, no. 11, pp. 4176. [Google Scholar]
101. Y. Wu, Z. Feng, P. Li and Q. Yu. (2020). “Relationship between ABO blood group distribution and clinical characteristics in patients with COVID-19,” Clinica Chimica Acta, vol. 509, pp. 220–223. [Google Scholar]
102. J. B. Galloway, S. Norton, R. D. Barker, A. Brooks, I. Carey et al. (2020). , “A clinical risk score to identify patients with COVID-19 at high risk of critical care admission or death: An observational cohort study,” Journal of Infection, vol. 81, no. 2, pp. 282–288. [Google Scholar]
103. G. Onder, R. Giovanni and B. Silvio. (2020). “Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy,” JAMA, vol. 323, no. 18, pp. 1775–1776. [Google Scholar]
104. L. Q. Li, Y. Q. Wang, Z. P. Wang, Y. Liang, T. B. Hung et al. (2020). , “COVID-19 patients’ clinical characteristics, discharge rate, and fatality rate of meta-analysis,” Journal of Medical Virology, vol. 92, no. 6, pp. 577–583. [Google Scholar]
105. G. Deiana, A. Azara, M. Dettori, F. Delogu, G. Vargiu et al. (2020). , “Deaths in SARS-Cov-2 positive patients in Italy: The influence of underlying health conditions on lethality,” International Journal of Environmental Research and Public Health, vol. 17, no. 12, pp. 4450. [Google Scholar]
106. D. J. Lundon, B. D. Kelly, S. Nair, D. M. Bolton, N. Kyprianou et al. (2020). , “Early mortality risk stratification after SARS-CoV-2 infection,” Medicina Intensive, . Ahead of print, https://doi.org/10.1016/j.medin.2020.06.011. [Google Scholar]
107. C. Chen, H. Wang, Z. Liang, L. Peng, F. Zhao et al. (2020). , “Predicting illness severity and short-term outcomes of COVID-19: A retrospective cohort study in China,” Innovation, vol. 1, no. 1, pp. 1–9. [Google Scholar]
108. J. K. Dey and S. K. Dey. (2020). “SARS-CoV-2 pandemic, COVID-19 case fatality rates and deaths per million population in India,” Journal of Bioinformatics, Computational and Systems Biology, vol. 2, no. 1, pp. 110. [Google Scholar]
109. A. Banerjee, L. Pasea, S. Harris, A. Gonzalez-Izquierdo and A. Torralbo. (2020). “Estimating excess 1-year mortality associated with the COVID-19 pandemic according to underlying conditions and age: A population-based cohort study,” Lancet, vol. 395, no. 10238, pp. 1715–1725. [Google Scholar]
110. F. Öztoprak and J. Aadil. (2020). “Case fatality rate estimation of COVID-19 for European countries: Turkey’s current scenario amidst a global pandemic, comparison of outbreaks with European countries,” European Journal of Medicine and Oncology, vol. 4, no. 2, pp. 149–159. [Google Scholar]
111. A. Basu. (2020). “Estimating the infection fatality rate among symptomatic COVID-19 cases in the United States: Study estimates the COVID-19 infection fatality rate at the US county level,” Health Affairs, vol. 39, no. 7, pp. 10–15. [Google Scholar]
112. L. Roques, K. K. Etienne, P. Julien, S. Antoine and S. Samuel. (2020). “Using early data to estimate the actual infection fatality ratio from COVID-19 in France,” Biology, vol. 9, no. 5, pp. 97. [Google Scholar]
113. L. F. Moriarty. (2020). “Public health responses to COVID-19 outbreaks on cruise ships—Worldwide, February–March 2020,” Morbidity and Mortality Weekly Report, vol. 69, no. 12, pp. 347–352. [Google Scholar]
114. J. P. Ioannidis, C. Sally and A. T. Martin. (2020). “Forecasting for COVID-19 has failed,” International Journal of Forecasting, . In press, https://doi.org/10.1016/j.ijforecast.2020.08.004. [Google Scholar]
115. A. M. Mandal. (2020). “Case fatality rate alone may be a misleading measure of overall COVID-19 mortality,” . Available: https://www.news-medical.net/news/20200729/Case-Fatality-Rate-alone-may-be-amisleading-measure-of-overall-COVID-19-mortality.aspx. [Google Scholar]
 | This work is licensed under a Creative Commons Attribution 4.0 International License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. |