DOI:10.32604/cmc.2020.013261
| Computers, Materials & Continua DOI:10.32604/cmc.2020.013261 | 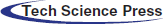 |
| Article |
Emergency Prioritized and Congestion Handling Protocol for Medical Internet of Things
Information Technology Department, Faculty of Computing and Information Technology, King Abdulaziz University, Jeddah, 21589, Saudi Arabia
*Corresponding Author: Sabeen Tahir. Email: stsheikh@kau.edu.sa
Received: 31 July 2020; Accepted: 11 September 2020
Abstract: Medical Internet of Things (MIoTs) is a collection of small and energy-efficient wireless sensor devices that monitor the patient’s body. The healthcare networks transmit continuous data monitoring for the patients to survive them independently. There are many improvements in MIoTs, but still, there are critical issues that might affect the Quality of Service (QoS) of a network. Congestion handling is one of the critical factors that directly affect the QoS of the network. The congestion in MIoT can cause more energy consumption, delay, and important data loss. If a patient has an emergency, then the life-critical signals must transmit with minimum latency. During emergencies, the MIoTs have to monitor the patients continuously and transmit data (e.g., ECG, BP, heart rate, etc.) with minimum delay. Therefore, there is an efficient technique required that can transmit emergency data of high-risk patients to the medical staff on time with maximum reliability. The main objective of this research is to monitor and transmit the patient’s real-time data efficiently and to prioritize the emergency data. In this paper, Emergency Prioritized and Congestion Handling Protocol for Medical IoTs (EPCP_MIoT) is proposed that efficiently monitors the patients and overcome the congestion by enabling different monitoring modes. Whereas the emergency data transmissions are prioritized and transmit at SIFS time. The proposed technique is implemented and compared with the previous technique, the comparison results show that the proposed technique outperforms the previous techniques in terms of network throughput, end to end delay, energy consumption, and packet loss ratio.
Keywords: Congestion control; MIoTs; emergency prioritization; energy-efficient
With the rapid developments of wireless transmissions, the area of wireless sensor networks has grown-up significantly supporting a range of wireless applications including healthcare systems [1]. A MIoTs creates a special purpose wireless network designed to function separately to connect different medical sensors and applications placed outside or inside of the patients’ body. The introduction of MIoTs for Biomonitoring will offer flexibility and cost-saving opportunities for both medical professionals and patients. The MIoTs network offers significant advantages like patients’ mobility due to portable monitoring applications and location-independent monitoring capability. A MIoT device being an independent device can locate the relevant network and transmit information to the remote databases for further processing. Current developments in wireless-enabled networking play an important role in the modification of sensor networking. As sensors are used for monitoring, controlling, and transmitting updates about the environments. These wireless technology-enabled sensors to lead in the medical industry, especially the Medical IoTs. New scientific developments in sensors, wireless connections, and biological sensing invent tiny, lightweight, ultra-low power, quick, and intelligent observing devices.
A WBAN consists of low power, lightweight, and intelligent sensor devices that monitor the patient’s health monitoring systems. These medical sensors provide continuous monitoring and real-time response to the user or physician. After sensing and collecting the data, sensors are responsible for the processing i.e., data abstraction, amplification, digitization, etc. and then forward to the coordinator device through wireless connections [2]. A coordinator device itself can be a sensor or aggregating device and in a few applications, it is found as an access point. These sensor devices are designed to decrease the delay and increase data accuracy and record. MIoTs has modernized the medical systems. However, these systems are still having some challenges regarding network topology, accurate data delivery, resource consumption, etc. Generally, a MIoTs consists of medical sensors and actuators, sensors are used to monitor internal or external body parameters like measurement of temperature, heartbeat, electrocardiogram (ECG), etc. The actuators are responsible to take necessary actions on sensed data according to the requirement or through user interaction where a smart device controls the user interaction, for example, an actuator equipped with a pump of insulin doses.
MIoTs considers different health parameters like Blood Pressure (BP), Body Temperature (T), glucose (G), Cholesterol (Ch), Electrocardiogram (ECG), Electromyography (EMG), Heart Rate (HR). BP is the amount of the force of blood pushing against blood vessels. The heart pumps blood into the blood vessels, which transport blood throughout the body. When a heart beats, it squeezes and pushes the blood through arteries to the whole body that creates pressure on the blood vessels. This pressure is called systolic pressure; its normal value is below 120. The pressure in the arteries when the heart rests between beats (during this time heart gets oxygen and full blood) called diastolic pressure. The normal value of diastolic pressure is below 80. Body temperature is a measurement of the body’s capability to produce and get rid of heat. It can be checked from the forehead, armpit, mouth, or ear. The normal temperature value is 98.6°F (37°C) [3], the BP stages are shown in Tab. 1 [4].
Table 1: Stages of blood pressure
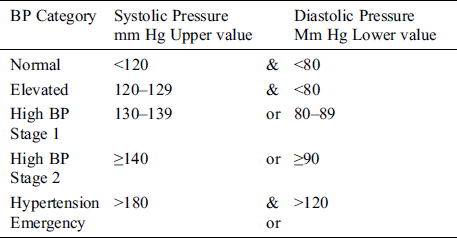
An ECG is a diagnostic apparatus, normally used to measure the heart functions. It checks your heart’s rhythm and electrical activity. Sensors attached to the skin detect the electrical signals produced by the heart each time it beats. The readings of an ECG on standard paper lets the time taken for the many stages of electrical depolarization to be measured in milliseconds. Normal range up to 440 ms (though varying with heart rate and may be slightly longer in females) [4,5]. Electromyography (EMG) is an Electrodiagnostic medication used to observing the electrical activities produced by skeletal muscles. This process is completed by electromyography that creates a record known as an electromyogram. Electromyography senses the electric potential created by muscle cells when these are neurologically started. The signals can be analyzed to sense medical irregularities, activation level, or to examine the biomechanics of body movement. Wireless sensor devices can be either wearable or implanted into a patient’s body. The WBAN communications can be characterized into three groups. The first group is Intra-body communication that manages the data handling of the body between sensors, actuators, and coordinator devices. The second group is Extra-body communications that confirm the communication links between WBAN and relevant networks. The final group is an inter-body communication system that deals with the data exchange between other WBANs. WBAN communication systems can be used in hospitals, aeroplanes, spaceships, at homes, babies monitoring an athlete, and sports analysis. BANs can provide interfaces for diagnostics, for remote monitoring of patients’ healthcare data, for the administration of medications in clinics/hospitals, and as an assistant to rehabilitation. A general layout of WBAN is described in Fig. 1.
Figure 1: A general layout of WBAN
The devices used in MIoTs have different sampling frequencies, high sampling frequency devices include accelerometers, electrocardiograms, electroencephalography, and electromyography. Low sampling frequency devices include carbon dioxide sensors, blood pressure sensors, and temperature sensors, etc. In a MIoT network, all the devices should get equal access to the network resources regardless of their sampling frequency. In MIoTs, data congestion and packet loss directly affect the Quality of Service QoS of the whole network. Due to the data congestion, the packet loss rate and latency increase and the system require more energy for data retransmission. In the MIoTs network, it is highly required to detect the congestion and avoid it before an emergency occurs [6,7].
As compared to the wireless sensor networks and ad-hoc networks, the MIoT network has some unique characteristics. In MIoTs most of the devices are battery-driven and they have no chance to replace or recharge the battery during their whole lifetime. Therefore, computation power, energy, and storage constraints are very limited. Ultra-low transmit power: To overcome the negative effect of the electromagnetic radiations and fulfil the necessities of the planned monitoring ratio, ultra-low transmit power is required. Frequent change of network topology: Due to the patients’ movement, the sensors or other relevant devices also moves that ultimately change the topology frequently. As the sensor devices are scattered, so these devices must be capable to efficiently monitor and gather the data, process it, and finally transmit to the coordinator device. The sensor devices normally monitor the data according to the predefined query-based, continuously, or event-based operations. The Dynamic QoS Requirements: with the heterogeneous data, MIoT networks need to support different QoS requirements. Usually, medical data can accept delays for monitoring data with fewer duty cycles. On the contrary, if there is an emergency then the life-critical signals along with the monitored data must transmit with the minimum delay.
During emergencies, medical sensors can collect a lot of information (e.g., ECG, BP, heart rate, etc.) and transmit to the respective medical staff through intermediate devices for further assistance. A load of continuous incoming data would create congestion that is related to packet loss, end-to-end delay, energy consumption, etc. The main concerns in medication are how to send the critical data information of high-risk patients to the physicians on time with high reliability using tiny sensors having a limited battery life [8–10]. What will happen, if a sensor’s battery dies, breakdowns or data packets get lost and a patient could not get the medication on time. This is one of the main reasons for congestion control in medical networks to be critical. Since the monitored data are important and sensitive, therefore it is essential to avoid data congestion because data containing medical information are directly linked to the patients’ life and wellbeing. In most of the existing congestion handling protocols, data transmission is minimized after the congestion is predicted. However, in the healthcare systems, it is harmful to minimize the data streams related to vital signs. Therefore, it is highly required to propose a congestion control technique for MIoTs concerning the relevant features and requirements. To cope with the MIoT networks, several functional and structural requirements need to be mentioned. The MIoT related issues in designing a remote cloud-based health care structure are network security, heterogeneity, network interoperability, interference reduction, scalability and data verification and authentication [11–13]. The purpose of this study is to enhance the efficacy of the MIoT network by handling the congestion and emergency. In this paper, a reliable and self-configurable MIoT protocol is described that integrates MIoTs with cloud computing for healthcare data sharing with respective medical staff and patients.
The rest of the paper structure is as follows: Section 2 will describe the related work of MIoTs. Section 3 elaborates on the proposed Emergency Prioritized and Congestion Handling Protocol for Medical IoTs (EPCP_MIoT). Section 4 describes the obtained simulation results and analysis. Finally, Section 5 presents the conclusions.
The amount of congestion control techniques has been proposed for MIoT networks. Congestion arises due to the heavy data load on a single device or a single link. During this situation, the network cannot manage more data than its predefined load capacity because of insufficient memory, slow processor, frequency contention, interference, and a burst of data traffic. If the data transmission rate of a sender device becomes higher than the receiver’s data processing ability, the network will become congested. The congestion concerns are data loss, queuing delay, bottleneck, reduction of network throughput, energy consumption, network lifetime, etc.
To overcome congestion, many congestion control techniques have been implemented, but there is still a need to enhance the features of these techniques. Due to energy constraints, WBAN sensors may not be capable to communicate with the coordinator device directly even the nodes are in the proximity of that device. If the devices will retransmit data, the process will consume more energy. An energy-efficient peering routing protocol is proposed for the indoor hospital environment. It calculates the communication cost for all neighbouring devices of a device and it constructs the routing table using communication cost. QoS aware peering routing protocol for reliability sensitive data [14] is a routing protocol for indoor WBAN. It calculates the reliability of all the paths between sources to the destination, and choose a path based on the QoS requirements. One more WBAN congestion control technique based on fuzzy logic proposed in Khan et al. [15], is detecting congestion by considering the local information of memory capacity and device rate. It distinguishes vital signals and ascribes priorities to them based on their status during congestion.
A fuzzy priority-based congestion control scheme in wireless body area networks (FPBCC) proposed in Gambhir et al. [16]. This protocol includes several biosensors to observe the patients and send the information to the remote data centre. This protocol is related to the Random Early Detection (RED) and active queue management techniques, it utilizes two single out of the fuzzy logic system to modify the drop maximum probability factor of the RED algorithm then it elevates the congestion of each sensor by utilizing two thresholds maximum and minimum. A fuzzy logic control based on the child device’s data load is used to adjust the transmission rate of the parent device. It includes three phases, in the first phase, a two-input-single-output fuzzy logic scheme manages a maximum drop probability factor for the RED algorithm, and input values are the typical queue size and its variations. Then two adaptive thresholds are utilized to determine the data congestion of each device. In case of congestion in the second phase, then it sends a notification named Implicit Congestion Notification (ICN). It uses a fuzzy logic controller with two input variables; transmit error rate and error variation. To optimize the transmission rate of each sensor device, it manages the traffic load parameter. The issue with FPBCC is routing of data, as its mentioned in the paper that all the sensors are connected to their coordinator devices probably their smart devices. As a whole network scenario, all the coordinator devices are further connected to all other available coordinator devices and then reach to the sink node. It means they created the link hop by hop, the link from sensors to the sink pass by many coordinator devices. This technique efficiently manages the traffic load but increases the delay and energy consumption of intermediate devices [17]. A Prioritization Based Congestion Control Protocol for Healthcare Monitoring Application in Wireless Sensor Networks is proposed (PBCCP) [18] that supports patient monitoring based on three scenarios. There are many biological signals, some of them are more critical and important. PBCCP uses service prioritization and grouped the vital signs into different classes. The intermediate computing device of the monitoring system gets medical data from all patients and shows the capability to analyze the data. If there is an anomaly detected in receiving data, it transmits a special message to the wireless device of the patient and allocates the high priority. Therefore, the data will be received on a priority basis at the intermediate device. It is predicted that different patients have different medical records in the system. Suppose a patient needs special care, that patient will be assigned high priority. In the monitoring system, PBCCP considers three health conditions for each patient normal, urgent, and critical. Patients having an urgent or critical condition will consume more network bandwidth than normal patients. The issue with this technique is, it continuously analyzes the system for anomaly detection and transmits a special message in case of anomaly detected. The other issue with this technique is, it did not set any monitoring modes to overcome energy consumption and decreasing the delay. It sets the priority for two types of patients which continually monitoring the patients and consumes resources.
Many types of MIoT systems have been proposed and implemented to handle different parameters like energy optimization, congestion, and delay [19]. There are still many points left to fulfil the requirements of MIoTs as challenging issues. The first requirement is the immediate transmission of emergency data. Most of the research focused on energy optimization and end to end delay but they did not overcome the issue of emergency data transmission on a priority basis. The other essential requirement for MIoT is the energy balance between sensors and coordinator devices [20,21]. Most available smart devices (smartphones, smartwatches, and wrist bands, etc.) mostly play the role of coordinator device in MIoT networks because they have enough battery resources than the sensor devices. The batteries of coordinator devices can be rechargeable whereas it is quite difficult to recharge the medical sensors especially the implanted sensors. IEEE802.15.6 standard technology uses a CSMA-based mechanism when transmitting emergency data from medical sensors [22–25].
The proposed technique is well-organized and an efficient technique, the network created by the MIoT devices is positioned on or near the patient’s body. Regarding channel quality, this has serious consequences. The employment of sensors on the patient’s body as well as the link to the other devices has a great impact on the quality of the channel. Sensors are small; therefore, the energy consumption is very limited. Radio consumed most of the sensor’s energy; MIoT protocols should consider the poor channel quality. To overcome the energy issues, sensors should enable different modes like sleep awake, etc.
3 The Proposed Emergency Prioritized and Congestion Handling Protocol for Medical IoTs
A remote healthcare structure requires an efficient, real-time, secure, and reliable service that makes patients’ life easy. The data sensing speed, retrieving, processing, and routing are the critical issues that degrade the performance of a system. During an emergency, a system is highly required to transmit accurately sensed data frequently in the smallest possible periods. For intelligent monitoring, low power, lightweight and small monitoring sensors are used in the proposed technique. These sensors are assigned different sensing modes based on the patient’s condition. Sensors collect the monitored data and forward it to the corresponding physician.
The proposed technique is a well-organized congestion handling technique for the MIoT environment. Suppose there are Med_S = {Med_S1, Med_S2,…, Med_Sn} Medical Sensors, which are implanted, wearable, or patchable with the patient’s body. In the proposed technique, first of all, a patient must register with the medical system and is assigned a Patient identification (P_id), Medical Sensor’s Code, and associated Physician Team abbreviated as (P_id, Med_S-Co, Ph_T). From a body-sensing point of view, a symptom has symbolized by using three variables (Sid, Vmax, Vmin). Where Sid is symptom id, Vmax is the symptom’s maximum value and Vmin is the symptom’s minimum value. It is defined, that each Med_S monitors its unique health parameter for its corresponding disease. All the notations used in the proposed work are defined in Tab. 2. Eq. (1) denotes medical sensor Med_Si only measures one correspondent health parameter for a specific disease. Whereas Eq. (2) describes the emergency status.
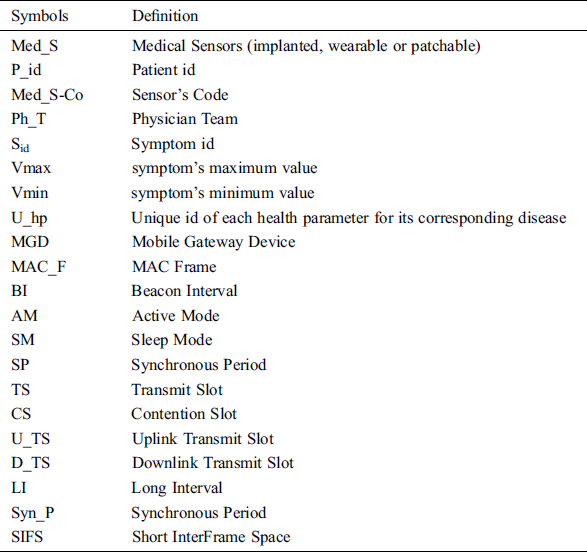


There are two modes of communications, local mode, and foreign mode, the local mode displays the entire data received from the MIoTs through the Bluetooth links. The foreign model is like a bridge between MIoTs and MGD. An android based MGD receives the monitored data updates after every 100 milliseconds and then filters it. An MGD receives the data from many connected MIoTs, and transmit it to the MCS for further processing. Where MCS can show the obtained results to the relevant physician and patients. MCS authenticates the users based on their registration information. Once the user authentication process is accomplished, the user can receive and transmit new data. Common users are patient, doctors, or any other authorized people. These users can access the data anytime from anyplace.
The main function of medical sensors is to monitor the body and collect vital signals. To handle the data congestion in medical systems, it is highly required to focus on many to one communication like many sensors to one coordinate device. In MIoT, two types of congestion may arise called device level and connection level. Device-level congestion occurs due to buffer overflow, where the data entrance rate is more than the data service rate. Congestion in connection-level occurs when several devices access a single wireless link at the same time. To handle the device congestion, the proposed technique sets different modes of data monitoring and processing (continuous monitoring mode, periodic monitoring mode, and on-demand monitoring mode). These monitoring modes are set according to the patient’s condition. Continuous monitoring executes when intensive monitoring of patients is required. During this mode, sensors continuously monitor and collect vital data information. The on-request monitoring process is executed based on requests from authorized users. The third monitoring mode is periodic monitoring that is based on the defined start and end time from the authorized system controller. As the signal from patients’ body is usually weak and combined with unwanted interference, therefore sensors upon receiving the signal must perform an amplification and filtering process. The amplification and filtering process removes the interference and increases signal strength. For example, an EMG signal is weak and contains unwanted noise. It needs to be carefully processed before using it for health monitoring. The amplification and filtering process to minimize unwanted noise components. This process maximizes the signal to noise ratio and minimizes signal distortion.
According to the proposed technique, all active Med_S(s) are connected with an MGD that receives the data from sensors and manage accordingly. An MGD consist of three important segments; data abstraction, classification, and prioritization. The data abstraction module extracts the essential medical data. As during the link establishment and communication, devices also transmit control messages to each other to make sure about their accurate functioning. In the classification process, data are entered in the relevant health parameters. Health parameters are different diseases like Blood Pressure (BP), Body Temperature (T), glucose Level (GL), Cholesterol (Ch), Electrocardiogram (ECG), Electromyography (EMG), and Heart Rate (HR). In prioritization, important vital signals for different data types (ECG, BP, EMG, GL, and T) concerning their priority level among the different number of devices are considered. The highest priority level is allocated to the heart rate signal, the second-highest priority is allocated to blood pressure, EMG and glucose are assigned third and fourth priority levels, and less priority is assigned to temperature. These priority levels can be changed based on the patients’ condition. In Fig. 2, each data type has its separate queue and each incoming data packet is routed to its corresponding sub-queue using a traffic class identifier located in MGD. The information about the health parameter is set in the header of the packet, and data is forwarded to the MAC layer based on priority levels using a weighted fair queuing scheduler. Each MGD is further connected to the Medical Cloud System (MDC). MGDs have interfaces through which patients and users can transmit their personal and medical records to the MDC. The respective physicians, patients, and hospital management can access the data anytime. Authentication and verification of users are required each time to access the MDC. The main requirement of MDC is, the data should be accurate and transmitted on time. It is possible when the whole system’s throughput is high, less congestion, and minimum delay.
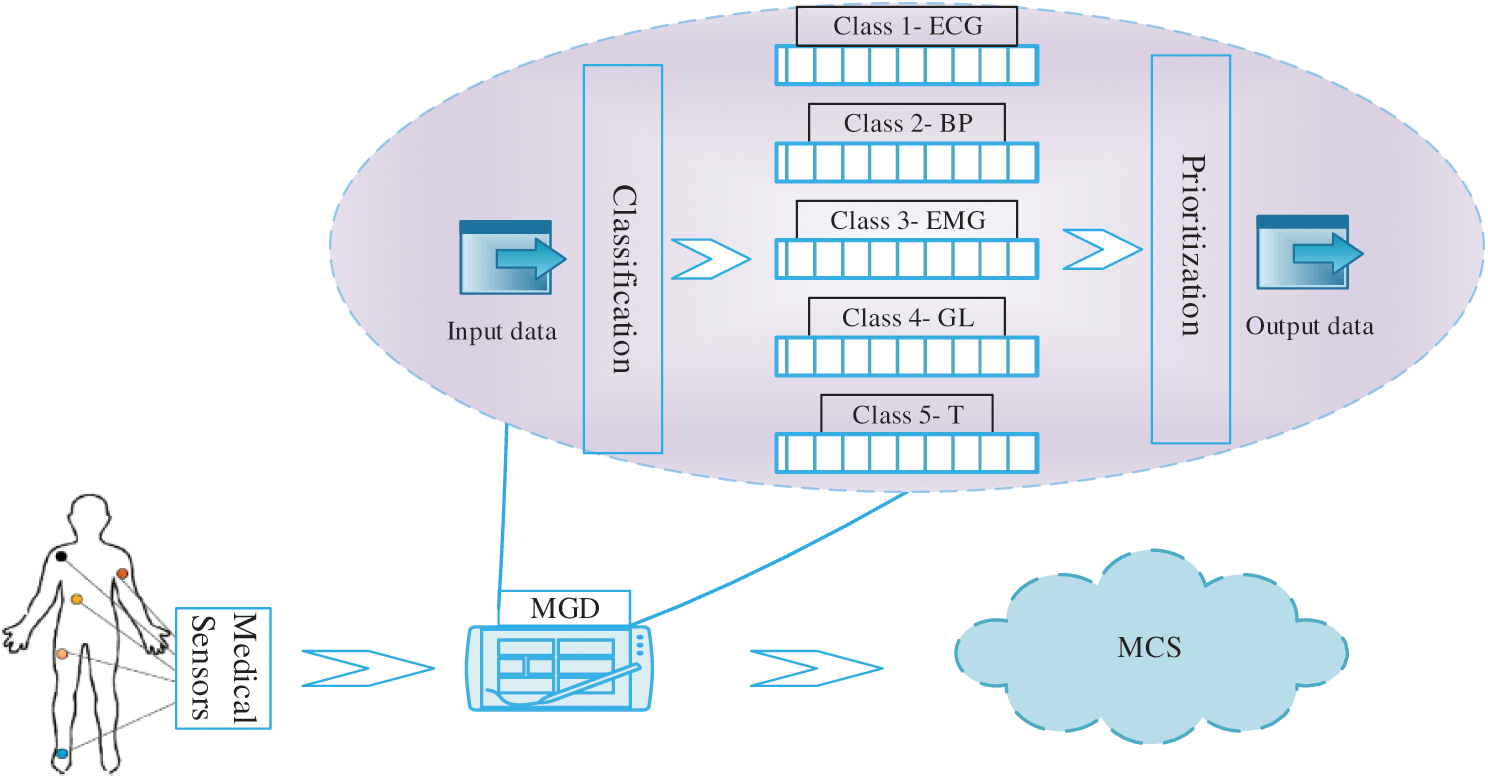
Figure 2: Data transmission, classification, and prioritization
In the beginning, the proposed technique enables different monitoring modes based on patients’ conditions. However, if sensors are continuously monitoring and sending data frequently to MGD, there can be data congestion on MGD. To handle the congestion, MGD performs classification and prioritization on receiving data. The MGD managed separate queues for all data types therefore in the classification process, incoming data stores according to the respective classes. In the prioritization process, data from all the classes are monitored. The highest priority is assigned to that class which crosses the threshold values. After passing by classification and prioritization, data is sent to the respective cloud system for further processing. In case of emergency, the cloud sends emergency alerts to the respective physicians. In the MIoT environment, it is highly required for immediate transmission of critical data when the patients are suffering from emergency conditions.
3.2 Emergency Data Prioritization and Transmission
An overall MAC Frame (MAC_F) structure is explained in Fig. 3, a superframe consists of MAC_F1 to MAC_Fn. Each single MAC_F consists of Beacon Interval (BI), Active Mode (AM), and Sleep Mode (SM). Moreover, each AM consisting of Synchronous Period (Syn_P), Transmit Slot (TS), and Contention Slot (CS). Furthermore, the TS composed of Uplink Transmit Slot (U_TS) and Downlink Transmit Slot (D_TS). The D_TS is denoted for the downlink transmission from MGD to the sensors whereas U_TS is the uplink transmission from the sensors to the MGD. An MGD creates a beacon packet and transmits to all connected sensors in a BI frame with Long Interval (LI). We used a default BI 650 ms. As each time frame consists of BI, AM, and SM, wherein radio frequency transceiver holds the options for the device’s sleep and wake up modes. There is no data transmission during the sleep mode. Sleep mode is effective to optimize the energy consumption. But there is a need to awake the device for data monitoring and transmission in case of any emergency condition. For example, a sensor transmits the data, and immediately after the transmission enables sleep mode. To synchronize each time frame between MGD and Med_S (s), the MGD periodically sends beacon packets. In case, if a sensor does not have any data to transmit, it has the option to neglect all forwarding frames and stay sleep.
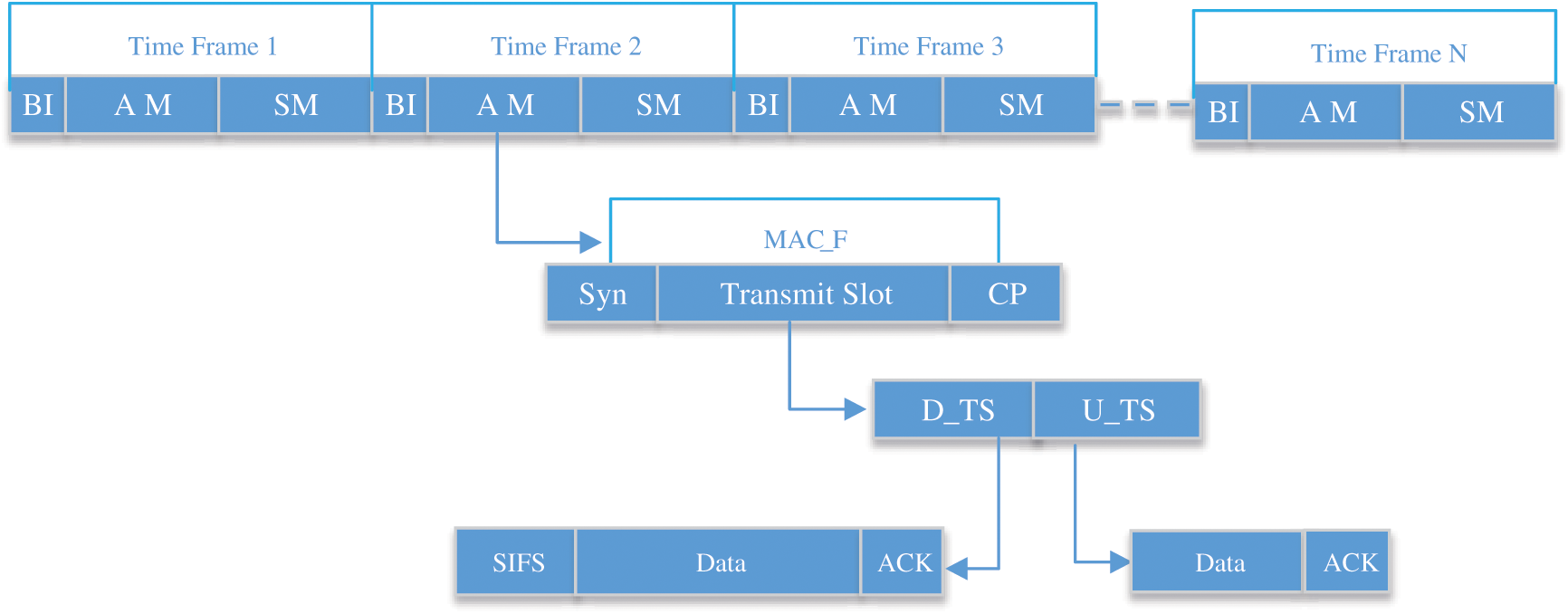
Figure 3: An overall MAC Frame (MAC_F) structure
The MGD transmits synchronous messages to the awaken sensors during the Syn_P slots that contain offset values for U_TS and D_TS, CS, and sleep mode. An MGD controls all the transmissions except CS. All Med_S(s) is dependent on the given instructions from an MGD and it has to decide which Med_S has to participate in the active slots. Med_S (s) in CSs are handled based on Carrier Sense Multiple Access/Collision Avoidance (CSMA/CA). In the case of the critical situation, the emergency data should be transmitted immediately without regard to the time frame matters. To priorities the emergency data, it should be transmitted in all time frames including sleep modes and contention slots. TS is allocated for the data transmission between devices (Med_S(s) to MGD, MGD to MCS). We have considered two-way transmissions U_TS and D_TS. D_TS let transmissions to be transmitted from MGD by using unicast or broadcast way. MGS can broadcast or send unicast data anytime, due to this way the Med_S(s) are not aware of when will they get the data or instructions.
The D_TS is composed of many slots including unicast and broadcast transmissions. The synchronous packet consists of all necessary information (receiver device address, transmission type, and time activation time). When a Syn_P received by a Med_S from its respective MGD, it can predict its sleep time and active time. Short InterFrame Space (SIFS) is included as shown in Fig. 4, it is the amount of the short time in microseconds needed for a wireless interface to process received frames and response with a response frame. The proposed work is utilized to support the prioritized emergency transmissions. U_TS also consists of many slots and distributed to all Med_S (s), during this state device does not have to be active. The Med_S(s) will be active after receiving the instructions based on their monitoring modes. Once the Med_S(s) get the activation slots’ information through synchronous packet they can access the assigned D_TS. If complete data is not transmitted during the D_TS, Med_S(s) can continue data transmission during CS(s). Received data and transmitted data are acknowledged through ACK packets during their respective transmissions. This whole process is collision-free; no data contention occurs. The D_TS(s) are utilized by MGD whereas U_TS(s) are utilized by the Med_S(s) for the transmission of monitored data.
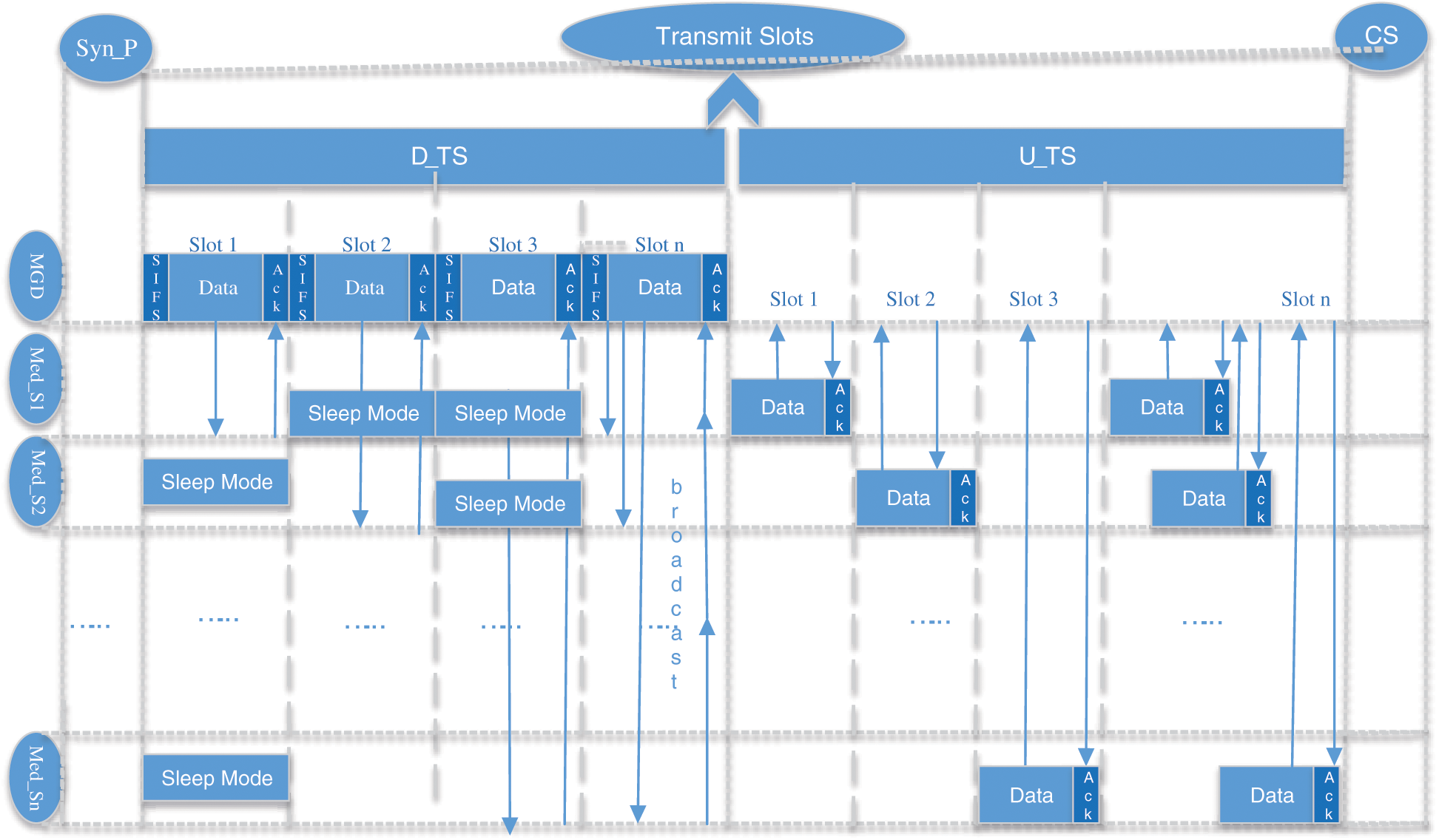
Figure 4: An active frame of transmission slot
Most of the time the data cannot be transmitted in one slot, so the leftover data is transmitted through the CS(s) from Med_S(s) to the MGD. In this period, devices can transmit the request for a new slot or request for the registration of new Med_S devices. As a whole, CS(s) allows transmissions including emergency data, control data packets for a new Med_S, remaining data packets, and for new uplink data. Whereas the transmissions in this duration are based on CSMA/CA. In case of emergency, we can reserve CS and transmit the data. In these transmissions, emergency data is prioritized. Same as others, data or requests during CS are acknowledged through negative or positive ACKs. As Med_S(s) are connected to the MGD and they have to transmit data to it, so after sending any type of requests or data they wait for ACKs from respective MGD. In Fig. 5, Suppose a new device has to send control messages to MGD, after receiving requests MGD will include it in its schedule and update other devices through the broadcast transmission. In case if an MGD is overloaded and it has to avoid congestion, it can discard the new device’s request by sending the negative ACK. The rejected devices can again try in the new beacon time.
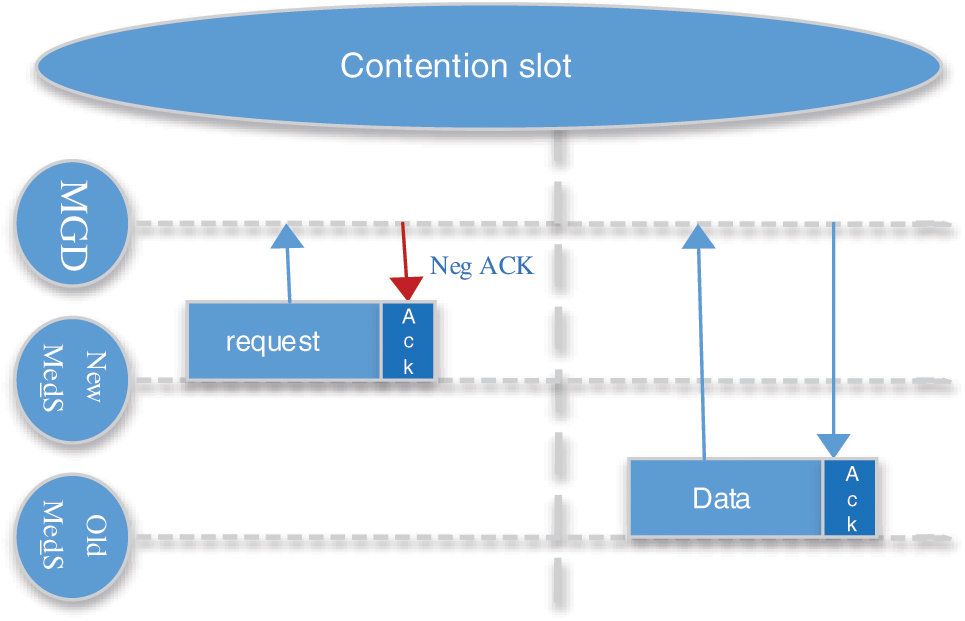
Figure 5: Transmission in contention slot
As a single time frame consists of BI, AM, and SM, SM is used for energy optimization. There is no normal data transmission during sleep mode only the emergency data can be transmitted. The MGD executes the duty cycle technique by switching SM and AM since the proposed technique adjusts emergency data transmission with the preservation of energy efficiency at many time frames. In medical networks, it the basic requirement to show minimum delay for the prompt delivery of emergency data. Emergency data is monitored due to the critical condition of the patients. In the proposed work, the emergency data is prioritized and can transmit anytime. It is depicted in Fig. 6, Med_Sn has emergency data in slot 1 during D_TS and U_TS for MGD. The system indicates data prioritization and starts immediate emergency data transmission through SIFS time even though Med_Sn is not assigned the time slots.
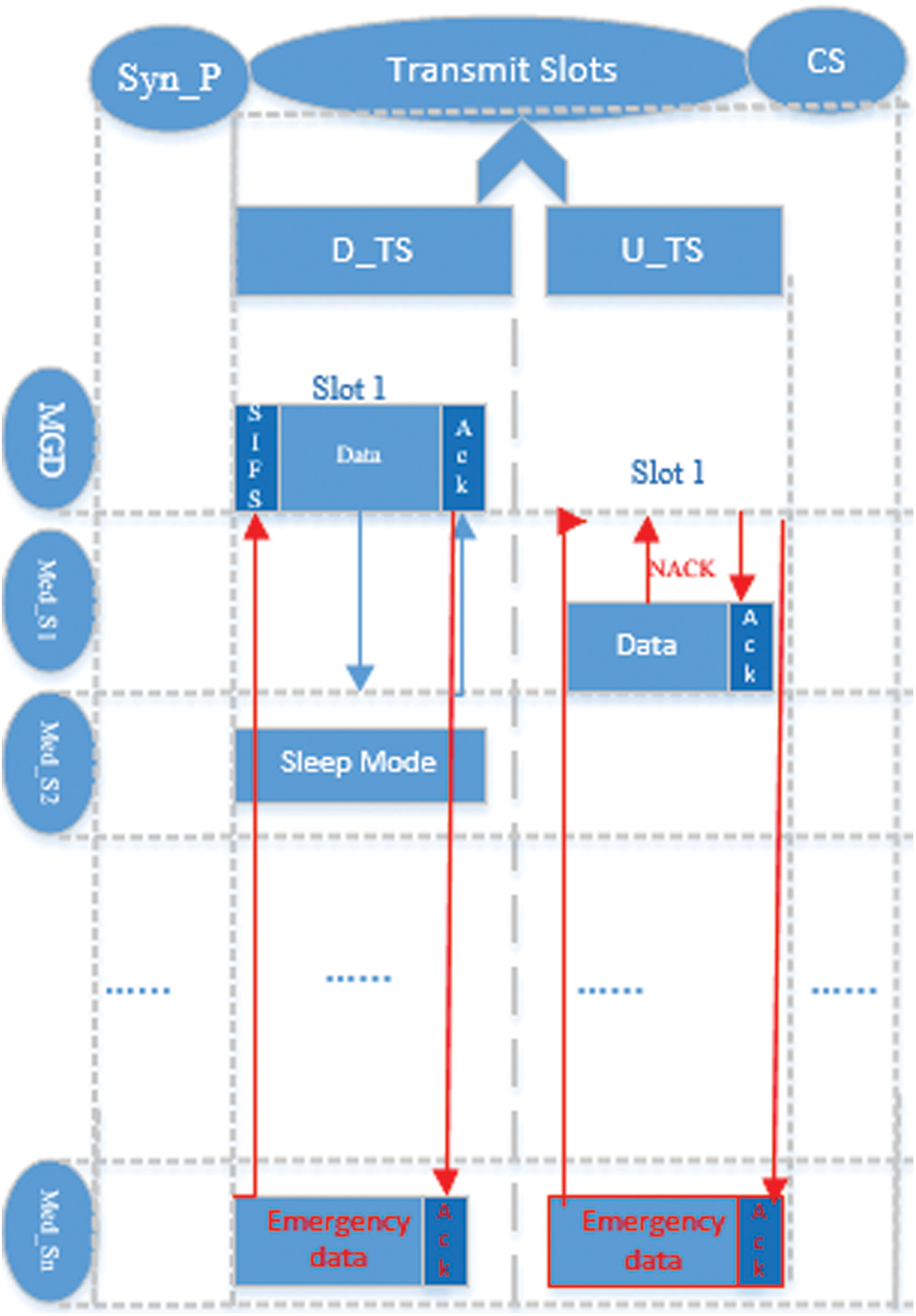
Figure 6: Emergency data transmission
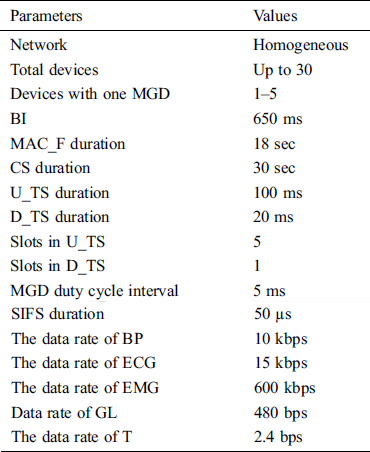
We have evaluated the performance of our proposed protocol EPCP_MIoT using simulators OPNET and MATLAB. The results are compared with a prioritization based congestion control protocol for healthcare monitoring application on a wireless sensor (PBCCP) and A fuzzy priority-based congestion control scheme in wireless body area networks (FPBCC). We have selected these two techniques because these are closely related to our technique. PBCCP is a congestion control protocol used for medical applications. According to this protocol, it monitors the patients’ real-time data. It uses a learning automata-based QAM mechanism at intermediary sensor devices to handle the congestion. This technique was assessed in terms of delay, packet loss, and queue length. The FPBCC is also a priority-based congestion protocol for wireless body area network in which the probability of data packet loss is calculated by the active queue management (QAM) method whereas the output transmits rate of each device is calculated by a fuzzy logic controller (FLC) and then a reasonable transmit rate is allocated to each device. It is evaluated in terms of throughput, delay, queue length, rate adjustment, energy, and packet loss. Different types are simulation parameters are selected shown in Tab. 3.
Table 3: Simulation parameters
End-to-end delay denotes the time taken for a data packet to be transmitted across a network from source to destination. It is an important parameter to know the performance of the MIoT networks. The end to end delay is calculated for all three techniques, EPCP_MIoT, PBCCP, and FPBCC. The comparison results show that the delay of the proposed technique EPCP_MIoT is less than the PBCCP and FPBCC. As it is mentioned in Fig. 7, the delay of EPCP_MIoT increasing because the devices take some time to be configured, they send and receive the control packets. As a result, the end to end delay of EPCP_MIoT is less than the other two techniques because it efficiently handles the congestion before it occurs. For this purpose, it adjusts its monitoring modes and priority levels in the beginning. This concept helps EPCP_MIoT to decrease the maximum end to end delay. EPCP_MIoT prioritizes the emergency data, in case of emergency it does not wait and reserve extra slots it starts transmission through SIFS time. From the results, it is clear the end to end delay of PBCCP and FPBCC is higher because they did not adjust the monitoring modes. Because of continuous monitoring, both techniques create node congestion and link congestion. It was observed that this congestion was happening from time to time. PBCCP categorizes the patients based on their conditions, normal, urgent, and critical, it takes continually more time for those patients who are in critical and urgent conditions. The FPBCC consumes more time because of its routing hop by hop. It follows the long route from sensors in the destination sink device. The data from different sensors is passed by many intermediate devices, it was seen some intermediate devices to create congestion. Therefore, to follow the longer route and congestion it creates the end to end delay. Even though when the technique solves the congestion issues it takes a reasonable time. The end to end delay can be calculated by the following Eq. (3):
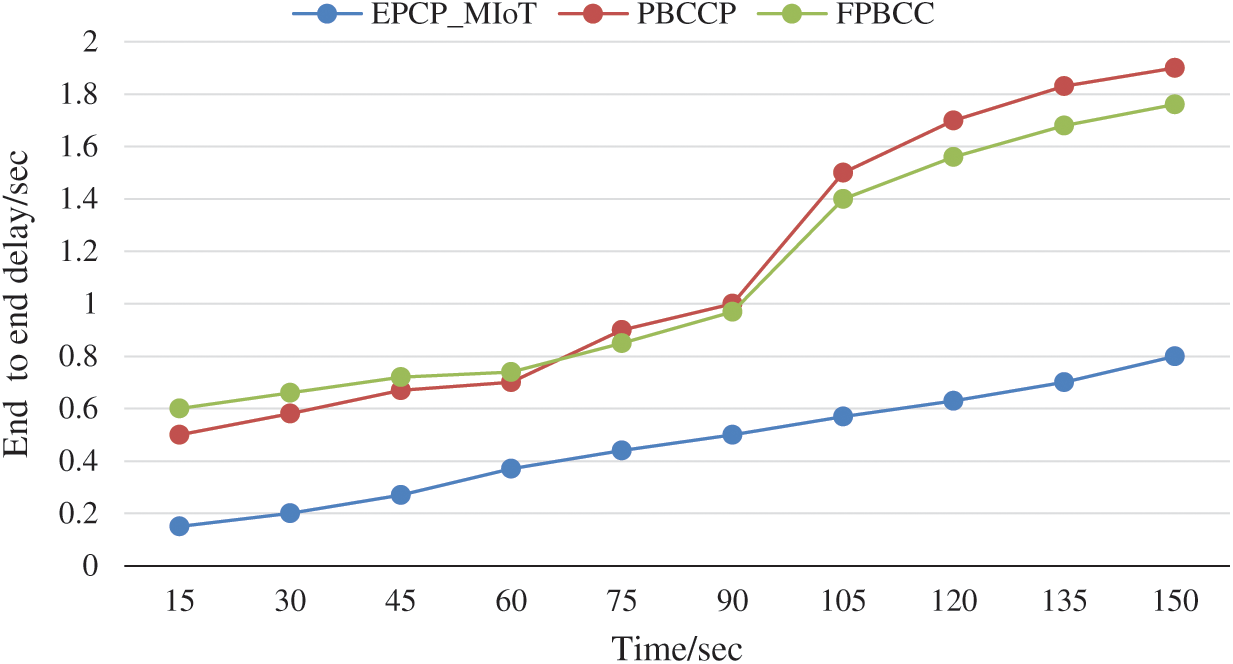
Figure 7: End to end delay vs. time

The network throughput is a critical metric; a higher network throughput is required in medical systems. As medical data need to be received as it is at their destinations. Throughput is the average rate of receiving data packets over a communication channel for the total number of data packets transmitted. Fig. 8. shows the comparison results of EPCP_MIoT with PBCCP and FPBCC. It is observed that the average throughput of the EPCP_MIoT is higher than PBCCP and FPBCC because it utilizes the network capacity well and as a result maintains an excellent throughput. Furthermore, EPCP_MIoT implemented data prioritization and monitoring modes to reduce congestion overhead. At the same time in case of emergency data transmission, EPCP_MIoT shows the best performance because each emergency data transmission can access the channel regardless of slots assignment. The average throughput of PBCCP has lower than the proposed technique because according to PBCCP all the sensor devices are required to train themselves based on feedback received from the other connected devices to ensure about receiving and dropping data packets. The calculation complexity of the whole procedure will, therefore, effect in dropping the performance of the overall network. The average throughput rate of FPBCC is lower because it could not manage the traffic load throughout the network. The average network throughput is calculated by the following Eq. (4):
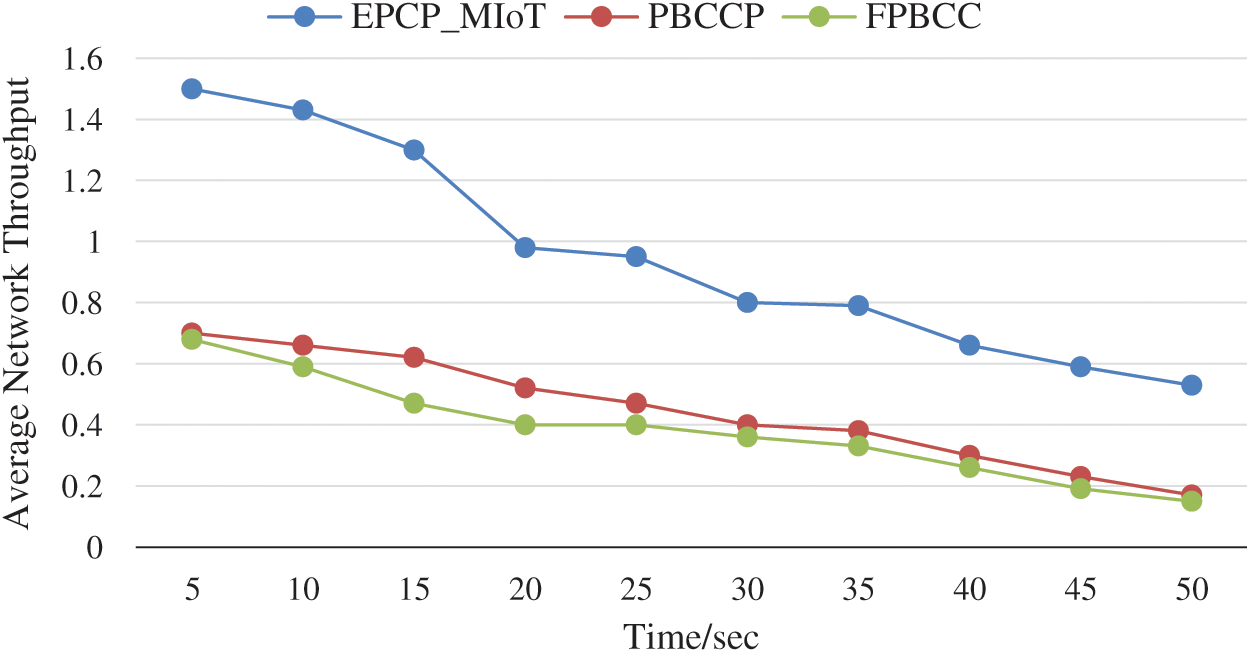
Figure 8: Average network throughput vs. time
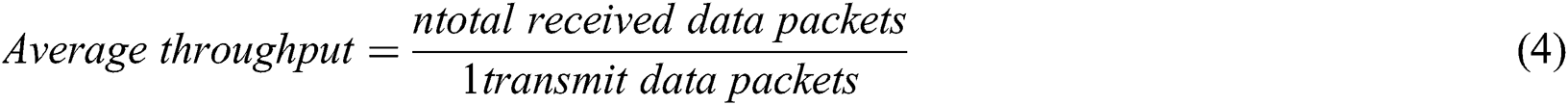
The packet loss ratio is the difference of total data packets transmitted by MIoTs and received at a destination device for the total data packets transmitted. Due to the transmission, some of the data packets may get lost. The packet loss rate can be calculated as the data packet loss per unit time. To evaluate the packet loss ratio of EPCP_MIoT, the results are compared with PBCCP and FPBCC. It is predicted in Fig. 9, the performance of EPCP_MIoT is highest as compared to the PBCCP and FPBCC. The performance of FPBCC is less because the devices could not manage the congestion appropriately. According to this technique, when the sink device received data and predicted anomaly then it’s assumed that there may be congestion. After detecting an anomaly, the sink device has to update the sender device about the congestion by replying to feedback messages. Now alternatively, FPBCC and PBCCP increase the network load and chance of collision. The EPCP_MIoT shows the best performance because it does not route the data packets hop by hop to any sink device. It efficiently manages the buffer capacity and avoids congestion. According to the EPCP_MIoT, MIoT devices examine their existing conditions and are capable to calculate the threshold values. They calculate the threshold values periodically to avoid congestion before it happens. Packet loss ratio can be calculated by the following Eq. (5):
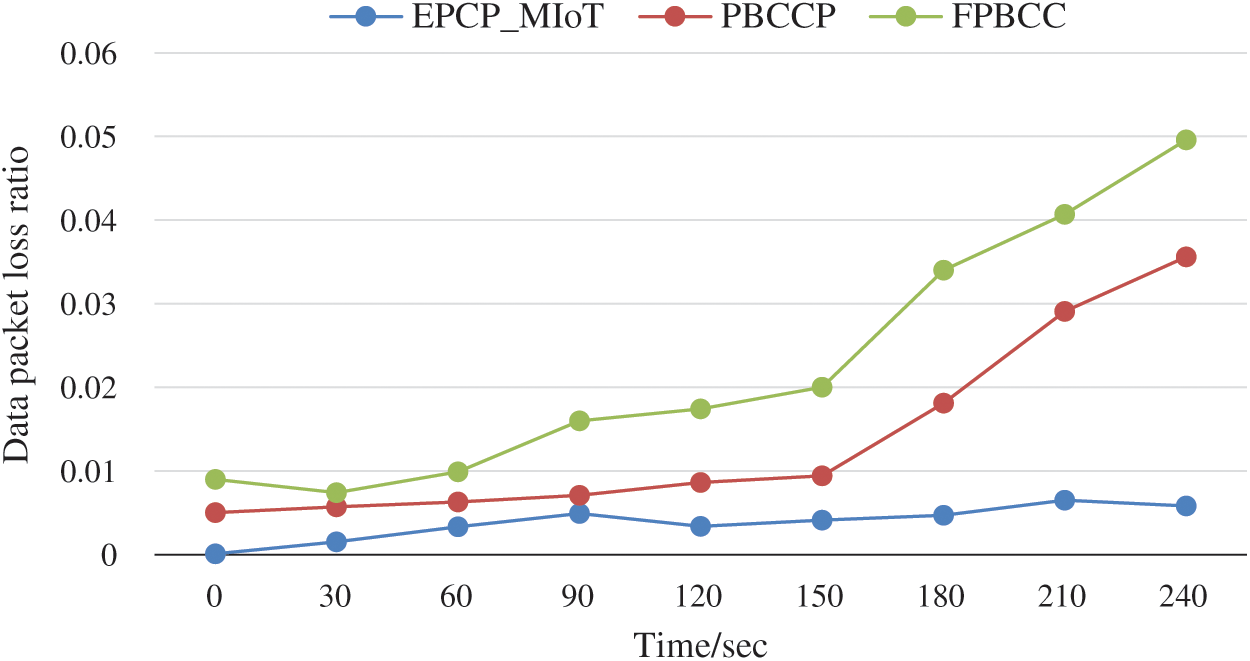
Figure 9: Data packet loss ratio vs. time

In Fig. 10, the average energy consumption of the EPCP_MIoT is analyzed and compared with PBCCP and FPBCC techniques. The energy consumption rate changes for each device with an increase in the transmission rate. The simulation results show that the average energy consumption of EPCP_MIoT is less than PBCCP and FPBCC for different types of data traffic. PBCCP and FPBCC show weak performance due to the messages broadcasted by the sink device to notify other devices about the possibility of the congestion. This happens because they did not accurately predict the congestion in the network. In PBCCP, patients having urgent or critical conditions will consume more energy than normal patients because physicians need their continuous monitoring data for taking essential decisions. The main issue with FPBCC is the inefficient routing of data that consumes more energy. As the sensors are tiny devices with limited battery power when they route the data hop by hop between the sensors and sink devices and wait for a long time for feedback messages will consume extra energy.
Figure 10: Average energy consumption vs. number of devices
It is predicted that the energy consumption of EPCP_MIoT is less because we have implemented sleep awake modes in the technique. The MIoTs sleep in the sleeping frame but at the same time, the MGD performs duty cycle for predicting the emergency data messages coming from any MIoT device even though it is not assigned the slots. In this slot, while the MIoTs must not send any general data packets, the MGD has to execute the duty cycle to receive the signal of the emergency data transmission in Sleep Frame. The MIoTs switch the mode in the awake state if an emergency signal is predicted. According to the EPCP_MIoT, emergency data can be transmitted anytime from any MIoT. By using this technique MGD receives the emergency data successfully while maintaining energy efficiency.
In healthcare monitoring systems, the philological signals have different priorities. Some signals are high priority signals and need to be transmitted as soon as possible to the concerned physicians. In this paper, a reliable Emergency Prioritized and Congestion Handling Protocol for Medical IoTs (EPCP_MIoT) is proposed that integrates the MIoTs with MGD and MCS. MIoTs monitors the body based on monitoring modes and transmits the data to the relative MGD. Where an MGD performs data abstraction, classification, and prioritization on receiving data. We have compared the results of EPCP_MIoT with other techniques PBCCP and FPBCC. The simulation results revealed that EPCP_MIoT outperforms PBCCP and FPBCC in terms of throughput, energy consumption, end to end delay, and packet loss. It is also predicted that EPCP_MIoT efficiently prioritized emergency data transmissions.
Funding Statement: This project was funded by the Deanship of Scientific Research (DSR), at King Abdulaziz University, Jeddah, under grant no. G: 292-612-1440. The authors, therefore, acknowledge with thanks DSR for technical and financial support.
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
References
1. K. H. Abdulkareem, A. M. Mazin, S. G. Saraswathy, A. M. Nasser, A. M. Ammar et al. (2019). , “A review of fog computing and machine learning: Concepts, applications, challenges, and open issues,” IEEE Access, vol. 7, pp. 153123–153140.
2. S. Ullah, H. Henry, B. Bart, L. Bnoit, B. Chris et al. (2012). , “A comprehensive survey of wireless body area networks,” Journal of Medical Systems, vol. 36, no. 3, pp. 065–1094.
3. I. Jahan, Md. Lizur Rahman, A. W. Reza and S. D. Barman. (2018). “Systolic blood pressure measurement from heart rate using IoT,” International Journal of Recent Technology and Engineering, vol. 7, no. 4, pp. 135–138.
4. K. J. P. Ortiz, J. P. O. Davalos, E. S. Eusebio and D. M. Tucay. (2018). “IoT: Electrocardiogram (ECG) monitoring system,” Indonesian Journal of Electrical Engineering and Computer Science, vol. 10, no. 2, pp. 480–489.
5. H. Huang, S. Hu and Y. Sun. (2019). “Energy-efficient ECG signal compression for user data input in cyber-physical systems by leveraging empirical mode decomposition,” ACM Transactions on Cyber-Physical Systems, vol. 3, no. 4, pp. 1–19.
6. M. A. Mohammed, B. Al-Khateeb, A. N. Rashid, D. A. Ibrahim and M. K. Abd Ghani. (2018). “Neural network and multi-fractal dimension features for breast cancer classification from ultrasound images,” Computers & Electrical Engineering, vol. 70, pp. 871–882.
7. R. Jaramillo, A. Quintero and S. Chamberl. (2016). “Rate control scheme for congestion control in wireless body area networks,” in 2016 IEEE 12th Int. Conf. on Wireless and Mobile Computing, Networking and Communications, New York, NY, USA, pp. 1–6.
8. L. P. Verma and M. Kumar. (2019). “An IoT based congestion control algorithm,” Internet of Things, vol. 9, pp. 1–12.
9. M. Shelke, T. Getenet, M. Akshay and M. Parikshit. (2016). “Fuzzy-based fault-tolerant low-energy adaptive clustering hierarchy routing protocol for wireless sensor network,” International Journal of Wireless and Mobile Computing, vol. 2, no. 11, pp. 117–112.
10. M. H. Nasser, M. Masha, H. Julian and Z. Behnam. (2020). “Internet of Things (IoT) and the energy sector,” Energies MDPI, vol. 13, pp. 1–27.
11. Y. Li, C. Xiang, C. Yang, W. Dexin and Y. Luliuting. (2018). “Smart choice for the smart grid: Narrowband Internet of Things (NB-IoT),” IEEE Internet of Things Journal, vol. 5, no. 3, pp. 1505–1515.
12. C. Pham, Y. Lim and Y. Tan. (2016). “Management architecture for heterogeneous IoT devices in home network,” in 2016 IEEE 5th Global Conf. on Consumer Electronics, Kyoto, pp. 1–5.
13. Z. Li, L. Yinghou, G. S. Kang, L. Jia, Y. Zheng et al. (2019). , “Interference steering to manage interference in IoT,” IEEE Internet of Things Journal, vol. 6, no. 6, pp. 10458–10471.
14. C. Sarkar, U. N. Akshy, R. V. Prasat, A. Rahim, N. Recardo et al. (2015). , “DIAT: A scalable distributed architecture for IoT,” IEEE Internet of Things Journal, vol. 3, no. 3, pp. 230–239.
15. Z. A. Khan, S. Shyamala, P. William and R. Bill. (2013). “A QoS-aware routing protocol for reliability sensitive data in hospital body area networks,” Procedia Computer Science, vol. 19, pp. 171–179.
16. S. Gambhir, V. Tickoo and M. Kathuria. (2015). “Priority-based congestion control in WBAN,” 2015 Eighth Int. Conf. on Contemporary Computing, Noida, pp. 428–433.
17. F. Pasandideh and A. A. Rezaee. (2018). “A fuzzy priority based congestion control scheme in wireless body area networks,” International Journal of Wireless and Mobile Computing, vol. 14, no. 1, pp. 1–15.
18. M. K. Abd. Ghani, M. A. Muhammad, M. A Arunkumar, N. Mostafa and D. A Ibrahim. (2020). “Decision-level fusion scheme for nasopharyngeal carcinoma identification using machine learning techniques,” Neural Computing and Applications, vol. 32, no. 3, pp. 625–638.
19. M. H. Yaghmaee, N. Bahalgardi and D. Adjeroh. (2013). “A prioritization based congestion control protocol for healthcare monitoring application in wireless sensor networks,” Wireless Personal Communications, vol. 72, no. 4, pp. 2605–2631.
20. A. M. Ammar, M. K. Ghani, N. Arunkuma, A. M. Mazin and M. Othman. (2019). “Enabling technologies for fog computing in healthcare IoT systems,” Future Generation Computer Systems, Elsevier, vol. 90, pp. 62–78.
21. S. Tahir, S. T. Bakhsh, A. Maysoon and A. Madini. (2019). “An energy-efficient fog-to-cloud internet of medical things architecture,” International Journal of Distributed Sensor Networks, vol. 15, no. 5, pp. 155014771985197.
22. S. T. Bakhsh. (2017). “Energy-efficient distributed relay selection in wireless sensor network for Internet of Things,” in 2017 13th Int. Wireless Communications and Mobile Computing Conf., Valencia, pp. 1802–1807.
23. S. Ford, The wellbeing and mental health of nurses must be a major consideration, 2012. [Online]. Available: https://www.nursingtimes.net/clinical-archive/assessment-skills/measuring-bodytemperature/5051350.article.
24. A. A. Adeniyia, A. A. Ganiyu, A. Lukman and O. A. Michael. (2005). “Modeling and performance analysis of dynamic random early detection (DRED) gateway for congestion avoidance,” in Internet and Multimedia Systems and Applications, EuroIMS, Grindelwald, Switzerland, vol. 5, pp. 623–636.
25. A. A. Mutlag, M. K. Abd. Ghani, M. A. Muhammad, M. S. Maashi, O. Mohd et al. (2020). , “MAFC: Multi-agent fog computing model for healthcare critical tasks management,” Sensors, vol. 20, no. 7, pp. 1853.
 | This work is licensed under a Creative Commons Attribution 4.0 International License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. |