 Open Access
Open Access
REVIEW
Surgical Ablation in Congenital Heart Disease: Advances in Techniques and Clinical Outcomes
1 Department of Cardiology, Erasmus Medical Center, Rotterdam, 3015GD, The Netherlands
2 Department of Cardiology, UT Southwestern Medical Center, Dallas, TX 75390, USA
3 Department of Cardiothoracic Surgery, Erasmus Medical Center, Rotterdam, 3015GD, The Netherlands
* Corresponding Author: Natasja M. S. de Groot. Email:
# Both authors contributed equally to this manuscript
Congenital Heart Disease 2024, 19(6), 577-592. https://doi.org/10.32604/chd.2025.062129
Received 11 December 2024; Accepted 20 January 2025; Issue published 27 January 2025
Abstract
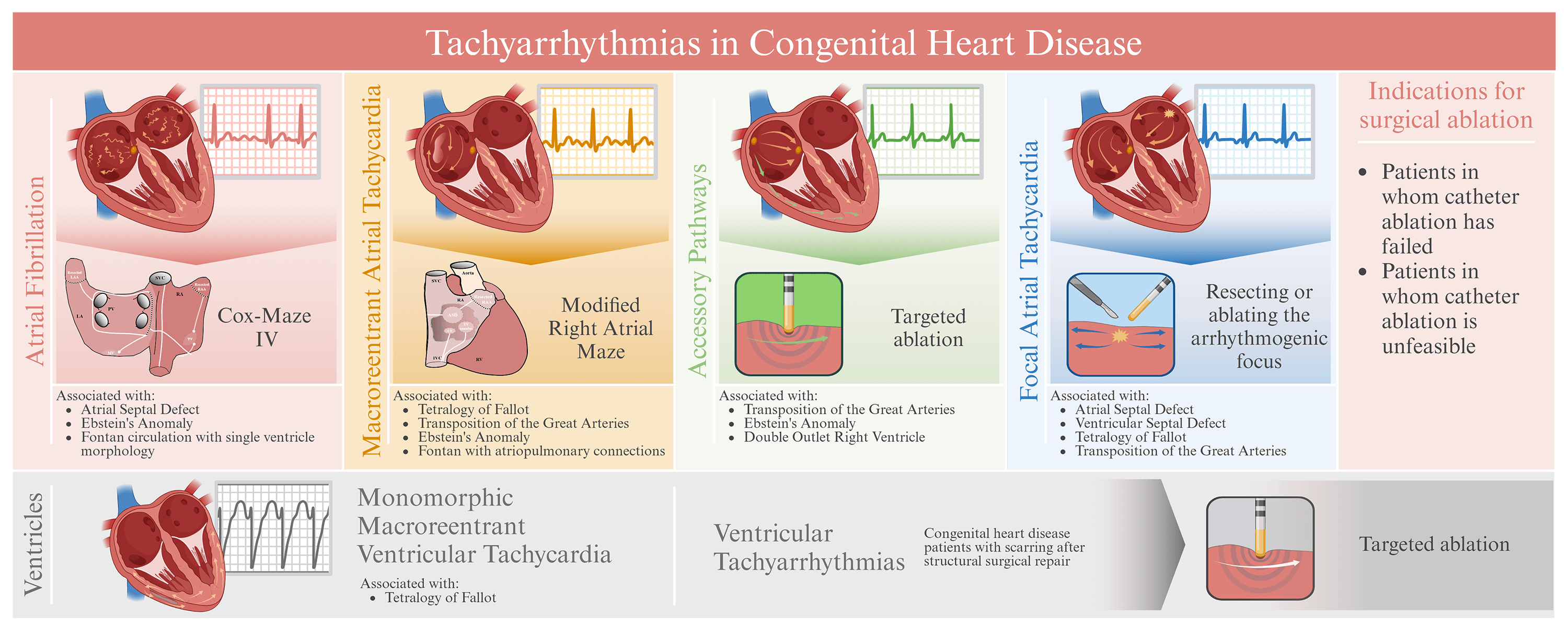
Surgical ablation (SA) has become an essential rhythm-control strategy for managing tachyarrhythmias in patients with congenital heart disease. Atrial tachyarrhythmias, such as atrial flutter and atrial fibrillation, are prevalent in congenital heart disease, affecting up to 50% of patients, and pose significant risks, including increased morbidity and mortality. Ventricular tachyarrhythmias, though less common, can lead to sudden cardiac death, particularly in conditions like Tetralogy of Fallot. Prior studies suggested that SA for tachyarrhythmias in patients with congenital heart disease offers significant benefits, including superior long-term rhythm control compared to catheter ablation (CA). Atrial tachyarrhythmia burden is effectively reduced by SA, such as the Cox-Maze IV procedure, thereby also improving the quality of life. Ablation strategies targeting critical isthmuses in the ventricles, such as between the tricuspid valve annulus and right ventricular outflow tract scar in patients with Tetralogy of Fallot, are effective in managing ventricular tachyarrhythmias. However, SA is associated with procedural risks, such as sinus node dysfunction and atrioventricular conduction block. Despite these risks, SA is recommended for congenital heart disease patients with symptomatic tachyarrhythmias unresponsive to drug therapy and CA, and it is increasingly considered as a prophylactic procedure in high-risk patients. Emerging innovative technologies, including enhanced mapping- and hybrid ablation techniques, are poised to further improve SA outcomes. The goal of this review is to assess the efficacy, outcomes, and risks of SA in congenital heart disease patients, compare the outcomes of SA with CA, and evaluate the risk-benefit ratio of (prophylactic) arrhythmia surgery. In summary, SA offers significant benefits, including long-term arrhythmia control and improved quality of life, particularly in patients in whom CA is unfeasible or has failed. Although SA is currently underutilized in clinical practice, the potential as a comprehensive treatment for specific patients with congenital heart disease underscores the importance of a patient tailored approach.Graphic Abstract
Keywords
Cite This Article
 Copyright © 2024 The Author(s). Published by Tech Science Press.
Copyright © 2024 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools