 Open Access
Open Access
ARTICLE
Efficacy of Intravenous Treprostinil in High-Risk Single Ventricle Patients Undergoing Glenn Procedure
1 Department of Pediatric Intensive Care Unit, National Center for Cardiovascular Disease, Fuwai Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, 100037, China
2 Department of Pharmacy, National Center for Cardiovascular Disease, Fuwai Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, 100037, China
* Corresponding Author: Xu Wang. Email:
# These authors contributed equally to this paper
Congenital Heart Disease 2024, 19(5), 489-498. https://doi.org/10.32604/chd.2024.054441
Received 28 May 2024; Accepted 18 October 2024; Issue published 31 December 2024
A correction of this article was approved in:
Correction: Efficacy of Intravenous Treprostinil in High-Risk Single Ventricle Patients Undergoing Glenn Procedure
Read correction
Abstract
Objective: Pulmonary hypertension is a crucial factor affecting the recovery after Glenn procedure. This study explores the effects of intravenous treprostinil on hemodynamic status and hospital postoperative recovery under different administration strategies. Methods: We retrospectively included pediatric patients admitted to Fuwai Hospital from 2019 to 2022 who underwent the Glenn procedure and had intraoperative measurements of mean pulmonary artery pressure (mPAP) >15 mmHg postoperatively. Patients with non-anatomical single ventricle physiology undergoing the Glenn procedure and those requiring postoperative extracorporeal membrane oxygenation were excluded. Due to the standardized use of treprostinil in our center starting in 2021, patients from 2019–2020 were included in Group 1, and patients from 2021–2022 were included in Group 2. The changes in hemodynamic data before and after medication for both groups of patients, as well as the differences in postoperative recovery, were compared. Results: Twenty-eight patients were eventually enrolled in the study. Group 1 consisted of 14 cases, with a maintenance dose of 11 ± 2 ng/(kg·min) 1 to 2 days postoperatively. Group 2 also consisted of 14 cases, with a maintenance dose of 26 ± 7 ng/(kg·min) 1 day postoperatively. After a 24-h observation period, the mPAP decreased from 17 ± 3 to 13 ± 3 mmHg (p < 0.001) in the first group and decreased from 18 ± 3 to 13 ± 3 mmHg (p < 0.001) in the second group. The vasoactive-inotropic score in the first group decreased from 9 (6,17) to 6 (4,9) (p = 0.001) and decreased from 12 (6,23) to 10 (3,15) (p = 0.002) in the second group. Group 2 patients had a shorter postoperative hospital stay than Group 1, with durations of 18 (11,22) days and 29 (19,47) days, respectively (p = 0.021). No severe adverse reactions occurred in all patients. Conclusion: Intravenous infusion of treprostinil in high-risk patients after the Glenn procedure can decrease pulmonary artery pressure, reduce vasoactive-inotropic score, and demonstrate satisfactory drug tolerance without severe adverse reactions. Standardized use of treprostinil facilitates postoperative recovery and shortens postoperative length of stay.Keywords
Abbreviations
| mPAP | Mean pulmonary artery pressure |
| VIS | Vasoactive-inotropic score |
The bidirectional superior cavopulmonary connection procedure, also known as the Glenn procedure, is typically the second-stage surgery for treating single ventricle patients [1]. The aim is to reduce ventricular preload and eventually prepare the patient for the third-stage Fontan procedure. Success of the surgery largely depends on the pulmonary artery pressure, in order to accommodate the non-pulsatile venous return. Increased mean pulmonary artery pressure (mPAP) has been clearly recognized as an independent high-risk factor, leading to increased postoperative complications and delayed recovery [2]. In contrast to the commonly used criterion of mPAP >20 mmHg [3], in single ventricle-related pulmonary hypertension (high-risk single ventricle), an mPAP >15 mmHg is the standard of diagnosis [4].
Patients with elevated pulmonary artery pressures may benefit from targeted pulmonary hypertension medications following Glenn procedure to reduce pulmonary circulation resistance, potentially improving hemodynamic status and surgical outcomes. Currently used targeted medications include endothelin receptor antagonists, phosphodiesterase −5 inhibitors or guanylate cyclase agonists, prostacycline and its analogues [5]. Agarwal et al. retrospectively reviewed 16 pediatric patients who underwent the Glenn procedure at a single center and studied the therapeutic effects of inhaled nitric oxide using a self-controlled method [6]. Eleven patients showed response to inhaled nitric oxide treatment, with effects including decreased Glenn pressure (from 22.4 to 17.1 mmHg, p < 0.001), improved PaO2/FiO2 (from 49 to 74.3, p = 0.001) and oxygenation index (from 17 to 12, p = 0.005), reduced inotrope score (from 14.9 to 11.4, p < 0.001), and decreased volume requirements (from 11.4 to 2.3 mL/kg, p < 0.001). However, five patients showed no response to inhaled nitric oxide treatment, all of whom had anatomical lesions. Hirono et al. [7] conducted a study on the clinical and hemodynamic improvements of single ventricle physiology patients with bosentan, including eight patients (five undergoing the Glenn procedure) who ultimately successfully underwent Fontan surgery after bosentan treatment. Mori et al. [8] conducted a multicenter retrospective study involving 42 single ventricle physiology patients with pulmonary vascular resistance index >2.5 wood units × m2, including 11 post-Glenn procedure patients. After receiving sildenafil treatment, the pulmonary vascular resistance index decreased from 3.2 ± 0.5 wood units × m2 to 1.6 ± 0.6 wood units × m2 (p < 0.001) in these 11 patients without adverse effects. Jeremiasen et al. [9] retrospectively analyzed pulmonary hypertension-related data from British children between 2004 and 2017, including 36 single ventricle physiology patients receiving pulmonary hypertension-targeted therapy, with eight of them having undergone the Glenn procedure. The drugs used included sildenafil and/or bosentan, with 56% of patients receiving combination therapy. Among 17 patients with hemodynamic parameters, mPAP decreased from 19 to 14 mmHg (p < 0.01). In 16 patients treated with single or initial combination therapy, oxygen saturation increased from 80% to 85% (p < 0.01). Oxygen saturation did not improve in patients treated with sequential combination therapy. Among the eight post-Glenn procedure patients, two eventually underwent Fontan surgery.
However, these studies still have limitations. Inhalation of nitric oxide depends on the respiratory support system, which cannot be continued after extubation. The studies on oral sildenafil and bosentan mainly involve outpatient follow-up after discharge, the absorption of drugs after the operation may be insufficient due to impaired gastrointestinal function, resulting in unstable efficacy in this period. If drugs administered via intravenous/subcutaneous administration could be found as bridge therapy for inhaled and oral targeted medications, it theoretically could lead to a smoother postoperative recovery by stabilizing pulmonary artery pressure.
Treprostinil is the preferred and required medication for severe pulmonary arterial hypertension patients [10]. Although there is some evidence suggesting the efficacy of treprostinil in treating pulmonary arterial hypertension related to congenital heart disease [11], for the specific disease of a single ventricle, there is very limited research evidence. Chen et al. [12] found a linear relationship between the blood concentration of Treprostinil and its dose. In this self-controlled study involved 8 pediatric functional single ventricle pulmonary arterial hypertension, the mPAP, pulmonary-to-systemic arterial pressure ratio, and the ratio between arterial oxygen partial pressure and inhaled oxygen concentration were used to evaluate the efficacy of treatment.
Sullivan et al. [13] conducted a cohort study that included 17 high-risk single-ventricle patients who received long-term treprostinil to facilitate surgical opportunities. Regarding surgical opportunities, 3 out of 6 patients (50%) after Glenn’s surgery were given the opportunity for Fontan surgery. However, current studies still have certain limitations: 1) The sample size of studies on treprostinil after Glenn surgery is small, and there is a lack of clinical studies specifically targeting Glenn patients; 2) For early postoperative patients, there is a lack of research on the standard use of treprostinil administration; 3) There is a lack of studies on the recovery after Glenn surgery.
In summary, the purpose of this study is to investigate, through a retrospective cohort study, whether standardizing the administration timing and maintenance dosage of treprostinil can improve the hemodynamics and postoperative recovery of high-risk single-ventricle heart patients following Glenn surgery.
2.1 Patient Inclusion and Grouping
This study analyzed pediatric patients who received the Glenn procedure at Fuwai Hospital between 2019 and 2022 retrospectively. Inclusion criteria included: 1) The mPAP >15 mmHg in the operating room after surgery completion (by direct needle manometry); 2) Postoperative intravenous infusion of treprostinil in the ICU. Exclusion criteria included: 1) Patients with non-anatomic single ventricle or single ventricle physiology undergoing Glenn procedure; 2) Postoperative use of extracorporeal membrane oxygenation assistance. Due to the standardized use of treprostinil in our center starting in 2021, patients from 2019–2020 were included in Group 1, and patients from 2021–2022 were included in Group 2.
Among a total of 184 patients after the Glenn procedure, 33 patients met the inclusion criteria. Among the 33 patients, 4 patients were excluded for non-anatomic single ventricle or single ventricle physiology, and 1 patient was excluded for receiving ECMO assistance, resulting in the final inclusion of 28 patients. Among them, there were 14 patients in the first Group who received maintaining treprostinil 1–2 days postoperatively ranging from 10–15 ng/(kg·min) with an average dose of 11 ± 2 ng/(kg·min). 14 patients were included in Group 2 who received maintaining treprostinil therapy within 1 day postoperatively ranged 20–40 ng/(kg·min) with an average dose of 26 ± 7 ng/(kg·min).
2.2 All Targeted Drug Administration Strategies
There were no patients being treated for pulmonary hypertension preoperatively. For patients after the Glenn procedure, blood pressure stability was initially maintained. Inhaled nitric oxide at 20 ppm was administered via the ventilator, gradually reducing the concentration before extubation, along with sildenafil at 0.5 mg/kg per dose, a maximum of 20 mg per dose, three times daily. After hemodynamic stability was achieved, an intravenous infusion of treprostinil was prescribed. Because of the limited clinical experience, the initial infusion rate was 4 ng/(kg·min), with increments of 2–4 ng/(kg·min) every 2 h until clinical improvement was achieved (atrial pressure, volume requirement, and tachycardia improvement), and the current dose was maintained for ongoing treatment. Standardized treprostinil treatment began in 2021, with an initial treatment dose of 5 ng/(kg·min), increasing by 5 ng/(kg·min) every 30 min until the maximum tolerated dose (indicated by blood pressure instability) was reached for maintenance treatment. Once gastrointestinal function recovered, oral medications were added, including bosentan at 2 mg/kg (up to 125 mg/kg) twice daily, as sequential combined treatment with sildenafil. After starting oral targeted drugs, we gradually reduced and discontinued the intravenous infusion of treprostinil, without transitioning to subcutaneous administration.
Record preoperative, intraoperative, and postoperative parameter data for both groups of patients. Preoperative data includes age, weight, heterotaxy syndrome, and mPAP measured by right heart catheterization in the catheterization laboratory before surgery. Intraoperative data includes concurrent surgeries such as atrioventricular valve plasty/correction of pulmonary vein stenosis, cardiopulmonary bypass duration, aortic cross-clamp duration, and mPAP measured in the operating room after surgery. Postoperative data includes treprostinil maintenance dose, hemodynamic parameters before and after the maintenance dose at 6, 12, 18, and 24 h, including mPAP, atrial pressure, and the vasoactivity-inotropic score calculated as dopamine dose (μg/kg/min) + dobutamine dose (μg/kg/min) + milrinone dose (μg/kg/min) × 10 + epinephrine dose (μg/kg/min) × 100 + vasopressin dose (U/kg/min) × 10000. Postoperative recovery parameters include mechanical ventilation duration, length of ICU stay and postoperative hospital stay, tachycardia, chest tube drainage, duration of chest tube placement, thromboembolic events, renal replacement therapy, reintubation, tracheostomy, in-hospital mortality, and adverse reactions to treprostinil treatment.
Statistical analyses were conducted utilizing IBM SPSS Statistics for Windows, version 25.0 (IBM Corp., Armonk, NY, USA). The Shapiro-Wilk test was employed to evaluate the normality of continuous variables. Continuous variables that followed a normal distribution were reported as mean ± standard deviation, while those not normally distributed were presented as median (interquartile range). Categorical variables were described using frequency (percentage). The study employs a one-way repeated measures analysis of variance to compare alterations in hemodynamic parameters before and after the administration of treprostinil, as well as between different groups. The assumption of sphericity is evaluated using Mauchly’s test of sphericity, with the Greenhouse-Geisser correction applied if necessary. Depending on the normality of the data distribution, comparisons of continuous variables between groups are conducted using either independent samples t-tests or Wilcoxon rank-sum tests. Categorical variables are analyzed using Fisher’s exact test where applicable. Missing values are estimated through the expectation-maximization algorithm. A p-value of 0.05 or less is regarded as the threshold for statistical significance.
This study has been reviewed and approved by the Ethics Committee of Fuwai Hospital, with the number: 2022-1859. Due to its retrospective nature, informed consent was waived. Throughout the research process, the ethical principles outlined in the Declaration of Helsinki in 1964 were followed. This retrospective analysis is based on anonymized data collected for routine clinical care and administrative purposes. Therefore, the need for informed consent was waived.
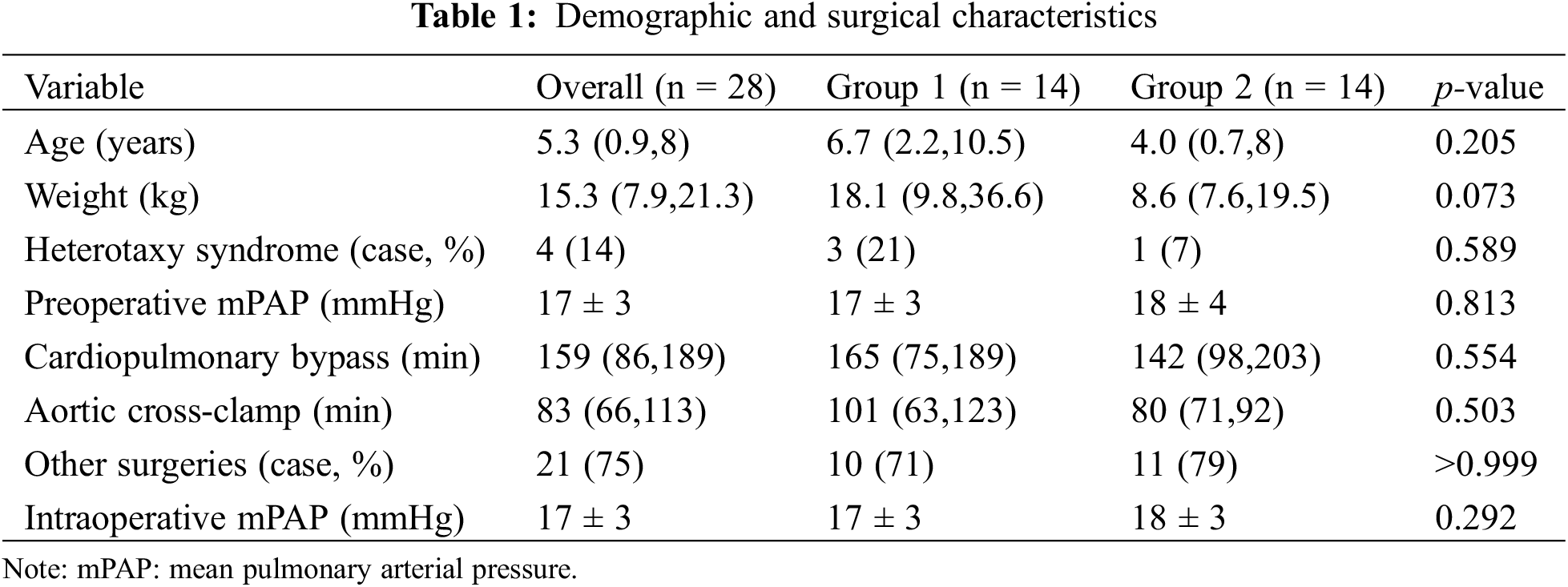
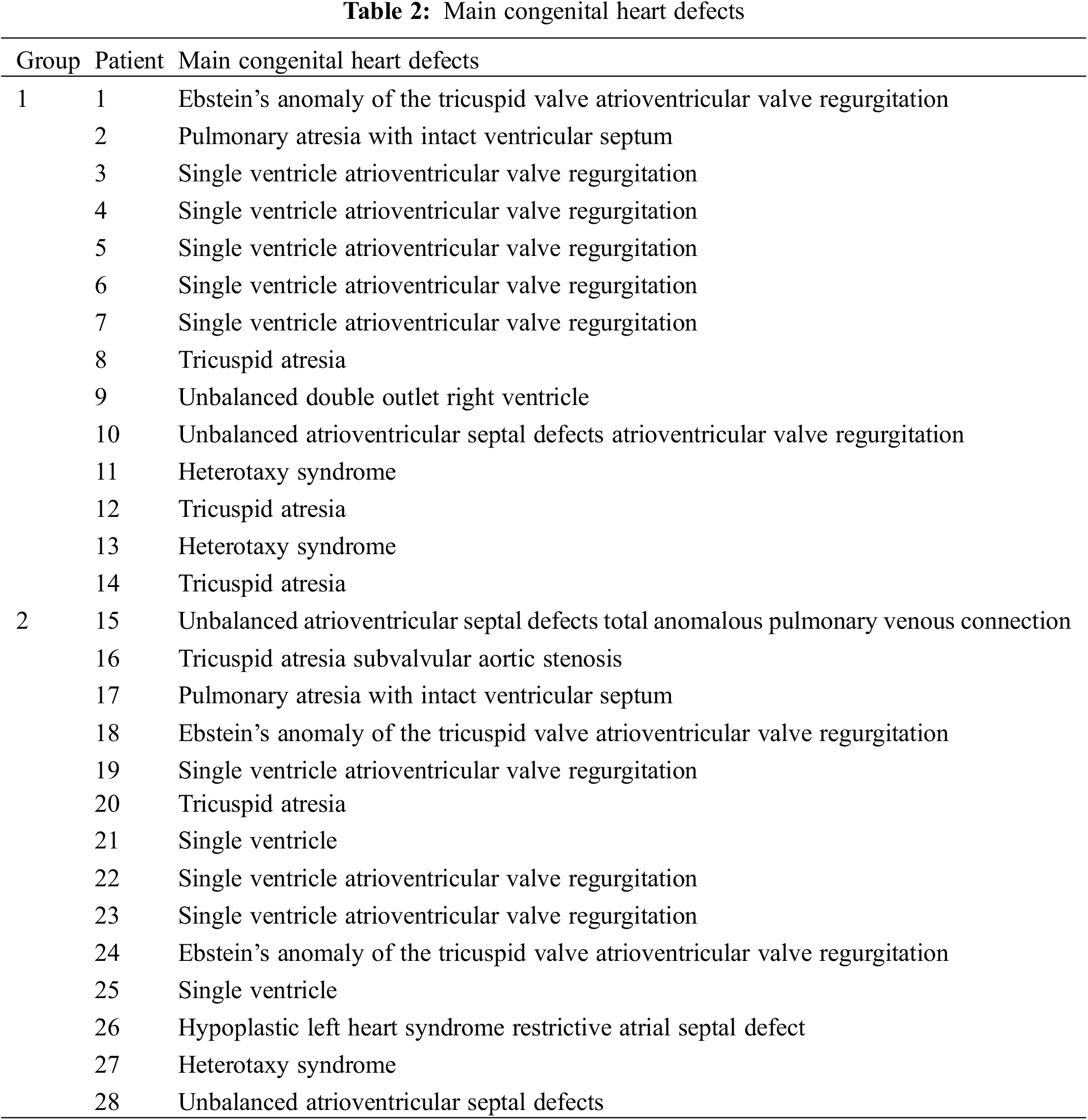
The demographic and surgical characteristics of the two groups of patients are shown in Table 1. The median age of all patients was 5.3 years, median weight was 15.3 kg, 14% had associated heterotaxy syndrome, and median cardiopulmonary bypass and aortic cross-clamp times were 159 and 83 min, respectively. Seventy-five percent of patients underwent concurrent additional cardiac surgeries, and both preoperative and intraoperative mPAP were 17 ± 3 mmHg. There was no statistical difference between the two groups in demographic and surgical characteristics, as detailed in Table 1. The main congenital heart defects in both groups are shown in Table 2.
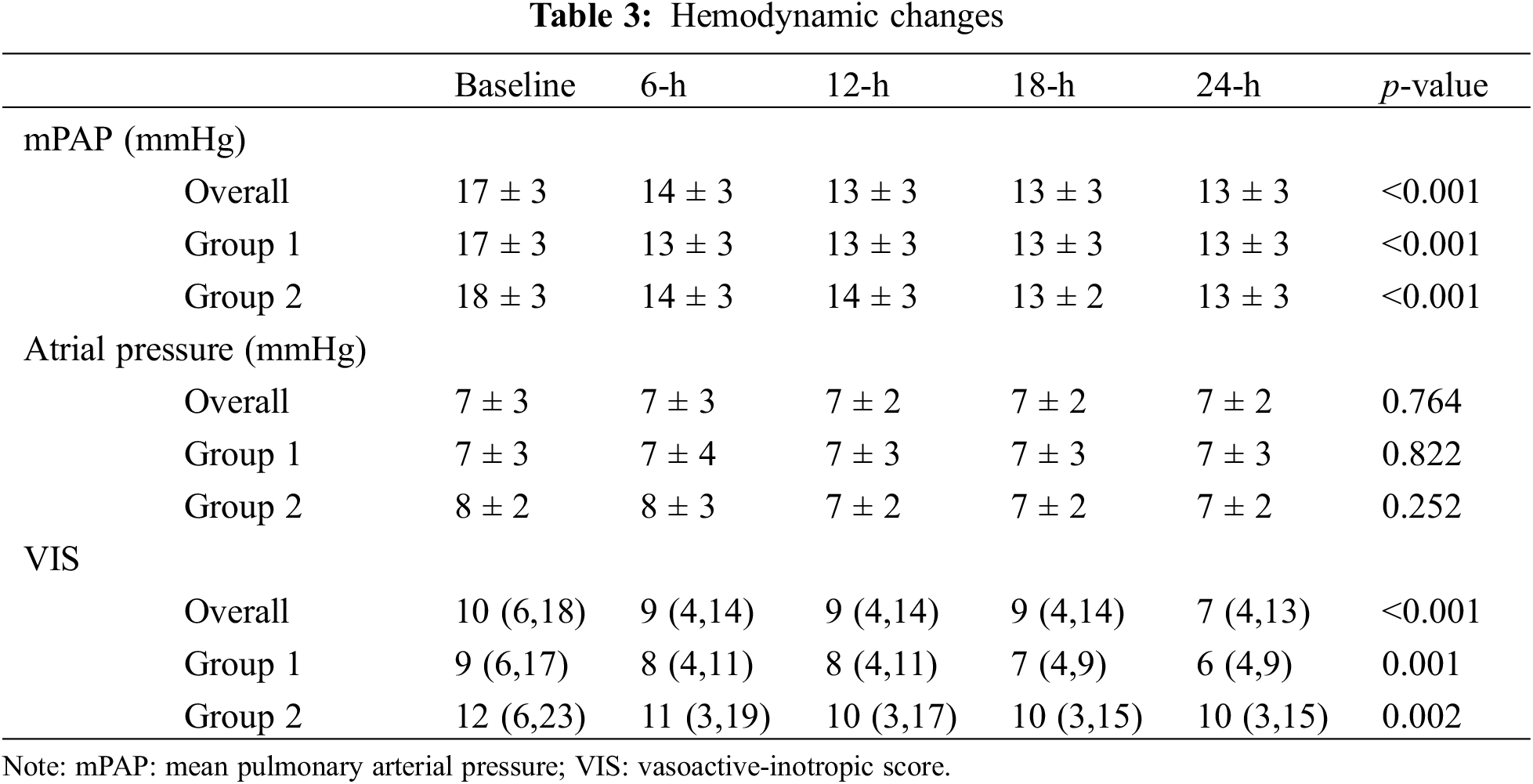
In terms of hemodynamic changes after the administration of treprostinil, as shown in Table 3, the decrease in mPAP was statistically significant in both groups, but there was no statistical difference between the two groups. There were no statistically significant differences in changes in atrial pressure among patients overall, in Group 1, in Group 2, or between groups. The decrease in vasoactive-inotropic score was statistically significant in both groups, but there was no statistical difference between the two groups.
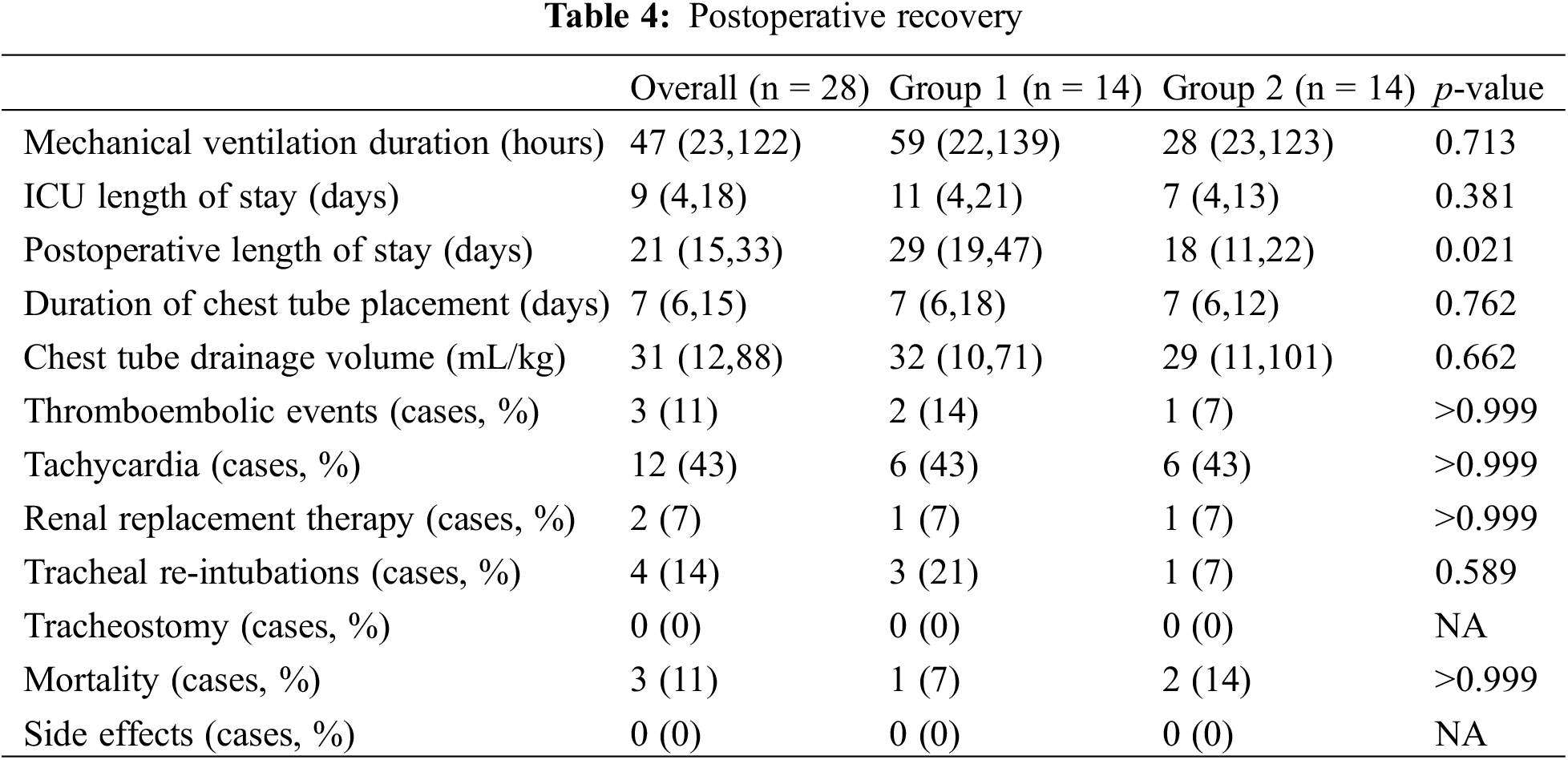
When comparing the postoperative recovery, the postoperative length of stay was 18 (11,22) days vs. 29 (19,47) days, shorter in Group 2 patients (p = 0.021). There were no severe side effects that occurred in the two groups. The details of postoperative recovery are shown in Table 4.
This study is the first investigation only focused on the effects of intravenous administration of treprostinil in high-risk Glenn procedures, with an emphasis on observing the impact of different administration strategies on hemodynamic status and postoperative recovery during hospitalization. Due to our center’s management strategy of early extubation in the ICU following the Glenn procedure and the inability to accurately calculate relevant indicators post-tracheal extubation, the effects of treprostinil on the oxygenation index were not studied.
The patients enrolled in this study were significantly older than the best-recommended age for Glenn’s operation, which was mainly due to the national conditions of our country. China, a large developing country, exhibits notable variations in its medical conditions across diverse regions. Many patients from poor areas do not receive timely treatment, resulting in delayed visits, increased pulmonary artery pressure, and increased incidence of cardiac malformations requiring surgical treatment. Since some patients undergoing Glenn procedure simultaneously require other cardiac surgeries to correct cardiac malformations, preoperative mPAP may overestimate pulmonary vasculature disease [14], hence an intraoperative mPAP >15 mmHg (after correcting the anatomical malformations) was used as the diagnostic criteria for the high-risk patient.
Our center began using treprostinil to treat high-risk patients after Glenn’s surgery in 2019. Initially, due to a lack of experience and concerns about early postoperative blood flow insufficiency [15], the dosage of treprostinil was titrated cautiously, the maintenance dose was chosen based on the effectiveness of the drug, after which the dose was not further increased. Based on experience, our center implemented a standardized strategy in 2021, with earlier administration times and higher maintenance doses. Therefore, the purpose is to compare the effects of these two different strategies in improving hemodynamics and postoperative recovery.
About the improvement in hemodynamics, through an observation period of 24 h, we found out that treprostinil can decrease pulmonary arterial pressure in patients after the Glenn procedure, suggesting that targeted drug therapy for pulmonary arterial hypertension also takes its effects in single ventricle patients. Although treprostinil theoretically reduces systemic vascular resistance, in this study, the vasoactive-inotropic score after treprostinil administration continued to decrease, suggesting a significant improvement in ventricular function under the maintaining dose used in this study. In the assessment of improvement in atrial pressure, it was found that there was no significant change in atrial pressure. Considering the findings of this study that treprostinil can improve ventricular function, it is speculated that the insignificant change in atrial pressure in patients may be attributed to its reduction of pulmonary vascular resistance, increase in the proportion of systemic-to-pulmonary circulation blood flow and ventricular volume load, which can offset its improvement in ventricular function by reducing systemic vascular resistance.
In discussing postoperative recovery, compared with Group 1, the postoperative hospital stay was significantly reduced in Group 2. In terms of cause analysis, although there was no statistical difference between the two groups in reducing pulmonary artery pressure, the pharmacological effects of treprostinil also included reducing systemic ventricular afterload and inhibiting smooth muscle cell proliferation [16]. It is speculated that the high dose of treprostinil exerted its comprehensive pharmacological effects, thereby improving the prognosis of the patients.
In addition to treprostinil, all patients enrolled in this study also received other targeted drugs, such as inhaled nitric oxide and oral bosentan/sildenafil, which also played an important role in improving postoperative recovery in high-risk patients. The purpose of treprostinil in our study was to bridge the window period when inhaled nitric oxide cannot be continued after tracheal extubation and oral drugs cannot be effective before gastrointestinal function recovery after the Glenn procedure. There was no difference in the administration schedules of inhaled nitric oxide and oral drugs between the two groups. In this condition, it was considered the difference in the treprostinil administration regimen contributed to the improvement in recovery in the standardized treatment group of patients.
In this study, three patients experienced postoperative death within 30 days after surgery, resulting in an overall mortality rate of approximately 11%. This relatively high mortality rate was considered to be related to the inclusion of high-risk patients in this study. It also suggested that for such high-risk patients, careful assessment of surgical indications was necessary. For patients at high risk, mechanical support could be considered if conditions permit [17], otherwise, palliative treatment might be considered.
This study also had certain limitations. 1) The sample size of the study is small, which may lead to the lack of statistical differences in some clinically significant results, and it is necessary to increase the sample size or conduct multicenter studies in the future to address the research deficiencies. 2) Since this study is a retrospective analysis, its evidence level is still inadequate, and future higher-level clinical studies are needed. 3) Long-term follow-up of these patients is needed in the future to study final outcomes such as the proportion of patients who completed total cavo-pulmonary connection surgery and overall mortality rate.
Intravenous infusion of treprostinil in high-risk patients after the Glenn procedure can decrease pulmonary artery pressure, reduce vasoactive-inotropic score, and demonstrate satisfactory drug tolerance without severe adverse reactions. Standardized use of treprostinil facilitates postoperative recovery and shortens postoperative length of stay.
Acknowledgement: None.
Funding Statement: This work was supported by the Clinical Research Foundation of the National Health Commission of the People’s Republic of China (grant numbers: 2022-GSP-GG-32, 2022-GSP-QN-13 and 2023-GSP-QN-5).
Author Contributions: Study conception and design: Xu Wang, Xiaofeng Wang; data collection: Xiaofeng Wang, Shilin Wang, Xingwei Chen; analysis and interpretation of results: Xia Li, Xiaofeng Wang, Shilin Wang, Xingwei Chen; draft manuscript preparation: Zhongyuan Lu, Wenlong Wang. All authors reviewed the results and approved the final version of the manuscript.
Availability of Data and Materials: The data underlying this article will be shared upon reasonable request with the corresponding author.
Ethics Approval: This study has been reviewed and approved by the Ethics Committee of Fuwai Hospital, with ID: 2022-1859. Due to its retrospective nature, informed consent was waived. The ethical principles outlined in the 1964 Helsinki Declaration were adhered to throughout the study.
Conflicts of Interest: The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Rao PS. Single ventricle-a comprehensive review. Children. 2021;8(6):441. doi:10.3390/children8060441. [Google Scholar] [PubMed] [CrossRef]
2. Tran S, Sullivan PM, Cleveland J, Kumar SR, Takao C. Elevated pulmonary artery pressure, not pulmonary vascular resistance, is an independent predictor of short-term morbidity following bidirectional cavopulmonary connection. Pediatr Cardiol. 2018;39(8):1572–80. doi:10.1007/s00246-018-1932-6. [Google Scholar] [PubMed] [CrossRef]
3. Simonneau G, Montani D, Celermajer DS, Denton CP, Gatzoulis MA, Krowka M, et al. Haemodynamic definitions and updated clinical classification of pulmonary hypertension. Eur Respir J. 2019;53(1):1801913. doi:10.1183/13993003.01913-2018. [Google Scholar] [PubMed] [CrossRef]
4. Baumgartner H, De Backer J, Babu-Narayan SV, Budts W, Chessa M, Diller GP, et al. 2020 ESC Guidelines for the management of adult congenital heart disease. Eur Heart J. 2021;42(6):563–645. doi:10.1093/eurheartj/ehaa554. [Google Scholar] [PubMed] [CrossRef]
5. Ruopp NF, Cockrill BA. Diagnosis and treatment of pulmonary arterial hypertension: a review. JAMA. 2022;327(14):1379–91. doi:10.1001/jama.2022.4402. [Google Scholar] [PubMed] [CrossRef]
6. Agarwal HS, Churchwell KB, Doyle TP, Christian KG, DrinkwaterJr DC, Byrne DW, et al. Inhaled nitric oxide use in bidirectional Glenn anastomosis for elevated Glenn pressures. Ann Thorac Surg. 2006;81(4):1429–34. doi:10.1016/j.athoracsur.2005.11.004. [Google Scholar] [PubMed] [CrossRef]
7. Hirono K, Yoshimura N, Taguchi M, Watanabe K, Nakamura T, Ichida F, et al. Bosentan induces clinical and hemodynamic improvement in candidates for right-sided heart bypass surgery. J Thorac Cardiovasc Surg. 2010;140(2):346–51. doi:10.1016/j.jtcvs.2010.03.023. [Google Scholar] [PubMed] [CrossRef]
8. Mori H, Park IS, Yamagishi H, Nakamura M, Ishikawa S, Takigiku K, et al. Sildenafil reduces pulmonary vascular resistance in single ventricular physiology. Int J Cardiol. 2016;221:122–7. doi:10.1016/j.ijcard.2016.06.322. [Google Scholar] [PubMed] [CrossRef]
9. Jeremiasen I, Tran-Lundmark K, Idris N, Tran PK, Moledina S. Pulmonary vasodilator therapy in children with single ventricle physiology: effects on saturation and pulmonary arterial pressure. Pediatr Cardiol. 2020;41(8):1651–9. doi:10.1007/s00246-020-02424-w. [Google Scholar] [PubMed] [CrossRef]
10. Ablonczy L, Tordas D, Kis E, Szatmári A. Use of subcutaneous Treprostinil in pediatric pulmonary arterial hypertension-Bridge-to-transplant or long-term treatment? Pediatr Transplant. 2018;22:e13106. [Google Scholar]
11. Skoro-Sajer N, Gerges C, Balint OH, Kohalmi D, Kaldararova M, Simkova I, et al. Subcutaneous treprostinil in congenital heart disease-related pulmonary arterial hypertension. Heart. 2018;104(14):1195–9. doi:10.1136/heartjnl-2017-312143. [Google Scholar] [PubMed] [CrossRef]
12. Chen X, Cai XM, Zhang MJ, Xu JH, Li H, Xu ZM. Pharmacokinetics of Treprostinil in children with functional single-ventricle pulmonary arterial hypertension: a randomized controlled trial. Ann Transl Med. 2021;9(14):1163. doi:10.21037/atm-21-3188. [Google Scholar] [PubMed] [CrossRef]
13. Sullivan RT, Handler SS, Feinstein JA, Ogawa M, Liu E, Ma M, et al. Subcutaneous treprostinil improves surgical candidacy for next stage palliation in single ventricle patients with high-risk hemodynamics. Semin Thorac Cardiovasc Surg. 2022;S1043–0679(22):00191–5. [Google Scholar]
14. Kido T, Burri M, Mayr B, Strbad M, Cleuziou J, Hager A, et al. Impacts of stage 1 palliation and pre-Glenn pulmonary artery pressure on long-term outcomes after Fontan operation. Eur J Cardiothorac Surg. 2021;60(2):369–76. doi:10.1093/ejcts/ezab079. [Google Scholar] [PubMed] [CrossRef]
15. Siddall E, Khatri M, Radhakrishnan J. Capillary leak syndrome: etiologies, pathophysiology, and management. Kidney Int. 2017;92(1):37–46. doi:10.1016/j.kint.2016.11.029. [Google Scholar] [PubMed] [CrossRef]
16. Skoro-Sajer N, Lang I, Naeije R. Treprostinil for pulmonary hypertension. Vasc Health Risk Manag. 2008;4(3):507–13. doi:10.2147/VHRM. [Google Scholar] [CrossRef]
17. Puri K, Adachi I. Mechanical support for the failing single ventricle at pre-fontan stage: current state of the field and future directions. Semin Thorac Cardiovasc Surg: Pediatr Card Surg Annu. 2021;24:10–8. doi:10.1053/j.pcsu.2021.04.004. [Google Scholar] [PubMed] [CrossRef]
Cite This Article
 Copyright © 2024 The Author(s). Published by Tech Science Press.
Copyright © 2024 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools