 Open Access
Open Access
REVIEW
The Effects of Laser Therapy in Treating Hypertrophic Scars and Keloids after Median Sternotomy: A Scoping Review
1 Adult Congenital Heart Disease Unit, IRCCS Policlinico San Donato, San Donato Milanese, Milan, 20097, Italy
2 Dermatology and Cosmetology Unit, IRCCS Ospedale San Raffaele, Milan, 20132, Italy
3 Faculty of Medicine and Surgery, Vita-Salute San Raffaele University, Milan, 20132, Italy
4 Health Professions Research and Development Unit, IRCCS Policlinico San Donato, San Donato Milanese, Milan, 20097, Italy
5 Department of Congenital Cardiac Surgery, IRCCS Policlinico San Donato, San Donato Milanese, Milan, 20097, Italy
6 Cardiac Surgery, IRCCS Policlinico San Donato, San Donato Milanese, Milan, 20097, Italy
7 Department of Biomedical Sciences for Health, University of Milan, Milan, 20133, Italy
* Corresponding Author: Laura Schianchi. Email:
Congenital Heart Disease 2024, 19(4), 363-374. https://doi.org/10.32604/chd.2024.053999
Received 15 May 2024; Accepted 29 August 2024; Issue published 31 October 2024
Abstract
Background: Hypertrophic scars and keloids, common complications following median sternotomy for cardiac surgery, significantly impact patient quality of life due to their aesthetic and symptomatic burden. Recent advancements in laser therapy have made it a prominent option for managing these complex scars, yet a comprehensive understanding of its efficacy is lacking. The aim of this scoping review is to explore the effects of laser therapy in managing hypertrophic scars and keloids after median sternotomy. Methods: This scoping review analyzed studies up to February 2024 from databases including PubMed, EMBASE, CINAHL, Scopus, Web of Science, and the Cochrane Library. We included any study that assessed laser therapy’s effects on hypertrophic scars and keloids following median sternotomy. Studies were selected based on predefined inclusion criteria without publication year, design, or origin restrictions. Results: Six studies met the inclusion criteria, involving a total of five RCTs and one review. These studies primarily tested 585 and 595-nm pulsed dye laser (PDL) treatments, focusing on scar appearance, patient symptoms, and treatment satisfaction. Most studies reported significant improvements in scar height reduction and patient symptom relief after treatment, with mixed results for scar erythema and elasticity. Adverse events were generally mild and transient. Conclusions: Laser therapy offers a beneficial approach for improving the appearance and symptoms of hypertrophic scars and keloids post-median sternotomy. However, further research is necessary to optimize treatment parameters and explore the long-term psychosocial impacts of this therapy. This review highlights the need for more comprehensive studies to establish standardized treatment protocols and evaluate their effectiveness.Keywords
Supplementary Material
Supplementary Material FilePatients undergoing cardiac surgery may develop post-operative complications, which can significantly impact their quality of life [1]. Post-operative adverse events have been associated with negative mental health outcomes, including delirium, anxiety, and depression [2]. In this context, the development of abnormal sternotomy scars following open-heart surgery may contribute to long-term patient morbidity [3]. Abnormal scars may range from hypertrophic to keloid and are reported to occur in 32% to 72% of patients [4].
A study in Europe involving Caucasian patients undergoing major cardiac surgery with median sternotomy and cardiopulmonary bypass reported an incidence of hypertrophic scar formation of about 30%, with an increased risk observed in young patients [5]. Conversely, keloids, though rarer, exhibit a higher prevalence in people of African and Asian descent, with rates varying from 0.09% in Europeans to 16% among the African population [6]. Hypertrophic scars result from an exaggerated inflammatory response in the healing process, characterized by rapid fibroblast growth, new blood vessel formation, and substantial collagen deposition. These scars may develop from various types of injuries, including burns, surgical wounds, and dermatitis, with surgeries being one of the leading causes [6]. While most post-surgical scars are deemed aesthetically and functionally acceptable, hypertrophic or keloidal scars may lead to significant aesthetic, psychological, and social distress [7].
Patients with complex sternotomy scars frequently report issues such as unsightliness, pain, itching, and restricted movement [8]. Moreover, these scars can have adverse effects on mental and social well-being, significantly impacting body image and influencing various aspects of daily life [9]. For instance, a substantial number of individuals with sternotomy scars have indicated that the scars negatively affect their self-esteem and self-confidence [10]. Women are more likely than men to express dislike or hatred towards their sternotomy or thoracotomy scars [11]. This observation is supported by literature describing that women with sternal scars reported that the scars made them feel less attractive despite reassurances from their partners [12,13]. Studies suggest that women may be more concerned about body image than men due to the significant societal pressure regarding their appearance [12,13].
The profound impact of sternotomy scars on both patients and their families underscores the urgent need for effective clinical interventions to enhance their quality of life. Despite the plethora of treatment options available, none currently offer definitive results for hypertrophic scars and keloids, creating a complex landscape for treatment selection [6,13]. This variability in outcomes and the significant costs associated with these therapies place a substantial financial burden on both government healthcare systems and patient families [14]. Meanwhile, laser technology has emerged as a leading treatment for various scar types, including those from extensive burns, due to its ability to coagulate microvasculature up to a depth of 1.2 mm in the dermis [15]. This technological advancement, while promising, highlights a critical gap in the current understanding and application of scar treatment—particularly, the effects of laser therapy on sternotomy-related scars have not been thoroughly evaluated [16]. This gap drives the necessity for a focused review of the literature, aiming to consolidate current knowledge on laser treatment outcomes for these specific scars and to identify areas lacking robust evidence. This scoping review intends to systematically explore the impact of laser therapy in managing hypertrophic scars and keloids following median sternotomy, aiming to summarize effective practices and pinpoint ongoing deficiencies in the field.
This study utilized a scoping review methodology conducted in accordance with Joanna Briggs Institute (JBI) manual [17]. Scoping reviews are particularly useful when the objective is to map the existing literature on a broad topic to identify key concepts, types of evidence, and gaps in research [18]. This approach is appropriate when investigating laser therapy for sternotomy scars because the topic is complex and multifaceted, potentially involving diverse intervention models, outcomes, and patient populations. Therefore, we conducted a scoping review to synthesize the existing literature on using laser therapy for treating sternotomy scars in patients who have undergone cardiac surgical procedures. We structured our research reporting and the presentation of results according to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis, specifically the extension for Scoping Reviews (PRISMA-ScR) [19].
The “Population, Concept, Context” (PCC) framework guided our search strategy [18]. This scheme defined our population as patients of any age who have undergone median sternotomy, the concept of various laser modalities used for scar treatment, and the context of any clinical setting or geographical location.
We focused on patients of all ages who have undergone a median sternotomy, a common surgical procedure used primarily in major heart surgeries. This demographic was chosen to explore the broad implications of post-operative sternal scar treatment, covering a wide age range, to understand potential variations in treatment outcomes across different life stages.
The concept central to our review is the application of various laser modalities for the treatment of scars. This concept includes, but is not limited to, different types of laser technologies, such as ablative lasers, which remove layers of skin; non-ablative lasers, which stimulate collagen production and skin rejuvenation without damaging the skin surface; and fractional lasers, which create microthermal treatment zones to induce tissue repair. The aim was to evaluate these diverse technologies’ effects, safety, and patient outcomes in managing sternotomy scars.
Our review was not limited to any specific clinical setting or geographical location. This broad context allowed us to capture a wide array of clinical applications and healthcare environments, from advanced tertiary hospitals in urban areas to smaller clinics in rural settings across different countries. This inclusiveness helped us understand how different healthcare infrastructures and local practices can influence the effectiveness and accessibility of laser treatments for sternotomy scars.
The selection of studies for this review was based on specific eligibility criteria designed to encompass a comprehensive range of literature. We included studies written in either English or Italian and focused on the effects of laser therapy on median sternotomy scars in patients of any age. To ensure a thorough exploration of the topic, we did not impose any restrictions regarding the year of publication, study design, or country of origin. This broad approach allowed us to capture the full spectrum of existing research related to our topic of interest. However, we excluded studies that investigated the effects of laser treatments on sternotomy scars in conjunction with other types of scars, such as those resulting from burns or other surgical procedures, to maintain a clear focus on the specific impacts of laser therapy on sternotomy scars alone.
2.4 Databases and Other Sources
Our literature review, comprehensive up to February 2024, encompassed several key databases and alternative sources. We searched PubMed, Embase, the Cumulative Index to Nursing and Allied Health Literature (CINAHL), Scopus, Web of Science (WoS), and the Cochrane Library. Additionally, we explored the grey literature through electronic platforms such as ResearchGate and Google Scholar to capture non-peer-reviewed studies and ongoing research. This multi-source strategy ensured a broad and inclusive collection of relevant data on the effects of laser therapy on median sternotomy scars.
Our search strategy was crafted based on the PCC framework. We customized the search terms for each electronic database consulted to align our queries with each database’s unique syntax and capabilities. We used the Boolean operator AND to combine the PCC criteria—ensuring that all elements were addressed in each search—while the OR operator was employed to enhance the sensitivity of the search within each individual criterion. Additionally, Medical Subject Headings (MeSH) terms were strategically utilized to further refine the search queries, allowing for more precise retrieval of relevant literature. The final versions of these search queries were executed on the 6th of February 2024, ensuring that our data was as current as possible.
The query used in PubMed was: (“Sternotomy”[MeSH Terms] OR “Cardiac Surgical Procedures”[MeSH Terms] OR “Sternotom*”[TW] OR “Cardiac Surgical Procedur*”[TW]) AND ((“Laser Therapy”[Mesh] OR “Laser*”[TW]) AND ((“Cicatrix, Hypertrophic”[Mesh]) OR (“Cicatrix”[Mesh]) OR (“Cicatrix*”[TW]))). In Embase: (Sternotomy/exp OR ‘Cardiac Surgical Procedures’/exp OR Sternotom* OR ‘Cardiac Surgical Procedur*’) AND ((‘Laser Therapy’/exp OR Laser*) AND ((‘Cicatrix, Hypertrophic’/exp) OR (Cicatrix/exp) OR (Cicatrix*))). In CINAHL: (INDEXTERMS(Sternotomy) OR INDEXTERMS(“Cardiac Surgical Procedures”) OR TITLE-ABS-KEY(Sternotom*) OR TITLE-ABS-KEY(“Cardiac Surgical Procedur*”)) AND ((INDEXTERMS(“Laser Therapy”) OR TITLE-ABS-KEY(Laser*)) AND ((INDEXTERMS(“Cicatrix, Hypertrophic”)) OR (INDEXTERMS(Cicatrix)) OR (TITLE-ABS-KEY(Cicatrix*)))). In WoS: (ALL = Sternotomy OR ALL = “Cardiac Surgical Procedures” OR ALL = Sternotom* OR ALL = “Cardiac Surgical Procedur*”) AND ((ALL = “Laser Therapy” OR ALL = Laser*) AND ((ALL = “Cicatrix, Hypertrophic”) OR (ALL = Cicatrix) OR (ALL = Cicatrix*))). In Cochrane Library: ([mh Sternotomy] OR [mh “Cardiac Surgical Procedures”] OR Sternotom*:ti,ab,kw OR (“Cardiac Surgical” NEXT Procedur*):ti,ab,kw) AND (([mh “Laser Therapy”] OR Laser*:ti,ab,kw) AND (([mh “Cicatrix, Hypertrophic”]) OR ([mh Cicatrix]) OR (Cicatrix*:ti,ab,kw))).
The records retrieved from various electronic databases were initially imported into the reference management software. The first step in processing these records involved removing any duplicate entries. Subsequently, the titles and abstracts were screened to determine their relevance based on the review’s inclusion and exclusion criteria. Studies that appeared to meet these criteria were then subjected to a thorough full-text review to confirm their suitability for inclusion in this scoping review.
A second author independently performed the same selection process to maintain objectivity and reliability in the study selection. This dual-review approach ensured the consistency and accuracy of the study’s inclusion. Discrepancies between reviewers regarding the eligibility of certain studies were resolved through discussion. In cases where consensus could not be reached, a third reviewer was consulted to provide an additional opinion and resolve any conflicts.
The outcomes of the search and the selection process were meticulously documented and organized following the guidelines of the PRISMA-ScR [19]. This structured approach facilitated transparency and comprehensiveness in reporting the review findings.
For an in-depth overview of the study selection process, please refer to the PRISMA flowchart illustrated in Fig. 1. The process began with identifying 74 records from the databases specified in our search strategy. The search did not yield additional studies from the grey literature. From these initial findings, 20 duplicate records were removed, leaving 54 titles and abstracts to be screened for relevance based on our inclusion criteria. Subsequent to this initial screening, 47 records were deemed ineligible and thus excluded from further consideration. The remaining 7 full-text articles were then carefully evaluated for eligibility. Of these, one article was excluded because its full text could not be retrieved online. Ultimately, 6 studies met all the pre-established eligibility criteria and were included in our scoping review.
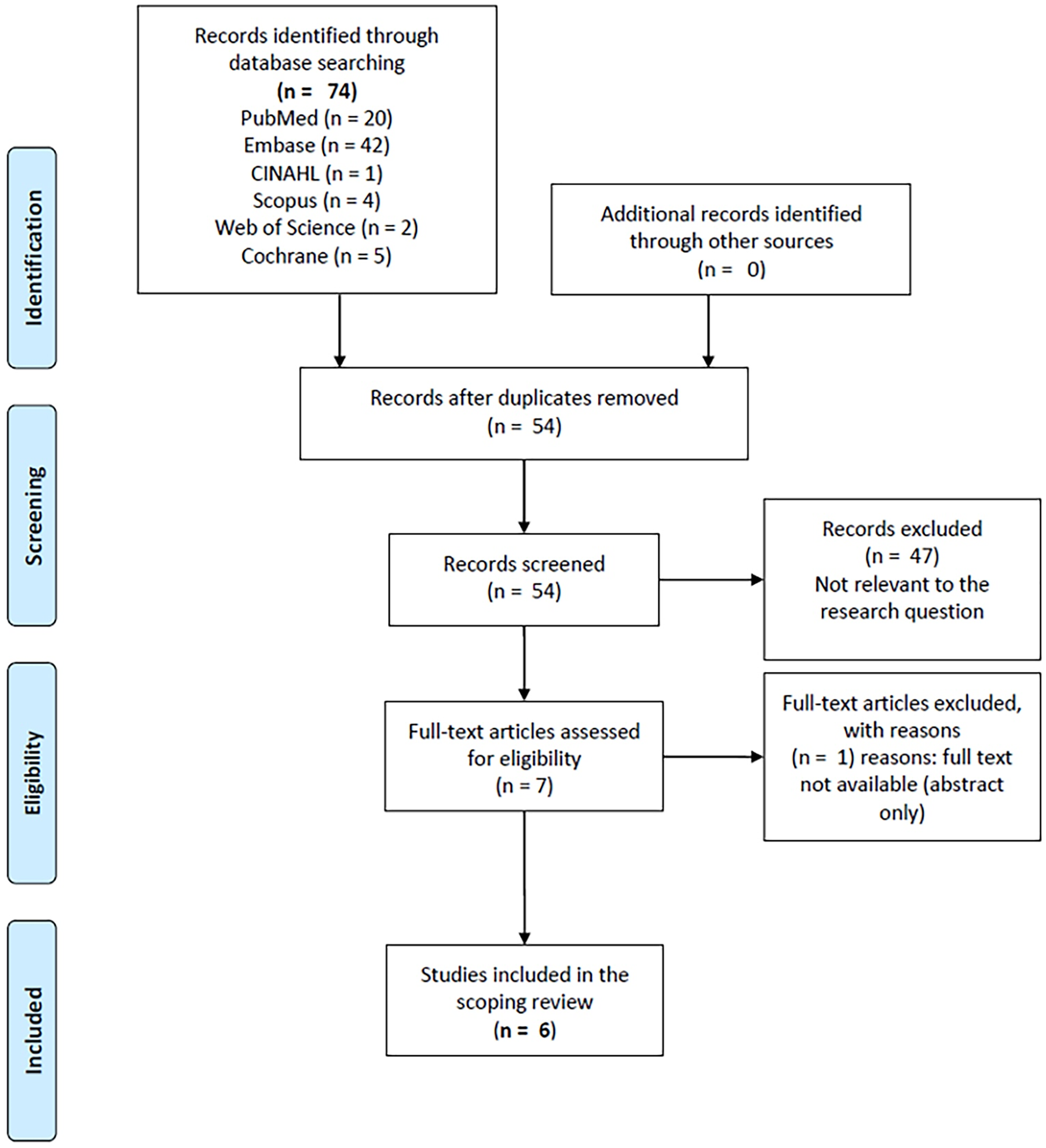
Figure 1: Flow diagram of the study selection process
A preliminary charting form was developed and tailored to align with the objectives of this scoping review to facilitate the data charting process. This form was designed to systematically capture essential information from the included studies. Key data points recorded included the outcomes identified in the reviewed literature, the intervention techniques employed, and the geographical diversity of the research. Additionally, significant findings regarding the effects of laser therapy were detailed in a narrative format, emphasizing the various outcome measures. Important aspects, such as the timing of treatments and any reported adverse events, were also documented. To ensure the accuracy and consistency of the data extracted, two authors independently charted the data. Subsequently, a third author reviewed the completed dataset to validate the findings and ensure that the charting adhered to the review’s stringent quality standards. This multi-author approach helped mitigate bias and reinforced the reliability of the data compilation process.
As shown in Table 1, this scoping review incorporated five randomized controlled trials (RCTs) and one review article, spanning publications from 1995 to 2011 [20–25]. The studies primarily involved adult participants with median sternotomy scars that were at least six months old and perceived by the patients as not healing well without any prior treatment. Geographically, only one RCT [22] and the review [20] were conducted in Europe, while the remaining studies originated from the USA [21,23–25].
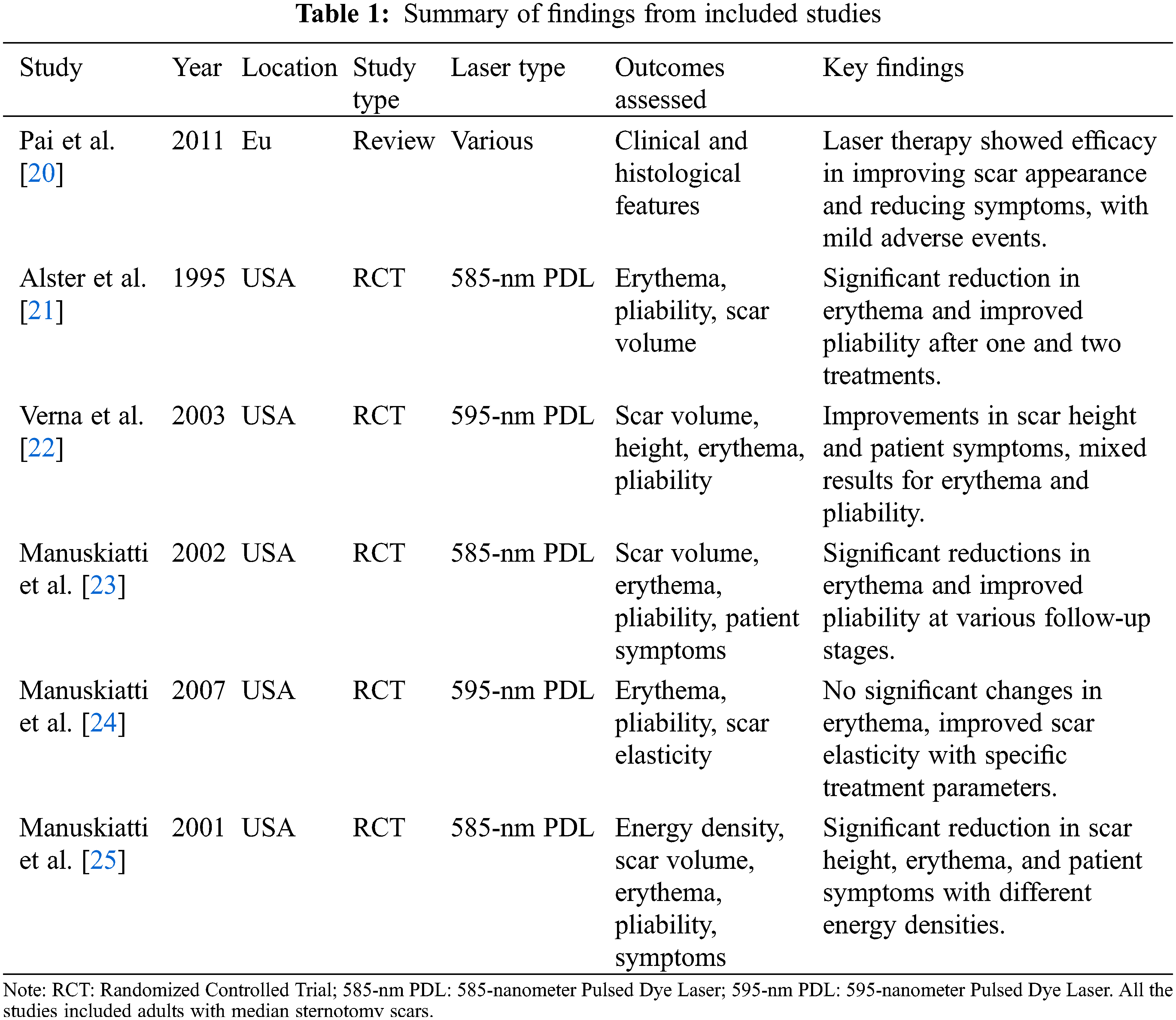
The interventions evaluated mainly involved two types of laser treatments: the 585-nm Pulsed Dye Laser (PDL) [25] and the 595-nm PDL [21,24]. The 595-nm PDL, which utilizes a longer wavelength, is considered a better option for patients with darker skin because it minimizes nonspecific damage to the pigmented epidermis compared to the 585-nm PDL. One of the RCTs, conducted by Manuskiatti et al. in 2001, specifically investigated the efficacy of the 585-nm PDL at varying energy densities (3, 5, and 7 J/cm2) [25]. Another study in 2007 explored the effects of the 595-nm PDL using different pulse widths (0.45 and 40 ms) [24].
Additionally, comparisons were made between laser radiation therapy and various other treatments, including intralesional triamcinolone acetonide (TAC), intralesional 5-fluorouracil (5-FU), combinations of TAC and 5-FU, silicone gel sheeting, and cryotherapy, as detailed in studies by Verna et al. in 2002 [22] and Manuskiatti et al. in 2003 [23]. These studies explored treating persistent sternotomy scars, highlighting the treatment’s relative efficacy and suitability for different skin types.
The included studies assessed several clinical and histological features of scars (see Table 1). Clinical features such as scar volume, height, erythema, and pliability were prominently evaluated, providing a quantitative basis for comparing treatment efficacy [21–25]. Histological analysis extended to examining changes in the epidermis, dermal sclerosis, and the presence of fibroblasts and mast cells, offering insights into the microscopic effects of the treatments [20–25]. Patient-reported symptoms, including pain, pruritus, tenderness, and burning sensations, were also frequently assessed, highlighting the subjective experiences related to scar treatment. Furthermore, immediate reactions to treatments and long-term adverse events were documented extensively in half of the studies, underscoring the safety profiles of the interventions.
3.3 Effects of Laser Therapy on Sternotomy Scar Clinical Features
The accumulated evidence from the included studies supports the efficacy of laser therapy in enhancing the clinical appearance of sternotomy scars (see Table 1). Notably, a significant reduction in scar height following laser treatment compared to baseline has been consistently reported across various studies [20,21,23–25]. However, results for erythema and pliability have been more variable, depending on the specific laser treatment parameters used [21–25].
For instance, Alster et al. observed a significant reduction in erythema after one and two treatments with a 585-nm PDL almost three decades ago, using a 450-ms pulse duration, a 5 mm spot size, and a fluence per pulse of 6.5–7.25 J/cm2 [21]. This study also noted improved pliability ratings after these treatments. Manuskiatti et al. further explored the 585-nm PDL with different energy densities over six treatment sessions, showing significant reductions in erythema by the 24th week and improved pliability in certain segments at various follow-up stages [25].
Another RCT indicated no significant differences in scar erythema between treated and untreated areas at any follow-up period. However, there were notable improvements in scar softness in treated segments at specific follow-ups [25]. A subsequent study by the same group found a significant reduction in erythema at week 32 with the 585-nm PDL, although no notable changes in softness were observed [24].
In a different setting, Manuskiatti et al. used the 595-nm PDL and did not observe any significant changes in scar erythema from the baseline up to 24 weeks, irrespective of the treatment settings [23]. However, this study reported significant improvements in the elasticity of scars treated with a 0.45-ms pulse width after three sessions, demonstrating that specific treatment parameters can influence the effectiveness of laser interventions on scar characteristics.
3.4 Effects of Laser Therapy on Patients’ Symptoms and Scar Perception
Laser therapy has shown considerable efficacy in alleviating pruritic or irritative sensations and reducing tenderness or burning after just one treatment session. This has led to high patient satisfaction with the therapy, as reported in studies by Alster et al. [21], Manuskiatti et al. [22], and Verna et al. [25]. Specifically, in the trial by Manuskiatti et al., patients experienced significant improvements in their symptoms, with 80% of participants (8 out of 10) in both the 3 and 5 J/cm2 irradiated segments reporting at least a 50% improvement [25]. In the 7 J/cm2 irradiated segments, 70% (7 out of 10) of patients reported similar levels of improvement.
Interestingly, even in non-laser-irradiated segments, 40% (4 out of 10) of the patients noted a 50% or greater improvement, suggesting some degree of placebo effect or systemic benefit from the treatment. However, it is important to note that most patients (60%, 6 out of 10) perceived little to no improvement in these untreated areas, rating them at either 0% or 25% improved. These findings underscore the potential of laser therapy not only in treating the physical aspects of sternotomy scars but also in enhancing patient perceptions and experiences related to scar symptoms.
The adverse events associated with laser therapy for sternotomy scars were generally mild and transient. During the laser treatment, approximately 90% of patients (9 out of 10) experienced a mild to moderate level of discomfort or pain, which they described as similar to the sensation of a rubber band snapping against the skin [24]. Additionally, purpuric discoloration and erosions secondary to blistering in the laser-treated areas were observed in two studies [24,25]. These side effects, however, were short-lived and resolved within a week with the application of a simple occlusive dressing using mupirocin ointment [25].
This scoping review aimed to explore the existing evidence on the effects of laser therapy for treating hypertrophic scars and keloids following median sternotomy in cardiac surgery patients [20–25]. We chose this study design due to the scarcity of comprehensive reviews and the limited published literature on the topic, which is crucial for assessing the feasibility of future primary studies. The review included six studies published over a span of 16 years, which collectively suggest that laser therapy is a viable treatment option for managing complicated sternotomy scars. This therapy improves scar appearance and alleviates patients’ symptoms with minimal and transient adverse events.
The main results indicate that laser therapy significantly improves scar appearance, with consistent reports of reductions in scar height and improvements in pliability and erythema [20,21,23–25]. Patient symptoms such as pain, pruritus, tenderness, and burning sensations were effectively alleviated, leading to high patient satisfaction. The adverse events associated with laser therapy were generally mild and transient, including discomfort during treatment and temporary purpuric discoloration and blistering, which resolved within a week. The review primarily evaluated the 585 and 595-nm PDL, finding the 595-nm PDL to be more suitable for patients with darker skin due to reduced nonspecific damage to the pigmented epidermis. Studies also explored different energy densities, pulse widths, and treatment sessions, indicating that specific parameters could influence the effects of laser therapy on scar characteristics.
This scoping review highlights several key differences between the patients, treatments used, and their efficacies across the included studies. These differences provide valuable insights into the factors that may influence the outcomes of laser therapy for hypertrophic scars and keloids following median sternotomy [20,21,23–25]. The studies primarily involved adult patients with median sternotomy scars that were at least six months old and perceived by the patients as not healing well without any prior treatment. While the majority of the studies were conducted in the USA, one study and a review were conducted in Europe. The patient populations varied slightly in terms of age and baseline scar characteristics, but all shared the common factor of having undergone cardiac surgery requiring a median sternotomy. This variability in patient demographics underscores the need to consider individual patient factors when assessing the efficacy of laser treatments in future research.
The 585-nm PDL was used in several studies and was effective in reducing erythema and improving scar pliability and height. The 595-nm PDL, which has a longer wavelength, was noted to be more suitable for patients with darker skin due to its reduced risk of nonspecific damage to the pigmented epidermis. Different studies explored various treatment parameters such as energy densities, pulse widths, and the number of treatment sessions. For instance, one study by Manuskiatti et al. investigated the efficacy of the 585-nm PDL at energy densities of 3, 5, and 7 J/cm2, demonstrating that higher energy densities were associated with greater improvements in scar characteristics [25]. Another study by the same group in 2007 examined the effects of different pulse widths (0.45 and 40 ms) using the 595-nm PDL, indicating that specific treatment settings can significantly influence treatment outcomes [24].
The described findings are supported by a recent systematic review of RCTs conducted over the past two decades, which examined the mitigation of post-surgical scars using various laser modalities and treatment protocols [26]. Most of these trials, which included the use of Diode, PDL, and CO2 lasers, demonstrated statistically significant improvements in scars managed with laser compared to control treatments. However, it is important to note that this review focused on general post-surgical scars, not specifically on scars resulting from cardiac surgery [26].
Regarding scar appearance, 5 out of 6 studies reported a statistically significant flattening of laser-treated segments compared to baseline [20,21,23–25]. This specific result is supported by recent research on burn scars, which found that various laser modalities effectively reduced scar thickness, particularly in thicker scars [27]. PDL has been shown to inhibit cell proliferation and reduce angiogenesis, both critical factors in abnormal scarring [26].
The results regarding erythema and pliability were mixed in the included literature. While one trial encompassed in our review indicated limited improvement over time with laser treatments [25], other recent studies have found that PDL lasers are particularly effective in reducing the erythema associated with vascular post-surgical scars [26]. A trial assessing the effectiveness of combined PDL and Non-ablative Fractional Laser (NAFL) treatment found significant improvements in scar thickness and stiffness as assessed by both patients and blinded physicians using the Patient and Observer Scar Assessment Scale (POSAS) [28].
In this scoping review, patients’ symptoms improved significantly after just one laser session, with high satisfaction levels reported in multiple trials [21,22,25]. It should be noted that these outcomes were not measured using validated tools, likely due to the age of the trials. The POSAS now appears to be the most appropriate tool for assessing the effects of laser treatment on all types of scars [26]. Consequently, there is a strong recommendation for more well-designed RCTs that include validated self-report scales to ensure reliable and accurate measurement of patient outcomes.
In addition, recent evidence highlights the advantages of early laser treatment for surgical scars [16,26,27]. Laser interventions are most beneficial when delivered within a month post-surgery [29], and this could also be true following median sternotomy, even if this aspect still requires testing. Best outcomes are typically seen after three sessions of PDL treatment, spaced between 2 to 10 weeks, beginning from the day sutures are removed [26]. This evidence suggests a critical window immediately after surgery where laser treatments could be most effective.
The decision to conduct a scoping review rather than a systematic review with meta-analysis was informed by the need first to map the research landscape’s breadth and depth. Such an approach is critical before undertaking a meta-analysis, as it helps to identify the range of available evidence, assess the consistency of study methodologies, and highlight areas requiring further investigation. Considering our findings, we also provided information to plan how to organize a priori hypotheses to explain the potential heterogeneity in a future meta-analysis by designing a priori meta-regression models and/or subgroup analysis based on several key factors that our study showed as possible sources of true differences between effects across studies: type of laser modality (e.g., 585, 595-nm PDL, ablative, non-ablative, fractional), treatment parameters (e.g., energy density, pulse duration, and number of treatment sessions), patient demographics, scar characteristics (hypertrophic vs. keloid), age of the scars, study design and quality scores,, and geographical areas. Therefore, this scoping review is a foundational step, encouraging more detailed and larger-scale studies that could support a comprehensive meta-analysis, providing clearer, evidence-based guidelines for treating scars in sensitive populations such as that of patients with congenital heart disease [30]. In this regard, future perspectives in the field of post-cardiac surgery, especially concerning patients with congenital heart disaese, highlight the critical need for tailored scar management strategies. As these patients often undergo multiple surgeries from a young age, minimizing and managing scarring is crucial for both physiological and psychological outcomes [31]. Advancements in laser therapy could be particularly transformative, focusing on early intervention protocols to optimize healing shortly after surgery. Further research should prioritize developing specific laser treatment guidelines. These initiatives should be supported by robust, well-designed clinical trials specifically targeting the population with congenital heart disease to refine current treatments and innovate new solutions that could significantly improve the patients’ quality of life.
Limitations
This scoping review has several limitations that warrant discussion. First, the specificity of the patient population (those undergoing median sternotomy) and the variability in scar types (hypertrophic and keloidal) may limit the generalizability of the findings to broader surgical contexts or other types of scars. Secondly, the small number of studies included and their potential methodological differences could impact the consistency and reliability of the aggregated results. Thirdly, the absence of validated measurement tools in most studies raises concerns about the accuracy of reported patient outcomes, emphasizing the need for updated research methodologies in future studies. Additionally, acknowledging the exploratory nature of the review, no quality assessment was conducted. This decision aligns with the scoping review methodology, which aims to map the existing literature rather than critically appraise the quality of individual studies. This approach, while providing a broad overview, limits the ability to assess the robustness of the findings comprehensively.
This scoping review has elucidated the potential benefits of laser therapy for treating hypertrophic scars and keloids following median sternotomy, particularly in post-cardiac surgery patients. The summarized evidence indicates that laser therapy could significantly improve scar appearance and alleviate symptoms with minimal adverse effects, supporting its viability as a therapeutic option. The limited scope and variability of the studies highlights the need for expanded research to ensure broader applicability and solidify laser therapy as a cornerstone in post-surgical scar management. The findings advocate for more comprehensive future research, particularly through well-designed randomized controlled trials incorporating validated measurement tools like the POSAS. Such studies should aim to refine treatment protocols to optimize patient outcomes, especially for early intervention. Furthermore, evidence is needed to support patients with CHD, who require a specific focus because they often endure multiple surgeries from an early age, leading to complex scarring issues.
Acknowledgement: We sincerely thank the authors of the studies included in this review. Their research and contributions have been fundamental in advancing our understanding of laser therapy for treating post-operative scars, particularly following median sternotomy.
Funding Statement: This research was partially funded by “Ricerca Corrente” funding from the Italian Ministry of Health to IRCCS Policlinico San Donato.
Author Contributions: The authors confirm their contributions to the paper as follows: study conception and design were led by Laura Schianchi, Rosario Caruso, and Massimo Chessa; Rosario Caruso, Arianna Magon, and Serena Francesca Flocco were involved in data collection; analysis and interpretation of results were conducted by Gianluca Conte, Karina Geraldina Zuniga Olaya, Erika Cioffi, Fabrizio Vaira, Matteo Riccardo Di Nicola, Giacomo Bortolussi, and Santo Raffaele Mercuri. Laura Schianchi prepared the draft manuscript. All authors reviewed the results and approved the final version of the manuscript.
Availability of Data and Materials: No original data are available as this work is a review of existing literature. All the materials and data used in this review are derived from previously published studies. Access to the detailed data from these studies can be requested directly from the corresponding authors of the individual articles.
Ethics Approval: Not applicable.
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
Supplementary Materials: The supplementary material is available online at https://doi.org/10.32604/chd.2024.053999.
References
1. Matsuda M, Takemura H, Yamashita A, Matsuoka Y, Sawa T, Amaya F. Post-surgical chronic pain and quality of life in children operated for congenital heart disease. Acta Anaesthesiol Scand. 2019;63(6):745–50. doi:10.1111/aas.2019.63.issue-6. [Google Scholar] [CrossRef]
2. Tigges-Limmer K, Sitzer M, Gummert J. Perioperative psychological interventions in heart surgery-opportunities and clinical benefit. Dtsch Arztebl Int. 2021;118(19):339–45. [Google Scholar] [PubMed]
3. Brocki BC, Thorup CB, Andreasen JJ. Precautions related to midline sternotomy in cardiac surgery: a review of mechanical stress factors leading to sternal complications. Eur J Cardiovasc Nurs. 2010;9(2):77–84. doi:10.1016/j.ejcnurse.2009.11.009. [Google Scholar] [PubMed] [CrossRef]
4. Berman B, Maderal A, Raphael B. Keloids and hypertrophic scars: pathophysiology, classification, and treatment. Dermatol Surg. 2017;43(1):S3–18. doi:10.1097/DSS.0000000000000819. [Google Scholar] [PubMed] [CrossRef]
5. Chello C, Nenna A, Chello M, Satriano UM, Cardetta F, Lusini M, et al. Statin treatment and hypertrophic scarring after cardiac surgery. Wound Repair Regen. 2021;29(1):129–33. doi:10.1111/wrr.v29.1. [Google Scholar] [CrossRef]
6. Knowles A, Glass DA. Keloids and hypertrophic scars. Dermatol Clin. 2023;41(3):509–17. doi:10.1016/j.det.2023.02.010. [Google Scholar] [PubMed] [CrossRef]
7. Frech FS, Hernandez L, Urbonas R, Zaken GA, Dreyfuss I, Nouri K. Hypertrophic scars and keloids: advances in treatment and review of established therapies. Am J Clin Dermatol. 2023;24(2):225–45. doi:10.1007/s40257-022-00744-6. [Google Scholar] [PubMed] [CrossRef]
8. Nakamura K. Factors affecting hypertrophic scar development in median sternotomy incisions for congenital cardiac surgery. J Am Coll Surg. 1997;185(3):218–23. doi:10.1016/S1072-7515(97)00059-8. [Google Scholar] [PubMed] [CrossRef]
9. Ngaage M, Agius M. The psychology of scars: a mini-review. Psychiatr Danub. 2018;30(Suppl 7):633–8. [Google Scholar] [PubMed]
10. Hsieh JC, Maisel-Campbell AL, Joshi CJ, Zielinski E, Galiano RD. Daily quality-of-life impact of scars: an interview-based foundational study of patient-reported themes. Plast Reconst Surg—Global Open. 2021 Aprile 15;9(4):e3522. doi:10.1097/GOX.0000000000003522. [Google Scholar] [PubMed] [CrossRef]
11. Crossland DS, Jackson SP, Lyall R, Hamilton JRL, Hasan A, Burn J, et al. Patient attitudes to sternotomy and thoracotomy scars. Thorac cardiovasc Surg. 2005 Aprile;53(2):93–5. doi:10.1055/s-2004-830422. [Google Scholar] [PubMed] [CrossRef]
12. Kirshbom PM, Myung RJ, Simsic JM, Kramer ZB, Leong T, Kogon BE, et al. One thousand repeat sternotomies for congenital cardiac surgery: risk factors for reentry injury. Ann Thorac Surg. 2009;88(1):158–61. doi:10.1016/j.athoracsur.2009.03.082. [Google Scholar] [PubMed] [CrossRef]
13. Lipman K, Wang M, Berthiaume E, Holloway J, Da Lio A, Ting K, et al. Evaluating current scar assessment methods. Ann Plast Surg. 2020;84(2):222–31. doi:10.1097/SAP.0000000000002029. [Google Scholar] [PubMed] [CrossRef]
14. Gauglitz GG. Management of keloids and hypertrophic scars: current and emerging options. Clin Cosmet Investig Dermatol. 2013;6:103–14. doi:10.2147/CCID.S35252. [Google Scholar] [PubMed] [CrossRef]
15. Alster TS, Handrick C. Laser treatment of hypertrophic scars, keloids, and striae. Semin Cutan Med Surg. 2000;19(4):287–92. doi:10.1053/sder.2000.18369. [Google Scholar] [PubMed] [CrossRef]
16. Chowdhury B, Kassir M, Salas-Alanis J, Nistico S, Galadari H, Fritz K, et al. Laser in surgical scar clearance: an update review. J Cosmet Dermatol. 2021;20(12):3808–11. doi:10.1111/jocd.v20.12. [Google Scholar] [CrossRef]
17. Aromataris E, Munn Z. JBI Manual for Evidence Synthesis. JBI; 2020. doi:10.46658/JBIMES-24-01. [Google Scholar] [CrossRef]
18. Pollock D, Peters MDJ, Khalil H, McInerney P, Alexander L, Tricco AC, et al. Recommendations for the extraction, analysis, and presentation of results in scoping reviews. JBI Evid Synth. 2023;21(3):520–32. doi:10.11124/JBIES-22-00123. [Google Scholar] [PubMed] [CrossRef]
19. Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–73. doi:10.7326/M18-0850. [Google Scholar] [PubMed] [CrossRef]
20. Pai VB, Cummings I. Are there any good treatments for keloid scarring after sternotomy? Inter Cardiovas Thora Sur. 2011;13(4):415–8. [Google Scholar]
21. Alster TS, Williams CM. Treatment of keloid sternotomy scars with 585 nm flashlamp-pumped pulsed-dye laser. Lancet. 1995;345(8959):1198–200. doi:10.1016/S0140-6736(95)91989-9. [Google Scholar] [PubMed] [CrossRef]
22. Verna G, Devalle L, Baglioni E, Renditore S, Cravero L, Kefalas N, et al. Sternal region keloids treatment: a comparative study between cryotherapy and laser therapy. Riv Ital Chir Plast. 2003;35(1–2):15–9. [Google Scholar]
23. Manuskiatti W, Fitzpatrick RE. Treatment response of keloidal and hypertrophic sternotomy scars: comparison among intralesional corticosteroid, 5-fluorouracil, and 585-nm flashlamp-pumped pulsed-dye laser treatments. Arch Dermatol. 2002 Settembre;138(9):1149–55. doi:10.1001/archderm.138.9.1149. [Google Scholar] [PubMed] [CrossRef]
24. Manuskiatti W, Wanitphakdeedecha R, Fitzpatrick RE. Effect of pulse width of a 595-nm flashlamp-pumped pulsed dye laser on the treatment response of keloidal and hypertrophic sternotomy scars. Dermatol Surg. 2007;33(2):152–61. [Google Scholar] [PubMed]
25. Manuskiatti W, Fitzpatrick RE, Goldman MP. Energy density and numbers of treatment affect response of keloidal and hypertrophic sternotomy scars to the 585-nm flashlamp-pumped pulsed-dye laser. J Am Acad Dermatol. 2001;45(4):557–65. doi:10.1067/mjd.2001.116580. [Google Scholar] [PubMed] [CrossRef]
26. Artzi O, Friedman O, Al-niaimi F, Wolf Y, Mehrabi JN. Mitigation of postsurgical scars using lasers: a review. Plast Reconst Surg–Global Open. 2020;8(4):e2746. doi:10.1097/GOX.0000000000002746. [Google Scholar] [PubMed] [CrossRef]
27. Cooper LE, Nuutila K, Kemp Bohan PM, Diaz V, Batchinsky M, Carlsson AH, et al. Analysis of the utility of CO2 and pulse-dye lasers together and separately in the treatment of hypertrophic burn scars. Ann Plast Surg. 2022 Agosto;89(2):166–72. doi:10.1097/SAP.0000000000003240. [Google Scholar] [PubMed] [CrossRef]
28. Kang BY, Ibrahim SA, Weil A, Reynolds KA, Johnson T, Wilson S, et al. Treatment of surgical scars with combination pulsed dye and fractional nonablative laser: a randomized controlled trial. Annals Surg. 2022;276(6):975–80. doi:10.1097/SLA.0000000000005377. [Google Scholar] [PubMed] [CrossRef]
29. Kent RA, Shupp J, Fernandez S, Prindeze N, DeKlotz CMC. Effectiveness of early laser treatment in surgical scar minimization: a systematic review and meta-analysis. Dermatol Surg. 2020;46(3):402–10. doi:10.1097/DSS.0000000000001887. [Google Scholar] [PubMed] [CrossRef]
30. Flocco SF, Dellafiore F, Caruso R, Giamberti A, Micheletti A, Negura DG, et al. Improving health perception through a transition care model for adolescents with congenital heart disease. J Cardiovasc Med. 2019;20(4):253–60. doi:10.2459/JCM.0000000000000770. [Google Scholar] [PubMed] [CrossRef]
31. Flocco SF, Caruso R. Advancing high-value transitional care: the central role of nursing and its leadership. In: Guide for advanced nursing care of the adult with congenital heart disease. 2022. p. 45–53. [Google Scholar]
Cite This Article
 Copyright © 2024 The Author(s). Published by Tech Science Press.
Copyright © 2024 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools