 Open Access
Open Access
CASE REPORT
Case Report: Surgical Correction of Transposition of the Great Arteries with Aortopulmonary Window
1 Department of Cardiothoracic Surgery, Children’s Hospital of Fudan University, Shanghai, 201102, China
2 Department of Pediatrics, Children’s Hospital of Fudan University (Xiamen Branch), Xiamen Children’s Hospital, Xiamen, 361006, China
* Corresponding Authors: Wenbo Zhang. Email: ; Ming Ye. Email:
Congenital Heart Disease 2024, 19(3), 275-278. https://doi.org/10.32604/chd.2024.051370
Received 04 March 2024; Accepted 18 April 2024; Issue published 26 July 2024
Abstract
Introduction: Transposition of the great arteries (TGA) with aortopulmonary window is a rare type of congenital heart disease with limited experience. We reported a neonate aged 25 days receiving the arterial switch operation and assisted with extracorporeal membrane oxygenation. Conclusion: TGA with aortopulmonary window can be safely correctly with the arterial switch operation.Keywords
Nomenclature
| TGA | Transposition of the great arteries |
| ASO | Arterial switch operation |
Transposition of the great arteries (TGA) is a commonly seen kind of complex congenital heart disease and needs timely surgical intervention in the neonatal period due to hypoxia and left ventricle degeneration. The arterial switch operation (ASO) has been reported with excellent clinical outcomes [1,2]. However, TGA with a large aortopulmonary window (APW) is a rare case with relatively complicated hemodynamic properties. Only a few cases have been reported and most of the cases were with a ventricular septal defect (VSD) [3,4]. Here we introduce a case with TGA/intact ventricular septum (IVS) and APW successfully corrected by the ASO procedure.
A term male newborn with a birth weight of 3 kg was transferred to our cardiac center due to hypoxia and heart murmur 1 day after birth. Echocardiography in our institution showed dextro-TGA/IVS with APW (type I) and no patent ductus arteriosus (PDA) was found (Fig. 1). Preoperative cardiac computed tomography (CT) proved the diagnosis and showed APW 7 mm above the pulmonary valve. The CT also showed coronary artery anatomy 1 LAD, Cx, and 2 RCA according to the Leiden classification. An elective arterial switch operation (ASO) was performed at 25 days with a body weight of 3.8 kg.
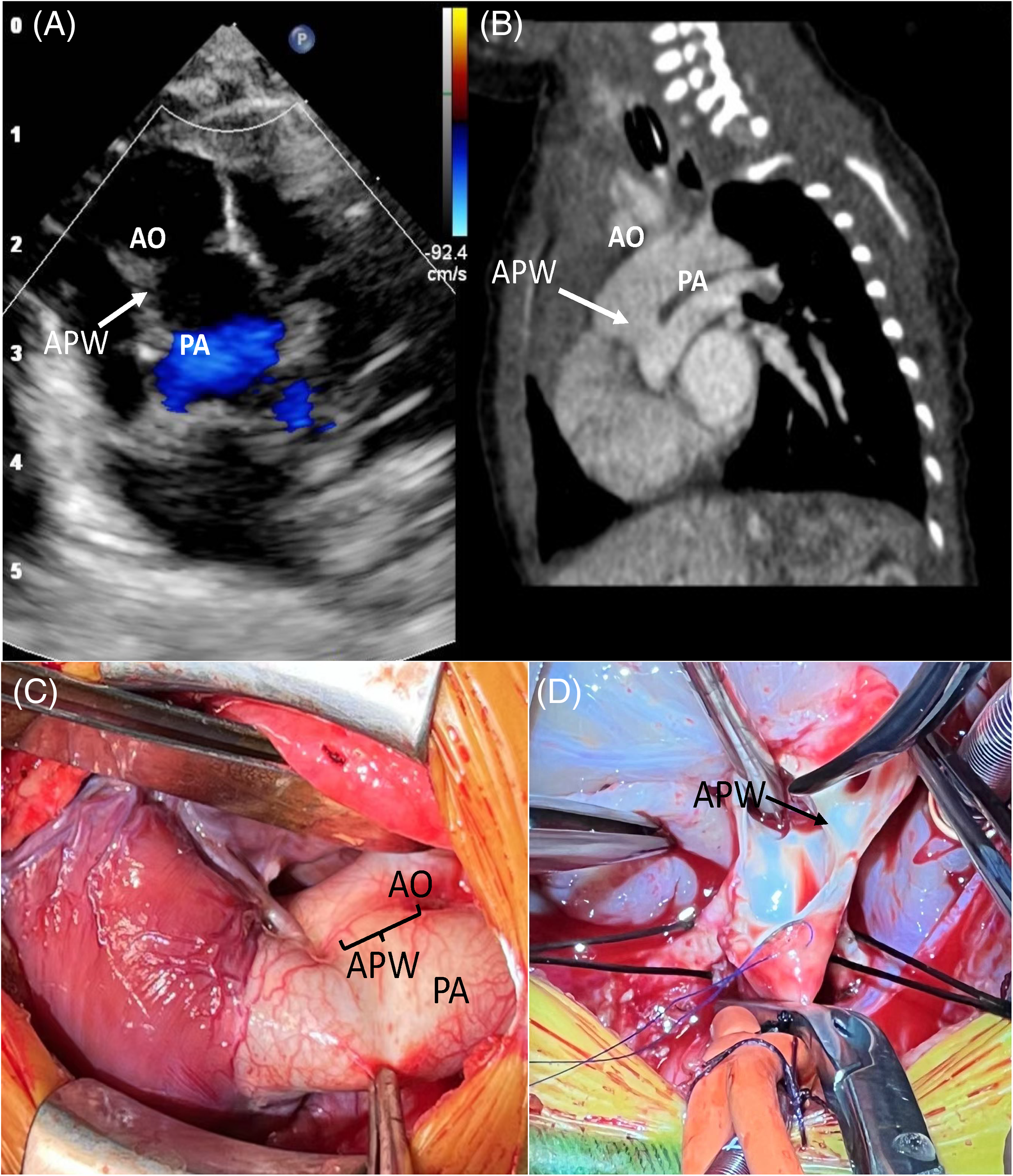
Figure 1: Preoperative echocardiography (A), computed tomography (CT) (B), and direct view (C, D) of this case. AO: Aorta, PA: Pulmonary artery; APW: Aortopulmonary window
We first inspected the anatomy of the coronary arteries and it turned out to be coherent with the CT scan. The APW was divided, and the main pulmonary artery and the aorta were transected at the distal side of the APW after routine cardiopulmonary bypass. The size of the APW was around 10 mm and the proximal anterior wall of the neoaorta was only 6–7 mm. After two coronary artery buttons were excised and anastomosed, we mobilized the branch pulmonary arteries to the hilum, and the LeCompte maneuver was performed. The distal end of the ascending aorta was then anastomosed directly to the pulmonary root, followed by right atriotomy and closure of patent foramen ovale. The neopulmonary was then reconstructed with an autologous pericardium patch. The heart recovered well after removing the aorta cross-clamp while the left ventricle became distended when decreasing the flow rate. The cardiopulmonary bypass time was 200 min and the aorta cross-clamp time was 122 min. Extracorporeal membrane oxygenation (ECMO) was finally applied after the surgery and weaned off 6 days after the ASO. Tracheal intubation was removed 2 days later and discharged 12 days later. The patient was followed up for 4 months and is growing well.
TGA/IVS is one of the most commonly seen cyanotic congenital heart diseases that needs timely surgery due to severe hypoxia and potential left ventricle degeneration. In this case, preoperative examination showed that the interaction between systemic and pulmonary circulation through APW is adequate to maintain oxygenation, and pulmonary artery pressure is presumably high enough to keep the left ventricle functioning. The ASO procedure was nothing special while problems occurred when weaning off cardiopulmonary bypass. One possible reason for that is the left ventricle degeneration at the time of the surgery. We usually perform the ASO for TGA/IVS patients 3–7 days after birth. The patient was transferred to our center 2 days after birth and we delayed the ASO procedure till three weeks later hoping for a larger aortic anterior wall. Though no signs of LV dysfunction were noticed before the surgery, an earlier intervention may help. Another possible reason is pulmonary artery hypertension. ECMO was a useful tool for patients with left ventricle dysfunction or pulmonary artery hypertension and it did help this patient. Only around twenty cases were reported with TGA and APW before and ECMO was not applied in these cases [5]. Our experience, including preoperative and postoperative management, might be a useful complement to these rare cases.
ASO for TGA with APW is appropriate while the timing of intervention needs careful evaluation. Pulmonary congestion caused by the unrestricted system to pulmonary shunt through APW and possible LV degeneration by TGA may require timely intervention.
Acknowledgement: All authors thank their surgery and nurse team.
Funding Statement: The authors received no specific funding for this study.
Author Contributions: The authors confirm contribution to the paper as follows: study conception and design: M. Ye, Q. Shi; data collection: Q. Shi, X. Lei; analysis and interpretation of results: X. Lei, W. Zhang; draft manuscript preparation: Q. Shi, X. Lei. All authors reviewed the results and approved the final version of the manuscript.
Availability of Data and Materials: None.
Ethics Approval: Ethic approval was waived due to its retrospective nature.
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
References
1. Fricke TA, Buratto E, Weintraub RG, Bullock A, Wheaton G, Grigg L, et al. Long-term outcomes of the arterial switch operation. J Thorac Cardiovasc Surg. 2022;163(1):212–9. doi:10.1016/j.jtcvs.2021.01.134. [Google Scholar] [PubMed] [CrossRef]
2. Nguyen MT, Doan AV, Tran VQ, Mai DD, Nguyen UH, Thinh Nguyen TL. The arterial switch operation in the developing world: risk factors and current outcomes. Ann Thorac Surg. 2024;117(3):543–9. doi:10.1016/j.athoracsur.2023.07.048. [Google Scholar] [PubMed] [CrossRef]
3. Krishnan P, Airan B, Shrivastava S, Rajani S, Rao IM, et al. Complete transposition of the great arteries with aortopulmonary window: surgical treatment and embryologic significance. J Thorac Cardiovasc Surg. 1991;101(4):749–51. [Google Scholar] [PubMed]
4. McKay M, Eisenring C, Greiten L, Reemtsen B. Arterial switch operation for complex d-transposition of the great arteries with aortopulmonary window. JTCVS Tech. 2023;19:123–4. doi:10.1016/j.xjtc.2023.02.013. [Google Scholar] [PubMed] [CrossRef]
5. Mishra A, Gandhi H, Sharma P, Patel H, Parmar D, Sheth M, et al. Transposition of great arteries with aortopulmonary window: our surgical experience. Ann Thorac Surg. 2014;97(1):196–201. doi:10.1016/j.athoracsur.2013.07.012. [Google Scholar] [PubMed] [CrossRef]
Cite This Article
 Copyright © 2024 The Author(s). Published by Tech Science Press.
Copyright © 2024 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools