 Open Access
Open Access
CASE REPORT
Bicuspidization Using the Open-Sleeve Technique for Congenital Aortic Stenosis during Infancy
Departments of Cardiovascular Surgery, Mt. Fuji Shizuoka Children’s Hospital, Shizuoka, 420-8660, Japan
* Corresponding Author: Toshi Maeda. Email:
Congenital Heart Disease 2024, 19(2), 177-183. https://doi.org/10.32604/chd.2024.050945
Received 23 February 2024; Accepted 15 April 2024; Issue published 16 May 2024
Abstract
Congenital aortic stenosis (cAS) frequently requires intervention during the neonatal or infantile period. However, surgical repair is challenging because of the narrow surgical space. We performed bicuspidization using the open-sleeve technique for cAS with a unicuspid aortic valve in two patients. Postoperatively, the patients were doing well without reintervention for the aortic valve for 8 and 6 years, respectively. Their aortic annular diameter increased along with somatic growth. Bicuspidization for neonates or infancy can be performed safely using the open-sleeve technique as its midterm results have been satisfactory.Graphic Abstract
Keywords
Congenital aortic stenosis (cAS) is a severe congenital heart disease that requires intervention during the neonatal or infantile period. Although balloon valvuloplasty (BVP) is a treatment option, surgery should be performed when aortic regurgitation (AR) is concurrently observed or BVP is ineffective. However, surgery is usually challenging because of the narrow surgical space and the complex form of the valves, such as the unicuspid aortic valve.
We previously reported an open-sleeve technique [1,2] for aortic valve repair with good surgical space. However, no studies have reported its mid- or long-term results. We herein report two cases and mid-term results of bicuspidization using the open-sleeve technique for cAS. This study has been approved by the institutional review board (Mt. Fuji Shizuoka Children’s Hospital, ID: 61). Informed consent was obtained from the parents of the patients.
A male neonate, weighing 2.18 kg, delivered spontaneously at 38 weeks was diagnosed with cAS immediately following birth. BVP was performed at 2 days, which led to a slight improvement in cAS. However, AR became severe, and acute heart failure developed. Thus, urgent surgery was planned. Transthoracic echocardiography revealed that his aortic annular diameter was 6.4 mm (103% of the normal annular diameter, Z score = 0.34) with an unicuspid aortic valve (Figs. 1A and 1B). During surgery, the aortic valve was exposed through transverse transection of the aorta 4 mm above the sinotubular junction under cardioplegic arrest. The aortic valve was functionally unicuspid with a well-developed posterior (left−none) commissure and less-developed anterior (left−right) commissure. The aorta was longitudinally incised at the anterior commissure to the ventriculoaortic junction (the open-sleeve technique) [1,2].
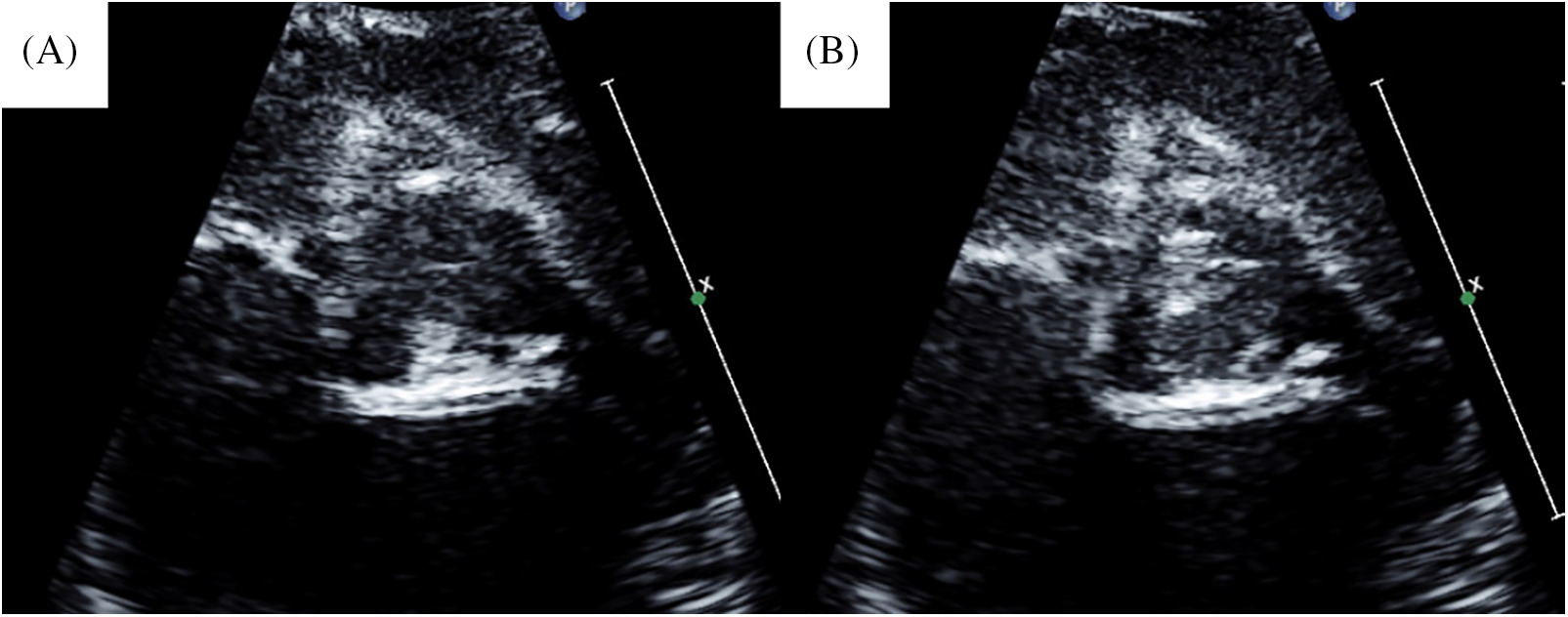
Figure 1: Preoperative echocardiogram of case 1. (A) Preoperative image in diastolic phase. (B) Preoperative image in systolic phase
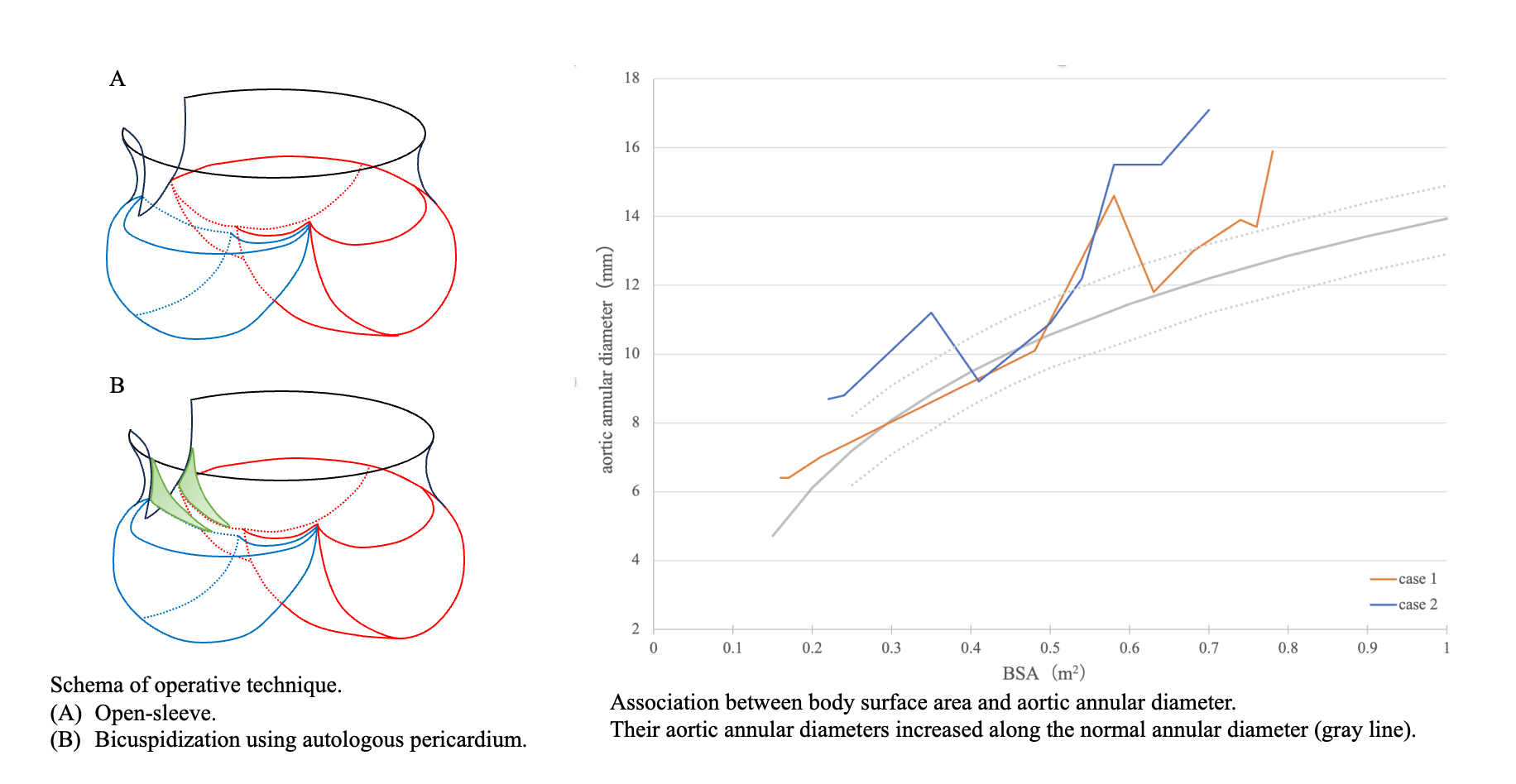
Simultaneously, the left and right cusps were divided at the anterior commissure. Both cusps were sliced to improve mobilization. We performed bicuspidization by commissuroplasty [3] using glutaraldehyde-treated (3 min) autologous pericardium (Figs. 2 and 3). The commissure was made along the longitudinal aortotomy site. Concomitantly, we performed coronary ostium augmentation of the left coronary artery. The cardiopulmonary bypass and cardiac arrest times were 157 and 87 min, respectively. Postoperatively, no AR was observed, and the peak velocity through the aortic valve was 1.9 m/s (Figs. 4A and 4B). A follow-up at 8 years postoperatively (Figs. 4C and 4D) revealed mild AR and a peak velocity of 3.9 m/s with mean pressure gradient of 35.9 mmHg. In addition, the end-diastolic posterior wall thickness was 6.49 mm (113% of normal, Z score = 1.7), which suggested left ventricular hypertrophy. He had no signs of heart failure. His aortic annular diameter increased along the normal annular diameter (Fig. 5), with a recent aortic annular diameter of 15.9 mm (113% of normal, Z score = 2.1).
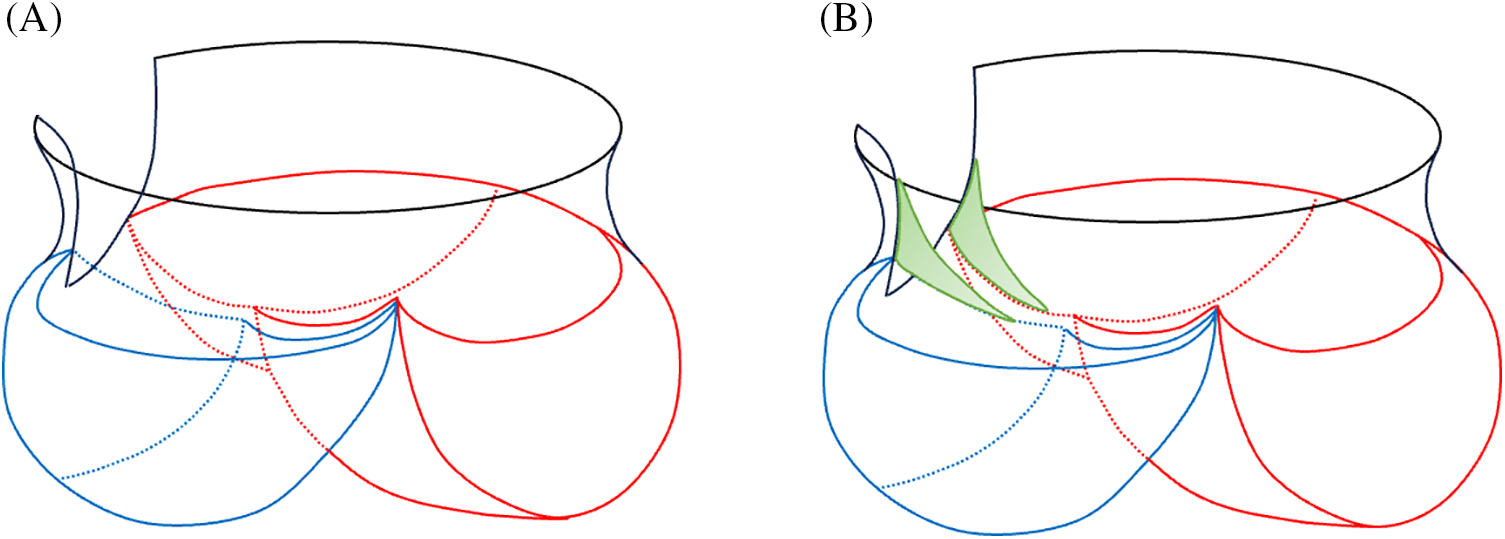
Figure 2: Schema of bicuspidization with commissuroplasty using the open-sleeve technique. (A) Open-sleeve technique by longitudinal incision at the less-developed anterior commissure. (B) Bicuspidization using glutaraldehyde-treated autologous pericardium (green)
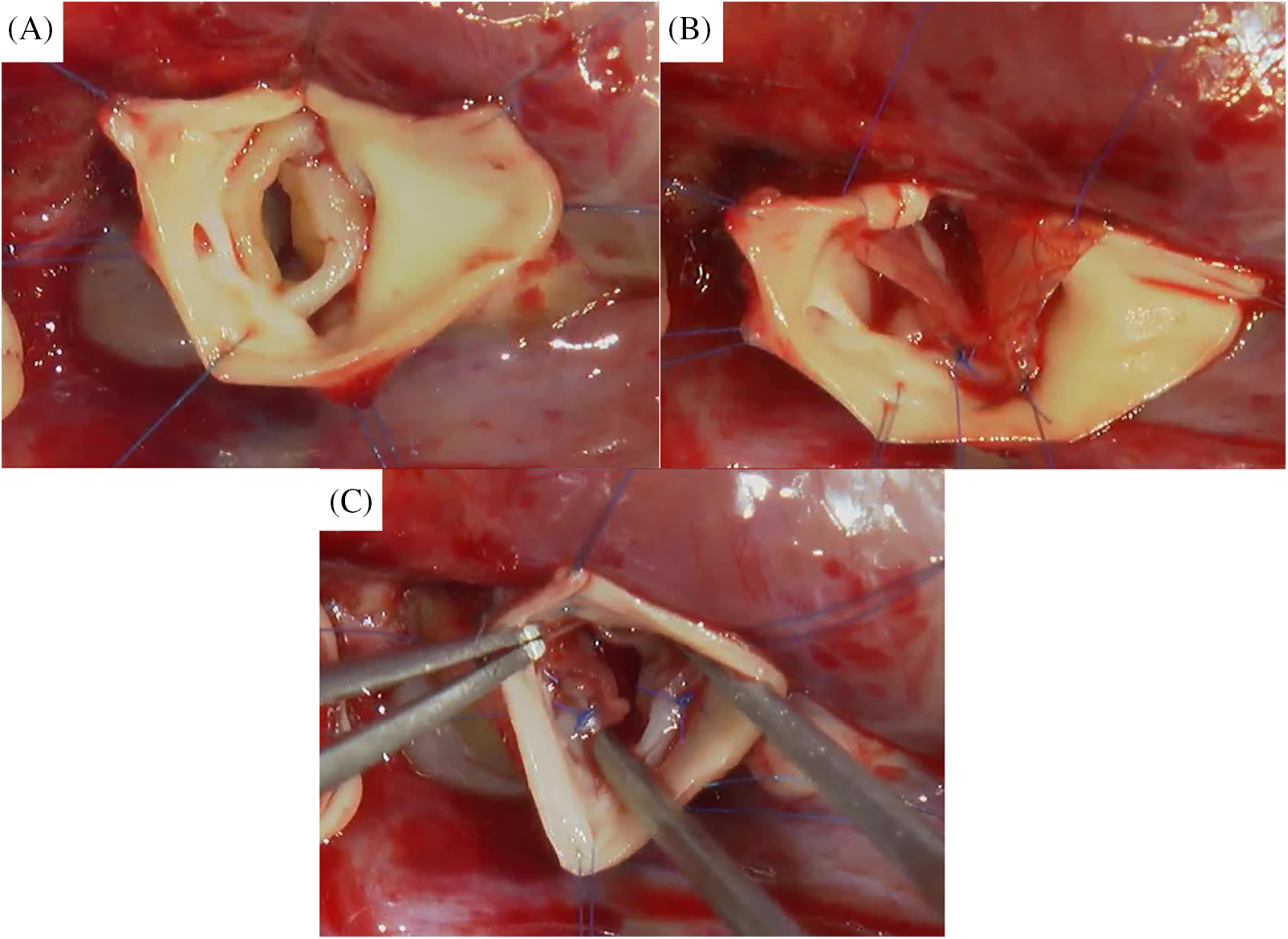
Figure 3: Intraoperative image. (A) Native aortic valve with open-sleeve technique. (B) Commissuroplasty with bicuspidization. (C) After the procedure
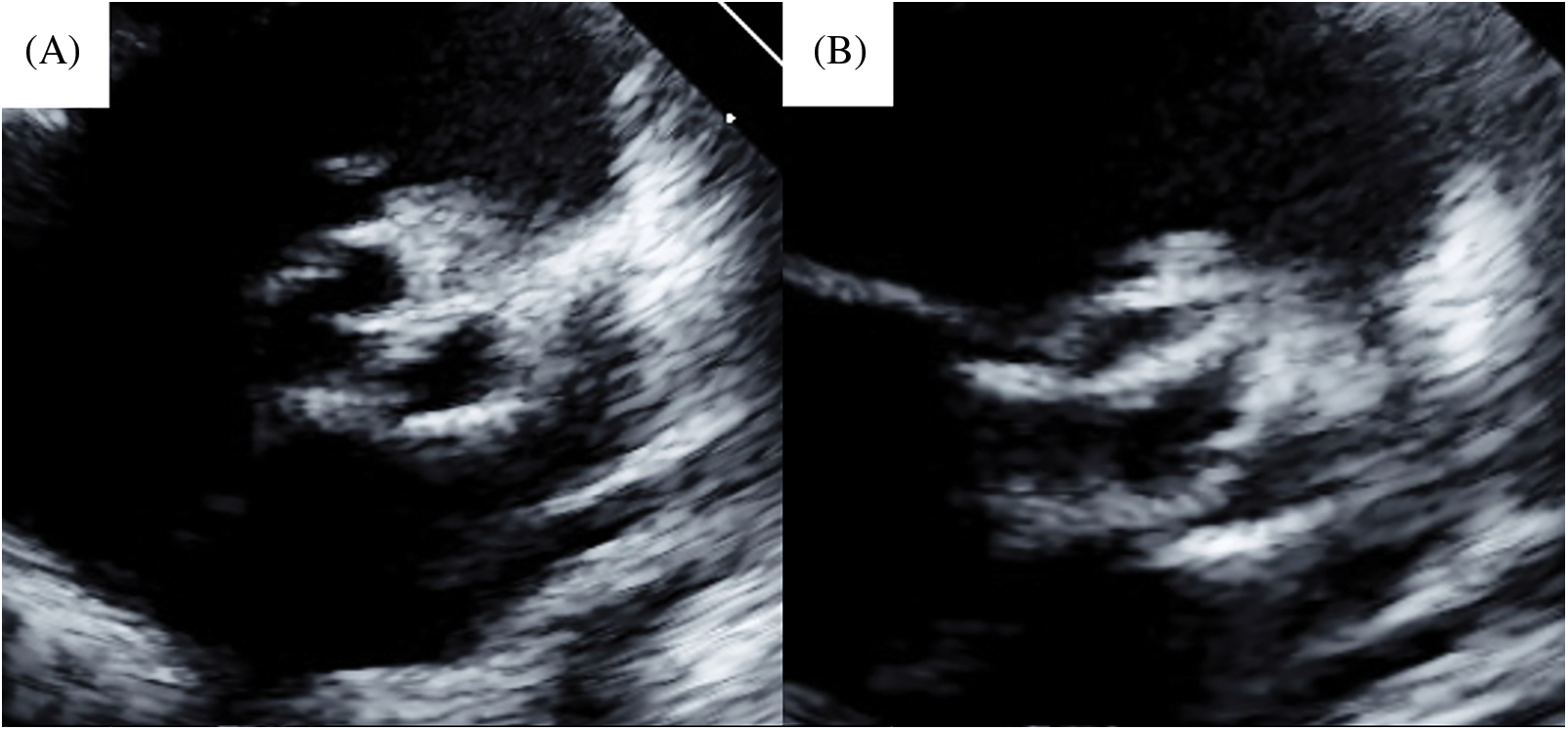
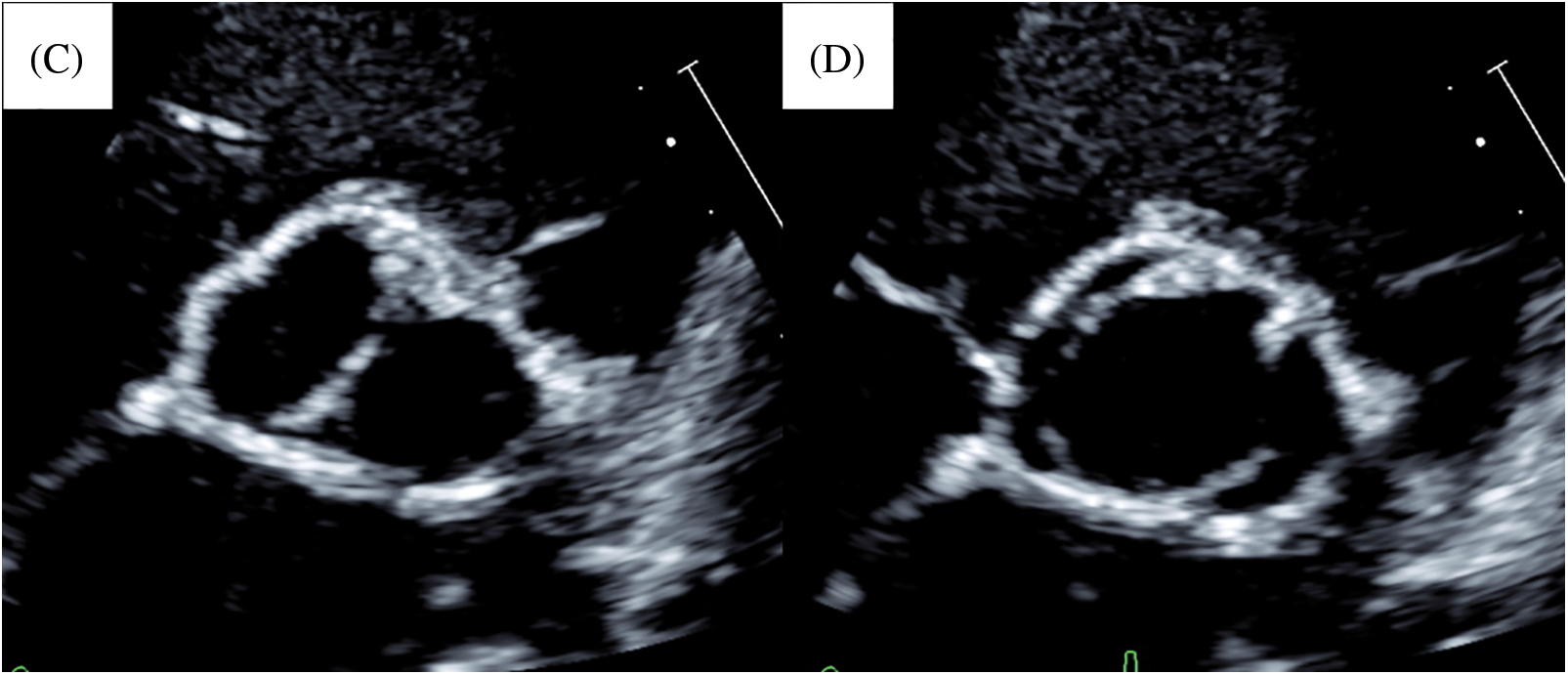
Figure 4: Postoperative and last follow-up echocardiogram of case 1. (A) Postoperative image in diastolic phase. (B) Postoperative image in systolic phase. (C) Last follow-up image in diastolic phase. (D) Last follow-up image in systolic phase
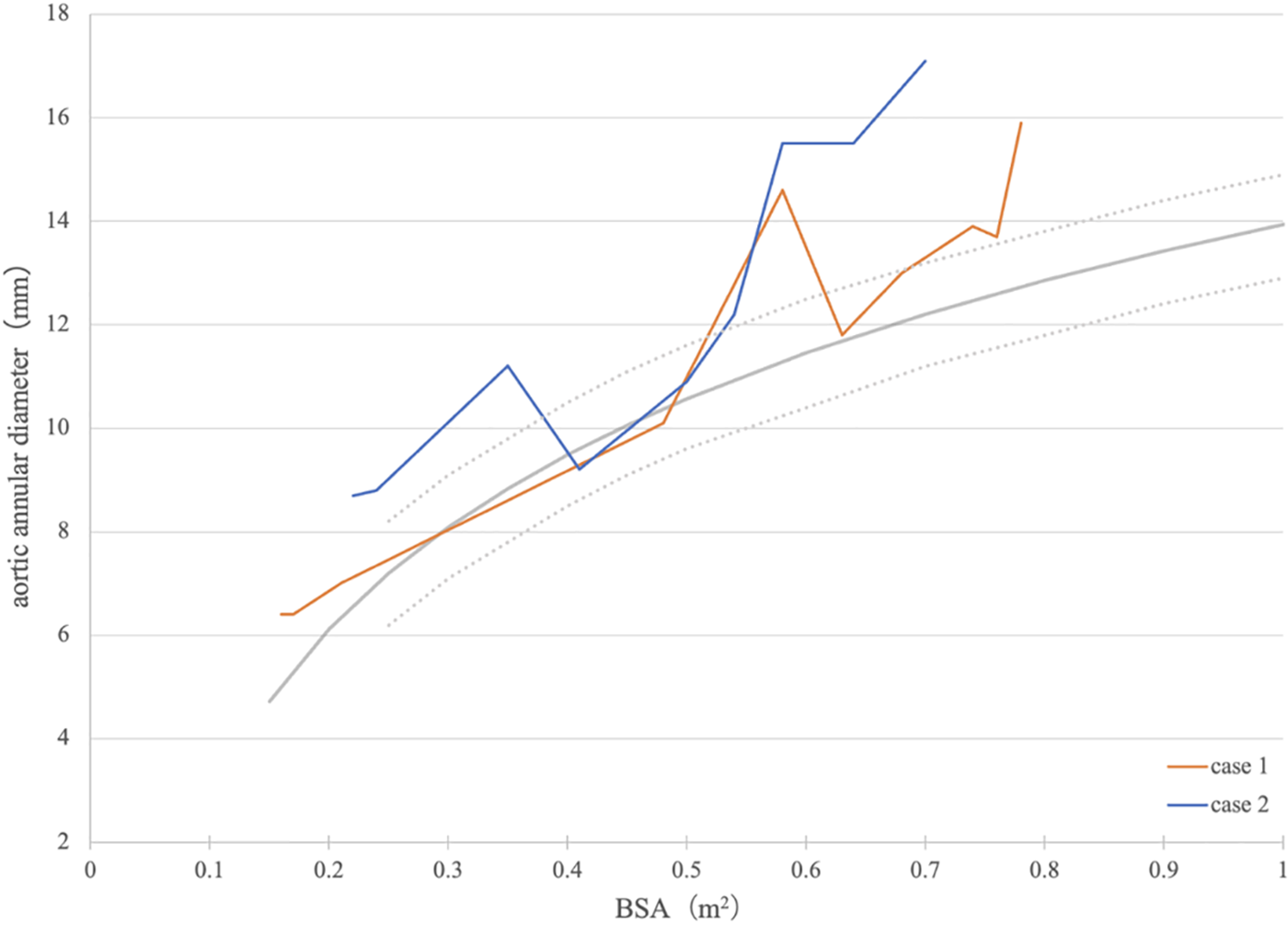
Figure 5: Association between body surface area and aortic annular diameter. The gray line and gray-dotted lines indicate the normal annular diameter and ±1 SD of the normal annular diameter, respectively. BSA, body surface area
A 2-month-old male neonate diagnosed with cAS, coarctation of the aorta, atrial septal defect, left pulmonary artery stenosis, and persistent left superior vena cava during the fetal period was delivered via cesarean section at 38 weeks and 5 days and weighed 3.15 kg. Moreover, he was diagnosed with bronchial stenosis, which was repaired at the age of 1 month. He weighed 3.7 kg at the age of 2 months, but his cAS worsened. Transthoracic echocardiography revealed that his aortic annular diameter was 8.7 mm (111% of the normal, Z score = 2.0) with a unicuspid aortic valve (Figs. 6A and 6B). We performed aortic valve repair by bicuspidization with glutaraldehyde-treated (3 min) autologous pericardium using the open-sleeve technique. His operative details have been previously reported [1]. Concomitantly, we performed coarctation repair, atrial septal defect closure, left pulmonary artery plasty, and translocation of the left superior vena cava to the right superior vena cava. The cardiopulmonary bypass and cardiac arrest times were 244 and 122 min, respectively. Postoperatively, AR was trivial, and the peak velocity through the aortic valve was 1.5 m/s (Figs. 6C and 6D). The peak velocity at the anastomotic site of the aorta was 1.5 m/s. A follow-up at 6 years postoperatively (Figs. 6E and 6F) revealed mild AR and a peak velocity through the aortic valve of 1.1 m/s. The peak velocity at the anastomotic site of the aorta could not be measured, but blood flow at the descending aorta did not show a coarctation pattern. His aortic annular diameter increased along the normal annular diameter (Fig. 5), with a recent aortic annular diameter of 17.1 mm (126% of normal, Z score = 3.6).
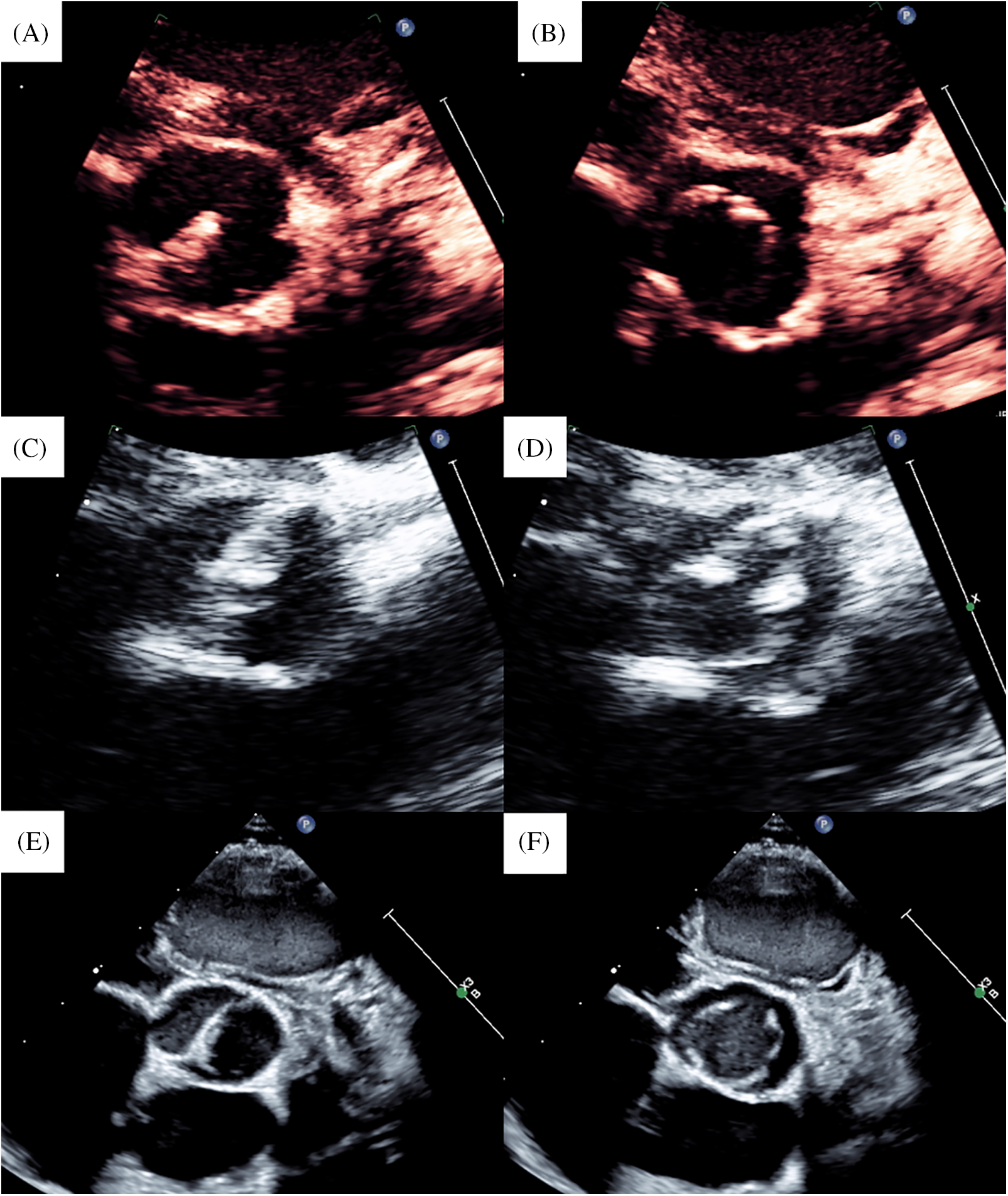
Figure 6: Echocardiogram of case 2. (A) Preoperative image in diastolic phase. (B) Preoperative image in systolic phase. (C) Postoperative image in diastolic phase. (D) Postoperative image in systolic phase. (E) Last follow-up image in diastolic phase. (F) Last follow-up image in systolic phase
Schafers et al. initially reported bicuspidization by commissuroplasty for cAS with unicuspid aortic valve [3], and Matsushima et al. and Chiu et al. reported its good long-term results [4,5]. However, these studies did not include neonates or infants. Although Schultz et al. and Notenboom et al. included outcomes of aortic valve repair for neonates or infants [6,7], they did not mention about bicuspidization for this population in detail.
BVP is usually selected for neonates because of the difficulty of valve repair and intolerance of surgery. Even at our institute, the first choice for cAS with unicuspid aortic valve is BVP. However, surgery must be performed when moderate or severe AR occurs concurrently or when BVP is ineffective, as in case 1. Moreover, when intervention for the aortic valve in neonates can be avoided, as in case 2, aortic valve repair is the first choice because of certain release of stenosis and control of regurgitation. Clear surgical space is required for fine valve repair in such aortic valve repair during neonatal or early infancy. We have previously reported an open-sleeve technique to solve this problem [1,2]. In this technique, the longitudinal incision of the aorta can be controlled by Valsalva, ventriculoaortic junction, or the ventricular muscle if required. In the two cases reported here, the aortic valve was unicuspid, and commissural height was low; therefore, achieving satisfactory valve function with commissurotomy only was challenging. Thus, we performed bicuspidization by commissuroplasty. The annular diameter was small because of their age. Therefore, we concomitantly used the open-sleeve technique for a clear and wide surgical space. Commissuroplasty can be performed at the site of longitudinal incision in a series when this incision is made at the opposite side of the well-developed commissure.
Our two cases showed that bicuspidization can be achieved during the neonatal or early infantile period using the open-sleeve technique with good mid-term results for the unicuspid aortic valve. At 8 and 6 years postoperatively, both patients are doing well without reintervention for the aortic valve. Moreover, their annular diameters increased along with the somatic growth, although growth disturbance may be a problem of the open-sleeve technique because of the incision to the annulus.
When aortic valve repair for cAS must be performed in infancy, the first repair is almost always a palliative procedure, and most cases require reintervention, particularly with stenosis progression [3]. Therefore, we must perform close follow-up, particularly in case 1, whose aortic stenosis progressed gradually. However, we hope that reintervention can be avoided for a longer time. From this point of view, bicuspidization using the open-sleeve technique in early infancy is a useful reparative technique for cAS with a unicuspid aortic valve.
Of course, the Ross procedure is another choice of surgery. However, the Ross procedure in the neonatal or early infantile period is controversial because of its results [8,9]. Moreover, Buratto et al. reported good outcomes for the Ross procedure in patients who had undergone aortic valve surgery previously [10]. Therefore, we prefer aortic valve repair for neonatal or infantile aortic valve disease.
Bicuspidization for neonates or early infants can be performed safely by using the open-sleeve technique as its midterm results have been satisfactory.
Acknowledgement: None.
Funding Statement: The authors received no specific funding for this study.
Author Contributions: The authors confirm contribution to the paper as follows: study conception and design: Toshi Maeda; data collection: Toshi Maeda, Hiroki Ito; analysis and interpretation of results: Toshi Maeda, Hiroki Ito; draft manuscript preparation: Toshi Maeda, Keiichi Hirose. All authors reviewed the results and approved the final version of the manuscript.
Availability of Data and Materials: The datasets generated during and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Ethics Approval: This study has been approved by the institutional review board (Mt. Fuji Shizuoka Children’s Hospital, ID: 61). Informed consent was obtained from the parents of the patients.
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
References
1. Murata M, Hirose K, Ikai A, Sakamoto K. Novel ‘open-sleeve technique’ for aortic valve plasty in congenital aortic stenosis. Interact Cardiovasc Thorac Surg. 2020;30(4):660. doi:10.1093/icvts/ivz296 [Google Scholar] [PubMed] [CrossRef]
2. Ishidou M, Hirose K, Ikai A, Sakamoto K. Open-sleeve technique: a new approach for aortic valve leaflet reconstruction in small children. Asian Cardiovasc Thorac Ann. 2022;30(6):729–32. doi:10.1177/02184923211050486 [Google Scholar] [PubMed] [CrossRef]
3. Schäfers HJ, Aicher D, Riodionycheva S, Lindinger A, Rädle-Hurst T, Langer F, et al. Bicuspidization of the unicuspid aortic valve: a new reconstructive approach. Ann Thorac Surg. 2008;85(6):2012–8. doi:10.1016/j.athoracsur.2008.02.081 [Google Scholar] [PubMed] [CrossRef]
4. Matsushima S, Heß A, Lämmerzahl JR, Karliova I, Abdul-Khali1 H, Schäfers HJ. Unicuspid aortic valve repair with bicuspidization in the paediatric population. Eur J Cardio-Thorac Surg. 2021;59(1):253–61. doi:10.1093/ejcts/ezaa285 [Google Scholar] [PubMed] [CrossRef]
5. Chiu P, Chávez M, Zubair M, Friedman KG, Marx GR, del Nido PJ, et al. Symmetric bicuspidizing repair for patients with congenital aortic or truncal valve disease. J Thorac Cardiocasc Surg. 2023;166(2):283–91. doi:10.1016/j.jtcvs.2022.10.015 [Google Scholar] [PubMed] [CrossRef]
6. Schultz A, Buratto E, Wallace FR, Fulkoski N, Weintraub RG, Brizard CP, et al. Outcomes of aortic valve repair in children resulting in bicuspid anatomy: is there a need for tricuspidization? J Thorac Cardiovasc Surg. 2022;164(1):186–96. doi:10.1016/j.jtcvs.2022.01.022 [Google Scholar] [PubMed] [CrossRef]
7. Notenboom M, Rhellab R, Etnel JRG, van den Bogerd N, Veen KM, Taverne YJHJ, et al. Aortic valve repair in neonates, infants and children: a systematic review, meta-analysis and microsimulation study. Eur J Cardio-Thorac Surg. 2023;64(3):ezad284. doi:10.1093/ejcts/ezad284 [Google Scholar] [PubMed] [CrossRef]
8. Rajab TK, Zorrila-Vaca A, Kavarana MN, Mokashi S, Sainathan S. Ross operation in neonates: a meta-analysis. Ann Thorac Surg. 2022;113(5):192–9. doi:10.1016/j.athoracsur.2020.11.008 [Google Scholar] [PubMed] [CrossRef]
9. Cleveland JD, Bansal N, Wells WJ, Wiggins LM, Kumar SR, Starnes VA. Ross procedure in neonates and infants: a valuable operation with defined limits. J Thorac Cardiovasc Surg. 2023;165(1):262–72. doi:10.1016/j.jtcvs.2022.04.015 [Google Scholar] [PubMed] [CrossRef]
10. Buratto E, Wallace FRO, Fricke TA, Brink J, d’Udekem Y, Brizard CP, et al. Ross procedures in children with previous aortic valve surgery. J Am Coll Cradiol. 2020;76(13):1564–73 [Google Scholar] [PubMed]
Cite This Article
 Copyright © 2024 The Author(s). Published by Tech Science Press.
Copyright © 2024 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools