 Open Access
Open Access
ARTICLE
Failure to Rescue as a Quality Metric in Congenital Heart Surgeries in a High-Complexity Service Provider Institution Located in a Middle-Income Country
1 Departamento de Anestesiología, Fundación Valle del Lili, Cali, 760032, Colombia
2 Centro de Investigaciones Clínicas, Fundación Valle del Lili, Cali, 760032, Colombia
3 Departamento de Cardiología Pediátrica, Fundación Valle del Lili, Cali, 760032, Colombia
4 Facultad de Medicina, Universidad Icesi, Cali, 760031, Colombia
5 Unidad de Cuidado Intensivo, Fundación Valle del Lili, Cali, 760032, Colombia
* Corresponding Author: Gustavo Cruz. Email:
Congenital Heart Disease 2024, 19(2), 207-218. https://doi.org/10.32604/chd.2024.044244
Received 25 July 2023; Accepted 03 January 2024; Issue published 16 May 2024
Abstract
Background: Failure to rescue has been an effective quality metric in congenital heart surgery. Conversely, morbidity and mortality depend greatly on non-modifiable individual factors and have a weak correlation with better-quality performance. We aim to measure the complications, mortality, and risk factors in pediatric patients undergoing congenital heart surgery in a high-complexity institution located in a middle-income country and compare it with other institutions that have conducted a similar study. Methods: A retrospective observational study was conducted in a high-complexity service provider institution, in Cali, Colombia. All pediatric patients undergoing any congenital heart surgery between 2019 and 2022 were included. The main outcomes evaluated in the study were complication, mortality, and failure to rescue rate. Univariate and multivariate logistic regression analysis was performed with mortality as the outcome variable. Results: We evaluated 308 congenital heart surgeries. Regarding the outcomes, 201 (65%) complications occurred, 23 (7.5%) patients died, and the FTR of the entire cohort was 11.4%. The presence of a postoperative complication (OR 14.88, CI 3.06–268.37, p = 0.009), age (OR 0.79, CI 0.57–0.96, p = 0.068), and urgent/emergent surgery (OR 8.14, CI 2.97–28.66, p < 0.001) were the most significant variables in predicting mortality. Conclusions: Failure to rescue is an effective and comparable quality measure in healthcare institutions and is the major contributor to postoperative mortality in congenital heart surgeries. Despite our higher mortality and complication rate, we obtained a comparable failure to rescue rate to high-income countries’ health institutions.Keywords
The high complexity of congenital heart surgeries (CHS) is related to a higher rate of complications and mortality compared to other types of surgeries [1]. In addition, congenital heart disease is the leading contributor to infant mortality resulting from birth defects and at least a third of pediatric patients with CHS have reported postoperative complications [2].
A complication within the in-hospital context refers to an adverse event associated with an acquired disease or a health center intervention, different from the expected natural course of evolution [3]. These events negatively affect outcomes, increasing the length of stay, hospital costs and mortality [4]. Throughout the years, the rate of postoperative complications and mortality in CHS have been used to determine the quality of service of health institutions [5].
However, morbidity and mortality depend greatly on non-modifiable individual factors, independent of the quality of health service and the institution [6,7]. This can cause significant differences in complication and mortality rates between health institutions that do not necessarily mean better or worse service quality. In an analysis of the largest database of CHS in North America, the CHS database of the society of thoracic surgeons (STS-CHSDB), postoperative outcomes and associated variables were evaluated. One of the most relevant findings was that morbidity and mortality largely depend on patient preoperative factors, their health status, and the complexity level of the surgery, variables unrelated to the institutions’ quality of service [6].
Failure to rescue (FTR), defined as the mortality of patients who experienced complications, has been an effective quality measure used in different pediatric surgical procedures [6,8–10]. Similarly, FTR studies have been conducted in CHS including institutions of different incomes, resources, and levels [4–6,9,11]. Our study aims to present the complications, 28-day mortality, and risk factors in pediatric patients undergoing CHS in a high-complexity University institution located in a middle-income country and compare it with other institutions that have conducted a similar study. Most of the literature regarding postoperative complications and mortality in CHS is focused on high-income countries, while there is limited knowledge about this topic in low and middle-income countries [11].
A retrospective observational study was conducted in a high-complexity university hospital, La Fundación Valle Del Lili in Cali, Colombia. All pediatric patients (under 18 years old) undergoing any CHS between November 2019 and May 2022 were included. Patients with any oncoproliferative disease were excluded. We only analyzed the patient´s first cardiovascular procedure. There was no change in personnel during the study period.
Patient demographics, preoperative clinical status, surgery conditions, and outcomes were searched in the patient´s medical records. Each patient was assigned a study ID to ensure anonymity. The variables were annotated in the institution’s clinical database management system by the researchers, a platform for protected data collection. For demographic variables, we identified the patients’ age, sex, weight, and height. Preoperative clinical variables included risk factors and established pathologies including low weight for age, low weight for height, prematurity, history of cardiac surgeries, number of cardiac surgeries in the actual hospitalization, and history of pulmonary, hepatic, neurologic, or endocrine disease. For the surgery condition variables, we established the diagnosis, the type of surgery performed, the RACHS-1, and the level of urgency (elective or urgent/emergency) for each procedure.
The main outcomes evaluated in the study were complication, 28-day mortality, and FTR rates. The definition of each complication was based on the classification established in the STS-CHS database (version 3.22) [6]. We included cardiovascular (cardiac dysfunction, cardiac failure, cardiac arrest, arrhythmias, pericardial effusion, systemic vein obstruction, pulmonary vein obstruction), respiratory (respiratory insufficiency, pneumonia, pneumothorax, pleural effusion, pulmonary hypertension, chylothorax), renal (renal failure), infectious (sepsis, endocarditis), reintervention (secondary to bleeding, cardiac or non-cardiac causes, and unplanned catheterization), neurological (deficits, seizures, stroke, subdural hematoma, intraventricular hemorrhage), wound-related (dehiscence and surgical site infection), anesthetic-related, rehospitalization within 28 days, multiorgan failure and other postoperative complications. Delayed sternal closure was not included as a complication because the sternum was often left open due to institutional protocol and the patient’s hemodynamic status.
Our institution is a high-complexity hospital with the necessary expertise and resources to manage postoperative complications, including extracorporeal membrane oxygenation (ECMO), renal replacement therapy, and inhaled nitric oxide for pulmonary hypertension. Intraoperative echocardiography was used in all surgeries. The most important indication for postoperative ECMO was ventricular failure with low cardiac output. Other conditions in which ECMO was used in different proportions were CPB weaning failure, pulmonary hypertension, cardiac arrest, and pulmonary failure.
All statistical analyses were performed using R statistical software version 4.2.1 (R Foundation for Statistical Computing) through RStudio 2022.12.0. For descriptive analysis, the normality of continuous variables was evaluated using the Shapiro-Wilk test. If the assumption of normality was rejected, these variables were presented as a median and interquartile range, and if not rejected, they were presented as a mean and a standard deviation. Qualitative variables were described using absolute frequencies and percentages. Operative 28-day mortality, rate of at least one complication, and FTR rate were calculated and presented with 95% confidence intervals.
Univariate and multivariate logistic regression analysis was performed with 28-day mortality as the outcome variable. For the multivariate logistic regression, predictors considered were those with a p-value less than 0.25 in the simple regression. These predictors included the occurrence of at least one complication, age, surgery priority, and CPB time. Multicollinearity in the logistic regression was assessed using the Variance Inflation Factor (VIF) for each term in the model. All analyses were conducted using the R statistical software version 4.2.1 via RStudio 2023.06.2.
This study was approved by the Institutional Ethics Committee (approval number 628-2022 Act No. I22-112 of November 02, 2022) following national and international recommendations for human research. In accordance with resolution 8430 of 1993, this study was considered risk-free, and the waiver of informed consent was requested and obtained.
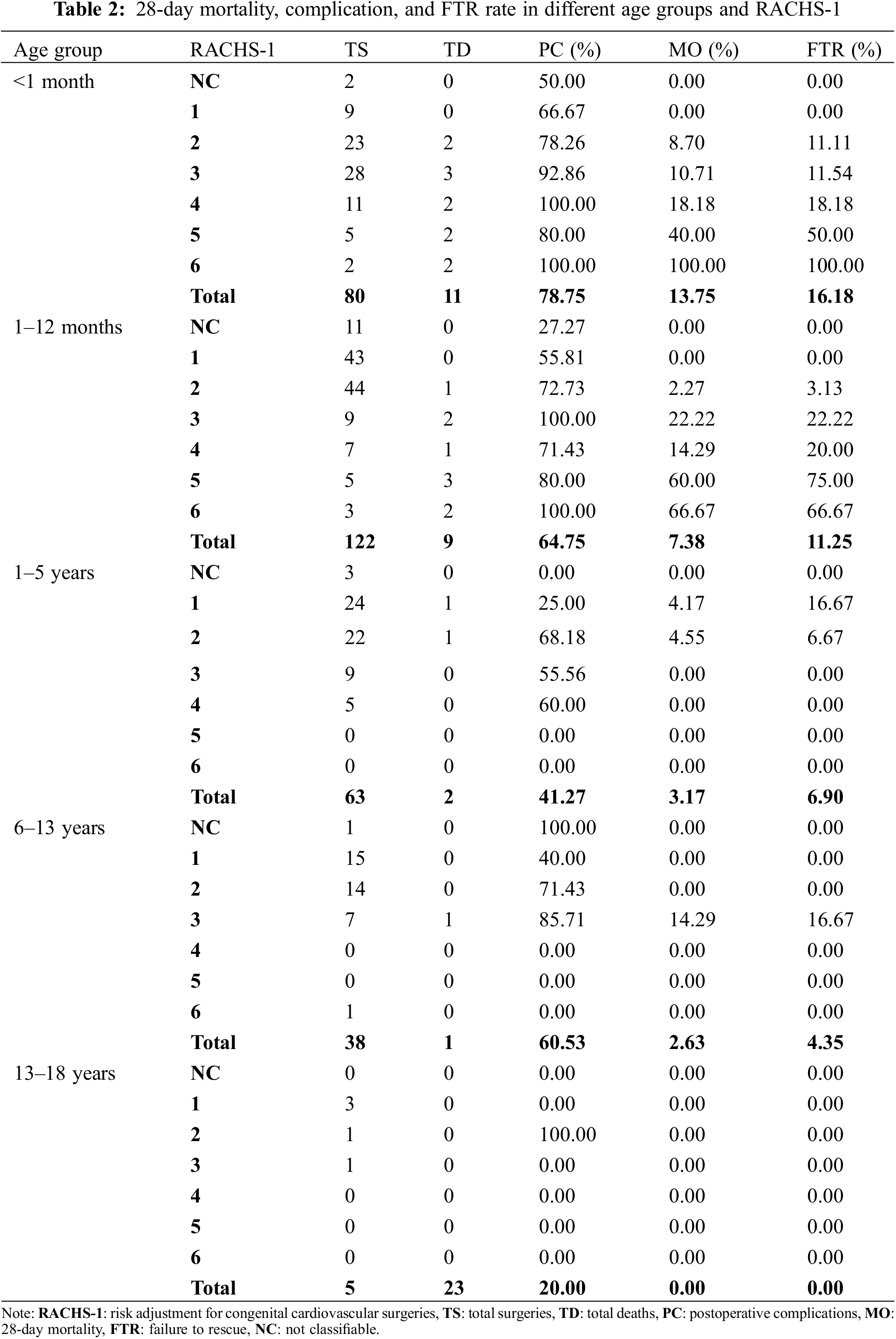
A total of 308 pediatric patients undergoing CHS were included. The socio-demographic information and clinical characteristics of the patients are presented in Table 1. The median age of the participants was 0.6 years (IQR, 0.2–3.0). The most common age group was infants (39.3%), followed by newborns (24.4%), toddlers (20.8%), kids (13.6%), and adolescents (1.9%). Regarding the outcomes, 201 (65%) complications occurred, 23 (7.5%) patients died, and the FTR of the entire cohort was 11.4% (Table 1). 28-day Mortality and FTR varied depending on the age group and the RACH-1 classification. Younger patients and surgeries of greater complexity (higher RACH-1) tended to have higher mortality and FTR (Table 2).
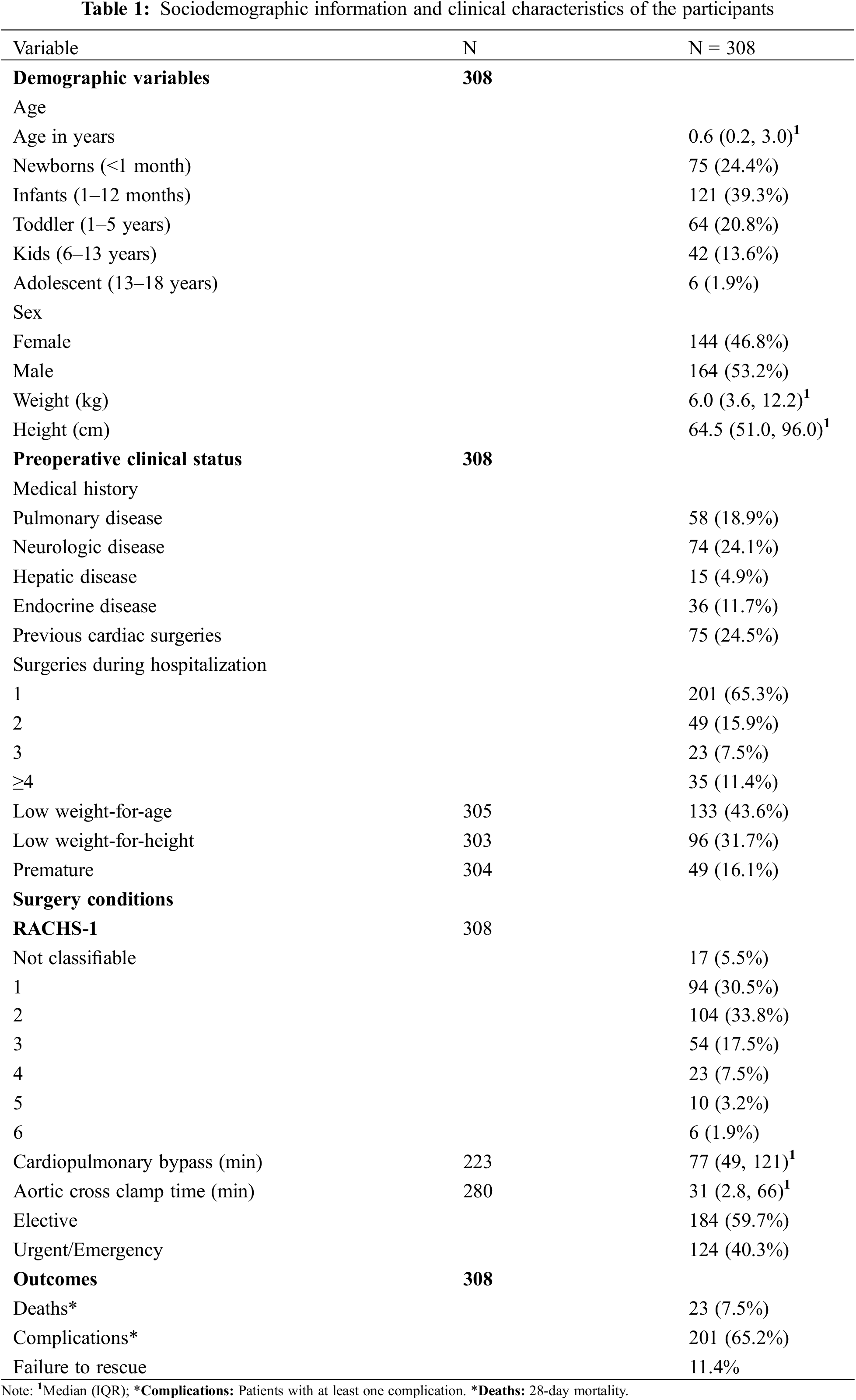
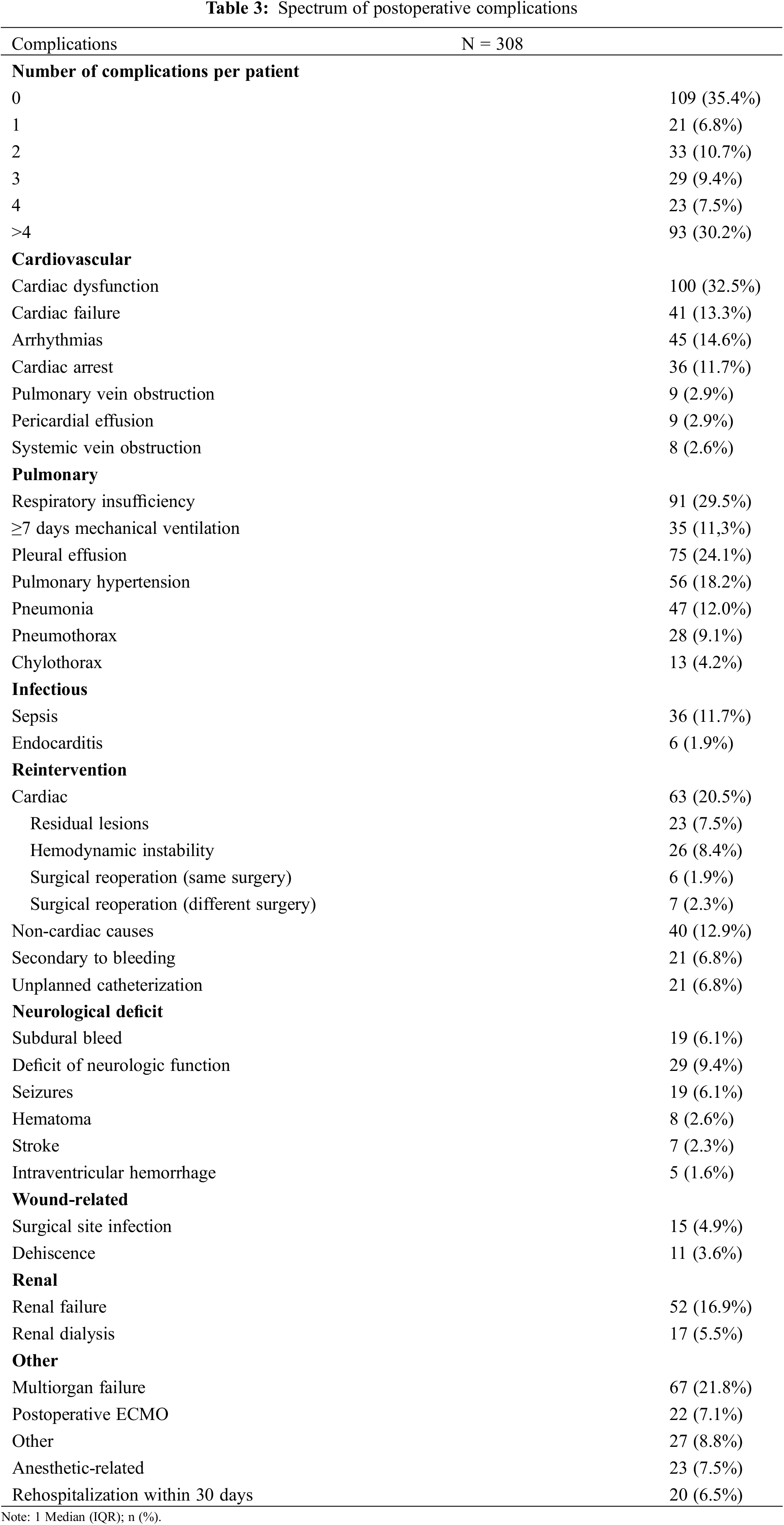
In our cohort, most of the patients who presented a postoperative complication had more than 4 complications (30%) (Table 3). The most common complications were cardiac dysfunction (33%), respiratory insufficiency (30%), pleural effusion (24%), and multiorgan failure (22%) (Table 3).
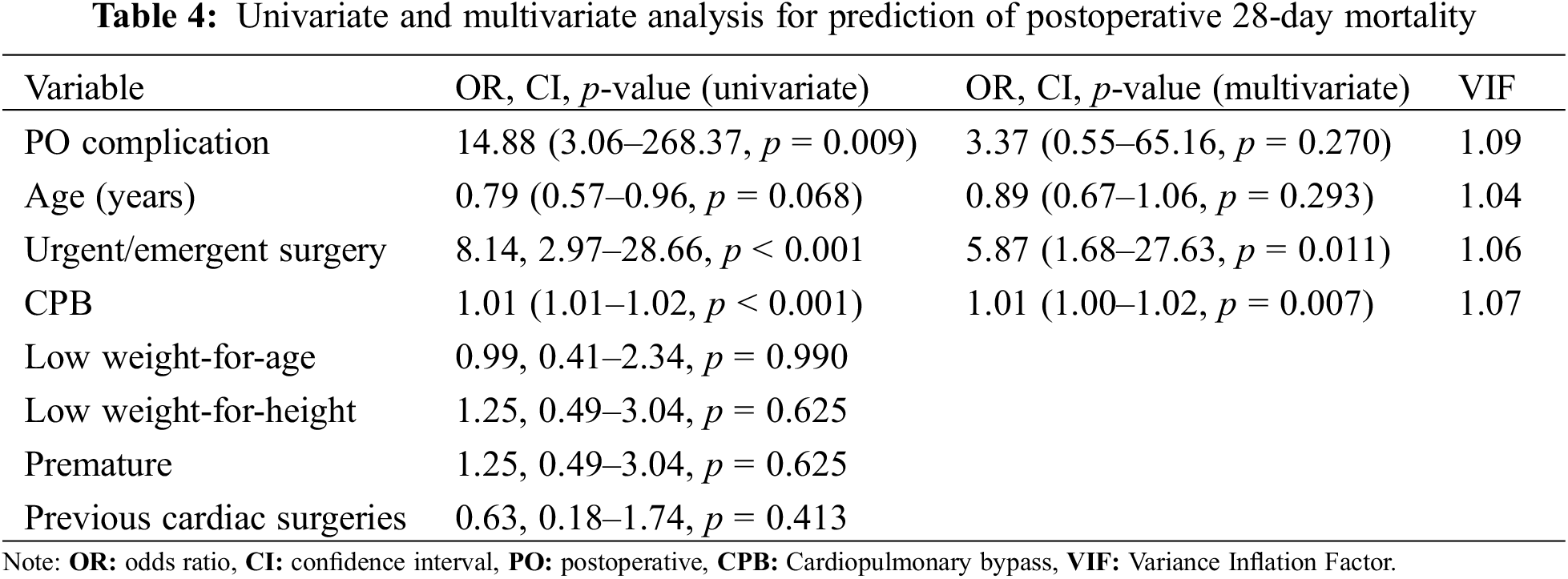
Within the univariate analysis, the variables of a postoperative complication (OR 14.88, CI 3.06–268.37, p = 0.009), age (OR 0.79, CI 0.57–0.96, p = 0.068), urgent/emergent surgery (OR 8.14, CI 2.97–28.66, p < 0.001) and Cardiopulmonary bypass (CPB) (OR 1.01, CI 1.01–1.02, p < 0.001), were the most significant in predicting 28-day mortality (Table 4). Therefore, these four variables were included in the multivariate analysis, finding that an urgent/emergent surgery was an independent risk factor for death. The VIFs for all variables were consistently below the threshold of 5, suggesting no multicollinearity issues within the model.
We compared our results with 2 similar studies: the STS-CHSDB (study 1) [12] and the Pediatric cardiac surgery program with limited systemic resources (study 2) [13]. In general, our patients were younger, and smaller, presented a significantly higher complication rate, and more urgent/emergent surgeries were performed. The mortality rate resulted in 3.7% in study 1 and 23.4% in study 2. On the other hand, FTR resulted in 9.1%, and 23.3%, respectively (Table 5).
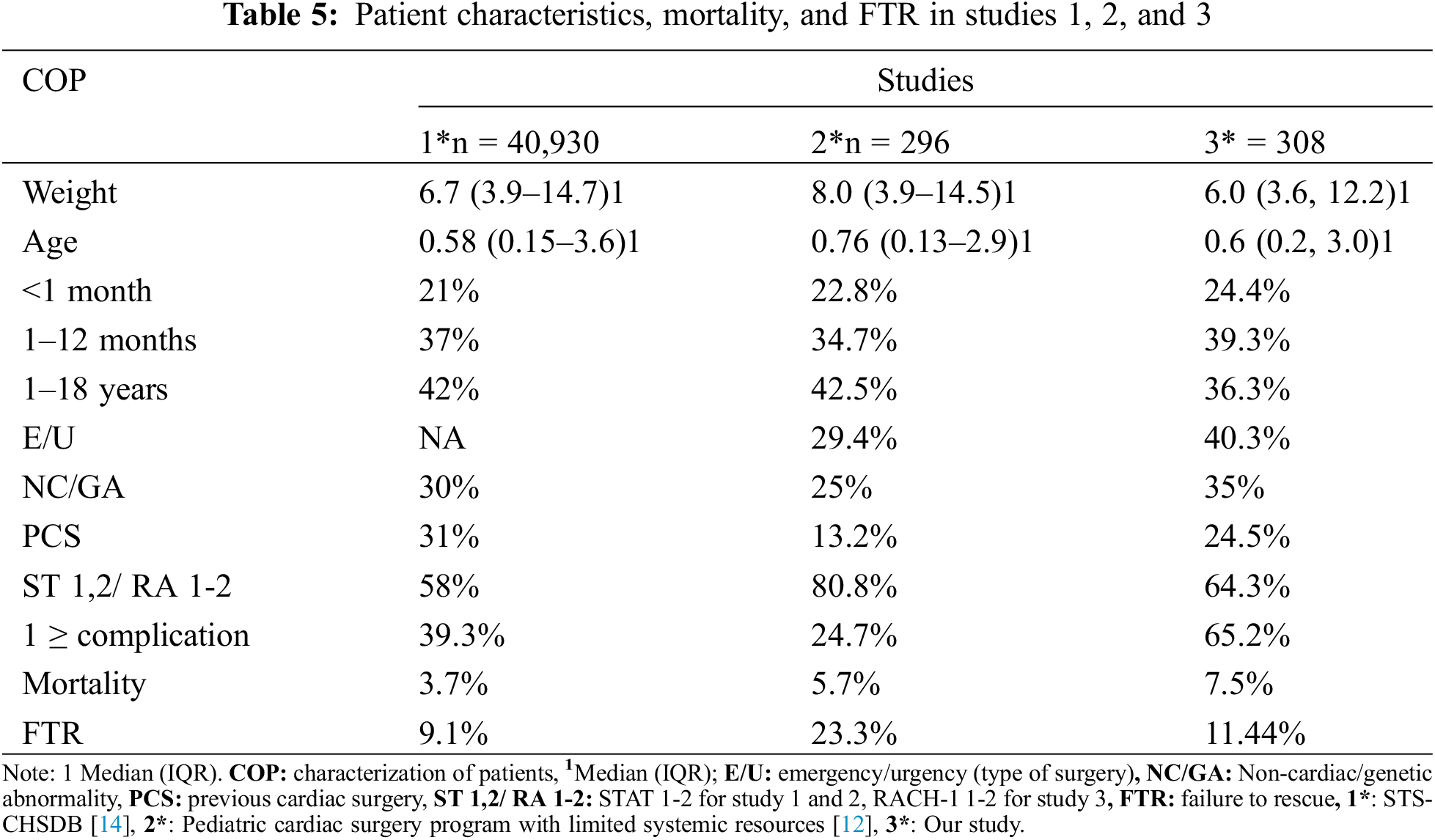
This study on pediatric patients undergoing CHS in a middle-income country institution revealed a higher 28-day mortality rate (7.5%) compared to the literature-reported range of 2%–6% [4–7,10,12]. Similarly, a higher rate of complications (65.2%) was observed in comparison to the rates in high-income countries (39%–44%) [10–14]. The higher mortality and complication rates can be attributed to our institution’s patients being generally unhealthier (Table 5). Although 64% of our cases were in the RACHS-1 1 and 2 category, 80% of deaths were linked to a RACHS-1 score of ≥3, as shown in Table 3. This suggests that severe outcomes predominantly occurred with higher RACHS-1 scores.
Another important factor that can explain the higher mortality and complication rate in our institution is our country’s primary care characteristics. Given that our institution is a high-complexity service provider in a middle-income country, patients are typically referred from institutions lacking specialized care to provide proper treatment. However, before surgery, issues like late access to health services and limited access to technology and medicines can worsen patients’ conditions, increase the urgency of the surgery, and affect the outcomes.
We showed that the presence of postoperative complications after CHS is a relevant risk factor for postoperative mortality (Table 4). Pasquali and colleagues reported that postoperative complications significantly alter a patient’s subsequent risk of death [7] and Polivenok et al. reported similar findings in an institution with limited resources [13]. Urgent/emergent surgery was identified as an independent risk factor for 28-day mortality. Notably, 40% of surgeries conducted in our study were of emergent or urgent nature. This variable was the most significant risk factor in the multivariate analysis, also accounting for the elevated complication and mortality rates observed in our research.
Despite the common assumption that hospitals with better quality performance have lower rates of postoperative complications, multiple studies in adults indicate a weak correlation between complication rates and hospital performance [7,9,10,13]. Comorbidities and preoperative conditions are the primary factors associated with complications. Conversely, Pasquali et al. showed that pediatric heart centers with superior performance do not necessarily exhibit a lower incidence of complications. Instead, they achieved a lower FTR rate [7]. Our study also yielded this finding, where even though our 28-day mortality rate (7.5%) and complication rate (65%) were higher compared to other studies, we were able to attain a comparable FTR rate (11%) to high-income countries’ health institutions (Table 5) [7,12–14].
In our study, the predominant complications observed were cardiac dysfunction, respiratory insufficiency, and multiorgan failure (Table 3). According to the STS-CHS database, cardiac dysfunction is characterized by one or more of the following indicators: tachycardia, oliguria, diminished skin perfusion, and an elevated requirement for inotropic support [6]. Notably, the most frequently observed clinical manifestations were tachycardia and an augmented need for inotropic support. Given that oliguria is an established marker for cardiac dysfunction, a substantial number of patients exhibiting renal failure also presented with cardiac dysfunction. This confluence likely amplified the incidence of multiorgan failure. The STS-CHS database (version 3.22) defined respiratory insufficiency complication by 3 subgroups depending on the management, including mechanical ventilation (MV) greater than 7 days, reintubation, or tracheostomy [6]. We included all patients in these three categories in one group of complications. A considerable number of patients with ongoing CHS were critically ill, though requiring MV support for more than 7 days (11.3%).
Previous studies report a wide range of the most frequent complications including postoperative bleeding, cardiac dysfunction, unplanned reoperation, acute renal failure, and surgical site infection [12–15]. This indicates the need for protocols and improvement strategies for each institution. Mortality and complications will differ according to the population characteristics and resources available. The result of this investigation also suggests that strategies for postoperative complications and management are critical for reducing mortality. Similar recommendations were reported in the STS-CHS database study [12].
This study was carried out in a single institution with a limited number of patients. Hence, results cannot be extrapolated to other programs. Furthermore, the postoperative complications included in the study were limited to complications established in the STS-CHS database, though, we did not capture every possible postoperative complication. However, this allowed an effective and objective comparison between studies.
Given the retrospective nature of this study, certain intraoperative parameters, specifically blood utilization, surgery duration, nitric oxide administration, and the use of inotropes and vasoconstrictors were not incorporated due to constraints in accessing the relevant information. This represents a limitation as these factors could potentially influence the FTR rate.
It is pertinent to acknowledge a limitation in our study regarding a methodological distinction when comparing the studies. While our study utilized the RACH-1 scoring system to determine the risk associated with the surgeries, comparison studies predominantly employed the STAT categories. Previous research suggests that the STAT categories offer a more accurate mortality risk prediction than the RACH-1 score. Additionally, it should be noted that in study 2, referenced in Table 5 [12], five additional postoperative complications, not encompassed within the STS-CHSDB, were incorporated. This inclusion may have influenced their FTR outcomes.
FTR is an effective and comparable quality measure in healthcare institutions and is a major contributor to postoperative mortality in CHS. We obtained a comparable FTR rate to high-income countries’ health institutions, despite a higher mortality and complication rate in our pediatric cardiac surgeries. Further characterization of postoperative complications across centers and strategies for complications prevention and management is essential to reduce mortality.
Acknowledgement: Not applicable.
Funding Statement: The authors received no specific funding for this study.
Author Contributions: GC: Investigation, Writing of the main manuscript, Conceptualization, Review of the manuscript. SP: Investigation, Writing of the main manuscript, Conceptualization, Review of the manuscript, Tables 1–4. JFV: Investigation, Editing, and Review of the main manuscript. JL: Investigation, Methodology, Statistical analysis, Tables 2 and 4. JFT: Investigation, Conceptualization, database, Review of the manuscript, JHM: Investigation, Review of the manuscript.
Availability of Data and Materials: All tables have been included in the article. However, please note that raw data base and additional information cannot be made available directly due to institutional safety measures and policies. Researchers interested in accessing the database may submit a formal request through a letter directed to our institution.
Ethics Approval: This study was approved by the Institutional Ethics Committee (approval number 628-2022 Act No. I22-112 of November 02, 2022) following national and international recommendations for human research. In accordance with resolution 8430 of 1993, this study was considered risk-free, and the waiver of informed consent was requested and obtained.
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
References
1. Normand ST, Zelevinsky K, Nathan M, Abing HK, Dearani JA, Galantowicz M, et al. Reevaluating congenital heart surgery center performance using operative mortality. Ann Thorac Surg. 2022;114(3):776–84. doi:10.1016/j.athoracsur.2021.11.076. [Google Scholar] [PubMed] [CrossRef]
2. Thom T, Haase N, Rosamond W, Howard VJ, Rumsfeld J. Heart disease and stroke statistics--2006 update: a report from the American heart association statistics committee and stroke statistics subcommittee. Circulation. 2006;113(6):e85–151. doi:10.1161/CIRCULATIONAHA.105.171600. [Google Scholar] [PubMed] [CrossRef]
3. Manekk RS, Gharde P, Gattani R, Lamture Y. Surgical complications and its grading: a literature review. Cureus. 2022;14(5):e24963. doi:10.7759/cureus.24963. [Google Scholar] [PubMed] [CrossRef]
4. Portuondo JI, Shah SR, Singh H, Massarweh NN. Failure to rescue as a surgical quality indicator: current concepts and future directions for improving surgical outcomes. Anesth. 2019;131:426–37. doi:10.1097/ALN.0000000000002602. [Google Scholar] [PubMed] [CrossRef]
5. Ma LW, Hatchimonji JS, Kaufman EJ, Sharoky CE, Smith BP, Holena DN. Failure to rescue as a center-level metric in pediatric trauma. Surg. 2019;165:1116–21. doi:10.1016/j.surg.2019.03.004. [Google Scholar] [PubMed] [CrossRef]
6. The Society of Thoracic Surgeons. STS congenital heart surgery database data specifications version 3.22; 2013. p. 423–35. Available from: https://www.sts.org/sites/default/files/documents/CongenitalDataSpecsV3_22.pdf. [Accessed 2023]. [Google Scholar]
7. Pasquali SK, He X, Jacobs JP, Jacobs ML, O’Brien SM, Gaynor JW. Evaluation of failure to rescue as a quality metric in pediatric heart surgery: an analysis of the STS congenital heart surgery database. Ann Thorac Surg. 2012;94:573–80. doi:10.1016/j.athoracsur.2012.03.065. [Google Scholar] [PubMed] [CrossRef]
8. Chan T, Lion KC, Mangione-Smith R. Racial disparities in failure-to-rescue among children undergoing congenital heart surgery. J Pediatr. 2015;166:812–8.E4. doi:10.1016/j.jpeds.2014.11.020. [Google Scholar] [PubMed] [CrossRef]
9. Pasquali SK, Li JS, Burstein DS, Sheng S, O’Brien SM, Jacobs ML, et al. Association of center volume with mortality and complications in pediatric heart surgery. Pediatr. 2012;129(2):e370–6. doi:10.1542/peds.2011-1188. [Google Scholar] [PubMed] [CrossRef]
10. Jacobs JP, O’Brien SM, Pasquali SK, Jacobs ML, Lacour-Gayet FG, Tchervenkov CI, et al. Variation in outcomes for benchmark operations: an analysis of the society of thoracic surgeons congenital heart surgery database. Ann Thorac Surg. 2011;92:2184–92. doi:10.1016/j.athoracsur.2011.06.008. [Google Scholar] [PubMed] [CrossRef]
11. Jenkins KJ, Gauvreau K. Center-specific differences in mortality: preliminary analyses using the risk adjustment in congenital heart surgery (RACHS-1) method. J Thorac Cardiov Sur. 2002;124:97–104. doi:10.1067/mtc.2002.122311. [Google Scholar] [PubMed] [CrossRef]
12. Agarwal HS, Wolfram KB, Saville BR, Donahue BS, Bichell DP. Postoperative complications and association with outcomes in pediatric cardiac surgery. J Thorac Cardiov Sur. 2014;148(2):609–16.E1. doi:10.1016/j.jtcvs.2013.10.031. [Google Scholar] [PubMed] [CrossRef]
13. Polivenok IV, Novick WM, Pyetkov AV, Cardarelli M. Perioperative complications in a paediatric cardiac surgery program with limited systemic resources. Cardiol Young. 2020;30:1659–65. doi:10.1017/S1047951120002486. [Google Scholar] [PubMed] [CrossRef]
14. Wallen TJ, Fults M, Fariha NJ, Le M, Blenden R, Soto R. Failure to rescue in humanitarian congenital cardiac surgery. Ann Thorac Surg. 2020;109(5):1475–9. doi:10.1016/j.athoracsur.2019.09.022. [Google Scholar] [CrossRef]
15. Althabe M, Ricardo Rodríguez R, Balestrini M, Charroqui A, Krynski M, Lenz AM, et al. Morbidity in congenital heart surgery in a public hospital in Argentina. Arch Argent Pediatr. 2018;116:e14–8. doi:10.5546/aap.2018.eng.e14. [Google Scholar] [PubMed] [CrossRef]
Cite This Article
 Copyright © 2024 The Author(s). Published by Tech Science Press.
Copyright © 2024 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools