 Open Access
Open Access
ARTICLE
Impact of Atrial Septal Defect Closure on Mortality in Older Patients
1 Division of Cardiology, Department of Medicine, Faculty of Medicine Siriraj Hospital, Mahidol University, Bangkok, Thailand
2 Her Majesty Cardiac Center, Faculty of Medicine Siriraj Hospital, Mahidol University, Bangkok, Thailand
3 Department of Medicine, Faculty of Medicine Siriraj Hospital, Mahidol University, Bangkok, Thailand
* Corresponding Author: Nithima Ratanasit. Email:
Congenital Heart Disease 2024, 19(1), 93-105. https://doi.org/10.32604/chd.2024.048631
Received 13 December 2023; Accepted 29 January 2024; Issue published 20 March 2024
Abstract
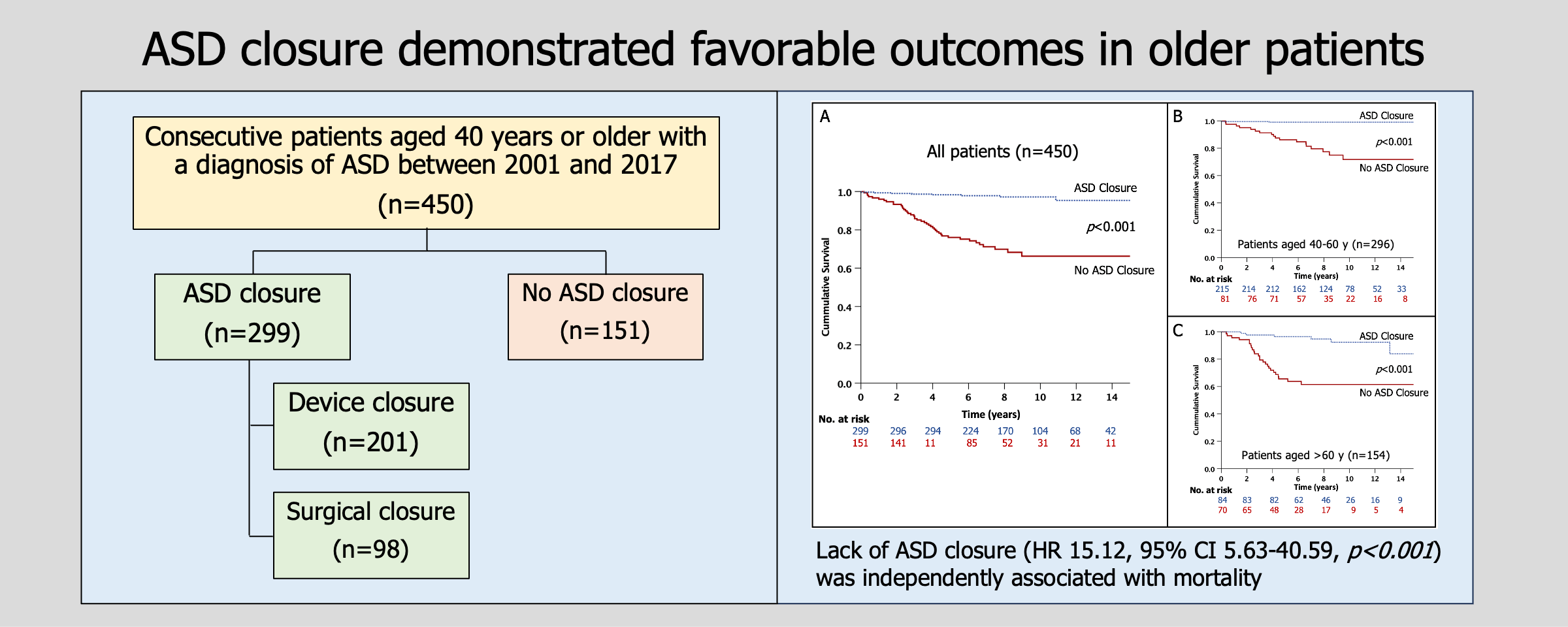
Background: Atrial septal defect (ASD) is a common form of adult congenital heart disease that can lead to long-term adverse outcomes if left untreated. Early closure of ASD has been associated with excellent outcomes and lower complication rates. However, there is limited evidence regarding the prognosis of ASD closure in older adults. This study aims to evaluate the mortality rates in older ASD patients with and without closure. Methods: A retrospective cohort study was conducted on patients aged 40 years or older with ASD between 2001 and 2017. Patients were followed up to assess all-cause mortality. Univariable and multivariable analyses were performed to identify the predictors of mortality. A p-value of <0.05 was considered statistically significant. Results: The cohort consisted of 450 patients (mean age 56.6 ± 10.4 years, 77.3% female), with 66% aged between 40 and 60 years, and 34% over 60 years. Within the cohort, 299 underwent ASD closure (201 with transcatheter and 98 with surgical closure). During the median follow-up duration of 7.9 years, 51 patients died. The unadjusted cumulative 10-year rate of mortality was 3% in patients with ASD closure, and 28% in patients without ASD closure (log-rank p < 0.001). Multivariable analysis revealed that age (hazard ratio [HR] 1.04, 95% confidence interval [CI] 1.006–1.06, p = 0.01), NYHA class (HR 2.75, 95% CI 1.63–4.62, p < 0.001), blood urea nitrogen (BUN) (HR 1.07, 95% CI 1.03–1.12, p < 0.001), right ventricular systolic pressure (RVSP) (HR 1.07, 95% CI 1.003–1.04, p = 0.01), and lack of ASD closure (HR 15.12, 95% CI 5.63–40.59, p < 0.001) were independently associated with mortality. Conclusion: ASD closure demonstrated favorable outcomes in older patients. Age, NYHA class, BUN, RVSP, and lack of ASD closure were identified as independent factors linked to mortality in this population.Graphic Abstract
Keywords
Abbreviations
| ASD | Atrial septal defect |
| CI | Confidence interval |
| HR | Hazard ratio |
| IQR | Interquartile range |
| LA | Left atrial |
| LV | Left ventricular |
| NYHA | New York Heart Association |
| PAP | Pulmonary artery pressure |
| PCWP | Pulmonary capillary wedge pressure |
| PVR | Pulmonary vascular resistance |
| RVSP | Right ventricular systolic pressure |
| SVR | Systemic vascular resistance |
Atrial septal defect (ASD) is a common congenital heart disease in adults, accounting for 25%–30% of newly diagnosed cases of congenital heart defects [1,2]. The abnormality is often diagnosed late or remains undetected until adulthood due to unrecognized signs and symptoms during childhood. However, older patients with ASD typically seek medical attention due to complications and hemodynamic abnormalities, including heart failure, pulmonary hypertension, and atrial arrhythmias, particularly atrial fibrillation [3,4].
Surgical repair, when performed early in childhood or adolescence and in the absence of pulmonary hypertension, has low mortality rates and leads to favorable long-term outcomes [5,6]. Although surgical repair can be performed with very low risk, even in the elderly, the comorbidities that may affect the operative risk need to be considered and then the risk is weighed against the potential benefit.
Transcatheter closure has become the first choice for secundum defect, when feasible, based on the morphology [7–9]. It has been widely accepted as the standard treatment due to its minimally invasive nature and lower complication rates [10,11]. Nevertheless, careful consideration is required when closing ASD in older patients due to potential long-term complications such as pulmonary hypertension, atrial arrhythmias, and right ventricular volume overload [12].
Previous studies have demonstrated the short-term clinical and morbidity benefits following ASD closure in older patients [3,4,12–15]. However, limited knowledge exists regarding the long-term adverse outcomes as well as the mortality benefit in this specific population. The objective of this study is to determine the long-term outcome, specifically assessing the all-cause mortality, in older patients (>40 years old) with and without ASD closure.
Consecutive patients aged 40 years or older with a diagnosis of ASD without severe left-sided valvular heart diseases or other significant congenital heart diseases, who underwent transthoracic echocardiography between 1st January 2001 and 31st January 2017 in a tertiary hospital were studied. If multiple echocardiographic studies were performed, only the first study was included in the data collection. Patients with incomplete electronic data, missing echocardiographic data, or insufficient follow-up time were excluded from the study. The institutional ethics committee approved this retrospective study and waived the requirement for additional written informed consent.
Clinical symptoms, comorbid diseases, and medication information were obtained from electronic medical records. The New York Heart Association (NYHA) class was determined at the time of the echocardiography. Laboratory results, including hemoglobin, blood urea nitrogen (BUN), and serum creatinine, were collected within a 3-month period of the echocardiography.
Echocardiography was performed according to the guideline recommendation [16]. ASD was visualized, and flow direction was demonstrated initially by transthoracic echocardiography. Transesophageal echocardiography was utilized to confirm diagnosis, assess ASD size and rim, determine pulmonary vein connection orientation, and identify associated cardiac defects. Left atrial (LA) volume and left ventricular (LV) mass were measured using the recommendations by the American Society of Echocardiography and indexed with body surface area [16]. Right ventricular systolic pressure (RVSP) was estimated using tricuspid regurgitation maximum velocity and right atrial pressure.
2.3 Right Heart Catheterization
In 242 patients (54%) right heart catheterization (RHC) was performed as part of clinical evaluation within 3 months after echocardiography. Patients were in chronic stable condition at the time of RHC. During the procedure, mean right atrial pressure (RAP), pulmonary artery pressure (PAP), mean pulmonary capillary wedge pressure (PCWP), and systemic arterial blood pressure were measured. Cardiac index, systemic vascular resistance (SVR), and pulmonary vascular resistance (PVR) were calculated using the Fick method.
Patient selection for undergoing the ASD closure procedure was determined by the cardiologist’s decision, as well as the closure techniques. The ASD closure procedures consisted of two techniques: transcatheter and surgical closure. The transcatheter technique involved the use of an ASD device delivered via a transvenous delivery system. The attending physician chose either Cocoon or Amplatzer septal occlude devices as per operator preference. For the surgical closure, a traditional surgical approach was employed. This involved a median sternotomy and cardiopulmonary bypass pump cannulation, followed by patch closure for direct interatrial septal repair.
Follow-up data were collected through clinical visits, medical records, and scripted telephone interviews. The patients were followed up to assess the all-cause mortality. Patients who were monitored for less than 4 years and were unable to be reached for the telephone interview were considered to have insufficient follow-up and were excluded from the study.
Statistical analyses were performed using IBM SPSS Statistics for Windows, version 20.0 (IBM Corp., Armonk, NY, USA). Continuous variables with a normal distribution were reported as mean ± standard deviation (SD), while continuous variables with a non-normal distribution were reported as median and interquartile range (IQR). The normality distribution of the variables was assessed using the Kolmogorov-Smirnov test. Categorical variables were presented as absolute numbers and percentages. Differences between groups were compared using the student’s unpaired t-test or Mann-Whitney U test for continuous variables, and the chi-square test or Fisher’s exact test for categorical variables, as appropriate. Mortality rates between the two groups were estimated using the Kaplan-Meier method and compared using the log-rank test. To analyze predictors of mortality, we conducted a Cox regression analysis to assess univariable predictors based on baseline characteristics, laboratory results, and echocardiographic variables. Variables with a p-value < 0.05 in the univariable analysis were included in the multivariable analysis, which aimed to identify independent predictors. The results of the Cox regression analysis are presented as hazard ratios (HR) with corresponding 95% confidence intervals (CI).
We identified 568 patients aged 40 years or older with a diagnosis of ASD. Of these, 113 were excluded due to insufficient follow-up time or being unreachable by telephone, and 5 were excluded due to incomplete electronic data or missing echocardiographic information. Therefore, a total of 450 patients were included in the final analysis. The mean age was 56.6 ± 10.4 years, and 77.3% were female. Hypertension was the most prevalent comorbidity, affecting 34.7% of the patients. Among the included patients, 222 (49.3%) had NYHA class I, 198 (44%) had class II, and the remaining were classified as class III. Most of the patients (423, 94%) had secundum ASD, while 17 had sinus venosus type, 8 had primum type, and 2 had coronary sinus type. Fourteen patients had associated anomalous pulmonary venous connections.
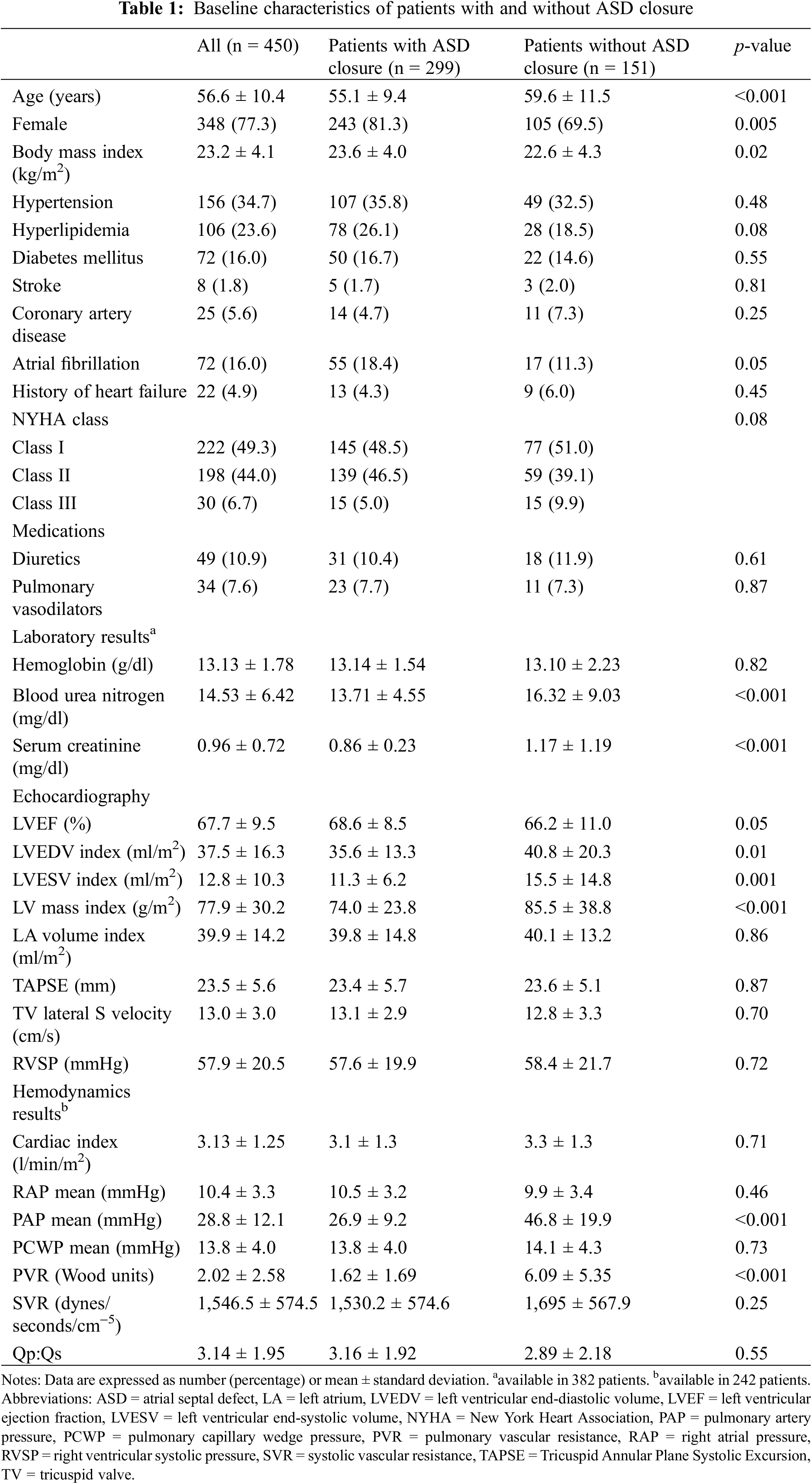
A total of 299 patients underwent ASD closure, with 201 and 98 undergoing transcatheter and surgical closure, respectively. One hundred fifty-one patients did not undergo ASD closure. The reasons for not undergoing closure included 19 with a significant right-to-left shunt/Eisenmenger syndrome, 56 with multiple comorbidities/severe frailty, 37 with severe pulmonary hypertension, 24 with a small ASD that did not meet the indication for closure, and 15 who denied closure. Table 1 summarizes the baseline characteristics of patients with and without ASD closure. Notably, patients with ASD closure were generally younger and more likely to be female. Additionally, they exhibited lower levels of BUN (13.71 ± 4.55 vs. 16.32 ± 9.03 mg/dl, p < 0.001) and serum creatinine (0.86 ± 0.23 vs. 1.17 ± 1.19 mg/dl, p < 0.001). Furthermore, patients with ASD closure had lower LV volume and mass index. In terms of RHC, these patients had significantly lower mean PAP (26.9 ± 9.2 vs. 46.8 ± 19.9 mmHg, p < 0.001) and PVR (1.62 ± 1.69 vs. 6.09 ± 5.35 mmHg, p < 0.001) than those without ASD closure.
During the median follow-up period of 7.9 (IQR 5.4, 11.1) years, 51 patients (11.3%) died. Forty-three patients without ASD closure died: 18 from heart failure, 4 from infection, 3 from cancer, 1 from advanced cirrhosis, 1 from intracerebral hemorrhage, and 16 from an unknown cause. Eight patients with ASD closure died, with one in the surgical closure group dying postoperatively from acute pulmonary embolism (the 30-day operative mortality was 1%, and the 30-day mortality after catheter closure was 0%). Seven died after hospital discharge (4 from infection and 3 from heart failure). The unadjusted cumulative 10-year rates of mortality for patients with and without ASD closure were 3% and 28%, respectively (p < 0.001). Table 2 presents the clinical characteristics of deceased and surviving patients. Deceased patients were older, more likely to be male, and had a higher NYHA class. Additionally, they exhibited a higher LV mass index (89.8 ± 43.2 vs. 76.4 ± 27.8 g/m2, p = 0.005) and elevated RVSP (67.7 ± 17.9 vs. 56.6 ± 20.5 mmHg, p < 0.001). Deceased patients had significantly higher mean PAP (49.75 ± 16.92 vs. 28.09 ± 11.24 mmHg, p < 0.001) and PVR (6.91 ± 1.69 vs. 1.83 ± 2.06 mmHg, p < 0.001) as determined by RHC. Notably, patients who underwent ASD closure, whether by transcatheter or surgery, had a significantly lower mortality rate compared to those without ASD closure (15.7% vs. 72.9%, p < 0.001).
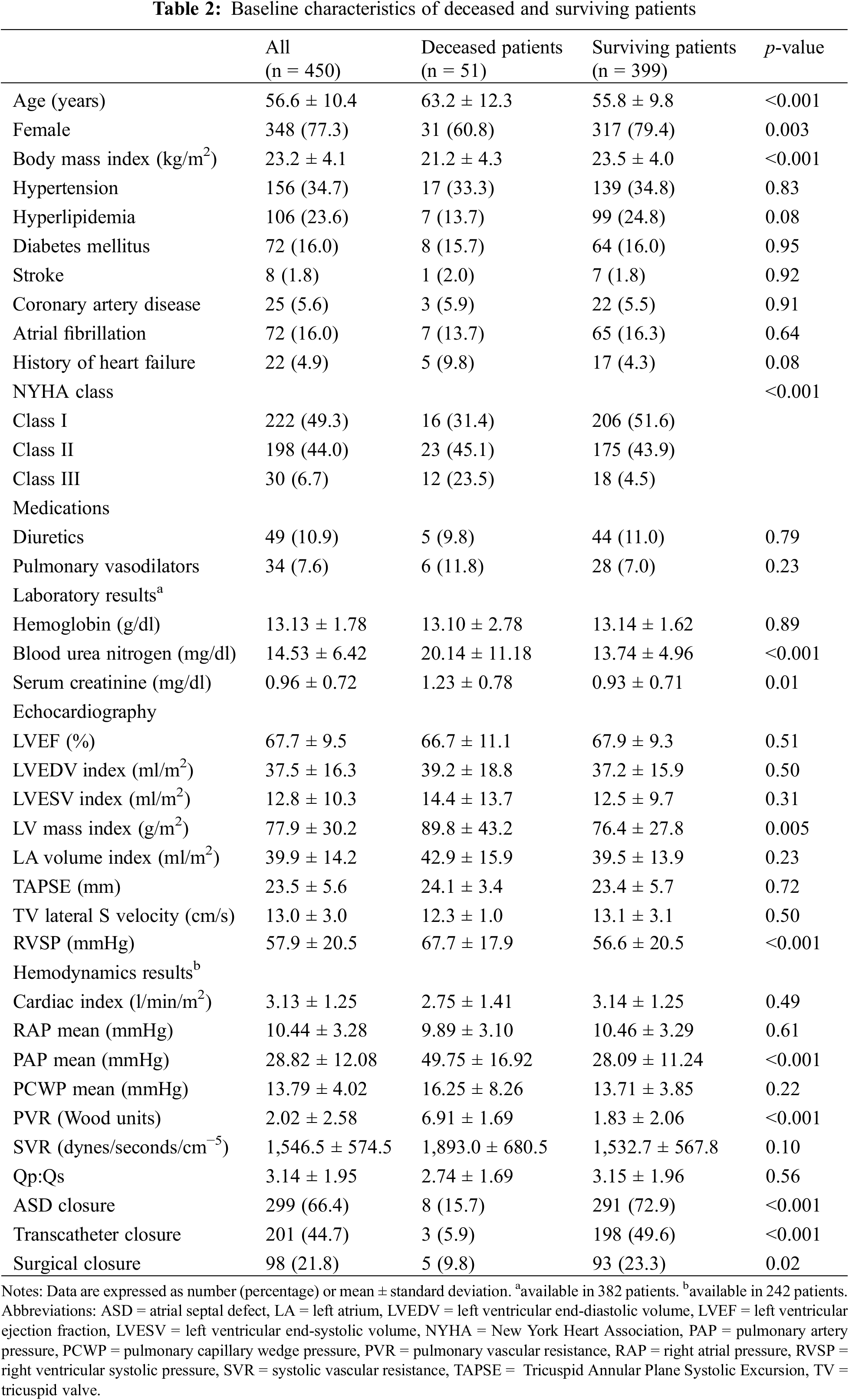
Fig. 1A presents the Kaplan-Meier curve, illustrating the comparison of mortality rates between patients with and without ASD closure in the entire cohort. Patients who underwent ASD closure had a significantly lower mortality rate compared to those without ASD closure (p < 0.001). When the patients were divided into two age groups, specifically 40–60 years (Fig. 1B) and over 60 years (Fig. 1C), it was consistent that patients with ASD closure exhibited a lower mortality rate in both age groups. Fig. 2 depicts the comparison of the mortality rates between patients who underwent transcatheter and surgical closure. There was no significant difference in the mortality rates between the two techniques (p = 0.05).
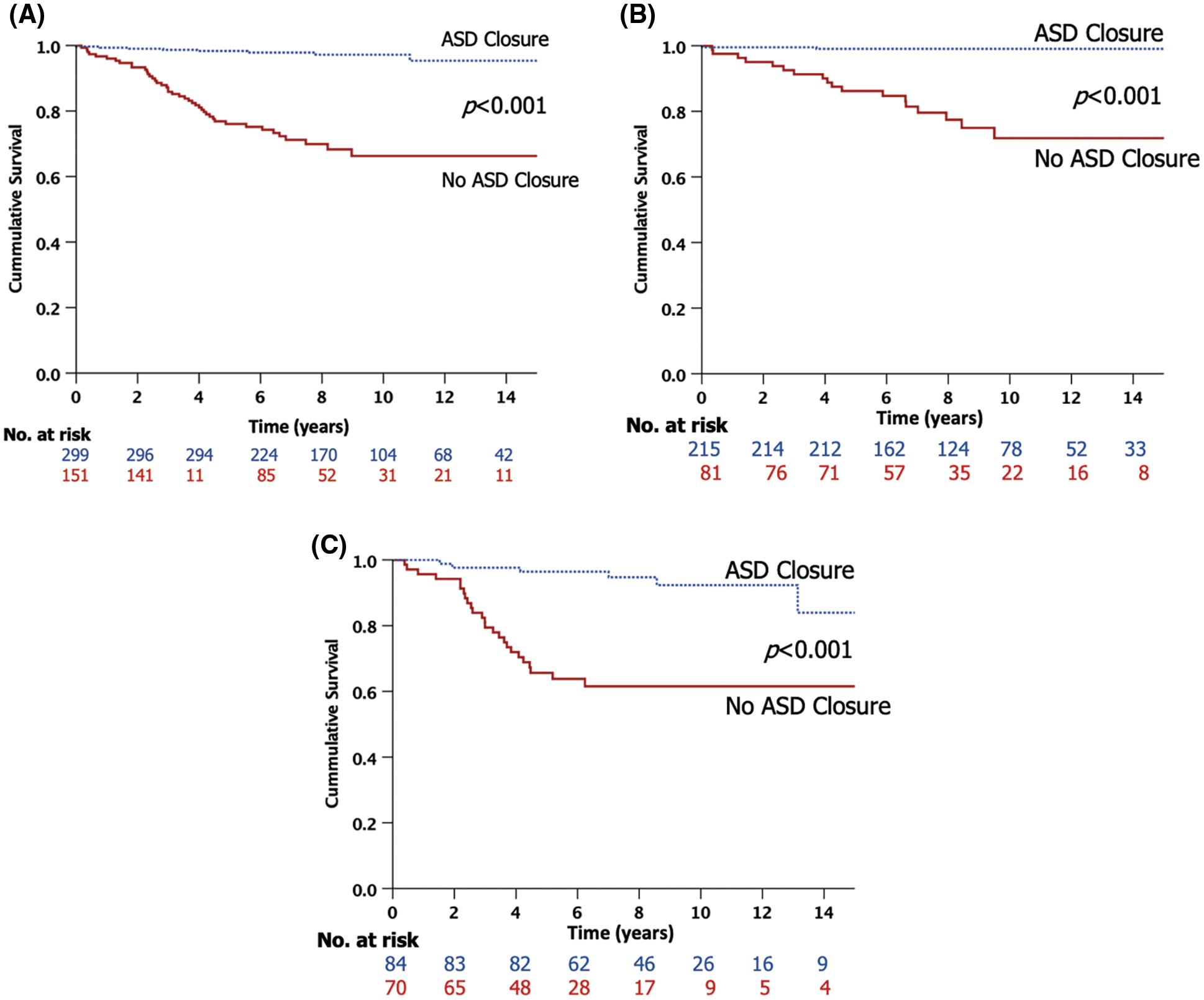
Figure 1: Kaplan-Meier survival analysis of atrial septal defect (ASD) patients stratified by ASD closure. (A) Patients of all ages. (B) Patients aged 40–60 years. (C) Patients aged over 60 years
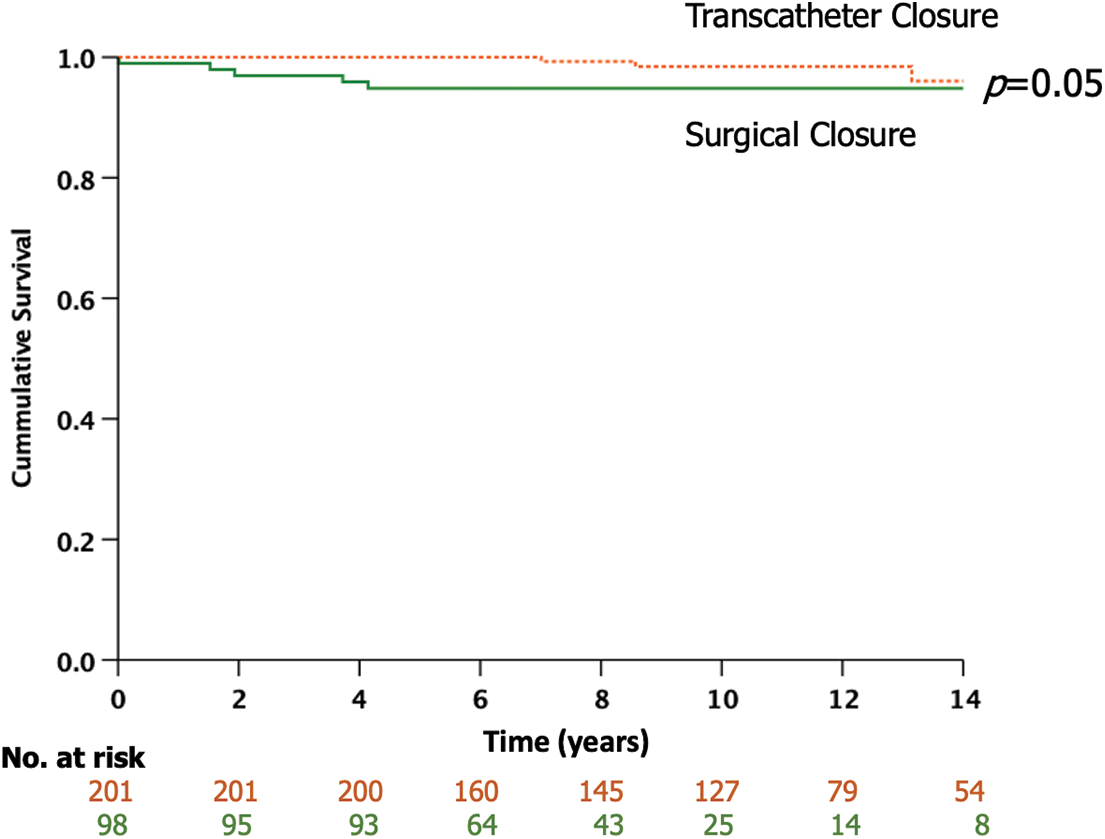
Figure 2: Kaplan-Meier survival analysis of atrial septal defect (ASD) patients stratified by transcatheter and surgical closure
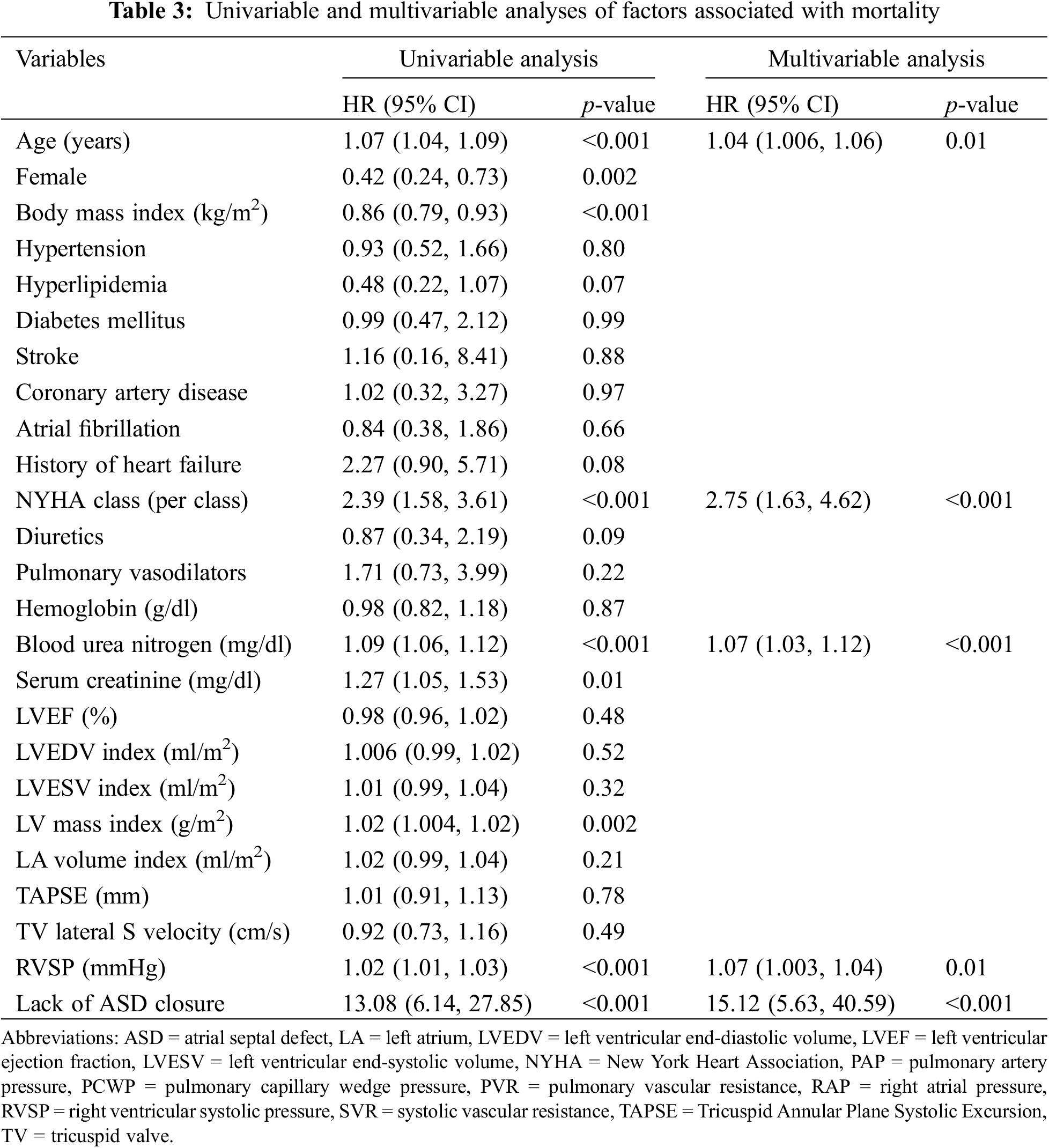
Table 3 shows univariable and multivariable analyses of factors associated with mortality. The results of the univariable analysis demonstrated age, male, body mass index, NYHA class, BUN, serum creatinine, LV mass index, RVSP, and lack of ASD closure were associated with mortality (p < 0.05 for all). The multivariable analysis, after adjusting for other variables, demonstrated that age (HR 1.04, 95% CI 1.006–1.06, p = 0.01), NYHA class (HR 2.75, 95% CI 1.63–4.62, p < 0.001), BUN (HR 1.07, 95% CI 1.03–1.12, p < 0.001), RVSP (HR 1.07, 95% CI 1.003–1.04, p = 0.01), and lack of ASD closure (HR 15.12, 95% CI 5.63–40.59, p < 0.001) were independently associated with mortality.
Our main findings revealed that older patients who underwent ASD closure had a significantly lower mortality rate compared to those without ASD closure. Age, NYHA class, BUN, RVSP, and lack of ASD closure were identified as independent factors associated with mortality. Furthermore, no significant difference in mortality rate was observed between patients who underwent transcatheter and surgical closure.
ASD closure in young adults offers several benefits, including the prevention of complications such as pulmonary hypertension and arrhythmias, improvement in symptoms, and reduction in long-term cardiovascular events such as heart failure [5,6,17]. Significant ASDs should be early occluded, and closure might offer benefits for older adults. However, the assessment of risks and benefits should be thoroughly considered before referral, particularly in the very old age group. Elderly individuals with ASDs often experience symptoms like dyspnea, palpitations, or paradoxical embolization, placing them at an increased risk of developing arrhythmias and pulmonary hypertension. The presence of pulmonary hypertension complicates the management of ASDs, presenting plausible scenarios involving both pre-capillary and post-capillary pulmonary hypertension linked to left-sided heart disease. These conditions add complexity to predicting the patient’s response to ASD closure, necessitating the use of various valid tools to assess hemodynamic changes immediately and during mid-term follow-up after ASD closure.
Several publications have demonstrated the benefits of ASD closure in older adults. For instance, Giordano et al. conducted a study involving 68 patients aged over 60 years and showed that transcatheter ASD closure was both safe and feasible. The closure procedure resulted in improvements in symptoms, right ventricle remodeling, and the overall hemodynamic profile of the patients [18]. A meta-analysis by Baroutidou et al. which included 18 cohorts, demonstrated that transcatheter ASD closure in patients over 60 years improves functional capacity, biventricular dimensions, pulmonary pressures, TR severity, and brain natriuretic peptide [19]. Some studies also showed the mortality benefit of transcatheter ASD closure in this population [19].
In our study, patients who underwent closure of ASD using either transcatheter or surgical methods had significantly lower mortality rates compared to patients without ASD closure. The unadjusted cumulative 10-year mortality rate was 3% for patients with closure vs. 28% for those without closure. These findings were consistent with the studies conducted by Humenberger et al. and Takaya et al. [12,20]. Humenberger et al. demonstrated that transcatheter closure of secundum ASD in 236 patients led to symptom improvement and regression of PAP and right ventricular size, regardless of age [12]. Similarly, Takaya et al. found that in patients aged over 50 years who underwent transcatheter closure of secundum ASD, those in the older age group had similar rates of mortality and hospitalization due to heart failure or stroke compared to the younger age group [20]. Our study also provided additional value by including one-third of patients who underwent surgical closure of ASD, and the mortality rate was also low in this population. This finding was consistent with the study conducted by Kotowyczetal et al. which showed no significant difference in the mortality rates between ASD patients who underwent transcatheter or surgical closure, despite the relatively young mean age of 43 years in their study [21].
In our study, the majority of patients (94%) had secundum ASD, while 4% had sinus venosus type, 2% had primum type, and 0.4% had coronary sinus type. The surgical closure of types other than the secundum type presents challenges due to technical difficulties. Surgical repair of sinus venosus ASD can result in pulmonary vein or superior vena cava stenosis, as well as injury to the sinus node or its arterial supply, resulting in postoperative low atrial rate or junctional rhythm [22]. Surgical repair of primum ASD is also challenging since it is preferably performed in younger patients to reduce the risk of persistent atrial arrhythmias or pulmonary hypertension later in life. Primum ASD is commonly associated with regurgitation of the atrioventricular valve, as well as a mitral valve cleft, both of which should be repaired. Coronary sinus type ASD is rare and often associated with the left superior vena cava (LSVC). The hemodynamic changes in coronary sinus type ASD depend on multiple conditions, such as the presence of the LSVC, whether the coronary sinus opening is expanded or constricted, and the presence of associated malformations like blood flow obstruction in the left or right atrioventricular system [23]. It is recommended that the procedure be performed in experienced centers.
Our study identified age, NYHA class, BUN, RVSP, and lack of ASD closure as independent factors associated with mortality. It is well-established that age and NYHA class are correlated with adverse events such as heart failure or cardiac mortality in this population. Furthermore, RVSP, which reflects the degree of right ventricular pressure load and pulmonary hypertension, is also recognized to be associated with congenital heart disease characterized by a left-to-right shunt. BUN was also identified as one of the independent predictors of mortality in our study. The prevalence of renal dysfunction is increasing in patients with congenital heart disease, particularly in the older population [24,25]. However, data regarding the prevalence, pathophysiology, and prognosis of kidney disease in the adult congenital heart disease population remain scarce. Dimopoulos et al. demonstrated that patients with congenital heart disease, including 13.8% with ASD, and moderately or severely declined glomerular filtration rate (GFR) (<60 ml/min/1.73 m2) had a 5-fold increase in their 6-year mortality rate compared to those with normal GFR [26]. Our results align with Dimopoulos’s study, indicating that renal dysfunction is significantly associated with mortality in patients with congenital heart disease. Therefore, the management of older patients with congenital heart disease should include careful consideration of renal function as a critical factor.
Our study had several limitations worth mentioning. Firstly, it is important to acknowledge that our study was retrospective in nature, introducing the possibility of bias, confounders, and incomplete data for some variables that cannot be completely eliminated. Specifically, patient selection for ASD closure, as well as the closure techniques, was determined by the cardiologists. Nevertheless, we employed the multivariable analysis to mitigate these limitations to the best extent possible. Secondly, our study was conducted at a single tertiary center, and it is important to consider that our center had a relatively low rate of surgical complications compared to others. Therefore, the generalizability of our findings to other centers may be limited. Thirdly, the lack of data regarding changes in echocardiographic parameters following ASD closure, as well as other clinical events such as heart failure events or new-onset atrial fibrillation needs mentioning. It is important to acknowledge that retrospective studies may not provide the most accurate assessment of these variables. However, despite these limitations, the observed mortality benefit was substantial enough to support the overall benefit of ASD closure in this specific population.
ASD closure demonstrated favorable outcomes in older patients. Age, NYHA class, BUN, RVSP, and lack of ASD closure were identified as independent factors linked to mortality in this population.
Acknowledgement: None.
Funding Statement: The authors received no specific funding for this study.
Author Contributions: The authors confirm contribution to the paper as follows: SK–Conception and design, research operation, data collecting, analysis and interpretation of data, discussion of the results, drafting of the manuscript or revising it critically for important intellectual content, and final approval of the manuscript submitted. YK–Conception and design, research operation, data collecting, analysis and interpretation of data, discussion of the results, drafting of the manuscript or revising it critically for important intellectual content, and final approval of the manuscript submitted. KK–Research operation, analysis and interpretation of data, discussion of the results, and final approval of the manuscript submitted. NR–Conception and design, research operation, data collecting, analysis and interpretation of data, discussion of the results, drafting of the manuscript or revising it critically for important intellectual content, and final approval of the manuscript submitted.
Availability of Data and Materials: The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics Approval: This study was approved by the Siriraj Institutional Review Board (SIRB), Faculty of Medicine Siriraj Hospital, Mahidol University (COA no. Si 760/2021). The need for consent was waived by the board due to its retrospective nature and as all personal identifying information was obliterated. The study protocol conforms to the ethical guidelines of the 1975 Declaration of Helsinki.
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
References
1. Lindsey JB, Hillis LD. Clinical update: atrial septal defect in adults. Lancet. 2007;369(9569):1244–6. [Google Scholar] [PubMed]
2. Tuan HX, Long PTP, Kien VD, Le MC, Son NV, Dalla-Pozza R. Trends in the prevalence of atrial septal defect and its associated factors among congenital heart disease patients in vietnam. J Cardiovasc Dev Dis. 2019;7(1):2. [Google Scholar]
3. Khan AA, Tan JL, Li W, Dimopoulos K, Spence MS, Chow P, et al. The impact of transcatheter atrial septal defect closure in the older population: a prospective study. JACC Cardiovasc Interv. 2010;3(3):276–81. [Google Scholar] [PubMed]
4. Nakagawa K, Akagi T, Taniguchi M, Kijima Y, Goto K, Kusano KF, et al. Transcatheter closure of atrial septal defect in a geriatric population. Catheter Cardiovasc Interv. 2012;80(1):84–90. [Google Scholar] [PubMed]
5. Roos-Hesselink JW, Meijboom FJ, Spitaels SE, van Domburg R, van Rijen EH, Utens EM, et al. Excellent survival and low incidence of arrhythmias, stroke and heart failure long-term after surgical ASD closure at young age. A prospective follow-up study of 21–33 years. Eur Heart J. 2003;24(2):190–7. [Google Scholar] [PubMed]
6. Attie F, Rosas M, Granados N, Zabal C, Buendía A, Calderón J. Surgical treatment for secundum atrial septal defects in patients >40 years old. A randomized clinical trial. J Am Coll Cardiol. 2001;38(7):2035–42. [Google Scholar] [PubMed]
7. Chessa M, Carminati M, Butera G, Bini RM, Drago M, Rosti L, et al. Early and late complications associated with transcatheter occlusion of secundum atrial septal defect. J Am Coll Cardiol. 2002;39(6):1061–5. [Google Scholar] [PubMed]
8. Majunke N, Bialkowski J, Wilson N, Szkutnik M, Kusa J, Baranowski A, et al. Closure of atrial septal defect with the Amplatzer septal occluder in adults. Am J Cardiol. 2009;103(4):550–4. [Google Scholar] [PubMed]
9. Shrivastava S, Shrivastava S, Allu SVV, Schmidt P. Transcatheter closure of atrial septal defect: a review of currently used devices. Cureus. 2023;15(6):e40132. [Google Scholar] [PubMed]
10. Butera G, Carminati M, Chessa M, Youssef R, Drago M, Giamberti A, et al. Percutaneous versus surgical closure of secundum atrial septal defect: comparison of early results and complications. Am Heart J. 2006;151(1):228–34. [Google Scholar] [PubMed]
11. Rosas M, Zabal C, Garcia-Montes J, Buendia A, Webb G, Attie F. Transcatheter versus surgical closure of secundum atrial septal defect in adults: impact of age at intervention. A concurrent matched comparative study. Congenit Heart Dis. 2007;2(3):148–55. [Google Scholar] [PubMed]
12. Humenberger M, Rosenhek R, Gabriel H, Rader F, Heger M, Klaar U, et al. Benefit of atrial septal defect closure in adults: impact of age. Eur Heart J. 2011;32(5):553–60. [Google Scholar] [PubMed]
13. Elshershari H, Cao QL, Hijazi ZM. Transcatheter device closure of atrial septal defects in patients older than 60 years of age: immediate and follow-up results. J Invasive Cardiol. 2008;20(4):173–6. [Google Scholar] [PubMed]
14. Jategaonkar S, Scholtz W, Schmidt H, Horstkotte D. Percutaneous closure of atrial septal defects: echocardiographic and functional results in patients older than 60 years. Circ Cardiovasc Interv. 2009;2(2):85–9. [Google Scholar] [PubMed]
15. Komar M, Przewlocki T, Olszowska M, Sobien B, Podolec P. The benefit of atrial septal defect closure in elderly patients. Clin Interv Aging. 2014;9:1101–7. [Google Scholar] [PubMed]
16. Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2015;28(1):1–39.e14. [Google Scholar] [PubMed]
17. Boudiche S, Chatti S, Amroussia R, Mghaieth F, Ziadi J, Farhati A, et al. Atrial septal defect closure in adults: a ten-year experience. Tunis Med. 2019;97(12):1362–9. [Google Scholar] [PubMed]
18. Giordano M, Gaio G, D’Alto M, Santoro G, Scognamiglio G, Cappelli Bigazzi M, et al. Transcatheter closure of atrial septal defect in the elderly: early outcomes and mid-term follow-up. Inte J Cardiol Congenital Heart Dis. 2020;1:100058. [Google Scholar]
19. Baroutidou A, Arvanitaki A, Farmakis IT, Patsiou V, Giannopoulos A, Efthimiadis G, et al. Transcatheter closure of atrial septal defect in the elderly: a systematic review and meta-analysis. Heart. 2023;109(23):1741–50. [Google Scholar] [PubMed]
20. Takaya Y, Akagi T, Kijima Y, Nakagawa K, Sano S, Ito H. Long-term outcome after transcatheter closure of atrial septal defect in older patients: impact of age at procedure. JACC Cardiovasc Interv. 2015;8(4):600–6. [Google Scholar] [PubMed]
21. Kotowycz MA, Therrien J, Ionescu-Ittu R, Owens CG, Pilote L, Martucci G, et al. Long-term outcomes after surgical versus transcatheter closure of atrial septal defects in adults. JACC Cardiovasc Interv. 2013;6(5):497–503. [Google Scholar] [PubMed]
22. Attenhofer Jost CH, Connolly HM, Danielson GK, Bailey KR, Schaff HV, Shen WK, et al. Sinus venosus atrial septal defect: long-term postoperative outcome for 115 patients. Circ. 2005;112(13):1953–8. [Google Scholar]
23. Shi H, Yan J, Wang Q, Hua Z, Li S, Zhang J. Surgical management of unroofed coronary sinus syndrome: a 20-year-single-center experience. J Card Surg. 2021;36(2):589–95. [Google Scholar] [PubMed]
24. El Sayegh S, Ephrem G, Wish JB, Moe S, Lim K. Kidney disease and congenital heart disease: partnership for life. Front Physiol. 2022;13:970389. [Google Scholar] [PubMed]
25. Gillesén M, Fedchenko M, Giang KW, Dimopoulos K, Eriksson P, Dellborg M, et al. Chronic kidney disease in patients with congenital heart disease: a nationwide, register-based cohort study. Eur Heart J Open. 2022;2(5):oeac055. [Google Scholar]
26. Dimopoulos K, Diller GP, Koltsida E, Pijuan-Domenech A, Papadopoulou SA, Babu-Narayan SV, et al. Prevalence, predictors, and prognostic value of renal dysfunction in adults with congenital heart disease. Circ. 2008;117(18):2320–8. [Google Scholar]
Cite This Article
 Copyright © 2024 The Author(s). Published by Tech Science Press.
Copyright © 2024 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools