 Open Access
Open Access
EDITORIAL
Femoral Access with Ultrasound-Guided Puncture and Z-Stitch Hemostasis for Adults with Congenital Heart Diseases Undergoing Electrophysiological Procedures
1 Arrhythmia and Electrophysiology Division, Department of Cardiology, University Heart Center Zurich, Zurich, Switzerland
2 Children’s Research Center, Zurich University Children’s Hospital, Zurich, Switzerland
3 Center for Integrative Human Physiology, University of Zurich, Zurich, Switzerland
* Corresponding Authors: Fu Guan. Email: ; Thomas Wolber. Email:
Congenital Heart Disease 2024, 19(1), 85-92. https://doi.org/10.32604/chd.2024.047266
Received 31 October 2023; Accepted 30 January 2024; Issue published 20 March 2024
Abstract
Aims: Although the application of ultrasound-guided vascular puncture and Z-stitch hemostasis to manage femoral access has been widely utilized, there is limited data on this combined application in adult congenital heart disease (ACHD) patients undergoing electrophysiological (EP) procedures. We sought to evaluate the safety and efficacy of ultrasound-guided puncture and postprocedural Z-stitch hemostasis for ACHD patients undergoing EP procedures. Methods and Results: The population of ACHD patients undergoing transfemoral EP procedures at the University of Zurich Heart Center between January 2019 and December 2022 was observed and analyzed. During the study period, femoral access (left/right, arterial/venous) was performed under real-time ultrasound guidance. At the end of the procedure, a single Z-stitch was performed at the puncture site. We evaluated the incidence of in-hospital complications associated with femoral access puncture in this population. Among 101 patients who had a total of 147 previous ipsilateral vascular punctures (mean 1.5 per person), 100 patients underwent successful femoral vascular access for EP procedures. The median age of the patients was 47 ± 15 years and 34 (34%) were male. Z-stitches were performed after the procedure in 100 patients with 303 femoral vascular accesses (mean 3 punctures per person). No patient developed vascular puncture relevant inguinal hematoma, pseudo aneurysm, arteriovenous fistula, venous or arterial thrombosis. Conclusion: In ACHD patients undergoing EP procedures, optimal femoral access management can be achieved with ultrasound-guided puncture and postprocedural Z-stitch hemostasis.Keywords
Vascular access complications are known as one of the most common complications during cardiac interventional procedures. The current use of large-diameter venous sheaths, perioperative anticoagulation, and multisite, or multiple times of punctures at the same site might increase puncture complications. Safe puncture and effective hemostatic techniques are critical to prevent these complications. In this regard, ultrasound-guided vascular puncture has been widely recommended in cardiac interventional procedures, which greatly increases the safety and accuracy of puncture, and the appropriate puncture site creates superior conditions for postoperative hemostasis. Meanwhile, the arterial puncture was closed by vascular suture devices such as collagen-based devices or suture-based devices [1], but the closure of venous access varies from center to center. However, more and more practices confirm that Z-suture is effective in achieving rapid and effective postoperative hemostasis and reducing the patient’s absolute bed rest and limitation of limb movement [2].
The number of electrophysiological procedures (EP) in adult patients with congenital heart disease (ACHD) is increasing. Preoperative oral anticoagulation is widely used in this population with a potential risk for thromboembolic complications [3]. EP procedures are often performed without interruption of oral anticoagulants. Observational data regarding puncture site outcomes in the ACHD population are limited. Our study sought to determine the efficacy and safety of vascular access by preprocedural ultrasound-guided puncture and postprocedural Z-stitch hemostasis for ACHD patients undergoing EP procedures.
We studied ACHD patients undergoing transfemoral EP procedures at the University Heart Center Zurich between January 2019 and December 2022. Medical records were reviewed retrospectively to identify patients diagnosed with CHD and underwent EP study or treated with catheter ablation for cardiac arrhythmias. Inclusion criteria included (1) an age of ≥18 years, (2) a CHD diagnosis, and (3) endocardial EP study/catheter ablation (combined with or without right heart catheterization). Patients were excluded from the cohort if there was no available information on the CHD diagnosis and related treatment. Written informed consent for catheter ablation/EP study was obtained from all patients before the procedure. Patients provided general consent for inclusion in retrospective research in our center. In this population, femoral vascular (left/right) punctures were performed with real-time ultrasound guidance, and a single Z-stitch was applied at the end of the procedure during sheath removal (Fig. 1). We sought to evaluate the safety and efficacy of ultrasound-guided femoral vascular puncture and Z-stitch hemostasis for ACHD patients undergoing EP procedures. This study complied with the Declaration of Helsinki and was approved by the local Ethics Committee (Cantonal Ethics Committee Zurich, Nr. 2016-00116). All patients signed informed consent for the procedure and the use of clinical data for scientific study.
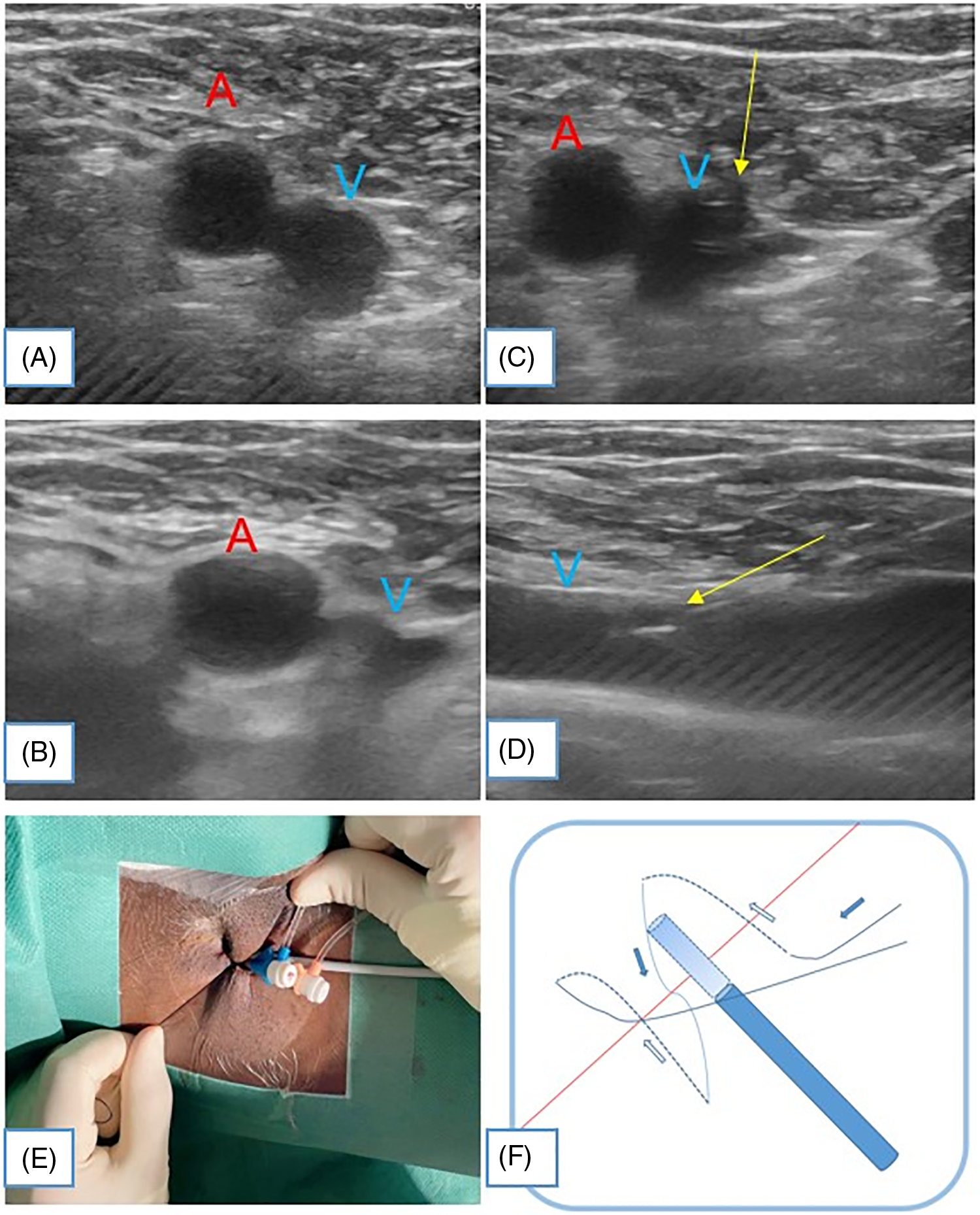
Figure 1: Ultrasound-guided femoral vein puncture and Z-stitch hemostasis. Short axis (A) and long axis views (B) of the puncture site to guide the femoral vein puncture. The vein is compressed by the real-time ultrasound probe (B) and may be confirmed by additional color or PW Doppler. A good response to compression suggests an appropriate site for hemostasis due to the reliable basal support of the femoral head. Puncture (arrow) is performed through the short axis (C) and tracked by the long axis (D) to avoid over-penetration of the inferior wall of the femoral vein causing possible injury to the deep femoral artery, which could lead to hematoma or even an AV fistula. During the removal of the sheath, prepare the knot for the Z-shaped stitch (E). (F) Schematic for Z-shaped stitch, solid lines and blue arrows indicate in vitro, dotted lines and white arrows indicate in subcutaneous tissue
The interventions were performed without interruption of oral anticoagulation, i.e., patients on warfarin had an international normalized ratio (INR) > 2, while for patients on novel oral anticoagulants, the last dose was taken the night before the procedure and the equivalent dose was restarted on the evening of the operation day. Intravenous heparin 2000–3000 IU was administered after a successful percutaneous puncture based on our experience. For patients with left atrial interventions, repetitive heparin doses were given, and activated clotting time (ACT) was monitored intraoperatively aiming at >300 s. At the end of the procedure, a single Z-stitch was applied at the puncture site and sheaths were removed immediately, without the use of protamine to antagonize heparin. Manual local compression was rarely required, or compression lasted less than a minute until the hemostasis was achieved. Therefore the duration of manual compression was not recorded intraoperatively. The patients were kept in bed in order to immobilize the right/left lower extremity for 4 to 6 h. The Z-stitch was removed 6–8 h after the procedure. Analgesics were used as needed.
At the time of hospital discharge, typically on the day following the intervention, the puncture site of all patients was clinically examined through inspection, palpation, and auscultation. In cases of pain or detection of a flow murmur during auscultation, vascular ultrasound with duplex sonography was additionally performed to exclude fistula, dissection, or thrombosis.
We evaluated the incidence of in-hospital complications associated with femoral access puncture in this population (Table 1). Among 101 patients who had 147 previous vascular punctures (mean 1.5 per person), 100 patients underwent successful femoral vascular punctures. Prior to the procedure, 3 (3%) were found to have unilateral venous occlusions. The median age of the patients was 47 ± 15 years and 34 (34%) were male. Two patients (2%) were underweight and 14 (14%) were overweight. Out of 303 femoral vascular accesses performed (mean 3 per person), there were two ipsilateral femoral arterial punctures. The arterial puncture was closed with an Angio-Seal closure device.
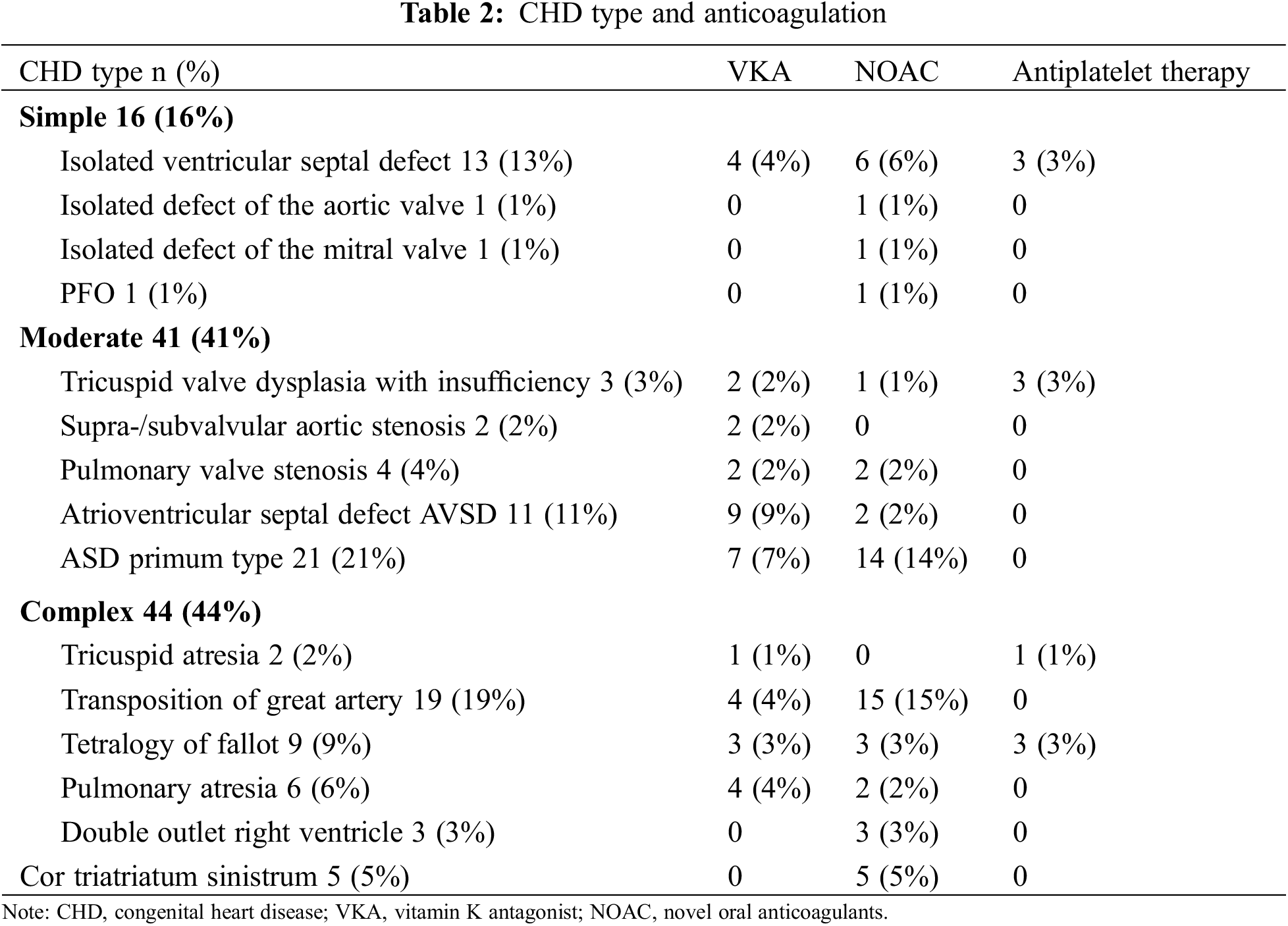
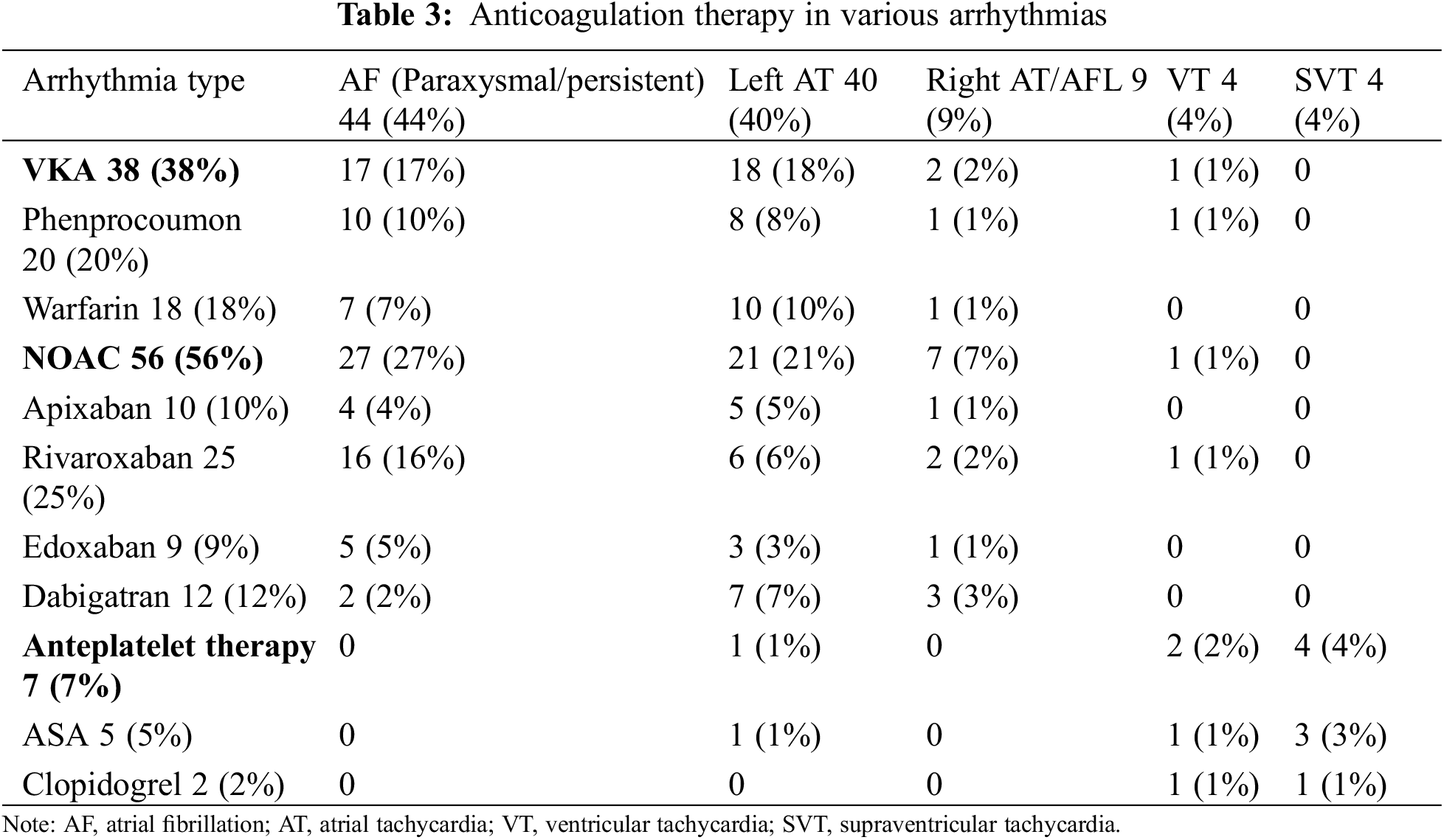
CHD types with grouping of complexity are shown in Table 2. The majority of the patients in the cohort had moderate to severe complex CHD (41% moderate complex, and 44% severe complex), as shown in Table 2. Anticoagulation and antiplatelet therapy were categorized according to the type of arrhythmia (Table 3). Atrial fibrillation (paroxysmal or persistent) and left-sided intraatrial tachycardia constituted the highest proportion, as a result, there was a high percentage of NOAC and VKA application in our cohort. There was no interruption of oral anticoagulation during the perioperative period. 38 (38%) patients were anticoagulated with VKA, 56 (56%) with NOAC, and 7 (7%) with aspirin/clopidogrel. The total operative time was 130 min, and 100 Z-sutures were performed at the end of the procedure. No patient had an associated inguinal hematoma, pseudo aneurysm, arteriovenous fistula, venous or arterial embolism, or stroke. In one patient, the procedure had to be terminated early because the guidewire could not be advanced. Venography confirmed preexistent femoral venous occlusion.
In this study, we observed a group of ACHD patients who underwent cardiac catheter ablation with uninterrupted anticoagulants. With the combined adoption of preprocedural ultrasound-guided vascular puncture and postprocedural Z-stitch hemostasis, no thromboembolic complications, hemorrhage, or vascular access complications were observed. This clinical protocol was proved to be efficient and safe in ACHD patients undergoing EP procedures.
Ultrasound-guided peripheral vascular puncture has become highly recommended for clinical procedures via peripheral access, including EP procedures [2]. Moreover, hemostasis with Z-stitch or figure-of-eight suture after sheath withdrawal has been shown to be safe and effective in these patients [6]. To our knowledge, this is the first report to describe the combined application of ultrasound-guided femoral access puncture and Z-stitch hemostasis in ACHD patients with previous ipsilateral venous/arterial punctures.
ACHD patients may pose a challenge because they often have a history of prior transfemoral catheterization procedures, such as right heart catheterization and interventional repair procedures. In addition, they might also suffer from a higher incidence of vascular alignment malformations [7,8]. This combined application is an effective approach for successful femoral vascular puncture followed by effective hemostasis, which is likely the result of the optimized localization for both vascular access and hemostasis. Thus, in our single-center, previously fully anticoagulated cohort of ACHD patients undergoing EP study and catheter ablation procedures, optimal hemostasis could be achieved using a Z-stitch combined with ultrasound-guided venous access.
In adult congenital heart disease (ACHD) patients undergoing electrophysiological (EP) procedures, the combined application of ultrasound-guided vascular puncture and Z-stitch hemostasis to manage femoral access is safe and efficient. It is highly suggestive to widely utilize this protocol as a clinical routine.
Acknowledgement: Special thanks to Matthias Greutmann and Francesca Bonassin for their insightful input in writing the article.
Funding Statement: The authors received no specific funding for this study.
Author Contributions: Conceptualization, F.G.; Data curation, F.G., M.G. and T.W.; Formal analysis, F.G. and M.G.; Investigation, F.G., M.G., H.S., F.B. and T.W.; Project administration and supervision, T.W., F.D.; Writing—original draft, F.G.; Writing review and editing, F.G., M.G., F.B., H.S., F.D. and T.W. All authors have read and agreed to the published version of the manuscript.
Availability of Data and Materials: The data that support the findings of this study are available from the corresponding author, upon reasonable request.
Ethics Approval: This study complied with the Declaration of Helsinki and was approved by the local Ethics Committee (Cantonal Ethics Committee Zurich, Nr. 2016-00116). All patients signed informed consent for the procedure and the use of clinical data for scientific study.
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
References
1. Bechara CF, Annambhotla S, Lin PH. Access site management with vascular closure devices for percutaneous transarterial procedures. J Vasc Surg. 2010;52(6):1682–96. doi:10.1016/j.jvs.2010.04.079. [Google Scholar] [PubMed] [CrossRef]
2. Kupó P, Pap R, Sághy L, Tényi D, Bálint A, Debreceni D, et al. Ultrasound guidance for femoral venous access in electrophysiology procedures-systematic review and meta-analysis. J Interv Card Electrophysiol. 2020;59(2):407–14. doi:10.1007/s10840-019-00683-z. [Google Scholar] [PubMed] [CrossRef]
3. Foerschner L, Kriesmair J, Telishevska M, Kottmaier M, Bourier F, Reents T, et al. Catheter ablation in adult congenital heart disease on uninterrupted oral anticoagulation: is it safe? Data from a large single-center study. Heart Rhythm. 2022;19(4):648–55. doi:10.1016/j.hrthm.2021.12.018. [Google Scholar] [PubMed] [CrossRef]
4. Kappetein AP, Head SJ, Généreux P, Piazza N, van Mieghem NM, Blackstone EH, et al. Updated standardized endpoint definitions for transcatheter aortic valve implantation: the valve academic research consortium-2 consensus document. J Am Coll Cardiol. 2012;60:1438–54. doi:10.1093/eurheartj/ehs255. [Google Scholar] [PubMed] [CrossRef]
5. Mehran R, Rao SV, Bhatt DL, Gibson CM, Caixeta A, Eikelboom J, et al. Standardized bleeding definitions for cardiovascular clinical trials: a consensus report from the bleeding academic research consortium. Circ. 2011;123(23):2736–47. doi:10.1161/CIRCULATIONAHA.110.009449. [Google Scholar] [PubMed] [CrossRef]
6. Pracon R, Bangalore S, Henzel J, Cendrowska-Demkow I, Pregowska-Chwala B, Tarnowska A, et al. A randomized comparison of modified subcutaneous “Z”-stitch versus manual compression to achieve hemostasis after large caliber femoral venous sheath removal. Catheter Cardiovasc Interv. 2018;91(1):105–12. [Google Scholar] [PubMed]
7. Mandato Y, Pecoraro C, Gagliardi G, Tecame M. Azygos and hemiazygos continuation: an occasional finding in emergency department. Radiol Case Rep. 2019;14(9):1063–8. doi:10.1016/j.radcr.2019.06.003. [Google Scholar] [PubMed] [CrossRef]
8. Ligon RA, Petit CJ. Not that atretic: use of an atretic femoral vein for transcatheter pulmonary valve implantation. Catheter Cardiovasc Interv. 2017;89(2):321–3. doi:10.1002/ccd.26687. [Google Scholar] [PubMed] [CrossRef]
Cite This Article
 Copyright © 2024 The Author(s). Published by Tech Science Press.
Copyright © 2024 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF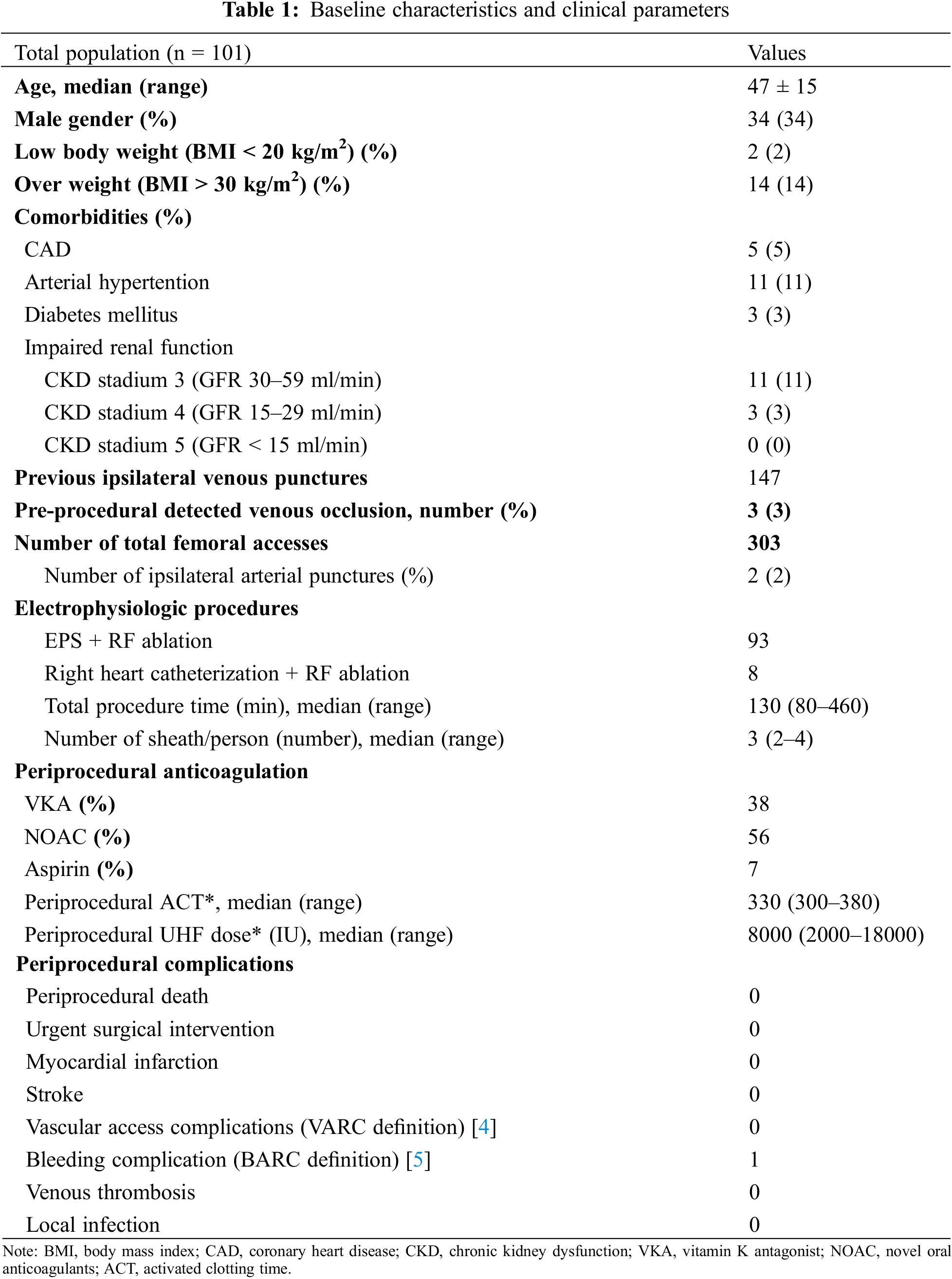
 Downloads
Downloads
 Citation Tools
Citation Tools