 Open Access
Open Access
ARTICLE
Impact of Social Determinants of Health on Self-Perceived Resilience: An Exploratory Study of Two Cohorts of Adults with Congenital Heart Disease
1 Department of Biostatistics, University of Washington, Seattle, WA, 98195, USA
2 Biostatistics Epidemiology and Analytics for Research (BEAR) Core, Seattle Children’s Research Institute, Seattle, WA, 98101, USA
3 College of Medicine, University of Washington, Seattle, WA, 98195, USA
4 Center for Clinical and Translational Research, Seattle Children’s Research Institute, Seattle, WA, 98101, USA
5 Department of Psychosocial Oncology and Palliative Care, Dana-Farber Cancer Institute; Department of Medicine, Boston Children’s Hospital, Boston, MA, 02215, USA
6 Department of Pediatrics, Harvard Medical School, Boston, MA, 02215, USA
7 Division of Pulmonary, Critical Care and Sleep Medicine, Department of Medicine & Cambia Palliative Care Center of Excellence, University of Washington, Harborview Medical Center, Seattle, WA, 98104, USA
8 Division of Cardiology, Department of Medicine & Cambia Palliative Care Center of Excellence, University of Washington, Seattle, WA, 98195, USA
* Corresponding Author: Jill M. Steiner. Email:
Congenital Heart Disease 2024, 19(1), 33-48. https://doi.org/10.32604/chd.2024.046656
Received 10 October 2023; Accepted 05 January 2024; Issue published 20 March 2024
Abstract
Social determinants of health (SDOH) affect quality of life. We investigated SDOH impacts on self-perceived resilience among people with adult congenital heart disease (ACHD). Secondary analysis of data from two complementary studies: a survey study conducted May 2021–June 2022 and a qualitative study conducted June 2020–August 2021. Resilience was assessed through CD-RISC10 score (range 0–40, higher scores reflect greater self-perceived resilience) and interview responses. Sociodemographic and SDOH (education, employment, living situation, monetary stability, financial dependency, area deprivation index) data were collected by healthcare record review and self-report. We used linear regression with robust standard errors to analyze survey data and performed a thematic analysis of interview data. Survey participants (N = 127) mean age was 42 ± 14 years; 51% were female, 87% white. ACHD was moderate (75%) or complex (25%); 41% functional class C or D. Resilience (mean 30 ± 7) varied by monetary stability: compared to people with difficulty paying bills, resilience was 15.0 points higher (95% CI: 6.9–23.1, p < 0.001) for people reporting having enough money and 14.2 points higher (95% CI: 5.9–22.4, p = 0.001) for those reporting just enough money. Interview participants’ (N = 25) mean age was 32 years (range 22–44); 52% were female, 72% white. ACHD was moderate (56%) or complex (44%); 76% functional class C or D. Participants discussed factors affecting resilience aligned with each of the major SDOH, prominently, economic stability and healthcare access and quality. Financial stability may be important for supporting self-perceived resilience in ACHD. This knowledge can inform the development of resilience interventions for this population.Graphic Abstract
Keywords
Patients with adult congenital heart disease (ACHD) often experience complex social and emotional challenges [1,2]. Many feel ill-equipped to effectively cope with illness and navigate healthcare and report poor health-related quality of life (QOL) [2,3]. Importantly, QOL and well-being are increasingly recognized to be impacted by social determinants of health (SDOH) [4]. The United States Department of Health and Human Services groups SDOH into 5 major domains: economic stability, healthcare access and quality, education access and quality, neighborhood and built environment, and social and community context [4]. Inequities in these SDOH domains are known to result in poor healthcare quality, increased disease burden, morbidity, and mortality [5,6]. In congenital heart disease, these impacts are clinically apparent across the lifespan, though studies are limited. A recent statement from the American College of Cardiology/American Heart Association called for the need to address SDOH as part of the effort to mitigate health disparities and holistically work toward healthcare equity [7]. They emphasized the need to examine access to lifelong care, provide relevant education and skill-building programs, and recognize and treat mental health concerns.
One concept central to well-being and good mental health is resilience, the process of harnessing personal resources to sustain physical and emotional well-being in the face of stress [8]. Resilience can be developed and strengthened through targeted interventions [9,10]. Personal “resilience resources,” such as skills in stress-management and meaning-making are associated with improved QOL among patients with chronic disease [11–13]. Resilience may be employed to improve QOL for patients with ACHD. However, first, a robust understanding of resilience in ACHD is necessary, as prior studies are scarce, have focused on psychological symptoms moreso than resilience or intervention efficacy, and display disparate results. Adolescents and adults with congenital heart disease often experience elevated psychological symptoms, which are associated with lower resilience. Coping style may play a role, as may childhood experiences, disease severity, and social support, among other factors [14]. SDOH likely also impacts patients’ self-perceptions of resilience, since the health- and life- challenges they face may shape the ways they experience and operationalize resilience. Therefore, the aim of this exploratory study was to investigate relationships between SDOH and patients’ perceptions of resilience among those with ACHD.
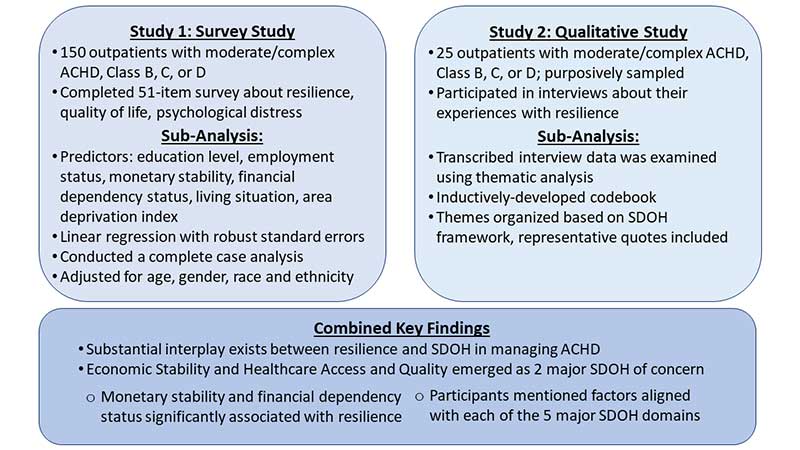
To evaluate the relationship between resilience and the major SDOH domains, we conducted secondary analyses of data from two complementary studies (Fig. 1). Each evaluated participants’ self-reported resilience and contained some SDOH data. We integrated these findings to provide a more comprehensive representation of relationships than either study provided alone. All participants provided informed consent and permission for medical record access. Both studies were approved by the University of Washington Institutional Review Board.
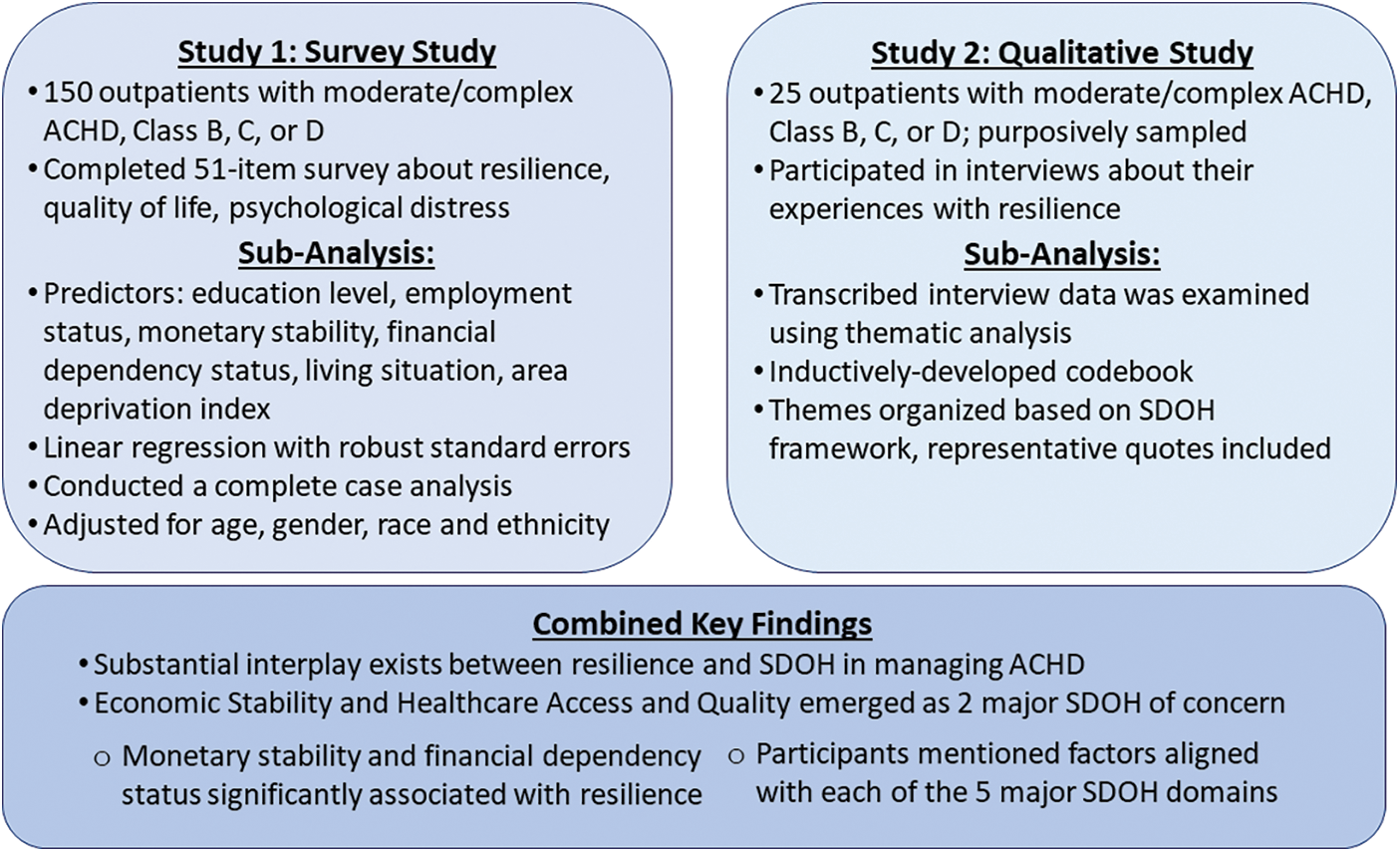
Figure 1: Overview of study design
2.1 Study 1: Survey Study [15]
Eligible participants were outpatients with confirmed ACHD who received care from the University of Washington ACHD program. ACHD anatomy was either moderate or complex, and the physiologic class was B, C, or D [16]. We excluded simple lesions and class A physiology to capture those most likely to feel impacted by their ACHD. Patients with another life-limiting illness or who were not able to independently participate in English were excluded.
Between May 2021 and June 2022, patients were approached at the time of or shortly following their ACHD clinic visit. Those who consented to participate were asked to complete an electronic survey via a personalized link provided over email. Paper surveys were available upon request. Participants received a $20 gift card for survey completion. Data were managed via REDCap.
The 51-item survey contained both standardized and investigator-developed items asking about resilience, quality of life, psychological distress, and demographic factors (race, ethnicity, education level, marital status, employment status) [SUPPLEMENT: Questionnaire]. Additional demographic data were extracted from the electronic medical record (age, gender, insurance type, and zip code used to calculate the area deprivation index [17]). Self-reported resilience was assessed with the Connor-Davidson Resilience Scale (CD-RISC 10) [18,19]. Questions in this 10-item tool evaluate personal problem-solving and approaches to adversity. Each item is scored on a 5-point scale (0–4), with an overall range of 0–40 points. Higher scores indicate higher self-perceived resilience; the mean score of a national random sample of United States adults was 32 (standard deviation 6). Predictors of interest for this analysis included: education level (reflecting Education Access and Quality), employment status, monetary stability, financial dependency status (reflecting Economic Stability), and living situation and area deprivation index (ADI, where higher scores reflect socioeconomic disadvantage) (reflecting Neighborhood and Built Environment).
We used linear regression with robust standard errors to investigate the association between resilience and predictors of interest. We fit separate models for each of the predictors, both unadjusted and adjusted for age, gender, race, and ethnicity. Due to the small numbers of participants in some categories, we excluded some participants (e.g., 2 transgender) or combined categories: race and ethnicity were categorized as White or Non-White; education was categorized as high school or less, 4-year college degree, graduate degree, or other; employment status was categorized as employed, unemployed, student, retired, or unable to work or disabled; monetary stability was categorized as difficulty paying bills no matter what, just enough to pay bills or enough money after paying bills. The same sample was used for all analyses; participants with missing outcomes, predictors of interest, or covariates (age, gender, race, and ethnicity) were excluded. We also conducted sensitivity analyses (1) removing a participant who had a reported resilience value of 0, and (2) combining the education categories of “high school or less” with “other”.
A p-value of 0.05 was used to indicate statistical significance. Statistical analyses were conducted using R (Version 4.2.2. Vienna, Austria: R Foundation for Statistical Computing).
2.2 Study 2: Qualitative Study [20]
Eligibility was the same as for Study 1. Participant selection was guided by maximum variation sampling [21] to ensure a diverse group on the following sociodemographic factors: age, gender, race and ethnicity, severity of ACHD lesion, and insurance type.
We conducted one-on-one interviews with participants from June to December 2020 and May to August 2021. Interviews were by phone or videoconference (based on patient preference) and audio recorded, transcribed verbatim, and de-identified. The interview guide [20] included queries exploring participants’ experiences with resilience. Prompts addressing sociodemographic impacts on resilience were provided if participants did not spontaneously discuss these issues. Participants received a $15 gift card for interview completion. Data were managed using Dedoose (Version 9.0, 2021. Los Angeles, CA, USA: SocioCultural Research Consultants, LLC).
The qualitative data were examined using thematic analysis [22]. Two analysts (KSB, a qualitative research scientist, and KS, a medical student trained in qualitative methods) reviewed interview excerpts marked as “SDOH” in initial coding and inductively developed a codebook specific to this question in collaboration with the study primary investigator (PI; JMS, a cardiologist physician scientist trained in qualitative methods). The codebook was further refined with reference to the SDOH framework [4] to generate a finalized codebook. Complete interview transcripts were coded by a primary (KS) and a secondary coder (KSB), with a third (JMS) acting as a tie breaker. The study team met weekly to resolve discrepancies, discuss themes, triangulate data with existing SDOH literature, and integrate findings. Lastly, the research team met for a final analysis session to reach a consensus on the presented themes.
3.1 Analysis of Study 1 Survey Data
Among the 150 enrolled participants, 23 (15%) were excluded due to missing data or few observations in a category (Table 1). Among the 127 participants included, the mean age was 42 years (standard deviation, SD: 14), 51% were female, and 12% identified as a race or ethnicity other than non-Hispanic White. ACHD was moderate for 76%, and 40% were functional class C or D. The mean resilience score was 30 (SD: 7). Survey participants excluded from this analysis had a mean resilience score of 26 (SD: 7) and tended to be single, people of color, with more severe ACHD, lower education, and reporting difficulty paying bills.
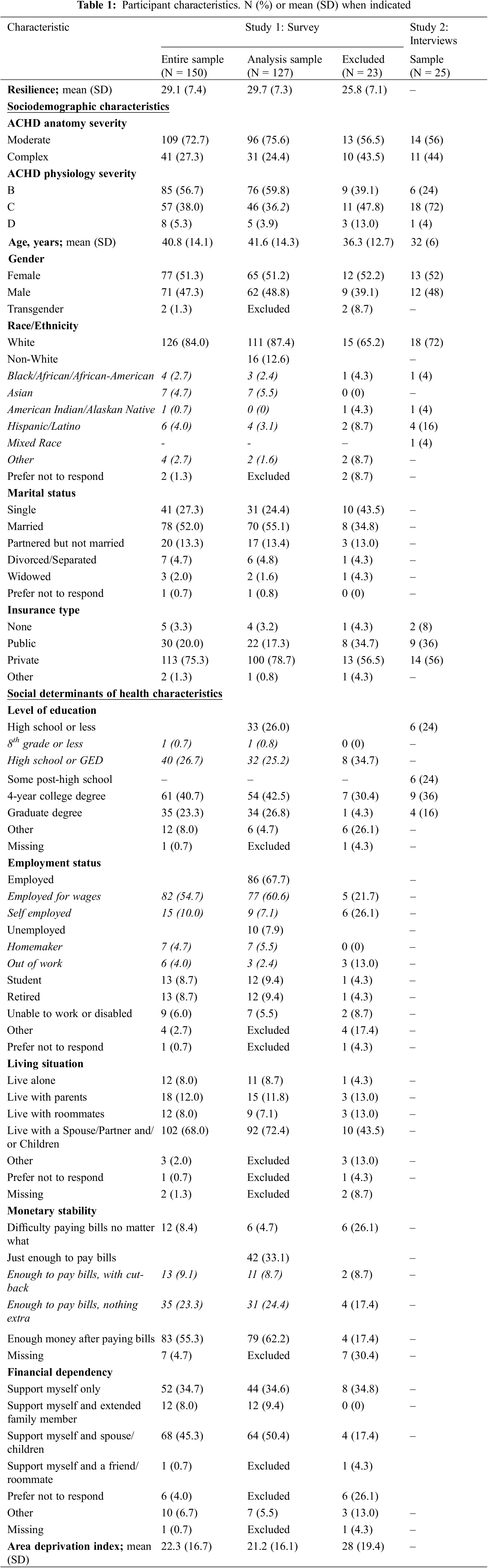
Monetary stability was associated with resilience based on both unadjusted and adjusted models (p = 0.002 for each, where the p-value refers to a test of any difference in pairwise means; Table 2, Fig. 2). Specifically, mean resilience was 15.0 points higher (95% CI: 6.9–23.1, p < 0.001) for people who reported having enough money after paying bills compared to those who reported having difficulty paying bills (Table 2, Fig. 2). Similarly, mean resilience was 14.2 points higher (95% CI: 5.9–22.4, p = 0.001) for people who reported having just enough money to pay bills compared to those who reported having difficulty paying bills. Results were similar after adjustment for age, gender, race and ethnicity (Table 2, Fig. 2).
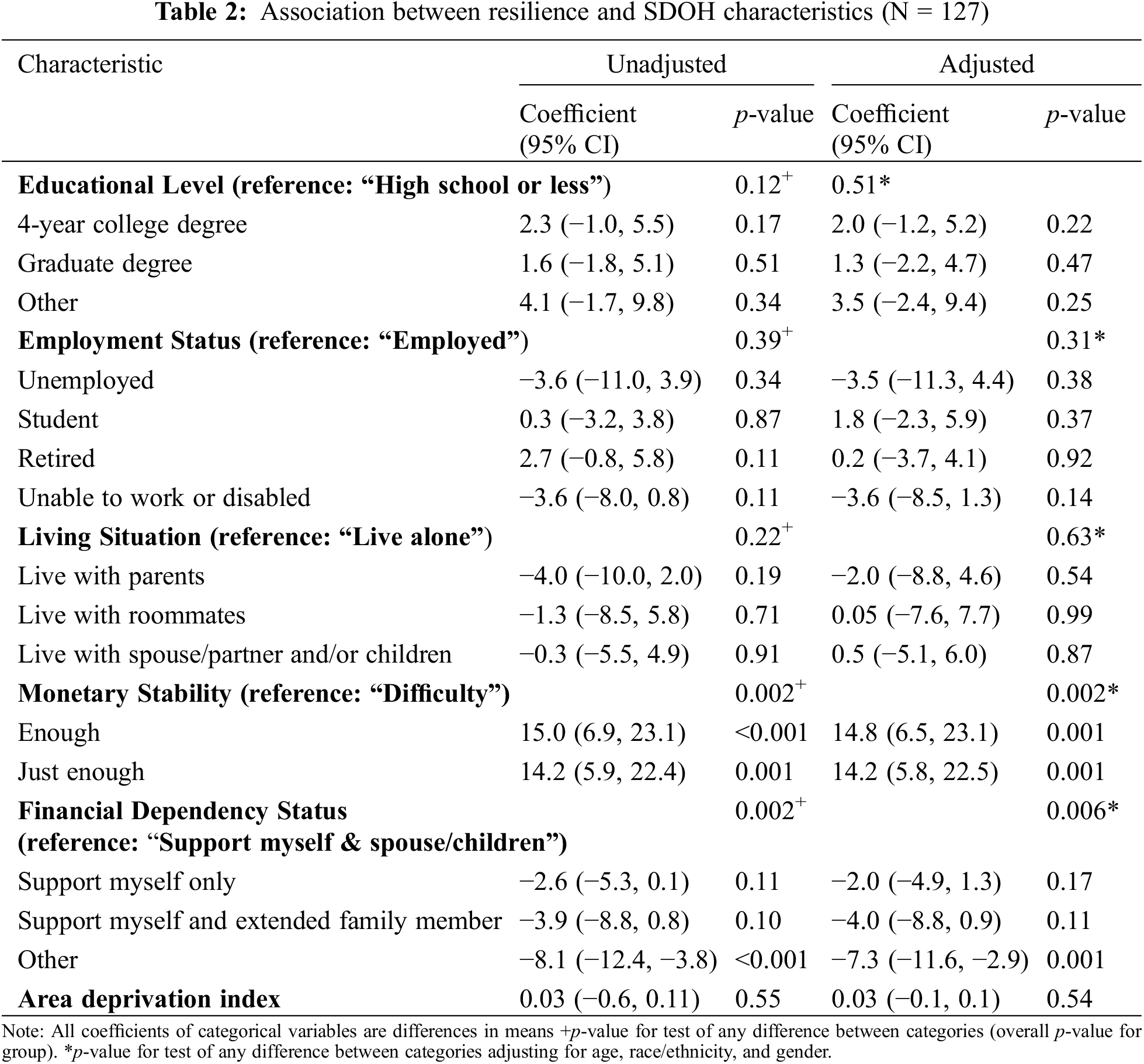
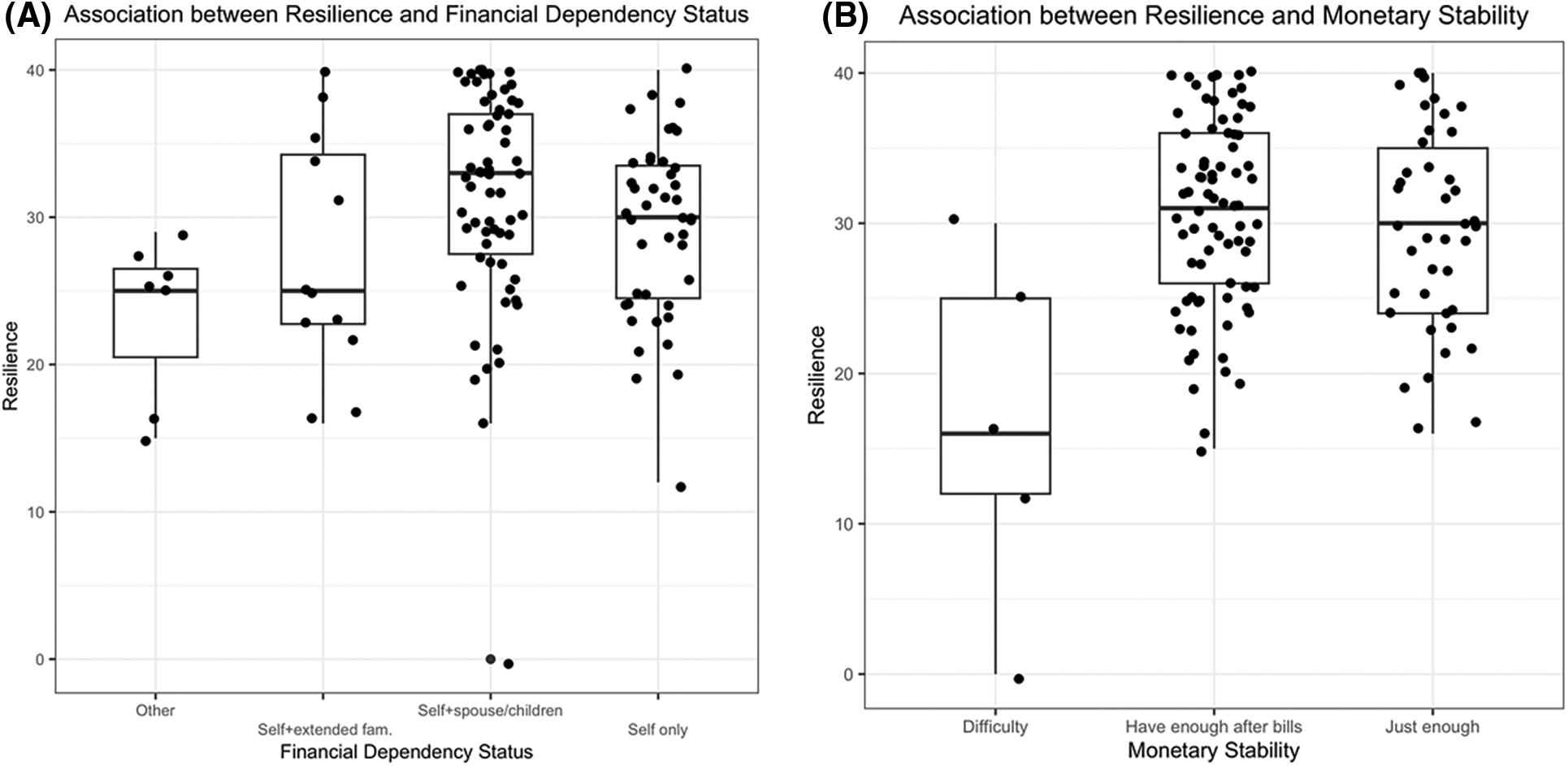
Figure 2: Boxplots of resilience by financial dependency (A) and monetary stability (B)
Financial dependency status was also associated with resilience based on both unadjusted and adjusted models (p = 0.002 and p = 0.006, respectively, for overall test of any difference among the 6 possible pairwise comparisons; Table 2, Fig. 2). Specifically, compared to people who supported themselves and a spouse or children, mean resilience was 8.1 points lower (95% CI 3.8–12.4, p < 0.001) for those who reported “other” financial dependency (Table 2, Fig. 2). Mean resilience was also significantly lower among those who reported “other” compared to people who support themselves only. We describe what “other” might represent in the Discussion section. We did not find evidence of a significant association among the other 4 pairwise comparisons. Results were similar in the adjusted models.
We did not find evidence of a significant association between resilience and education, employment, living situation, or area deprivation index. Results were similar in sensitivity analyses.
3.2 Analysis of Study 2 Interview Data
We conducted interviews with 25 participants (16 by telephone, 9 by videoconference). Interview length was 34 to 76 min. Participants’ median age was 32 years (range 22–44), 52% were female, and 28% identified as people of color. Participants’ ACHD was moderate (56%) or complex (44%); 76% were functional class C or D (Table 1).
Across all interviews and in addressing their relationship with resilience as it relates to living with ACHD, participants frequently mentioned factors aligned with each of the 5 major SDOH domains (Table 3). These topics emerged even though SDOH was not defined or explicitly referred to by interviewers. Overlaid on this was the emotional toll that accompanied these concerns (Fig. 3). Additionally, the concepts of privilege and inequity as they related to healthcare were universally mentioned in relation to resilience, underscoring their impact across multiple SDOH categories. Sociodemographic influences like race, ethnicity, gender, and age intersected with both positive and negative healthcare experiences influencing resilience. However, participants indicated that they were hesitant or not prepared to discuss these in detail. “I’ve tried really, really hard not to have opinions on that subject [race], in all ways, shapes, or forms.” -37yo man, IIIC disease.
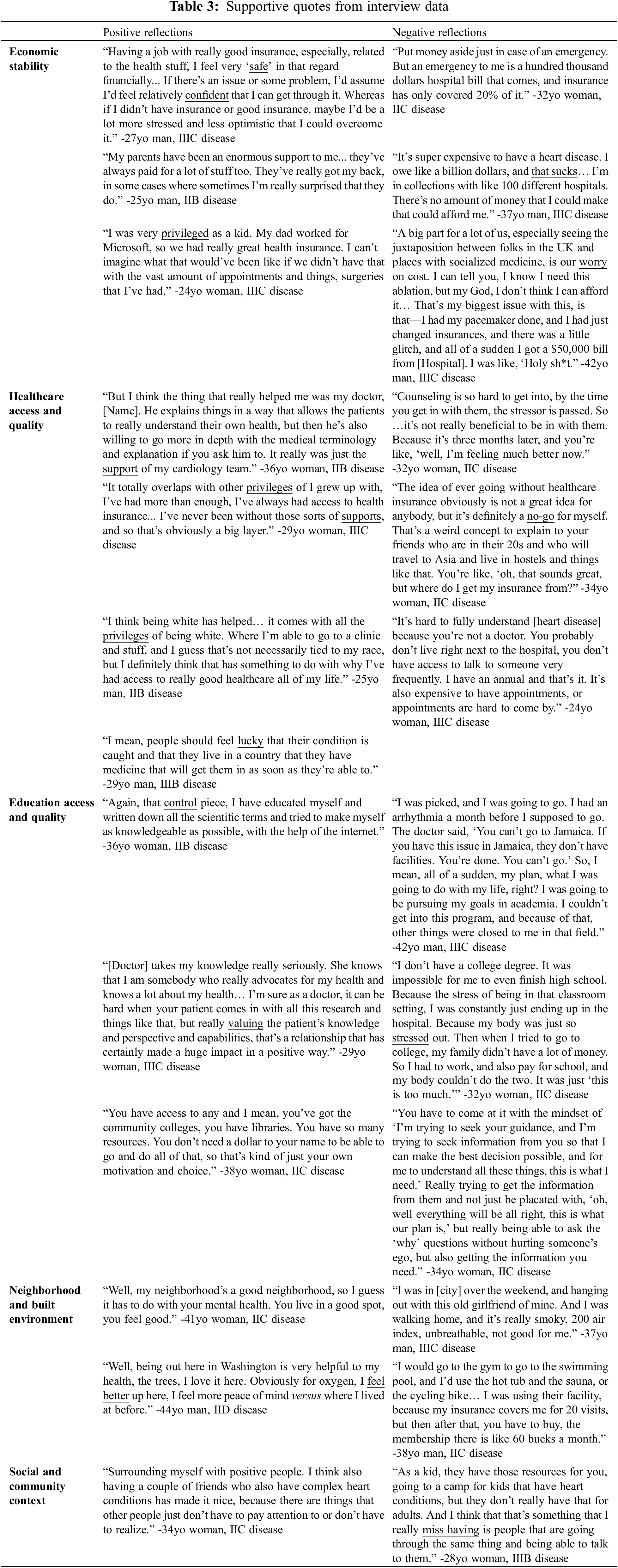
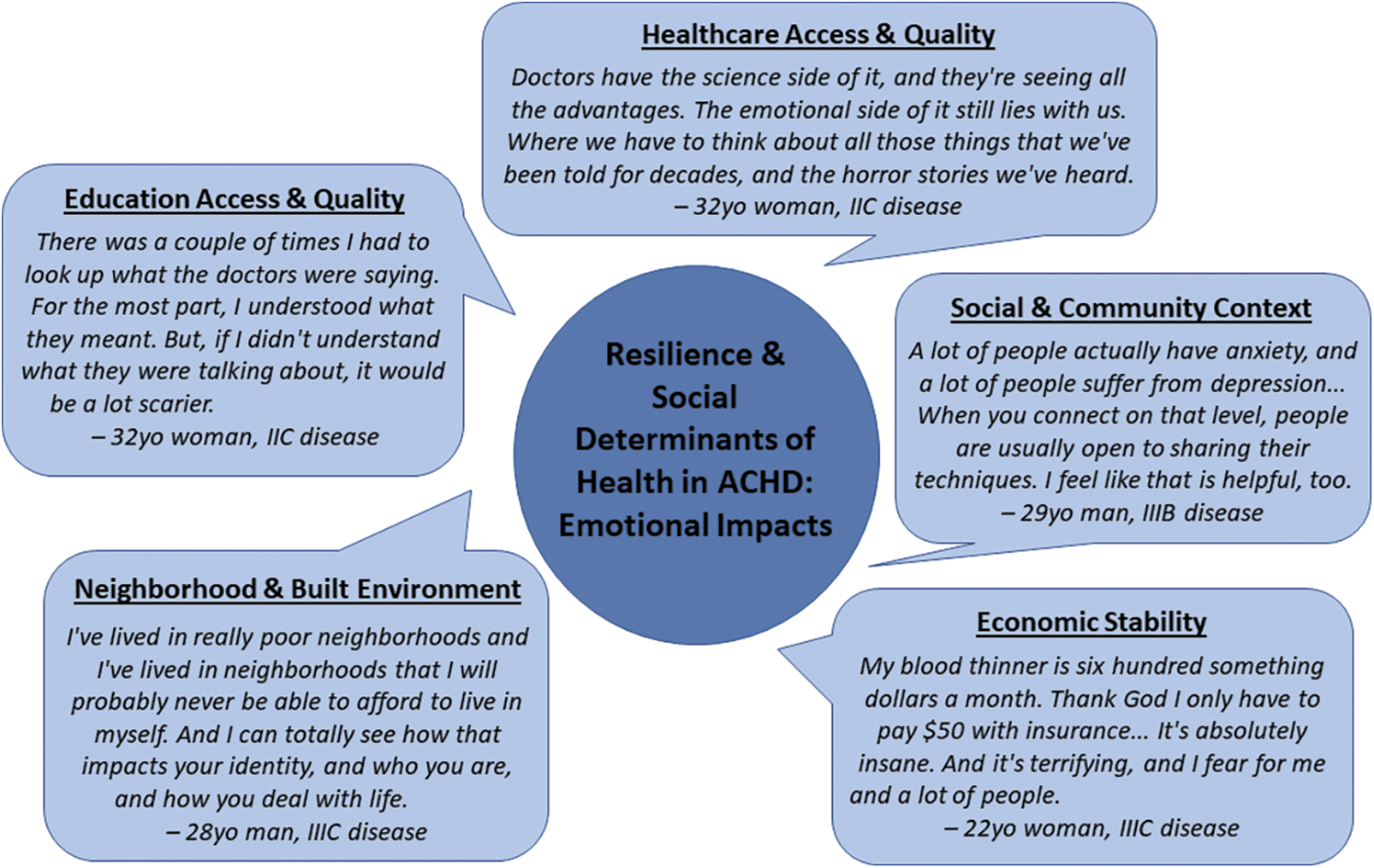
Figure 3: Resilience & social determinants of health in ACHD: Emotional impacts
The impact of ACHD on respondents’ assessment of Economic Stability was the most commonly referenced SDOH domain. Usually, this was mentioned when discussing the importance of maintaining health insurance. Participants reported that medical debt could be devastating to their mental health and ability to feel resilient in addition to financially. “The second I get kicked off my parents’ insurance, I’m not going to be okay. That is a huge fear. It is a huge, huge fear because I see my medical bills… Not having insurance is not an option. If I did not have insurance, I would die.” -22yo woman, IIIC disease. Costs related to living a healthy lifestyle like eating healthy food and affording gym membership were referenced as additional barriers to participants feeling resilient and confident in managing their heart health. “When you go shopping in a store, the healthier foods are the more expensive, and when you’re on a budget or you don’t have enough, you kind of have to make your meal stretch.” -24yo woman, IIIC disease.
Healthcare Access and Quality was the second most commonly referenced SDOH domain and often related to Economic Stability because of healthcare costs. Participants reflected on the fact that they are able to access ACHD-specific care as patients of our program: “I have such a strong heart team at [Hospital] that I think that alleviates quite a lot of my stress.” -38yo woman, IIC disease. Having trusted providers was important in feeling able to effectively manage their ACHD, especially as discussions have changed as they got older or encountered new ACHD-related consequences. However, they also discussed this SDOH as it related to decisions on where to live, whether to travel, and which hospitals to go to in the event of an emergency, recognizing the limited availability of ACHD-specific medical, and even more rare, mental health care.
Participants additionally discussed Education Access and Quality—both in learning more about their heart disease and being limited in acquiring formal education by having ACHD. Being knowledgeable about their ACHD helped some participants feel in control of a largely uncontrollable situation, supporting their ability to feel resilient. Participants reported studying their ACHD either in school projects or independently to enhance their own understanding of their disease. This helped them know what to ask at appointments and comprehend test results and clinician recommendations. Participants mentioned appreciation for clinicians who engaged them in conversations about their ACHD and who valued their input. Additionally, several participants reported not being able to achieve their desired level or type of formal education because of their ACHD. For some, the physical, mental, or financial cost was too much on top of having to manage or make concessions to their ACHD. For others, having ACHD precluded them from participating in certain educational opportunities like sports or study abroad programs, making them feel less than and challenging their resilience.
Neighborhood and Built Environment and Social and Community Context were less prominently endorsed SDOH domains, but still present. Participants linked their well-being to living in places where they felt supported. Having the environmental and social resources necessary to effectively manage the physical and emotional impacts of their ACHD was expressed as crucial to their resilience. Air quality and access to hiking trails and exercise facilities were mentioned, as were the quality of local stores and school systems. Additionally important was the ability of their communities to nurture a sense of belonging. Often, this was mentioned in the context of feeling connected to other people with ACHD, through avenues like social media or advocacy foundations. Community support also extended to other groups and settings, like exercising with a group who had relatable trauma or another chronic illness. These relationships were characterized as offering validation, confidence, and encouragement, which helped participants feel able to engage in their own health.
Consideration of how the SDOH affects outcomes beyond morbidity and mortality in ACHD is a key factor in providing care recommendations that are realistic and aligned with patients’ life needs. In this study, we demonstrated a substantial interplay between resilience and SDOH with regard to how patients manage their ACHD. Note this is self-reported resilience, the ability of a person to feel resilient, which likely is influenced by more than one’s cardiac health. Economic Stability and Healthcare Access and Quality emerged as two of the major SDOH of concern for this population. Assessment using both quantitative and qualitative methods offered novel and complementary insights into these relationships.
In the context of exploring resilience as related to a lifelong illness like ACHD, the SDOH domain of Economic Stability may reflect the financial strain which often accompanies medical care in the US. Medical care is expensive, and ACHD can limit the ability to pursue employment of a certain type or compensation level [23,24]. Findings from this study suggest that financial hardship may compound ACHD-related stress and undermine a person’s sense of resilience, resulting in a lower score for self-reported resilience. A patient may be less likely to have an advanced imaging study, for example, if taking time off work translates to lower wages, or if the cost of the study means having to forego another purchase. The finding of lower resilience among people who reported “other” regarding whom they support financially may reflect similar hardship: although we cannot be certain, this may represent less secure relationships, such as supporting elderly parents or those who are unable to independently support themselves. This indication of additional impactful arrangements suggests a need for a future, deeper investigation into financial dependency to better understand its significance. Interestingly, however, concerns over economic stability were present in this study despite this group having relatively favorable ADI scores. ADI has been demonstrated to correlate with adverse cardiac events as well as healthcare utilization in ACHD [25].
Beyond wages, maintaining the ability to work in order to afford insurance can be an additional challenge to self-perceived resilience, particularly if ACHD limits a person’s physical or mental health or cognitive abilities [23]. This concern reflects the SDOH of Healthcare Access and Quality. Interestingly, although the majority of participants in this study had health insurance and all were established at a large ACHD center, many still reported in interviews their concerns about inadequate coverage and fear of losing their insurance. Often, having insurance is not enough—rather, it is having the “right” type or level of insurance which will cover recommended care and be accepted at centers where high-quality ACHD care can be provided [7].
The scarcity of comprehensive ACHD care is an additional barrier to Healthcare Access and Quality. There are not enough ACHD providers or programs compared to patients needing services, and those that exist are disproportionately in urban areas [26]—which often come with a higher cost of living. Salciccioli and colleagues demonstrated that almost half of patients live more than one hour from ACHD care, and that these were patients disproportionately more likely to live below the federal poverty level and lack health insurance [27]. For such patients, the cost of travel to care in terms of money and time is an additional stressor which could impact a person’s ability to feel resilient.
Up to 40% of people with ACHD are estimated to have a gap in care, either at the time of pediatric transition or as adults [28]. Although for some this is related to inaccurate knowledge about the need for lifelong care, more often it is related to inequitable access to specialized ACHD care, either based on affordability or location. Poor physical health outcomes are associated with inequitable care access, as are mental health outcomes [7]. Resilience is not necessarily equitable either [29]. Taken together, one’s capacity to build and utilize resilience may be severely affected by these SDOH. For example, in the qualitative study which contributed to these data [20], interview participants with private insurance and higher levels of education had more often heard of resilience and able to provide their own definitions of it. As demonstrated here, it could be that people who are less socially or financially secure have not had the chance to reflect upon or consolidate their resilience, if they are constantly living in high-stress mode. Yet that does not mean they are not resilient, only their ability to report feeling resilient when asked.
As awareness grows regarding the associations between SDOH and ACHD physical and mental health outcomes, as well as resilience, action resulting in change is imperative [7]. Comprehensive neurodevelopmental evaluation in childhood could help identify social support needs early in life. Sponsorship at the policy level could result in expanded insurance coverage and job training to promote financial stability. Asking about SDOH needs during clinical encounters, ensuring robust mental health care is integrated into ACHD clinics, and the continued expansion of ACHD care to underserved areas could further ease SDOH-related burdens and improve health equity. Such changes would undoubtedly help patients manage stressors impacted by their ACHD, and would likely strengthen their ability to build resilience and use it to thrive. Additionally, rigorously-designed resilience-building interventions [30], which account for impactful SDOH concerns, can also be applied in ACHD.
Key limitations of this study should be considered. Primarily, these findings are constrained by the boundaries of the original datasets, the goals of which were not specifically to evaluate SDOH. However, SDOH was a consideration when creating both the survey and interview guide. A dedicated study investigating specific SDOH could provide additional depth or different findings. Second, the quantitative and qualitative methods used here complement each other, providing a more comprehensive assessment of the 5 major SDOH than either study alone. However, each has limitations: statistical associations between predictors and outcomes may not be causal, and unmeasured variables or small numbers in groups may influence these relationships. Qualitative research explores the breadth and depth of experiences, providing perspective beyond the capabilities of a survey though not necessarily fully representative of a population. Despite efforts to include diverse perspectives, participants in both studies were predominantly non-Hispanic White, highly educated, privately insured, and received care at a large subspecialty ACHD center in the Pacific Northwest United States. People who live in other regions, belong to different demographic groups, or who do not have access to subspecialty care may experience differential relationships between resilience and SDOH. Additionally, it was necessary to combine some demographic groups for statistical analysis, which limits representation and may mask certain associations. However, the quantitative findings of this study were not different between unadjusted and adjusted analyses, suggesting a nonsignificant impact in this instance.
In conclusion, SDOH is associated with self-reported resilience in ACHD, in particular those reflecting financial concerns such as Economic Stability and Healthcare Access and Quality. Knowledge of these relationships can inform the development of tailored resilience interventions for this population.
Acknowledgement: Erin Abu-Rish Blakeney, PhD, RN; Vea Freeman; Crystal Brown, MD, MS; J. Randall Curtis, MD, MPH for their contributions to this study. REDCap is supported by the UW Institute of Translational Health Sciences, funded by UL1TR002319, National Center for Advancing Translational Sciences, National Institutes of Health.
Funding Statement: This study is supported by K23HL15180 (NIH/NHLBI, Steiner) and a grant from the American College of Cardiology Foundation.
Author Contributions: Osom: formal analysis, visualization, writing-original draft, writing-review & editing. Barton: methodology, formal analysis, visualization, writing-original draft, writing-review & editing. Sexton: formal analysis, writing-review & editing. Brumback: methodology, writing-review & editing, supervision. Yi-Frazier: writing-review & editing, supervision. Rosenberg: writing-review & editing, supervision. Engelberg: writing-review & editing, supervision. Steiner: conceptualization, data curation, formal analysis, funding acquisition, supervision, visualization, writing-original draft, writing-review & editing.
Availability of Data and Materials: Available upon request.
Ethics Approval: All participants provided informed consent and permission for medical record access. Both studies were approved by the University of Washington Institutional Review Board.
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
References
1. Steiner JM, Kovacs AH. Adults with congenital heart disease—facing morbidities and uncertain early mortality. Prog Pediatr Cardiol. 2018;48(9):75–81. doi:10.1016/j.ppedcard.2018.01.006. [Google Scholar] [CrossRef]
2. Kovacs AH, Moons P. Psychosocial functioning and quality of life in adults with congenital heart disease and heart failure. Heart Fail Clin. 2014;10(1):35–42. [Google Scholar] [PubMed]
3. Kovacs AH, Landzberg MJ, Goodlin SJ. Advance care planning and end-of-life management of adult patients with congenital heart disease. World J Pediatr Congenit Heart Surg. 2013;4(1):62–9. doi:10.1177/2150135112464235. [Google Scholar] [PubMed] [CrossRef]
4. Department of Health and Human Services. Healthy people 2030: social determinants of health. 2021. Available from: https://health.gov/healthypeople/objectives-and-data/social-determinants-health (accessed on 14/12/2018). [Google Scholar]
5. Singh GK, Daus GP, Allender M, Ramey CT, Martin EK, Perry C, et al. Social determinants of health in the United States: addressing major health inequality trends for the nation, 1935–2016. Int J Matern Child Health. 2018;6(2):139–64. [Google Scholar]
6. Braveman P, Egerter S, Williams DR. The social determinants of health: coming of age. Annu Rev Public Health. 2011;32:381–98. [Google Scholar] [PubMed]
7. Lopez KN, Baker-Smith C, Flores G, Gurvitz M, Karamlou T, Gallegos FN, et al. Addressing social determinants of health and mitigating health disparities across the lifespan in congenital heart disease: a scientific statement from the American Heart Association. J Am Heart Assoc. 2022;11(8):1–21. [Google Scholar]
8. Luthar SS, Cicchetti D, Becker B. The construct of resilience: a critical evaluation and guidelines for future work. Child Dev. 2000;71(3):543–62. doi:10.1111/1467-8624.00164. [Google Scholar] [PubMed] [CrossRef]
9. Rosenberg AR, Bradford MC, McCauley E, Curtis JR, Wolfe J, Scot Baker K, et al. Promoting resilience in adolescents and young adults with cancer: results from the PRISM randomized controlled trial. Cancer. 2018;124(19):3909–17. [Google Scholar] [PubMed]
10. Steinhardt M, Dolbier C. Evaluation of a resilience intervention to enhance coping strategies and protective factors and decrease symptomatology. J Am Coll Health. 2008;56(4):445–53. [Google Scholar] [PubMed]
11. Lee S, Kim S, Young Choi J. Coping and resilience of adolescents with congenital heart disease. J Cardiovasc Nurs. 2014;29(4):340–6. [Google Scholar] [PubMed]
12. Ring A, Ring A, Ring GA, Marson A, Whitehead MM. Does the concept of resilience contribute to understanding good quality of life in the context of epilepsy? Epilepsy Behav. 2016;56:153–64. [Google Scholar] [PubMed]
13. Rosenberg AR, Syrjala KL, Martin PJ, Flowers ME, Carpenter PA, Salit RB, et al. Resilience, health, and quality of life among long-term survivors of hematopoietic cell transplantation. Cancer. 2015;121(23):4250–7. [Google Scholar] [PubMed]
14. McGrath LB, Kovacs AH. Psychological resilience: significance for pediatric and adult congenital cardiology. Prog Pediatr Cardiol. 2019;54:101129. [Google Scholar]
15. Steiner JM, Nassans K, Brumback LC, Stout KK, Longenecker CT. Key psychosocial health outcomes and association with resilience among patients with adult congenital heart disease. J Am Coll Cardiol: Adv. 2023. (In Press). [Google Scholar]
16. Stout KK, Daniels CJ, Aboulhosn JA, Bozkurt B, Broberg CS, Colman JM, et al. AHA/ACC guideline for the management of adults with congenital heart disease. J Am Coll Cardiol. 2018;139(12):e698–800. doi:10.1016/j.jacc.2018.08.1029. [Google Scholar] [PubMed] [CrossRef]
17. University of Wisconsin School of Medicine and Public Health. Area deprivation index. 2020. Available from: https://www.neighborhoodatlas.medicine.wisc.edu/ (accessed on 14/12/2018). [Google Scholar]
18. The Connor-Davidson Resilience Scale (CD-RISCHome. Available from: http://www.connordavidson-resiliencescale.com/ (accessed on 28/04/2019). [Google Scholar]
19. Connor KM, Davidson JRT. Development of a new resilience scale: the Connor-Davidson Resilience Scale (CD-RISC). Depress Anxiety. 2003;18(2):76–82. [Google Scholar] [PubMed]
20. Steiner JM, Abu-Rish Blakeney E, Baden AC, Freeman V, Yi-Frazier J, Curtis JR, et al. Definitions of resilience and resilience resource use as described by adults with congenital heart disease. International Journal of Cardiology Congenital Heart Disease. 2023;12(14):100447. doi:10.1016/j.ijcchd.2023.100447. [Google Scholar] [PubMed] [CrossRef]
21. Palinkas LA, Horwitz SM, Green CA, Wisdom JP, Duan N, Hoagwood K. Purposeful sampling for qualitative data collection and analysis in mixed method implementation research. Adm Policy Ment Hlth. 2015;42(5):533–44. [Google Scholar]
22. Braun V, Clarke V. Thematic analysis. In: APA Handbook of Research Methods in Psychology, Vol 2: Research Designs: Quantitative, Qualitative, Neuropsychological, and Biological. Washington DC, USA: American Psychological Association; 2012. p. 57–71. [Google Scholar]
23. Ladoucer M, Iserin L, Cohen S, Boujemline A, Boujemline Y, Bonnet D. Key issues of daily life in adults with congenital heart disease. Arch Cardiovasc Dis. 2013;106:404–12. [Google Scholar] [PubMed]
24. Steiner JM, Dhami A, Brown CE, Stout KK, Curtis JR, Engelberg RA, et al. It’s part of who I am: the impact of congenital heart disease on adult identity and life experience. Int J Cardiol Hypertens Congenital Heart Disease. 2021;4:100146. doi:10.1016/j.ijcchd.2021.100146. [Google Scholar] [CrossRef]
25. Tillman AR, Colborn KL, Scott KA, Davidson AJ, Khanna A, Kao D, et al. Associations between socioeconomic context and congenital heart disease related outcomes in adolescents and adults. Am J Cardiol. 2021;139:105–15. doi:10.1016/j.amjcard.2020.10.040. [Google Scholar] [PubMed] [CrossRef]
26. Congenital Heart Association: Clinic directory. 2023. Available from: https://www.achaheart.org/your-heart/resources/clinic-directory/ (accessed on 30/06/2023). [Google Scholar]
27. Salciccioli KB, Oluyomi A, Lupo PJ, Ermis PR, Lopez KN. A model for geographic and sociodemographic access to care disparities for adults with congenital heart disease. Congenit Heart Dis. 2019;14(5):752–9. doi:10.1111/chd.12819. [Google Scholar] [PubMed] [CrossRef]
28. Gurvitz M, Valente AM, Broberg C, Cook S, Stout K, Kay J, et al. Prevalence and predictors of gaps in care among adult congenital heart disease patients: HEART-ACHD (The Health, Education, and Access Research Trial). J Am Coll Cardiol. 2013;61(21):2180–4. [Google Scholar] [PubMed]
29. Rosenberg AR, Brown CE, Rosa WE, Yi-Frazier JP. When resilience is cliche and resilience resources are taboo: how language and policies exacerbate mental health disparities. Lancet Child and Adolescent Health. 2023;7(4):236–7. doi:10.1016/S2352-4642(23)00005-6. [Google Scholar] [PubMed] [CrossRef]
30. Helmreich I, Kunzler A, Chmitorz A, König J, Binder H, Wessa M, et al. Psychological interventions for resilience enhancement in adults. Cochrane Database Syst Rev. 2017;2017(2):CD012527. [Google Scholar]
Cite This Article
 Copyright © 2024 The Author(s). Published by Tech Science Press.
Copyright © 2024 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools