 Open Access
Open Access
ARTICLE
Impact of Social Determinants of Health on Self-Perceived Resilience: An Exploratory Study of Two Cohorts of Adults with Congenital Heart Disease
1 Department of Biostatistics, University of Washington, Seattle, WA, 98195, USA
2 Biostatistics Epidemiology and Analytics for Research (BEAR) Core, Seattle Children’s Research Institute, Seattle, WA, 98101, USA
3 College of Medicine, University of Washington, Seattle, WA, 98195, USA
4 Center for Clinical and Translational Research, Seattle Children’s Research Institute, Seattle, WA, 98101, USA
5 Department of Psychosocial Oncology and Palliative Care, Dana-Farber Cancer Institute; Department of Medicine, Boston Children’s Hospital, Boston, MA, 02215, USA
6 Department of Pediatrics, Harvard Medical School, Boston, MA, 02215, USA
7 Division of Pulmonary, Critical Care and Sleep Medicine, Department of Medicine & Cambia Palliative Care Center of Excellence, University of Washington, Harborview Medical Center, Seattle, WA, 98104, USA
8 Division of Cardiology, Department of Medicine & Cambia Palliative Care Center of Excellence, University of Washington, Seattle, WA, 98195, USA
* Corresponding Author: Jill M. Steiner. Email:
Congenital Heart Disease 2024, 19(1), 33-48. https://doi.org/10.32604/chd.2024.046656
Received 10 October 2023; Accepted 05 January 2024; Issue published 20 March 2024
Abstract
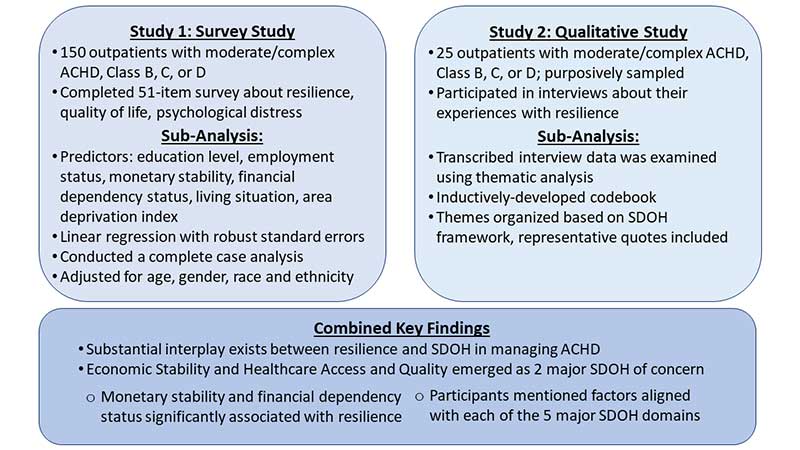
Social determinants of health (SDOH) affect quality of life. We investigated SDOH impacts on self-perceived resilience among people with adult congenital heart disease (ACHD). Secondary analysis of data from two complementary studies: a survey study conducted May 2021–June 2022 and a qualitative study conducted June 2020–August 2021. Resilience was assessed through CD-RISC10 score (range 0–40, higher scores reflect greater self-perceived resilience) and interview responses. Sociodemographic and SDOH (education, employment, living situation, monetary stability, financial dependency, area deprivation index) data were collected by healthcare record review and self-report. We used linear regression with robust standard errors to analyze survey data and performed a thematic analysis of interview data. Survey participants (N = 127) mean age was 42 ± 14 years; 51% were female, 87% white. ACHD was moderate (75%) or complex (25%); 41% functional class C or D. Resilience (mean 30 ± 7) varied by monetary stability: compared to people with difficulty paying bills, resilience was 15.0 points higher (95% CI: 6.9–23.1, p < 0.001) for people reporting having enough money and 14.2 points higher (95% CI: 5.9–22.4, p = 0.001) for those reporting just enough money. Interview participants’ (N = 25) mean age was 32 years (range 22–44); 52% were female, 72% white. ACHD was moderate (56%) or complex (44%); 76% functional class C or D. Participants discussed factors affecting resilience aligned with each of the major SDOH, prominently, economic stability and healthcare access and quality. Financial stability may be important for supporting self-perceived resilience in ACHD. This knowledge can inform the development of resilience interventions for this population.Graphic Abstract
Keywords
Cite This Article
 Copyright © 2024 The Author(s). Published by Tech Science Press.
Copyright © 2024 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools