 Open Access
Open Access
ARTICLE
Use of Patient-Specific “4D” Tele-Education to Enhance Actual and Perceived Knowledge in Congenital Heart Disease (CHD) Patients
1 Department of Inpatient Cardiology, Boston Children’s Hospital, Boston, 02115, USA
2 Department of Cardiology, Children’s National Hospital, Washington, 20001, USA
3 Department of Cardiology, Noninvasive Cardiac Imaging, University of Pittsburgh Medical Center Children’s Hospital of Pittsburgh, Pittsburgh, 15224, USA
* Corresponding Author: Molly Clarke. Email:
Congenital Heart Disease 2024, 19(1), 5-17. https://doi.org/10.32604/chd.2024.046328
Received 27 September 2023; Accepted 09 January 2024; Issue published 20 March 2024
Abstract
Background: Patients with congenital heart disease (CHD) will transition to lifelong adult congenital cardiac care. However, their structural heart disease is challenging to convey via two-dimensional drawings. This study utilized a tele-educational environment, with personalized three-dimensional (3D) modeling and health Details (3D + Details = “4D”), to improve actual and perceived knowledge, both important components of transition readiness in CHD patients. Methods: Participants aged ≥13 years with a history of CHD and cardiac magnetic resonance imaging (MRI) studies were eligible. Cardiac MRI datasets were then used to segment and create 3D heart models (using Mimics, Materialize Inc.). Participants first completed the MyHeart Questionnaire, a validated survey of actual knowledge. A tele-educational session was then scheduled, during which participants were shown a 3D model of a normal heart, followed by their personal 3D heart model and specific health details. Participants then repeated the actual knowledge survey, in addition to questionnaires assessing perceived knowledge pre- and post-session, as well as a satisfaction survey. Results: Twenty-two patients were included. Actual knowledge increased from 75% ± 15% to 89% ± 20% (p = 0.00043) and perceived knowledge increased in five of seven questions. Actual knowledge correlated with perceived knowledge (r = 0.608, p < 0.0001). Ninety-one percent of participants ranked the 3D model as “very satisfactory” and ninety-five percent ranked the educational session as “very helpful” or “extremely helpful.” Conclusions: The use of “4D” tele-education increased both actual and perceived knowledge and may help improve transition readiness in CHD patients.Keywords
Supplementary Material
Supplementary Material FileNomenclature
| CHD | Congenital Heart Disease |
| ACHD | Adult Congenital Heart Disease |
Pediatric patients with congenital heart disease (CHD) must transition to lifelong adult congenital cardiac care [1]. With more CHD patients surviving into adulthood [2], approximately 50% do not successfully transition to adult CHD (ACHD) care [3,4], which has a significant impact on long term mortality and morbidity. The most common reasons for failure include a general lack of overt symptoms and/or unclear guidance on reasons for long-term follow-up [4]. One key aspect to CHD transition readiness is a patients’ knowledge of their heart disease, including a basic understanding of the cardiac anatomy and prior surgical interventions. Increased medical condition knowledge correlates with greater transition readiness [5,6], and other studies have addressed educational programs on knowledge and transition readiness as a whole [7–9].
Educational sessions utilizing patient-specific three-dimensional (3D) models offer the potential to enhance the overall educational experience for CHD patients. Traditionally, cardiologists have utilized two-dimensional (2D) imaging in the form of diagrams or still-frame images, which only partially present the cardiac anatomy. However, 2D imaging does not fully capture the unique anatomy for each individual, even for those with the same CHD diagnosis. Patient-specific 3D models have been used to enhance communication between providers and parents [10]. Our group and others have shown its efficacy for medical trainees [11,12] and patients [13]. Other strategies include educational sessions with individualized health professional-led didactics, videos, video games, and/or the use of ACHD “passports” [7–9,14,15] to succinctly summarize a patient’s cardiac medical history, key vital signs, and diagnostics; however, these did not include 3D models. How a virtual 3D model and patient-specific health details can impact transition readiness has not been fully explored.
This study aims to expand the scope of these models to include adults with CHD and focus on specific metrics that correlate with transition readiness. We uniquely combined the use of both 3D modeling and ACHD “passports” to deliver one-on-one educational sessions for CHD/ACHD patients. We called these sessions “4D” given they included 3D modeling and health Details (3D + Details = “4D”). We aim to investigate the feasibility of this strategy for improving patient knowledge and transitional readiness.
We aim to evaluate whether education with 3D cardiac imaging models improves patients’ (adolescents and adults) understanding of their specific heart disease as measured by actual and perceived knowledge; to determine the relationship between actual knowledge and perceived knowledge; and to describe patient satisfaction with the use of digital 3D cardiac models as an educational tool.
Participants aged 13 years old or older with a history of CHD who have had previous cardiac magnetic resonance imaging (MRI) were eligible for enrollment. Ethical approval was granted by the Children’s National Hospital Institutional Review Board (IRB). All patients were consented at Children’s National Hospital, which services all CHD patients in the Washington, DC area with approximately twenty thousand outpatient cardiology visits, five hundred cardiovascular surgical cases, and five hundred cardiac MRI studies on an annual basis. Children’s National also has a dedicated ACHD program and services the majority of ACHD patients in the Washington DC area. Study participants were identified and consented by a nurse, either in the pediatric cardiology outpatient clinic or in an outpatient radiology suite prior to the patient’s clinically-indicated MRI. In some patients with significant stent artifact on MRI, previous computed tomography data was used to supplement the 3D modeling process. All complexities of CHD were included. Select comorbidities including severe developmental delay and select genetic syndromes with intellectual impairment were considered exclusion criteria. Only English-speaking patients and those with reliable internet connections to attend remote appointments were included.
As part of an IRB-approved study, participants were recruited through review of electronic health records or during routinely scheduled surveillance MRI studies. After consent, the coordinator scheduled a tele-education session with the patient and/or parent. A total of thirty-four patients consented for the study. Five were consented in cardiology clinic, three of whom completed the educational session. Twenty-nine were consented in the radiology suite, nineteen of whom completed the educational session. There were twelve participants who dropped out from the study (Fig. 1).
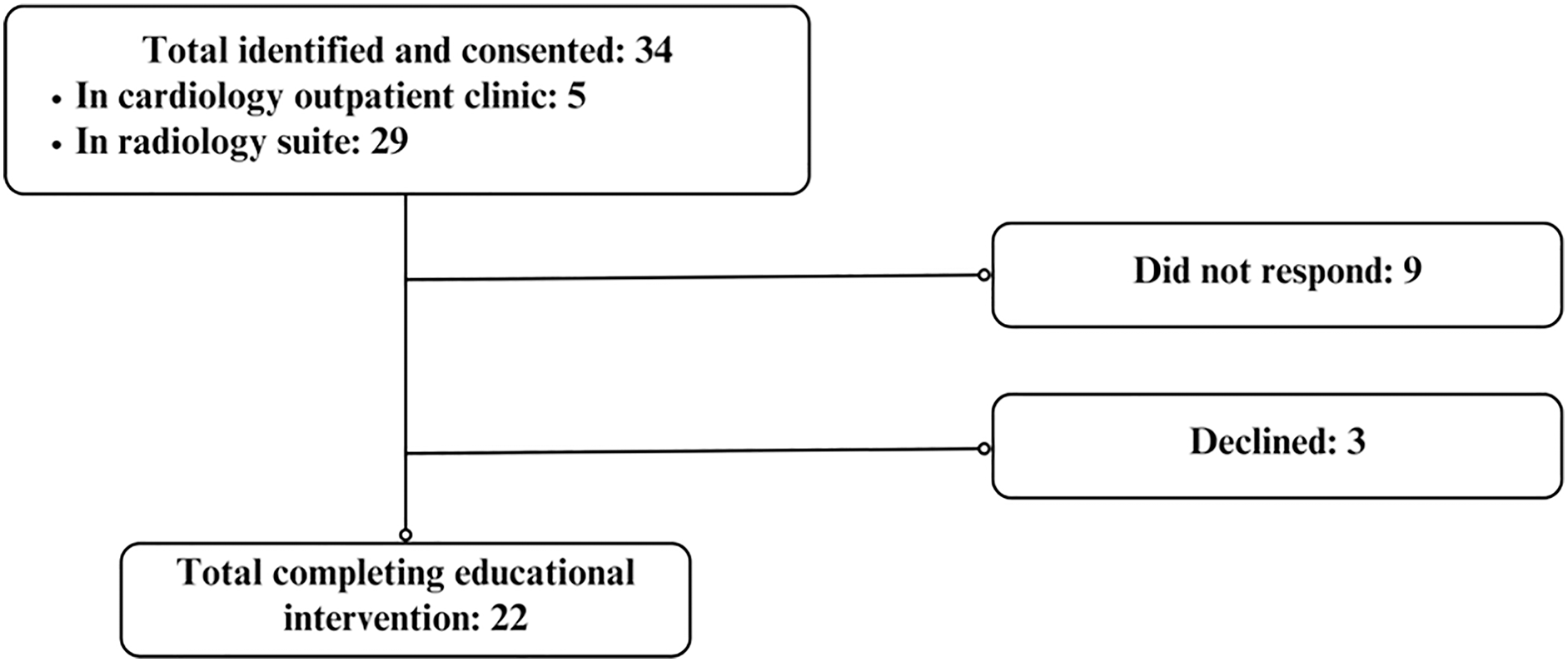
Figure 1: Recruitment flow chart
The 3D datasets were imported into Mimics (Materialise Inc.; Leuven, Belgium) and the relevant intracardiac anatomy was segmented. The segmented imaging dataset was then exported into a stereolithography (STL) file.
The study coordinator and participant together completed the “4D” Passport that included important patient-specific CHD information (e.g., name of CHD, medications, allergies, need for subacute bacterial endocarditis prophylaxis, resting heart rate, most recent electrocardiogram) in addition to the 3D model.
2.4 Pre-Intervention Questionnaire
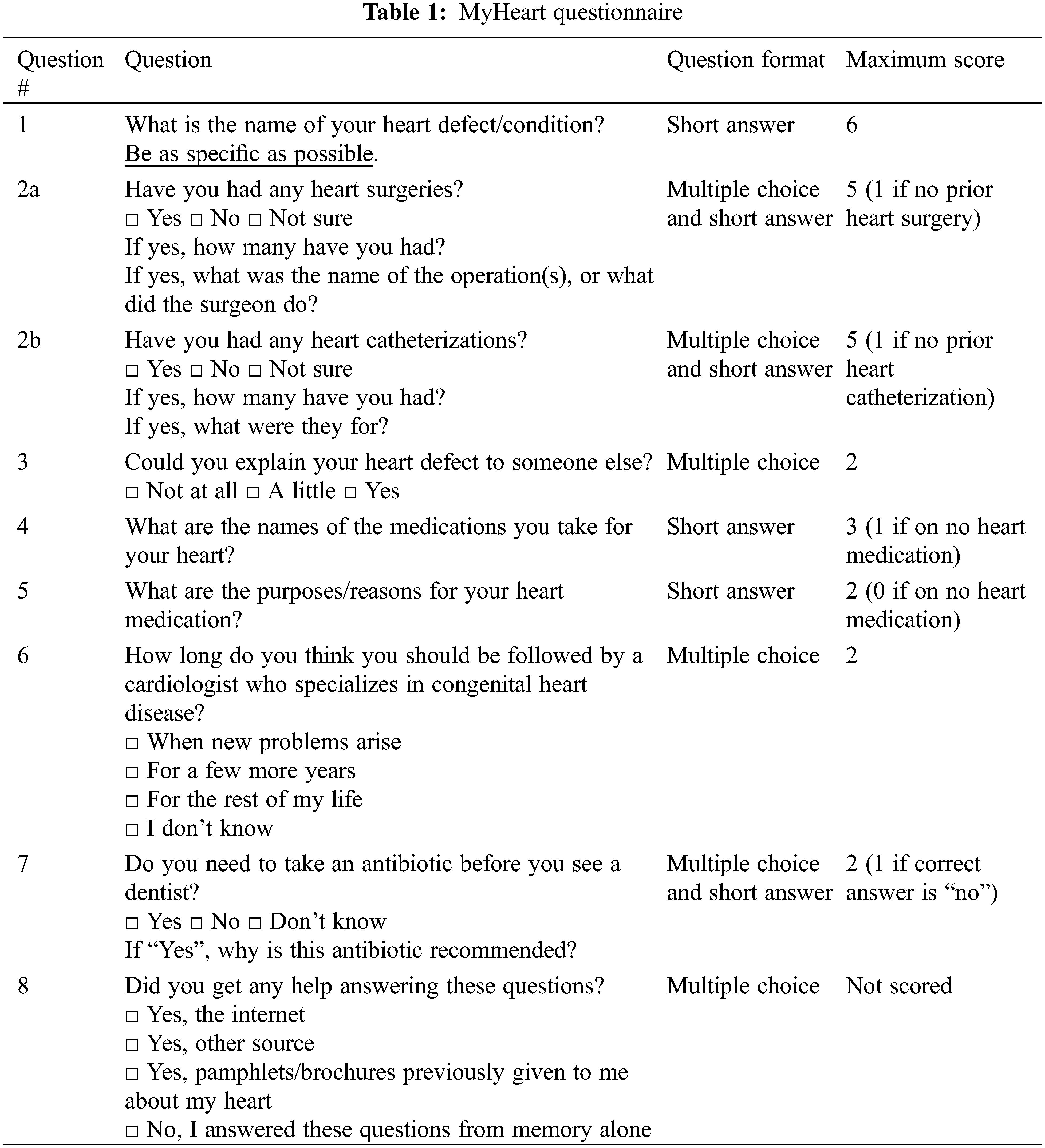
Participants were first asked to complete a survey assessing actual knowledge; in this study, actual knowledge is defined by the MyHeart questionnaire. This is a validated questionnaire that has been applied by Mackie et al. [8,9] and Stewart et al. [5] to assess patient medical condition knowledge. The MyHeart questionnaire was chosen as it was developed solely for the CHD population, and it also tests the level of specific disease knowledge in domains that our intervention aims to improve. The content of the MyHeart scale is described in Table 1. Question 4 was the only question that was modified; we did not test for the dose of the medication(s).
Educational sessions with participants occurred using teleconferencing via Zoom (Zoom Video Communications; San Jose, CA). An educational curriculum similar to one used in a previous study was applied [13]. The same pediatric cardiologist completed the curriculum with the study subjects, first focusing on normal intracardiac anatomy, then transitioning to the learner’s specific anatomy, and key points (Supplement 1). All of this was discussed with language in concordance with participants’ level of understanding. Fig. 2 depicts the software that is used to display the model, Cardiac Review 3D (Indicated Inc.). The customized 3D software allows for transparency of individual models and can also clip through the heart for viewing of anatomic relations in different planes. No clinical recommendations were made during the education session. Questions and active participation were encouraged during this discussion; however, those related to clinical management were deferred to the primary cardiologist. Finally, patients participated in filling in important health details in the “4D” passport via a fact sheet including a digital copy of the 3D model. The “4D” passport summarized the information about the patient’s medical information and anatomy (Supplement 1).
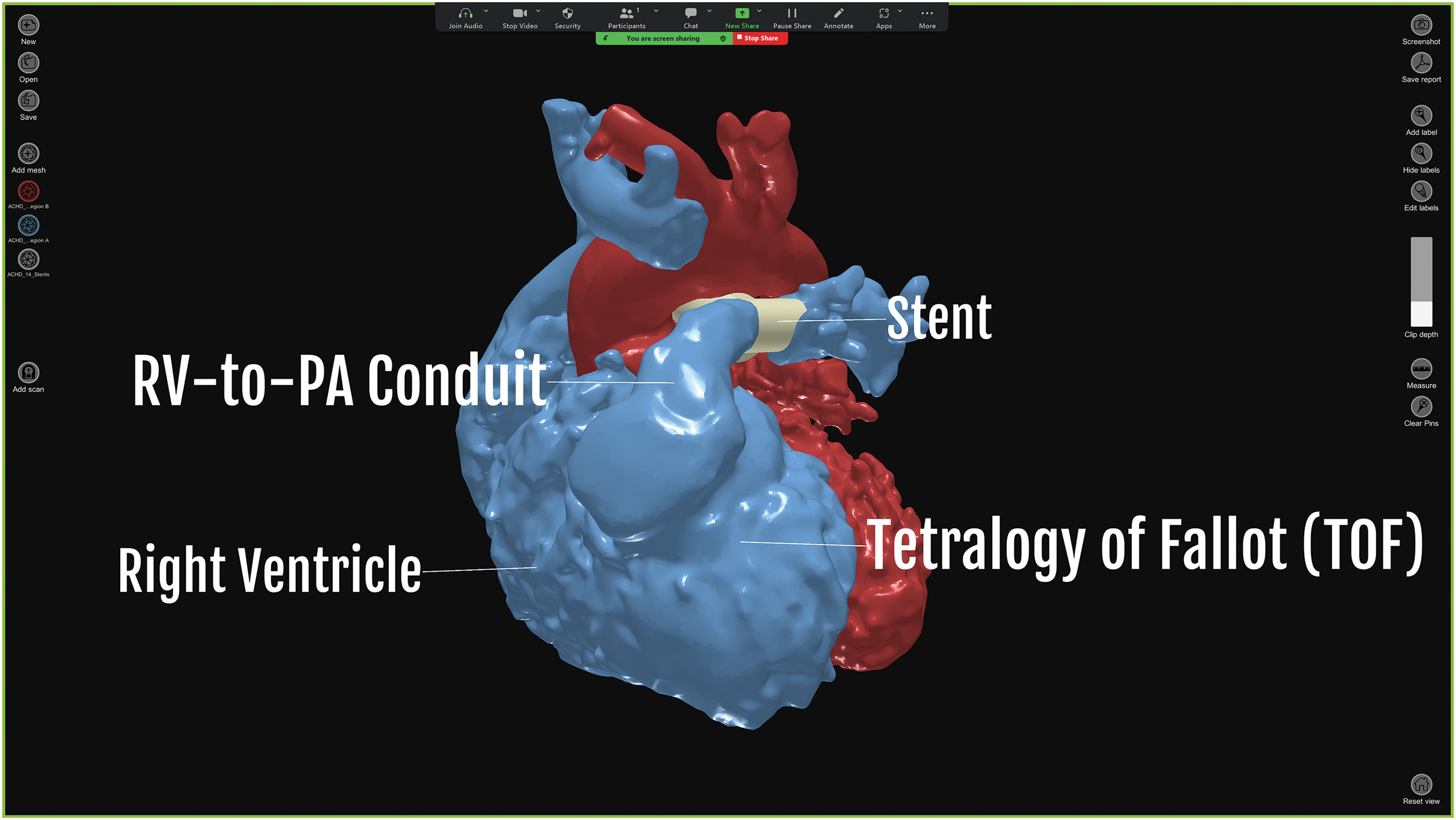
Figure 2: Software used for 3D display of CHD model via Zoom
2.6 Post-Intervention Questionnaires
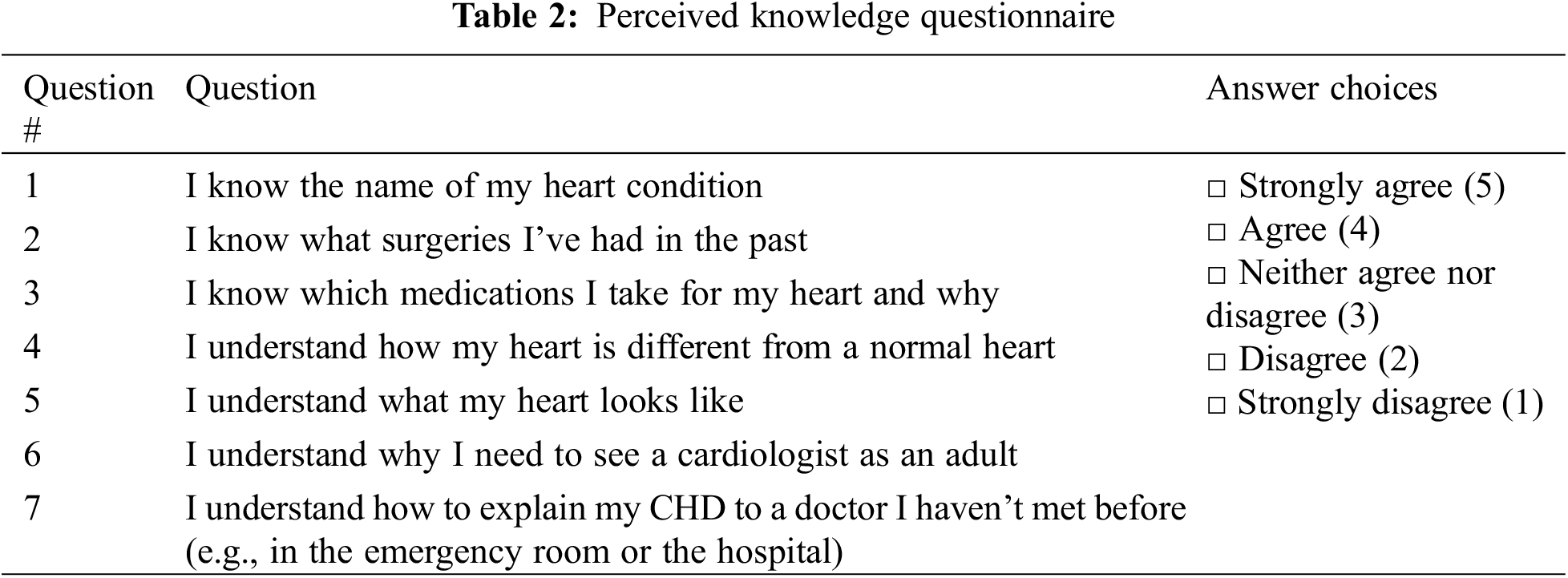
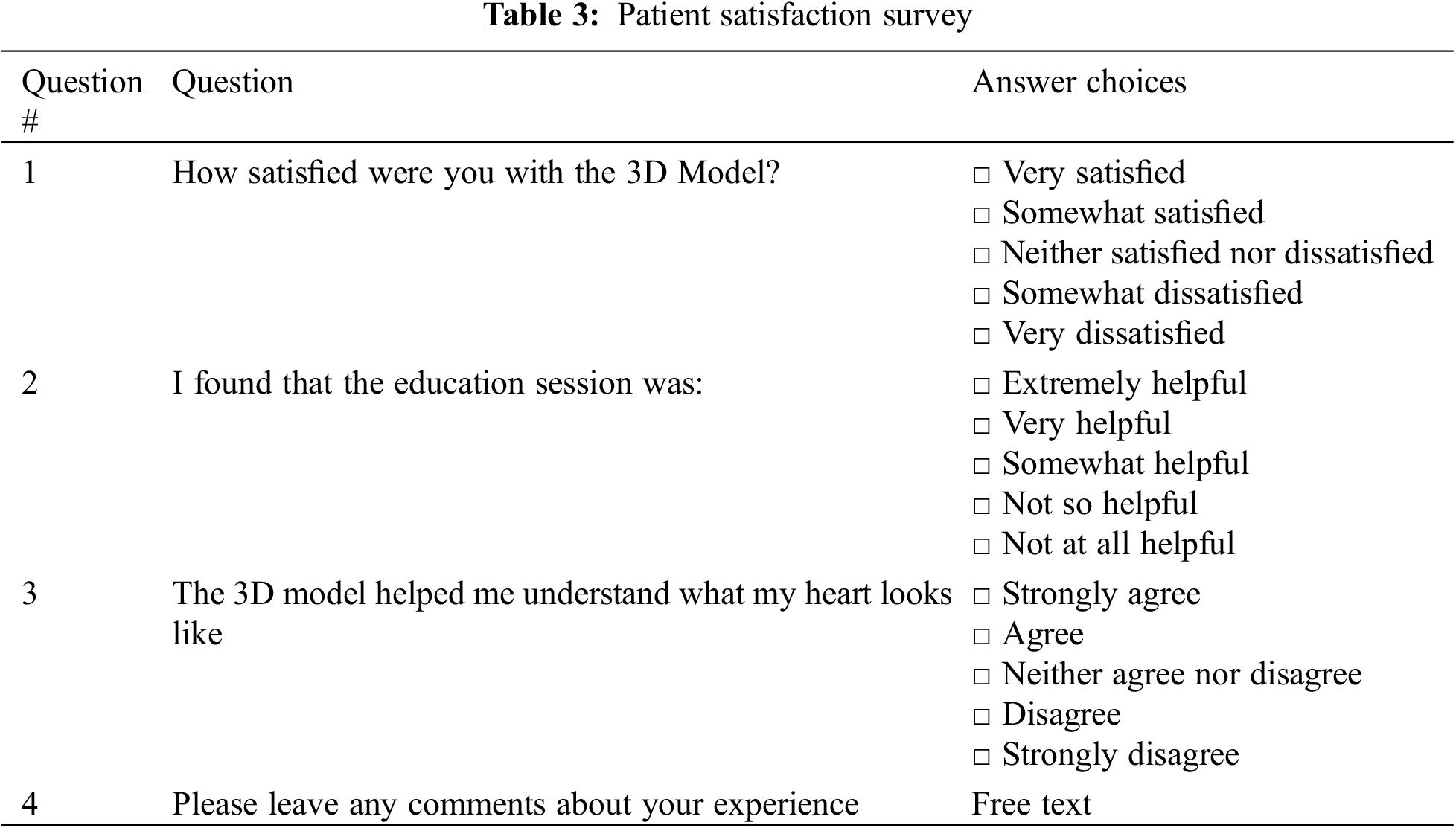
Immediately following the Zoom conference call, participants completed the same actual knowledge questionnaire. The patients then also completed pre- and post-perceived knowledge questionnaires (Table 2). These were administered together after the intervention to prevent recall bias. The questionnaire was based off Transition Tools developed by pediatric and adult congenital cardiologists [16]. Finally, participants completed a patient satisfaction survey (Table 3). Participants and parents were asked, via Likert scale, to rate the different tools that were used during the consultation. Patients were given the opportunity to provide free text comments.
After the session was finished and patients had completed their questionnaires, patients were provided with a video of their 3D model spinning 360°, a 3D portable document format (PDF) file of their model, and STL files of their 3D model that could be used for printing, if they so desired.
Actual knowledge was scored using the same method as Mackie et al. (Supplement 2). These tests were independently scored by two evaluators (MC, YHL) at least six months after the intervention to avoid observer bias.
Inter-rater reliability was assessed using intraclass correlation coefficient. These are rated as follows: 0.0–0.20 as none to slight, 0.21–0.40 as fair, 0.41–0.60 as moderate, 0.61–0.80 as substantial, and 0.81–1.00 as almost perfect agreement [17,18]. Wilcoxon signed rank test was used to determine whether significant differences existed between pre- and post-intervention actual knowledge scores. Pearson correlation coefficient was used to determine the relationship between perceived knowledge and actual knowledge. Multivariate analyses were also completed to determine potential influences on the primary outcome of actual knowledge improvement. Variables included age, gender, self-reported race, pre-test scores, and complexity of the CHD based on The Society of Thoracic Surgeons-European Association for Cardio-Thoracic Surgery (STAT) category [19] of their surgical history (separating the cohort into STAT category ≥3 and <3).
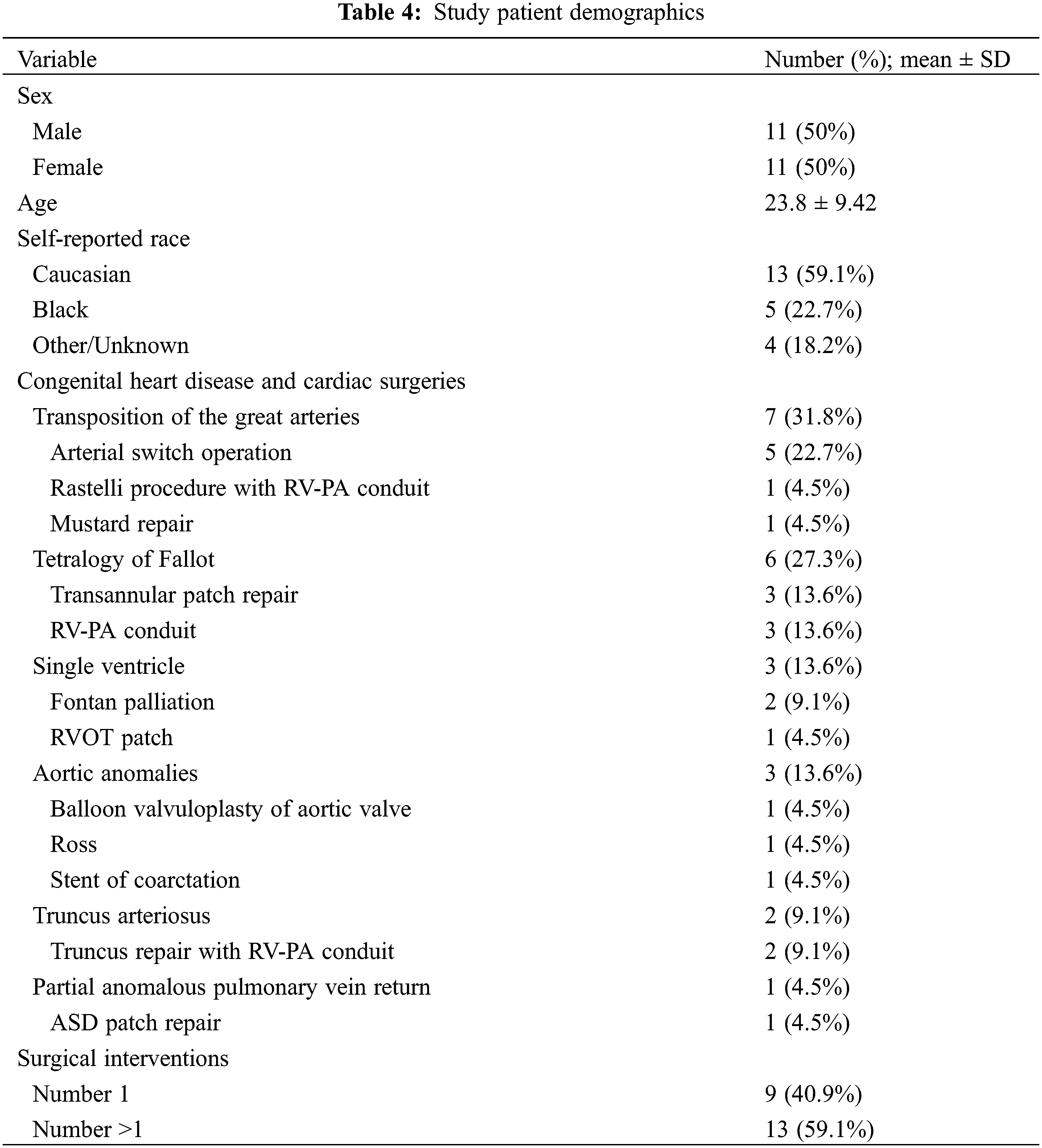
Twenty-two participants (50% female) completed the educational session and questionnaires. Their demographics are listed in Table 4. The average age was 24 with an inter quartile range of 15–28 years and a range of 13–42 years. The most common congenital heart disease types were Transposition of the Great Arteries and Tetralogy of Fallot.
3.2 Actual Knowledge, Perceived Knowledge, Satisfaction, and Qualitative Comments
Intraclass correlation coefficient was 0.89 (p < 0.0001). Actual knowledge increased from 75% ± 15% to 89% ± 20% (p = 0.00043). Perceived knowledge increased in five of seven questions. Actual knowledge correlated with perceived knowledge (r = 0.608, p < 0.0001). Ninety-one percent of patients ranked the 3D model as “very satisfactory;” ninety-five percent ranked the educational session as “very helpful” or “extremely helpful.” Questionnaire results are summarized in Table 5.
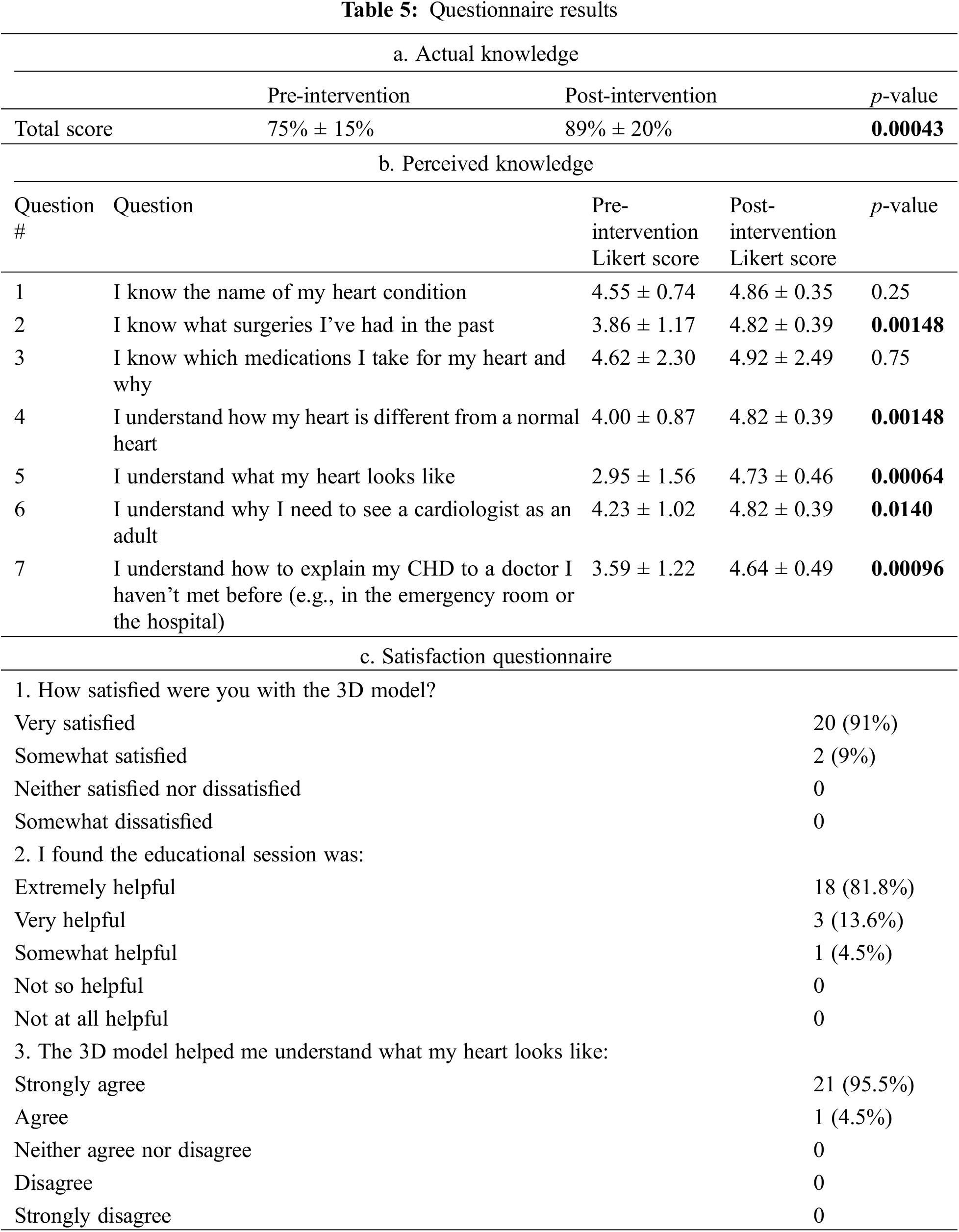
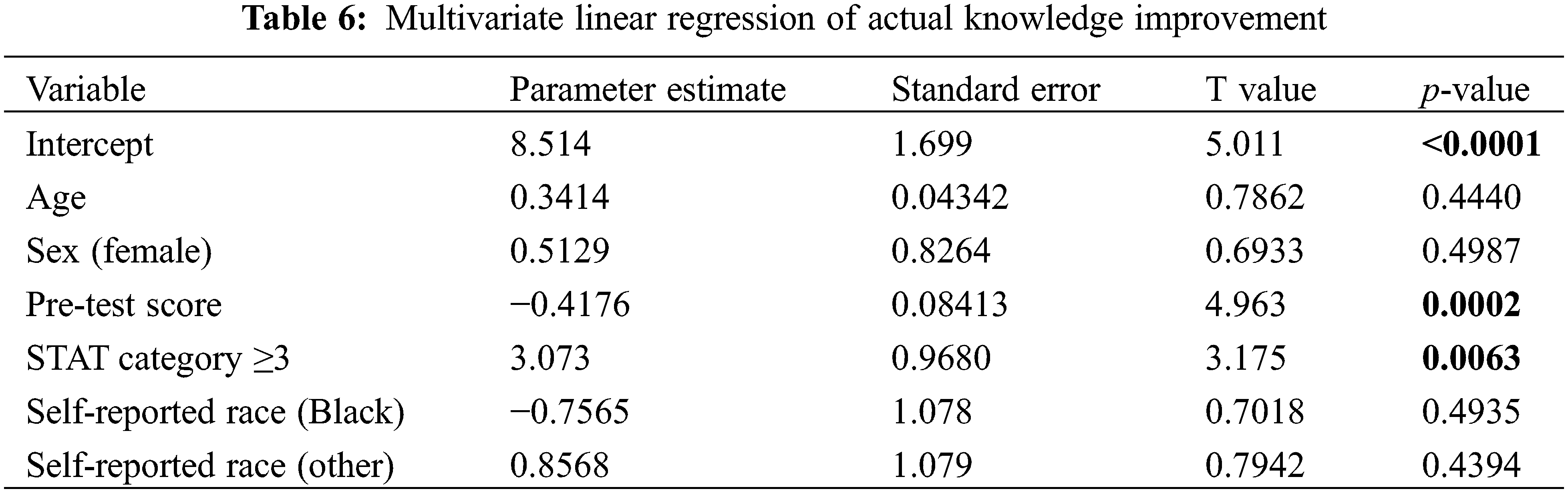
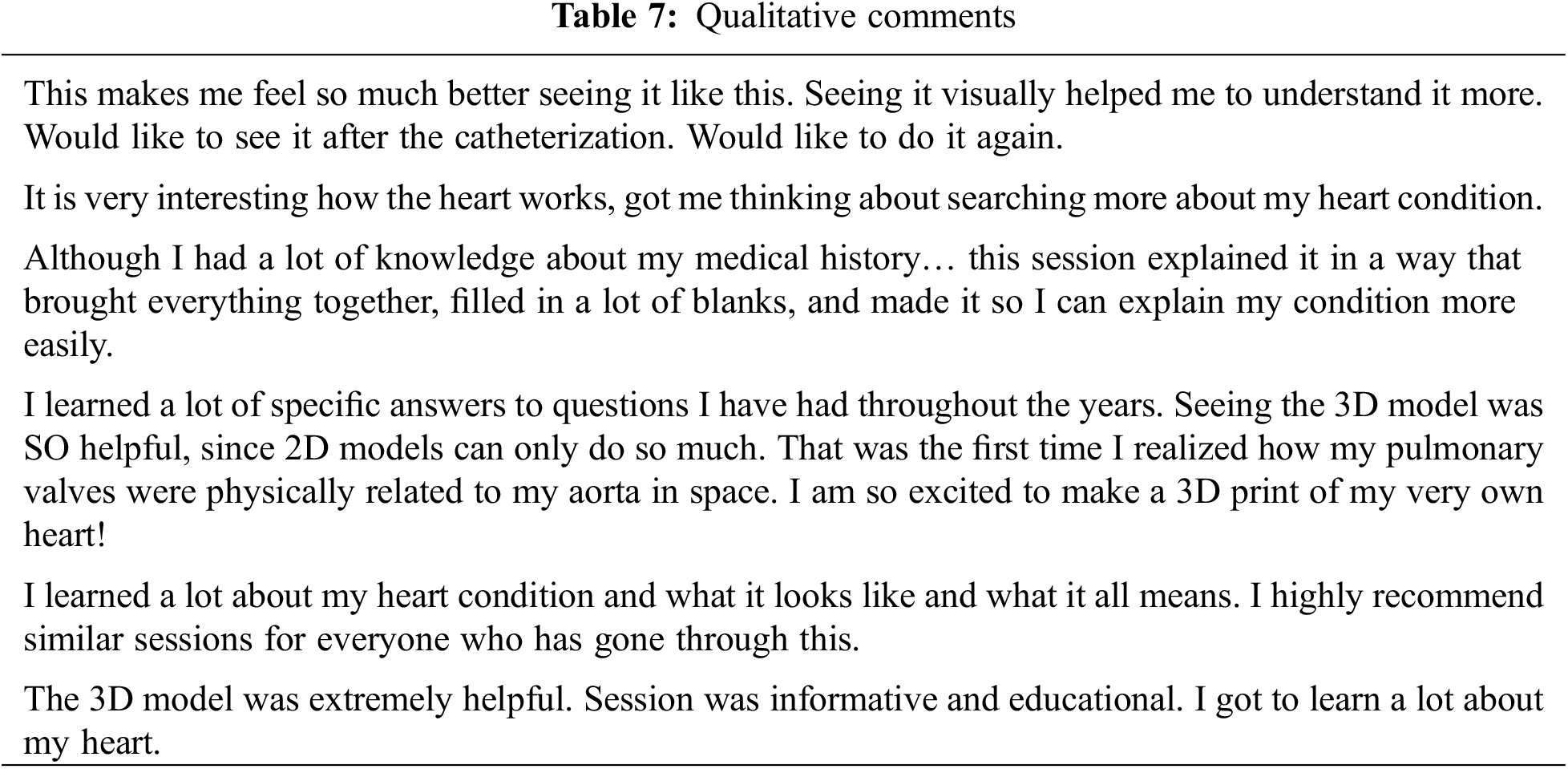
On multivariate analysis, we found that improvement in actual knowledge scores was associated with lower baseline score and STAT category ≥3, but independent of age, gender or race (Table 6). Likewise, baseline actual knowledge scores were not associated with age, gender, race, or STAT category (Supplementary Table S1). Study participants’ qualitative comments regarding the educational session are presented in Table 7.
This study prospectively implemented a tele-education session using 3D models as a tool to improve each adolescent or adult patient’s knowledge of his/her specific CHD. This study also utilized the “4D”-passport including the 3D model and a summary of all the patient’s pertinent CHD information. This educational strategy was found to increase both actual and perceived knowledge for prospective ACHD patients.
Transition readiness for ACHD is a multi-faceted assessment, of which a patient’s actual and perceived knowledge should be a critical element. Perceived knowledge in particular can be readily and quickly ascertained in the clinical setting. Uzark et al. developed a unique questionnaire assessing the following domains: knowledge deficits, self-efficacy, and self-management behaviors [6]. They found perceived knowledge to be an accurate reflection of actual knowledge, which was consistent with our study. The MyHeart Questionnaire developed by Mackie et al. tested actual knowledge [8] in addition to self-efficacy and self-advocacy. The aspect of actual patient medical knowledge is not always investigated in transitional readiness [9,20–25]. Additionally, actual patient knowledge in some studies has been tested, but not tied to outcomes related to transition readiness [7,16,26–28]. However, in general, knowledge deficits were found to be significantly negatively correlated with self-efficacy and self-management [8,29]. Thus, strategies to improve patient knowledge such as our “4D” passport should continue to be developed.
The “4D” educational session allowed for both visual representation with the 3D model and integration of pertinent health details simultaneously. Patients with a complex Mustard baffle can visualize the potential regions of narrowing and understand why further follow-up and subsequent interventions are required. The need for prophylactic antibiotics could be understood by visualizing the implanted transcatheter valve in the heart. The reasons for long-term follow-up for repaired Tetralogy of Fallot could be conveyed by visualizing the dilation of the right heart from chronic pulmonic insufficiency. Our multivariate analysis suggests that the use of the “4D” passport could potentially be targeted to those with CHD complexity or those with less baseline understanding of their own CHD condition.
While these virtual models were not tangible, participants still found the 3D models to be useful when presented in a teleconference setting. Furthermore, the use of teleconferencing and digital models and 3D PDF files allowed this study to be conducted during the COVID-19 pandemic, while still allowing patients an opportunity to interact with their personalized model and avoiding the need to individually print each 3D model which has resource implications [30,31].
To date, there have been few studies utilizing virtual, patient-specific 3D models for patient-specific education in CHD. Biglino et al. determined that a majority of parents rated the 3D models as “very useful” and allowed for more immediate understanding compared to 2D images [10]. Other studies have used the creation of a passport, online tools, or virtual apps, but did not incorporate a 3D model [8,9,14]. For medical trainees, such models allow for better spatial understanding of complex cardiac conditions and have been generally met with increased learner satisfaction [11,12]. In our study [13], we successfully used digital 3D models and demonstrated improvement in measured actual knowledge under the same schema as Biglino et al. [10]. Thus, this educational strategy should serve as a useful component for CHD patients to be educated about transition readiness in the long term.
This study has several limitations, including the limited sample size and the lack of a control group which may affect the generalizability of the results. We acknowledge that this is a relatively small pilot study compared to the number of patients cared for at our institution, but we hope to incorporate some of the elements from the study into clinical practice as 3D models have been used for patient education on an ad hoc basis. Only English-speaking patients were included. The perceived knowledge questionnaire used questions from established questionnaires [16]; however, some of the questions were modified (to tailor towards assessment of the 3D intervention) and were not validated. Also, only immediate post-intervention knowledge was tested without any long-term follow-up or outcomes data, although this was not attempted due to concerns of the COVID-19 pandemic remaining a significant confounder. Finally, the study also focused mainly on the domain of knowledge and did not assess other domains of transition readiness (e.g., self-efficacy, self-management, self-advocacy). Future studies should focus on these aspects, in addition to determining usefulness for patient knowledge and satisfaction for providers in the outpatient and/or emergency setting. In addition to a larger sample size, studies will also stratify effectiveness by the complexity of CHD.
In conclusion, the “4D” tele-education intervention increased patient actual and perceived knowledge. Also, patients were satisfied with the intervention and with their personalized 3D model. This increase in knowledge may help to improve transition readiness and successful transition to adult care. More research must be completed to study the long-term effectiveness of this intervention.
Acknowledgement: The authors would like to acknowledge the patients and parents who generously agreed to volunteer their time and attention to this study.
Funding Statement: The authors received no specific funding for this study.
Author Contributions: The authors confirm contribution to the paper as follows: study conception and design: M. Clarke, N. Klein, L. Olivieri, Y. Loke; data collection: K. Hamann, M. Clarke; analysis and interpretation of results: M. Clarke, Y. Loke; draft manuscript preparation: M. Clarke, Y. Loke. All authors reviewed the results and approved the final version of the manuscript.
Availability of Data and Materials: Readers can access the data used in the study by contacting the corresponding author.
Ethics Approval: Research involving human subjects complied with all relevant national regulations, institutional policies and is in accordance with the tenets of the Helsinki Declaration (as revised in 2013) and has been approved by the authors’ Institutional Review Board (Children’s National Hospital). All the patients consented for the study.
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
Supplementary Materials: The supplementary material is available online at 10.32604/chd.2024.046328.
References
1. Gurvitz M, Dunn JE, Bhatt A, Book WM, Glidewell J, Hogue C, et al. Characteristics of adults with congenital heart defects in the United States. J Am Coll Cardiol. 2020;76(2):175–82. [Google Scholar] [PubMed]
2. Downing KF, Nembhard WN, Rose CE, Andrews JG, Goudie A, Klewer SE, et al. Survival from birth until young adulthood among individuals with congenital heart defects: cH STRONG. Circ. 2023;148(7):575–88. [Google Scholar]
3. Jacobsen RM. Outcomes in adult congenital heart disease: neurocognitive issues and transition of care. Pediatr Clin N Am. 2020;67(5):963–71. [Google Scholar]
4. Yeung E, Kay J, Roosevelt GE, Brandon M, Yetman AT. Lapse of care as a predictor for morbidity in adults with congenital heart disease. Int J Cardiol. 2008;125(1):62–5. [Google Scholar] [PubMed]
5. Stewart KT, Chahal N, Kovacs AH, Manlhiot C, Jelen A, Collins T, et al. Readiness for transition to adult health care for young adolescents with congenital heart disease. Pediatr Cardiol. 2017;38(4):778–86. [Google Scholar] [PubMed]
6. Uzark K, Yu S, Lowery R, Afton K, Yetman AT, Cramer J, et al. Transition readiness in teens and young adults with congenital heart disease: can we make a difference? J Pediatr. 2020;221:201–6.e1. [Google Scholar] [PubMed]
7. Ladouceur M, Calderon J, Traore M, Cheurfi R, Pagnon C, Khraiche D, et al. Educational needs of adolescents with congenital heart disease: impact of a transition intervention programme. Arch Cardiovasc Dis. 2017;110(5):317–24. [Google Scholar] [PubMed]
8. Mackie AS, Islam S, Magill-Evans J, Rankin KN, Robert C, Schuh M, et al. Healthcare transition for youth with heart disease: a clinical trial. Controlled Clinical Trial. 2014;100(14):1113–8. [Google Scholar]
9. Mackie AS, Rempel GR, Kovacs AH, Kaufman M, Rankin KN, Jelen A, et al. Transition intervention for adolescents with congenital heart disease. J Am Coll Cardiol. 2018;71(16):1768–77. [Google Scholar] [PubMed]
10. Biglino G, Capelli C, Wray J, Schievano S, Leaver LK, Khambadkone S, et al. 3D-manufactured patient-specific models of congenital heart defects for communication in clinical practice: feasibility and acceptability. BMJ Open. 2015;5(4):e007165. [Google Scholar] [PubMed]
11. Loke YH, Harahsheh AS, Krieger A, Olivieri LJ. Usage of 3D models of tetralogy of Fallot for medical education: impact on learning congenital heart disease. BMC Med Educ. 2017;17(1):54. [Google Scholar] [PubMed]
12. Tarca A, Woo N, Bain S, Crouchley D, McNulty E, Yim D. 3D printed cardiac models as an adjunct to traditional teaching of anatomy in congenital heart disease-A randomised controlled study. Heart, Lung Circ. 2023;32(12):1443–50. doi:10.1016/j.hlc.2023.09.021. [Google Scholar] [PubMed] [CrossRef]
13. Liddle D, Balsara S, Hamann K, Christopher A, Olivieri L, Loke YH. Combining patient-specific, digital 3D models with tele-education for adolescents with CHD. Cardiol Young. 2022;32(6):912–7. [Google Scholar] [PubMed]
14. Valente AM, Landzberg MJ, Gianola A, Harmon AJ, Cook S, Ting JG, et al. Improving heart disease knowledge and research participation in adults with congenital heart disease (the health, education and access research trial: HEART-ACHD). Int J Cardiol. 2013;168(4):3236–40. [Google Scholar] [PubMed]
15. Ricci P, Dimopoulos K, Bouchard M, Zhiya CC, Castro Meira V, Pool D, et al. Transition to adult care of young people with congenital heart disease: impact of a service on knowledge and self-care skills and correlates of a successful transition. Eur Heart J Qual Care Clin Outcomes. 2023;9(4):351–7. [Google Scholar] [PubMed]
16. Gurvtiz M, Mackie A, Jedekin R, Lopez K, Saidi A, Chowdhury D, et al. ACC releases CHD transition tools. 2016. Available from: https://www.acc.org/Membership/Sections-and-Councils/Adult-Congenital-and-Pediatric-Cardiology-Section/Section-Updates/2016/07/21/16/34/ACC-Releases-CHD-Transition-Tools (accessed on 06/09/2020). [Google Scholar]
17. McHugh ML. Interrater reliability: the kappa statistic. Biochem Medica. 2012;22(3):276–82. [Google Scholar]
18. Cohen J. Weighted kappa: nominal scale agreement with provision for scaled disagreement or partial credit. Psychol Bull. 1968;70(4):213–20. [Google Scholar] [PubMed]
19. O’Brien SM, Clarke DR, Jacobs JP, Jacobs ML, Lacour-Gayet FG, Pizarro C, et al. An empirically based tool for analyzing mortality associated with congenital heart surgery. J Thorac Cardiovasc Surg. 2009;138(5):1139–53. [Google Scholar] [PubMed]
20. Wood DL, Sawicki GS, Miller MD, Smotherman C, Lukens-Bull K, Livingood WC, et al. The transition readiness assessment questionnaire (TRAQits factor structure, reliability, and validity. Acad Pediatr. 2014;14(4):415–22. [Google Scholar] [PubMed]
21. Chan JT, Soni J, Sahni D, Mantis S, Boucher-Berry C. Measuring the transition readiness of adolescents with type 1 diabetes using the transition readiness assessment questionnaire. Clin Diabetes: A Publ Am Diabetes Assoc. 2019;37(4):347–52. [Google Scholar]
22. Klassen AF, Grant C, Barr R, Brill H, Kraus de Camargo O, Ronen GM, et al. Development and validation of a generic scale for use in transition programmes to measure self-management skills in adolescents with chronic health conditions: the TRANSITION-Q. Child: Care, Health Dev. 2015;41(4):547–58. [Google Scholar] [PubMed]
23. Ekim A, Kolay M, Ocakci AF. Readiness for transition from pediatric to adult care for adolescents with chronic heart disease. J Spec Pediatr Nurs. 2018;23(1):e12199. doi:10.1111/jspn.12199. [Google Scholar] [PubMed] [CrossRef]
24. Gilleland J, Amaral S, Mee L, Blount R. Getting ready to leave: transition readiness in adolescent kidney transplant recipients. J Pediatr Psychol. 2012;37(1):85–96. [Google Scholar] [PubMed]
25. Burström Å, Acuña Mora M, Öjmyr-Joelsson M, Sparud-Lundin C, Rydberg A, Hanseus K, et al. Ready for transfer to adult care? A triadic evaluation of transition readiness in adolescents with congenital heart disease and their parents. J Fam Nurs. 2019;25(3):447–68. [Google Scholar]
26. Moons P, de Volder E, Budts W, de Geest S, Elen J, Waeytens K, et al. What do adult patients with congenital heart disease know about their disease, treatment, and prevention of complications? A call for structured patient education. Heart (Br Cardiac Soc). 2001;86(1):74–80. [Google Scholar]
27. van Deyk K, Pelgrims E, Troost E, Goossens E, Budts W, Gewillig M, et al. Adolescents’ understanding of their congenital heart disease on transfer to adult-focused care. Am J Cardiol. 2010;106(12):1803–7. [Google Scholar] [PubMed]
28. Mackie AS, Rankin KN, Yaskina M, Gingrich J, Williams E, Schuh M, et al. Transition preparation for young adolescents with congenital heart disease: a clinical trial. J Pediatr. 2022;241:36–41.e2. [Google Scholar] [PubMed]
29. Huang HR, Chen CW, Chen CM, Yang HL, Su WJ, Wang JK, et al. A positive perspective of knowledge, attitude, and practices for health-promoting behaviors of adolescents with congenital heart disease. Eur J Cardiovasc Nurs. 2018;17(3):217–25. [Google Scholar] [PubMed]
30. Luo H, Meyer-Szary J, Wang Z, Sabiniewicz R, Liu Y. Three-dimensional printing in cardiology: current applications and future challenges. Cardiol J. 2017;24(4):436–44. [Google Scholar] [PubMed]
31. Asif A, Lee E, Caputo M, Biglino G, Shearn AIU. Role of 3D printing technology in paediatric teaching and training: a systematic review. BMJ Paediatr Open. 2021;5(1):e001050. [Google Scholar] [PubMed]
Cite This Article
 Copyright © 2024 The Author(s). Published by Tech Science Press.
Copyright © 2024 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools