 Open Access
Open Access
ARTICLE
Risk Factors for Abuse in Children with Congenital Heart Disease Presenting at a Pediatric Tertiary Care Hospital
1 School of Nursing, University of California, Los Angeles, California, USA
2 Department of Pediatrics, Children’s Hospital Los Angeles, Audrey Hepburn CARES Center, Los Angeles, California, USA
3 Keck School of Medicine of the University of Southern California, Los Angeles, California, USA
4 Department of Pediatrics, Critical Care Medicine, Children’s Hospital Los Angeles, Los Angeles, California, USA
5 Department of Pediatrics Heart Institute, Children’s Hospital Los Angeles, Los Angeles, California, USA
* Corresponding Author: Kristi K. Westphaln. Email:
Congenital Heart Disease 2023, 18(6), 657-670. https://doi.org/10.32604/chd.2023.044179
Received 23 July 2023; Accepted 30 October 2023; Issue published 19 January 2024
Abstract
Background: Congenital heart disease (CHD) is a chronic medical condition often diagnosed at birth and requires surgical intervention, multiple hospitalizations, and lifelong care. This can put significant stress on the family, leading to altered maternal mental health, bonding and attachment issues, and the potential for child abuse. The purpose of this study is to explore the characteristics of a sample of young children with CHD who experienced hospitalization with concurrent concern for child abuse in a free-standing pediatric tertiary care hospital. Methods: Electronic medical records were reviewed for children aged 0–5 years old who were hospitalized with concern for child abuse between 2016 and 2020. Variables were extracted related to the history of presentation, and sociodemographics including SDOH, admission, and discharge condition/follow-up. Descriptive statistics were used to characterize the sample and correlations to identify an association with abuse type. Results: Out of 251 hospitalizations involving concern for child abuse, 49 (19.5%) had a diagnosis of CHD. The majority of cases were neglect (51%), <1 year of age (80%), male (57%), Hispanic ethnicity (45%), and publicly insured (90%). CHD severity was moderate to severe (71%) with multiple co-occurring medical conditions (genetic syndrome, failure to thrive (FTT), prematurity, history of a feeding tube, developmental delay, and intrauterine drug exposure). Correlations associated with physical abuse were age, maternal mental health, head injury, and history of Child Protective Services (CPS) involvement. Neglect correlated with age, FTT, head injury, history of a feeding tube, previous CPS involvement, and substance use. Correlates specifically related to prenatal substance use included age, maternal mental health status, history of domestic violence, CPS involvement, feeding tube, FTT, lack of housing, employment status, and public insurance. Conclusions: Our study highlights the risk for abuse in children with CHD, regardless of defect severity. The most common abuse type was neglect (mostly prenatal substance use) which was associated with few child characteristics, but many parent/caregiver and neighborhood factors. This underscores the need for individual and/or family-based screening and approaches to provide psychological support and needed resources to assist parents of children with CHD to prevent abuse. Interventions should focus on families of low socioeconomic status with limited support and/or resources.Keywords
In the United States (US), child abuse affected more than 600,000 children with an estimated 1820 deaths in 2021 [1]. Children less than 1 year of age are at higher risk for abuse with over 76% of cases reflecting the result of neglect by a parent or caregiver [1]. Children at risk often have underlying behavioral or functional disorders or co-occurring medical conditions placing insurmountable stress on the parents and/or family unit [2]. Parents of children with congenital heart disease (CHD) exhibit more stress than those of children with other chronic diseases [3–6].
When a child is born with CHD, parents may experience shock, disbelief, despair, and grief over the loss of an anticipated healthy child [7]. Shortly after birth, many of these infants undergo medical and surgical interventions, intensive care unit (ICU) stays, and prolonged hospitalization. This traumatic experience is often associated with psychological strains for parents/caregivers. When parents/caregivers experience mental health difficulties, this can increase the risk for child abuse [8] and affect families who have a child born with CHD. In most societies, the mother typically provides the primary role of child caregiving. Depression, anxiety, somatization, hopelessness, and posttraumatic stress symptoms are frequently found in parents of children with CHD, with mothers reporting more symptoms than fathers [9]. These mental health conditions can have a significant impact on caregiver responsiveness which can affect the child-parent interaction/attachment and, ultimately, infant development [10,11].
Despite the stress that parents report with having a child with CHD, many face overwhelming emotions, physical and financial strains associated with disparities in social determinants of health (SDOH), and other practical challenges [3,12]. This could potentially lead to abuse that may be unintentional in nature. Given that little is known about risk factors contributing to abuse among children with CHD, the purpose of this study was to explore characteristics of a sample of young children with CHD who experienced hospitalization with concurrent concern for child abuse and/or neglect.
2.1 Study Design and Population
This study is a secondary analysis of a retrospectively collected electronic medical record (EMR) dataset (years 2016 to 2020) of children (ages 0–5 years) with CHD hospitalized with concern for child abuse and/or neglect at Children’s Hospital Los Angeles (CHLA). CHLA is a large tertiary free-standing, urban children’s hospital that serves diverse families residing in Los Angeles [13]. Los Angeles County is a highly populated, geographic region with low per capita income, wide ethnic diversity (almost 50% Hispanic or Latino, 14% Asian, and 7.5% African American), and many possessing public health insurance and experiencing poverty, housing challenges, and food insecurity [13,14]. Thus, highlighting this high-risk area for potential abuse and/or neglect.
The Gelberg-Andersen Behavioral Model for Vulnerable Populations (GABMVP) was used to assist in the investigation of the cohort characteristics [13–15]. The GABMVP model depicts the relationship of predisposing, enabling, and need factors to the utilization of health or other types of post-discharge services and health outcomes [13–15] (Fig. 1). Along with guidance from the GABMVP, variable selection for this study was determined a priori based upon a review of the literature [1,15–17], and consultation with physicians, nurses, and social workers with expertise in child abuse and neglect.
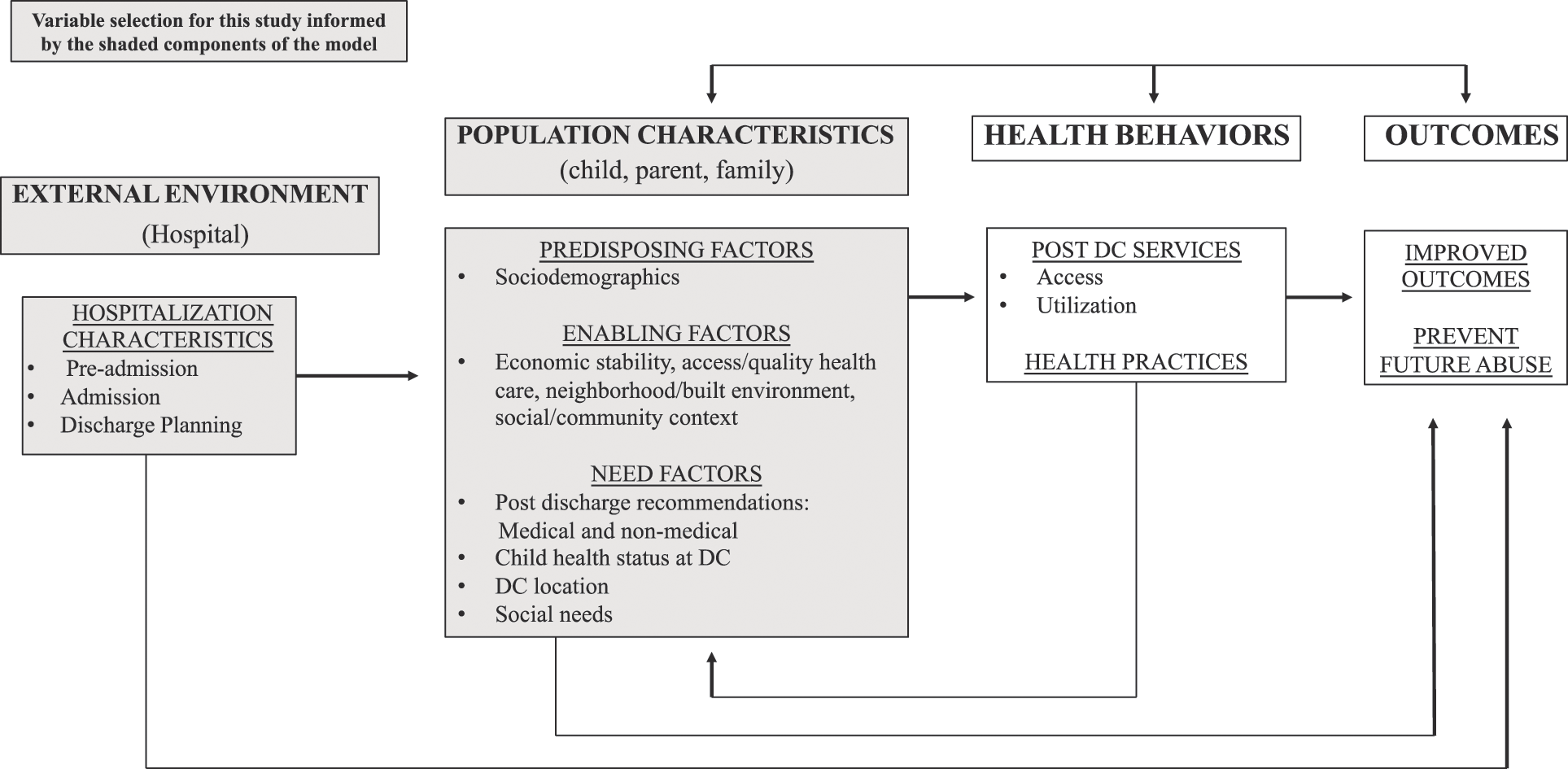
Figure 1: Adaptation of the Gelberg-Andersen behavioral model for vulnerable populations
The analytic sample for this study was constructed using a four-step process. First, a list of medical record numbers (MRNs) was generated by the CHLA Information Technology Team that represented (1) children aged 0-years, (2) hospitalized at CHLA from 2016–2020, and (3) had an International Classification of Diseases, Tenth Revision (ICD-10) code that was consistent with an injury or diagnosis associated with possible child abuse or neglect, which yielded 2245 children. The list of ICD-10 codes was created by a multidisciplinary team consisting of two pediatric nurse practitioners, a board-certified child abuse pediatrician, a social worker with expertise in child maltreatment, and a pediatric trauma surgeon. The 2016–2020 date range was selected to remain consistent with using ICD-10 vs. ICD-9 coding and to avoid confounding by the coronavirus disease (COVID) pandemic stay-at-home orders.
Each MRN identified during the initial abstraction was verified for inclusion by a member of the research team confirming the presence of a concern for child abuse and/or neglect during the hospitalization as operationalized by documentation in the EMR (e.g., admission note, discharge summary, official child abuse reporting document, social work note, and/or a note from the CHLA child protection team). Completion of the verification process yielded a total of 251 cases that represented hospitalizations with concern for child abuse. The final study sample included only cases that were affiliated with a CHD diagnosis (n = 49) (Fig. 2).
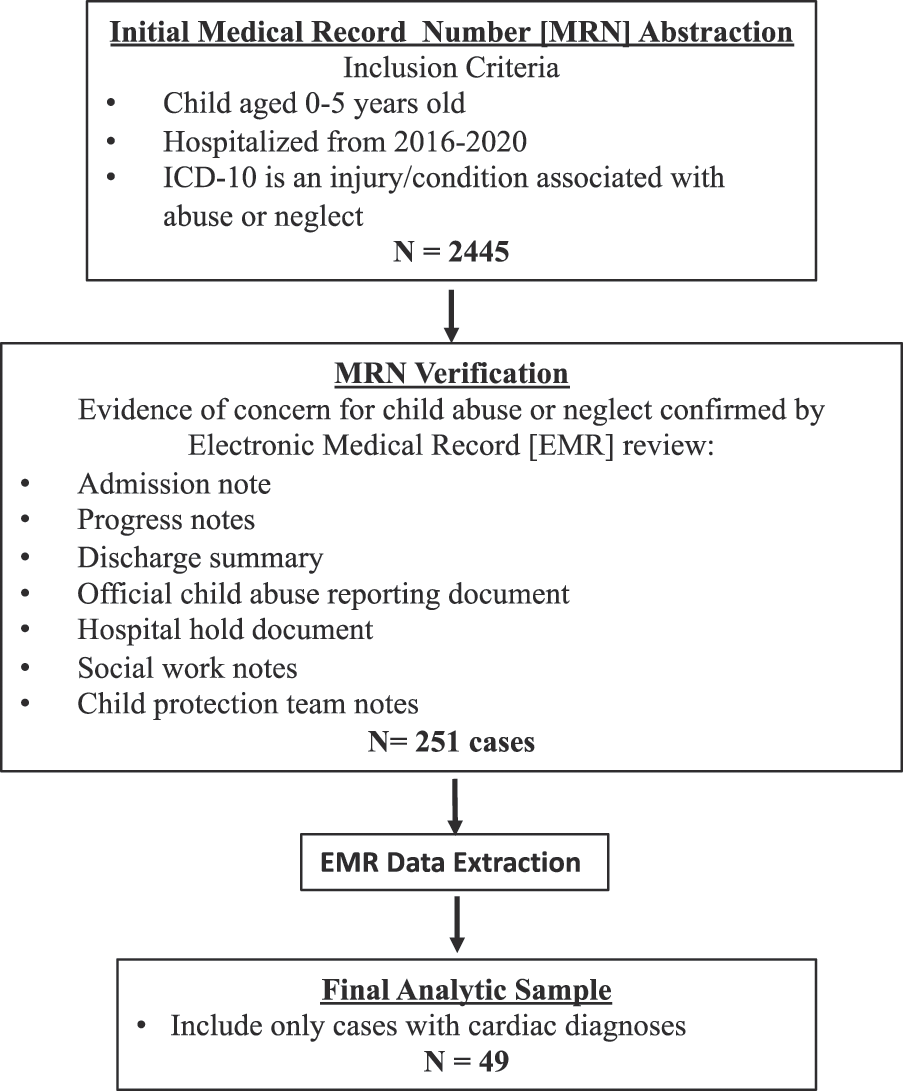
Figure 2: Study sample screening for child abuse cases
Data were extracted from the EMR by members of the research team on variables pertaining to demographics, SDOH, hospitalization, and post-discharge follow up recommendations. To assure high-quality data collection and data entry, 20% of the total sample was audited for accuracy and demonstrated a 96% interrater agreement.
2.3 Social Determinants of Health (SDOH) Variables
Data describing the presence of challenges related to SDOH involving housing, food, transportation, employment, previous CPS involvement, domestic violence, substance use or abuse, incarceration, and maternal mental health concerns were assessed by reviewing documentation within notes written by the social work and/or child protection team. If challenges or concerns in any of these areas were documented in the EMR (e.g., food insecurity, homelessness, difficulty finding and maintaining a job, or the family does not have a car), these variables were coded as “yes.”
Descriptive statistics (frequencies, percentages) were used to characterize the sample. Chi-squared was used to assess categorical variables and comparisons between abuse type, and Spearman’s Rho correlations were used to examine associations between demographic, clinical, and SDOH variables per abuse type. All analyses were conducted with the Statistical Package for the Social Sciences version 28.0 [18] with a significance set at a p-value < 0.05.
3.1 Abuse Type Characteristics and Follow-Up
The variable abuse types and their associated demographic and clinical characteristics are highlighted in Table 1. Neglect was the most common form of abuse in the CHD population (51%) compared to physical abuse (12%) and the “other” category of prenatal substance use (37%). Physical abuse and neglect were more prevalent in children up to 1 year of age (80%). However, prenatal substance use was more common in infants less than 30 days of life (67%). CHD severity was widely distributed across mild, moderate, and severe defects. However, severe types of CHD were most commonly associated with physical abuse (83%), neglect (40%), and prenatal substance use (56%). Co-occurring medical conditions were consistent across all types of abuse with genetic syndromes, previous history of failure to thrive, developmental delays, feeding tube use (nasogastric or gastrostomy), and intrauterine drug exposure. Of note, greater than 83% of the sample had state-subsidized medical care (e.g., MediCal, California Children’s Services).
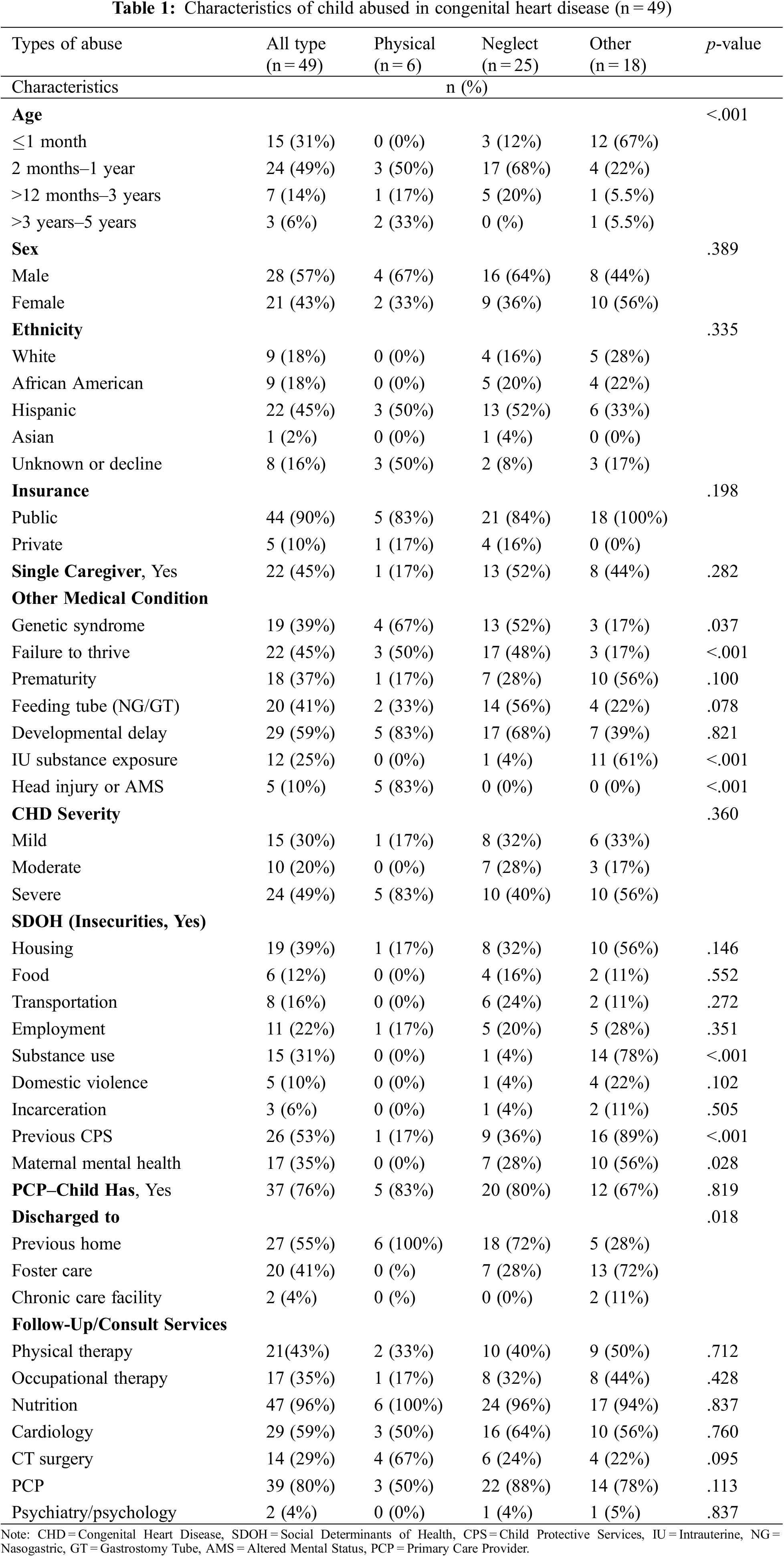
3.2 Social Determinants of Health and Follow-Up Related to Abuse Type
SDOH, including social needs related to housing, food, transportation, employment, and other key factors, were assessed across abuse types listed in Table 1. Parental/caregiver insecurities associated with child neglect were lack of housing (32%), transportation (24%), employment (20%), history of previous CPS involvement (36%), and parent mental health challenges (32%). The prenatal substance use category was associated with housing, predominantly homelessness (56%), unemployment (28%), substance use/abuse (78%), history of CPS involvement (89%), and parent mental health challenges (78%). With a limited number in the physical abuse category (n = 6), this made it difficult to assess prominent insecurities but housing (17%), employment (17%), and history of CPS involvement (17%) were identified.
Discharge and follow-up care characteristics are outlined in Table 1. Nutrition consultation, occupational therapy, and physical therapy were provided as routine services across all abuse categories. Of those children that suffered possible physical abuse (5 out of 6 with head injuries), the majority were discharged home to their known home (100%) and received discharge recommendations to follow up with cardiac surgery, cardiology, and their primary care provider (PCP). Children that suffered neglect were discharged back to their previous home (72%) or placed in foster care (28%) and also received discharge recommendations to follow up with cardiac surgery, cardiology, and their PCP. The prenatal substance use category was primarily discharged into medical foster care (61%) with discharge recommendations to follow up with cardiology (56%) and their PCP (78%). Of note, only a few children received a referral for outpatient mental health services, which may be explained by 80% of the sample being less than one year of age.
3.3 Demographic, Clinical, and SDOH Variables Associated with Abuse Type
The demographic, clinical, and SDOH variables associated with abuse type are listed in Table 2. Only a few variables were negatively correlated with physical abuse which included previous CPS involvement (r = −.272; p = .050) and maternal mental health (r = −.272; p = .050). Since the majority of the physical abuse sample involved head injuries, these variables were strongly correlated (r = .798; p < .001). Neglect was negatively correlated with head injury (r = −.317, p = .026), history of CPS involvement (r = −.311, p = .030) and more strongly correlated with a history of substance use most commonly reported as alcohol, cannabis, heroin, and methamphetamines (r = −.510, p = <.001). Failure to thrive (r = .393, p = .005) and feeding tube (nasogastric and gastrostomy) use (r = .414, p = .003) showed moderate correlations with neglect.
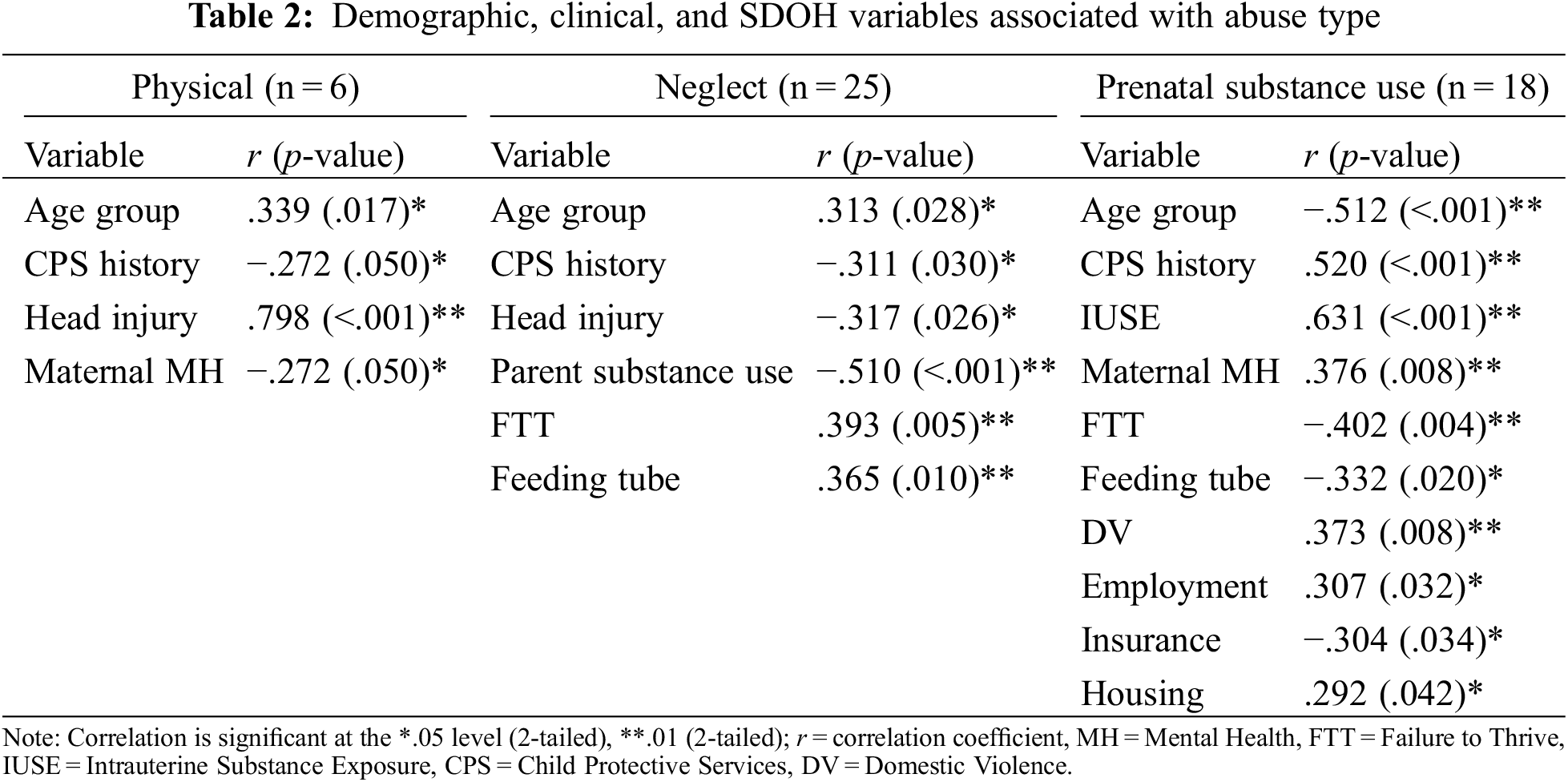
The majority of variables that correlated with prenatal substance use also had the most disparities related to SDOH. Almost half experienced housing issues (r = .292, p = .042) related to homelessness or being in transitional housing via a rehabilitation program. Others experienced domestic violence, unemployment, and/or maternal mental health challenges where community resources were provided. A strong correlation was associated with intrauterine drug exposure (r = .631, p < .001), whereas weak to moderate correlations were identified among infants less than 30 days of life (r = −.512, p = <.001), a history of CPS involvement, history of FTT, and feeding tube use.
This is the first study of which we are aware to report on child abuse in the CHD population located in an urban, high-risk geographical area. Challenges related to caregiver mental health symptoms and/or diagnoses [7,8] may be compounded by health care disparities [3,12], limited personal resources and support, having a child with chronic medical needs [19], and substance use [1], which can heighten the risk for child abuse. We found few children suffering possible physical abuse, but the ones who did have head and/or skeletal injuries. The majority of abuse cases were related to neglect, with children being less than one year of age, using some type of feeding tube for nutrition (e.g., nasogastric or gastrostomy), and having a diagnosis of FTT. Significant caregiver characteristics that were collected on the primary caregiver at the time of admission included maternal mental health challenges and previous or current substance use. Previous involvement with CPS was a salient family-level characteristic. Thus, the risk factors for child abuse and/or neglect in children with a medically complex condition, combined with situational factors such as alternations in parent mental health, poor access to resources, and low SES, may contribute to a constellation of circumstances that create the ideal condition or “perfect storm” for abuse in the CHD population compared to other children. These findings warrant the need for early environmental and mental health screening of parents or caregivers as they adjust to their “new normal” in caring for a child with CHD [20,21].
4.1 Failure to Thrive and Neglect
FTT is a term commonly used for a child who is not demonstrating adequate weight gain as expected for age and height. This is a physical sign suggestive of an underlying condition related to a variety of factors such as biological (genetic or metabolic), psychosocial (abuse or neglect), or environmental (poverty). Approximately 30%–60% of children with CHD have FTT related to their cardiac condition or a co-occurring genetic syndrome that impairs growth and development [22]. The cause of growth failure or FTT is most likely multifactorial and includes a hypermetabolic state, inadequate caloric intake, swallowing dysfunction, malabsorption, gastroesophageal reflux, immaturity of the gastrointestinal tract, and/or genetic factors. Furthermore, nearly half of all infants with single ventricle CHD will require feeding supplementation with nasogastric or gastrostomy tube feedings [23]. However, all cases, in our study, had documented concerns and evaluations for FTT resulting from accidental, neglectful, and/or deliberate actions by the parent or caregiver.
Risk factors that one might presume may contribute to neglect such as a single parent, genetic syndrome, and CHD severity were not associated with any of the abuse types. Our findings are consistent with the literature demonstrating that 30–80% of caregivers of children with CHD experience mental health distress (anxiety, depression, and posttraumatic stress disorder) that appear to be unrelated to CHD severity [4] and substance abuse were related to the broad abuse type of neglect and, more specifically, prenatal substance use [24]. One European study in adults with CHD self-reported the incidence and type of child maltreatment which showed higher rates of emotional abuse/neglect and sexual abuse and lower rates of physical abuse which was highly correlated with participant’s current mental health status (anxiety and depression) and quality of life [25]. However, there are no related studies that describe risk factors for child abuse in CHD.
4.2 Infants with Prenatal Substance Exposure (IPSE)
This study identified infants with prenatal substance exposure (IPSE) in an “other” category in which the infants were less than 30 days of life and had a positive toxicology screen confirming intrauterine substance exposure. This sub-group had many SDOH variables as risk factors. Many parents were unhoused or in transitional housing, unemployed, and had mental health challenges and many families experienced domestic violence and had a history of CPS involvement.
Child abuse is often viewed within the context of postnatal life. While it is generally agreed upon that parent/caregiver substance use disorders and intrauterine exposure to drugs or alcohol negatively impact child safety and health outcomes, not all states define prenatal drug or alcohol exposure as abuse [1,26]. Currently, 25 states view prenatal substance use as child abuse and have punitive policies in place for offenders [27]. In California, prenatal substance use is not considered child abuse and is not a punishable crime, however, a positive newborn drug screen is reportable to CPS [26–29]. Maternal substance use and/or polysubstance use for non-medical purposes, despite black box warnings against prenatal use (e.g., alcohol, cannabis, methamphetamines, opiates, or heroin), has dramatically increased over the past two decades [30]. This public health concern is heightened due to the potential effects on the developing fetus and could be a non-inherited cause for CHD [4,31]. Prenatal substance use has been reported to cause an increased incidence of complications such as placental insufficiency, intrauterine growth restriction and premature birth, neonatal withdrawal or abstinence syndrome, and congenital anomalies [4,25]. However, there are conflicting reports related to prenatal substance use and its association with CHD. With abortion rights being overturned in many states, the ability of women with substance use and/or the inability to care for a child with complex medical needs, will not be able to access this option. This is further compounded by punitive or criminal consequences for prenatal substance use, which has been shown to decrease the utilization of both prenatal care and drug treatment programs [24]. Thus, we may see an increase in the number of infants born with sequelae of intrauterine substance exposure and other complex medical needs, particularly CHD, that could impact our healthcare system and state resources.
4.3 Follow-Up Care Considerations
Our study also highlights key follow-up care considerations for children who experience hospitalization with concern for child abuse or neglect who also have CHD. At discharge, the majority of the cases were instructed to follow up with their PCP, and cardiology clinic, and received referrals for outpatient state-provided rehabilitation services (e.g., physical and occupational therapy). Furthermore, evidence supports that children with CHD have greater utilization of healthcare services when compared to other children in the US including five times the use of home health services, eight times the use of special medical equipment, three times more prescription medications, and two times more special education services [12]. Very few of the cases received inpatient consultation or outpatient follow-up recommendations for psychology or psychiatry. The limited family-centered approach to maternal and child psychology or psychiatry follow-up services may reflect the age of the study population (e.g., 0–5 years of age), challenges with billing and reimbursement for inpatient mental health services, the critical shortage of mental health providers, or disparities in accessing mental health services. While many of the cases in the physical and neglect subgroups were discharged home to their known home, the majority of cases in the IPSE category were discharged into foster placement or a group home.
4.4 Child Abuse in CHD and Public Health Policy Implications
Multiple reports on parental/caregiver stress have shown a negative impact on marital relationships often leading to divorce [3,6,7]. Families of children with chronic medical conditions often live in a state of increased vigilance, amplified anxiety, and emotional exhaustion [7]. Mental health concerns compounded by financial and environmental stressors can potentially lead to child abuse or neglect. Children with CHD are considered a vulnerable population with parents facing high levels of distress related to emotional, physical, and financial challenges that can impact the whole family. Similar to other groups of children with special healthcare needs or medical complexity [32], many children with CHD are living longer, requiring high utilization of healthcare resources [12,31], and both children and parents may lack mental health skills and support to cope with daily life stressors [2,4,33]. Left unaddressed, these factors may contribute to an increased risk for child abuse or neglect and exacerbate poor physical, mental, or behavioral outcomes for those children who suffer abuse [34–37].
Poor parent mental health, especially maternal mental health, is of particular concern [8,38,39]. Parent/Caregiver mental health screening received attention before the COVID-19 pandemic in non-mental health care settings such as pediatric primary care [40–42], pediatric oncology [43], and adult cardiology [4]. Additionally, findings from a systematic review examining the pre-pandemic mental health among parents of children with CHD supported the implementation of a model of pediatric cardiology follow-up care that would integrate both mental health screening and the provision of services into practice [4]. Despite previous efforts to better integrate mental health within some populations, a gap remains between the post-pandemic population of children and parents/caregivers that would benefit from mental health services (e.g., parents/caregivers or children with CHD or other types of special health care needs) and their ability to access and receive those services. Stronger policy efforts are needed to build a larger mental health workforce and bolster access to high-quality mental health services for populations with greater underlying stressors, including those impacted by SDOH and/or systemic inequities [31].
A growing body of literature supports the association between the risk for child abuse with low family socioeconomic status and neighborhood poverty [44–46]. Structural neighborhood factors such as housing instability, limited access to high-quality child care, and financial insecurity contribute greater risk for child abuse than individual parent/caregiver factors [46]. Racial and ethnic disproportionality within the context of living in impoverished neighborhoods and involvement with the child welfare system position children and families of color at great disadvantage, however race and ethnicity are not risk factors for child abuse [47]. To reduce the prevalence and consequences of child abuse, greater emphasis is needed on addressing these structural inequities. Some of the most effective Federal Safety Net Programs that support impoverished children and families involve tax credits (e.g., Child Tax Credit and End Income Tax Credit), food and nutrition (e.g., Supplemental Nutrition Assistance Program and Supplemental Nutrition Program for Women, Infants, and Children), cash assistance (Temporary Assistance for Needy Families and Supplemental Security Income), and public health insurance (Medicaid and the Children’s Health Insurance Program) [48].
Finally, state-level policies on prenatal substance use and the legalization or access to substances (alcohol, cannabis, and opioids) for self-medication or recreational use during the perinatal period may better serve the health and well-being of children by placing more emphasis on prevention and facilitating entry into cessation programs. Intrauterine drug exposure can impact parental bonding and child attachment to parents/caregivers, growth and development, and neurocognitive function. This is especially salient for children with CHD, as many of them already have neurologic deficits related to their clinical condition or medical/surgical interventions. Approaches that combine rapid access to services to reduce prenatal substance exposure with completing an infant needs assessment and safety plan may be more effective than employing mandated reporting of prenatal substance use as a means to criminalize substance use.
This study was conducted at a single center in Los Angeles with a small sample size, so study findings may not be generalizable to all CHD or child abuse populations. Some of the variables of interest were limited or potentially underestimated (e.g., SDOH) due to the retrospective design and availability of data in the EMR. Our sample size limited our statistical analyses to correlations, which do not imply causation. The use of ICD codes to identify child abuse cases is not without limitations. Given that ICD codes exist for billing rather than clinical purposes, they do not always capture all injuries or conditions that are concerning for abuse and are often assigned by coders rather than clinicians [49,50]. If clinicians do not directly specify a diagnosis involving child abuse on the clinical problem list or discharge diagnosis list, there is a possibility that this may be missed or inaccurately entered by coders [49,50]. Additionally, clinicians may be hesitant to assign a formal child abuse diagnosis because child abuse is not always definitively confirmed during hospitalization or upon discharge home from the hospital. We also acknowledge that the cases captured in our sample reflect hospitalizations with concern for child abuse and/or neglect rather than cases of confirmed abuse. Despite the challenges of using ICD-10 codes and EMR data, we incorporated a rigorous process to validate the accuracy of each case included in this study. Additional contributions of this study include a novel application of the GABMVP model and a greater understanding of child abuse risk factors within the medically complex CHD population.
Findings from this study described characteristics associated with a sample of young children with CHD who were hospitalized with concern for child abuse and/or neglect. Neglect was a common abuse type, with a large portion of the sample involving IPSE. Associations to child characteristics were sparse, however many associations were found to involve parent/caregiver and/or environmental factors. The severity of CHD did not demonstrate a greater association with abuse type. This study highlights the need for early individual and/or family-based screening and approaches to provide psychological support and needed resources to help parents of all children with CHD in order to prevent abuse. Additionally, policy-level interventions should focus on mitigating the negative effects of poverty and bolstering resources for parents, particularly among families living in impoverished communities and/or having children with medical complexity or special health care needs.
Acknowledgement: We acknowledge the work of Mohit Mehra and Sergio Fajardo with CHLA informational technology for their assistance with obtaining the EMR dataset; Vincent Li, Benjermin Fan, and Kinnedy Houston for their support with data extraction; and consultants Dr. Ryan Spurrier, Nurse Practitioner Maria Bautista Durand, and Licensed Clinical Social Worker Sandy Himmelrich for sharing their clinical expertise in caring for children and families with concern for child abuse and/or neglect.
Funding Statement: The authors received no specific funding for this study.
Author Contributions: Study concept and design: KKW and NAP; Data collection: KKW, LS, JS; Analyses and interpretation of results: KKW and NAP; Draft manuscript preparation: KKW; Critical revision of the paper for important intellectual content: All authors; Approval of the final version of the manuscript: All authors.
Availability of Data and Materials: The dataset with the variables used for preparing this paper is available upon request from the first author.
Ethics Approval: The authors assert that all procedures contributing to this work comply with ethical standards set forth by the Institutional Review Boards (IRB) from CHLA and the University of California Los Angeles (UCLA). This study was reviewed by both IRBs (CHLA IRB #23-00104 and UCLA IRB #23-001006) and determined exempt, including approval to waive informed consent.
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
References
1. United States Department of Health & Human Services, Administration for Children and Families, Administration on Children, Youth and Families, Children’s Bureau (2023). Child Maltreatment 2021. https://www.acf.hhs.gov/cb/report/child-maltreatment-2021 (accessed on 07/10/2023). [Google Scholar]
2. Caicedo, C. (2014). Families with special needs children: Family health, functioning, and care burden. Journal of the American Psychiatric Nurses Association, 20(6), 398–407 [Google Scholar] [PubMed]
3. Kolaitis, G. A., Meentken, M. G., Utens, E. M. W. J. (2017). Mental health problems in parents of children with congenital heart disease. Frontiers in Pediatrics, 8(5), 102. [Google Scholar]
4. Woolf-King, S. E., Anger, A., Arnold, W. A., Weiss, S. J., Teitel, D. (2017). Mental health among parents of children with critical congenital heart defects: A systematic review. Journal of the American Heart Association, 6(2), 1–14, e004862. [Google Scholar]
5. Ehrler, M., Wettach, C., Beck, I., Valsangiacomo Buechel, E. R., Latal, B. et al. (2023). Mental health-related quality of life in mothers of children with surgically repaired congenital heart disease: A 13-year longitudinal study. Quality of Life Research, 32, 2975–2986 [Google Scholar] [PubMed]
6. Kratz, L., Uding, N., Trahms, C., Villareale, N., Kieckhefer, G. (2009). Managing childhood chronic illness: Parent perspectives and implications for parent–provider relationships. Families, Systems and Health, 27, 303–313 [Google Scholar] [PubMed]
7. Landolt, M. A., Ystrom, E., Stene-Larson, K., Holmstrom, H., Vollrath, M. E. (2014). Exploring causal pathways of child behavior and maternal mental health in families with a child with congenital heart disease: A longitudinal study. Psychological Medicine, 44(16), 3421–3433 [Google Scholar] [PubMed]
8. Ayer, S., Bond, R., Webb, R., Miller, P., Bateson, K. (2019). Perinatal mental health and risk of child maltreatment: A systematic review and meta-analysis. Child Abuse and Neglect, 98, 104172. [Google Scholar]
9. Golfenshtein, N., Hanlon, A. L., Deatrick, J. A., Medoff-Cooper, B. (2017). Parenting stress in parents of infants with congenital heart disease and parents of healthy infants: The first year of life. Comprehensive Child and Adolescent Nursing, 40(4), 294–314 [Google Scholar] [PubMed]
10. Golfenshtein, N., Hanlon, A. L., Deatrick, J. A., Medoff-Cooper, B. (2020). The associations between infant development and parenting stress in infants with congenital heart disease at six and twelve months of age. Journal of Pediatric Nursing, 51, 1–7 [Google Scholar] [PubMed]
11. Carey, L. K., Nicholson, B. C., Fox, R. A. (2002). Maternal factors related to parenting young children with congenital heart disease. Journal of Pediatric Nursing, 17(3), 174–183 [Google Scholar] [PubMed]
12. McClung, N., Glidewell, J., Farr, S. L. (2018). Financial burdens and mental health needs in families of children with congenital heart disease. Congenital Heart Disease, 13(4), 554–562. https://doi.org/10.1111/chd.12605 [Google Scholar] [PubMed] [CrossRef]
13. Center for Nonprofit Management (2022). Community health needs assessment: Children’s hospital Los Angeles. https://www.chla.org/sites/default/files/2023-03/CHLA-2022-CHLA-CHNA-Report-final-version.pdf (accessed on 02/06/2023). [Google Scholar]
14. United States Census Bureau Quick Facts: Los Angeles City, California (2022). https://www.census.gov/quickfacts/fact/table/losangelescitycalifornia/PST045222 (accessed on 07/10/2023). [Google Scholar]
15. Stein, J. A., Andersen, R., & Gelberg, L. (2007). Applying the Gelberg-Andersen behavioral model for vulnerable populations to health services utilization in homeless women. Health Psychology, 12(5), 791–804. [Google Scholar]
16. Stein, J. A., Andersen, R. M., Robertson, M., Gelberg, L. (2012). Impact of hepatitis B and C infection on health services utilization in homeless adults: A test of the Gelberg-Andersen behavioral model for vulnerable populations. Health Psychology, 31(1), 20–30 [Google Scholar] [PubMed]
17. Andersen, R. M., Davidson, P. L., Baumeister, S. E. (2013). Improving access to care. In: Kominski, G. F. (Ed.Changing the U.S. health care system: Key issues in health services policy and management, 4th editionpp. 33–69. San Francisco, California, Jossey-Bass. [Google Scholar]
18. IBM Corp. Released (2021). IBM SPSS statistics for windows, version 28.0. Armonk, NY, IBM Corp. [Google Scholar]
19. Legano, L. A., Desch, L. W., Messner, S. A., Idzerda, S., Flaherty, E. G., Council on Child Abuse and Neglect, Council on Children with Disabilities. (2021). Maltreatment of children with disabilities. Pediatrics, 147(5), e2021050920 [Google Scholar] [PubMed]
20. Imperial-Perez, F., Pike, N. A., Eastwood, J., Doering, L., Heilemann, M. S. (2022). Caregiving for infants with single ventricle heart disease in the interstage period during COVID-19: A continuous process of compromise. World Journal for Pediatric & Congenital Heart Surgery, 13(4), 443–450. [Google Scholar]
21. Nayeri, N. D., Roddehghan, Z., Mahmoodi, F., Mahmoodi, P. (2021). Being parent of a child with congenital heart disease, what does it mean? A qualitative research. BMC Psychology, 9, 33 [Google Scholar] [PubMed]
22. Medoff-Cooper, B., Ravishankar, C. (2013). Nutrition and growth in congenital heart disease: A challenge in children. Current Opinion in Cardiology, 28, 122–129 [Google Scholar] [PubMed]
23. Williams, R. V., Zak, V., Ravishankar, C., Altmann, K., Anderson, J. et al. (2011). Factors affecting growth in infants with single ventricle physiology: A report from the pediatric heart network infant single ventricle trial. Journal of Pediatrics, 159, 1017–1022 [Google Scholar] [PubMed]
24. Feng, Y., Yu, D., Yang, L., Da, M., Wang, Z. et al. (2014). Maternal lifestyle factors in pregnancy and congenital heart defects in offspring: Review of the current evidence. Italian Journal of Pediatrics, 40, 85 [Google Scholar] [PubMed]
25. Proskynitopoulos, P. J., Heitland, I., Glahn, A., Bauersachs, J., Westhoff-Black, M. et al. (2021). Prevalence of child maltreatment in adults with congenital heart disease and its relationship with psychological well-being, health behavior, and current cardiac function. Frontiers in Psychiatry, 12, 686169 [Google Scholar] [PubMed]
26. Child Welfare Information Gateway (2020). Parental substance use as child abuse. https://www.childwelfare.gov/pubPDFs/parentalsubstanceuse.pdf (accessed on 07/15/2023). [Google Scholar]
27. Guttmacher Institute. (2023). Substance abuse during pregnancy. https://www.guttmacher.org/state-policy/explore/substance-use-during-pregnancy (accessed on 07/15/2023). [Google Scholar]
28. Atkins, D. N., Durrance, C. P. (2020). State policies that treat prenatal substance use as child abuse or neglect fail to achieve their intended goals. Health Affairs, 39(5), 756–763 [Google Scholar] [PubMed]
29. Canfield, M., Radcliffe, P., Marlow, S., Boreham, M., Gilchrist, G. (2017). Maternal substance use and child protection: A rapid evidence assessment of factors associated with loss of child care. Child Abuse & Neglect, 70, 11–27. [Google Scholar]
30. Tran, E. L., England, L. J., Park, J., Deny, C. H., Kim, S. Y. (2023). Systematic review: Polysubstance prevalence estimates reported during pregnancy, U.S., 2009–2020. Maternal and Child Health Journal, 27, 426–458 [Google Scholar] [PubMed]
31. Devyani Chowdhury, D., Johnson, J. N., Baker-Smith, C. M., Jaquiss, R. D. P., Mahendran, A. K. et al. (2021). Health care policy and congenital heart disease: 2020 focus on our 2030 future. Journal of the American Heart Association, 10(20), e020605 [Google Scholar] [PubMed]
32. Cohen, E., Kuo, D. Z., Agrawal, R., Berry, J. G., Bhagat, S. K. et al. (2011). Children with medical complexity: An emerging population for clinical and research initiatives. Pediatrics, 127(3), 529–538 [Google Scholar] [PubMed]
33. Bayer, N. D., Wang, H., Yu, J. A., Kuo, D. Z., Halterman, J. S. et al. (2021). A national mental health profile of parents of children with medical complexity. Pediatrics, 148(2), e2020023358. [Google Scholar]
34. Keeshin, B. R., Strawn, J. R., Luebbe, A. M., Saldana, S. N., Wehry, A. M. et al. (2014). Hospitalized youth and child abuse: A systematic examination of psychiatric morbidity and clinical severity. Child Abuse & Neglect, 38, 76–83. [Google Scholar]
35. Lauterbach, D., Armour, C. (2016). Symptom trajectories among child survivors of maltreatment: Findings from the longitudinal studies of child abuse and neglect (LONGSCAN). Journal of Abnormal Child Psychology, 44, 369–379 [Google Scholar] [PubMed]
36. Weber, S., Jud, A., Landolt, M. A. (2016). Quality of life in maltreated children and adult survivors of child maltreatment: A systematic review. Quality of Life Research, 25(2), 237–255 [Google Scholar] [PubMed]
37. Norman, R. E., Byambaa, M., De, R., Butchart, A., Scott, J. et al. (2012). The long-term health consequences of child physical abuse, emotional abuse, and neglect: A systematic review and meta-analysis. PLoS Medicine, 9(11), e1001349 [Google Scholar] [PubMed]
38. Lyons-Ruth, K., Wolfe, R., Lyubchik, A. (2000). Depression and the parenting of young children: Making the case for early preventive mental health services. Harvard Review of Psychiatry, 8, 148–153 [Google Scholar] [PubMed]
39. Miklush, L., Connelly, C. D. (2013). Maternal depression and infant development: Theory and current evidence. American Journal of Maternal Child Nursing, 38(6), 369–374 [Google Scholar] [PubMed]
40. SIu, A. L., Bibbins-Domingo, K., Grossman, D. C., Baumann, L. C., Davidson, K. W. et al. (2016). Screening for depression in adults: US preventive services task force recommendation statement. Journal of the American Medical Association, 315, 380–387 [Google Scholar] [PubMed]
41. Parkhurst, J. T., Friedland, S. (2020). Screening for mental health problems in pediatric primary care. Pediatric Annals, 49(10), e421–e425 [Google Scholar] [PubMed]
42. Kerker, B. D., Storfer-Isser, A., Stein, R. E., Garner, A., Szilagyi, M. et al. (2016). Identifying maternal depression in pediatric primary care: Changes over a decade. Journal of Developmental and Behavioral Pediatrics, 37(2), 113–120 [Google Scholar] [PubMed]
43. Wiener, L., Kazak, A. E., Noll, R. B., Patenaude, A. F., Kupst, M. J. (2015). Standards for the psychosocial care of children with cancer and their families: An introduction to the special issue. Pediatric Blood and Cancer, 62(suppl 5), S419–S424 [Google Scholar] [PubMed]
44. Coulton, C. J., Crampton, D. S., Irwin, M., Spilsbury, J. C., Korbin, J. E. (2007). How neighborhoods influence child maltreatment: A review of the literature and alternative pathways. Child Abuse & Neglect, 31(11–12), 1117–1142. [Google Scholar]
45. Maguire-Jack, K., Font, S. A. (2017). Community and individual risk factors for physical child abuse and child neglect: Variations by poverty status. Child Maltreatment, 22(3), 215–226 [Google Scholar] [PubMed]
46. Maguire-Jack, K., Sattler, K. (2023). Neighborhood poverty, family economic well-being, and child maltreatment. Journal of Interpersonal Violence, 38(5–6), 4814–4831 [Google Scholar] [PubMed]
47. Dettlaff, A. J., Boyd, R. (2020). Racial disproportionality and disparities in the child welfare system: Why do they exist, and what can be done to address them? The ANNALS of the American Academy of Political and Social Science, 692(1), 253–274. [Google Scholar]
48. Hoynes, H. W., Schanzenbach, D. W. (2018). Safety net investments in children. https://www.brookings.edu/wp-content/uploads/2018/03/HoynesSchanzenbach_Text.pdf (accessed on 07/10/2023). [Google Scholar]
49. Schnitzer, P. G., Slusher, P. L., Kruse, R. L., Tarleton, M. M. (2011). Identification of ICD codes suggestive of child maltreatment. Child Abuse & Neglect, 5(2011), 3–17. [Google Scholar]
50. Bautista-Durand, M., McLaughlin, C. M., Imagawa, K. K., Upperman, J. S., Jensen, A. R. (2019). Identifying targets to improve coding of child physical abuse at a pediatric trauma center. Journal of Trauma Nursing, 26(5), 239–242. [Google Scholar]
Cite This Article
 Copyright © 2023 The Author(s). Published by Tech Science Press.
Copyright © 2023 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools