 Open Access
Open Access
ARTICLE
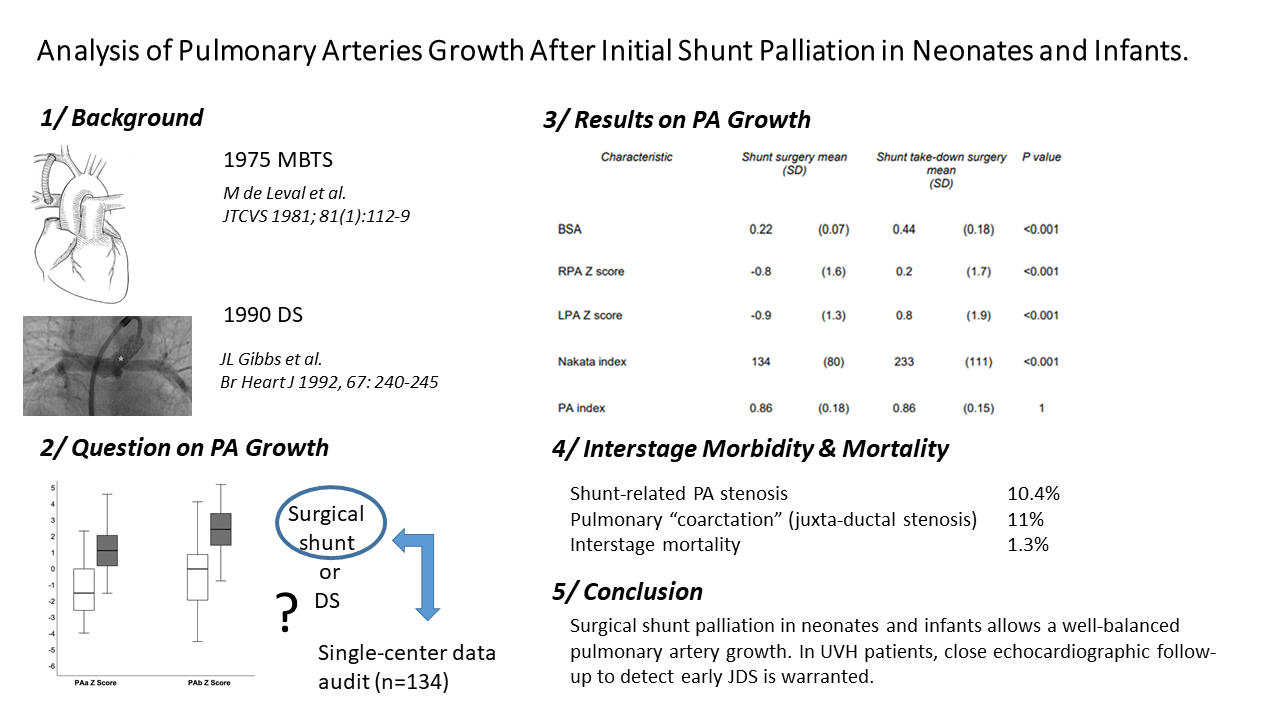
Analysis of Pulmonary Arteries Growth after Initial Shunt Palliation in Neonates and Infants
1 Department of Cardiovascular and Thoracic Surgery, Université catholique de Louvain (UCLouvain)—Cliniques Universitaires Saint-Luc, Brussels, B-1200, Belgium
2 Department of Pediatric Cardiology, Université catholique de Louvain (UCLouvain)—Cliniques Universitaires Saint-Luc, Brussels, B-1200, Belgium
3 Department of Anesthesiology, Université catholique de Louvain (UCLouvain)—Cliniques Universitaires Saint-Luc, Brussels, B-1200, Belgium
4 Department of Pediatric Intensive Care, Université catholique de Louvain (UCLouvain)—Cliniques Universitaires Saint-Luc, Brussels, B-1200, Belgium
* Corresponding Author: Alain J. Poncelet. Email:
# Co-first authors
Congenital Heart Disease 2023, 18(5), 525-537. https://doi.org/10.32604/chd.2023.042341
Received 26 May 2023; Accepted 07 August 2023; Issue published 10 November 2023
Abstract
Objective: Despite increasing enthusiasm for neonatal repair, patients with ductal-dependent circulation (pulmonary/systemic) or restrictive pulmonary blood flow still require initial palliation. Ductal stenting has emerged as an endovascular approach whereas modified-Blalock-Taussig and central shunt remain surgical references. In this study, we analyzed the relationship between pulmonary artery growth, sites of shunt connection, or antegrade pulmonary blood flow in surgically placed shunts. The need for secondary catheter-based interventions or pulmonary arterioplasty was also investigated. Methods: A retrospective single-center study analyzing 175 patients undergoing surgery for a central or modified-Blalock-Taussig shunt. Outcome growth variables were right pulmonary artery/left pulmonary artery diameters/Z scores, the indexed sum area (right pulmonary artery + left pulmonary artery), and the pulmonary symmetry index. Three imaging modalities were used: angiography, computed tomography, and echocardiography. Results: At baseline, pulmonary arteries were larger in patients with antegrade pulmonary blood flow (Nakata index 137 vs. 114, p = 0.047) as well as in patients receiving a modified-Blalock-Taussig shunt (Nakata index 138 vs. 84, p < 0.001). At the time of shunt takedown, both the right pulmonary artery and left pulmonary artery had normalized their diameter. The Nakata index increased from 134 to 233 mm2/m2 (p < 0.001). The pulmonary artery index remained stable (0.86) over time. During the inter-stage period, shunt-related pulmonary artery stenosis and juxta-ductal stenosis were diagnosed in 16 (10%) and 17 patients (11%), respectively. Conclusions: Surgical shunt palliation allows normal pulmonary artery growth. Pulmonary artery stenosis was either shunt-related (10%) or secondary to juxta-ductal stenosis (11%). Close echographic follow-up allows early diagnosis and treatment of juxta-ductal stenosis.Graphic Abstract
Keywords
Supplementary Material
Supplementary Material FileCite This Article
 Copyright © 2023 The Author(s). Published by Tech Science Press.
Copyright © 2023 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools