 Open Access
Open Access
ARTICLE
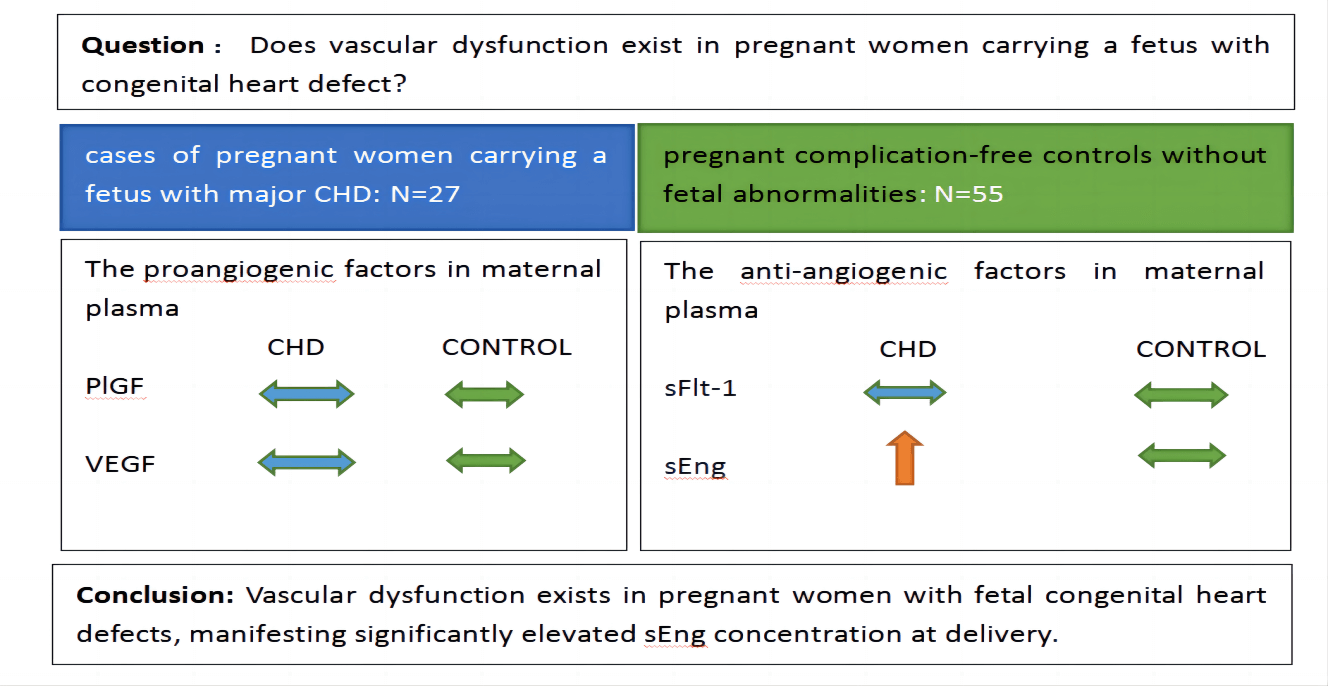
Maternal Vascular Dysfunction in Congenital Heart Defects
1 Department of Obstetrics and Gynecology, Nanfang Hospital, Southern Medical University, Guangzhou, 510515, China
2 Department of Obstetrics and Gynecology, Guangdong Provincial People’s Hospital (Guangdong Academy of Medical Sciences), Southern Medical University, Guangzhou, 510080, China
3 Prenatal Diagnosis Centre, Guangdong Provincial People’s Hospital (Guangdong Academy of Medical Sciences), Southern Medical University, Guangzhou, 510080, China
4 Department of Cardiovascular Surgery, Guangdong Cardiovascular Institute, Guangdong Provincial People’s Hospital (Guangdong Academy of Medical Sciences), Southern Medical University, Guangzhou, 510080, China
5 Global Health Research Center, Guangdong Cardiovascular Institute, Guangdong Provincial People’s Hospital (Guangdong Academy of Medical Sciences), Southern Medical University, Guangzhou, 510080, China
* Corresponding Authors: Haiping Wang. Email: ; Liping Huang. Email:
Congenital Heart Disease 2023, 18(5), 561-570. https://doi.org/10.32604/chd.2023.030511
Received 10 April 2023; Accepted 07 August 2023; Issue published 10 November 2023
Abstract
Background: Research on fetal congenital heart defect (CHD) mostly focuses on etiology and mechanisms. However, studies on maternal complications or pathophysiology are limited. Our objective was to determine whether vascular dysfunction exists in pregnant women carrying a fetus with congenital heart defects. Methods: We conducted a case-control study. 27 cases of pregnant women carrying a fetus with major CHD admitted to our hospital for delivery between April 2021 and August 2022 were selected. Every case was matched with about 2 pregnant complication-free controls without fetal abnormalities. The proangiogenic and anti-angiogenic factors and pregnancy outcomes were compared. Results: The proangiogenic factors include vascular endothelial growth factor (VEGF) and placental growth factor (PlGF). The anti-angiogenic factors involve soluble fms-like tyrosine kinase 1 (sFlt-1) and soluble endoglin (sEng). No differences were found in maternal plasma concentrations of PlGF, VEGF, and sFlt-1 between case-control groups when analyzed at 36 weeks ≤ gestational age (GA) < 39 weeks and 39 weeks ≤ GA ≤ 41 weeks. The concentrations of sEng in maternal plasma in the fetal CHD group were significantly higher than those in the control group: 0.60 (0.77) vs. 0.32 (0.26) ng/ml at 36 weeks ≤ GA < 39 weeks, p = 0.001 and 0.75 (0.55) vs. 0.28 (0.27) ng/ml at 39 weeks ≤ GA ≤ 41 weeks, p < 0.001. Conclusion: Vascular dysfunction exists in pregnant women with fetal congenital heart defects, manifesting significantly elevated sEng concentration at delivery.Graphic Abstract
Keywords
Cite This Article
 Copyright © 2023 The Author(s). Published by Tech Science Press.
Copyright © 2023 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools