 Open Access
Open Access
ARTICLE
Intraoperative Blood Glucose Levels and Postoperative Acute Kidney Injury in Pediatric Patients Having Congenital Heart Surgery under Cardiopulmonary Bypass
1 Department of Anesthesiology, Fuwai Hospital, National Centre for Cardiovascular Diseases, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, China
2 Department of Anesthesiology, Fuwai Hospital, Chinese Academy of Medical Sciences, Shenzhen, China
3 Department of Anesthesiology, Peking Union Medical College Hospital, Beijing, China
* Corresponding Authors: Jianhui Wang. Email: ; Fuxia Yan. Email:
# Contributed equally as co-first authors
Congenital Heart Disease 2023, 18(4), 475-488. https://doi.org/10.32604/chd.2023.028017
Received 22 November 2022; Accepted 21 May 2023; Issue published 15 September 2023
Abstract
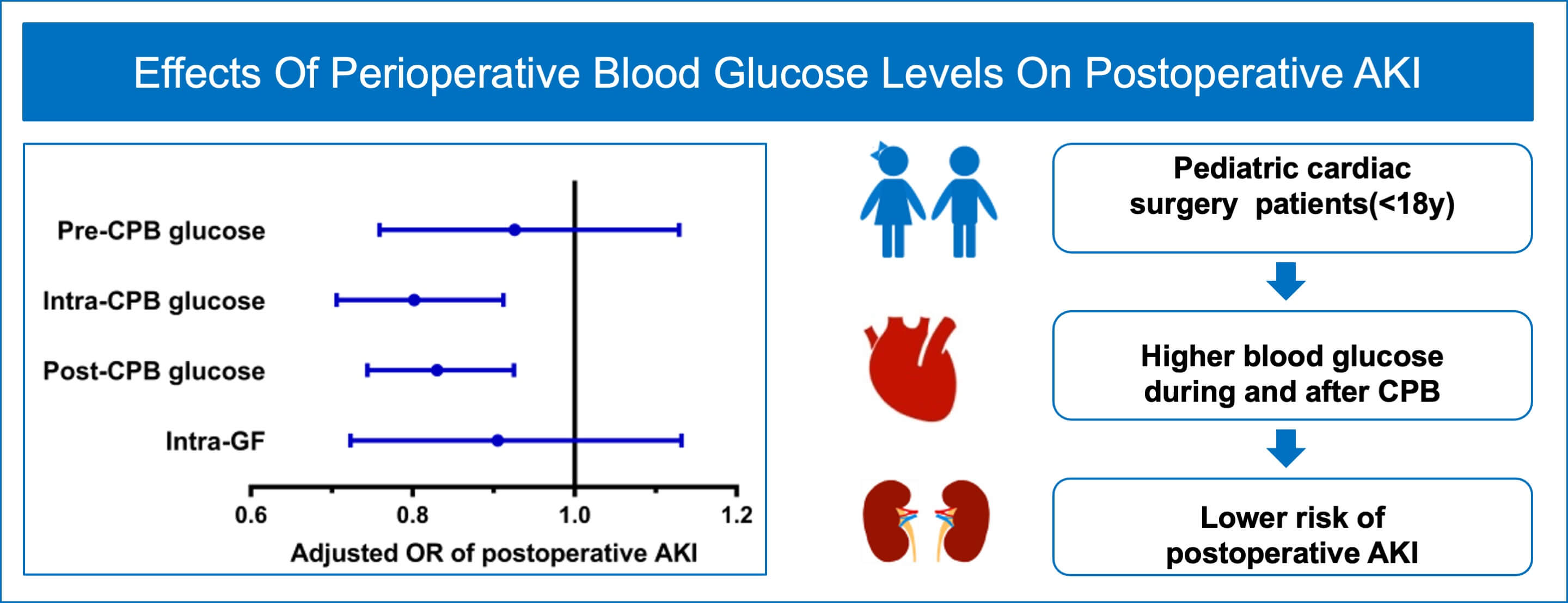
Purpose: This study sought to explore the effect of intraoperative mean blood glucose levels and variability on postoperative acute kidney injury (AKI) in children undergoing congenital cardiac surgery. Methods: We conducted a prospective nested case-control study in children (age < 18 years) undergoing congenital heart surgery with cardiopulmonary bypass (CPB) at the Fuwai Hospital between April 01, 2022 and July 30, 2022. Cases were individuals who developed AKI within the first postoperative 7 days (AKI group) and controls were those without AKI (Non-AKI group) according to KDIGO criteria. AKI and Non-AKI groups unmatched and 1:1 matched by age, sex, and baseline serum creatinine were separately analyzed. Multivariate logistic and conditional logistic regressions were used to assess the associations between blood glucose variables and AKI. Results: 688 consecutively approached patients were included in the final analysis. On multivariate analysis, intra-CPB (adjusted odds ratio [OR] 0.802; 95% confidence interval [CI], 0.706 to 0.912; p = 0.001) and post-CPB (adjusted OR 0.830; 95% CI, 0.744 to 0.925; p = 0.001) blood glucose levels were associated with postoperative AKI. There were no significant differences in pre-CPB blood glucose (adjusted OR 0.926; 95% CI, 0.759 to 1.129; p = 0.446) or intraoperative glycemic fluctuations (adjusted OR 0.905; 95% CI, 0.723 to 1.132; p = 0.382) between AKI and Non-AKI groups. Results based on matched cases and controls were consistent with those from the unmatched analyses. Conclusion: Higher intraoperative blood glucose levels during and after CPB were protective factors against postoperative AKI in pediatric patients after congenital heart surgery.Graphic Abstract
Keywords
Cite This Article
 Copyright © 2023 The Author(s). Published by Tech Science Press.
Copyright © 2023 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools