 Open Access
Open Access
ARTICLE
“I Dread the Heart Surgery but it Keeps My Child Alive”—Experiences of Parents of Children with Right Ventricular Outflow Tract Anomalies during the Assessment for Cardiac Reoperation
1 Department of Cardiology, Pediatric Heart Center, Skåne University Hospital, Lund, Sweden
2 Department of Clinical Sciences Lund, Pediatrics, Lund University, Lund, Sweden
3 Department of Care Science, Faculty of Health and Society, Malmö University, Malmö, Sweden
4 Department of Paediatrics, The Queen Silvia Children’s Hospital, Gothenburg, Sweden
5 The Department of Health Sciences, University West, Trollhättan, Sweden
* Corresponding Author: Birgitta Svensson. Email:
Congenital Heart Disease 2023, 18(3), 349-359. https://doi.org/10.32604/chd.2023.028391
Received 15 December 2022; Accepted 29 March 2023; Issue published 09 June 2023
Abstract
Background: Parents of children with complex right ventricular outflow tract (RVOT) anomalies are confronted with their child’s need for heart surgery early in life and repeated reoperations later on. Preoperative assessment needs to be performed whenever an indication for reoperation is suspected. The aim was to illuminate the experiences of parents of children diagnosed with RVOT anomalies, in particular, how they experience their child’s heart disease and everyday life during the assessment and after the decision on whether to perform a reoperation. Method: Individual interviews (n = 27) were conducted with nine parents on three occasions between 2014 and 2016 and analyzed using reflexive thematic analysis. Results: The analysis resulted in the following five main coexisting themes: The heart surgery keeps my child alive illuminates parents’ experiences during and after the assessment and emphasizes that heart surgery, although dreaded, is central for their child’s survival; Everyday struggles illuminates the different struggles parents had to face to ensure that their child would be in the best possible condition; the remaining three themes, Unconditional love, Trust in life, and Togetherness, illuminate the ways in which the parents gained inner strength and confidence in their everyday lives. Conclusion: Although the parents were grateful for the assessment and had learned to navigate among the fears it aroused, they experienced several distressing situations during the assessment process that should be addressed. By inviting both the parents and their child to participate in the child’s care, individualized support can take into account the needs of both parents and child.Keywords
Parents of children with complex right ventricular outflow tract (RVOT) anomalies, such as tetralogy of Fallot (TOF), double outflow of right ventricle (DORV), and common arterial trunk (CAT), are confronted with their child’s need for surgery early in life and reoperations later on. Preoperative assessment including multiple clinical and imaging procedures needs to be performed whenever an indication for reoperation is suspected [1]. Previous research has shown that parents of children with different types of congenital heart disease (CHD) report more stress, depression, and anxiety than parents of healthy children or parents of children with other diseases [2–4]. In addition, previous research has shown that both the waiting time before heart surgery and the hospitalization for the surgery are major sources of stress for parents of younger children with CHD [5–8]. This applies to the whole family, which has to adapt to this trauma and disruption to family life during this time [8]. The repeated assessment for children with RVOT anomalies can guide the need for reoperation, so it is important to be aware of how parents experience this period of uncertainty, from the start of the assessment until they receive a decision about their child’s need for further surgery. How their children experience everyday life during and after this assessment, has been described in a recently published study by our group [9] which showed that the children’s fear of surgery was awoken at the start of the assessment; however, this fear had no impact on their everyday life until the decision about the need for reoperation. To the best of our knowledge, this is the first study to explore the experiences of everyday life for parents of children with RVOT anomalies during a period covering the preoperative assessment through the decision making and after reoperation, when the last interview was conducted. A better understanding of the parents’ experiences is one way for health care providers to gain insights into how to improve the support given to parents [2,6]. Thus, the aim of this study was to illuminate how these parents experienced their children’s heart disease and everyday life during this assessment and after the decision on whether to perform a reoperation.
An inductive design with a constructionist approach [10] was chosen to capture the parents’ experiences, using semi-structured individual interviews at three different data collection times. A constructionist approach in this context means that the parents’ experiences, obtained herein via interviews, are used to construct particular realities which will become the focus of research [10]. All the collected data were analyzed using reflexive thematic analysis following Braun et al. [11–13], a method that allows the researcher to interpret the meaning behind the words expressed by the interviewees. When using thematic analysis (TA), according to Braun and Clarke, it is important to decide which branch of TA, coding reliability, codebook or reflexive approach is suitable for the study [12]. A reflexive TA requires time and space for both immersion of engagement in the data and distancing [13].
2.2 Procedure and Participants
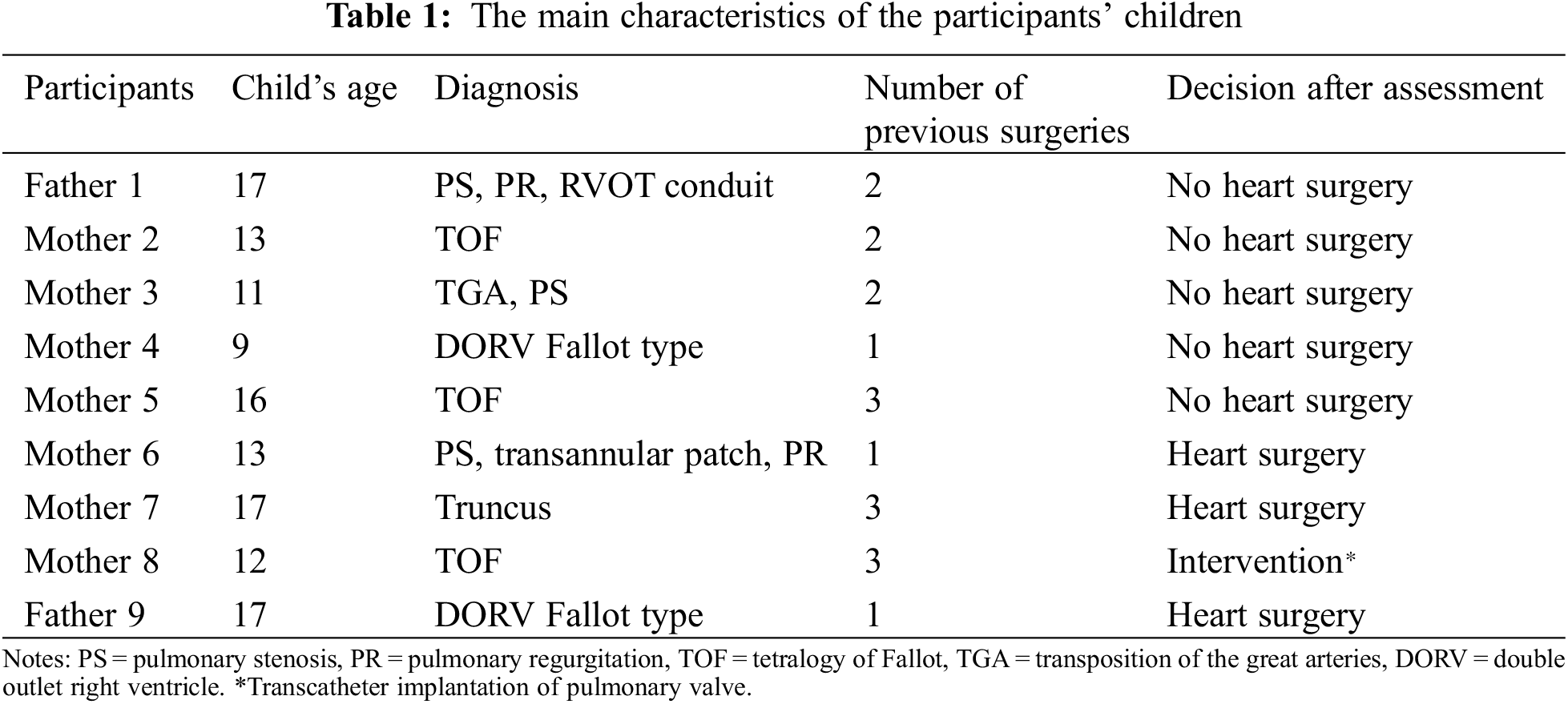
Nine parents participated in the study. Their children were 9–17 years of age (Table 1). The inclusion criteria were being a parent of a child aged between 9 and 18 years with a diagnosis of RVOT anomalies who had undergone a surgically repaire and completed an MRI examination to assess the need for pulmonary valve replacement. The exclusion criteria were parents of children unable to speak and understand Swedish or unable to participate in an interview situation due to cognitive impairment. The parents of 15 children were eligible to participate in the study. Of these, the parents of 6 children declined to participate either due to the lack of time given the child’s school load or in order to spare the child from knowing about the need for eventual reoperation. All the parents were invited by two nurses at two university hospitals in Sweden. After having been given oral and written information about the study, the parents were given some time to consider their possible participation. The nine parents who gave their written informed consent to participate were then contacted by the first author (BS), who provided further information if needed. The participants had not had contact with BS outside of this study.
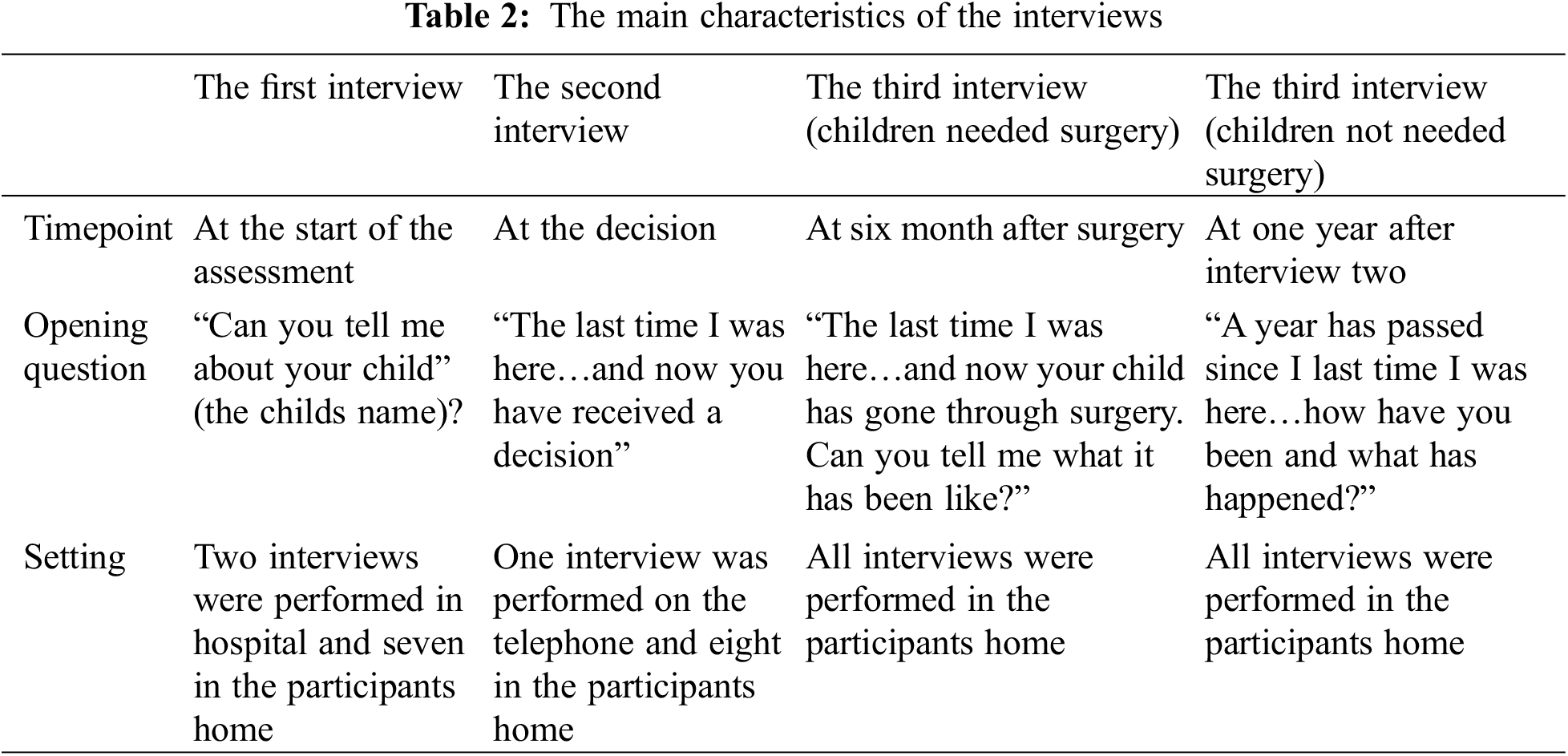
A semi-structured interview guide was developed based on a literature review focusing on the research aim. Central issues in the interview guide were: (1) the parents’ experiences of everyday life during and after their child went through an assessment and received a decision about whether or not heart surgery was necessary, (2) experiences of their child’s heart disease and heart surgeries, (3) its impact on the whole family’s everyday life, and (4) their thoughts about their child’s leisure, schooldays, and future. Follow-up questions such as: How did you feel? Can you describe it? were asked to elicit in-depth responses. All interviews were conducted by the first author (BS) and digitally recorded after the approval of the participants. All three interviews (Table 2) lasted from 86 to 169 min per participant (median 135 min). At the end of the interview all participants were asked whether there was something else they wanted to tell the interviewer and asked how they felt after having participated in the interview. The rationale for doing this was to identify any participants who were affected negatively by the interview and in need of professional support. Lastly, the parents received a contact number of a psychologist in case they needed such support.
The data were analyzed using reflexive thematic analysis according to Braun et al. [11–13], in which the researcher plays an active part in the process of producing knowledge. “The analytic process involves immersion in the data, reading, reflecting, questioning, imagining, wondering, writing, retreating, and returning” [14]. The analysis started with a phase of familiarization which was performed by BS, who had transcribed all the interviews. The first reflections were written down immediately after the interviews and further reflections were written when the interviews were in verbatim transcripts. The familiarization continued with BS reading through the whole dataset on two occasions with an open curious mind and at the same time making casual notes shaped by the research question. During the second phase, codes were generated. This was a more active phase of systematically identifying meanings in the whole dataset. The codes were at first semantic, which mean they were identified and described at a surface meaning of the data, [11] but became more latent as the coding progressed. The codes were written in a table, together with extracts from the dataset and were sorted manually. The third phase consisted of a theme development process, where the themes were developed from the generated codes. Building themes was an active analysis phase and gave meaning at the intersection of the data, the research question, and the researchers’ experience and subjectivity. In the fourth and fifth phase, the themes were revised, defined, and checked against the whole dataset. A thematic map was created to show how the themes interacted and what overarching story they told. At first, the thematic map included many candidate themes which finally emerged as five coexisting themes. The sixth phase started when the report was produced and was the final test of how the themes worked, both on an individual level with the dataset but also on an overall level. The candidate themes were reworked and refined by BS in consultation with co-authors MB and AW, and in the last phase also with PL. To ease the reading of the quotes, all hesitations and repetitions were removed. Where more than just hesitations and repetitions have been removed, this is indicated in the quotes below by (…); this has only been done where it did not alter the meaning in accordance to Braun et al. [10].
The interviewer BS has a long experience within pediatric cardiology and has, as a nurse, extensive experience of interacting with parents in different care situations. A reflexivity journal was created at the beginning of the interviews and kept throughout the whole procedure, which further facilitated a questioning, reflexive thinking. According to Lincoln et al. [15] transferability was promoted by describing the settings and the participant characteristics and dependability was enhanced by the fact that only one interviewer (BS) conducted all the interviews. In addition, rigor was enhanced by using Braun et al.’s 15-point checklist of criteria for good thematic analysis [11].
The analysis produced five main coexisting themes (Fig. 1). The first theme, the heart surgery keeps my child alive, illuminates parents’ experiences during and after the assessment for reoperation, which is a recurrent event in their child’s life. It emphasizes that the heart is central for their child’s survival and that it needs to be monitored. The second theme, Everyday struggles, illuminates the different struggles parents had to face in order to provide their child with the best possible conditions in everyday life. The other three themes, Unconditional love, Trust in life, and Togetherness, illuminate how and in what way the parents gain inner strength and confidence in their everyday life.
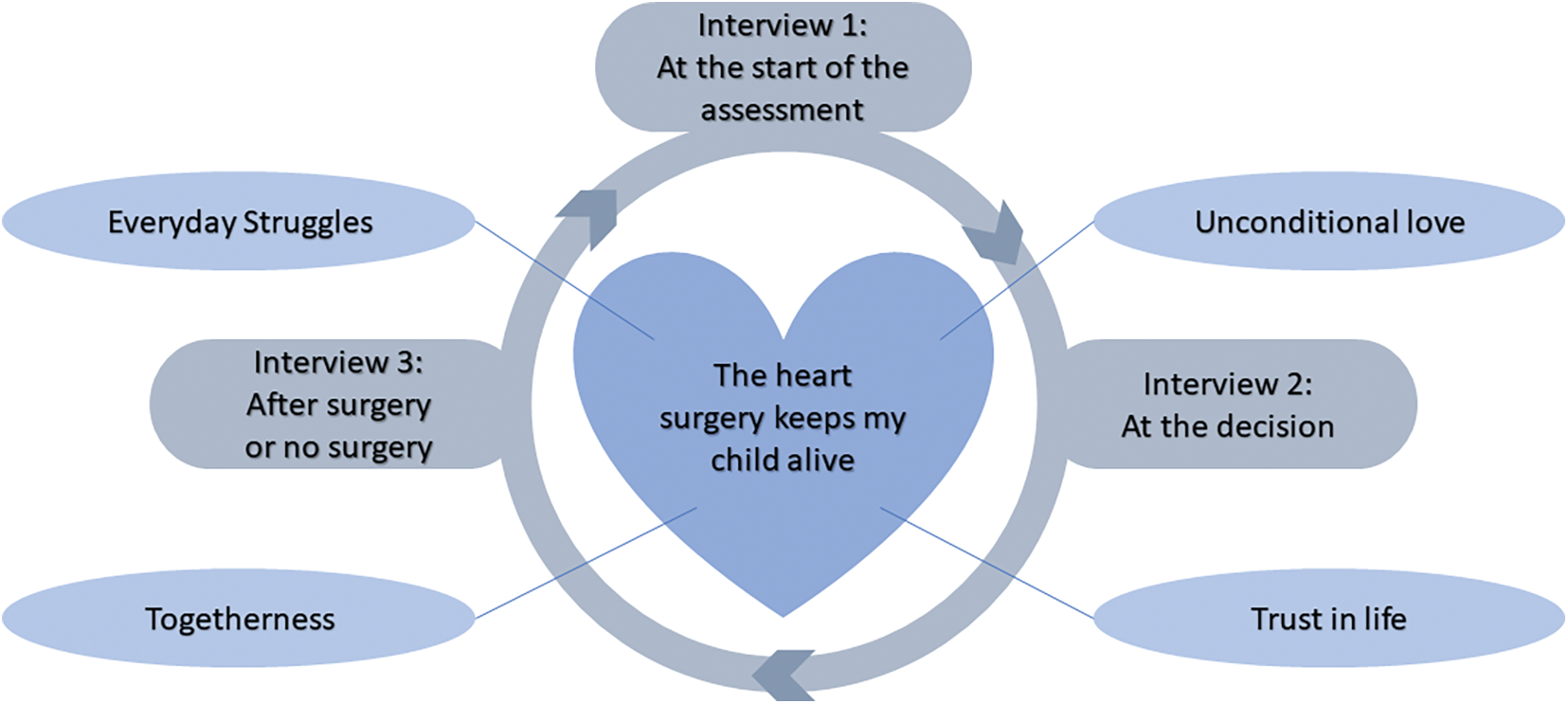
Figure 1: Thematic map of the dataset
3.1 The Heart Surgery Keeps My Child Alive
Even though the assessment was a period when both worries that the child might need a reoperation and memories of previous operations came to life, the parents found it reassuring that their child’s heart was being closely monitored, since a well-functioning heart kept the child alive. The greatest fear for the parents was to lose their child or that the reoperation may lead to complications that would leave their child disabled and unable to live life as before. They were worried about how many times their child could safely be operated on. As one parent expressed it, “It is heartbreaking that they continue to put her at risk through more operations”(M4), but at the same time they were aware that the surgery had improved their child’s heart, which was a prerequisite for life itself. The parents of children who did not need surgery were aware that the heart valve had lasted so much longer than they were initially told, which meant that every day was a day closer to the future surgery. The outcome of the assessment, the decision that a reoperation was either necessary or not necessary, was communicated to the parents by phone, letter, or in one case at a hospital visit. The parents thought it would have been easier if they could receive the decision face to face and felt that all family members should receive the same information, especially if the decision was for heart surgery.
For those parents whose children did not feel the need of reoperation, the time leading up to the operation could be dominated by managing the child’s heightening fear of dying as the time for the surgery approached. The waiting time between the decision and the surgery was also described as being on endless constant alert, including always having the phone within reach in case someone from the hospital should call. The parents commented that a shorter waiting time would have made it much easier for them. When the time for surgery arrived, the real world outside disappeared as soon as they entered the hospital world. The parents gave accounts of unexpected clinical situations in connection with the operations, which did not turn out as planned. Some of these accounts reflected the parents’ feeling of insufficient information from the health care providers before the surgery.
Most of the parents’ struggles in their everyday life took place in school, where they had to fight for their child’s rights, for example by highlighting that school scheduling needed to include breaks or by repeatedly pointing out the child’s need for support to be able to manage a full day. The parents’ everyday life also included other kinds of struggles, such as preparing the child for a hospital visit or helping the child with endurance issues. For themselves it could involve managing anxiety far beyond the usual parental worries. The parents described needing a huge inner strength sometimes to help their child, for example when helping the child to calm down after a panic attack before an examination in the hospital or when answering difficult questions, for example, whether the child was going to die during surgery. They felt they had no instruction manual, instead they had to trust their intuitive feelings about how to handle such situations. “I just feel it was pure instinct, that it has to be now or she will be in despair if she knows it (the MRI) won’t be done (M5)”. The parent felt they should always be there and do everything for their child, even if the situations and challenges sometimes made them feel either inadequate or powerless as a parent.
You feel so powerless, you don’t quite know what to do, it’s not something you can do by yourself, well of course you can support, encourage and cheer them up and all this that I do and give a lot of warmth and love and this that is needed (…) I feel inadequate, I don’t know what to do, I wish I could do something, that I could just conjure, use magic, anything to be able to take this away (M4).
When the parents reflected over future surgery, they faced a new challenge compared to earlier surgeries. Their child was now older with an increased awareness and therefore needed to be prepared in a different way. At the same time, they had to take care of their own worries and protect their child from those worries. Parents appreciated it when the health care providers addressed the child directly, and they wanted help in mentally preparing their child for surgery or explaining heart disease at the child’s level of understanding.
The parents’ unconditional love originated from the time when they could have lost their newborn child. They remembered moments containing an emotional mix of heartfelt joy, great fear, love, and an almost overwhelming gratitude. The parents’ worst memories were of the child being handed over to the anesthesiologist, when the child was baptized before the operation, or when they were not able to hold their child before the transfer to the operating table, and these memories were still, many years later, etched in their consciousness. Their feelings of gratitude were aroused when they understood that their child’s heart disease could be treated and also when seeing that there were others who were worse off than themselves. When they looked back, they saw a distressing time, but their child was alive, so the outcome was good. Parents talked of the closeness they felt to the child with heart disease and how this child was dear to their heart in a different way than the child’s siblings, even though they did not love this child more than their other children.
She becomes like a ‘child of the heart’ they are called and you become very close to each other, you do. Although I have children before who are also dear to me but it becomes a bit special precisely when they are so small from the beginning (F1).
Unconditioned love was evident in how the parents described their child’s personality and their relationship. Together with that love and the child’s joie de vivre, positive outlook, fighting spirit, and inner strength, the parents themselves gained inner strength and confidence. The parents expressed relief that their child still felt so well, and it became apparent that the child’s health status had an impact on the parents’ wellbeing, so when their child was well, the parents were well.
The parents’ experienced a trust in life, and with that comes an acceptance of how everything has become as it is now. It had also given them a further insight that life is fragile and cannot be taken for granted. The parents revealed that time had shown the impossible to be possible, when getting used to the thought that their child would require several operations in life.
Being used to it did not mean that the parents were free from worries. Their best coping strategy was to postpone the anxiety until later, when it was time for surgery. Trust in and gratitude to the health care staff facilitated this procedure. The experience of feeling well treated by the health care providers was something the parents had in common, and it gave them a feeling of comfort and security. “In addition to their professional knowledge there is a heart so they are interested, really interested in people”(F9). The parents’ feeling of trust extended to their child’s future: they saw the future path as bright, even though there were worries in the far distance. Nevertheless, it was important to the parents that their child should enjoy life and find happiness in the here and now and be able to follow his or her dreams.“But I think his best time is actually ahead of him”(M7). This trust in life itself and in their child gave them the strength to deal with difficulties on their way through life.
The feeling of togetherness was an important source of strength in the parents’ everyday life. Togetherness was on the whole a feasible option for coping with having a child with heart disease. Support from other people, to be able to share the burden was invaluable. Talking to others, either a partner, friend, or workmate, was the most common way of feeling less alone and being helped through difficulties. Sharing with others who were in a similar situation felt especially meaningful, since a basic understanding already existed, and at the same time it became a way of processing their own experiences. Parents expressed the importance of building a network consisting of close friends, family, and specialists around themselves but also around their child. “Make a network, build a network around yourself to be able to handle this because you can’t handle everything yourself, you can’t” (M6).
Another form of togetherness was illustrated by having faith in God, praying and knowing that others were praying for them, which was a source of strength and hope. The most important kind of togetherness was to have the family close; in the arms of the family, both the parents and their child could rest and gain strength. The child with heart disease brought the family closer, even if the journey started with navigation in unknown waters.
Parents of children with complex RVOT anomalies are aware that their child will need reoperations but they live with an uncertainty of when this will happen. Since the majority of these children will undergo pulmonary valve replacement, MRI along with other imaging and clinical investigations are often used in order to best assess the need for reoperation [16]. The results of the present study showed that the parents were grateful for this assessment since it provided a thorough check-up of their child’s heart. Dormant fears and new worries were awakened about whether their child would have to undergo a reoperation, but they had learned to navigate through them. They described critical situations, such as how the clinical decision after the assessment was presented to them and the period of waiting for the heart surgery after a decision for reoperation. The results also showed how the parents viewed their bond to their children, how they were coping with a range of challenges, and what they needed in order to ease the burden of having a child going through surgery while at the same time holding themselves together.
A previous study with parents to children with a specific complex CHD, namely single ventricle, showed that the parents experienced the last surgical palliation as a transition point [17]. For parents of children with complex RVOT anomalies, there is no “final surgery”, as their children typically need reoperations throughout their lifetime. This need for repeated operations, that the child will never be free of the fear of surgery, is a challenge for the parents. This challenge may have contributed to an adaptation process, perhaps facilitated by their child’s inner strength and well-being thus far [9]. They had adapted to and developed strategies for suppressing their worries and anxiety until the more critical situations, especially when a reoperation become a reality. A previous study showed that although mothers managed to get rid of their fear and anxiety one year after their child’s surgery, they still had a feeling of lack of control [18]. In the present study, six month after surgery, the parents experienced relief and strength with traces of adaptation. We have earlier shown that their children adapted to managing their heart disease in their everyday life and could cope with the knowledge that future heart surgeries were likely [9]. An adaptation and development of strategies for managing the child’s CHD is shown to be essential to coping for parents too [3], and this adaptation process may affect their need for support which could be valuable information for the health care providers.
When the parents in the present study entered the hospital for the child’s heart surgery, the real world outside disappeared and their whole focus was on their child. Hospitalization in connection to surgery has been recalled in previous studies as being a situation when parents needed to employ additional strategies or support [19] and a time when parents experienced a constant level of stress during the whole hospital stay [20] and even beyond [21]. In order to ease the burden, it has been shown that providing thorough preoperative information could make the hospitalization less traumatic [22]. Such aspects of care would likely have facilitated the hospitalization period for the parents in the present study. It is also worth noting the finding in that study that parents of children undergoing heart surgery had higher levels of anxiety before their child’s surgery than for parents of children undergoing other surgeries [22].
The parents unconditional love and closeness were characteristic of the parents’ relationship with their child and may derive from the time of the child’s birth, diagnosis, and early heart surgery, when the parents faced their worst fear: the possibility of losing their child. Unconditional love as a source of strength has not been found in previous research, but similar findings of closeness related to a stronger bonding during hospital stays have been reported [23]. The vital bonding between child and parents [19] is a prerequisite for this unconditional love and may take place in the hospital, although bonding may be more difficult in the context of a hospital stay with an infant [23]. With this in mind, health care providers should aim to facilitate and strengthen this bonding process. A previous study [24] showed that being interviewed helped mothers to infants to cope with the stress connected with their infants surgery. They suggest therefor a mental health professional to assist the mothers to tell their story.
The parents in this study gained strength from togetherness which also included the strength they drew from praying or having faith in something bigger than themselves. The fact that faith has a positive role and could be one way of gaining inner strength has been shown in previous studies with parents of children with CHD [6,19,25]. In one study, where most of the recruited parents of infants with CHD had clear religious beliefs, the parents experienced that those beliefs had a protective effect against anxiety, reduced their care burden, and further improved their quality of life [26]. In a secular country like Sweden, health care providers may need to have an open mind to consider faith as a resource that can give parents inner strength; and they should thus support and facilitate the parents in drawing on their faith.
The present study shows that there is a need for a lifelong follow-up with individualized support to meet the challenges, such as to prepare their child for heart surgery when he or she is older and has new questions and fears. This was seen to be especially hard when the child did not feel any need for reoperation, and the parents felt relieved when the health care providers turned directly to their child. A child-centered approach [27] within health care, taking both the child perspective, meaning the parents’ view of their child’s experiences, and the child’s own inner perspective, would be ideal. By inviting both the parents and their child to participate from the start of the assessment, the decision may be delivered according to the parents’ and their child’s wishes. Additionally, their individual needs during the time from the decision to the surgery may then be taken care of. Previous studies have shown that the waiting time for heart surgery is stressful for the parents [7,8,28] and also that the parents want to participate in their child’s care [29]. There can be obstacles in health care to the participation of children, and in order to remove these obstacles, health care providers have to discuss and reflect upon their attitudes to children’s participation in their own care [30].
Although the parents were grateful for the assessment and had learned to navigate among the fears it aroused, they experienced several stressful situations during the assessment process that must be addressed. By understanding the parents’ experiences and their sources of inner strength, health care providers can better aid the parents to cope with the experience. Furthermore, by inviting both the parents and their child to participate in the child’s care, an individualized support that takes into account both the parents’ and the child’s needs can be created.
More studies are needed to further explore the experiences of parents of children with these and other types of complex congenital heart disease in order to enable healthcare providers to tailor the way the decision making is shared with these families.
The small sample size could be regarded as a limitation; however, in thematic analysis, both qualitative and quantitative aspects of the data need to be considered. The qualitative aspect is the most important, namely that the data should be rich and complex to enable a deep and nuanced analysis. Although there were few participants, the criteria were met by the rich qualitative data. The quantitative aspect is counted in number of interviews [31]. The data analyzed in this study came from 27 interviews (all nine participants being interviewed three times, with no dropouts) which is considered sufficient [13,31].
Acknowledgement: The authors thank the parents for opening their homes and hearts and so generously sharing their experiences.
Funding Statement: This study was supported by the Pediatric Heart Center at Skåne University Hospital Lund and Lund University, and by the Swedish Children’s Heart Association.
Author Contributions: The authors confirm their contribution to the paper as follows: study conception and design: BS, MB, PL, AW; data collection: BS; analysis and interpretation of results: BS; draft manuscript preparation: BS, MB; review of the draft manuscript: MB, PL, AW. All authors reviewed the results and approved the final version of the manuscript.
Ethics Approval: Research involving human subjects complied with all relevant national regulations, institutional policies and is in accordance with the tenets of the Declaration of Helsinki (as revised in 2013) [32]. It was approved by the Ethical Review Board at Lund University (Approval Number 2014/66).
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
References
1. Ho, J. G., Schamberger, M. S., Hurwitz, R. A., Johnson, T. R., Sterrett, L. S. et al. (2015). The effects of pulmonary valve replacement for severe pulmonary regurgitation on exercise capacity and cardiac function. Pediatric Cardiology, 36, 1194–1203. https://doi.org/10.1007/s00246-015-1143-3 [Google Scholar] [PubMed] [CrossRef]
2. Wei, H., Roscigno, C. I., Hanson, C. C., Swanson, K. M. (2015). Families of children with congenital heart disease: A literature review. Heart & Lung, 44, 494–511. https://doi.org/10.1016/j.hrtlng.2015.08.005 [Google Scholar] [PubMed] [CrossRef]
3. Jackson, A. C., Frydenberg, E., Liang, R. P. T., Higgins, R. O., Murphy, B. M. (2015). Familial impact and coping with child heart disease: A systematic review. Pediatric Cardiology, 36, 695–712. https://doi.org/10.1007/s00246-015-1121-9 [Google Scholar] [PubMed] [CrossRef]
4. Golfenshtein, N., Hanlon, A. L., Deatrick, J. A., Medoff-Cooper, B. (2017). Parenting stress in parents of infants with congenital heart disease and parents of healthy infants: The first year of life. Comprehensive Child and Adolescent Nursing, 40(4), 294–314. https://doi.org/10.1080/24694193.2017.1372532 [Google Scholar] [PubMed] [CrossRef]
5. Wei, H., Roscigno, C. I., Swanson, K. M., Black, B. P., Hudson-Barr, D. et al. (2016). Parents’ experiences of having a child undergoing congenital heart surgery: An emotional rollercoaster from shocking to blessing. Heart & Lung, 45, 154–160. https://doi.org/10.1016/j.hrtlng.2015.12.007 [Google Scholar] [PubMed] [CrossRef]
6. Harvey, K. A., Kovalesky, A., Woods, R. K., Loan, L. A. (2013). Experiences of mothers of infants with congenital heart disease before, during and after complex cardiac surgery. Heart & Lung, 43, 399–406. [Google Scholar]
7. Sjostrom-Strand, A., Terp, K. (2019). Parents’ experiences of having a baby with a congenital heart defect and the child’s heart surgery. Comprehensive Child and Adolescent Nursing, 42(1), 10–23. https://doi.org/10.1080/24694193.2017.1342104 [Google Scholar] [PubMed] [CrossRef]
8. Lan, S. F., Mu, P. F., Hsieh, K. S. (2007). Maternal experiences making a decision about heart surgery for their young children with congenital heart disease. Journal of Clinical Nursing, 16, 2323–2330. https://doi.org/10.1111/j.1365-2702.2007.02004.x [Google Scholar] [PubMed] [CrossRef]
9. Svensson, B., Liuba, P., Wennick, A., Berghammer, M. (2023). “The only thing I wonder is when I will have surgery again”: Everyday life for children with right ventricle outflow tract anomalies during assessment for heart surgery. Cardiology in the Young, 33(3), 396–401. https://doi.org/10.1017/S1047951122000907 [Google Scholar] [PubMed] [CrossRef]
10. Braun, V., Clarke, V. (2013). Successful qualitative research: A practical guide for beginners. London: Sage. [Google Scholar]
11. Braun, V., Clarke, V. (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3(2), 77–101. https://doi.org/10.1191/1478088706qp063oa [Google Scholar] [CrossRef]
12. Braun, V., Clark, V. (2019). Reflecting on reflexive thematic analysis. Qualitative Research in Sport Exercise and Health, 11(4), 589–597. https://doi.org/10.1080/2159676X.2019.1628806 [Google Scholar] [CrossRef]
13. Braun, V., Clark, V. (2022). Conceptual and design thinking for thematic analysis. Qualitative Psychology, 9(1), 3–26. https://doi.org/10.1037/qup0000196 [Google Scholar] [CrossRef]
14. Braun, V., Clark, V. (2020). Can I use TA? Should I not use TA? Comparing reflexive thematic analysis and other pattern-based analytic qualitative approaches. Counselling and Psychotherapy Research, 21, 37–47. https://doi.org/10.1002/capr.12360 [Google Scholar] [CrossRef]
15. Lincoln, Y. S., Guba, E. G. (1985). Naturalistic inquiry. Beverly Hills, CA: Sage. [Google Scholar]
16. Mohamed, I., Stamm, R., Keenan, R., Lowe, B., Coffey, S. (2020). Assessment of disease progression in patients with repaired tetralogy of fallot using magnetic resonance imaging: A systematic review. heart. Lung and Circulation, 19, 1613–1620. https://doi.org/10.1016/j.hlc.2020.04.017 [Google Scholar] [PubMed] [CrossRef]
17. Lumsden, M. R., Smith, D. M., Twigg, E., Guerrero, R., Wittkowski, A. (2020). Children with single ventricle congenital heart defects: An interpretative phenomenological analysis of the lived experience. Progress in Pediatric Cardiology, 59. https://doi.org/10.1016/j.ppedcard.2020.101297 [Google Scholar] [CrossRef]
18. Menahem, S., Poulakis, Z., Prior, M. (2008). Children subjected to cardiac surgery for congenital heart disease. part 2-parental emotional experiences. Interactive Cardiovascular and Thoracic Surgery, 7, 605–608. https://doi.org/10.1510/icvts.2007.171066 [Google Scholar] [PubMed] [CrossRef]
19. Lumsden, M. R., Smith, D. M., Twigg, E., Wittkowski, A. (2019). Coping in parents of children with congenital heart disease: A systematic review and meta-synthesis. Journal of Child and Family Studies, 28(7), 1736–1753. https://doi.org/10.1007/s10826-019-01406-8 [Google Scholar] [CrossRef]
20. Franck, L. S., Mcquillan, A., Wray, J., Grocott, P. W., Goldman, A. (2010). Parent stress levels during children’s hospital recovery after congenital heart surgery. Pediatric Cardiology, 31, 961–968. https://doi.org/10.1007/s00246-010-9726-5 [Google Scholar] [PubMed] [CrossRef]
21. Woolf-King, S. E., Anger, A., Arnold, E. A., Weiss, S. J., Teitel, D. (2017). Mental health among parents of children with chronical congenital heart defects: A systematic review. American Heart Association, 6, e004862. https://doi.org/10.1161/JAHA.116 [Google Scholar] [CrossRef]
22. Pomicino, L., Maccacari, E., Buchini, S. (2017). Levels of anxiety in the 24 h before and after their child’s surgery: A descriptive study. Journal of Clinical Nursing, 27, 278–287. https://doi.org/10.1111/jocn.13895 [Google Scholar] [PubMed] [CrossRef]
23. Jordan, B., Franich-Ray, C., Albert, N., Anderson, V., Northam, E. et al. (2014). Early mother-infant relationships after cardiac surgery in infancy. Archives of Disease in Childhood, 99, 641–645. https://doi.org/10.1136/archdischild-2012-303488 [Google Scholar] [PubMed] [CrossRef]
24. Re, J., Dean, S., Menahem, A. (2013). Infant cardiac surgery: Mothers tell their story: A therapeutic experience. World Journal for Pediatric and Congenital Heart Surgery, 4, 278–285. https://doi.org/10.1177/2150135113481480 [Google Scholar] [PubMed] [CrossRef]
25. Wei, H., Roscigno, C. I., Swanson, K. M. (2017). Healthcare providers’ caring: Nothing is too small for parents and children hospitalized for heart surgery. Heart & Lung, 46, 166–171. https://doi.org/10.1016/j.hrtlng.2017.01.007 [Google Scholar] [PubMed] [CrossRef]
26. Liu, J. F., Xie, W. P., Lei, Y. Q., Cao, H., Chen, Q. (2021). The relationship between religious beliefs and mental state, care burden, and quality of life in parents of infant patients with congenital heart disease. Cardiology in the Young, 14, 1–5. https://doi.org/10.1017/S1047951121004200 [Google Scholar] [PubMed] [CrossRef]
27. Söderbäck, M., Coyne, I., Harder, M. (2011). The importance of including both a child perspective and the child’s perspective within health care settings to provide truly child-centred care. Journal of Child Health Care, 15, 99–106. https://doi.org/10.1177/1367493510397624 [Google Scholar] [PubMed] [CrossRef]
28. Kosta, L., Harms, L., Franich-Ray, C., Anderson, V., Northam, E. et al. (2015). Parental experiences of their infant´s hospitalization for cardiac surgery. Child: Care, Health and Development, 41(6), 1057–1065. https://doi.org/10.1111/cch.12230 [Google Scholar] [PubMed] [CrossRef]
29. Gramszlo, C., Karpyn, A., Abigail, C., Demianczyk, A. C., Shillingford, A. et al. (2020). Parent perspectives on family-based psychosocial interventions for congenital heart disease. The Journal of Pediatrics, 216, 51–57. https://doi.org/10.1016/j.jpeds.2019.09.059 [Google Scholar] [PubMed] [CrossRef]
30. Schalkers, I., Parsons, C. S., Bunders, J. F. G., Dedding, C. (2016). Health professionals’ perspectives on children’s and young people’s participation in health care: A qualitative multihospital study. Journal of Clinical Nursing, 25, 1035–1044. https://doi.org/10.1111/jocn.13152 [Google Scholar] [PubMed] [CrossRef]
31. Terry, G., Hayfield, N., Clarke, V., Braun, V. (2017). Thematic analysis. In: SAGE handbook of qualitative research in psychology. London: Sage. [Google Scholar]
32. Association, W. M. (2013). World medical association declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA, 310 (20), 2191–2194. https://doi.org/10.1001/jama.2013.281053 [Google Scholar] [PubMed] [CrossRef]
Cite This Article
 Copyright © 2023 The Author(s). Published by Tech Science Press.
Copyright © 2023 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools