 Open Access
Open Access
ARTICLE
Effects of General Anesthesia on the Results of Cardiac Catheterization in Pediatric Patients with Ventricular Septal Defect
1 Department of Pediatric Cardiology, Aichi Children’s Health and Medical Center, Obu, 474-8710, Japan
2 Department of Pediatrics, Nagoya University Graduate School of Medicine, Nagoya, 466-8560, Japan
* Corresponding Author: Taichi Kato. Email:
Congenital Heart Disease 2023, 18(2), 235-243. https://doi.org/10.32604/chd.2023.027590
Received 08 November 2022; Accepted 03 January 2023; Issue published 15 March 2023
Abstract
Background: There is no gold standard sedation method for pediatric cardiac catheterization. In congenital heart diseases with intracardiac shunts, hemodynamic parameters are prone to change depending on the ventilation conditions and anesthetics, although few studies have examined these effects. The purpose of this study was to investigate the effects of two different sedation methods on the hemodynamic parameters. Methods: This study retrospectively evaluated consecutive patients with ventricular septal defect (VSD) below 1 year of age who underwent cardiac catheterization at Aichi Children’s Health and Medical Center, who were divided into age- and VSD diameter-matched general anesthesia (GA) and monitored anesthesia care (MAC) under the natural airway groups (n = 40 each), for comparison of hemodynamic parameters. Results: In the GA group, arterial blood pH and arterial partial pressure of oxygen were significantly higher (p < 0.01), whereas arterial partial pressure of carbon dioxide was significantly lower than in the MAC group (p < 0.01). Mean pulmonary artery pressure (p < 0.05) and systemic blood pressure (p < 0.01) were lower in the GA group. Pulmonary vascular resistance index (p < 0.01) and systemic vascular resistance index (p < 0.01) were also significantly lower in the GA group than the MAC group. There were no significant differences in pulmonary blood flow index, systemic blood flow index, and pulmonary/systemic blood flow ratio between the two groups. Conclusions: Cardiac catheterization under GA in VSD patients results in different hemodynamic parameters compared to that under MAC. In particular, when using pulmonary artery pressure and pulmonary vascular resistance measured under GA for judgment regarding the surgical indications or perioperative management, consideration should be given to the fact that these parameters might be lower compared to those measured under MAC.Keywords
Congenital heart diseases (CHD) have great impacts on life prognosis and are frequently found in more than 1% of newborns [1]. Among them, CHD with left-to-right shunts, such as ventricular septal defect (VSD), are common, with some of them requiring surgical treatment. Cardiac catheterization is an important examination for understanding the hemodynamics of CHD with left-to-right shunts and deciding the therapeutic strategy [2].
Pediatric cardiac catheterization can be performed under sedation and intravenous anesthesia without artificial ventilation (monitored anesthesia care: MAC), or under general anesthesia (GA) with artificial ventilation [3,4]. In addition, a consensus statement by the Society for Cardiovascular Angiography and Interventions (SCAI), the Society for Pediatric Anesthesia (SPA) and the Congenital Cardiac Anesthesia Society (CCAS) states that there is no specific sedation method recommended for all CHD [5]. Although ventilation methods and anesthetics can affect the hemodynamics of CHD, only a few reports have discussed how the hemodynamic parameters used to determine surgical indications are affected by sedation methods. In addition, there is no report describing which sedation method should be used to measure indexes such as Qp/Qs and pulmonary vascular resistance index (PVRI), to determine the surgical indications for CHD with left-to-right shunt.
In Aichi Children’s Health and Medical Center, cardiac catheterization was conventionally performed under MAC by pediatric cardiologists. However, since 2017, when anesthesiologists have been in charge of sedation, cardiac catheterization has been performed under GA in all cases. Therefore, it was possible to compare the results of cardiac catheterizations performed under different sedation methods. The purpose of this study was to compare hemodynamic parameters in VSD patients measured during cardiac catheterization under MAC vs. those measured under GA, and to investigate the effects of each sedation method on the hemodynamic parameters. The ultimate goal of this study was to clarify pitfalls when using the parameters measured under GA for judgment regarding the surgical indications and perioperative management.
2.1 Study Design and Population
This was a single-center, retrospective, observational study. The subjects were consecutive VSD patients less than 1 year of age who underwent cardiac catheterization between May 2016 and August 2021 at Aichi Children’s Health and Medical Center. All patients underwent cardiac examination because of high pulmonary blood flow and for consideration of surgical indications. Hemodynamic parameters during cardiac catheterization were retrospectively examined and compared between consecutive cases in the general anesthesia (GA) group and the MAC group. Cases with structural abnormalities that might affect the amount of left-to-right shunt, such as pulmonary valve stenosis, aortic valve stenosis, coarctation of the aorta, large atrial septal defect, patent ductus arteriosus and complex structural heart diseases were excluded.
Patients with chromosomal abnormalities including trisomy 21 and systemic diseases that could affect examination results were also excluded.
2.2 Sedation and Anesthesia Methods
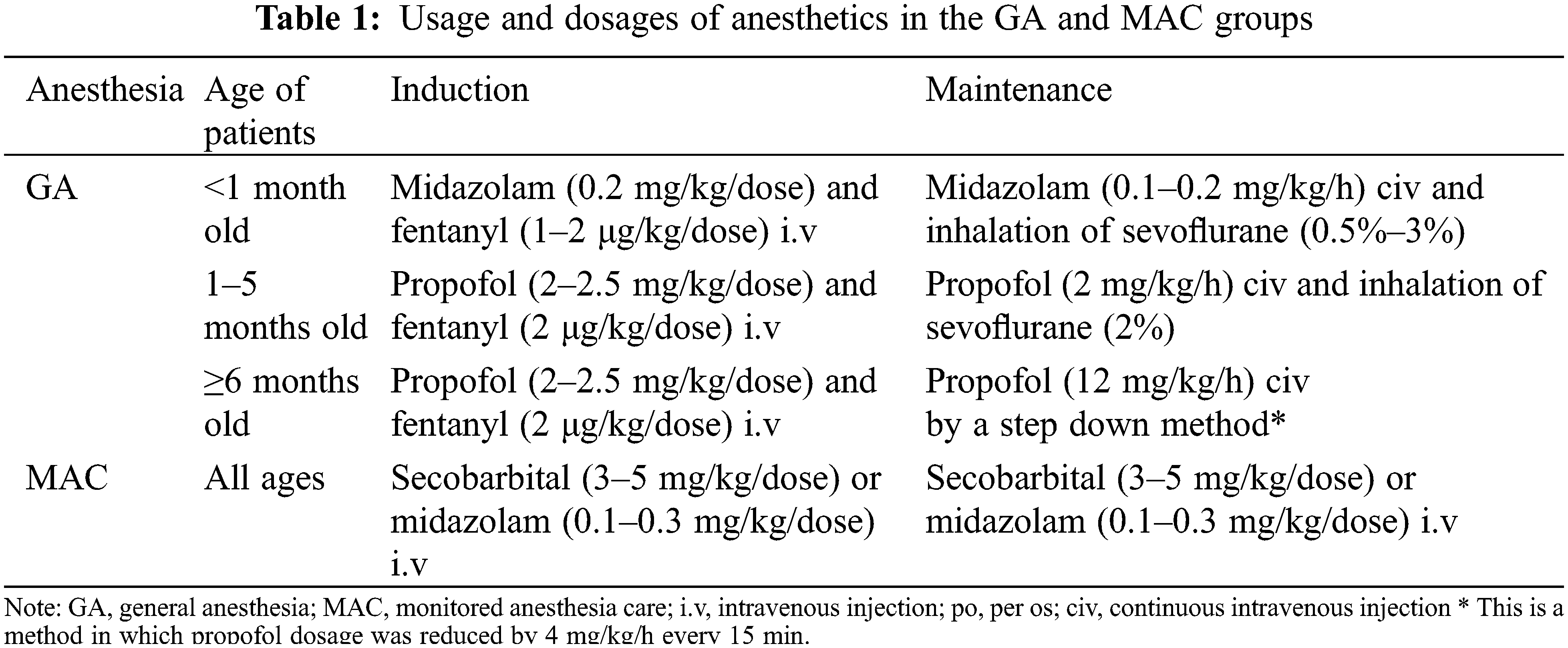
As premedication before sedation, midazolam (0.5 mg/kg) was orally administered in the GA group, pentazocine hydrochloride (0.3–0.5 mg/kg/dose) and hydroxyzine hydrochloride (0.5–1.0 mg/kg/dose) were administered by intravenous injection in the MAC group. The usage and dosage of anesthetics in GA and MAC are shown in Table 1.
General anesthesia under intubation and artificial ventilation was performed by anesthesiologists. Oxygen was only used at the time of anesthesia induction, and catheterization was started after the patient breathed room air for at least 5 min. During catheterization, positive end-expiratory pressure was set as 5 cmH2O, and inspiratory pressure was set to avoid hyperventilation and hypoventilation by monitoring the end tidal CO2. MAC method under the spontaneous respiration was performed by pediatric cardiologists. In both groups, 1% lidocaine (maximum dose: 5 mg/kg/dose) was used for local anesthesia at the puncture site.
We investigated pH, arterial partial pressure of oxygen (PaO2) and arterial partial pressure of carbon dioxide (PaCO2) in arterial blood gas analysis, and heart rate (HR) at the start of catheterization. In all cases, the values of mean pulmonary artery pressure (PAP), mean systemic artery pressure (SAP), pulmonary/systemic artery pressure ratio (Pp/Ps), central venous pressure (CVP), and pulmonary artery wedge pressure (PAWP) measured during cardiac catheterization were evaluated. In addition, pulmonary blood flow index (QpI), systemic blood flow index (QsI), pulmonary/systemic blood flow ratio (Qp/Qs), PVRI, systemic vascular resistance index (SVRI) and pulmonary/systemic vascular resistance ratio (Rp/Rs) were also examined and compared between the two groups. Qp and Qs were calculated based on the Fick principle. VSD diameters in echocardiography were measured using the EPIQ7 imaging system (Philips Ultrasound Inc., Bothell, WA, USA). Maximum VSD diameters were measured in one of the following echo views: left ventricle short-axis, great arteries short-axis, apical four-chamber, apical five-chamber, and left ventricle long-axis.
Continuous data are expressed as the median and interquartile range (IQR), i.e., the first to third IQR. All statistical analyses were performed with EZR (Saitama Medical Center, Jichi Medical University, Saitama, Japan), which is a graphical user interface for R (The R Foundation for Statistical Computing, Vienna, Austria). More precisely, it is a modified version of R commander designed to add statistical functions frequently used in biostatistics [6].
Welch’s t-test was used for normally distributed variables, and Mann-Whitney U-test was used for non-normally distributed variables. Pearson correlation analyses were performed on the correlations between mean PAP, PVRI and the results of arterial blood gas analysis. A two-sided p value less than 0.05 was considered statistically significant.
This study was conducted in accordance with the principles of the Declaration of Helsinki and the ethical guidelines issued by the Ministry of Health, Labour, and Welfare, Japan. Ethics approval was obtained from the local ethics committee of Aichi Children’s Health and Medical Center (approval number 2021060, approval date October 29, 2021). Since this study was a retrospective observational study, an opt-out procedure was used to obtain consent for study participation and the need for written consent from the patient’s family was waived.
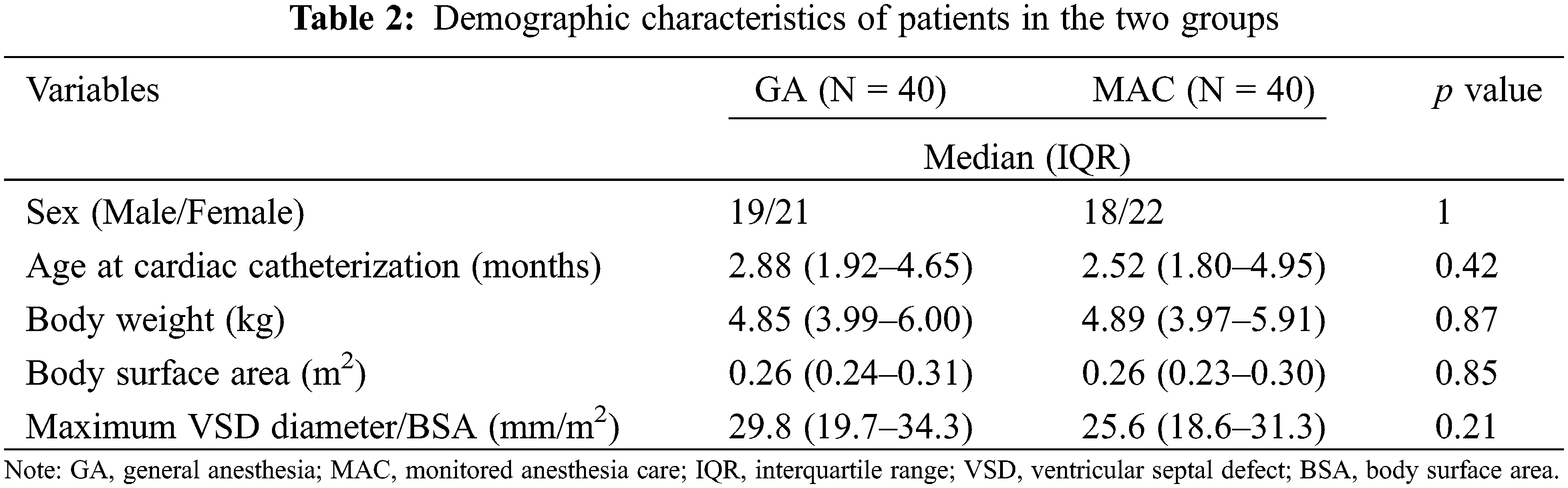
Between May 2016 and August 2021, 40 patients each were included in the GA and MAC groups. Table 2 shows the demographic characteristics of each group. There were no significant differences between the GA and MAC groups in terms of sex, age and body weight at the time of examination. The average values of the maximum VSD diameter divided by body surface area were not different between the two groups.
Regarding the results of arterial blood gas analysis at the start of examinations, median pH was significantly higher in the GA group compared with the MAC group [7.40 (7.37–7.43) vs. 7.36 (7.35–7.38), p < 0.01]. PaO2 was also significantly higher in the GA group compared with the MAC group [94.4 (86.5–104.6) vs. 84.1 (74.5–97.2) mmHg, p < 0.01]. In contrast, PaCO2 was significantly lower in the GA group than in the MAC group [37.6 (35.2–40.8) vs. 44.7 (41.5–47.0) mmHg, p < 0.01].
Table 3 shows a comparison of hemodynamic parameters between the two groups. HR was lower in the GA group compared with the MAC group [124 (120–134) vs. 129 (125–135) beats per minute, p = 0.046]. Mean PAP and mean SAP were also significantly lower in the GA group compared with the MAC group [28.5 (22.0–35.0) vs. 35.5 (21.7–45.2) mmHg, p = 0.037, and 51.0 (46.0–54.2) vs. 57.0 (52.0–60.2) mmHg, p < 0.01, respectively]. Regarding Pp/Ps, no difference was observed between the two groups. On the other hand, CVP and PAWP were significantly higher in the GA group compared to the MAC group (p < 0.01).
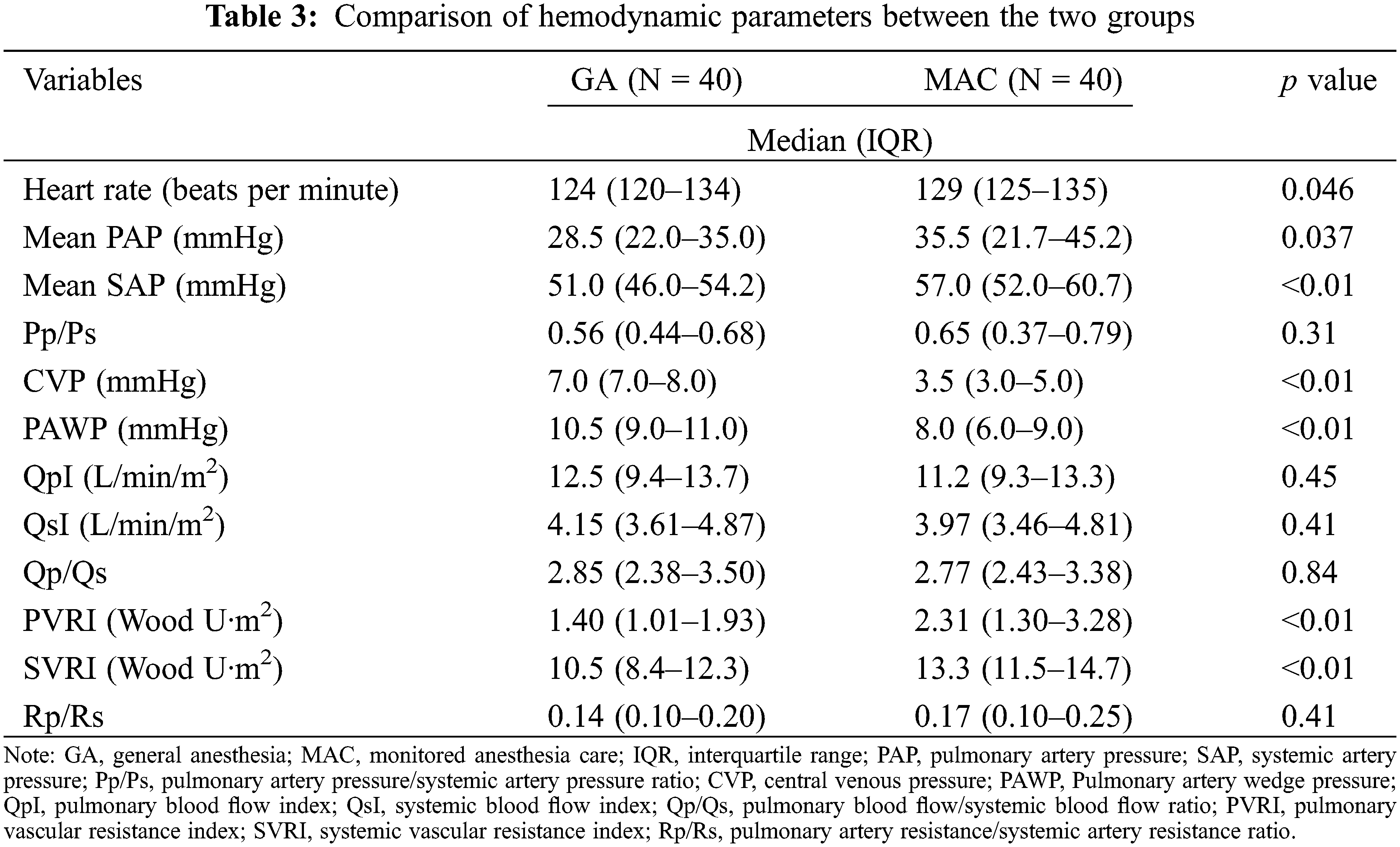
Comparing the indexes calculated based on the Fick principle, QpI, QsI and Qp/Qs were not different between the two groups. Comparing vascular resistance, both PVRI [1.40 (1.01–1.93) vs. 2.31 (1.30–3.28) Wood U·m2, p < 0.01] and SVRI [105 (8.4–12.3) vs. 13.3 (11.5–14.7) Wood U·m2, p < 0.01] were lower in the GA group than in the MAC group. There was no significant difference in Rp/Rs between the two groups.
Fig. 1 shows the correlation between mean PAP, PVRI and the results of arterial blood gas analysis. PAP and PVRI were most correlated with PaO2 among PaCO2, PaO2, and pH.
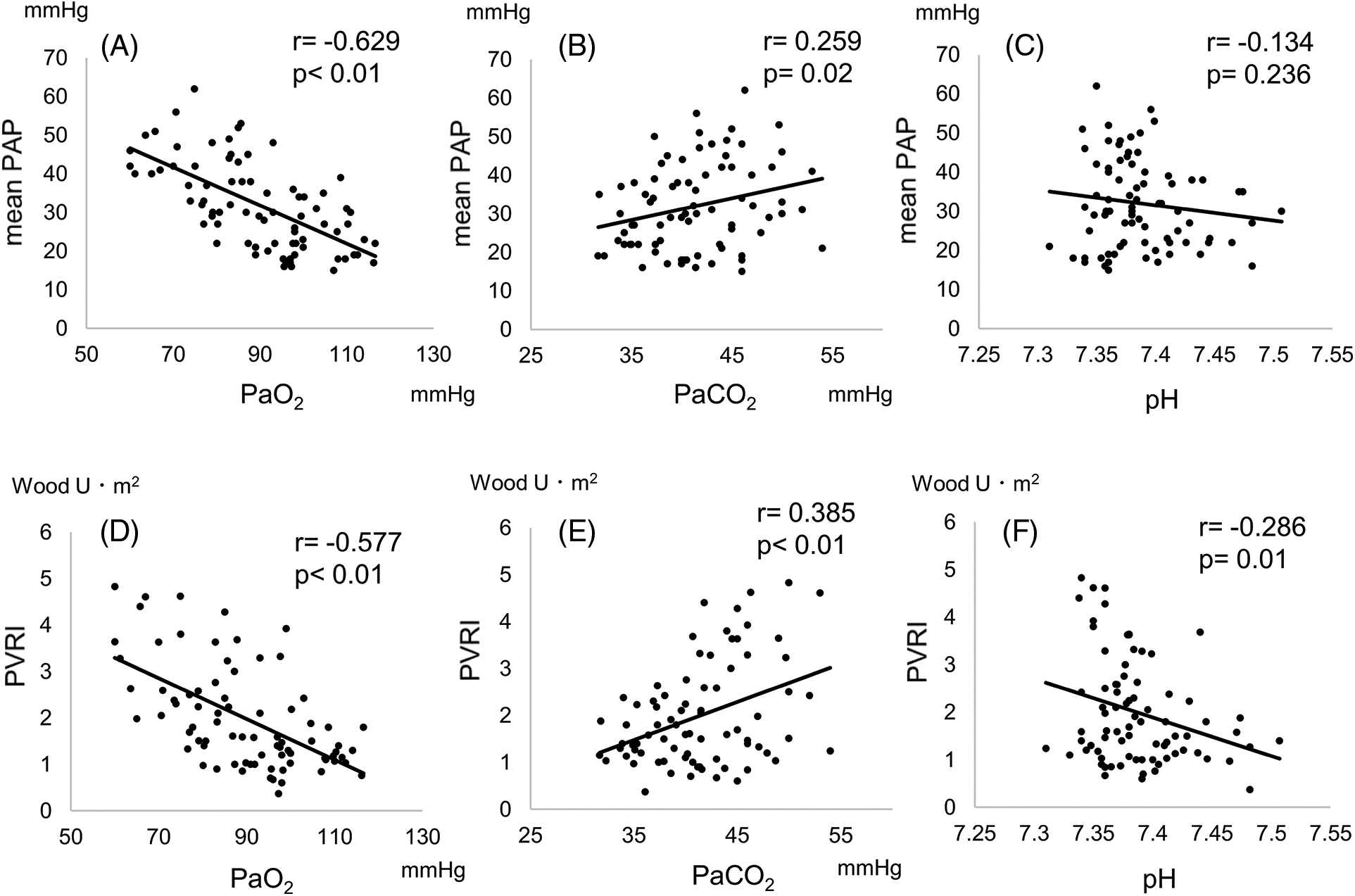
Figure 1: (A), (B), (C) Correlation between mean PAP and PaO2, PaCo2 and pH. (D), (E), (F) Correlation between PVRI and PaO2, PaCO2 and pH. r, correlation coefficient
This retrospective, observational study showed similarities and differences in hemodynamic parameters depending on the anesthesia method used for cardiac catheterization in pediatric VSD patients. In cardiac catheter examinations under GA in VSD patients, both, pulmonary and systemic arterial pressure and pulmonary and systemic vascular resistance were lower, so that QpI, QsI and Qp/Qs were not different compared to examinations under MAC. The results of this study provide important information related to the use of hemodynamic parameters measured under different sedation methods for judging surgical indications and for the perioperative management of VSD patients.
Only a few previous reports have described the differences in hemodynamic parameters measured during cardiac catheterization due to differences in anesthesia methods. When interpreting the differences in the results of catheterization under different anesthesia methods, it is necessary to understand the effects of ventilation methods and the anesthetics used. The parameters examined in this study might have been affected by differences in ventilation methods. Positive pressure ventilation (PPV) associated with GA provides reliable airway management and PaCO2 control. On the other hand, under anesthesia without reliable airway management, patients might develop hypoxemia, hypercapnia and respiratory acidosis due to upper airway narrowing and hypoventilation, leading to an increase in PVR and alteration of shunt physiology [7,8]. In our study, hypoventilation was avoided in the GA group by reliable airway management with tracheal intubation, leading to a lower PaCO2 and higher PaO2 than in the MAC group. Arterial blood pH was also significantly higher in the GA group, indicating the avoidance of respiratory acidosis. All of these conditions probably contributed to the significantly lower PVRI in the GA group. In our study, PaO2 correlated better with PVRI and mean PAP than PaCO2 and pH. None of the patients in our study developed significant respiratory acidosis or alkalosis in either group, which may result in the weak correlation of PVRI and mean PAP with pH.
Qp/Qs may be influenced by the increase in mean intrathoracic pressure due to PPV. For the right ventricular circulation, PPV reduces systemic venous blood return that is, right heart preload [9]. For the left heart circulation, increased mean intrathoracic pressure due to PPV and PEEP reduces the difference between the left ventricular internal and external pressures, thereby reducing left ventricular afterload, which is synonymous with systemic vascular resistance [9]. Based on these mechanisms, PPV may reduce left-to-right shunt volumes in patients with interventricular shunts. However, our data showed no difference in Qp/Qs between the two groups, which may be due to the combined effect of above-mentioned changes in hemodynamics by PPV and the effect of anesthetics described later. In addition, if alveolar hyperinflation occurs due to positive pressure ventilation, PAWP increases due to capillary compression, leading to an increase in CVP [9,10]. The significantly higher CVP and PAWP in the GA group in this study were also probably due to the increased intrathoracic pressure.
Focusing on anesthetics, lower HR, arterial pressure and vascular resistance in the GA group might have been affected by anesthetics. Midazolam used in the MAC group has little effect on hemodynamics [11]. Secobarbital is a type of barbiturate that has hypotensive and negative inotropic effects [12]. Propofol used in the GA group has been reported to reduce HR, SAP and SVR, as well as PAP and PVR [13,14]. Hickey et al. reported that fentanyl did not change HR, cardiac index, mean PAP and PVR after surgery in patients with repaired CHD [15], suggesting that the effect of fentanyl on hemodynamics might be small. Regarding inhalation anesthetics, Laird et al. reported that sevoflurane does not change the pulmonary/systemic blood flow ratio among patients with atrial septal defect (ASD) or VSD [16]. In our study, both systemic/pulmonary artery pressure and vascular resistance were lower in the GA group, which was consistent with the effects of the anesthetics used. Under the influence of ventilation methods and anesthetics, PVR and SVR showed parallel differences between the two groups, which might have resulted in the absence of differences in Qp/Qs, contrary to the expectation that shunt physiology might be altered by a difference in sedation methods.
The results of cardiac catheterization are used to measure the amount of left-to-right shunt and evaluate pulmonary hypertension in VSD patients, and to determine surgical indications. Patients with low Qp/Qs or extremely high PAP and vascular resistance might not be indicated for surgery [17]. Although the results of cardiac catheterization are important for determining therapeutic strategies, and these results can vary depending on the sedation methods, there is no specific sedation method that is considered the gold standard for cardiac catheterization. According to a report in 2014 by Miura et al. [3] in Japan, pediatric cardiac catheterizations were performed under MAC in 52% of cases, and examinations under GA with airway management were performed in 34.9%. In multicenter studies in North America, 70% of pediatric cardiac catheterizations were performed under GA, although there were differences between institutions [4]. In 2016, the SCAI, SPA and CCAS issued a joint statement on cardiac catheterization for the diagnosis and treatment of CHD [5]. However, this joint statement mentions the kind of physicians who should be in charge of sedation and perioperative management, and does not refer to specific preferred sedation methods or anesthetics. In our study, there was no significant difference in Qp/Qs between MAC and GA, suggesting that differences in anesthesia methods have limited impact on Qp/Qs for determination of surgical indications in VSD cases. On the other hand, since PAP and PVR were lower under GA, it should be noted that when using PAP and PVRI in determining surgical indications, they might be underestimated compared to under awake conditions with a natural airway. Rp/Rs may be a more appropriate indicator, as no significant difference was found between GA and MAC in our study. However, this hypothesis needs to be tested. Larger prospective studies are needed to determine which sedation method is more appropriate to use to determine surgical indications in VSD patients. Further studies should also aim to establish the preferred sedation method during cardiac catheterization or the criteria for treatment indications depending on the sedation method used.
The limitations of this study are that it was a retrospective study and was not a comparison between GA and MAC among the same patients and during the same time period. However, since both the GA group and the MAC group included consecutive patients with the same indications for cardiac catheterization, were almost the same age, and the VSD diameter was adjusted for body surface area, we considered that comparisons of each hemodynamic parameter were appropriate. Although different physicians were in charge of anesthesia or sedation for each case, the anesthesia method was standardized and the effect on the results was limited. In this study, since we focused on VSD, which is a simple left-to-right shunt heart disease, it is unclear whether the same results will be achieved in heart diseases with right-to-left shunt, such as Tetralogy of Fallot or complex heart diseases with pulmonary and systemic circulations supplied in parallel, such as single ventricle defects. In addition, different results might be obtained in patients after right heart bypass surgery, such as the Glenn operation or Fontan operation, in which the hemodynamics are greatly affected by the increase in intrathoracic pressure due to positive pressure ventilation. The results in older children are also unknown, because this study targeted patients below the age of 1 year, in order to minimize differences in patient characteristics. Additionally, patients with chromosomal abnormalities such as trisomy 21 were not included in the study. Some patients with chromosomal abnormalities are more likely to have upper airway obstruction, therefore differences in ventilation methods may affect the results of cardiac catheterization. Further studies need to be conducted to clarify the effects of general anesthesia on the results of cardiac catheterization in these patients.
Hemodynamic parameters in VSD patients measured by cardiac catheterization are affected by the sedation methods used. In this study, QpI, QsI, and Qp/Qs did not differ regardless of the sedation method used, although PAP and PVRI were found to be lower under GA. When using these parameters for determination of the surgical indications or perioperative management of VSD patients, the effects of sedation methods on these parameters should be considered. Larger prospective studies are needed to determine the preferred sedation method during cardiac catheterization or the criteria to be used as treatment indications depending on the sedation method in VSD patients.
Funding Statement: The authors received no specific funding for this study.
Author Contributions: All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work. The authors confirm contribution to the paper as follows. Study conception and design: Go, Kato, Yasuda; data collection: Go, Kito, Morimoto; analysis and interpretation of results: Go, Kawai, Yamamoto, Fukazawa; draft manuscript preparation: Go, Kato. All authors reviewed the results and approved the final version of the manuscript.
Availability of Data and Materials: De-identified data will be available through email request to the corresponding author.
Ethics Approval: This study was approved by the ethics committee of Aichi Children’s Health and Medical Center (approval number 2021060) and the patient consent was waived due to its retrospective nature.
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
References
1. Marelli, A. J., Mackie, A. S., Ionescu-Ittu, R., Rahme, E., Pilote, L. (2007). Congenital heart disease in the general population. Circulation, 115(2), 163–172. https://doi.org/10.1161/CIRCULATIONAHA.106.627224 [Google Scholar] [PubMed] [CrossRef]
2. Deutsch, N., Swink, J., Matisoff, A. J., Olivieri, L. J., Cross, R. R. et al. (2019). Anesthetic considerations for magnetic resonance imaging-guided right-heart catheterization in pediatric patients: A single institution experience. Paediatric Anaesthesia, 29(1), 8–15. https://doi.org/10.1111/pan.13512 [Google Scholar] [PubMed] [CrossRef]
3. Miura, M., Kato, H., Doi, S., Park, I., Nakagawa, M. et al. (2014). National survey on deep sedation for diagnostic and interventional cardiac catheterization procedures performed at Japanese Society of Pediatric Cardiology and Cardiac Surgery Institutions. Pediatric Cardiology and Cardiac Surgery, 30(5), 580–587. https://doi.org/10.9794/jspccs.30.580 [Google Scholar] [CrossRef]
4. Lin, C. H., Desai, S., Nicolas, R., Gauveau, K., Forester, S. et al. (2015). Sedation and anesthesia in pediatric and congenital cardiac catheterization: A prospective multicenter experience. Pediatric Cardiology, 36(7), 1363–1375. https://doi.org/10.1007/s00246-015-1167-8 [Google Scholar] [PubMed] [CrossRef]
5. Odegard, K. C., Vincent, R., Baijal, R., Daves, S. M., Gray, R. G. et al. (2016). SCAI/CCAS/SPA expert consensus statement for anesthesia and sedation practice: Recommendations for patients undergoing diagnostic and therapeutic procedures in the pediatric and congenital cardiac catheterization laboratory. Anesthesia and Analgesia, 123(5), 1201–1209. https://doi.org/10.1213/ANE.0000000000001608 [Google Scholar] [PubMed] [CrossRef]
6. Kanda, Y. (2013). Investigation of the freely-available easy-to-use software “EZR” (Easy R) for medical statistics. Bone Marrow Transplant, 48(3), 452–458. https://doi.org/10.1038/bmt.2012.244 [Google Scholar] [PubMed] [CrossRef]
7. Andropoulos, D. B., Stayer, S. A., Russel, I. A., Mossad, E. B. (2010). Anesthesia for congenital heart disease, 2nd edition, pp. 338–355. Hoboken, New Jersey: Wiley-Blackwell. [Google Scholar]
8. Friesen, R. H., Alswang, M. (1996). Changes in carbon dioxide tension and oxygen saturation during deep sedation for pediatric cardiac catheterization. Paediatric Anaesthesia, 6(1), 15–20. https://doi.org/10.1111/j.1460-9592.1996.tb00346.x [Google Scholar] [PubMed] [CrossRef]
9. Cheifetz, I. M. (2014). Cardiorespiratory interactions: The relationship between mechanical ventilation and hemodynamics. Respiratory Care, 59(12), 1937–1945. https://doi.org/10.4187/respcare.03486 [Google Scholar] [PubMed] [CrossRef]
10. Gödje, O., Peyerl, M., Seebauer, T., Lamm, P., Mair, H. et al. (1998). Central venous pressure, pulmonary capillary wedge pressure and intrathoracic blood volumes as preload indicators in cardiac surgery patients. European Journal of Cardio-Thoracic Surgery, 13(5), 533–540. https://doi.org/10.1016/S1010-7940(98)00063-3 [Google Scholar] [PubMed] [CrossRef]
11. Jobeir, A., Galal, M. O., Bulbul, Z. R., Solymar, L., Darwish, A. et al. (2003). Use of low-dose ketamine and/or midazolam for pediatric cardiac catheterization: Is an anesthesiologist needed? Pediatric Cardiology, 24(3), 236–243. https://doi.org/10.1007/s00246-002-0339-5 [Google Scholar] [PubMed] [CrossRef]
12. Price, H. L. (1960). General anesthesia and circulatory homeostasis. Physiological Reviews, 40(2), 187–218. https://doi.org/10.1152/physrev.1960.40.2.187 [Google Scholar] [PubMed] [CrossRef]
13. Deutschman, D. S., Harris, A. P., Fleisher, L. A. (1994). Changes in heart rate variability under propofol anesthesia. A possible explanation for propofol-induced bradycardia. Anesthesia and Analgesia, 79, 373–377. [Google Scholar] [PubMed]
14. Hammarén, E., Hynynen, M. (1995). Haemodynamic effects of propofol infusion for sedation after coronary artery surgery. British Journal of Anaesthesia, 75, 47–50. [Google Scholar]
15. Hickey, P. R., Hansen, D. D., Wessel, D. L., Lang, P., Jonas, R. A. (1985). Pulmonary and systemic hemodynamic responses to fentanyl in infants. Anesthesia and Analgesia, 64, 483–486. [Google Scholar] [PubMed]
16. Laird, T. H., Stayer, S. A., Rivenes, S. M., Lewin, M. B., McKenzie, E. D. et al. (2002). Pulmonary-to-systemic blood flow ratio effects of sevoflurane, isoflurane, halothane, and fentanyl/midazolam with 100% oxygen in children with congenital heart disease. Anesthesia Analgesia, 95, 1200–1206. [Google Scholar] [PubMed]
17. Kozlik-Feldmann, R., Hansmann, G., Bonnet, D., Schranz, D., Apitz, C. et al. (2016). Pulmonary hypertension in children with congenital heart disease (PAH-CHD, PPHVD-CHD). Expert consensus statement on the diagnosis and treatment of paediatric pulmonary hypertension. The European paediatric pulmonary vascular disease network, endorsed by ISHLT and DGPK. Heart, 102, ii42–ii48. [Google Scholar] [PubMed]
Cite This Article
 Copyright © 2023 The Author(s). Published by Tech Science Press.
Copyright © 2023 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools