 Open Access
Open Access
CASE REPORT
Pentalogy of Cantrell with Pentalogy of Fallot and Left Ventricular Diverticulum
Department of Cardiac Surgery, The First Affiliated Hospital of Xinjiang Medical University, Urumqi, China
* Corresponding Author: Qiang Huo. Email:
(This article belongs to the Special Issue: Nightmare Case Reports in Congenital Heart Disease)
Congenital Heart Disease 2023, 18(1), 73-78. https://doi.org/10.32604/chd.2023.026404
Received 02 September 2022; Accepted 17 November 2022; Issue published 09 January 2023
Abstract
Pentalogy of Cantrell is a congenital anomaly characterized by a combination of birth defects involving the sternum, diaphragm, pericardium, abdominal wall, and heart. Pentalogy of Cantrell is a rare anomaly with high mortality. This paper describes the treatment of a 9-month-old girl with pentalogy of Cantrell, pentalogy of Fallot, and left ventricular diverticulum. The patient is alive and well 13 years after surgery.Keywords
Pentalogy of Cantrell is a rare congenital syndrome involving defects of the abdominal wall, sternum, diaphragm, pericardium, and heart [1]. A large number of patients with pentalogy of Cantrell die soon after birth, and relatively few studies have been reported. Patients with pentalogy of Cantrell have a poor prognosis and high early mortality. The survival of patients with pentalogy of Cantrell depends on the severity of cardiac and associated malformations [2]. To date, only a few successful cases of congenital heart surgery have been reported in patients with pentalogy of Cantrell. Herein, we report a successful total correction of cardiac defects in a 9-month-old girl with pentalogy of Cantrell, pentalogy of Fallot, and left ventricular diverticulum.
A 9-month-old girl was admitted to our department because of cyanosis, cardiac murmur, and epigastric mass. She had moderate cyanosis and clubbing of the fingers, and her oxygen saturation was approximately 80%. A 3/6 grade systolic murmur was found in the 4th intercostal of the left parasternal area. In addition, a physical examination revealed a defect of the lower sternum and a superficial pulsatile purple mass in the midline, extending from the subxiphoid region into the umbilicus (Fig. 1). The electrocardiogram showed sinus rhythm, right-axis deviation, and right ventricular hypertrophy. Echocardiography showed cardiac dextrorotation, overriding aortic roots, right ventricular hypertrophy, severe right ventricular outflow tract obstruction, a large subaortic ventricular septal defect of 12 mm, an ostium atrial septal defect of 7 mm, and a left ventricular diverticulum extending into the abdominal wall.

Figure 1: Preoperative view: defect of the lower sternum and a superficial pulsatile purple mass extending from the subxiphoid region into the umbilicus
Surgery was performed successfully with a transthoracic and abdominal approach from the suprasternal fossa to the umbilicus. Surgical exploration revealed a short and thin sternum with no xiphoid process. The pericardium had a partial defect and was adherent to the sternum. Cardiac dextrorotation was observed. A diverticulum arose from the apex of the left ventricle, protruded through a defect in the pericardium and diaphragm into the extraperitoneal tissue, and extended down to the umbilicus (Fig. 2). Surgery was performed using hypothermic cardiopulmonary bypass. The left ventricular diverticulum was resected, and the incision was closed using a 4-0 polypropylene suture. The heart was repositioned into the pericardial cavity. The ventricular septal defect was closed using Dacron. The right ventricular outflow tract was reconstructed with a double-layer patch (inner layer: autologous pericardium; outer layer: Dacron patch). The atrial septal defect was closed by running a suture (Fig. 3). No defect was found in the peritoneum. The chest and abdominal wall are not herniated from thoracic or abdominal viscera except for the left ventricular diverticulum. Pediatric surgeon isolated bilateral rectus abdominis muscles, closed their anterior sheaths using interrupted sutures, and closed the skin. The partial abdominal reconstruction without the use of prosthetics was performed.
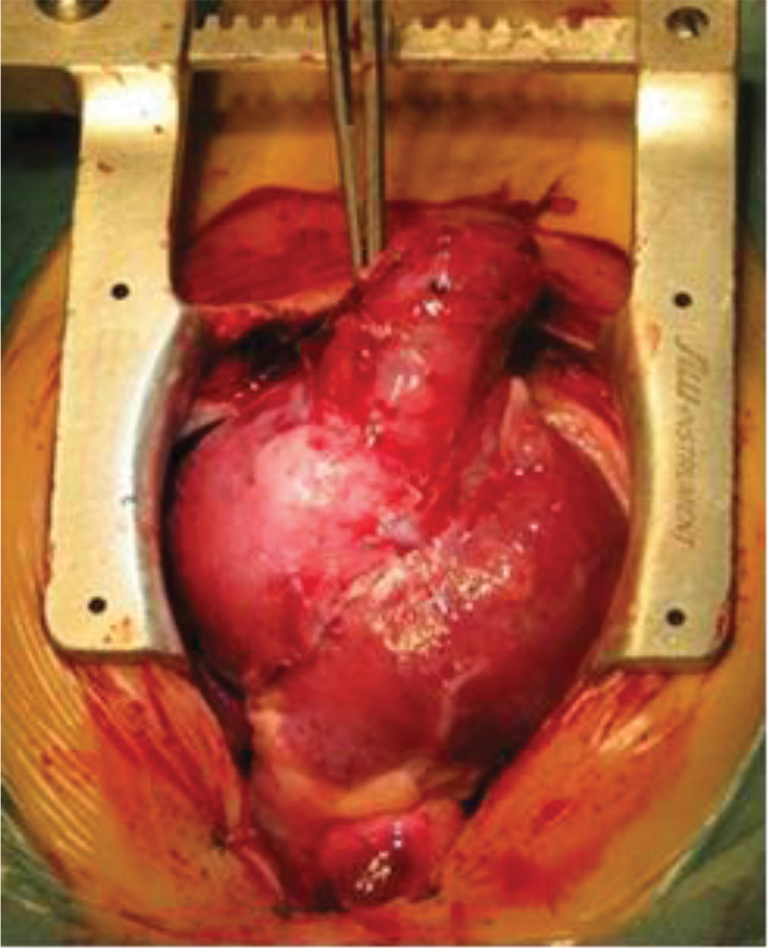
Figure 2: Intraoperative view: the left ventricle diverticulum protruded through a defect in the pericardium and diaphragm into the extraperitoneal tissue, and extended down to the umbilicus
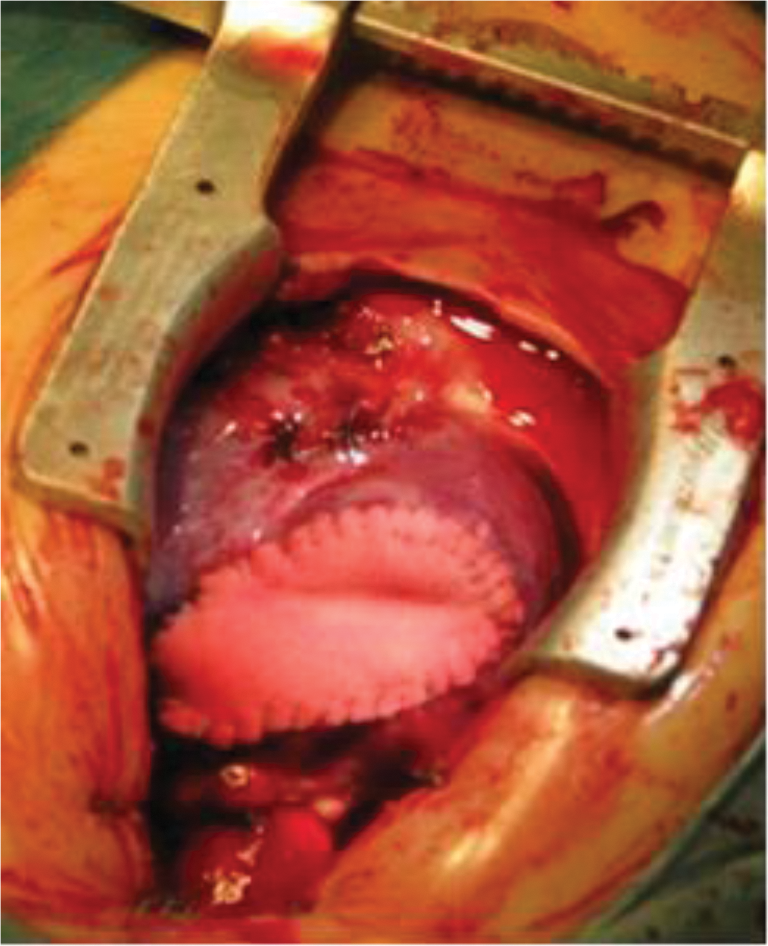
Figure 3: Intraoperative view: after left ventricle diverticular resection and repair of intracardiac malformations
The postoperative recovery was eventful. The child was discharged home on postoperative day 10. The child is currently alive and well 13 years after surgery (Fig. 4). She normally developed with age-appropriate activities.
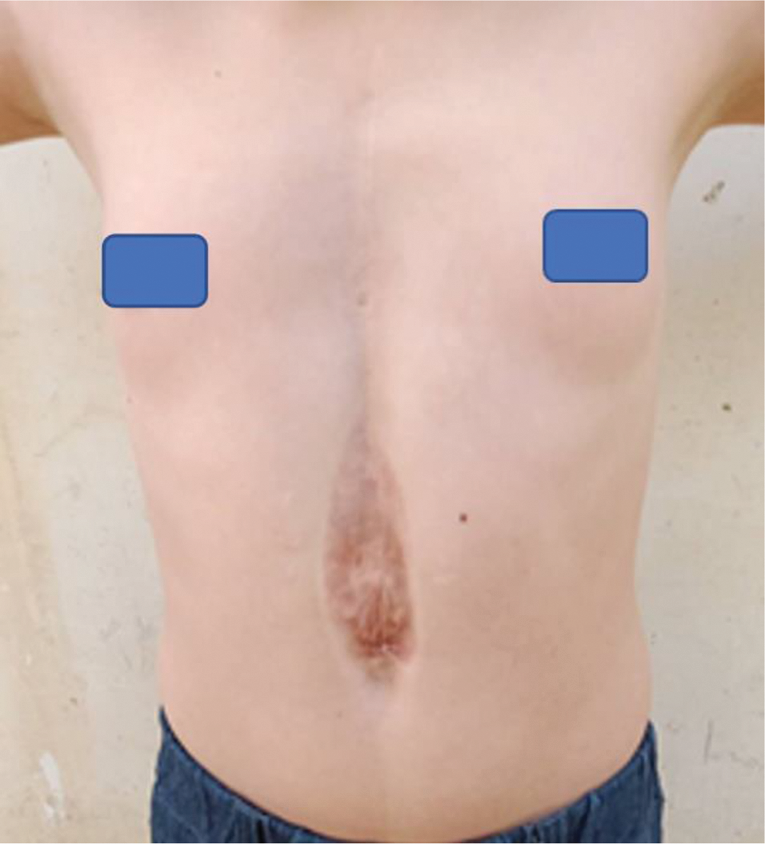
Figure 4: Postoperative view (11 years after surgery)
Pentalogy of Cantrell is a rare syndrome associated with congenital anomalies first described in 1958 [1]. It is estimated to be from 1 in 65,000 to 1 in 200,000 live births [3]. In the pentalogy of Cantrell, the survival rate remains as low as 37.3%, with few patients surviving in their early years [4]. Pentalogy of Cantrell is commonly associated with defects of the sternum, anterior diaphragm, pericardium, abdominal wall, and heart. The most common intracardiac defects are ventricular septal defect (72%), followed by an atrial septal defect (53%), pulmonary stenosis (33%), tetralogy of Fallot (20%), and left ventricular diverticulum (20%) [1,4]. These patients’ prognosis depends on their cardiac abnormalities, extracardiac defects, and postoperative complications.
The congenital diverticulum is a rare cardiac anomaly [5]. It is usually single and commonly arises from the left ventricular apex [6]. The morbidity and mortality associated with the left ventricular diverticulum vary. The complications of ventricular diverticulum include arrhythmias, embolism, endocarditis, spontaneous or traumatic rupture, and sudden death [2,7]. Patients with a ventricular diverticulum should be carefully evaluated for pentalogy of Cantrell. Correction of the ventricular diverticulum must be performed at an early stage because of the risk of spontaneous rupture and sudden death by tachyarrhythmias [8].
Pentalogy of Fallot is the association of tetralogy of Fallot with an atrial septal defect. The presentation we have noted with a left ventricular diverticulum and tetralogy of Fallot has rarely been reported before [7,9–12]. Few case studies in the literature have reported successful repair of the minor forms of the pentalogy.
In pentalogy of Cantrell, surgical treatment aims to correct heart, thoracic, and abdominal malformations. Surgical timing and approach are determined by the severity of the patient’s condition. Single- and multi-stage surgical repairs have been described and adopted in patients with pentalogy of Cantrell [2,13]. The major perioperative and postoperative problem is to avoid the high abdominal and intrathoracic pressure that occurs when the heart is repositioned in a small thoracic cavity [8]. The multiple organs are immature during the newborn period. Surgical correction at the neonatal stage has higher mortality [4,14,15]. Despite up-to-date surgical standards, neonatal surgery remains a major challenge for the surgeon, anesthetist, pediatrician, and nurse. The basic principle in unstable patients is to focus on saving the child’s life; thus, a multi-stage operation may be preferable and delayed repair should allow for some growth of the thoracic cavity.
The patient had left ventricular diverticulum and hypoxia episodes, thus requiring immediate surgery. She was 9 months old, and her physiology was more stable than a newborn. In addition, she had an incomplete expression of the pentalogy of Cantrell because the diaphragmatic defect was in continuity with a pericardial defect. The preoperative and intraoperative evaluation indicated enough space for repositioning the heart to the deeper thorax while avoiding high abdominal and intrathoracic pressures. In this case, resection of the diverticulum was combined with correction of the pentalogy of Fallot, and thoracoabdominal defects occurred in a single stage. The child is currently alive and well 13 years after surgery, with no apparent differences in growth, development, and physical activity compared with children of a similar age.
In conclusion, we describe the rare combination of pentalogy of Cantrell with pentalogy of Fallot and left ventricular diverticulum. In this case, through the cooperation of team members from all associated fields of medicine, one-stage repair of these complex anomalies is technically feasible.
Authorship: Study conception and design: W. M. Zhang and Q. Huo; Data collection: Z. Liu; Draft manuscript preparation: W. M. Zhang and T. Zhu; Manuscript revision: Q. Huo. All authors reviewed the results and approved the final version of the manuscript.
Availability of Data and Materials: The data underlying this article are available in the article.
Ethics Approval: This study was approved by Institutional Review Board of the First Affiliated Hospital of Xinjiang Medical University, and the informed consent was obtained from the patient.
Funding Statement: The authors received no specific funding for this study.
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
References
1. Cantrell, J. R., Haller, J. A., Ravitch, M. M. (1958). A syndrome of congenital defects involving the abdominal wall, sternum, diaphragm, pericardium, and heart. Surgery, Gynecology & Obstetrics, 107(5), 602–614. [Google Scholar]
2. Zhang, X., Xing, Q., Sun, J., Hou, X., Kuang, M. et al. (2014). Surgical treatment and outcomes of pentalogy of Cantrell in eight patients. Journal of Pediatric Surgery, 49(8), 1335–1340. DOI 10.1016/j.jpedsurg.2014.06.003. [Google Scholar] [CrossRef]
3. Williams, A. P., Marayati, R., Beierle, E. A. (2019). Pentalogy of Cantrell. Seminars in Pediatric Surgery, 28(2), 106–110. DOI 10.1053/j.sempedsurg.2019.04.006. [Google Scholar] [CrossRef]
4. Vazquez-Jimenez, J. F., Muehler, E. G., Daebritz, S., Keutel, J., Nishigaki, K. et al. (1998). Cantrell’s syndrome: A challenge to the surgeon. The Annals of Thoracic Surgery, 65(4), 1178–1185. DOI 10.1016/S0003-4975(98)00089-7. [Google Scholar] [CrossRef]
5. Singh, N., Bera, M. L., Sachdev, M. S., Aggarwal, N., Joshi, R. et al. (2010). Pentalogy of Cantrell with left ventricular diverticulum: A case report and review of literature. Congenital Heart Disease, 5(5), 454–457. DOI 10.1111/j.1747-0803.2009.00375.x. [Google Scholar] [CrossRef]
6. Cianciulli, T. F., Del Carmen Gonzalez Colaso, P., Saccheri, M. C., Lax, J. A., Redruello, H. J. et al. (2009). Left ventricular diverticulum, a rare echocardiographic finding: Two adult patients and review of the literature. Cardiology Journal, 16(1), 76–81. [Google Scholar]
7. Hill, M. A., Kwon, J. H., Rajab, T. K., Kavarana, M. N. (2022). Pentalogy of Cantrell with a left ventricular diverticulum and muscular VSD. The Annals of Thoracic Surgery, 113(6), e461–e463. DOI 10.1016/j.athoracsur.2021.07.093. [Google Scholar] [CrossRef]
8. Korver, A. M., Haas, F., Freund, M. W., Strengers, J. L. (2008). Pentalogy of Cantrell: Successful early correction. Pediatric Cardiology, 29(1), 146–149. DOI 10.1007/s00246-007-9032-z. [Google Scholar] [CrossRef]
9. Tuluce, K., Gurgun, C., Yavuzgil, O., Ceylan, N., Tuluce, S. Y. (2012). Two different pentalogies in an adult patient: A pentalogy of Cantrell associated with a pentalogy of Fallot. European Heart Journal-Cardiovascular Imaging, 13(10), 878–879. DOI 10.1093/ehjci/jes076. [Google Scholar] [CrossRef]
10. Alayunt, A., Yagdi, T., Alat, I., Posacioglu, H., Buket, S. (2001). Left ventricular diverticulum associated with Cantrell’s syndrome and tetralogy of Fallot in an adult. Scandinavian Cardiovascular Journal, 35(1), 55–57. DOI 10.1080/140174301750101546. [Google Scholar] [CrossRef]
11. Fernandez, M. S., Lopez, A., Vila, J. J., Lluna, J., Miranda, J. (1997). Cantrell’s pentalogy. Report of four cases and their management. Pediatric Surgery International, 12(5–6), 428–431. DOI 10.1007/BF01076959. [Google Scholar] [CrossRef]
12. Fukazawa, M., Orita, H., Hirooka, S., Uchino, H., Washio, M. et al. (1995). A case of pentalogy of Cantrell with tetralogy of Fallot and left ventricular diverticulum. Kyobu Geka, 48(9), 759–762. [Google Scholar]
13. Liu, Y., Yang, J., Jin, Z., Zhu, H., Yu, S. et al. (2014). One-stage surgical correction in pentalogy of Cantrell with left ventricular diverticulum. Journal of Cardiac Surgery, 29(3), 413–416. DOI 10.1111/jocs.12309. [Google Scholar] [CrossRef]
14. Meeker, T. M. (2009). Pentalogy of Cantrell: Reviewing the syndrome with a case report and nursing implications. The Journal of Perinatal & Neonatal Nursing, 23(2), 186–194. DOI 10.1097/JPN.0b013e3181a3b4e5. [Google Scholar] [CrossRef]
15. Engum, S. A. (2008). Embryology, sternal clefts, ectopia cordis, and Cantrell’s pentalogy. Seminars in Pediatric Surgery, 17(3), 154–160. DOI 10.1053/j.sempedsurg.2008.03.004. [Google Scholar] [CrossRef]
Cite This Article
 Copyright © 2023 The Author(s). Published by Tech Science Press.
Copyright © 2023 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools