 Open Access
Open Access
ARTICLE
Prevalence of Congenital Heart Disease at Extremely High Altitudes in Tibet and the Establishment of a New Free Treatment Model
1
Weifang Medical University, Weifang, China
2
Department of Cardiology, Shandong University Zibo Central Hospital, Zibo, China
3
Binzhou Medical University, Yantai, China
4
Department of Ultrasound, Shandong University Zibo Central Hospital, Zibo, China
5
Department of Anesthesiology, Shandong University Zibo Central Hospital, Zibo, China
6
Department of Anorectal Surgery, Shandong University Zibo Central Hospital, Zibo, China
7
Department of Obstetrics, Shandong University Zibo Central Hospital, Zibo, China
8
Department of Ultrasonography, Qilu Hospital Huantai Branch, Zibo, China
9
Department of Cardiology, Zichuan District Hospital, Zibo, China
10 Department of Cardiology, Zhoucun District Hospital, Zibo, China
11 Department of Cardiology, Zhangdian District Hospital, Zibo, China
12 Department of Cardiology, Boshan District Hospital, Zibo, China
13 Department of Ultrasound, Zibo Municipal Hospital, Zibo, China
14 Department of Ultrasound, Zibo First Hospital, Zibo, China
* Corresponding Author: Bo Li. Email:
Congenital Heart Disease 2022, 17(6), 709-716. https://doi.org/10.32604/chd.2022.018657
Received 08 August 2021; Accepted 25 October 2021; Issue published 11 October 2022
Abstract
Background: This study aimed to illustrate the prevalence of CHD by screening children in extremely high-altitude areas (over 4000 m to even 5000 m above sea level) and explore an aid model for early diagnosis and treatment for the Tibetan population. Methods: A total of 2242 students from different schools in Ngamring County, Xigaze city, Tibet from September 2019 to September 2020 were selected for screening. The students were examined through the inquiry of their current medical history and family history, cardiac auscultation and a physical examination, in order to screen out the suspected cases of CHD, and then the suspected cases were confirmed by cardiac color ultrasound examinations. After that, positive patients were be transferred to Shandong Province for free treatment. Results: The prevalence of CHD among children in Ngamring County was 3.70% (83 cases), which is the highest incidence rate ever reported. The most common type of CHD was patent ductus arteriosus (PDA), accounting for 55.42% of the total number of cases screened, followed by atrial septal defect (ASD) and ventricular septal defect (VSD), accounting for 28.92% and 12.05%, respectively. The prevalence of CHD in children at high altitude was significantly higher than that in children at low altitude. The children with CHD were transferred to Shandong Province for surgery, the operations were successful and their recoveries went well. Conclusions: The results show that high altitude is closely related to the prevalence of CHD, and the incidence in Ngamring County is much higher than that in previous reports.Keywords
Congenital heart disease (CHD) refers to the abnormal anatomical structure and function of the heart or large blood vessels during embryonic development. CHD not only seriously affects the life and quality of life of children but also brings substantial mental and economic burdens to families. In addition to genetic factors, many scholars believe that the pathogenesis of CHD is also related to environmental stimulation, and hypoxia and the cold are important influencing factors [1–3]. Ngamring is one of the counties under the jurisdiction of Xigaze city in the Tibet Autonomous region, with complex and diverse topography, basically composed of high mountains, wide valleys and lake basins, with an average altitude of 4513 meters, and climatic characteristics such as low pressure, low temperature, low oxygen and high radiation. Ngamring is one of the low-income areas in Tibet, with a weak economic foundation and poor medical conditions, and it just recently dropped out of the poverty-stricken county list in 2019.
Ngamring County has a population of more than 50,000 and an area of 39,600 square kilometers, a typical characteristic of a large sparsely populated area. As a result, there are no epidemiological data on CHD thus far in this extremely high-altitude region. The geographical and harsh climate of alpine hypoxia, coupled with the limited local medical conditions and the weak health awareness of residents, make the treatment of congenital heart disease difficult, which seriously affects the physical and mental health of children.
In recent years, the more developed areas along the eastern coast have provided targeted assistance to many impoverished counties in Tibet. Among them, Zibo City, Shandong Province has provided targeted assistance to Ngamring County. Multiple screenings for congenital heart disease have been conducted in the past two years. Various ways of raising funds for providing free treatment to children with congenital heart disease who have been screened have greatly improved the quality of life of the children. This assistance and treatment plan belongs to a new type of congenital heart disease treatment model with the participation of government and social forces and has important reference value and promotional significance.
In addition, the present study is the highest altitude (range from 4020 to 5156 meters) CHD report that is currently known. Understanding congenital heart disease and heart abnormalities in this area will further improve human understanding of congenital heart disease and provide more complete data for the development of better prevention and treatment advice.
From September 2019 to September 2020, this study conducted CHD screening for students from different schools in various townships under the jurisdiction of Ngamring County, Xigaze City, Tibet Autonomous Region. The average altitude of each township is 4513 meters above sea level. A total of 2242 students were screened.
First, the CHD screening team conducted a preliminary survey of the subjects, including current and family history inquiries, physical examinations and cardiac auscultation, and those with any of the following symptoms were further diagnosed by color Doppler echocardiography: (1) children who develop cyanosis after crying or activity and have a family history of heart disease (2) clubbing; (3) Grade II and above heart murmurs detected by auscultation; and (4) dyspnea during calm periods or after exercise. For the children who were diagnosed with CHD by color Doppler echocardiography, the screening team judged the severity of the disease and gave medical advice.
SPSS 18.0 software (Chicago, Illinois, USA) was used for all statistical analyses, and the data are expressed as numbers or percentages (%). A P < 0.05 was considered to be statistically significant.
3.1 General Information of the Participants
Among the 2242 children screened in this study, there were 1129 boys (50.36%) and 1113 girls (49.64%), ranging in age from 1 to 16, with an average age of 8.9 ± 4.6 years.
3.2 Prevalence of CHD in Children in Ngamring
Among the 2242 children examined, 972 (382 in 2019 and 590 in 2020) were examined by echocardiography. Eighty-three cases of CHD were diagnosed, with a prevalence of 3.70%. The largest constituent ratio was PDA (46 cases), accounting for 55.42% of the total cases screened, the second was ASD (24 cases, 28.92%), and the third largest was VSD (10 cases, 12.05%). No children with severe CHD were found in this screening. The details are shown in Table 1 and Fig. 1.
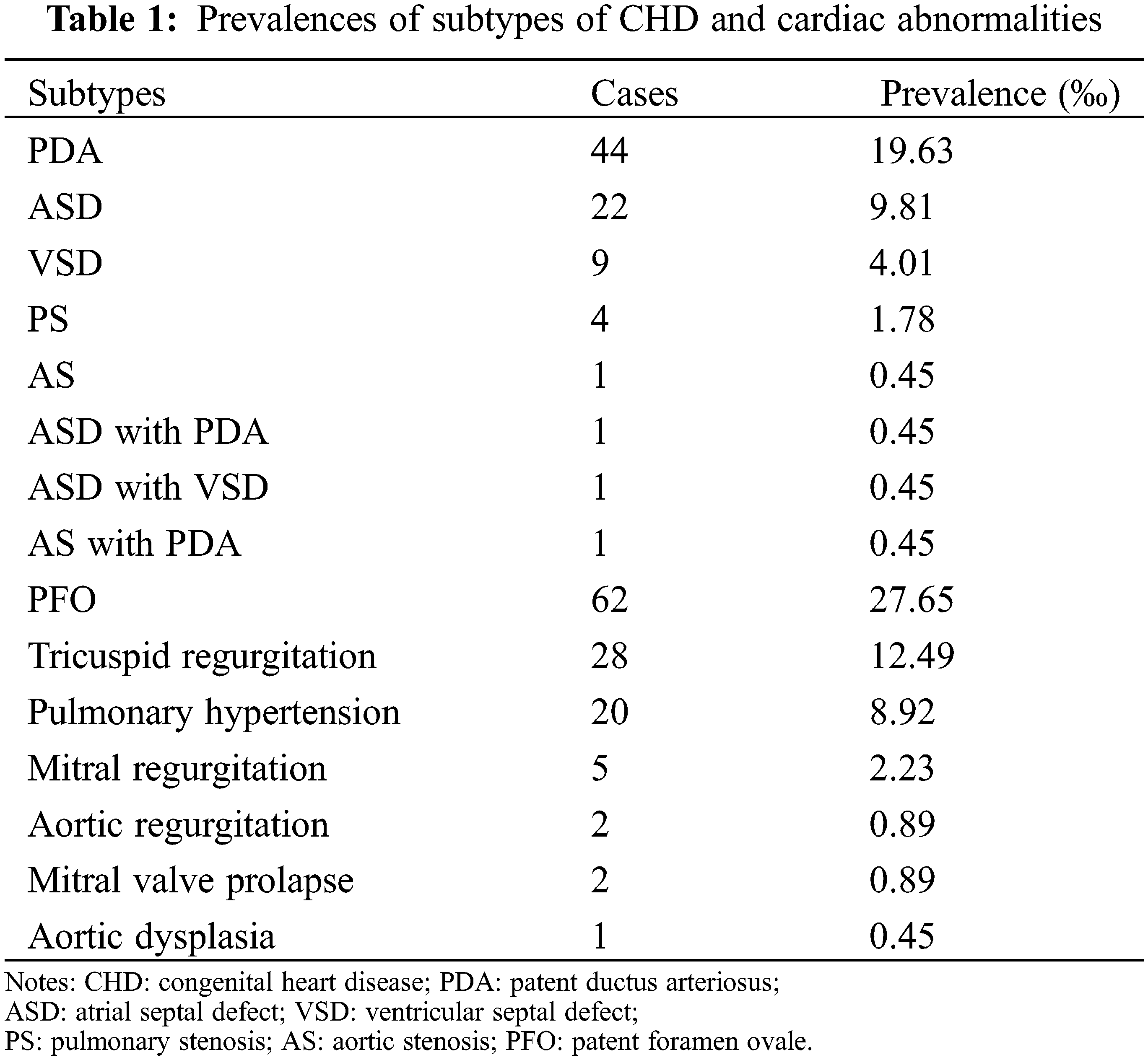
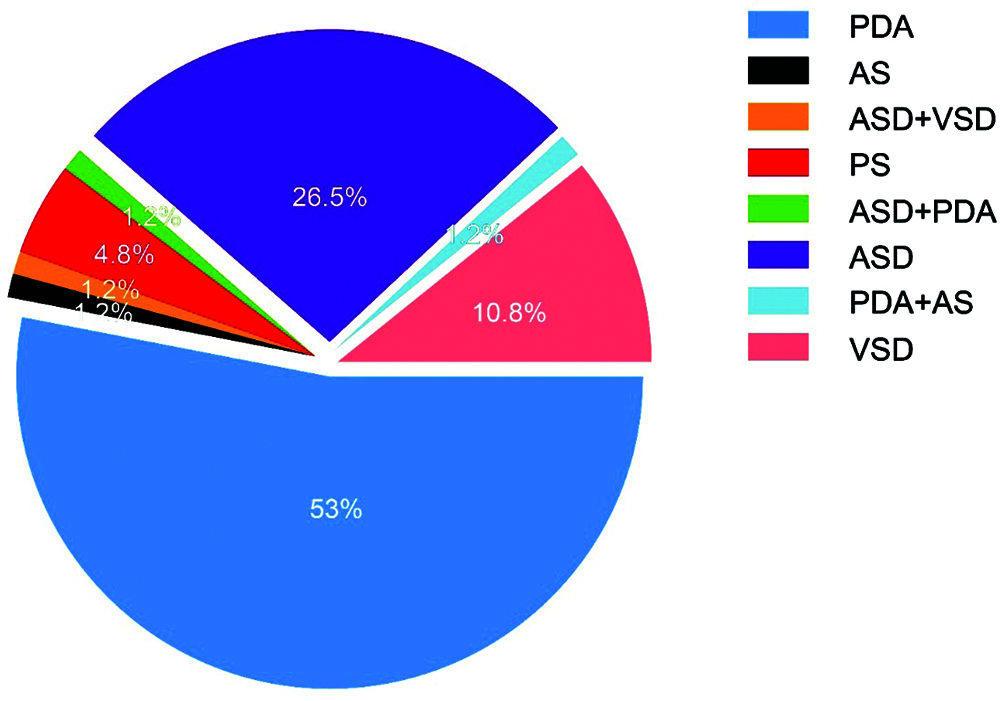
Figure 1: Subtypes of CHD
3.3 Prevalence of Different CHD Subtypes
Among the 83 children with CHD, 57 cases were single-type CHD (without any other cardiac abnormalities), accounting for 68.67% of the total number of CHD cases. Twenty-six cases of compound CHD and other cardiac abnormalities accounted for 31.33% of the total number of CHD cases. The present study showed that a single type of CHD was more common in this area. At the same time, the detection of compound CHD also suggested that a comprehensive examination should be carried out to avoid a missed diagnosis. In addition to CHD, we also found that some children have structural or functional abnormalities that did not affect their quality of life, such as a PFO within 5 mm and mild valvular regurgitation, which do not need intervention for the time being. As shown in Table 1, 2242 screened children were found to have such mild lesions, the most common being PFO (62), followed by tricuspid regurgitation (28) and pulmonary hypertension (20).
3.4 Prevalence of CHD at Different Altitudes
Through the analysis of the prevalence of CHD in children at different altitudes, it was found that the prevalence of CHD was significantly correlated with altitude. This conclusion was further confirmed by Pearson correlation analysis (R = 0.512, P = 0.030). The details are shown in Table 2 and Fig. 2.
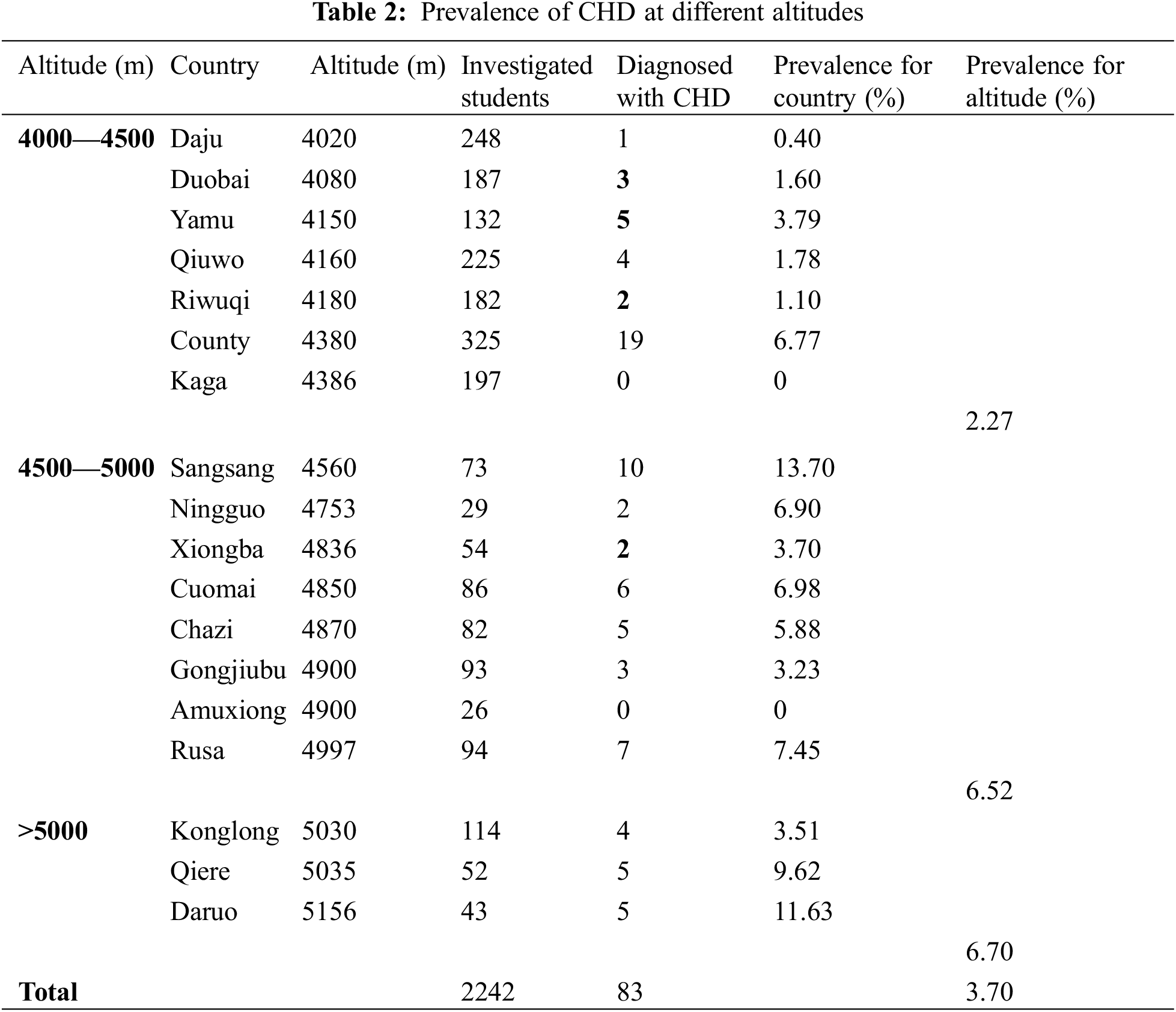
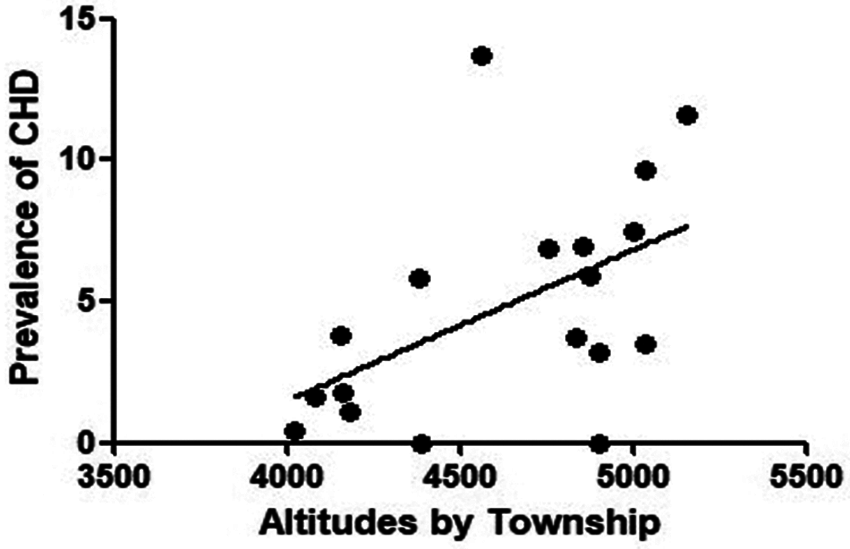
Figure 2: Correlation between CHD prevalence and altitude
3.5 Prevalence Analysis of CHD by Sex
Among the 83 children with CHD, 42 were girls, with a composition ratio of 50.60%, and 41 were boys, with a composition ratio of 49.40%. The prevalence of CHD was 3.77% in girls and 3.63% in boys. Pearson correlation analysis showed that there was no significant correlation between the prevalence of CHD and sex differences (X2 = 0.032, P = 0.895).
3.6 Intervention and Follow-Up Results for Children with CHD in Ngamring
A total of 164 children with previous or current suspected CHD or other cardiac abnormalities were detected in this screening. After a comprehensive analysis of the disease, the screening team concluded that 81 children did not need surgery because they had only mild cardiac structural or functional changes that did not affect their quality of life, such as PFO within 5 mm and mild valvular regurgitation, and only needed regular follow-up observation. One child could not tolerate surgery because of her poor general condition, and 5 children underwent CHD surgery. The screening team made recommendations on surgical treatment for 77 children. After communicating with them, 45 children’s families refused surgical treatment because of inconvenient transportation or other factors, and the other 32 children and their families agreed to surgical treatment. A total of 17 children underwent surgery in Zibo Central Hospital (8 in 2019 and 9 in 2020), and 15 children underwent surgery in Jinan Central Hospital in 2020. Among the 32 children, 18 children had PDA, 8 children had ASD, 1 child had PDA+AS, 1 child had ASD+VSD, and 1 child had PDA+ASD. In the other 3 children, no abnormalities were found after comprehensive evaluation during the operation. All 29 children who underwent surgery were operated on successfully and recovered well after the operation. The details are shown in Fig. 3.
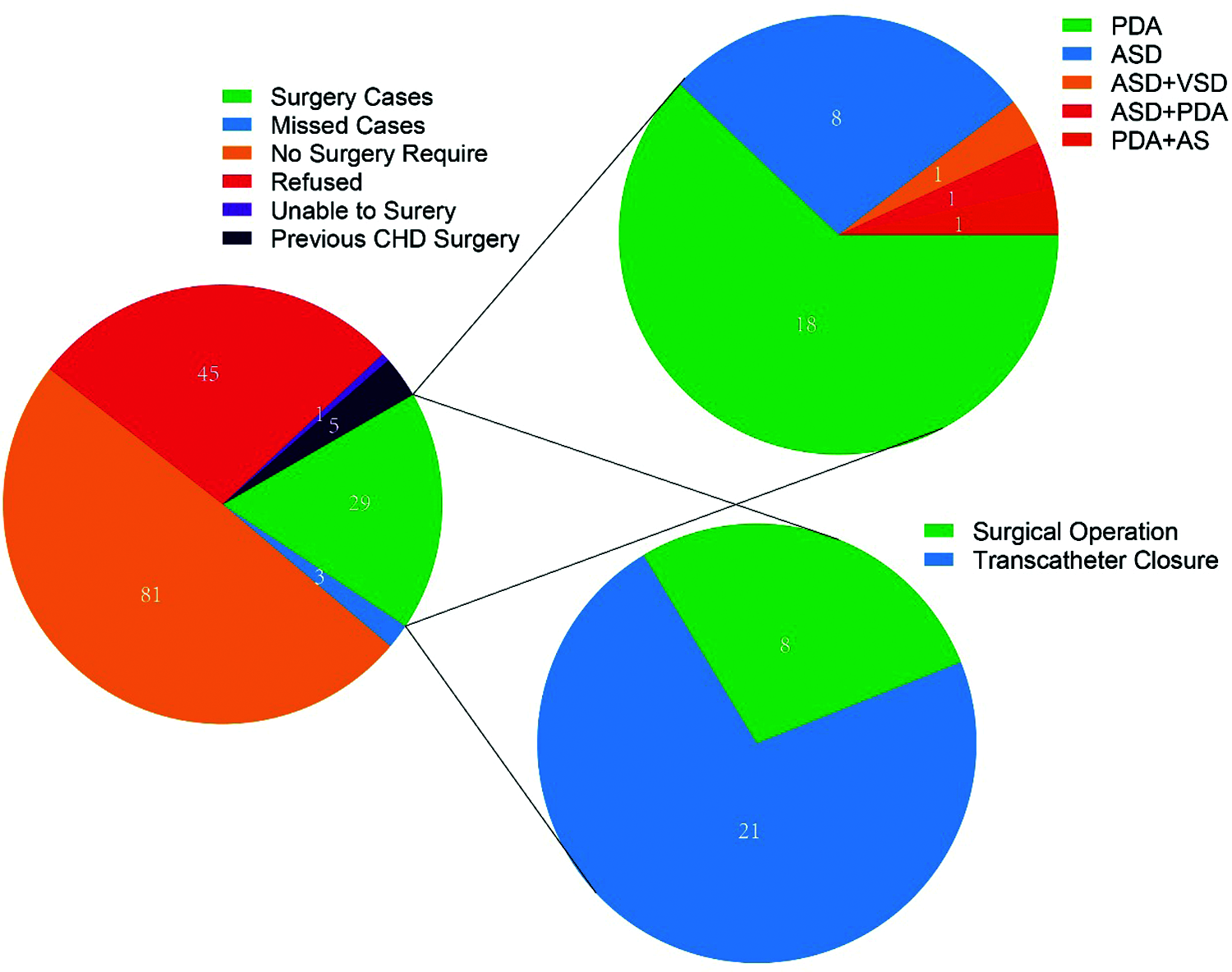
Figure 3: Operation details
Data have shown that CHD is the most common congenital malformation in China and even in the world, and more than one million babies with CHD are born every year [4]. From 1980 to 2019, the total CHD birth prevalence rate in China increased, except for a slight decrease in 1990–1994, and it showed a sharp upward trend in 2005–2019 [5]. CHD not only seriously affects the quality of life of the population born with it but also increases the family burden. In previous studies of the prevalence of CHD in high-altitude areas, Ecuador showed an incidence rate of 0.71%, with an altitude range from 2500 to 3264 m [6], while Nagqu city of Tibet in China showed an incidence rate of 0.52%, with an average altitude of 4000 m [7]. However, in the present screening for 2 years in Ngamring County, the prevalence of CHD was 3.70%, which was much higher than that in previous reports. Although there are a number of reasons, higher altitude (4020–5156 m), lower atmospheric pressure and oxygen content are undoubtedly the first to blame. Low partial pressure of oxygen inhibits the contraction and spontaneous closure of ductus arteriosus after birth [8]. This study confirmed the positive correlation between CHD prevalence and high-altitude locations.
Among the CHD cases screened at this time, the most common type of CHD was PDA, which was consistent with previous research results [7]. To our surprise, most cases are relatively simple congenital heart diseases. Among the two years of screening, we did not find patients with complicated congenital heart diseases, such as tetralogy of Fallot. We suspected that patients with complicated congenital heart disease might die prematurely in such a poor living environment with low oxygen. In contrast, children who survived were often patients with milder illnesses and less impacted hemodynamics. In some previous studies on the prevalence of CHD at high altitude, there was no consistent conclusion on sex differences in the prevalence of VSD [9–11]. In this screening, all the children with VSD were boys, who may be related to the higher early mortality of VSD and different physique of girls than boys, so there were few girls who survived VSD. Of course, it is also possible that there is a sex difference in the prevalence of VSD at high altitude, and further research is needed on this issue. In this study, the incidence of VSD was relatively low, possibly because nearly half or more of VSD cases can be closed naturally before children reach preschool age. Our screening targets were mainly school-age children, which is why VSD had a low incidence rate.
There are still some limitations of this study. Since this study selected school children in Xigaze for screening, the data obtained are the prevalence rate of CHD rather than the incidence rate of CHD in newborns. In this sense, screening newborns in the future may provide more additional and precise information.
In addition, from the perspective of social welfare, this CHD screening project was a part of the developed coastal areas’ aid to Tibet in China. The hospitalization and round-trip expenses of all 32 surgical patients was sponsored by government funds and public welfare enterprises. However, although the governments of Shandong Province and Zibo city provided enough funding and all children were treated free of charge, more than half of the Tibetan families refused treatment for various reasons. This also prompted us to consider how to improve the health awareness of Tibetan people, especially those in remote pastoral areas, which is a social problem that urgently needs to be solved. Although the patients with congenital heart disease screened this time have not been fully treated, this program provided a good example for the future treatment of congenital heart disease in Tibet.
Xigaze City is located in a high-altitude area, with backward economic conditions and a lack of medical resources. There are few studies on the prevalence of CHD in Tibet. This study conducted CHD screening on children in various townships in the Xigaze area, filled the gap in the data on the prevalence of CHD in this area, and provided data and clinical guidance for the prevalence, prevention and treatment of CHD in high-altitude areas.
The round-trip expenses of the children from Tibet who traveled to Shandong for surgery are borne by the ninth Tibet aid working group. All the expenses of the children who received surgery in Zibo Central Hospital during their hospitalization were coordinated by the ninth Tibet aid working group of Zibo City and jointly borne by the Medical Insurance Bureau and Yangzijiang Medicine, with a total cost of 518021.18 yuan. All the expenses of the children who received surgery in Jinan Central Hospital during their hospitalization were borne by the Red Cross Fund, with a total cost of 562012.82 yuan.
Ethical Approval: The Ethics Committee of Zibo Central Hospital approved the study and written informed consent was obtained from the guardians of the children.
Funding Statement: The authors received no specific funding for this study.
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
References:
1. Whayne, Thomas Jr, F. (2014). Altitude and cold weather: Are they vascular risks? Current Opinion in Cardiology, 29(4), 396–402. DOI 10.1097/HCO.0000000000000064. [Google Scholar] [CrossRef]
2. Madrigano, J., Mittleman, M. A., Baccarelli, A., Goldberg, R., Melly, S. et al. (2013). Temperature, myocardial infarction, and mortality: Effect modification by individual- and area-level characteristics. Epidemiology, 24(3), 439–446. DOI 10.1097/EDE.0b013e3182878397. [Google Scholar] [CrossRef]
3. Paranka, M. S., Brown, J. M., White, R. D., Park, M. V., Kelleher, A. S. et al. (2018). The impact of altitude on screening for critical congenital heart disease. Journal of Perinatology, 38(5), 530–536. DOI 10.1038/s41372-018-0043-9. [Google Scholar] [CrossRef]
4. van der Linde, D., Konings, E. E., Slager, M. A., Witsenburg, M., Helbing, W. A. et al. (2011). Birth prevalence of congenital heart disease worldwide: A systematic review and meta-analysis. Journal of the American College of Cardiology, 58(21), 2241–2247. DOI 10.1016/j.jacc.2011.08.025. [Google Scholar] [CrossRef]
5. Zhao, L., Chen, L., Yang, T., Wang, T., Zhang, S. et al. (2020). Birth prevalence of congenital heart disease in China, 1980–2019: A systematic review and meta-analysis of 617 studies. European Journal of Epidemiology, 35(7), 631–642. DOI 10.1007/s10654-020-00653-0. [Google Scholar] [CrossRef]
6. González-Andrade, F. (2020). High altitude as a cause of congenital heart defects: A medical hypothesis rediscovered in Ecuador. High Altitude Medicine & Biology, 21(2), 126–134. DOI 10.1089/ham.2019.0110. [Google Scholar] [CrossRef]
7. Chun, H., Yue, Y., Wang, Y., Dawa, Z., Zhen, P. et al. (2019). High prevalence of congenital heart disease at high altitudes in Tibet. European Journal of Preventive Cardiology, 26(7), 756–759. DOI 10.1177/2047487318812502. [Google Scholar] [CrossRef]
8. Zheng, J. Y., Tian, H. T., Zhu, Z. M., Li, B., Han, L. et al. (2013). Prevalence of symptomatic congenital heart disease in Tibetan school children. The American Journal of Cardiology, 112(9), 1468–1470. DOI 10.1016/j.amjcard.2013.07.028. [Google Scholar] [CrossRef]
9. Zhao, Q. M., Liu, F., Wu, L., Ma, X. J., Niu, C. et al. (2019). Prevalence of congenital heart disease at live birth in China. The Journal of Pediatrics, 204, 53–58. DOI 10.1016/j.jpeds.2018.08.040. [Google Scholar] [CrossRef]
10. Han, S., Wei, C. Y., Hou, Z. L., Li, Y. X., Ding, Y. C. et al. (2020). Prevalence of congenital heart disease amongst schoolchildren in southwest China. Indian Pediatrics, 57(2), 138–141. [Google Scholar]
11. Cao, Y., Liu, Y. M., Li, X. F., Chi, H. T., Li, T. C. (2017). Prevalence and composition of CHD at different altitudes in Tibet: A cross-sectional study. Cardiology in the Young, 27(8), 1497–1503. DOI 10.1017/S1047951117000567. [Google Scholar] [CrossRef]
Cite This Article
 Copyright © 2022 The Author(s). Published by Tech Science Press.
Copyright © 2022 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools