 Open Access
Open Access
ARTICLE
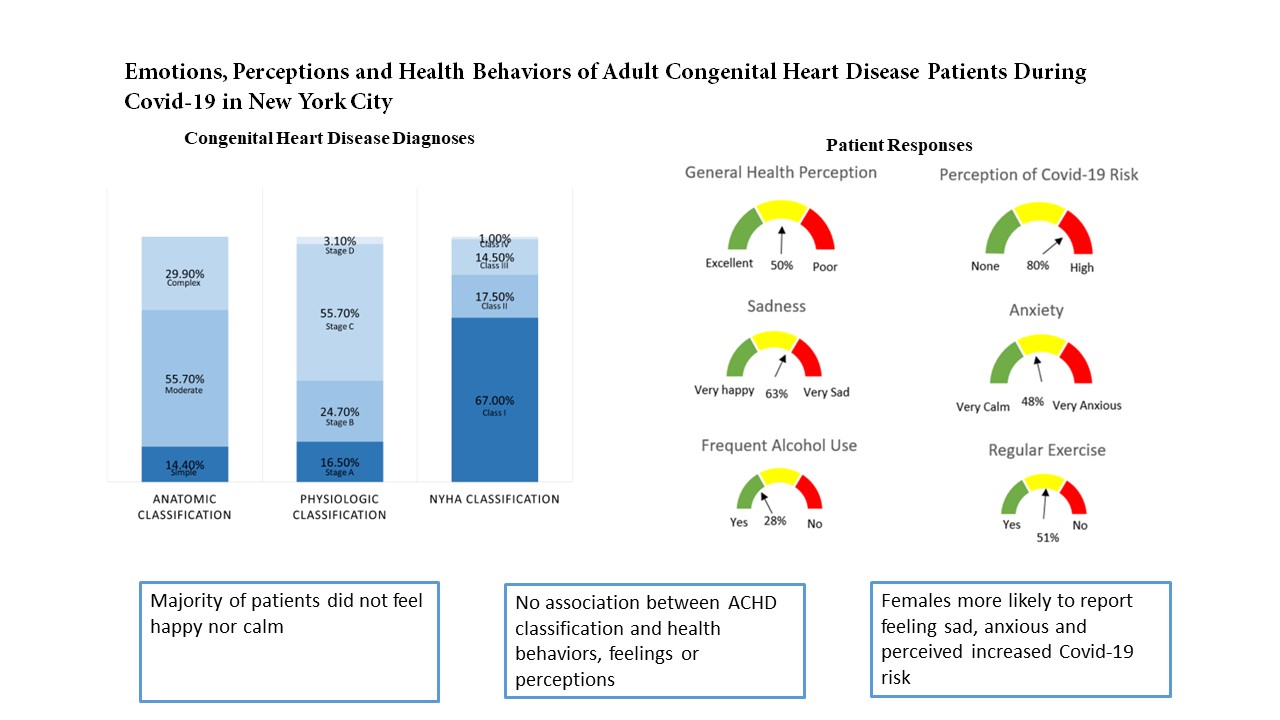
Emotions, Perceptions and Health Behaviors of Adult Congenital Heart Disease Patients during COVID-19 in New York City
1 Leon H. Charney Division of Cardiology, NYU Grossman School of Medicine, New York, USA
2 Department of Medicine, NYU Grossman School of Medicine, New York, USA
3 Department of Psychiatry, NYU Grossman School of Medicine, New York, USA
4 Department of Cardiology, Mount Sinai Morningside, New York, USA
* Corresponding Author: Dan G. Halpern. Email:
Congenital Heart Disease 2022, 17(5), 519-531. https://doi.org/10.32604/chd.2022.024174
Received 25 May 2022; Accepted 25 July 2022; Issue published 06 September 2022
Abstract
Background: Adults with congenital heart disease (ACHD) have increased prevalence of mood and anxiety disorders. There are limited data regarding the influence of the COVID-19 pandemic on the mental health and health behaviors of these patients. Objective: The purpose is to evaluate the perceptions, emotions, and health behaviors of ACHD patients during the COVID-19 pandemic. Methods: In this cross-sectional study of ACHD patients, we administered surveys evaluating self-reported emotions, perceptions and health behaviors. Logistic regressions were performed to determine the adjusted odds of displaying each perception, emotion and health behavior based on predictor variables. Results: Ninety-seven patients (mean age 38.3 years, 46.4% female, 85.6% moderate or complex lesion) completed the survey. The majority of patients reported feeling moderately or very sad (63.1%), and 48.4% of patients identified themselves as feeling moderately or very anxious. The majority of patients perceived their risk of COVID-19 as moderate or high. Females were more likely to report feeling sad and anxious (95% CI 1.06–10.96, p-value 0.039, and 95% CI 1.44–15.30, p-value = 0.012, respectively), and were associated with higher odds of having a perceived increased risk of COVID-19 (95% CI 1.33–10.59, p-value 0.012). There was no association between ACHD anatomic or physiologic classification and perceptions, emotions and health behaviors. Conclusions: Females were more likely to report feeling sad, anxious and an increased risk of COVID-19 in comparison to males. These findings indicate the need for mental health support and promotion of health behaviors during the pandemic amongst all ACHD patients, regardless of underlying condition.Graphic Abstract
Keywords
Adults with congenital heart disease (ACHD) represent a heterogeneous, unique population with lifelong complex medical problems, which often coincide with psychological challenges [1]. ACHD patients have increased prevalence and risk of mood and anxiety disorders, as well as significantly higher risk of post-traumatic stress disorders, which may be related to numerous hospitalizations, active medical needs and developmental challenges in childhood [1–3]. The 2018 ACC/AHA ACHD guidelines emphasize the importance of mental health support and positive health behaviors to improve general and cardiovascular health outcomes amongst this patient population [4].
The severe acute respiratory syndrome coronavirus 2 (COVID-19) pandemic has revealed unprecedented challenges internationally, particularly amongst patients with chronic illness. Studies have demonstrated that the COVID-19 pandemic is associated with distress, anxiety, fear, depression and insomnia, and previous epidemics have been associated with increased suicide rates [5]. The COVID-19 pandemic has led to an increase in sedentary behavior and a change in physical activity during quarantine in the general population [6]. During the COVID-19 pandemic, children with congenital heart disease were found to have fewer active lifestyles, as well as an increase in BMI, in comparison to before the pandemic [7,8]. In a study of young ACHD patients in Switzerland, congenital heart patients were more concerned about their health during the pandemic than their healthy peers [9]. Another study based in British Columbia found that a substantial proportion of ACHD patients reportedly significant psychological distress during the pandemic [10].
While there are now more adults than children living with congenital heart disease due to advances in medicine and surgery, there are limited data on the mental health and behaviors of ACHD patients during the COVID-19 pandemic in the United States. The purpose of this study is to evaluate perceptions, emotions and health behaviors during the COVID-19 pandemic on an ACHD cohort at a large academic medical center in New York City, one of the first epicenters of the pandemic.
In this cross-sectional study, we included adults 18 years of age or older with a history of congenital heart disease. Patients who were nonverbal, pregnant or had significant cognitive impairment were excluded. Patients who met inclusion criteria were recruited through two methods. Patients were invited to participate during routine clinic visits and patients received an email invitation with initial study information. The study recruitment period was complete after 100 participants volunteered. Study protocols were approved by the NYU Office of Science and Research Institutional Review Board (study number i20-02053).
We administered surveys to explore patient self-reported emotions, perceptions, and health behaviors during the pandemic. The survey questions were adapted based on two published surveys. The Coronavirus Health Impact Survey (CRISIS) was developed during the pandemic to assess COVID-19 relevant behavioral and social science domains, with proven feasibility, psychometric structure, and construct validity [11]. The Health Behaviors Scale–Congenital Heart Disease is a tool that has been utilized, validated and published amongst adults with congenital heart disease, notably in the large, international APPROACH-IS study [12]. In our survey, the COVID-19 pandemic was defined as starting in March 2020. To evaluate emotions, we included questions from the CRISIS survey that utilized a Likert scale to assess self-reported range of emotions. To evaluate perception of physical health, we included a question from the CRSIS survey that utilized a Likert scale. To evaluate perception of patient’s COVID-19 risk, we developed a question using a Likert scale to range perception of COVID-19 risk. To evaluate health behaviors, we included the questions in the Health Behaviors-Scale–Congenital Heart Disease questionnaire dedicated to evaluating substance use and exercise [13].
Demographic data were obtained from the surveys and extracted through medical record review of EPIC (Epic Systems, Verona, WI). The baseline data were obtained from EPIC from March 2019–2020. The following demographic data points were collected via the institution’s electronic medical record: Age (years), gender, (male, female), weight (lbs.), body mass index (BMI), primary diagnosis of congenital heart disease and type of repair, complexity of primary congenital heart disease diagnosis (simple, moderate, complex), physiological classification of congenital heart disease based on ACHD guidelines (A,B,C or D), NYHA functional classifications (I–IV), repaired (yes, no), age of most recent surgery and procedure, co-morbidities (including clinical diagnosis of depression and clinical diagnosis of anxiety), current medications, history of arrhythmia, hemoglobin, cyanosis (SpO2 < 90%), systemic ventricle, diagnosis of depression, diagnosis of anxiety.
Baseline patient characteristics of the sample were examined using descriptive analyses and summarized using frequencies and percentages. Logistic regressions with multivariate analysis were performed to determine the adjusted odds of displaying each clinically significant outcome of emotions, perceptions, and health behaviors based on predictor variables of age, sex, ACHD classification, education status, employment, depression and anxiety. These predictor variables were selected based on the Approach-IS trial, which looked at associations between similar predictor variables and health behaviors. This analytic plan was based on the approach utilized in the international APPROACH-IS study, which looked for associations between similar demographic variables and health behavior outcomes [12]. Statistical significance was defined as p-value less than 0.05.
Of the 80 participants invited to participate during their routine clinic visit, 78 volunteered to participate. There were 2 patients who declined to participate; one patient reported he did not have time and the other patient reported she was “too anxious” to complete a survey. In addition, a one-time email was sent to the ACHD program patients who have an email address listed with an invitation to participate; the first 28 participants that expressed interest via email in participating in the survey were invited to participate. No further participants were accepted as we had reached our sample goal. Three patients who expressed interest via email did not meet inclusion criteria. Of the 25 interested participants, there were 19 participants that responded to follow up information regarding the consent process and then completed the survey. There was a total of 97 participants.
There were 45 (46.4%) female participants, and the average age of the participants was 38.3 years. Of the participants, 85.6% had previously undergone open heart surgery (Table 1). Based on the ACC/AHA ACHD 2018 anatomic classification system, our study included patients with simple (14.4%), moderate (55.7%) and complex (29.9%) heart disease. Based on the ACC/AHA ACHD 2018 physiologic classification system, the majority of patients in our study were class C (55.7%) functional status, followed by class B (24.7%), class A (16.5%), and class D (3.1%) (Fig. 2). The most common diagnosis was repaired tetralogy of Fallot (Fig. 1). There were 24 (24.7%) patients admitted to the hospital in the year prior to the pandemic. Of the patients admitted, 12 (50%) of the patients were admitted for cardiac reasons such as arrhythmia or heart failure exacerbation. At baseline, 35.1% of patients had a clinical diagnosis of depression, 48.5% of patients had a clinical diagnosis of anxiety, and 36.1% were taking anti-depressants. There were 18 patients who were suspected of having a COVID-19 infection (10 patients had a positive test, 1 patient was diagnosed by a doctor without a test, and 7 patients had symptoms but were unable to get tested).

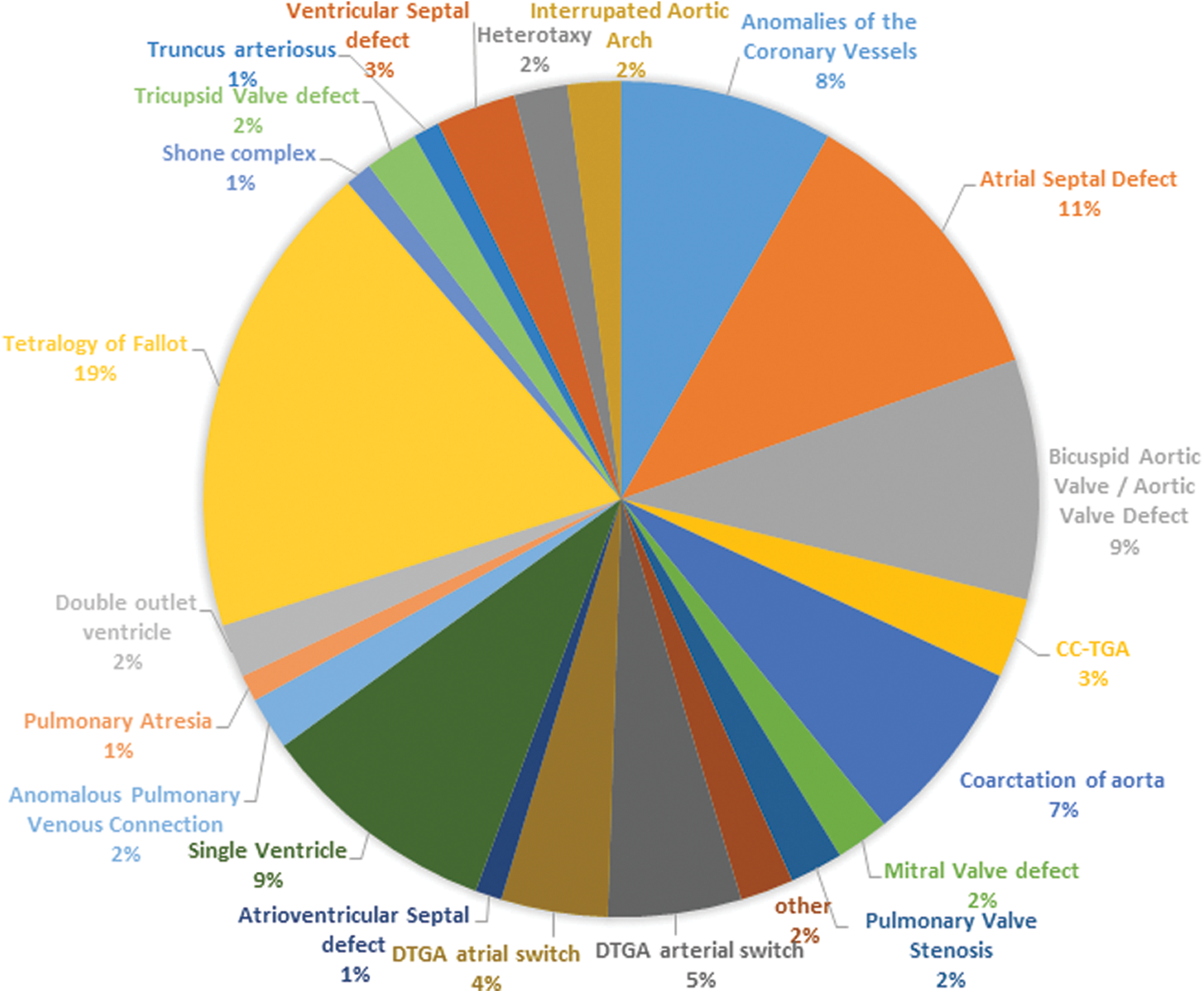
Figure 1: Distribution of ACHD diagnoses
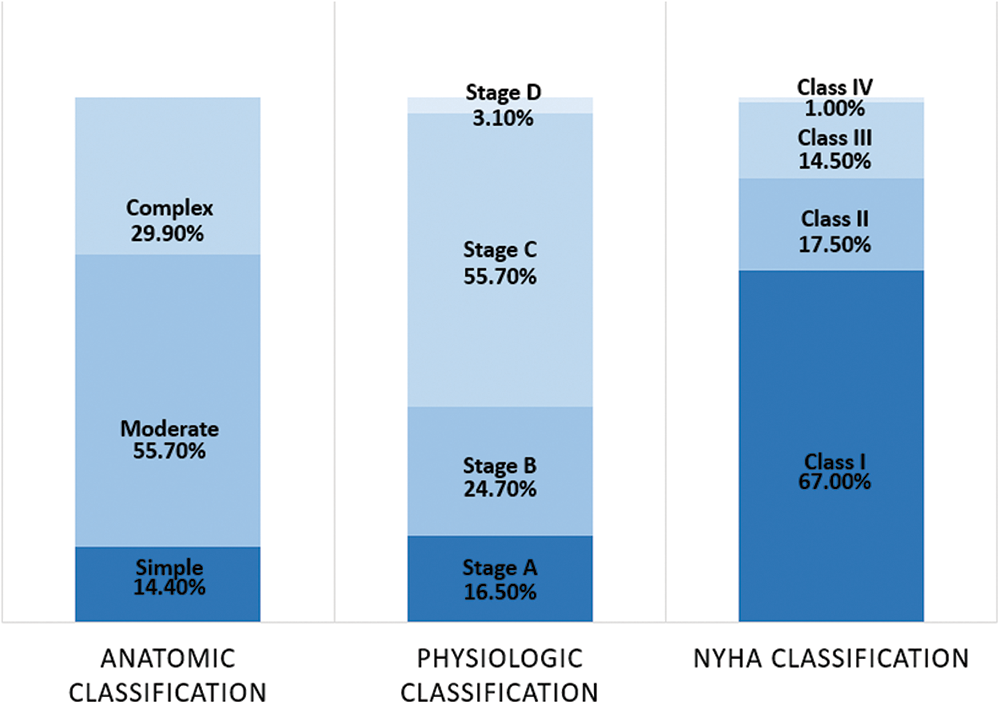
Figure 2: Distribution of anatomic, physiological and NYHA classifications
This figure demonstrates the percentages of ACHD diagnoses of patients included in this study.
This figure demonstrates the breakdown of patients in the study by ACC/AHA ACHD 2018 anatomic and physiological classification system, and New York Heart Association Functional Classification system.
Patients identified their self-rated physical health most commonly as “good” (49.5%). The majority of patients perceived their risk of COVID-19 as moderate or high (79.4%). The majority of patients reported feeling moderately or very sad (63.1%), and 48.4% of patients identified themselves as feeling moderately or very anxious (Table 2).

There were 26.8% of patients that reported frequent alcohol use. Of the 66 patients (68.0%) who reported drinking alcohol, 14 (21.2%) reported drinking 4 or more times per week and 18 (27.3%) reported having at least 3 drinks at a time. There were 34.0% of patients that reported drug use (the majority of drug use was marijuana). During the COVID-19 pandemic, 50.5% of patients reported they participated in regular exercise (Table 3). Fig. 3 summarizes the emotions, perceptions and health behaviors.

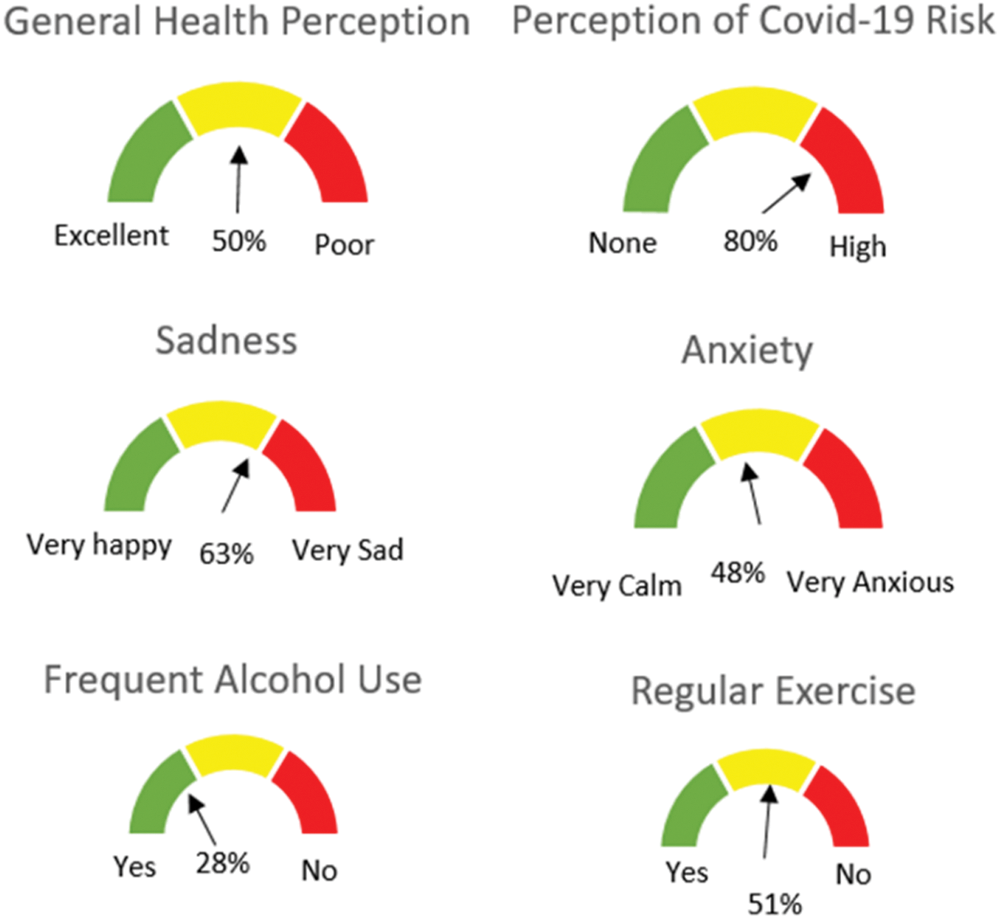
Figure 3: Key takeaways of perceptions, emotions and health behaviors
This figure demonstrates the patient responses to questions regarding emotions, perceptions and behaviors.
3.5 Perceptions and Emotions by Predictor Variables
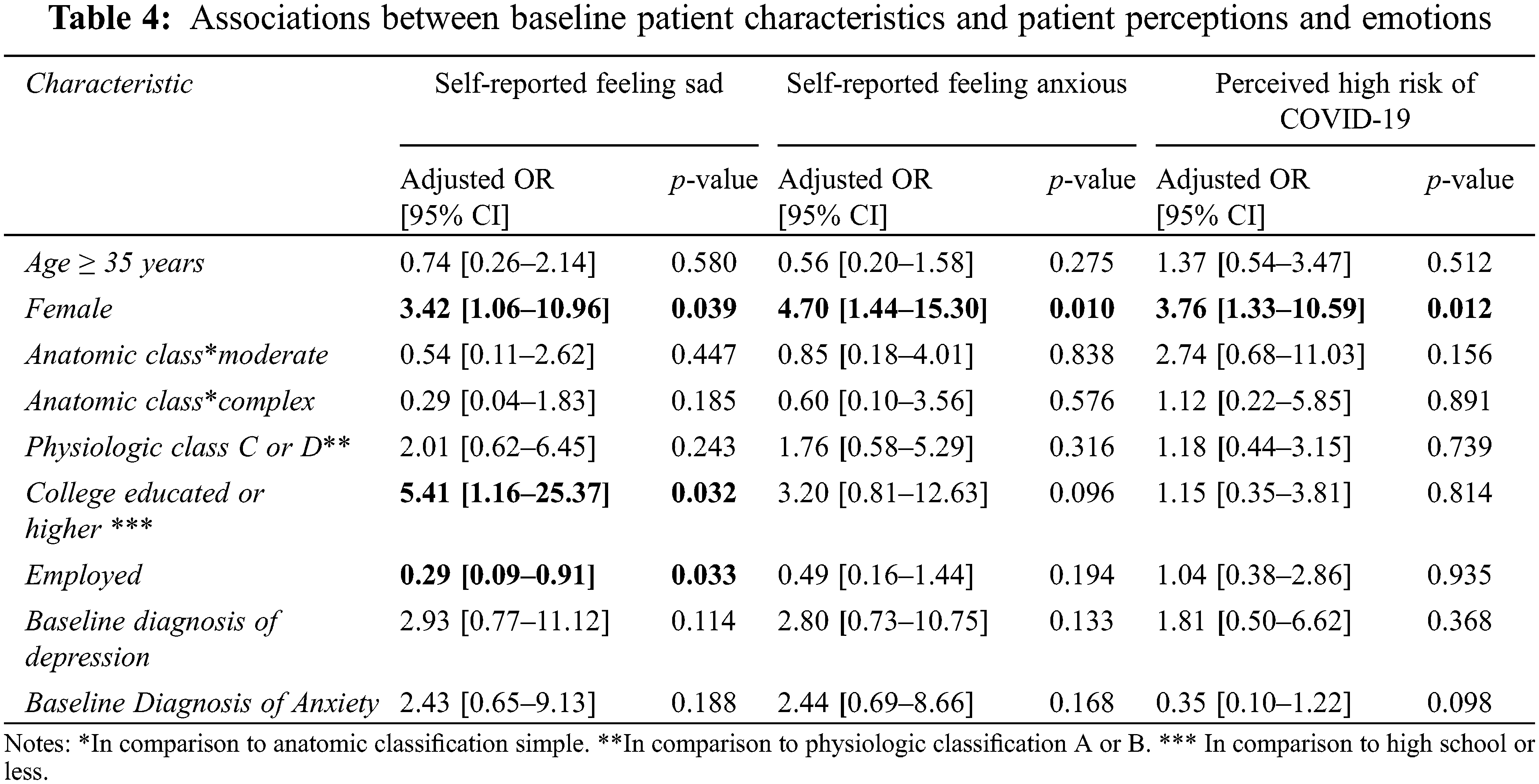
Females were more likely than males to report feeling sad and feeling anxious (95% CI 1.06–10.96 with p-value 0.039, and 95% CI 1.44–15.30 with p-value = 0.012, respectively). There were associations between status of employment, education level and feeling sad. There was no association between ACHD anatomic and physiologic classification and perceived COVID-19 risk. However, female sex was associated with higher odds of having a perceived high risk of COVID-19 (95% CI 1.33–10.59; p-value 0.012; see Table 4).
3.6 Health Behaviors by Predictor Variables
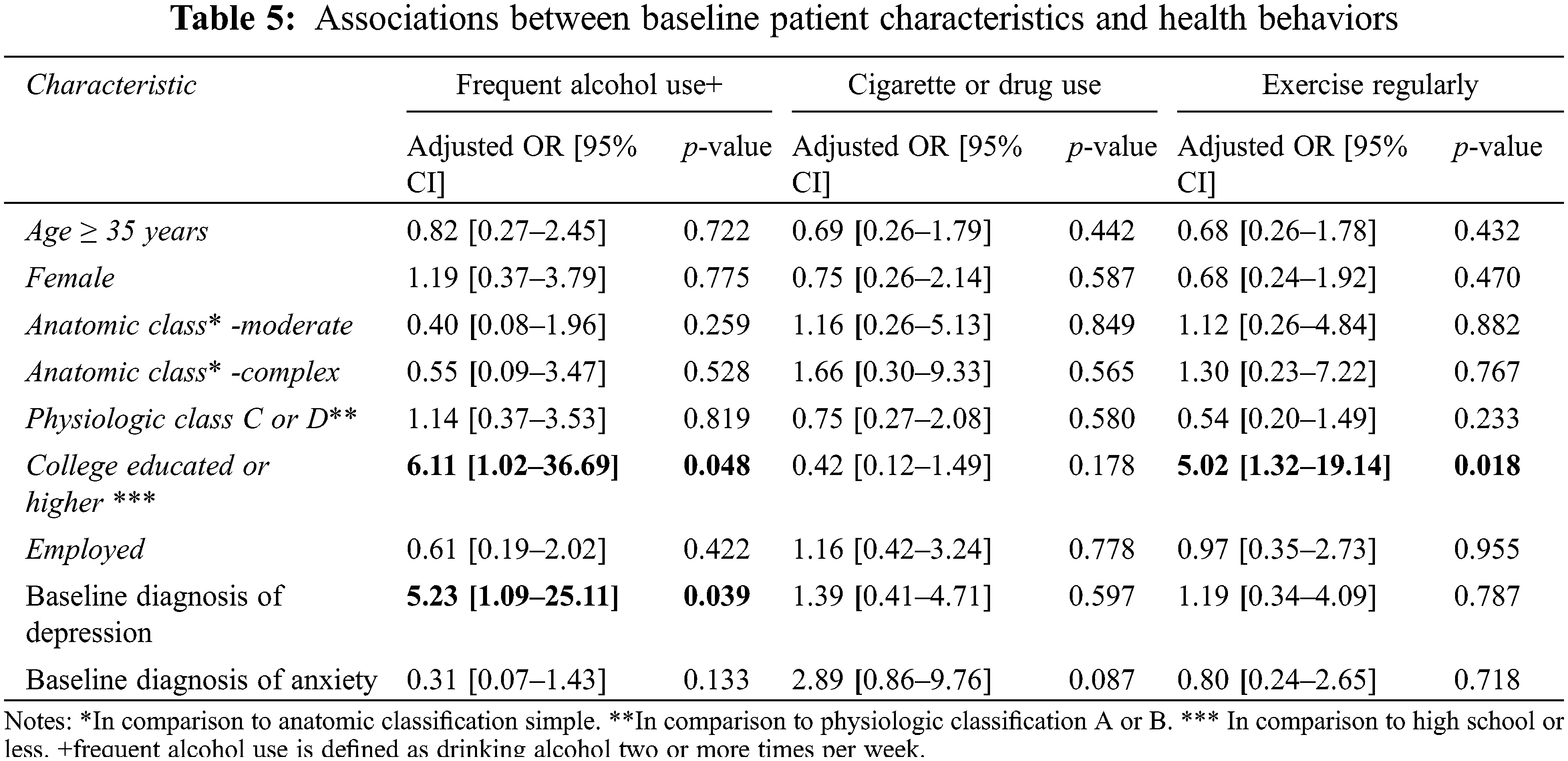
Having a college or higher education was associated with higher odds of frequent alcohol use but also with regular exercise (95% CI 1.02–36.69 with p-value = 0.048 and 95% CI 1.32–19.14 with p-value = 0.018, respectively). There was no significant relationship between ACHD classification and health behaviors (see Table 5).
Our study investigates perceptions, emotions and health behaviors during the COVID-19 pandemic in a diverse population of ACHD patients, of whom the majority were moderate anatomic complexity and classes B or C physiologic stage. The majority of patients were neither happy nor calm, reinforcing the need for increased mental health resources and collaboration with social work to support ACHD patients during the pandemic [14].
While the majority of patients perceived themselves to be in at least good physical health, most patients reported their risk of COVID-19 to be moderate or high. Interestingly, there was no association between ACHD anatomic, or physiologic classification and perception of COVID-19 risk. A recent large international registry of COVID-19 in ACHD patients demonstrated that the most vulnerable populations to COVID-19 were those with worse physiological stage (of note, this study defining high-risk groups was not published at the time this survey was conducted). According to this registry, patients with the following conditions had a 15% or greater chance of having severe case of COVID-19 or fatality: Eisenmenger physiology, cyanosis (SpO2 < 90%), pulmonary arterial hypertension, congenitally corrected transportation of the great arteries and transposition of the great arteries s/p atrial switch [15]. These high-risk patients were not any more likely to perceive themselves as at an increased risk from COVID-19 in our study. A study with a slightly older cohort of ACHD patients in Canada also found no consistent trend in responses with regard to ACHD anatomic or physiologic classification [10]. Prior studies have demonstrated deficits among ACHD patients in awareness and knowledge about their congenital heart disease, which has been attributed to difficulty in care transitions and being lost to follow-up [16]. This lack of awareness may also impact their understanding of their risk related to COVID-19. At the time of initiation of the survey, per CDC, patients with heart disease may be more likely to have severe infection from COVID-19, but there was not data specifically for ACHD patients and COVID-19 readily available. The lack of correlation between ACHD anatomic or physiologic classification and perception of COVID-19 risk suggests that there are other factors influencing one’s risk perception beyond their underlying condition.
Females with ACHD were more likely to perceive themselves as having a high risk of COVID-19 in comparison to males with ACHD. The female sex was also associated with higher odds of feeing sad or anxious in comparison to males. These findings are consistent with studies of the ACHD population prior to COVID-19, which have shown that female sex is more likely to be associated with anxiety symptoms [10,17,18]. Women may be more likely to perceive their own need for and seek mental health support, which may impact their self-awareness and self-reporting [19]. During the pandemic, women may have had a greater disruption in their everyday life. The increased burdens of childcare and housework disproportionately affected women, as well as a persistent reduction in employment and increased likelihood of job loss and income reduction amongst women [20–22].
There was no significant relationship between ACHD anatomic or physiologic classification and health behaviors including regular exercise and substance use; health behaviors were instead associated with demographics such as level of education. In our study, 50.5% of patients reported participation in regular exercise during the pandemic. The APPROACH-IS trial, a multicenter, international study of over 4000 patients with ACHD that utilized the Health Behaviors-Congenital Heart Disease surveys, demonstrated that only 34% of ACHD patients in the US subgroup reported participation in sports. Higher education level was associated with higher odds of regular exercise in both studies [12]. The pandemic allowed many individuals to work from home, follow adjusted schedules and reduce commuting time, which may have allowed more time for exercise. Our study also showed that employed individuals were less likely to feel sad. The portion of the Approach-IS study focusing on quality of life found that lack of employment was associated with lower quality of life as well [23].
We also found that higher education was associated with higher odds of frequent alcohol use. In the literature, the relationship between education level and alcohol use varies, depending on the type of alcohol use, definition of frequent alcohol use, and the sample of participants [24,25]. One small study on health behaviors prior to the pandemic in a young ACHD cohort showed that over half of young adults reported significant substance use, with 41% of ACHD patients using marijuana, 81% of patients using alcohol, and 44% of patients binge drinking [26]. Drug and alcohol use in the ACHD population is concerning due to the arrhythmogenic potential of marijuana and myopathic, hepatotoxic and arrhythmogenic effects of alcohol in ACHD patients [26].
We reviewed studies of the impact of COVID-19 on the general population to compare findings to our data amongst ACHD patients, although not a direct comparison. The Coronavirus health and Impact Survey (CRISIS), which was also used in the general population of almost 2,000 adults in the US and UK during the pandemic, demonstrated associations between the female gender and feelings and moods, similar to our study [11]. COVID-19 worries were the first (UK) or second (US) most important predictor of current mood states amongst adults, which suggest that fear and worry about COVID-19 are significant factors impacting adverse mental health outcomes [11]. Another study of greater than 1000 US adults found unemployment to be associated with symptoms of depression and stress [27]. Interestingly, our study seemed to have relatively high exercise rates during the pandemic, while other studies of adults generally showed decreased physical activity and increased sedentary lifestyle [28,29].
Our study did not demonstrate a statistical correlation between baseline diagnosis of depression and self-reported feeling sad. We suspect many of our patients with anxiety and depression may be well managed and receiving treatment, as 35.1% of patients had depression at baseline, 48.5% had anxiety at baseline, and 36.1% were taking an anti-depressant agent. These baseline rates are similar to prior studies in the ACHD population; one review reports 24% of ACHD patients have depression and 38% have anxiety [1]. Additionally, when the baseline diagnoses of depression and anxiety were combined together for statistical analysis, there was a strong correlation between baseline mental health condition diagnosis and feeling sad/anxious. Further studies should also evaluate the association between COVID-19 risk perception and depression and anxiety, as COVID-19 worries, and pandemic-associated life changes are noted to be drivers of adverse mental health outcome [11].
This study is limited by its small sample size and lack of serial measures. While there is data regarding health behaviors and emotions of ACHD patients from pre-COVID-19 and data during the pandemic in the general population, we do not have data on this specific cohort prior to the pandemic to use as a comparison point. We also acknowledge the limitations of the self- report and recall biases. There is self-report bias in reporting substance use, and patients may want to present themselves in a positive light and therefore downplay their poor health behaviors, although anonymity was assured. Additionally, there was a selection bias, as a majority of patients in the study were recruited via clinic visit. Patients who do not attend routine clinic visits may have responded differently to questions than those who do. Patients who expressed interest via email may also respond differently to questions than those who did not express interest in participating in a voluntary survey.
This study is the first to investigate health behaviors, in addition to perceptions and emotions, of ACHD patients in New York City during the pandemic. Many of our ACHD patients reported feeling moderately to severely sad and depressed during the pandemic. While the majority of patients perceived themselves to be in at least good physical health, most patients reported themselves to be at a higher risk of COVID-19. There was no association between ACHD anatomic or physiologic classification and emotions, perceptions or behaviors; instead, outcomes were more likely to be influenced by gender and other demographic characteristics. Females with ACHD were more likely to report feeing sad or anxious and perceive themselves as having a high risk of COVID-19 in comparison to males. These findings indicate the need for further evaluation and promotion of referral to mental healthcare when appropriate. ACHD clinicians play an important role in increasing patient awareness and knowledge about their condition and associated risks in relation to COVID-19. In our ACHD clinical practice, we augmented the mental health support and initiatives that we offer during the COVID-19 pandemic through a streamlined referral system to ACHD social work and mental health providers, a virtual support group, and a peer mentorship program to match patients to likeminded individuals. The next step would be a follow up study to evaluate the efficacy of these initiatives. We encourage ACHD providers to adapt health promotion and intervention efforts to improve optimal health behaviors and offer additional mental health support during the pandemic amongst all ACHD patients, regardless of underlying condition.
Authorship: Jodi L. Feinberg, study conception and design. Peter Sheng, analysis and interpretation of results. Stephanie Pena, data collection and analysis. Adam Small, analysis and interpretation of results. Susanna Wendelboe, data collection and analysis. Katlyn Nemai, study conception and design. Vikram Agrawal, analysis and interpretation of results. Dan G. Halpern, study conception and design. All authors reviewed the results and approved the final version of the manuscript.
Availability of Data and Materials: Data available upon reasonable request to the corresponding author.
Funding Statement: The authors received no specific funding for this study.
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
References
1. Andonian, C., Beckmann, J., Biber, S., Ewert, P., Freilinger, S. et al. (2018). Current research status on the psychological situation of adults with congenital heart disease. Cardiovascular Diagnosis & Therapy, 8(6), 799–804. DOI 10.21037/cdt.2018.12.06. [Google Scholar] [CrossRef]
2. Kovacs, A., Saidi, A. S., Kuhl, E. A., Sears, S. F., Silversides, C. et al. (2009). Depression and anxiety in adult congenital heart disease: Predictors and prevalence. International Journal of Cardiology, 137(2), 158–164. DOI 10.1016/j.ijcard.2008.06.042. [Google Scholar] [CrossRef]
3. Roseman, A., Kovacs, A. H. (2019). Anxiety and depression in adults with congenital heart disease: When to suspect and how to refer. Current Cardiology Reports, 21(11), 145. DOI 10.1007/s11886-019-1237-2. [Google Scholar] [CrossRef]
4. Stout, K. K., Daniels, C. J., Aboulhosn, J. A., Bozkurt, B., Broberg, C. S. et al. (2019). 2018 AHA/ACC guideline for the management of adults with congenital heart disease: Executive summary: A report of the American college of cardiology/American heart association task force on clinical practice guidelines. Journal of American College of Cardiology, 139, e637–e697. DOI 10.1161/CIR.0000000000000602. [Google Scholar] [CrossRef]
5. Sher, L. (2020). The impact of the COVID-19 pandemic on suicide rates. QJM: An International Journal of Medicine, 113(10), 707–712. DOI 10.1093/qjmed/hcaa202. [Google Scholar] [CrossRef]
6. Wang, X., Lei, S. M., Le, S., Yang, Y., Zhang, B. et al. (2020). Bidirectional influence of the COVID-19 pandemic lockdowns on health behaviors and quality of life among Chinese adults. International Journal Environmental Research and Public Health, 17(15), 5575. DOI 10.3390/ijerph17155575. [Google Scholar] [CrossRef]
7. Hemphill, N. M., Kuan, M. T. Y., Harris, K. (2020). Reduced physical activity during COVID-19 pandemic in children with congenital heart disease. Canadian Journal of Cardiology, 36(7), 1130–1134. DOI 10.1016/j.cjca.2020.04.038. [Google Scholar] [CrossRef]
8. Gentili, F., Cafiero, G., Perrone, M. A., Bianco, M., Salvati, A. et al. (2021). The effects of physical inactivity and exercise at home in young patients with congenital heart disease during the COVID-19 pandemic. International Journal Environmental Research and Public Health, 18(19), 1–10. DOI 10.3390/ijerph181910065. [Google Scholar] [CrossRef]
9. Wehrle, F. M., Landolt, M. A., Latal, B., Rometsch, S., Greutmann, M. (2020). Impact of the COVID-19 pandemic on health-related concerns, quality of life and psychological adjustment in young adults with congenital heart disease. Congenital Heart Disease, 15(5), 301–308. DOI 10.32604/CHD.2020.013078. [Google Scholar] [CrossRef]
10. Janzen, M. L., LeComte, K., Sathananthan, G., Wang, J., Kiess, M. et al. (2022). Psychological distress in adults with congenital heart disease over the COVID-19 pandemic. Journal Health of the American Heart Association, 11(9), 1–12. DOI 10.1161/JAHA.121.023516. [Google Scholar] [CrossRef]
11. Nikolaidis, A., Paksarian, D., Alexander, L., Derosa, J., Dunn, J. et al. (2021). The coronavirus health and impact survey (CRISIS) reveals reproducible correlates of pandemic-related mood states across the Atlantic. Scientific Reports, 11(1), 1–13. DOI 10.1038/s41598-021-87270-3. [Google Scholar] [CrossRef]
12. Holbein, C. E., Peugh, J., Veldtman, G. R., Apers, S., Luvckx, K. et al. (2020). Health behaviours reported by adults with congenital heart disease across 15 countries. European Journal of Preventative Cardiology, 27(10), 1077–1087. DOI 10.1177/2047487319876231. [Google Scholar] [CrossRef]
13. Goossens, E., Luyckx, K., Mommen, N., Gewillig, M., Budts, W. et al. (2013). Health risk behaviors in adolescents and emerging adults with congenital heart disease: Psychometric properties of the health behavior scale–congenital heart disease. European Journal of Cardiovascular Nursing, 12(6), 544–557. DOI 10.1177/1474515113475934. [Google Scholar] [CrossRef]
14. Feinberg, J. F., Cecchin, F., Gonzalez, A., Johnson, E., Halpern, D. G. (2020). Managing the adult congenital heart disease patient in the COVID-19 pandemic–A New York perspective. Congenital Heart Disease, 15(3), 141–146. DOI 10.32604/CHD.2020.012039. [Google Scholar] [CrossRef]
15. Broeberg, C. S., Kovacs, A. H., Sadeghi, S., Rosenbaum, M. S., Lewis, M. J. et al. (2021). COVID-19 in adults with congenital heart disease. Journal of American College of Cardiology, 77(13), 1644–1655. DOI 10.1016/j.jacc.2021.02.023. [Google Scholar] [CrossRef]
16. Heery, E., Sheehan, A. M., While, A. E., Coyne, I. (2015). Experiences and outcomes of transition from pediatric to adult health care services for young people with congenital heart disease: A systematic review. Congenital Heart Disease, 10(5), 413–427. DOI 10.1111/chd.12251. [Google Scholar] [CrossRef]
17. Eslami, B., Sundin, Ö., Macassa, G., Khankeh, H. R., Soares, J. J. (2013). Anxiety, depressive and somatic symptoms in adults with congenital heart disease. Journal of Psychosomatic Research, 74(1), 49–56. DOI 10.1016/j.jpsychores.2012.10.006. [Google Scholar] [CrossRef]
18. Fereitas, I. R., Castro, M., Sarmento, S. L., Moura, C., Viana, V. et al. (2013). A cohort study of psychosocial adjustment and psychopathology in adolescents and young adults with congenital heart disease. British Medical Journal, 3, e001138. DOI 10.1136/bmjopen-2012-001138. [Google Scholar] [CrossRef]
19. Andrade, L. J., Alonso, J., Mneimneh, Z., Wells, J. E., Al-Hamzawi, A. et al. (2014). Barriers to mental health treatment: Results from the WHO world mental health surveys. Psychological Medicine, 44, 1303–1317. DOI 10.1017/S0033291713001943. [Google Scholar] [CrossRef]
20. Deryugina, T., Shurchkov, O., Stearns, J. (2021). COVID-19 disruptions disproportionately affect female academics. American Economic Association Papers and Proceedings, 111, 164–168. DOI 10.1257/pandp.20211017. [Google Scholar] [CrossRef]
21. Albanesi, S., Kim, J. (2021). Effects of the COVID-19 recession on the US labor market: Occupation, family, and gender. Journal of Economic Perspectives, 35(3), 3–24. DOI 10.1257/jep.35.3.3. [Google Scholar] [CrossRef]
22. Dang, H. A., Nguyen, C. V. (2020). Gender inequality during the COVID-19 pandemic: Income, expenditure, savings, and job loss. World Development, 140, 105296. DOI 10.1016/j.worlddev.2020.105296. [Google Scholar] [CrossRef]
23. Apes, S., Kovacs, A. H., Luyckx, K., THomet, C., Budts, W. et al. (2016). Quality of life of adults with congenital heart disease in 15 countries: Evaluating country-specific characteristics. Journal of the American College of Cardiology, 67(19), 2237–2245. DOI 10.1016/j.jacc.2016.03.477. [Google Scholar] [CrossRef]
24. Assari, S., Lankarani, M. M. (2016). Education and alcohol consumption among older Americans; black-white differences. Frontiers in Public Health, 4, 67. DOI 10.3389/fpubh.2016.00067. [Google Scholar] [CrossRef]
25. Rosoff, D. B., Clarke, T. K., Adams, M. J., McIntosh, A. M., Smith, G. D. et al. (2021). Educational attainment impacts drinking behaviors and risk for alcohol dependence: Results from a two-sample mendelian randomization study with ∼780,000 participants. Molecular Psychiatry, 26, 1119–1132. DOI 10.1038/s41380-019-0535-9. [Google Scholar] [CrossRef]
26. Reid, G. J., Webb, G. D., McCrindle, B. W., Irvine, M. J., Siu, S. C. (2008). Health behaviors among adolescents and young adults with congenital heart disease. Congenital Heart Disease, 3, 16–25. DOI 10.1111/j.1747-0803.2007.00161.x. [Google Scholar] [CrossRef]
27. Jewell, J. S., Farewell, C. V., Welton-Mitchell, C., Lee-Winn, A., Walls, J. et al. (2020). Mental health during the COVID-19 pandemic in the United States: Online survey. JMIR Formative Research, 4(10), e22043. DOI 10.2196/22043. [Google Scholar] [CrossRef]
28. Romm, K. T., Patterson, B., Wysota, C. N., Wang, Y., Berg, C. J. (2022). Predictors of negative psychosocial and health behavior impact of COVID-19 among young adults. Health Education Research, 36(4), 3850397. DOI 10.1093/her/cyab026. [Google Scholar] [CrossRef]
29. Chen, L., Li, J., Xia, T., Matthews, T. A., Tseng, T. et al. (2021). Changes of exercise, screen time, fast food consumption, alcohol, and cigarette smoking during the COVID-19 pandemic among adults in the United States. Nutrients, 13(10), 3359. DOI 10.3390/nu13103359. [Google Scholar] [CrossRef]
Cite This Article
 Copyright © 2022 The Author(s). Published by Tech Science Press.
Copyright © 2022 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools