 Open Access
Open Access
ARTICLE
Minimally Invasive Surgical Technique in Double Aortic Arch with Distal Atretic Left-Side in Infant: From a Single-Surgeon Clinical Experience
Pediatric Cardiac Surgery Center of Fuwai Hospital, Beijing, China
* Corresponding Author: Zhongdong Hua. Email:
Congenital Heart Disease 2022, 17(5), 533-539. https://doi.org/10.32604/chd.2022.020496
Received 03 February 2022; Accepted 26 May 2022; Issue published 06 September 2022
Abstract
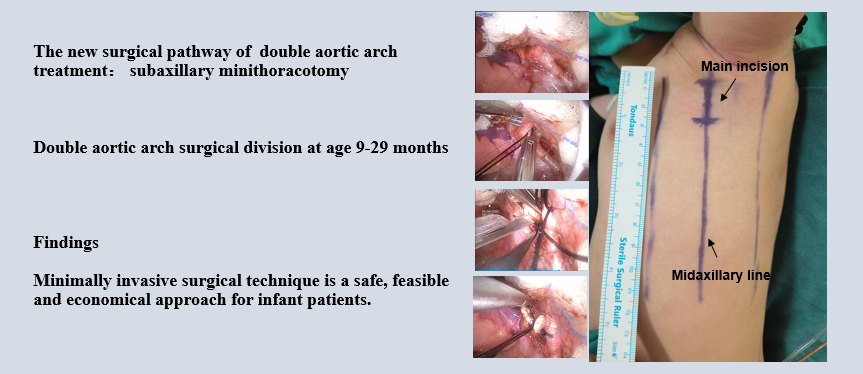
Background: Double aortic arch (DAA) with distal left-sided aortic arch atresia (LAAA) can form complete vascular ring by ligamentum connection. We aimed to introduce an uncommon DAA-LAAA diagnosis and treatment by the minimally invasive surgical technique (MIST). Methods: We retrospectively reviewed 7 cases of DAA-LAAA that were treated from January 2017 to July 2021. All infant patients underwent surgical repair by minimally invasive surgical technique. Mean follow-up was 14.43 months (range, 5–21 months). Results: There were seven patients with DAA-LAAA, including six males and one female. Median age was 19.29 months (range, 9.0–29.0 months). Median weight was 11.30 kg (range, 9.6–13.0 kg). Three patients were found severe tracheal compression by cardiac computed tomography angiography (cCTA). Six patients with isolated DAA-LAAA were performed operations through left subaxillary minithoracotomy, and one patient with ventricular septal defect (VSD) was performed operation concurrently under the cardiopulmonary bypass (CPB) through right subaxillary minithoracotomy. All patients had symptom improvement in the postoperative period and discharged successfully. Follow-up data showed good results in short-term. Conclusions: We introduce a new surgical pathway for DAA-LAAA treatment with good symptomatic relief in short-term. MIST is a safe, feasible and economical approach for infant patients.Graphic Abstract
Keywords
Abbreviation
| DAA | Double aortic arch |
| LAAA | Left-sided aortic arch atresia |
| MIST | Minimally invasive surgical technique |
| cCTA | Cardiac computed tomography angiography |
| VSD | Ventricular septal defect |
| CPB | Cardiopulmonary bypass |
Double aortic arch (DAA) is a common structure of complete vascular ring that may compress trachea and esophagus, constitutes about 46%–76% in all symptomatic vascular ring [1]. DAA with distal left-sided aortic arch atresia (LAAA) is an extremely rare DAA variant. DAA-LAAA may be result of persistence of bilateral fourth pharyngeal aortic arch and abnormal interruption of left-sided aortic arch in the embryonic period. LAAA commonly originated from the ascending aorta, giving rise to the left common carotid artery and left subclavian artery in sequence. The interrupted site located at the distal of left subclavian artery with ligamentum connection (Fig. 1). The patient with DAA-LAAA may present compression symptoms of airway and esophagus in infancy, including vomiting, wheezing, shortness of breath, dysphagia, irritable cough, recurrent respiratory tract infection and so on.
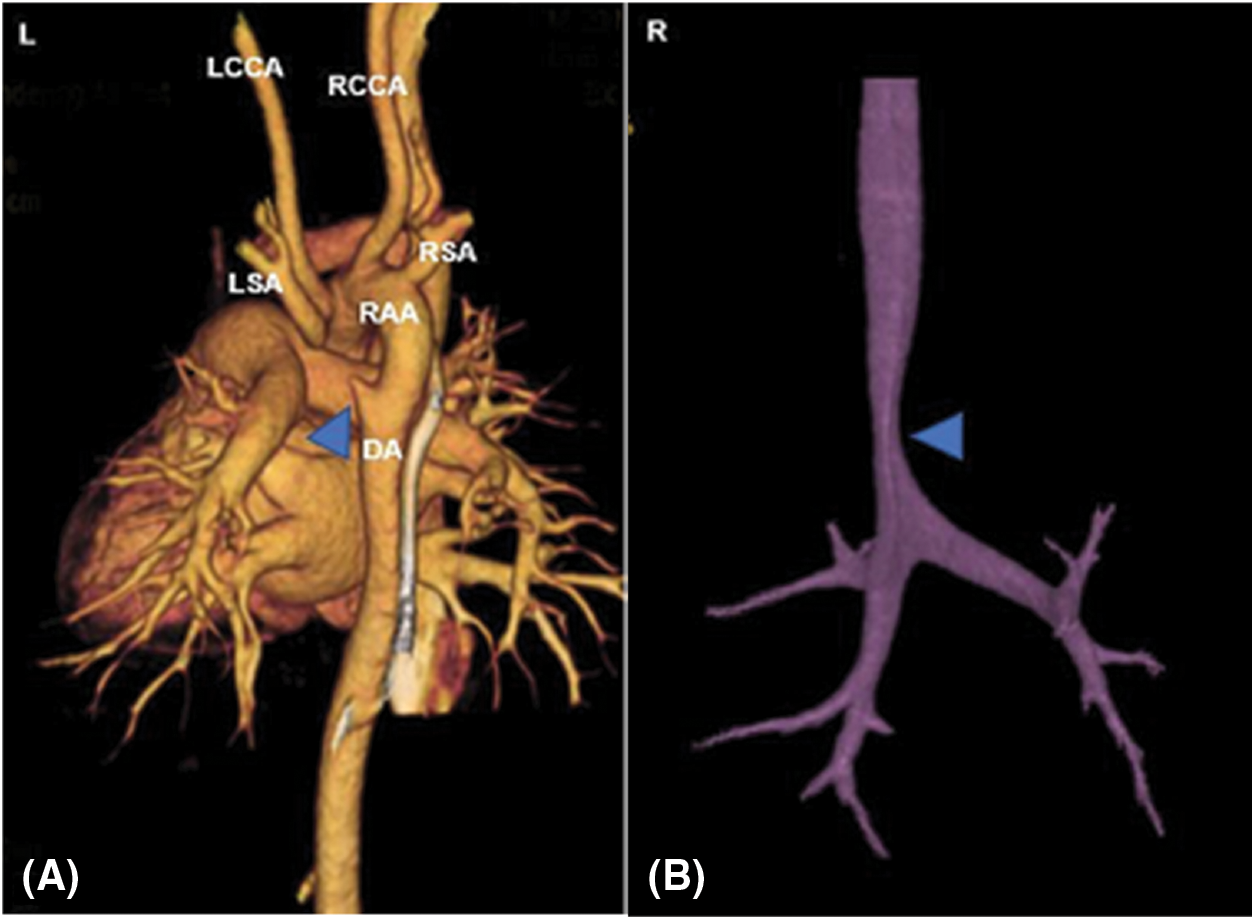
Figure 1: (A) Three-dimensional reconstruction images described anatomy of vascular ring. The stump of DA was showed by a sign (Δ). RAA, right aortic arch; RSA, right subclavian artery; LSA, left subclavian artery; RCCA, right common carotid artery; LCCA, left common carotid artery; DA, descending aorta. (B) Tracheal reconstruction by cCTA. Trachea compression by DAA-LAAA was showed by a sign (Δ)
At present, the left posterolateral thoracotomy pathway and video-assisted thoracoscopic technique are both feasible and safe for vascular ring division [2]. However, the left posterolateral thoracotomy as a traditional pathway is inaesthetic and more invasive. The video-assisted thoracoscopic technique is not widely spread, especially in the developing countries. At our center, we applied a new subaxillary minithoracotomy pathway to perform operation for infant patients. This study introduced a minimally invasive surgical technique (MIST) for a broad range of congenital heart disease for infant patients.
We conducted an observational, retrospective, single-surgeon (Z.D.H) study. This study reviewed seven patients with DAA-LAAA performed operations from January 2017 to July 2021. This study was approved by the Institutional Review Board of Fuwai Hospital (Approval No. 2021-1506) and the patient consent was waived due to its retrospective nature. The symptoms were evaluated by the self-made DAA symptoms scores (Table 1) on admission. All patients were taken echocardiography and cardiac computed tomography angiography (cCTA) during hospital stay. Three-dimensional reconstruction images by cCTA provided a detailed assessment of the aortic arch, branch vessels and trachea. The operations were performed through subaxillary minithoracotomy. Follow-up data were collected by DAA symptoms scores and echocardiography during routine clinical visits and telephone visits.
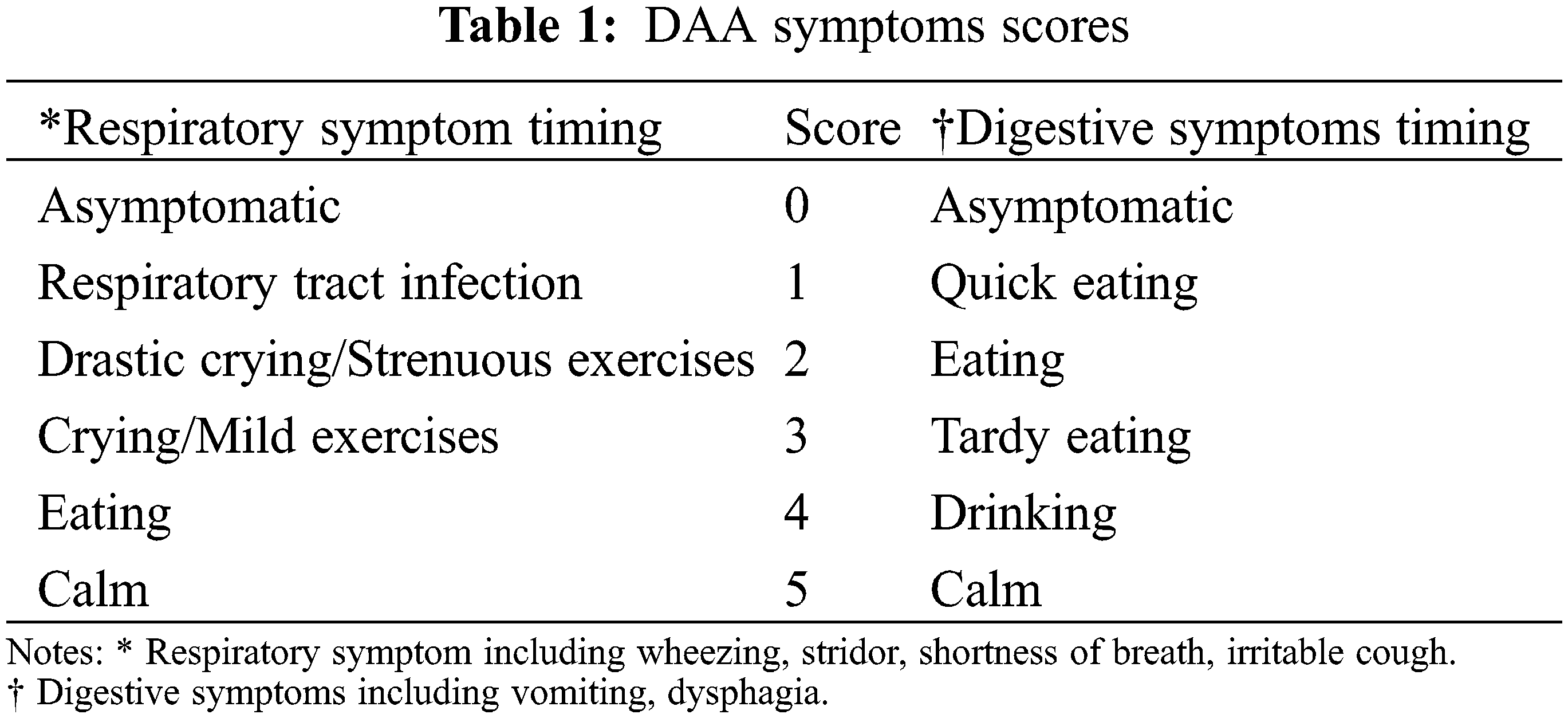
The self-made DAA symptoms scores can effectively evaluate obstruction status of tracheal and esophagus by DAA for infant patients. The symptoms include respiratory and digestive systems. The obstruction status is scored from 0 to 5 with different causes. It can conveniently describe compressing status when the onset of symptoms is caused by particular timing. The causes of symptoms were collected and summarized by medical history of patients.
Continuous data were expressed as median and interquartile range. Categorical data were expressed as counts. Statistical analyses were performed by using the Statistical Package for Social Sciences, version 22.0 (SPSS, Inc., Chicago, IL, USA).
After the induction of general anesthesia, the patients were taken the right side-lying position for isolated DAA-LAAA. The left arm was wrapped and elevated over the head to expose the axillary region with a balloon prop. The skin incision took place in the left midaxillary line from 2nd to 4th rib. The vertical incision was about 3–4 cm in length. We entered thoracic cavity at 3rd intercostal space. The lung was compressed and pushed posteriorly to expose the aortic arch by a wet sponge. The soft tissue retractor (HTKD Medical, Beijing, China) was used to protect skin and optimize surgical exposure. The pleura overlying left-sided aortic arch was dissected carefully. The aortic arch and branch vessels were dissociated completely. Care was taken to distinguish the arterial ligament and not injure the vagus nerve. The ligamentum connection which located the distal of left-sided aortic arch was clamped and divided with a running suture (Video 1).
For a patient additional perimembranous VSD, the patient took the left side-lying position. The skin incision was placed in the right midaxillary line from 2nd to 5th rib. The vertical incision was about 4–5 cm in length. Firstly, we perform operation at 3rd intercostal space for DAA-LAAA division. The thymus and pleura covering the ascending aorta, right aortic arch and descending aorta were detached carefully. The descending aorta was usually in the deep side neighboring the thoracic duct and recurrent laryngeal nerve. The ligamentum connection was clamped and divided, and the ends were closed with a running suture. Finally, we switched to 4th intercostal space to expose the pericardium. The pericardium was opened and hung by three stay sutures. The CPB was established and commenced under mild hypothermia. The cardioplegia was achieved by the antegrade infusion. The VSD was repaired through the incision of right atrial (Fig. 2).
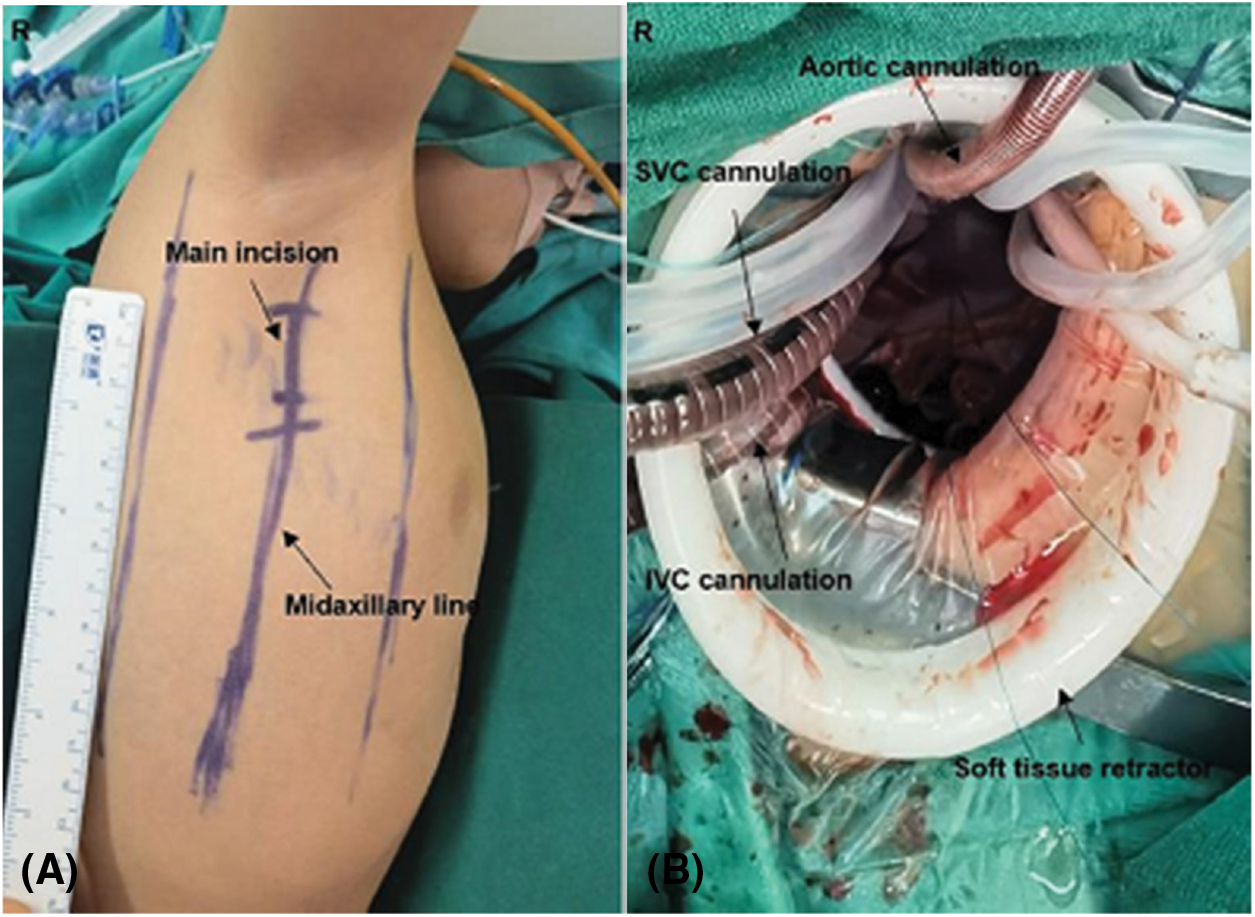
Figure 2: (A) The patient was placed in the left lateral position for repair of DAA-LAAA with VSD. (B) The surgical field from surgeon’s view for repair of DAA-LAAA with VSD. IVC, inferior vena cava; SVC, superior vena cava
A total of seven patients underwent operations by MIST. Table 2 summarized perioperative data for all patients. There were six males and one female in our study. Median age was 19.29 months (range, 7.0–29.0 months). Median weight was 11.30 kg (range, 9.6–13.0 kg). All patients were hospitalized with significant symptoms, such as wheezing, shortness of breath, vomiting, dysphagia, recurrent respiratory tract infection or irritable cough. Median respiratory symptoms scores was 2.29 (range, 1, 0–3.0) and digestive symptoms scores was 1.0 (range, 0–2.0). One patient was auscultated with heart murmur. Echocardiography revealed perimembranous VSD (4 mm). The cCTA found serious tracheal compression in three patients with significant respiratory symptoms. The tracheal compression site usually located upward side of tracheae bifurcation.
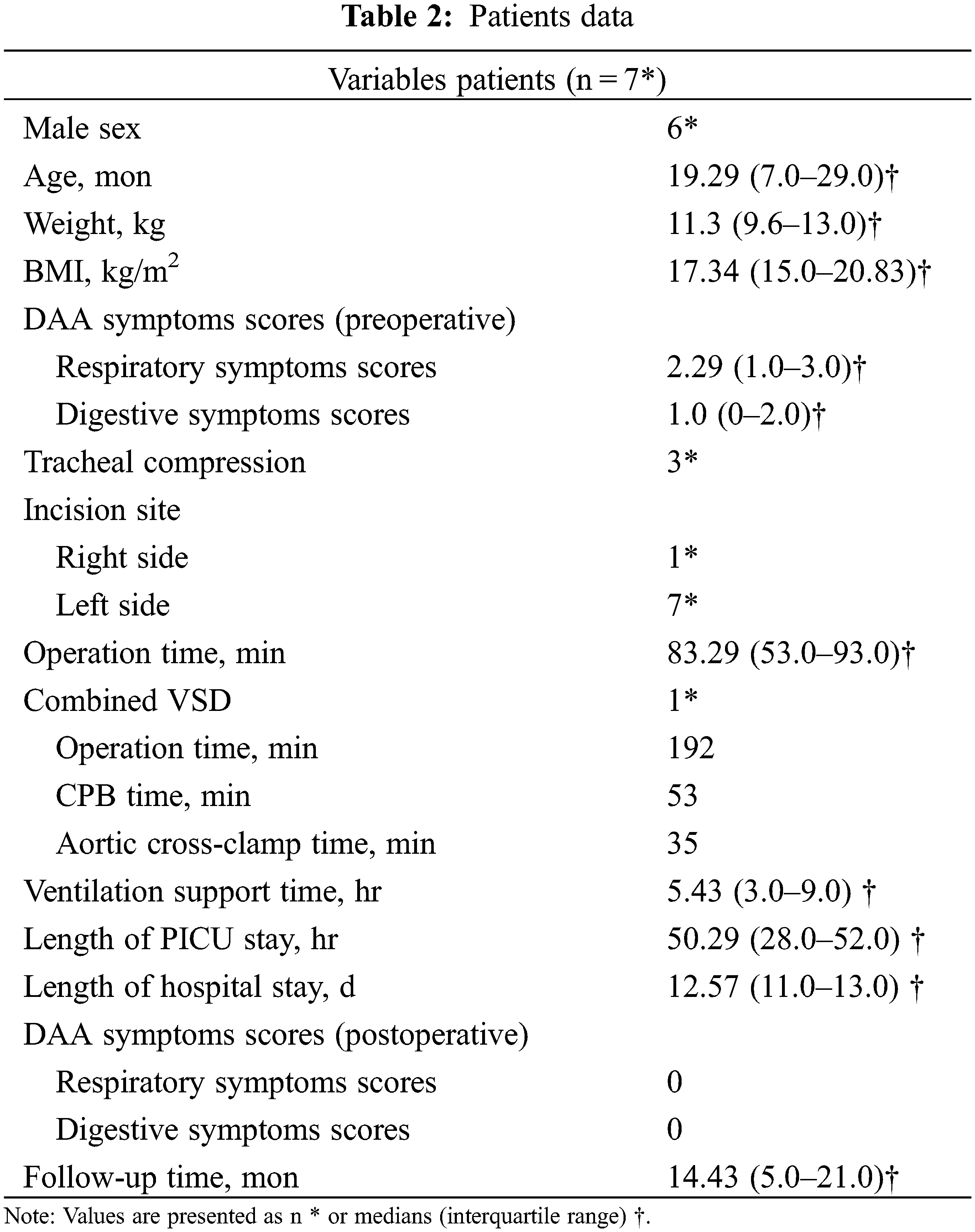
The operations were taken by MIST. The median operation time of isolated DAA-LAAA was 65.17 min (range, 49.3–88.5 min). For the DAA-LAAA with VSD, the operation time was 192 min. The CPB time was 53 min and aortic cross-clamp time was 35 min. Median ventilation support time was 5.43 h (range, 3.0–9.0 h). No one happened bleeding, chylothorax, vocal cord paresis and in-hospital death during the postoperative period. Most patients had a short stay in pediatric intensive care unit (PICU) (38 h in average), whereas the youngest patient (3 months old) had a long stay (124 h) with severe pneumonia. All patients had good symptom improvement during hospitalization. Length of hospital stay in average was 12.57 d (range, 11.0–13.0 d). At clinic visit within 1 month after discharge, the echocardiography revealed aortic arch was with normal anatomic structure. We took telephone visits for all patients by DAA symptoms scores in short-term follow-up. All infant patients reported resolution in symptoms with good healthy growth.
At present, the left posterolateral thoracotomy pathway and video-assisted thoracoscopic technique are both feasible approaches for DAA treatment [2,3]. The left posterolateral thoracotomy as a traditional pathway is inaesthetic and more invasiveness. And the serratus anterior muscle injury can increase risk of musculoskeletal deformities [4]. The video-assisted thoracoscopic technique can effectively avoid complications of scoliosis, shoulder muscle dysfunction and chest wall deformity comparing with left posterolateral thoracotomy pathway [4,5]. However, video-assisted thoracoscopic technique possibly increased risk of bleeding [2]. Furthermore, thoracoscopic technique needs more special sized instruments for infants in different age [2]. As a result, the younger infant patients with low weight maybe limitation [2].
The subaxillary minithoracotomy is a covert and cosmetic pathway in the midaxillary line. Thoracic muscles and nerves can be spared during the procedure. The soft tissue retractor can protect the skin and optimize the surgical exposure so that it can make a good balance between minimal incision and feasibly operating under direct vision. The coronal distance of thoracic cavity is shallow for infant, which is suitable for operating with regular instruments. The blood pressure monitoring of upper and lower limbs can help us to distinguish the ligamentum connection, arterial ligament and descending aorta, especially for the younger infant. We reported a DAA-LAAA patient with VSD through right subaxillary minithoracotomy. It is feasible to divide DAA at 3rd intercostal space. By switching to 4th intercostal space, we established CPB and VSD repair with enough space.
The lung injury is common but not serious in the postoperative period. The younger infant patients with early respiratory symptoms may present a high risk of ventilator-associated lung injury and pneumonia after operation [6]. The DAA symptoms scores can help us to investigate symptoms effectively, and it can reflect serious compression of airway and esophagus with higher scores. Primary airway malacia is also not rare among the infants, with an estimated incidence of at least 1 in 2100 [7]. It can be evaluated by the cCTA. We should pay more attention to the DAA patients with serious airway symptoms in the preoperative period, because they may tend a high risk of respiratory complication during postoperative period.
At our center, subaxillary minithoracotomy pathway is a routine approach for infant patients with congenital heart diseases, such as atrial septal defect, VSD, patent ductus arteriosus, partial anomalous pulmonary venous connection, Tetralogy of Fallot and so on [8]. We aim to pursue a better pathway for infant patients which is characteristic with cosmetic incision, less injury and economical treatment. Minimal subaxillary thoracotomy is a safe pathway for DAA-LAAA treatment. And it was also good choice for DAA-LAAA with intracardiac anomalies. DAA symptoms scores is an effective method to assess compression status of airway and esophagus for infants. MIST is a safe, feasible and economical approach with good results in short-term.
Authors Contribution: Qi Liu: Data collection, manuscript redaction; Shoujun Li: Funding acquisition, supervision, visualization; Zhongdong Hua: Conceptualization, supervision, visualization.
Funding Statement: This study was supported by the CAMS Innovation Fund for Medical Sciences (CIFMS) [2020-I2M-C&T-A-009] and the National Key R&D Program of China [2017YFC1308100].
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
References
1. Yang, Y., Jin, X., Pan, Z., Li, Y., Wu, C. (2019). Diagnosis and surgical repair of congenital double aortic arch in infants. Journal of Cardiothoracic Surgery, 14(1), 160. DOI 10.1186/s13019-019-0976-x. [Google Scholar] [CrossRef]
2. Herrin, M. A., Zurakowski, D., Fynn-Thompson, F., Baird, C. W., Del Nido, P. J. et al. (2017). Outcomes following thoracotomy or thoracoscopic vascular ring division in children and young adults. The Journal of Thoracic and Cardiovascular Surgery, 154(2), 607–615. DOI 10.1016/j.jtcvs.2017.01.058. [Google Scholar] [CrossRef]
3. Backer, C. L., Bharadwaj, S. N., Eltayeb, O. M., Forbess, J. M., Popescu, A. R. et al. (2019). Double aortic arch with kommerell diverticulum. The Annals of Thoracic Surgery, 108(1), 161–166. DOI 10.1016/j.athoracsur.2019.01.062. [Google Scholar] [CrossRef]
4. Safa, N., Wei, S., Saran, N., Guadagno, E., Laberge, J. M. et al. (2021). Musculoskeletal deformities after thoracic surgery in children: An observational long-term follow-up study. Journal of Pediatric Surgery, 56(1), 136–141. DOI 10.1016/j.jpedsurg.2020.09.024. [Google Scholar] [CrossRef]
5. Burke, R. P., Chang, A. C. (1993). Video-assisted thoracoscopic division of a vascular ring in an infant: A new operative technique. Journal of Cardiac Surgery, 8(5), 537–540. DOI 10.1111/j.1540-8191.1993.tb00409.x. [Google Scholar] [CrossRef]
6. Guess, R., Vaewpanich, J., Coss-Bu, J. A., Phongjitsiri, S., Kennedy, C. et al. (2018). Risk factors for ventilator-associated events in a PICU. Pediatric Critical Care Medicine, 19(1), e7–e13. DOI 10.1097/PCC.0000000000001371. [Google Scholar] [CrossRef]
7. Boogaard, R., Huijsmans, S. H., Pijnenburg, M. W., Tiddens, H. A., de Jongste, J. C. et al. (2005). Tracheomalacia and bronchomalacia in children: Incidence and patient characteristics. Chest, 128(5), 3391–3397. DOI 10.1378/chest.128.5.3391. [Google Scholar] [CrossRef]
8. An, K., Li, S., Yan, J., Wang, X., Hua, Z. (2022). Minimal right vertical infra-axillary incision for repair of congenital heart defects. The Annals of Thoracic Surgery, 113(3), 896–902. DOI 10.1016/j.athoracsur.2021.01.052. [Google Scholar] [CrossRef]
Cite This Article
 Copyright © 2022 The Author(s). Published by Tech Science Press.
Copyright © 2022 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools