
 | Congenital Heart Disease |  |
DOI: 10.32604/CHD.2021.015749
ARTICLE
A Rare Long Term Survival Case of Complete Pentalogy of Cantrell in Adult after One-Staged Surgery
1Department of Cardiovarscular Surgery, Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, 430022, China
2Department of Ultrasound, Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, 430022, China
3Department of Radiology, Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, 430022, China
*Corresponding Author: Nianguo Dong. Email: hhdongnianguo@aliyun.com
Received: 10 January 2021; Accepted: 08 April 2021
Abstract: Pentalogy of Cantrell is a rare congenital abnormality. Even with high-quality medical care and staged corrective surgeries in professional hospitals, the mortality rate is still very high and long-term prognosis is poor. Survival is largely determined by the complexity and severity of cardiac abnormalities, the efficiency of abdominal wall closure and postoperative complications. A 24-year-old male patient with complete pentalogy of Cantrell was diagnosed. One-stage surgical repair of all abnormalities were completed. The patient recovered well and had been follow-up for 7 years. He has a good cosmetic outcome, with no signs of cardiac dysfunction. No complications were noted.
Keywords: Pentalogy of cantrell; adult; one-stage surgery
Complete pentalogy of Cantrell is a rare congenital abnormality, including five anomalies: various congenital intracardiac malformations, and defects in diaphragmatic pericardium, the anterior diaphragm, lower sternum, and midline supraumbilical abdominal wall. Even with high-quality medical care and staged corrective surgeries in professional hospitals, the mortality rate is still very high and long-term prognosis is poor. Survival is largely determined by the complexity and severity of cardiac malformations, the efficiency of abdominal wall closure and postoperative complications. We now present our experience in using one-stage surgical repair to treat a rare case of complete pentalogy of Cantrell in adult.
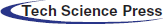
A 24-year-old male patient with a extrathoracic heart extending into supraumbilical abdominal wall (Fig. 1A) presented with symptoms of tachypnea, mild cyanosis and clubbing fingers. Physical examination showed a thoracoabdominal wall defect. The xyphoid was absent and the sternum was short. Oxygen saturation was 85%. 3/VI systolic murmur could be heard at the 2nd∼4th intercostal space near the right sternal border. Chest X-ray showed bilateral pulmonary congestion, dextroversion and enlarged right heart (Fig. 1B). The echocardiogram showed situs solitus, a 3.2 cm secundum atrial septal defect, functional single atrium, a 2.8 cm subaortic ventricular septal defect, double outlet right ventricle, overriding aorta with 80% of the aortic orifice over the right ventricle, and subpulmonary valve outflow tract stenosis (Fig. 1C).
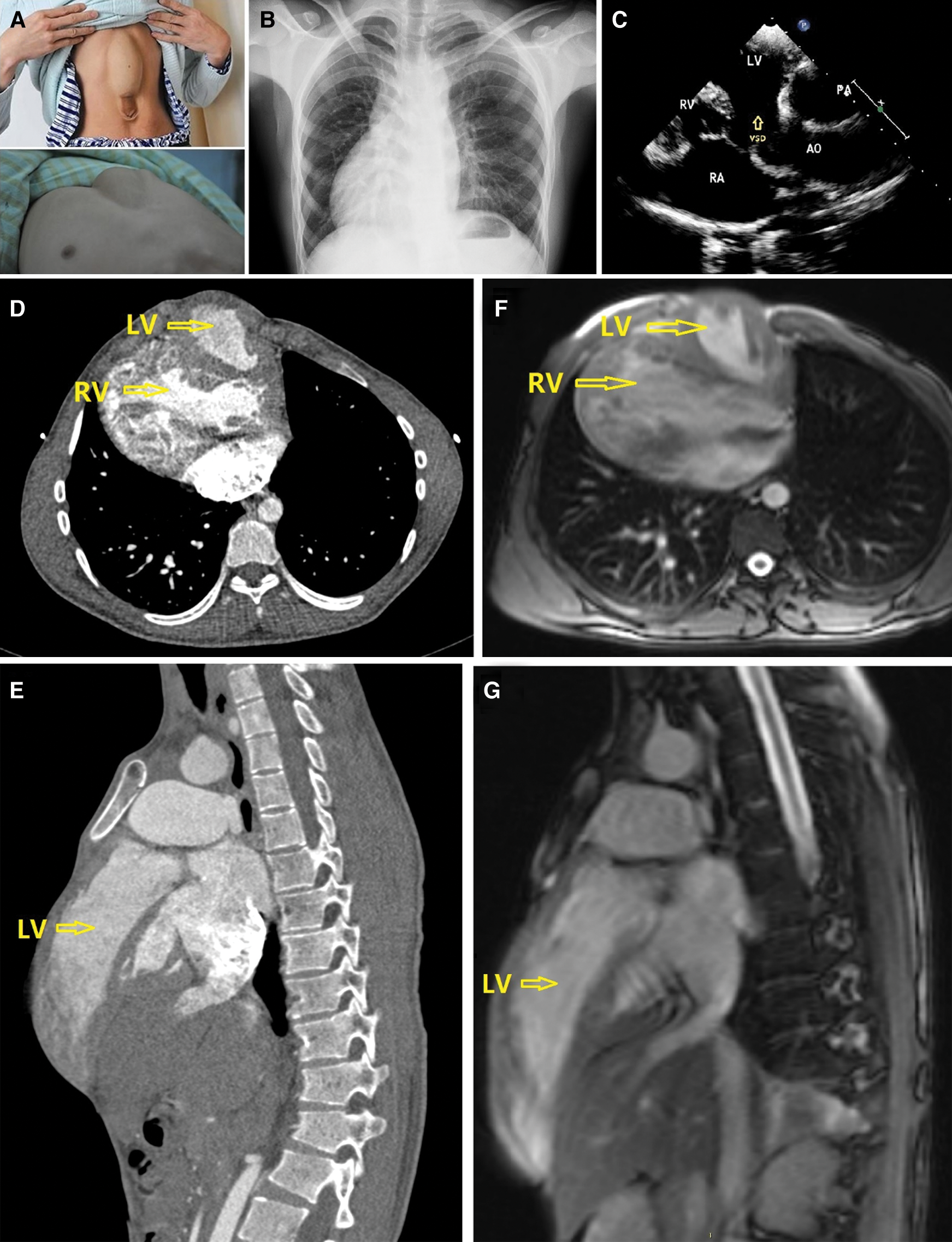
Figure 1: (A) The extrathoracic heart. (B) Chest X-ray. (C) Echocardiogram. (D,E) CTA. (F,G): MRI. LV, left ventricle; RV, right ventricle; RA, right atrium; AO, aortic orifice; PA, pulmonary artery; VSD, ventricular septal defect
CTA and MRI showed a ventral thoracoabdominal wall defect with the two ventricles protruding through the defective of anterior diaphragm into epigastrium (Figs. 1D–1G). Double outlet right ventricle, subpulmonary valve outflow tract stenosis, and the diameter of systolic phase and diastolic phase are 0.5 cm and 1.5 cm. Diameter of pulmonary truncus are 3.4 cm, right pulmonary artery is 1.8 cm, left pulmonary artery are twist and diameter are 1.2 cm. Subaortic ventricular septal defect are 2.8 cm, secundum atrial septal defect are 3.2 cm.
After the short sternum was opened, the skin incision above the protruding heart was performed and the hypoderm was separated from the heart. The heart showed a clockwise rotation with the left ventricle anterior to the right ventricle and deviation of the apex of the heart to the right. It was covered with thin pericardial tissue. We modified ligamentum teres which was redundant and sutured to excess of diaphragm and pericardium. Some loose sutures are taken to avoid tamponade. A bovine pericardial patch was sutured underneath to repair diaphragmatic defect (Fig. 2A). Liver anomaly was not disturbed.
Figure 2: (A) Bovine pericardial patch. (B) Obstructing muscle bundles of the RVOT. (C) Dacron patch. (D) Medpor patch
Second, after cannulation of the aorta, the superior vena cava and femoral vein, cardiopulmonary bypass was started. The heart was arrested with cardioplegia (30 mL/kg). The excellent exposure of the ventricular septal defect and obstructive muscle bundles in the right ventricular outflow tract (RVOT) was achieved through an incision in the right atrium and a right ventriculostomy. After obstructive muscle bundles of the RVOT was resection, the ventricular septal defect was closed with a Dacron patch (Balance Medical Inc., Beijing, China) using a 5–0 polypropylene (Prolene, Ethicon, New Brunswick, New Jersey, USA) running suture (Figs. 2B and 2C). The atrial septal defect was also closed with a Dacron patch using a 5–0 polypropylene. The RVOT was eventually bovine pericardial patch augmented.
Third, chest wall reconstruction was attempted by separating bilateral sternal bar flaps. And, simple approximation of the cartilage was insufficient for covering the protruding ventricle. Thus, a large patch repair was included for the chest wall reconstruction operation. The Medpor patch (Porex Surgical Inc., Atlanta, Georgia, USA) was cut into the appropriate size and affixed onto the left and right costal cartilage by using steel wire (Fig. 2D). The Medpor patch corner stitches allowed even distribution of the tension. The bottom area of the patch was used to reinforce the diaphragm and peritoneum defects. The patient tolerated the procedure well.
After drains were inserted, the wound was closed. Total operation time was 8 hours. Cardio- pulmonary bypass time was 146 mins and cross-clamping time was 114 min. Mechanical ventilation time was 3 days. The patient transferred out of the intensive care unit on day 7.
The patient recovered well during the hospitalization. Postoperative echocardiogram showed cardiac deformities were corrected, no obstruction of RVOT, and no residual shunt (Fig. 3A). The patient discharged on postoperative day 21 (Fig. 3B). The 7 years follow-up revealed that he was well and the reconstruction had remained rigid (Figs. 3C and 3D). He has a good cosmetic outcome, with no signs of reherniation or cardiac dysfunction. No complications were noted.
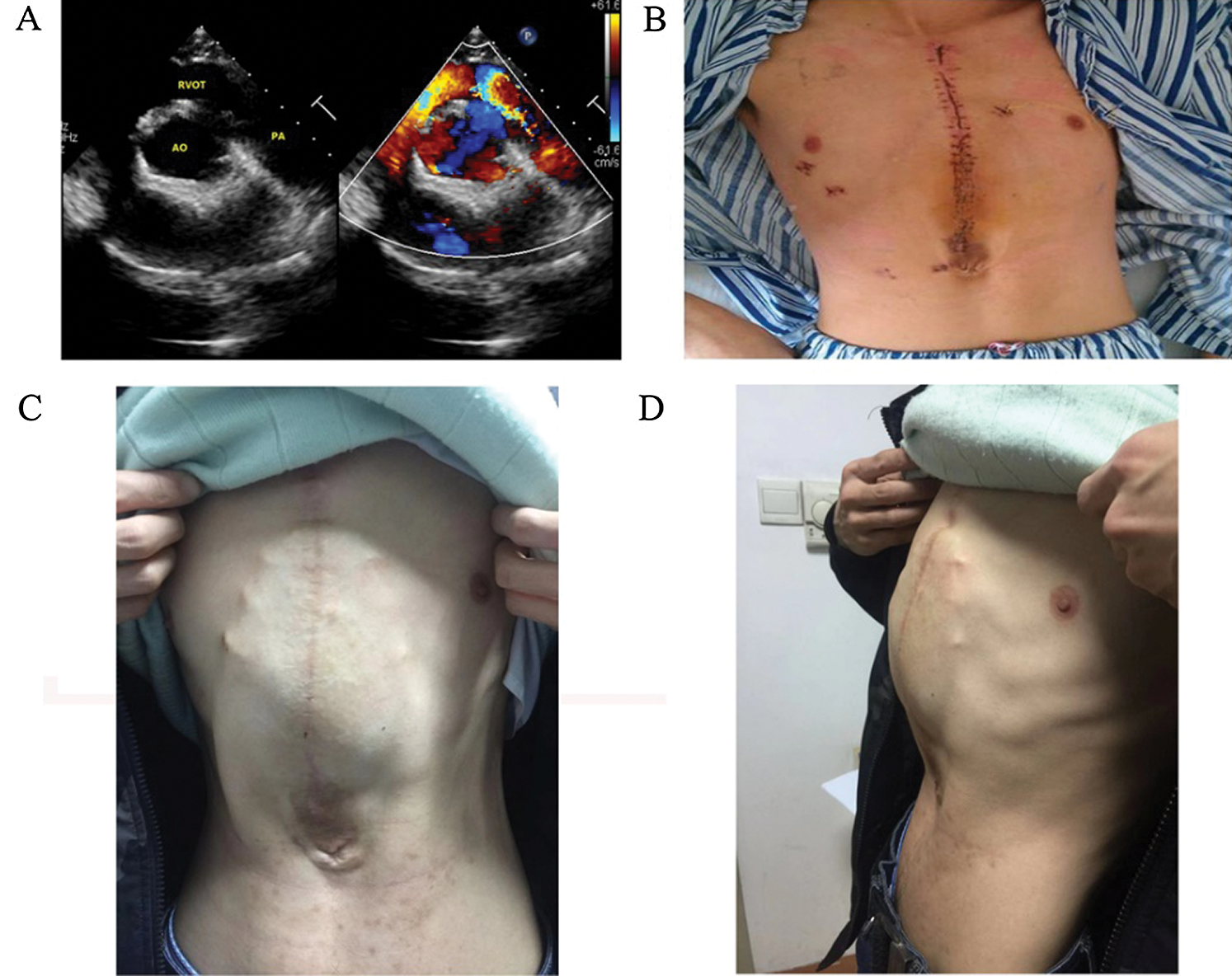
Figure 3: (A) Postoperative echocardiogram. (B) Postoperative image of the patient from views of anterior on day 21. (C,D), Postoperative image of the patient from views of anterior and left lateral in the 7th years
Pentalogy of Cantrell is a rare congenital anomaly, first described by Cantrell et al. [1] in 1958. It occurs in 1 per 65,000 live births and was found to be more common in boys than in girls (1.35:1) [2]. The full spectrum includes the following 5 anomalies: defects in the anteriordiaphragm, midline supraumbilical abdominal wall, diaphragmatic pericardium, and lower sternum, and various congenital intracardiac abnormalities. In 1972, Toyama proposed the following classification of pentalogy of Cantrell, based on 60 cases described in the literature [3]: Class 1 definite diagnosis and all five defects are present. Class 2 probable diagnosis, if the four defects are present including: intracardiac and ventral abdominal wall defects. Class 3 incomplete expression, with the various combinations of defects present and includes a sternal abnormality.
The precise anatomic identification of the components of the pentalogy of Cantrell is extremely important for treatment planning and prognostication. Multimodality imaging with echocardiogram, CTA, and MRI remains helpful for pretreatment planning. Echocardiogram will lead to the diagnosis of the intracardiac anomalies. CTA and MRI were chosen for its capacity to demonstrate the segmental anatomy and the position of the heart relative to the bones of the thoracic cage. With the clinical presentation and multimodality imaging findings reported, we arrived at a diagnosis of class I pentalogy of Cantrell for this adult patient, which is very rare. The complex combination of the aforementioned cardiovascular anomalies suggested a poor prognosis.
The mortality rate is high for pentalogy of Cantrell, and no more than 5% of them survive [4]. Further, studies have shown that even with high-quality medical care in professional tertiary centers and with multiple corrective surgeries, the mortality rate is still very high and long-term prognosis is poor [5]. Treatment of patients with pentalogy of Cantrell causes serious concern and distress for parents and presents a major challenge for a multidisciplinary team involving a surgeon and anesthetist. Survival is largely determined by the severity and complexity of cardiac malformations, the efficiency of abdominal wall closure and postoperative complications.
In 1912, Wieting first reported surgical treatment by repositioning the diverticulum into the pericardial sac and closing the opening in the diaphragm [6]. The surgical intervention consists of corrective or palliative cardiovascular surgery, correction of ventral hernia and diaphragmatic defects, and correction of associated anomalies. In the past, successful surgery has been accomplished despite its high mortality rate, but the surviving cases did not have, or had only minor degrees of ectopia cordis with small omphaloceles and simple cardiac malformations [7]. The crucial problem seems to be the avoidance of high abdominal and intrathoracic pressures postoperatively, as they cannot be tolerated in the presence of severe cardiac malformations. Because of the complexity of the syndrome, the treatment of defects is difficult and often requires multistage corrective procedures. According to many researchers, the effectiveness and success of treatment as well as long-term survival depend primarily on the type of diagnosed heart defect. In recent years, some new aspects of Pentalogy of Cantrell management, such as the fetal diagnostic possibilities and the possible transcatheter interventions, could improve the survival of such patients [8–10]. However, first, these management were used for newborn or infant. Second, the patients received palliative operations.
In this patient, one-stage surgical repair of all malformations was completed. First, the severe cardiac malformations were corrected satisfactory. Second, we planned a strategy of reconstruction for this patient include the following: (1) rigid protection of the heart without compression, (2) minimal donor site morbidity. The sternal bars found in patients with sternal clefts are often thick, and bisection allows a substantial increase in surface coverage without a significant compromise in the strength. Fixation of the Medpor patch in the midline restores continuity of the thoracic cage, creating a dynamic reconstruction. In this case, where the extent of the flaps is short of the midline, we propose combining this technique with Medpor patch. A Medpor patch was used for repairing the lower sternal defect, acting as a shield for the heart. The ventral part of diaphragm was reconstructed with bovine pericardium patch.
Postoperative complications vary depending on the timing of surgery and on the materials used for the reconstruction of the defects. Early postoperative death is common in patients with complex cardiac anomalies, or in those having postoperative complications like respiratory insufficiency, bowel dysmotility, intraabdominal and pulmonary hypertension [11]. Late deaths are usually a complication of cardiac dysfunction, infections, or adhesive small bowel obstruction [11,12]. The long-term prognosis depends on the severity of the cardiac and associated malformations. All those complications were avoided in this patient and the cardiac function was satisfied during follow up. The patient returned to work 1 year after surgery.
In conclusion, we have demonstrated a Class 1 pentalogy of Cantrell with clinical and imaging findings. Echo, CTA and MRI can be highly useful in accurate pretreatment assessment of the complex anomalies associated with pentalogy of Cantrell. To our knowledge, this is the first reported case of complete pentalogy of Cantrell in adult received operation and survived until now in P.R. China. Despite this, pentalogy of Cantrell still remains a therapeutic challenge for surgeons.
Ethical Approval: Informed consent for publication of photographs was obtained from the patient.
Funding Statement: Supported by grants from the National Natural Science Foundation of China (81873502 and 31330029), the Fundamental Research Funds for the Central Universities (2017KFYXJJ250), and Scientific Research Fund of Union Hospital, Tongji Medical College, Huazhong University of Science and Technology (02.03.2017-307).
Conflicts of Interest:The authors declare that they have no conflicts of interest to report regarding the present study.
1. Cantrell, J. R., Haller, J. A., Ravitch, M. M. (1958). A syndrome of congenital defects involving the abdominal wall, sternum, diaphragm, pericardium and heart. Surgery, Gynecology & Obstetrics, 107(5), 602–614. [Google Scholar]
2. Vazquez-Jimenez, J. F., Muehler, E. G., Daebritz, S., Keutel, J., Nishigaki, K. et al. (1998). Cantrell’s syndrome: A challenge to the surgeon. Annals of Thoracic Surgery, 65(4), 1178–1185. [Google Scholar]
3. Toyama, W. M. (1972). Combined congenital defects of the anterior abdominal wall, sternum, diaphragm, pericardium, and heart a case report and review of the syndrome. Pediatrics, 50(5), 778–792. [Google Scholar]
4. Baeza, H. C., Escobar, I. M., Garcia, C. L., Sanchez, M. L., Najera, G. H. (2008). Pentalogia de Cantrell. Informe de cuatro casos. Revista Medica del Instituto Mexicano del Seguro Social, 46(4), 673–676. [Google Scholar]
5. O’Gorman, C. S., Tortoriello, T. A., McMahon, C. J. (2009). Outcome of children with pentalogy of Cantrell following cardiac surgery. Pediatric Cardiology, 30(4), 426–430. DOI 10.1007/s00246-009-9410-9. [Google Scholar] [CrossRef]
6. Gula, G., Yacoub, M. (1977). Syndrome of congenital ventricular diverticulum and midline thoracoabdominal defects. Thorax, 32(3), 365–369. DOI 10.1136/thx.32.3.365. [Google Scholar] [CrossRef]
7. Halbertsma, F. J., van Oort, A.,van der Staak, F. (2002). Cardiac diverticulum and omphalocele: Cantrell’s pentalogy or syndrome. Cardiology in the Young, 12(1), 71–74. DOI 10.1017/S1047951102000148. [Google Scholar] [CrossRef]
8. Tanaka, T., Kubo, S., Kamei, N. (2020). Successful balloon valvuloplasty using direct puncture of the heart for pentalogy of Cantrell with complete ectopia cordis, low birth weight, single ventricle and severe pulmonary stenosis. Cardiology in the Young, 30(12), 1951–1953. DOI 10.1017/S1047951120002863. [Google Scholar] [CrossRef]
9. Galeczka, M., Fiszer, R., Knop, M. T., Smerdzinski, S., Szkutnik, M. et al. (2019). Successful atrial septal defect transcatheter closure in a patient with pentalogy of Cantrell and ectopia cordis. Postepy Kardiol Interwencyjnej, 15(2), 247–250. [Google Scholar]
10. McMahon, C. J., Walsh, K. P. (2013). Transcatheter right ventricular outflow tract stent implantation in a child with pentalogy of Cantrell, double outlet right ventricle, and severe pulmonary stenosis. Catheterization and Cardiovascular Interventions, 82(7), 1164–1167. DOI 10.1002/ccd.24852. [Google Scholar] [CrossRef]
11. Wheeler, D. S., St. Louis, J. D. (2007). Pentalogy of Cantrell associated with hypoplastic left heart syndrome. Pediatric Cardiology, 28(4), 311–313. DOI 10.1007/s00246-007-0016-9. [Google Scholar] [CrossRef]
12. Rahn, S., Bahr, M., Schalamon, J., Saxena, A. K. (2008). Single-center 10-year experience in the management of anterior abdominal wall defects. Hernia: The Journal of Hernias and Abdominal Wall Surgery, 12(4), 345–350. DOI 10.1007/s10029-008-0336-6. [Google Scholar] [CrossRef]
 | This work is licensed under a Creative Commons Attribution 4.0 International License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. |