

 | Congenital Heart Disease |  |
DOI: 10.32604/CHD.2021.015062
ARTICLE
Scimitar Syndrome: Role of Right Atrial Longitudinal Strain. A Case Report
1Division of Cardiology, Department of Medical and Surgical Sciences, Magna Graecia University, Catanzaro, Italy
2Cardiovascular Research Center, Magna Graecia University, Catanzaro, Italy
3Department of Paediatric Cardiology, Royal Brompton Hospital, London, UK
4Department of Radiology, Magna Graecia University, Catanzaro, Italy
5Mediterranea Cardiocentro, Napoli, Italy
*Corresponding Author: Ciro Indolfi. Email: indolfi@unicz.it
Received: 09 November 2020; Accepted: 22 January 2021
Abstract: We describe a case of a rare congenital heart disorder, scimitar syndrome, diagnosed in an adult woman presenting with dyspnea on exertion, chest pain and recurrent episodes of pulmonary infections. The hallmark of the syndrome is the presence of an enlarged anomalous pulmonary vein draining into the inferior vena cava. Speckle tracking echocardiography, including the often-forgotten atrial strain evaluation, is a sensitive parameter that should be routinely used for a better clinical and prognostic evaluation of patients with congenital heart disease (CHD).
Keywords: Scimitar syndrome; RV overload; congenital heart disease; myocardial strain
A 51-year-old woman came to the emergency room complaining about chest pain and dyspnea on exertion. She reported fever and coughing for one week. Her general practitioner prescribed her antibiotics and corticosteroids. However, after an initial improvement, she got worse. About her past medical history, she reported recurrent episodes of pulmonary infections since she was a child. She denied remarkable pathologies and family history of sudden cardiac death. Electrocardiogram (ECG) at arrival showed sinus rhythm and no signs of overt acute ischemia or pulmonary embolism (PE). No ECG signs of right atrial (RA) or right ventricle (RV) overload were evident. Cardiac markers (Troponin T, CK-Mb) and D-Dimer were normal. Transthoracic echocardiography (TTE) revealed right ventricular (RV) enlargement with moderate-to-severe tricuspid regurgitation (TR) and normal left ventricular (LV) function. She was hospitalized to our Cardiology Unit to identify the cause of symptoms and RV overload. The patient provides her consent to publication.
Possible alternative diagnoses include PE, arrhythmogenic right ventricular dysplasia (ARVD), pulmonary hypertension (PH) and Congenital Heart Disease (CHD) with left-to-right shunt. As the patient complained about chest pain coronary artery disease (CAD) must be ruled out.
• CHD could remain undiagnosed until adulthood and left-to-right shunt disorders should be suspected in case of RV overload.
• Computed tomography angiography (CTA) is the gold standard to diagnose anomalous venous return but non-invasive echocardiographic evaluation, including Speckle Tracking Echocardiography (STE), could provide important diagnostic and prognostic information.
On physical examination she had a 2/6 systolic murmur at the left lower sternal border and no clinical signs of heart failure. She was afebrile and her blood pressure was 105/70 mmHg. The TTE confirmed the RV and atrial enlargement (RV Basal 50 mm; RV Mid 40 mm; Right Ventricular Outflow Tract (RVOT) Parasternal short axis proximal 34 mm; RVOT Parasternal Long Axis 32 mm; Right Atrial Volume index, RAVi, 45 ml/m2), with normal RV function (Tricuspid annular plane systolic excursion, TAPSE, 26 mm; Fractional Area Change, FAC, 41%) (Fig. 1). The Color-Doppler showed turbulent flow along the atrial septum, without overt shunt. A moderate-to-severe TR (Proximal Isovelocity Surface Area, PISA, Radius 7 mm; vena contracta 7 mm; TR Vmax 3.05 m/s) with PAPs = 45 mmHg was also evident. The inferior vena cava (IVC) had normal diameter (15 mm) with normal collapsibility during inspiration. Left ventricle and atrium were normal (LV End Diastolic Diameter, LVEDD, 46 mm; LV End Systolic Diameter, LVESD, 26 mm; Left Atrium Volume index, LAVi, 27 ml/m2; Ejection Fraction (EF) 57% Simpson Biplane; E/A 1.5; average E/e’ 4.5). Right Ventricular Global Longitudinal Strain (GLS–25.1%) and RV Free Wall Longitudinal Strain (RV FWLS–26.9%) were within the normal range (Fig. 1).
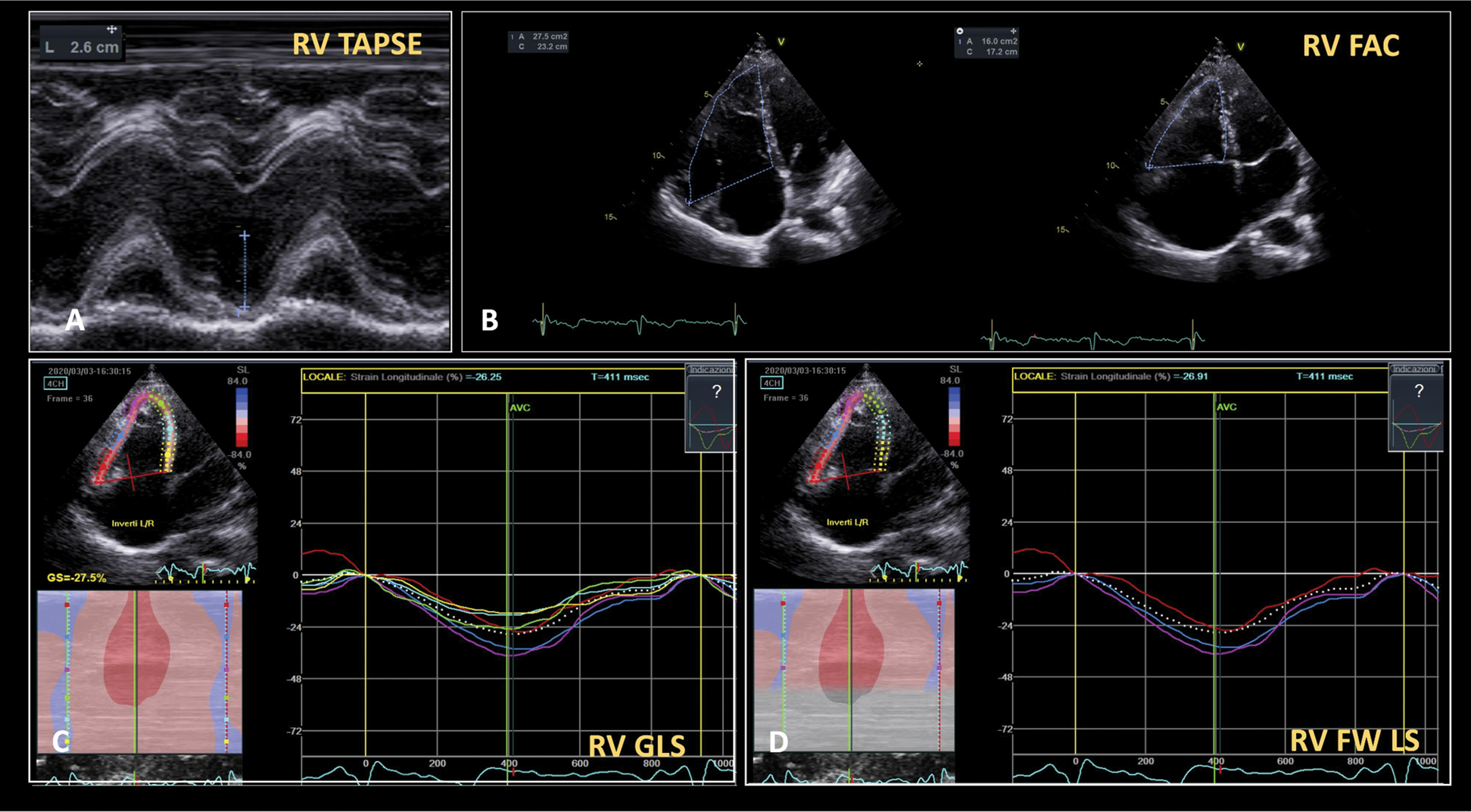
Figure 1: Right ventricular function evaluation. RV function evaluation using both TAPSE (Panel A), RV FAC (Panel B) and STE-based RV Global Longitudinal Strain (Panel C) and RV Free Wall Longitudinal Strain (Panel D). All indexes reveal normal RV function. FAC = Fractional Area Change. RV = Right Ventricular. STE = Speckle Tracking Echocardiography. TAPSE = Tricuspid Annular Plane Systolic Excursion
However, left and right atrial strain were below the reference ranges (Left Atrial Strain 27.3%; Right Atrial Strain 18.7%) [1,2] (Fig. 2).
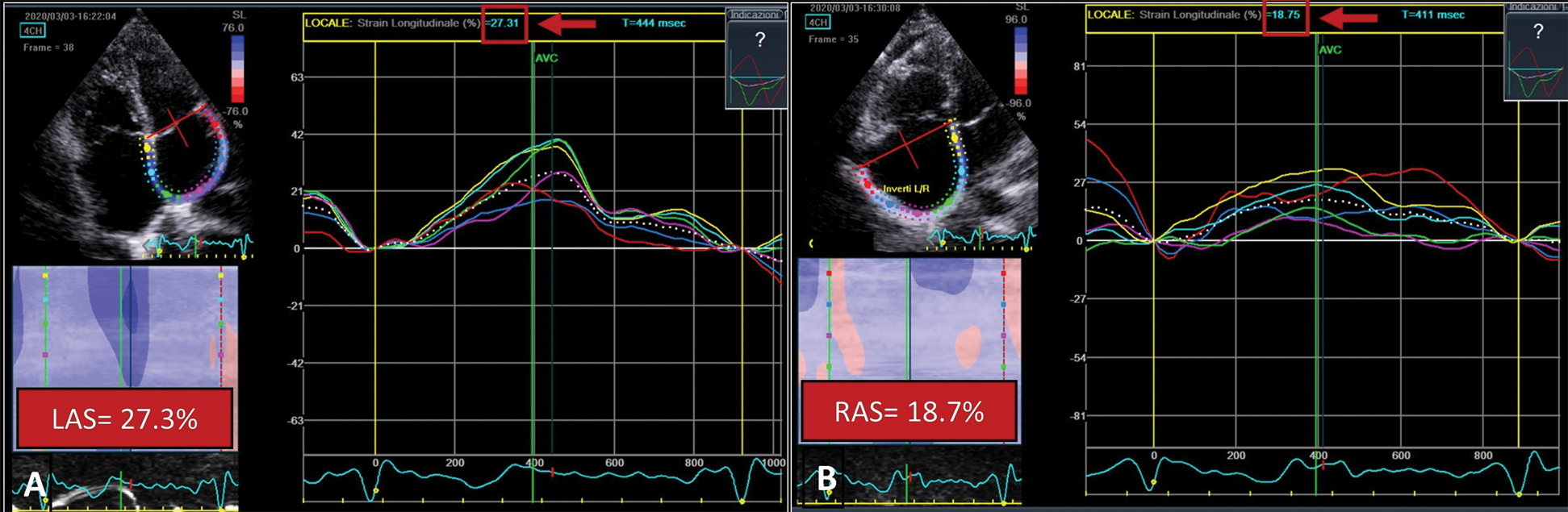
Figure 2: Atrial strain. Measurement of left atrial (Panel A) and right atrial (Panel B) longitudinal strain by speckle tracking. The atrial endocardial border is traced, divided in 6 regions and then analyzed by a semi-automatic software. After approval, segmental longitudinal strain curves are generated (solid-colored lines). The dashed line represents the average strain. Both indexes are below reference ranges. LAS = Left Atrial Strain; RAS = Right Atrial Strain
Non-invasive Myocardial Work Index (MWI) [3] showed fair strain-pressure loop (Fig. 3).
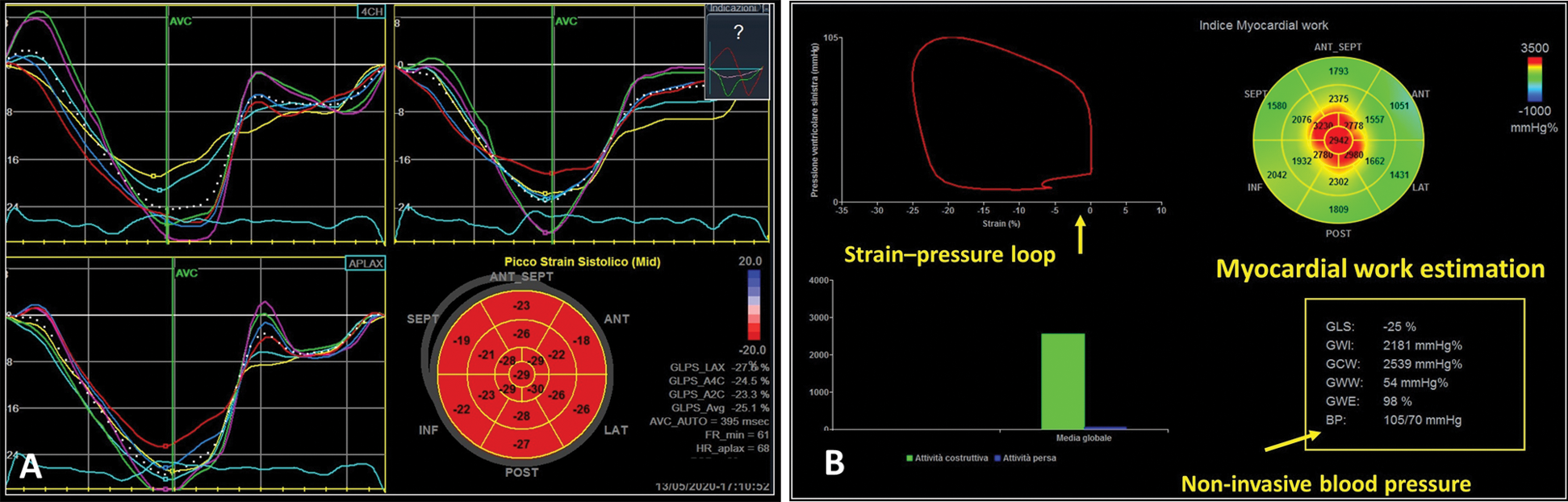
Figure 3: Non-Invasive Myocardial Work estimation. Panel A. Measurement of left ventricular longitudinal strain in the three apical long-axis views. Panel B. Myocardial Work estimation through a dedicated software (GE Healthcare). The area within the non-invasive left ventricular pressure-strain loop represents the global Myocardial Work Index (MWI). Segmental Myocardial Work is reported on the bull’s eye. Global Constructive Work, Global Wasted Work and Global Work Efficiency are also shown on the bottom right
The chest X-ray showed the absence of pleuro-parenchymal lesions but revealed an abnormal, enlarged pulmonary vein running along the right heart border (Fig. 4).
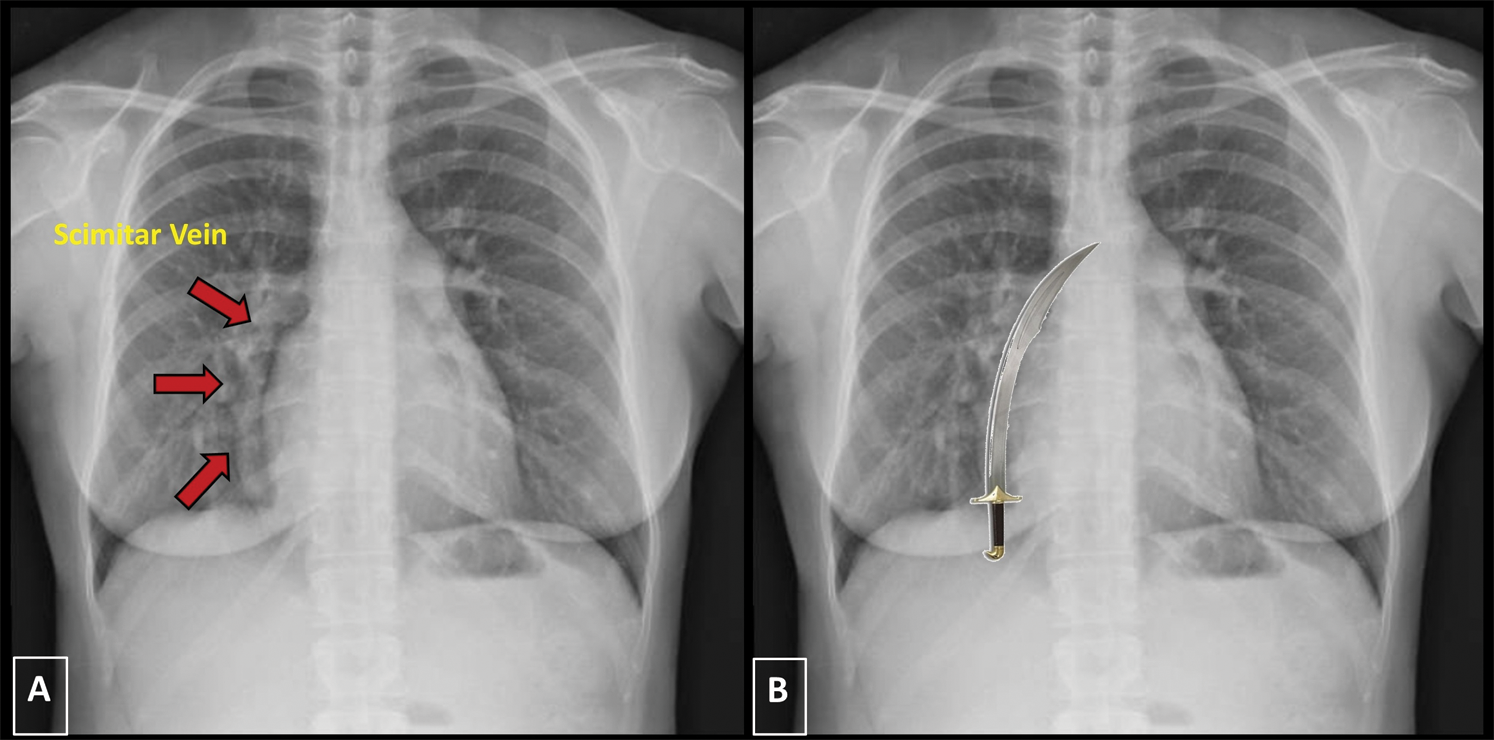
Figure 4: Chest X-ray. Panel A. In a posteroanterior (PA) view the chest X-ray shows a curved tubular opacity along the right heart border (red arrows). Panel B. The anomalous, enlarged, draining vein has the shape of the typical Turkish sword, the scimitar
A Computed Tomography Angiography (CTA) showed no filling defects in both pulmonary arteries but a partial anomalous pulmonary venous return (PAPVR), with a large vein originating from the right lung parenchyma draining into the IVC, complete absence of the usual right inferior pulmonary vein and a hypoplastic upper right vein draining into the LA. The right lung was slightly hypoplastic compared to the left, with right basal congestion, suggesting Scimitar Syndrome (Fig. 5).
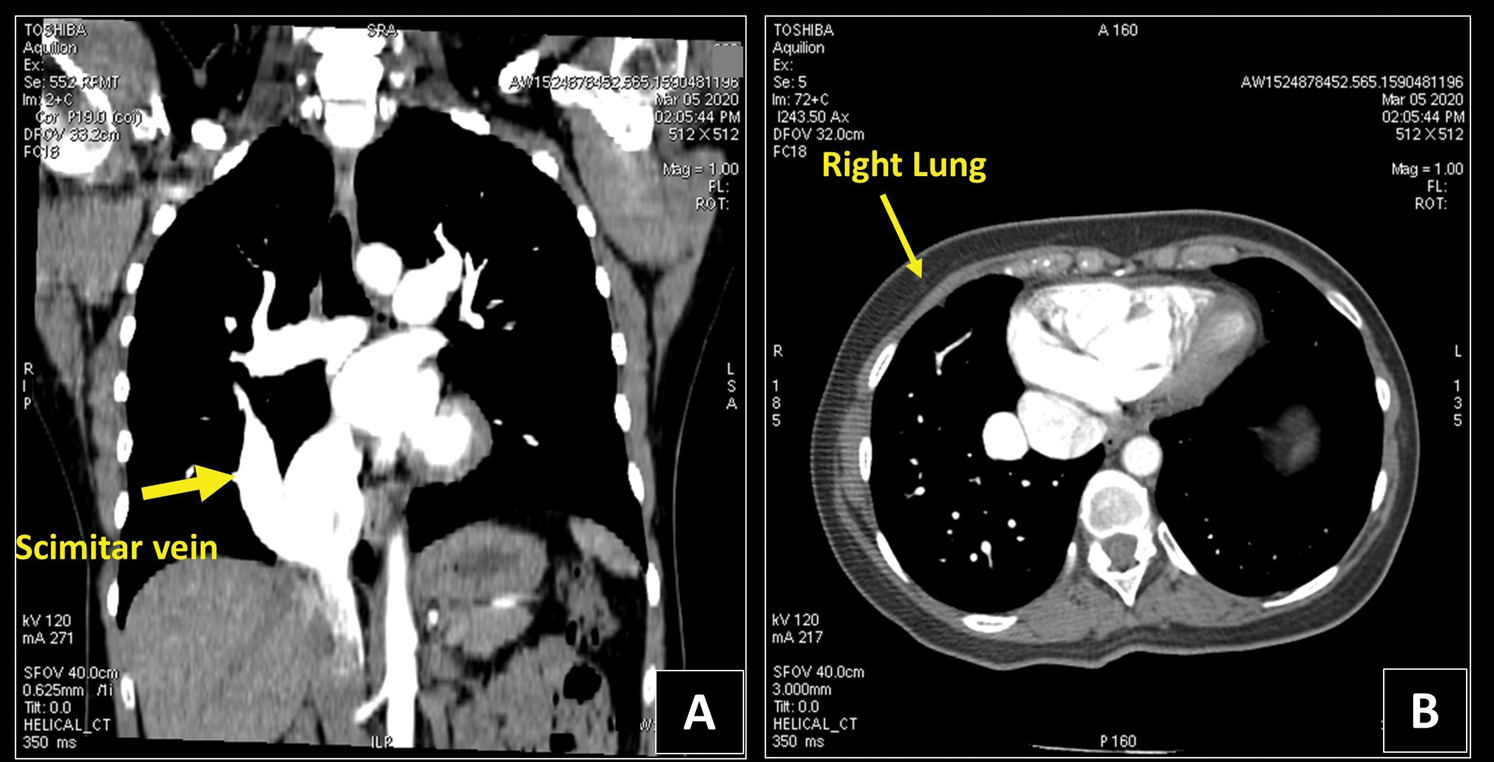
Figure 5: Chest CT. Panel A. The coronal CT view reveals an anomalous enlarged right vein, draining blood from the right lung to the inferior vena cava (yellow arrow). Panel B. The right lung is hypoplastic and more congested if compared to the left one at the CT exam. CT = Computed Tomography
A coronary CTA was then performed to rule out CAD, excluding both stenosis and abnormal origin of coronary arteries. Furthermore, the atrial septum was confirmed intact.
The patient complained about shortness of breath on exertion and, despite the two-dimensional (2D)-standard echo evaluation indicated RV enlargement but normal biventricular function, STE revealed reduced atrial strain, suggesting increased ventricular filling pressure and initial diastolic disfunction. According to the current recommendation [4], she was referred for surgical correction.
The scimitar syndrome is a rare CHD characterized by an abnormal pulmonary venous drainage into the IVC, variably associated with hypoplasia of the right lung and of the right pulmonary artery, systemic arterial supply for some part of the lung, atrial septal defect and heart dextroposition. The abnormal pulmonary vein is usually enlarged and runs along the right heart border, resembling the typical Turkish sword (“scimitar”) at chest X-ray (Fig. 4) [5]. Its clinical presentation varies from severe congestive heart failure to mild symptoms. In our patient, RV enlargement secondary to acute PE was excluded after a normal D-Dimer dosage, and CAD was ruled out after performing a coronary CT, according to the current guidelines and the pre-test probability for CAD [6]. ARVD was rejected as cause of RV enlargement because the current diagnostic criteria [7] were not fulfilled. CHD are often underdiagnosed in adult; in case of signs of RV overload and absence of septal defects an anomalous return of pulmonary vein must be investigated. Echocardiographic examination is crucial in the diagnostic pathway of these patients, although PAPVR is a frequently missed diagnosis at echocardiography. In addition to already consolidated conventional echocardiographic indices, STE have demonstrated to have a good reproducibility and capability to detect even subtle myocardial dysfunction [8]. A novel diagnostic tool, MWI, is capable to provide additional information on LV function with good accuracy, taking also into account load condition [3]. This index has demonstrated to detect even subtle myocardial disfunction in several clinical setting [9] and could be used in the routinely evaluation of patients with CHD to better evaluate myocardial performance. Myocardial work indices were completely normal in our patient, confirming a preserved left ventricular function already assessed by 2D ejection fraction and global longitudinal strain. However, as the use of MWI in this context has not been validated yet, this finding should be considered purely informative and cannot represent a relevant element to direct clinical management. Atrial strain is often overlooked during standard echocardiographic examination. However, LA strain has demonstrated to be an indirect index of LV filling pressure, diastolic dysfunction and to predict worse prognosis [10]; Right atrial function estimated by STE plays a crucial role in case of RV overload; in fact, a preserved RA contractility is essential in maintaining a proper RV output in the presence of elevated diastolic filling pressures. Identifying the failure of the right atrium in compensating the pressure overload of the RV, that often predicts RV dysfunction, might allow to better comprehend the stage of the disease and the hemodynamic of the patient. However, its diagnostic and prognostic role in patients with anomalous venous return is not yet well defined yet, despite its association with worse prognosis in several clinical setting including CHD [11]. Multi-chamber strain is a useful tool capable to provide crucial information on myocardial function, providing reliable prognostic information and holding a wide range of potential clinical applications in patients with CHD.
The scimitar syndrome is a rare and underdiagnosed PAPVR characterized by anomalous drainage of the right pulmonary vein in IVC. The assessment of ventricular function should take advantage of the information provided by advanced echocardiographic tools such as speckle tracking echocardiography and myocardial work non-invasive estimation, capable of identifying even subtle myocardial dysfunction. Moreover, the often-overlooked atrial function could provide additional insights about the hemodynamic of the patient and should always be included in the pre-operative echocardiographic assessment of patients with CHD.
Funding Statement: The authors received no specific funding for this study.
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
1. Brand, A., Bathe, M., Hübscher, A., Baldenhofer, G., Hättasch, R. et al. (2018). Normative reference data, determinants, and clinical implications of right atrial reservoir function in women assessed by 2D speckle-tracking echocardiography. Echocardiography, 35(10), 1542–1549. DOI 10.1111/echo.14092. [Google Scholar] [CrossRef]
2. Sugimoto, T., Robinet, S., Dulgheru, R., Bernard, A., Ilardi, F. et al. (2018). Echocardiographic reference ranges for normal left atrial function parameters: Results from the EACVI NORRE study. European Heart Journal—Cardiovascular Imaging, 19(6), 630–638. DOI 10.1093/ehjci/jey018. [Google Scholar] [CrossRef]
3. Russell, K., Eriksen, M., Aaberge, L., Wilhelmsen, N., Skulstad, H. et al. (2013). Assessment of wasted myocardial work: A novel method to quantify energy loss due to uncoordinated left ventricular contractions. American Journal of Physiology-Heart and Circulatory Physiology, 305(7), H996–H1003. DOI 10.1152/ajpheart.00191.2013. [Google Scholar] [CrossRef]
4. Vida, V. L., Guariento, A., Milanesi, O., Gregori, D., Stellin, G. et al. (2018). The natural history and surgical outcome of patients with scimitar syndrome: A multi-centre European study. European Heart Journal, 39(12), 1002–1011. DOI 10.1093/eurheartj/ehx526. [Google Scholar] [CrossRef]
5. Kuiper-Oosterwal, C. H., Moulaert, A. (1973). The scimitar syndrome in infancy and childhood. European Journal of Cardiology, 1(1), 55–61. [Google Scholar]
6. Knuuti, J., Wijns, W., Saraste, A., Capodanno, D., Barbato, E. et al. (2020). 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes. European Heart Journal, 41(3), 407–477. DOI 10.1093/eurheartj/ehz425. [Google Scholar] [CrossRef]
7. Marcus, F. I., McKenna, W. J., Sherrill, D., Basso, C., Bauce, B. et al. (2010). Diagnosis of arrhythmogenic right ventricular cardiomyopathy/dysplasia: Proposed modification of the Task Force Criteria. European Heart Journal, 31(7), 806–814. DOI 10.1093/eurheartj/ehq025. [Google Scholar] [CrossRef]
8. Bansal, M., Cho, G. Y., Chan, J., Leano, R., Haluska, B. A. et al. (2008). Feasibility and accuracy of different techniques of two-dimensional speckle based strain and validation with harmonic phase magnetic resonance imaging. Journal of the American Society of Echocardiography, 21(12), 1318–1325. DOI 10.1016/j.echo.2008.09.021. [Google Scholar] [CrossRef]
9. Sabatino, J., de Rosa, S., Leo, I., Spaccarotella, C., Mongiardo, A. et al. (2020). Non-invasive myocardial work is reduced during transient acute coronary occlusion. PLoS One, 15(12), e0244397. DOI 10.1371/journal.pone.0244397. [Google Scholar] [CrossRef]
10. Sabatino, J., di Salvo, G., Prota, C., Bucciarelli, V., Josen, M. et al. (2019). Left atrial strain to identify diastolic dysfunction in children with cardiomyopathies. Journal of Clinical Medicine, 8(8), 1243. DOI 10.3390/jcm8081243. [Google Scholar] [CrossRef]
11. Prota, C., di Salvo, G., Sabatino, J., Josen, M., Paredes, J. et al. (2019). Prognostic value of echocardiographic parameters in pediatric patients with Ebstein’s anomaly. International Journal of Cardiology, 278(Suppl. 2), 76–83. DOI 10.1016/j.ijcard.2018.10.046. [Google Scholar] [CrossRef]
 | This work is licensed under a Creative Commons Attribution 4.0 International License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. |