
 | Congenital Heart Disease |  |
DOI: 10.32604/CHD.2020.011709
ARTICLE
Long-Term Healthcare Utilization, Medical Cost, and Societal Cost in Adult Congenital Heart Disease
1Department of Public Health and Primary Care, Ghent University, Ghent, Belgium
2KU Leuven Department of Public Health and Primary Care, Academic Center for Nursing and Midwifery, KU Leuven–University of Leuven, Leuven, Belgium
3Faculty of Medicine and Health Sciences, Centre for Research and Innovation in Care, Division of Nursing and Midwifery, University of Antwerp, Antwerp, Belgium
4Research Foundation Flanders (FWO), Brussels, Belgium
5Department of Pediatric Cardiology, University Hospital Ghent, Ghent, Belgium
6KU Leuven Department of Cardiovascular Sciences, KU Leuven–University of Leuven, Leuven, Belgium
7Division of Congenital and Structural Cardiology, University Hospitals Leuven, Leuven, Belgium
8Pediatric and Congenital Cardiology Division, St-Luc University Hospital, Brussels, Belgium
9Department of Adult Congenital Cardiology, Ghent University Hospital, Ghent, Belgium
10McGill Adult Unit for Congenital Heart Disease Excellence (MAUDE Unit), McGill University Health Center, Montreal, Quebec, Canada
11Institute of Health and Care Sciences, University of Gothenburg, Gothenburg, Sweden
12Department of Pediatrics and Child Health, University of Cape Town, Cape Town, South Africa
*Corresponding Author: Ruben Willems. Email: Ruben.Willems@ugent.be
# Shared last author
Received: 20 May 2020; Accepted: 11 September 2020
Abstract: Objective: Cost-of-illness studies in Adult Congenital Heart Disease (ACHD) have mainly been limited to hospitalizations. This is the first paper to provide a comprehensive overview from a societal perspective including inpatient and outpatient medical costs, and absenteeism- and unemployment-related societal costs. Methods: A retrospective longitudinal (2006–2015) database analysis was performed in Belgium combining administrative and clinical databases (n = 10,572). Trends in resource use and costs per patient year were standardized to assess the impact of changes in the patient population composition. Generalized Linear Mixed Models assessed the impact of age, sex, lesion complexity, and time. Costs were converted to 2018 values. Results: Medical costs per patient year increased from €3490 to €4536 with a milder increase in patients with severe lesions. Although unemployment-related costs decreased, total societal costs increased due to more long-term (≥1 yr) invalidity. An increase in long-term invalidity was particularly found in patients ≥30 yrs and in patients with mild or moderate lesions. Resource use (e.g., dental care, nursing care, physiotherapy, emergency department) increased substantially in all patient groups over time. The annual percentage of patients with severe lesions receiving any cardiac and specialized cardiac follow-up increased with respectively 11 and 13 percent points to 81% and 52%, with a simultaneous decrease in hospitalization rate. Conclusion: Medical cost increases in ACHD are most pronounced in patients with mild and moderate lesions, relatable to their higher age. Economic data are necessary to allocate resources efficiently to ensure sustainable, qualitative care in an ageing patient population with strong increases in medical and long-term invalidity-related costs.
Keywords: Healthcare economics; adult congenital heart disease; health services
Medical progress, in combination with stronger organizational structures and improvements in general healthcare have seen a rapidly expanding adult patient population with congenital heart disease (CHD) [1,2]. Substantial yearly increases in absolute hospitalization numbers have been reported worldwide [3], and have imposed a growing burden on financial resources [4].
Costs have mainly been estimated based on hospitalizations rather than on outpatient care, despite the fact that the latter is a key element in care for adult congenital heart disease (ACHD) as lifelong follow-up is recommended to detect deterioration in a timely manner [5]. According to a recent systematic review, the number of outpatient cardiology visits increased by 8.2%–11.4% per year in the last few decades [3]. To the best of our knowledge, no cost data have been published on outpatient cardiac care, although such data could be beneficial in determining the most appropriate care level [5]. Moreover, literature on other outpatient healthcare utilization (HCU) remains scarce [6,7]. Previous research on hospitalization and outpatient care showed the importance of stratifying results by age, sex, and lesion complexity [3].
Furthermore, whether absenteeism and unemployment rates are higher in the ACHD population than in the general population appeared to vary by country [8]. Societal cost estimates are scarce [9].
A Belgian study was hence carried out (i) to describe long-term (2006–2015) inpatient and outpatient HCU, (ii) to calculate the associated medical costs for the health insurance and the patient (‘health expenditures’), as well as absenteeism-related and unemployment-related societal costs, and (iii) to determine the impact of age, sex, time, and lesion complexity. This study aims to address a knowledge gap that has already been identified by Task Force 5 at the 32nd Bethesda conference. The call was made then to study ACHD economics from a broad perspective, including outpatient medical costs and societal costs. This call had previously only been addressed to a minor extent, as described in the previous paragraphs [10].
A detailed description of the Belgian Congenital Heart Disease Database combining Administrative and Clinical data (BELCODAC) has been published elsewhere [11]. Briefly, the BELCODAC holds healthcare utilization data from ten consecutive years (i.e., 2006–2015), and clinical data from the same time period and before (e.g., information on early interventions). In particular, ten databases from five organizations were merged:
• The Intermutualistic Agency (IMA) is the umbrella organization of the seven Belgian sickness funds. The IMA delivered three population-level databases: (i) The population database (sociodemographic information), (ii) The pharmanet database (information on medications and their supply), and (iii) The medical claims database (medical care information).
• Statistics Belgium collects, processes and distributes data about Belgian society, and delivered four population-level databases: (i) The death certificate database, (ii) The sociodemographic database, (iii) The socioeconomic database, and (iv) The tax income statistics of the Belgian Federal Public Service Finance, also known as the Impôt des personnes Physiques CALculé (IPCAL) database.
• Ghent University Hospital, University Hospitals Leuven and St-Luc University Hospitals each provided part of the study population and delivered clinical information.
ACHD care is quite well-established in Belgium (11.4 million inhabitants), with four specialized hospitals designated to provide the full spectrum of CHD care, including congenital cardiac surgery [12], and established outpatient clinics in affiliated satellite centers. Three out of the four specialized hospitals took part in this study. Ghent University Hospital and University Hospitals Leuven selected all CHD patients who attended the specialized clinic at least once in their life. Patients of St-Luc University Hospital with severe lesions were included to ensure a reasonable sample size, so that cost-of-illness estimates would be stable for all subgroups [13]. An open cohort study was applied, with the inclusion of all living patients, and 18 years or older on 1 January during at least one year of the study period (2006–2015).
Results are reported as the annual percentage of patients requiring a certain type of HCU, and the per patient year number of visits per HCU type. Outpatient cardiology visits were classified as pediatric, ACHD, or general cardiology visits. Other HCU were hospitalizations (both cardiac and noncardiac) and length of stay (LOS), general practitioner (GP) visits, emergency department (ED) visits, outpatient visits to noncardiac medical specialists, dental care visits, physiotherapy visits and nursing visits (e.g., wound care in a home situation or outpatient visits).
Medical costs consisted of hospitalization, outpatient, and pharmaceutical costs. Out-of-pocket costs and reimbursed costs were analyzed separately. The societal costs consisted of unemployment and medical-related absenteeism costs. The latter was further classified as absenteeism for less than 1 year (in Belgium called ‘incapacity to work’), and absenteeism for more than 1 year (‘invalidity’). Short-term absenteeism (i.e., of less than one month for white-collar employees (≈clerical staff) and self-employees, and less than 14 days for blue-collar employees (≈manual workers)) was not included in the available data as this period is covered by the employer. Societal costs were calculated by multiplying the number of days unable to work by the average cost of absenteeism in Belgium [14], thus representing the potential productivity gain with full employment. All costs were inflated to 2018 euro values using the consumer price index [15].
The same epidemiological approach as in a recent paper on trends in palliative home care was used [16]. First, trends in HCU were plotted with descriptive, actual rates per year. Second, direct standardization was used to adjust for changes in the patient cohort composition during the study period. Standardization was based on age category (i.e., 18–29 y, 30–39 y, and ≥40 y), sex (i.e., men, women), and lesion complexity (i.e., mild, moderate, and severe) as defined by Task Force 1 at the 32nd Bethesda Conference [17]. The first year of the study period (i.e., 2006) was used as the base year, and that year’s composition of patient population characteristics (i.e., eighteen categories based on age category, sex, and lesion complexity) were kept constant over the entire study period. Then, for each year in the study period, the actual rate of HCU within each of the eighteen categories was applied to the base year’s patient population distribution to obtain the standardized HCU rate per year:
Here Hct stands for HCU (e.g., number of hospitalizations) in a given category c (e.g., 18–29 year old man with severe lesion) in a given year t (e.g., 2006–2015); Nct is the number of patient years in the given category c in the given year t; Nc2006 is the number of patient years in the given category c in 2006; N2006 is the total number of patient years in 2006.
The closer the actual and standardized (std) HCU rates were, the less impact possible changes in patient population composition had (or the composition was stable), and the more strongly the trends in HCU were impacted by within-group variation. Conversely, more pronounced differences between the actual and standardized HCU rates suggested a changing patient population composition in terms of age, sex, and complexity.
All data showed positively skewed distributions. Generalized linear mixed models with the log-link function and a negative binomial distribution were used to assess the impact of time, sex, lesion complexity, and age on count data such as HCU. A gamma distribution was applied if the dependent variable reflected cost data. Collinearity diagnostics were conducted, and tolerance values of 0.4 or lower were considered to reflect multicollinearity. p-values of ≤0.05 were considered statistically significant.
The analysis was performed using SAS Enterprise Guide V.7.1 (SAS Institute, Cary, NC, USA).
2.5 Patient and Public Involvement Statement
Not applicable.
A complete overview of the results can be found in Appendix.
3.1 Study Population Characteristics
The patient population increased by 36.6% from 7408 in 2006 to 10,122 in 2015. The mortality rate was low, with less than 1% of patients dying each year (i.e., varying between 20 deaths in 2006 and 68 deaths in 2015). Mortality was significantly higher in patients with severe lesions than in patients with mild lesions (Odds Ratio (OR) = 1.67) or moderate lesions (OR = 1.39). Mortality was also significantly higher in patients ≥40 y compared to patients 18–29 yrs (OR = 5.72) and patients 30–39 yrs (OR = 4.32). Sex distribution was nearly equal. The average age increased over the study period by 1.6 years reaching 38.3 years. Patients with mild lesions represented over half of the patient population throughout the study period, but the number of patients with moderate and severe lesions increased proportionally (Fig. 1).
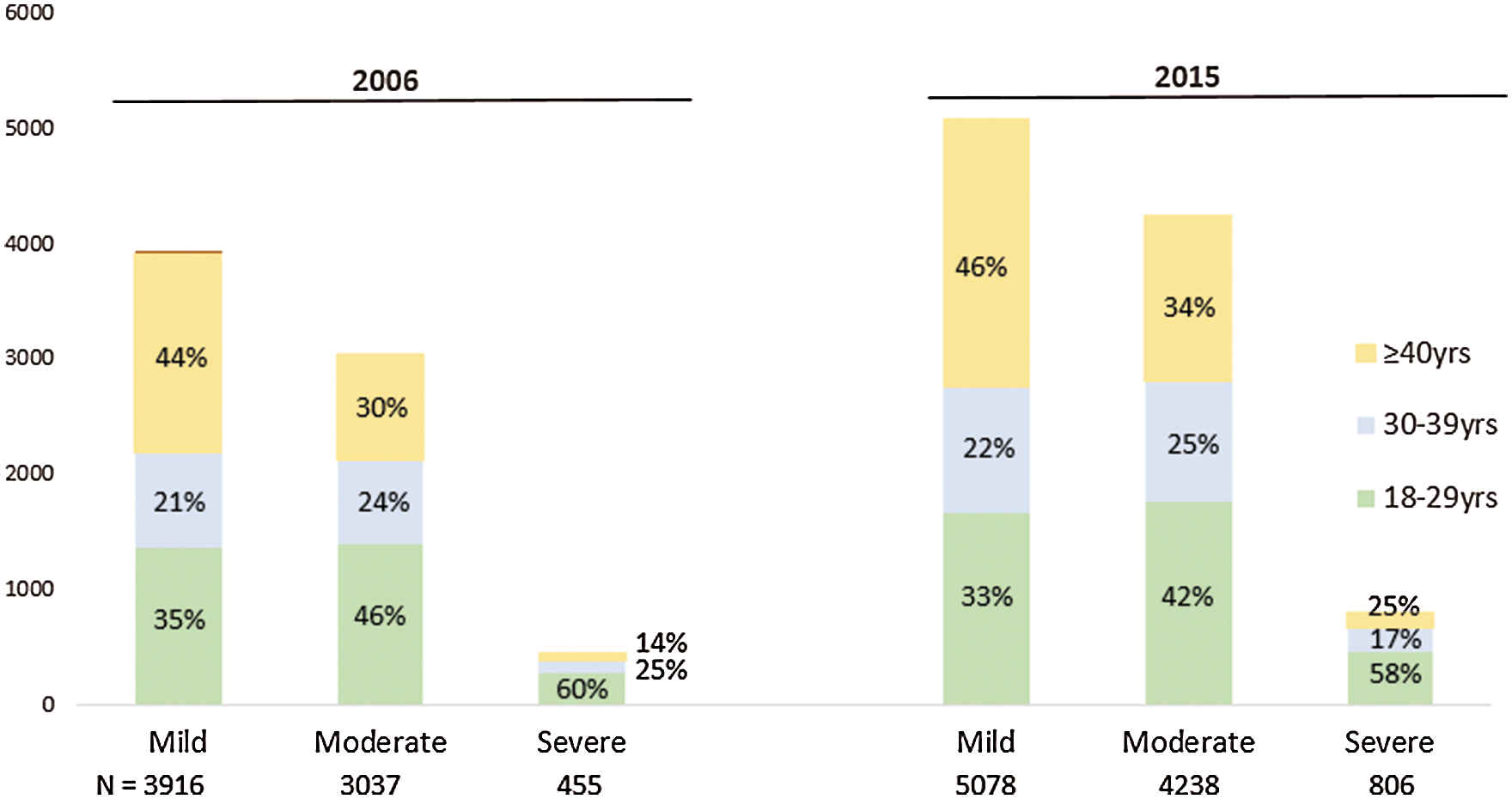
Figure 1: Demographics, stratified for age and lesion complexity, for the first and last year of the study period
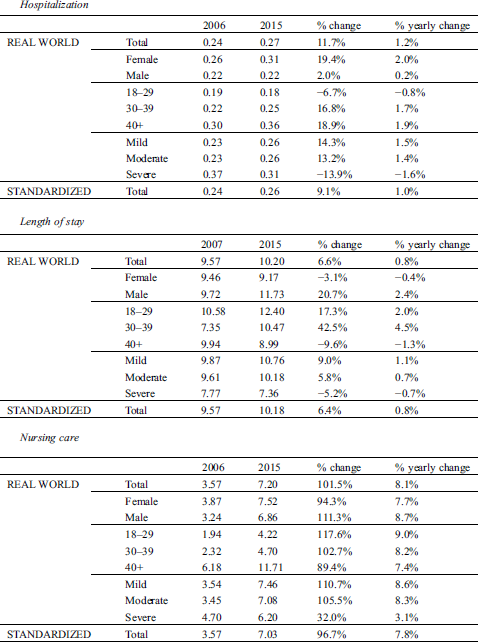
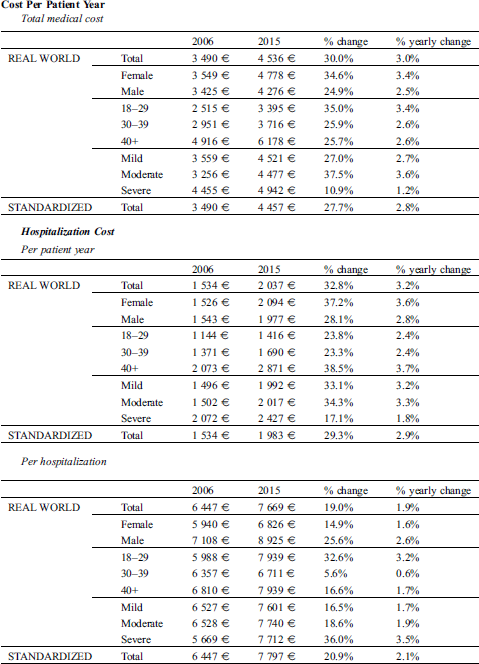
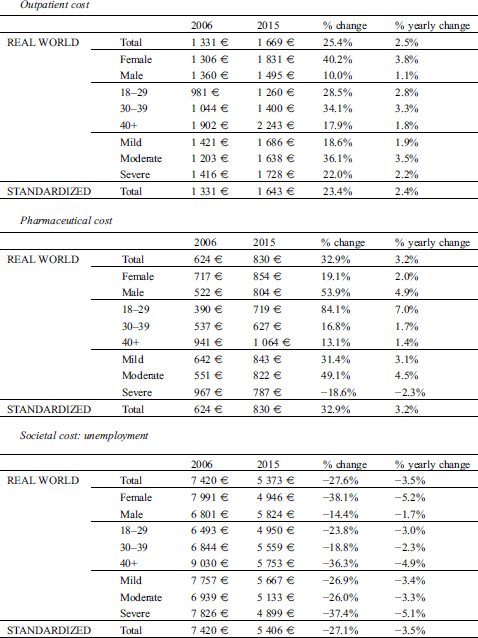
Trends. Medical costs per patient year increased by an average of 3% per year from €3490 to €4536 (std: €4457). The annual percentage increase appeared to be lower in patients with severe lesions (1.2% per year; Appendix). Hospitalization, outpatient and pharmaceutical costs accounted for ± 45%, 38%, and 18% of the total cost (Fig. 2). Hospitalization costs increased faster than outpatient costs (3.2% vs. 2.5% per year; Appendix).
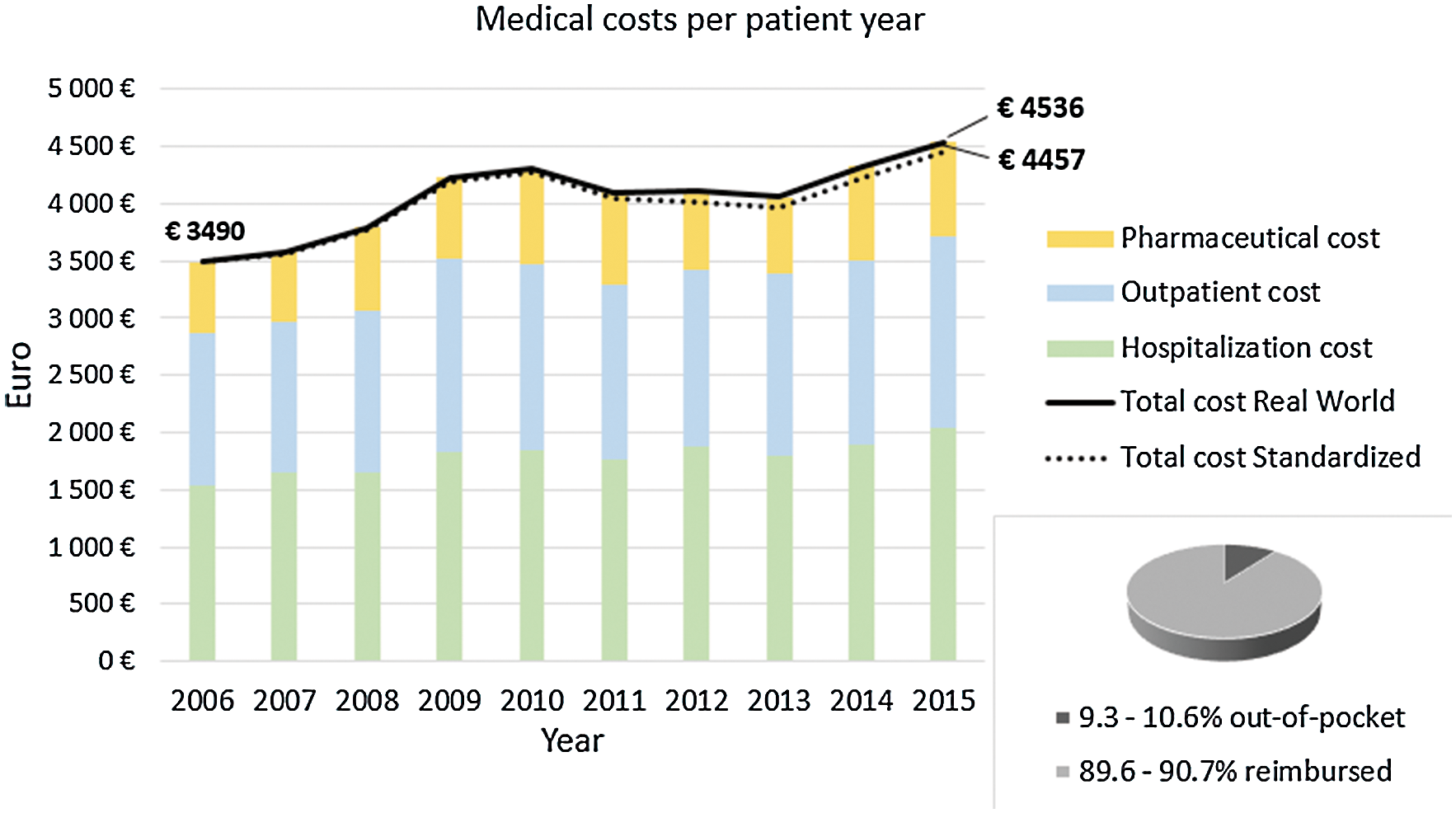
Figure 2: Medical costs per patient year, stratified for pharmaceutical, outpatient and hospitalization costs. Repartition between out-of-pocket and reimbursed costs
Determinants. Higher total medical costs were found in older age categories, patients with severe lesions, and women (Tab. 1).
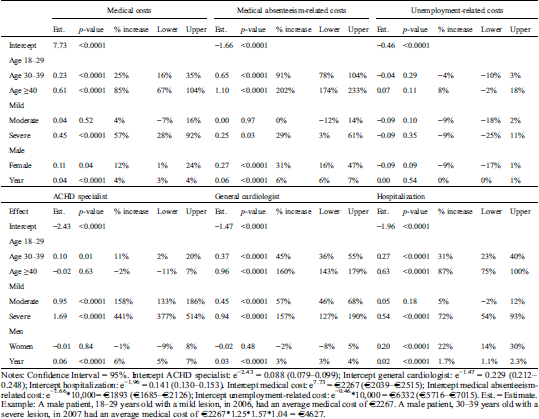
Table 1: Generalized Linear Mixed Model with annual outpatient cardiology visits, hospitalization, medical cost, medical absenteeism-related cost, and unemployment-related cost as dependent variables
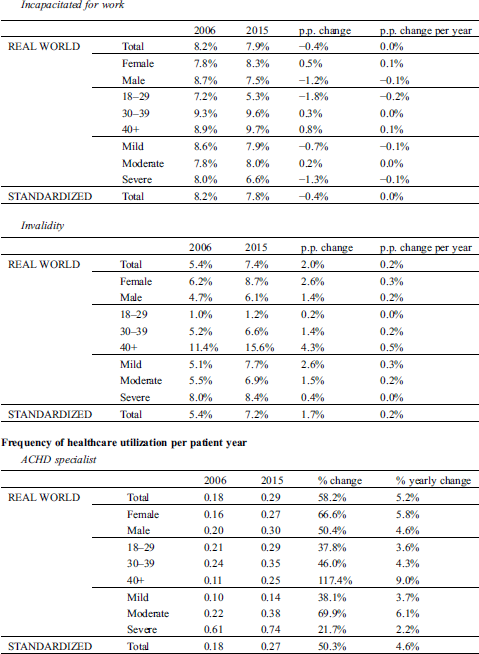
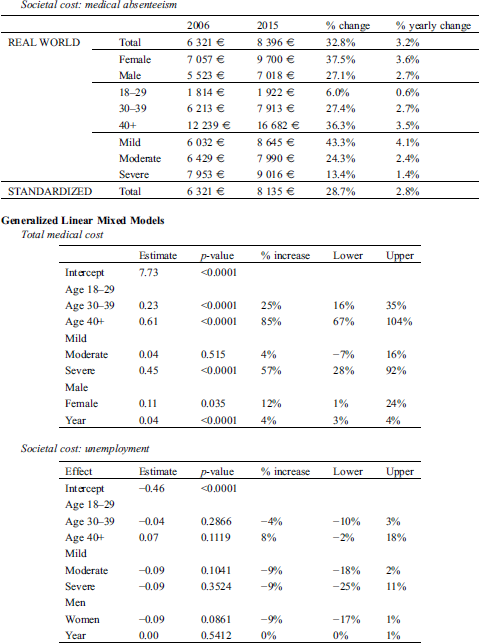
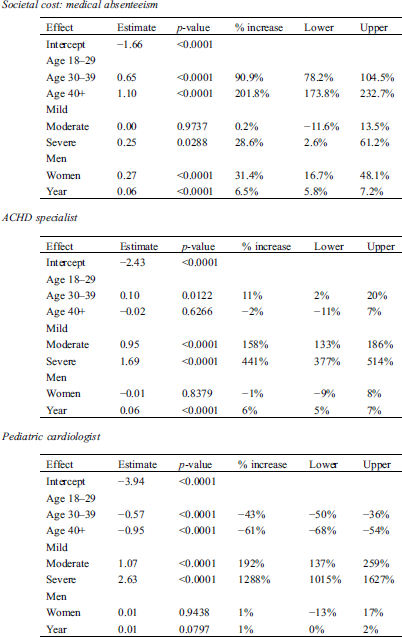
Trends. (Fig. 3) shows a 2.0 percent point (p.p.) increase to 7.4% (std: 7.2%) for invalidity while incapacity to work decreased 0.4 p.p. to 7.9% (std: 7.8%). Absenteeism-related costs per patient year increased from €6321 to €8396 (std: €8135). The increase was most pronounced in age categories ≥30 yrs and in patients with mild lesions.
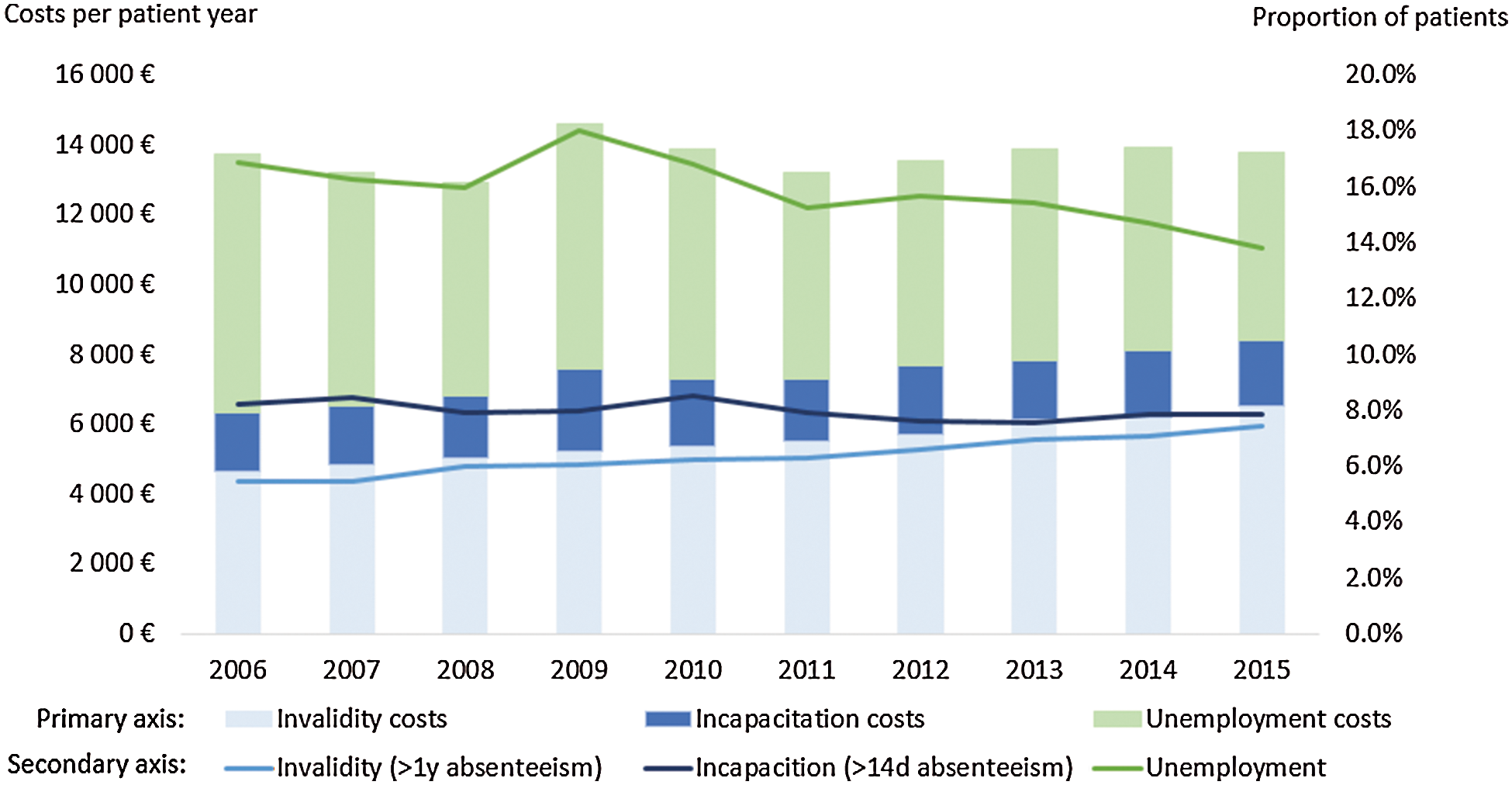
Figure 3: Bars: Real world societal costs related to absenteeism (invalidity + incapacitation) and unemployment. Lines: Proportion of patients being unemployed, incapacitated, or invalid for at least one day during a year
The proportion of patients unemployed for at least one day in a year decreased 3.1 p.p. to 13.8% (std: 13.8%). Unemployment-related costs per patient year decreased from €7420 to €5373 (std: €5406). The decrease was most pronounced in patients with severe lesions and in age category ≥40 yrs (Appendix).
Determinants. Higher absenteeism-related costs were found in older age categories, patients with severe lesions, and women. However, no covariates had a significant impact on unemployment-related costs (Tab. 1).
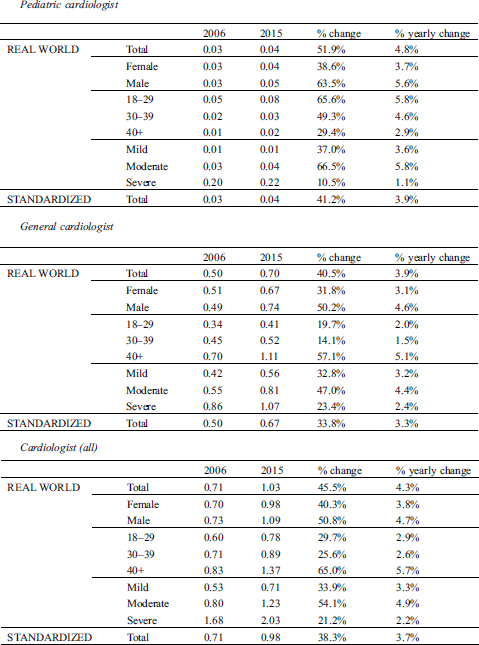
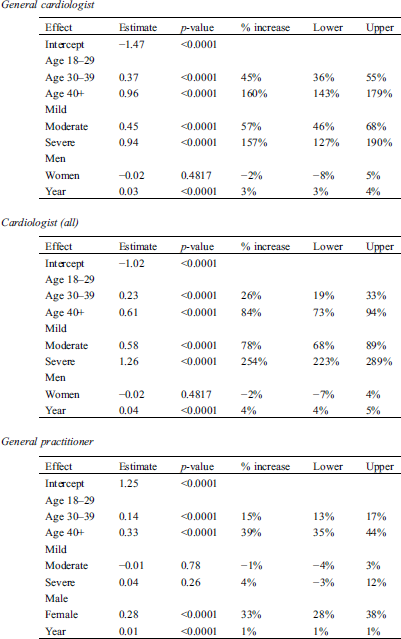
4.4 Outpatient Cardiology Visits
Trends. Forty-seven percent of patients visited a cardiologist in 2015, an 11.6 p.p. increase compared to 2006. In particular, there were increases in the proportion of patients with at least one visit to ACHD specialists (8.7 p.p. to 21%) and to general cardiologists (6.6 p.p. to 35%) (Fig. 4). In 2015, 81% (+10.9 p.p.) of patients with severe lesions had at least one cardiology visit, and 52% (+12.7 p.p.) had at least one ACHD specialist visit (Fig. 5). This all corresponded to an increase in total cardiology visits per patient year from 0.71 to 1.03 (std: 0.98). General cardiology visits were most common, with an increase from 0.50 to 0.70 (std: 0.67) visits per patient year. Likewise, ACHD specialist visits increased from 0.18 to 0.29 (std: 0.27) visits per patient year. The relative increase was strongest in the ≥40 yrs age group and in patients with moderate lesions (Appendix).
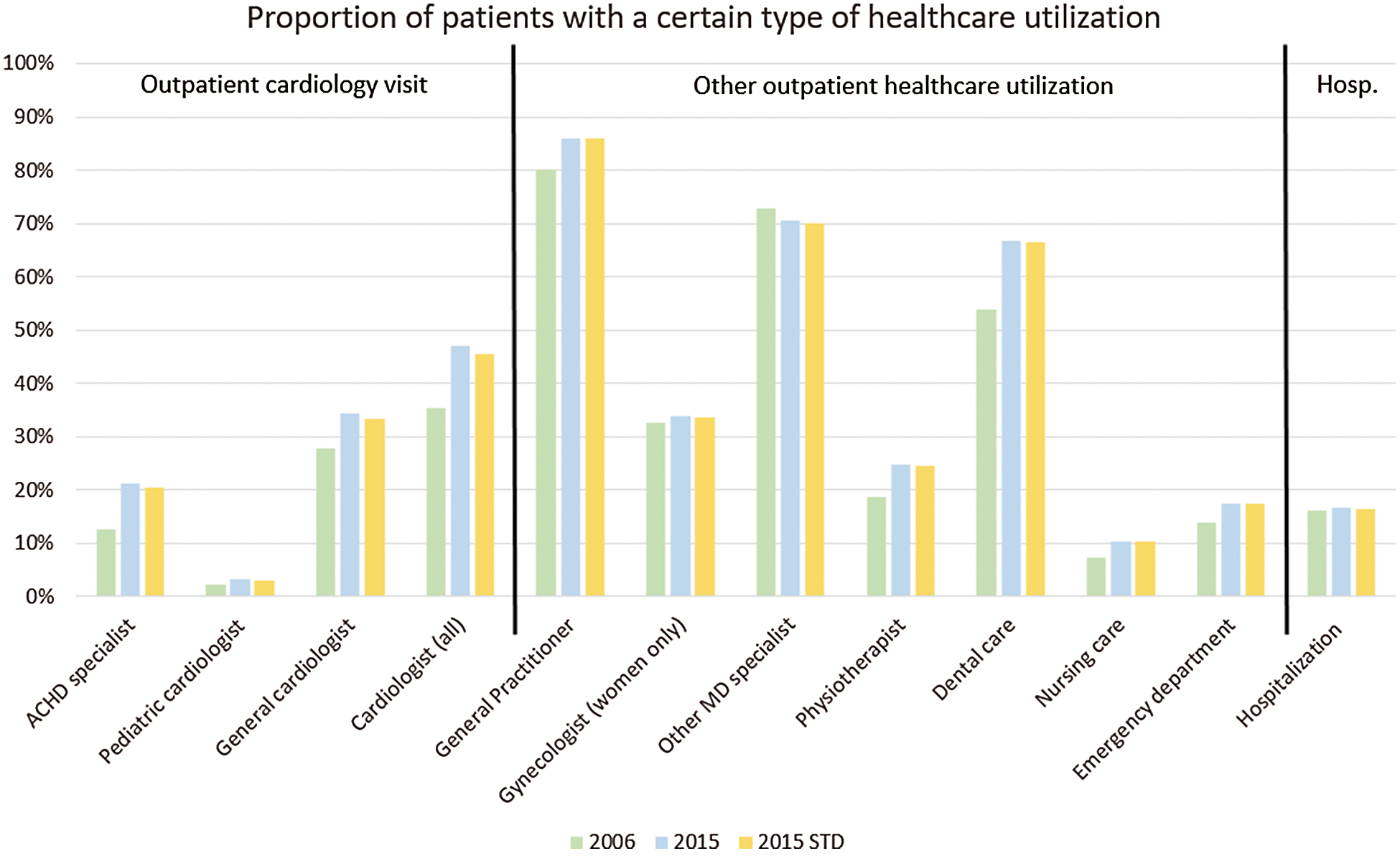
Figure 4: Real world proportion of patients per healthcare utilization type with at least one encounter. 2006 vs. 2015. ACHD: Adult congenital heart disease; MD: medical doctor. Please note that stratified results to lesion complexity, age, or sex can be found in the appendix online. Stratified results to lesion complexity for outpatient cardiology visits could be found in (Fig. 5)
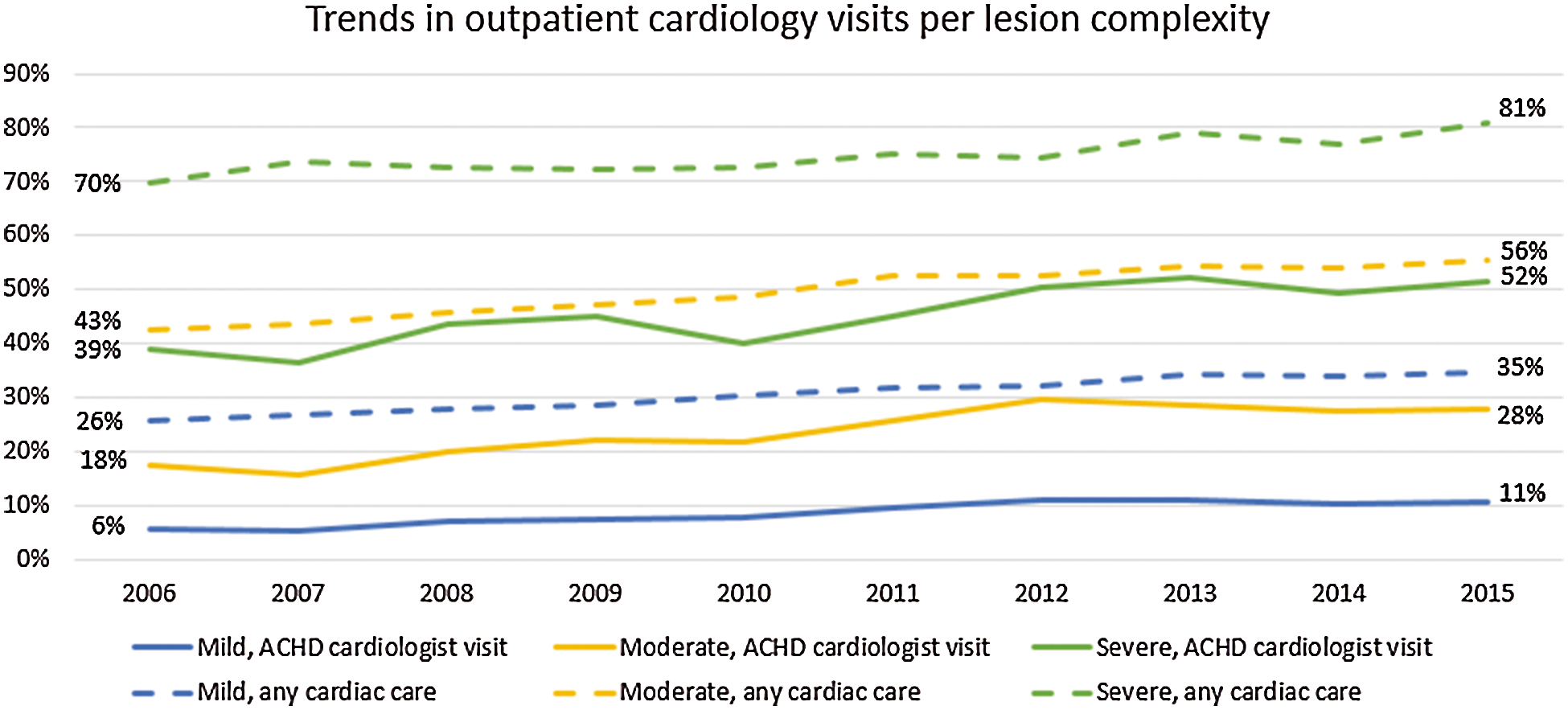
Figure 5: Real world proportion of patients with at least one encounter to a general cardiologist or an ACHD specialist. 2006 to 2015, per year, stratified for lesion complexity
Determinants. The ACHD specialist was visited significantly more by patients aged 30–39, and the general cardiologist by those aged ≥40 yrs. Higher lesion complexity was related to significantly more visits to all three cardiologist types. Sex did not have an impact (Tab. 1).
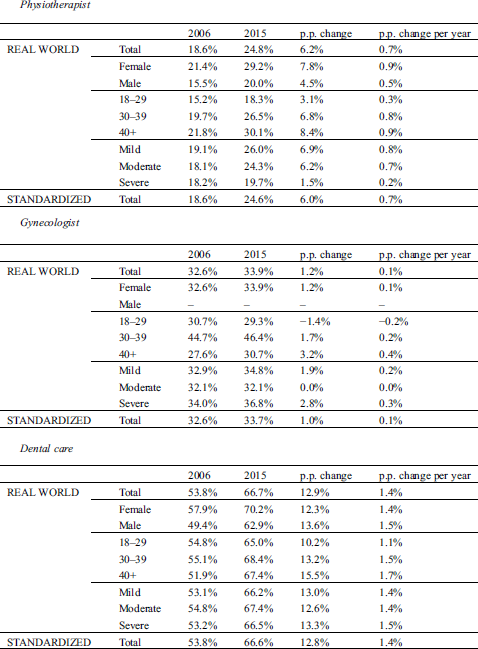
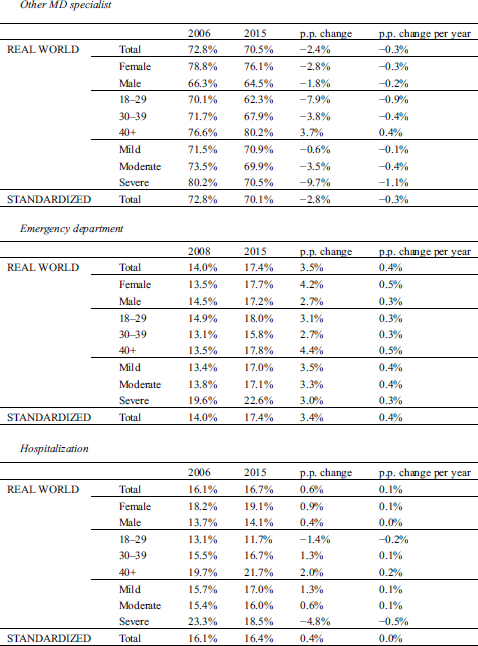
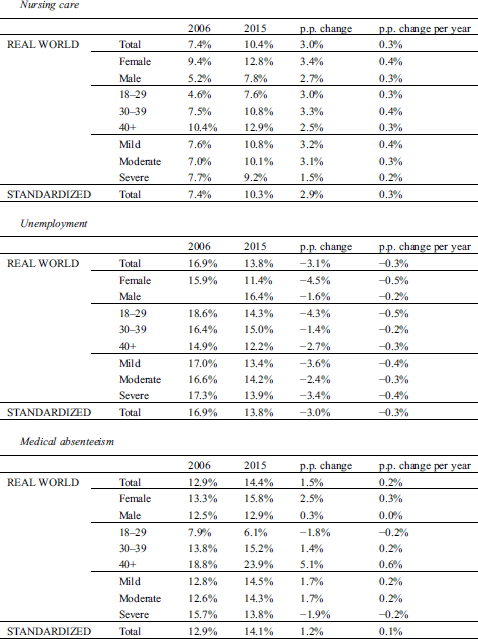
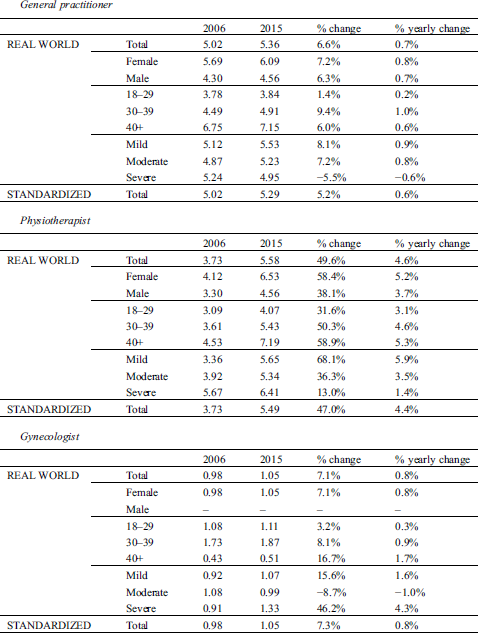
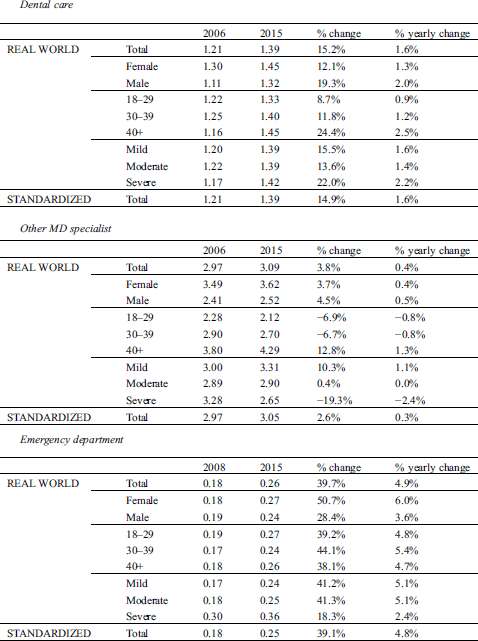
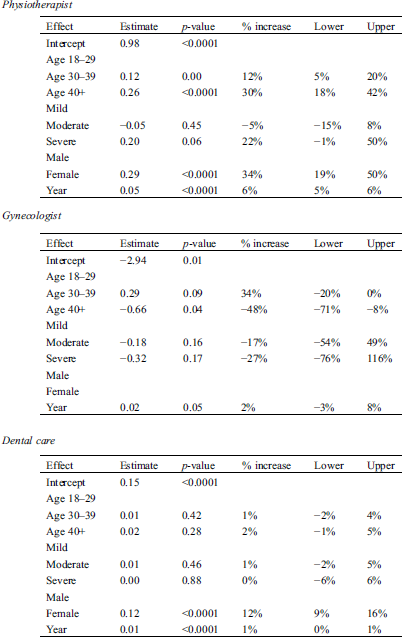
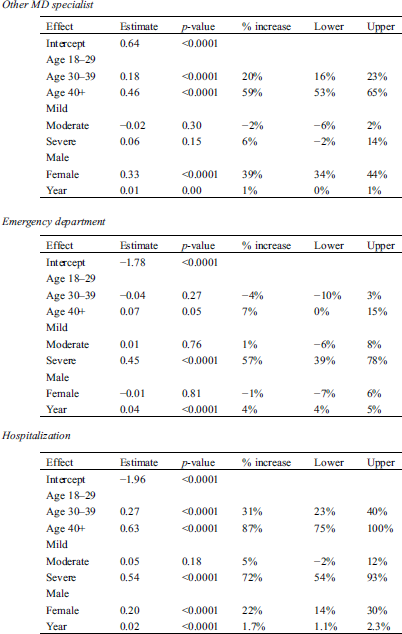
Trends. The annual percentage of patients with at least one outpatient visit to a particular health professional increased over time, except for visits to other MD specialists (Fig. 4). This corresponded to increases of 101.7%, 49.6%, 15.2%, 7.1%, and 39.7%, respectively in nursing care visits, physiotherapist care visits, dental care visits, gynaecology visits, and ED visits per patient year (Appendix).
Determinants. The effect of age and lesion complexity varied by type of HCU, but overall, women appeared to incur significantly more HCU (Appendix).
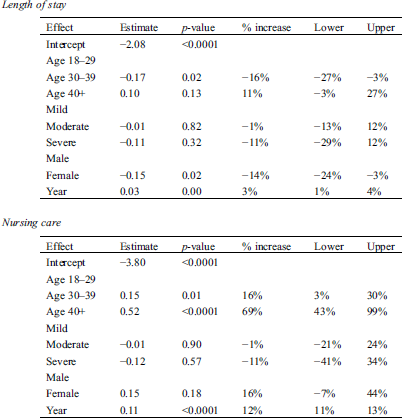
Trends. The annual hospitalization rate remained stable over time with 16%–17% of patients being hospitalized (Fig. 4). The number of hospitalizations per patient year however increased from 0.24 to 0.27 (std: 0.26), and the average LOS per hospitalization increased from 9.57 to 10.20 days (std: 10.18). Importantly, such an increase was only noted in patients with mild or moderate lesions: Decreases in hospitalization rate from 0.37 to 0.31 and in LOS from 7.8 to 7.4 days were found in patients with severe lesions (Appendix).
Determinants. The hospitalization rate was 72% (54%–93%) higher in patients with severe lesions than in patients with mild lesions. LOS did not differ significantly for lesion complexity. Age categories 30–39 and ≥40 yrs were associated with respectively 31% (23–40%) and 87% (75–100%) more hospitalizations. Women were 22% (14–30%) more hospitalized than men with a 14% (3–24%) shorter LOS (Tab. 1).
This longitudinal, multicenter cost-of-illness study made use of a retrospective database linking administrative and clinical data. This study showed substantial increases in per patient year medical and absenteeism-related costs, as well as a decrease in unemployment-related costs. The standardized values, adjusting for the ageing and more complex patient population, mitigated the increase in medical and absenteeism-related costs to a limited extent. In other words, there would have been a slightly smaller cost increase if the patient population composition had remained stable over time.
Medical costs. The percentage increase in medical costs over time is higher in patients with mild or moderate lesions than in patients with severe lesions. Possible explanations for this include the greater age of the group with mild to moderate lesions, leading to a more rapid increase in comorbidities, a suboptimal fit between care needs and care received, technological evolution [3], or simply because patients with severe lesions already incurred high costs before and had an increased mortality rate. A previous study on medical costs in Belgium was conducted in 1997 [18]. Adjusting for inflation and excluding pharmaceutical costs (as not all pharmaceutical costs were available), medical costs did not increase between 1997 and 2006 while our results showed a 29% increase between 2006 and 2015. This older study was correctly framed as a pilot study because, apparently, an excessively high cost estimate resulted from selection bias as only patients seen by an ACHD specialist were selected. For example, the hospitalization rate in that study was substantially higher [18]. Despite the limitations to this comparison, it seems that costs have recently accelerated, driven by strong increases in outpatient HCU, while the hospitalization rate per patient year has increased more slowly. However, this acceleration was also encouraged by the increasing cost per hospitalization which could be explained by the longer LOS [19], and the greater disease burden, related to the ageing patient population over time [19,20].
Societal costs. Only one previous (US) study calculated the productivity loss cost following hospitalization [9]. In our study, we calculated the productivity loss cost, taking into account absenteeism and unemployment. The societal costs of adults with CHD appeared to be higher than their medical costs. Note that only part of these costs could be attributed specifically to the ACHD pathology as absenteeism and unemployment are prevalent in the general population as well. Unemployment and invalidity were the most important cost components of societal costs, with an increasing role being placed by invalidity-related costs. Invalidity appeared to become more prevalent over time, similarly to trends observed in the general population [21]. General explanations include medical progress leading to better survival, increasing labor market participation, and policy measures such as a higher retirement age [22]. Invalidity in the ACHD population was higher than in the general population (7.4% vs. 5%) despite the fact that invalidity normally occurs more often after the age of 50 [21], while our ACHD cohort was relatively young. Unemployment (and its related costs) decreased, while in the general population it remained stable between 2006 and 2015 and only decreased after 2015 [23], offering positive prospects. Recent research has demonstrated lower unemployment and invalidity rates in Belgium than in other countries [8]. Hence, even more pressing societal costs may be encountered elsewhere.
Outpatient cardiology visits. Fewer outpatient cardiology visits were counted among patients with mild lesions than in previous European studies, while comparable rates were found for patients with moderate and severe lesions [20,24]. One in five patients with severe lesions had no cardiac follow-up in the last year of the study period, but increasing numbers of patients received specialized care while hospitalization rates decreased. Furthermore, general cardiology visits remained more prevalent in patients with mild and moderate lesions and in patients ≥40 yrs. In light of the results of Mylotte et al. [25] and Cordina et al. [26], who demonstrated clinical benefits following ACHD specialist visits, special attention should be given to guiding patients towards specialist care. However, more research is needed to settle the debate about shared care for patients with mild and moderate lesions.
In order to correctly interpret the trends in outpatient cardiology visits (cfr. Figs. 4 and 5), it is important to know that the Belgian ACHD medical care system has undergone continuous development in recent decades. The Belgian healthcare system is characterized by a high degree of accessibility and freedom of choice. Most ACHD patients were diagnosed in childhood, during which time they are followed by pediatric cardiologists. During adolescence, the pediatric cardiologist makes the call to start the transition process to adult services. For example, the transition program of Ghent University Hospital, which has been described in detail by de Hosson et al. [27] developed gradually during the study period, before becoming fully operational in 2015. The development of such transition programs has taken many years, and is a major aspect of the continuously improving ACHD medical care system. Better transition to adult services is surely one of the reasons that an increasing proportion of ACHD patients are receiving regular follow-up by ACHD specialists. All ACHD patients are encouraged to remain under periodic specialized follow-up as the long-term consequences are yet to be scrutinized. A decision can be made in consultation between the patient and the ACHD specialist to have periodic follow-up elsewhere as well. In this regard, Goossens et al. [28] demonstrated a low lost-to-follow-up rate after transition in Belgium. As mentioned before, patients also have the freedom to remain under the follow-up of a pediatric cardiologist, although this is generally exceptional, all the more since admission to pediatric services is not allowed above age 15.
Other. Other outpatient HCU in this study is higher than in the Dutch study of Schoormans et al. [7] (e.g., >80% vs. 40% of patients visiting a GP in the course of a year). Apart from healthcare system differences, dissimilarities in research aims may explain these differences. Schoormans et al. [7] assessed cardiac disease-related outpatient visits only, whereas we assessed outpatient visits regardless of cause. Our longitudinal analysis revealed increases in most types of HCU which were more pronounced in patients with mild and moderate lesions. This is in line with the results obtained for outpatient cardiology visits (in this and in previous research [25]): Patients with mild and moderate lesions are older, leading to a more pronounced increase in HCU. One important type of HCU is dental care to prevent infective endocarditis [29]. Annual visits are highly recommended for many patients with ACHD. An increase in dental care has been noted over the study period, resulting in 67% of the patients receiving dental care in 2015. This is substantially lower than found in a recent self-reporting study (86% in Belgium) [30], suggesting a self-reporting bias, and warranting continued patient education. Dental care in adults with CHD is, however, better than dental care in the general population (±50%) [31].
Sex. Previous literature on sex disparities was inconclusive even though there seemed to be a tendency towards more HCU in women [3]. This study supported the thesis of higher medical costs in women although the cost per hospitalization was higher in men. Several explanations can be put forward to explain this disparity such as the impact of pregnancy management and –related hospitalization [32]. Previous research also suggested that, overall, women experience fewer barriers to making use of available healthcare services subsequently leading to a lower need for long-term inpatient care [33].
A particular strength of this study is that the cost estimations are sound and robust as our approach meets the most important recommendations on how to conduct a cost-of-illness study: Our calculation stems from a database linking clinical, demographic, resource use, and actual cost data [34–36], taking into account a broad range of cost components [13]. A number of limitations should be addressed as well. First, the retrospective data were not primarily gathered to answer specific research questions [37]. For example, we were not able to specifically determine details of hospitalizations such as the medical department in which they took place. Administrative databases are also prone to miscoding and missing data [37]. However, retrospective database research is a low-cost solution to providing a large sample size, which counters the small number of miscoded and missing data [37]. Second, the BELCODAC is built on all ACHD patients affiliated with the two Flemish tertiary centers. Only patients with severe lesions were included from the third center. However, the oversampling of patients with severe lesions does not impede generalization because the patients included from the third hospital accounted for less than 2% of included patients. Third, although our study sample is comparable to those in other countries [11], an initial selection bias towards more severe lesions cannot be excluded as only patients who were ever seen in an academic hospital were included. Patients with less severe lesions who never need to be referred to an academic hospital were thus missed [11]. Fourth, we did not analyze HCU for specific congenital anomalies separately. For example, we did not analyze different mild lesions separately despite possible differences in HCU [3]. Fifth, our calculation did not include HCU that cannot be reimbursed. For example, adult psychotherapy is only reimbursed in some rare cases, and is therefore only partly included in our analyses. Sixth, how societal costs should be calculated has been a point of discussion for many years. Every estimation is a function of some assumptions. In our calculations, for example, as suggested by Hankivsky et al. [38], we made use of the average population earnings in order to not discriminate by sex, age or profession.
Despite some limitations, this study has important added value because, to date, no comprehensive cost-of-illness research had been conducted in the ACHD population. The importance and applicability of cost-of-illness studies for clinicians and policy makers is manifold as it can help determine the most appropriate care level, populate cost-effectiveness models, and provide insight into future budget impact. This study demonstrated increased access to specialized cardiac care, lower unemployment, and more long-term invalidity. Overall, the medical cost increase is most pronounced for patients with mild or moderate lesions, probably due to their higher age. The analysis of past data adds to our understanding of the future financial burden of ACHD care with unchanged policies. It is a collective responsibility to provide our patients with appropriate care while making efforts to limit the financial burden on both patients and society.
Availability of Data and Materials: Not available.
Ethical Approval: The study was approved by the privacy commission (SCSZG/17/184) and the ethical committees of the participating hospitals (S59858, B670201731994, 2017/26JUI/332).
Contributions: RW, JDB, and LA designed the study protocol. RW analyzed the data and wrote the manuscript draft. All authors contributed substantially to the construction of the database, the conceptualization and design of the manuscript, revised the manuscript critically for important intellectual content, and approved the manuscript to be submitted.
Acknowledgement: The authors thank all employees working at StatBel and the InterMutualistic Agency for their contribution to the data collection and their valuable input on the selection of the variables.
Funding Statement: This work was supported by Research Foundation Flanders [G097516N to PM and 12E9816N to EG], the Fondation Nationale de Reserche en Cardiologie Pédiatrique, and the King Baudouin Foundation (Fund Joseph Oscar Waldmann-Berteau & Fund Walckiers Van Dessel). Julie De Backer is supported as senior clinical researcher, Eva Goossens as postdoctoral researcher, and Liesbet Van Bulck as pre-doctoral researcher by the Research Foundation Flanders.
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
1. Marelli, A. J., Ionescu-Ittu, R., Mackie, A. S., Guo, L., Dendukuri, N. et al. (2014). Lifetime prevalence of congenital heart disease in the general population from 2000 to 2010. Circulation, 130(9), 749–756. DOI 10.1161/circulationaha.106.627224.
2. Khairy, P., Ionescu-Ittu, R., Mackie, A. S., Abrahamowicz, M., Pilote, L. et al. (2010). Changing mortality in congenital heart disease. Journal of the American College of Cardiology, 56(14), 1149–1157. DOI 10.1016/j.jacc.2010.03.085.
3. Willems, R., Werbrouck, A., De Backer, J., Annemans, L. (2019). Real-World Healthcare Utilization in adult congenital heart disease. Cardiology in the Young, 29(5), 553–563. DOI 10.1017/S1047951119000441.
4. Mackie, A. S., Tran, D. T., Marelli, A. J., Kaul, P. (2017). Cost of congenital heart disease hospitalizations in Canada: A population-based study. Canadian Journal of Cardiology, 33(6), 792–798. DOI 10.1016/j.cjca.2017.01.024.
5. Baumgartner, H., Bonhoeffer, P., De Groot, N. M., de Haan, F.,Deanfield, J. E. et al. (2010). ESC Guidelines for the management of grown-up congenital heart disease (new version 2010). European Heart Journal, 31(23), 2915–2957. DOI 10.1093/eurheartj/ehq249.
6. Mackie, A. S., Pilote, L., Ionescu-Ittu, R., Rahme, E., Marelli, A. J. (2007). Health care resource utilization in adults with congenital heart disease. American Journal of Cardiology, 99(6), 839–843. DOI 10.1016/j.amjcard.2006.10.054.
7. Schoormans, D., Sprangers, M. A., Pieper, P. G., van Melle, J. P.,van Dijk, A. P. et al. (2011). The perspective of patients with congenital heart disease: Does health care meet their needs? Congenital Heart Disease, 6(3), 219–227. DOI 10.1111/j.1747-0803.2011.00521.
8. Sluman, M. A., Apers, S., Sluiter, J. K., Nieuwenhuijsen, K., Moons, P. et al. (2019). Education as important predictor for successful employment in adults with congenital heart disease worldwide. Congenital Heart Disease, 14(3), 362–371. DOI 10.1111/chd.12747.
9. Seckeler, M. D., Thomas, I. D., Andrews, J., Joiner, K., Klewer, S. E. (2016). A review of the economics of adult congenital heart disease. Expert Review of Pharmacoeconomics & Outcomes Research, 16(1), 85–96. DOI 10.1586/14737167.2016.1140575.
10. Skorton, D. J., Garson, A.Jr., Allen, H. D., Fox, J. M., Truesdell, S. C. et al. (2001). Task force 5: Adults with congenital heart disease: Access to care. Journal of the American College of Cardiology, 37(5), 1193–1198. DOI 10.1016/S0735-1097(01)01274-8.
11. Ombelet, F., Goossens, E., Willems, R., Annemans, L., Budts, W. et al. (2020). Creating the BELgian COngenital heart disease Database combining Administrative and Clinical data (BELCODACRationale, design and methodology. International Journal of Cardiology, 316, 72–78. DOI 10.1016/j.ijcard.2020.05.059.
12. Belgian Government. (2014). Koninklijk Besluit houdende vaststelling van de normen waaraan de zorgprogramma's “cardiale pathologie” moeten voldoen om erkend te worden [Royal Resolution on the norms care programs ‘cardiac pathology’ should meet in order to be certified]. http://www.ejustice.just.fgov.be/eli/besluit/2004/07/15/2004022658/justel.
13. Clabaugh, G., Ward, M. M. (2008). Cost-of-illness studies in the United States: A systematic review of methodologies used for direct cost. Value in Health, 11(1), 13–21. DOI 10.1111/j.1524-4733.2007.00210.x.
14. European Commission. (2018). European Statistics. Labour Cost Levels by NACE Rev. 2 Activity. https://appsso.eurostat.ec.europa.eu/nui/show.do?dataset=lc_lci_lev&lang=en.
15. European Commission. (2018). European Statistics. Harmonised Index of Consumer Prices. https://ec.europa.eu/eurostat/web/hicp/data/database.
16. Maetens, A., Deliens, L., Van den Block, L.,Beernaert, K., Cohen, J. (2019). Are we evolving toward greater and earlier use of palliative home care support? A trend analysis using population-level data from 2010 to 2015. Journal of Pain and Symptom Management, 58(1), 19–28. DOI 10.1016/j.jpainsymman.2019.04.008.
17. Warnes, C. A., Liberthson, R., Danielson, G. K., Dore, A., Harris, L. et al. (2001). Task force 1: The changing profile of congenital heart disease in adult life. Journal of the American College of Cardiology, 37(5), 1170–1175. DOI 10.1016/S0735-1097(01)01272-4.
18. Moons, P., Siebens, K., De Geest, S., Abraham, I., Budts, W. et al. (2001). A pilot study of expenditures on, and utilization of resources in, health care in adults with congenital heart disease. Cardiology in the Young, 11(3), 301–313. DOI 10.1017/S1047951101000336.
19. Cedars, A. M., Burns, S., Novak, E. L., Amin, A. P. (2016). Lesion-specific factors contributing to inhospital costs in adults with congenital heart disease. American Journal of Cardiology, 117(11), 1821–1825. DOI 10.1016/j.amjcard.2016.03.016.
20. Tutarel, O., Kempny, A., Alonso-Gonzalez, R., Jabbour, R., Li, W. et al. (2014). Congenital heart disease beyond the age of 60: Emergence of a new population with high resource utilization, high morbidity, and high mortality. European Heart Journal, 35(11), 725–732. DOI 10.1093/eurheartj/eht257.
21. Saks, Y. (2017). Een beter inzicht in het verloop van het aantal begunstigden van de invaliditeitsverzekering [A better insight in the course of the number of beneficiaries of the invalidity insurance]. Economisch tijdschrift, September, 59–73. https://www.nbb.be/doc/ts/publications/economicreview/2017/ecotijdii2017.pdf.
22. National Institute for Health and Disability Insurance. (2016). Statistieken over de invaliditeit van werknemers en werklozen in 2015 [Statistics on invalidity of employees en unemployed in 2015]. https://www.inami.fgov.be/nl/statistieken/uitkeringen/2015/Paginas/statistieken-invaliditeit.aspx.
23. European Commission. (2020). European statistics. Unemployment rate by sex and age 2006-2015. https://appsso.eurostat.ec.europa.eu/nui/show.do?dataset=une_rt_a&lang=en.
24. Engelfriet, P., Boersma, E., Oechslin, E., Tijssen, J., Gatzoulis, M. A. et al. (2005). The spectrum of adult congenital heart disease in Europe: Morbidity and mortality in a 5 year follow-up period. The Euro Heart Survey on adult congenital heart disease. European Heart Journal, 26(21), 2325–2333. DOI 10.1093/eurheartj/ehi396.
25. Mylotte, D., Pilote, L., Ionescu-Ittu, R., Abrahamowicz, M., Khairy, P. et al. (2014). Specialized adult congenital heart disease care: The impact of policy on mortality. Circulation, 129(18), 1804–1812. DOI 10.1161/CIRCULATIONAHA.113.005817.
26. Cordina, R., Nasir Ahmad, S., Kotchetkova, I., Eveborn, G., Pressley, L. et al. (2018). Management errors in adults with congenital heart disease: Prevalence, sources, and consequences. European Heart Journal, 39(12), 982–989. DOI 10.1093/eurheartj/ehx685.
27. de Hosson, M.,De Backer, J., De Wolf, D., De Groote, K., Demulier, L. et al. (2020). Development of a transition program for adolescents with congenital heart disease. European Journal of Pediatrics, 179(2), 339–348. DOI 10.1007/s00431-019-03515-4.
28. Goossens, E., Stephani, I., Hilderson, D., Gewillig, M., Budts, W. et al. (2011). Transfer of adolescents with congenital heart disease from pediatric cardiology to adult health care: an analysis of transfer destinations. Journal of the American College of Cardiology, 57(23), 2368–2374. DOI 10.1016/j.jacc.2010.11.068.
29. Di Filippo, S., Delahaye, F., Semiond, B., Celard, M., Henaine, R. et al. (2006). Current patterns of infective endocarditis in congenital heart disease. Heart, 92(10), 1490–1495. DOI 10.1136/hrt.2005.085332.
30. Holbein, C. E., Peugh, J., Veldtman, G. R., Apers, S., Luyckx, K. et al. (2019). Health behaviours reported by adults with congenital heart disease across 15 countries. European Journal of Preventive Cardiology, 27(10), 1077–1087. DOI 10.1177/2047487319876231.
31. Bottenberg, P., Vanobbergen, J., Declerck, D., Carvalho, J. C. (2019). Oral health and healthcare utilization in Belgian dentate adults. Community Dentistry and Oral Epidemiology, 47(5), 381–388. DOI 10.1111/cdoe.12484.
32. Shum, K. K., Gupta, T., Canobbio, M. M., Durst, J., Shah, S. B. (2018). Family planning and pregnancy management in adults with congenital heart disease. Progress in Cardiovascular Disease, 61(3–4), 336–346. DOI 10.1016/j.pcad.2018.08.001.
33. Osika Friberg, I., Krantz, G., Maatta, S., Jarbrink, K. (2016). Sex differences in health care consumption in Sweden: A register-based cross-sectional study. Scandinavian Journal of Public Health, 44(3), 264–273. DOI 10.1177/1403494815618843.
34. Greenberg, D., Mohamed Ibrahim, M. I. B., Boncz, I. (2014). What are the challenges in conducting cost-of-illness studies? Value in Health Regional Issues, 4, 115–116. DOI 10.1016/j.vhri.2014.08.003.
35. Durand-Zaleski, I. (2008). Why cost-of-illness studies are important and inform policy. Vascular Medicine, 13(3), 251–253. DOI 10.1177/1358863X08091738.
36. Riley, G. F. (2009). Administrative and claims records as sources of health care cost data. Medical Care, 47(7 Suppl 1), S51–S55. DOI 10.1097/MLR.0b013e31819c95aa.
37. Sedgwick, P. (2014). Retrospective cohort studies: Advantages and disadvantages. British Medical Journal, 348, g1072. DOI 10.1136/bmj.g1072.
38. Hankivsky, O., Friesen, J., Varcoe, C., MacPhail, F., Greaves, L. et al. (2004). Expanding economic costing in health care: Values, gender and diversity. Canadian Public Policy/Analyse De Politiques, 30(3), 257–282. DOI 10.2307/3552302.
Appendix
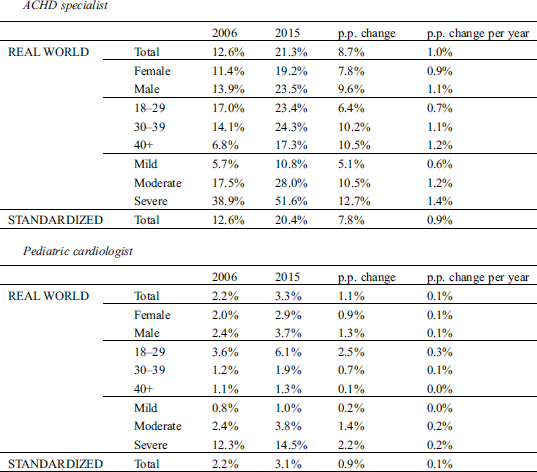
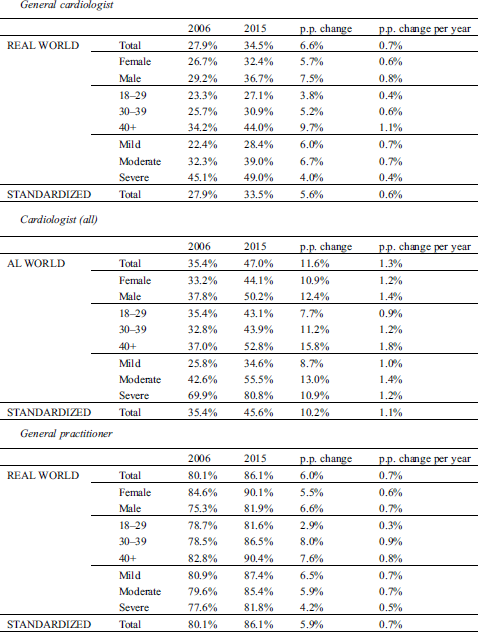
Proportion of Patients Making Use of a Certain Type of Healthcare Utilization
 | This work is licensed under a Creative Commons Attribution 4.0 International License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. |