

 | Congenital Heart Disease |  |
DOI: 10.32604/CHD.2020.011527
ARTICLE
Positional Hypoxemia from Persistent Left Superior Vena Cava Draining to the Left Atrium
1Division of Pediatric Cardiology, Seattle Children’s Hospital and the University of Washington School of Medicine, Seattle, WA 98105, USA
2Division of Pediatric Pulmonary and Sleep Medicine, Seattle Children’s Hospital and the University of Washington School of Medicine, Seattle, WA 98105, USA
*Corresponding Author: Naveed Rabbani. Email: Naveed.Rabbani@SeattleChildrens.org
Received: 15 May 2020; Accepted: 30 July 2020
Abstract: Persistent left superior vena cava (PLSVC) is a relatively common congenital venous anomaly that typically drains into the coronary sinus without hemodynamic significance. Rarely a PLSVC drains directly into the left atrium, forming a right-to-left shunt that can result in hypoxemia and potential paradoxical embolism. We present the case of a 2-year-old medically complex child on chronic mechanical ventilation with eventual diagnosis of episodic hypoxemia due to a PLSVC draining into the left atrium with position-dependent venous flow. The lesion was identified with contrast echocardiography and cardiac MRI. Subsequent occlusion with a vascular plug resulted in resolution of the child’s positional hypoxemia. This case extends available reports for this rare presentation of PLSVC and serves as a reminder of the importance of injection site in contrast echocardiography.
Keywords: Venous anomalies; echocardiography; congenital heart disease; right-to-left shunting; hypoxemia
Persistent left superior vena cava (PLSVC) is the most common congenital anomaly of the thoracic venous system. In the vast majority of cases, a PLSVC drains into the coronary sinus and subsequently into the right atrium without hemodynamic consequence. Rarely, a PLSVC may drain into the left atrium, resulting in a right-to-left shunt that can lead to hypoxemia or paradoxical embolism. We present the case of a 2-year-old medically complex boy with a PLSVC draining to the roof of the left atrium who presented with head-position-dependent hypoxemia. The case extends available reports, serving as a reminder of the broad differential for hypoxemia and the importance of injection site for contrast echocardiogram studies.
We describe the case of a 2-year-old medically complex boy with extreme prematurity, bronchopulmonary dysplasia requiring mechanical ventilation via tracheostomy, and restrictive perimembranous ventricular septal defect (VSD) who presents to cardiology clinic with positional hypoxemia.
The patient was born at 26 weeks of gestation via urgent Caesarian section due to fetal decelerations to a 37-year-old G1P1 woman with pregnancy complicated by pre-eclampsia, intra-uterine growth restriction, and prenatally-diagnosed VSD. His prolonged postnatal hospitalization was complicated by severe bronchopulmonary dysplasia and tracheomalacia with chronic hypercarbic and hypoxemic respiratory failure requiring tracheostomy and mechanical ventilation. An echocardiogram at one week of age showed a large patent ductus arteriosus with low velocity bidirectional flow, a moderate perimembranous VSD with low-velocity left-to-right flow, and a patent foramen ovale with left-to-right flow.
Throughout his 14 month hospitalization, the patient tolerated slow weans of ventilator settings despite requiring a higher than expected fraction of inspired oxygen and experiencing intermittent desaturation events. These desaturation events were initially attributed to multifactorial respiratory system disease. Serial echocardiograms showed no evidence of pulmonary hypertension and demonstrated all four pulmonary veins draining in to the left atrium, resolution of the patent ductus arteriosus, and the perimembranous VSD becoming more pressure and volume restricted due to impingement of the septal leaflet of the tricuspid valve. Saline contrast echocardiography with right arm injection was performed due to continued intermittent hypoxemic episodes, failing to identify a right-to-left shunt.
After discharge, further progression in ventilator weans was limited by persistent episodic hypoxemia at home. Over time, the patient’s parents noted a pattern of reproducible cyanosis with head turn to the right, which they demonstrated for providers at a follow up appointment in pulmonary clinic when the patient was 24 months old. The positional hypoxemia was not associated with hypoventilation (no changes in end-tidal CO2 or exhaled tidal volumes) and was not responsive to supplemental oxygen, but improved with return of head to neutral position, raising concern for a position-dependent shunt. Review of past echocardiograms suggested a possible PLSVC in the absence of a dilated coronary sinus. Saline contrast echocardiography with injection in the left arm showed vigorous contrast return to the left atrium, suggestive of a PLSVC to left atrial connection (Fig. 1). This was further confirmed on cardiac MRI for surgical planning, demonstrating a PLSVC draining into the left atrium with a small bridging vein between the right and left superior vena cavae. With the patient’s head turned to the right, there was a 50% decrease in flow in the right SVC and a compensatory increase in flow in the left SVC (Fig. 2).
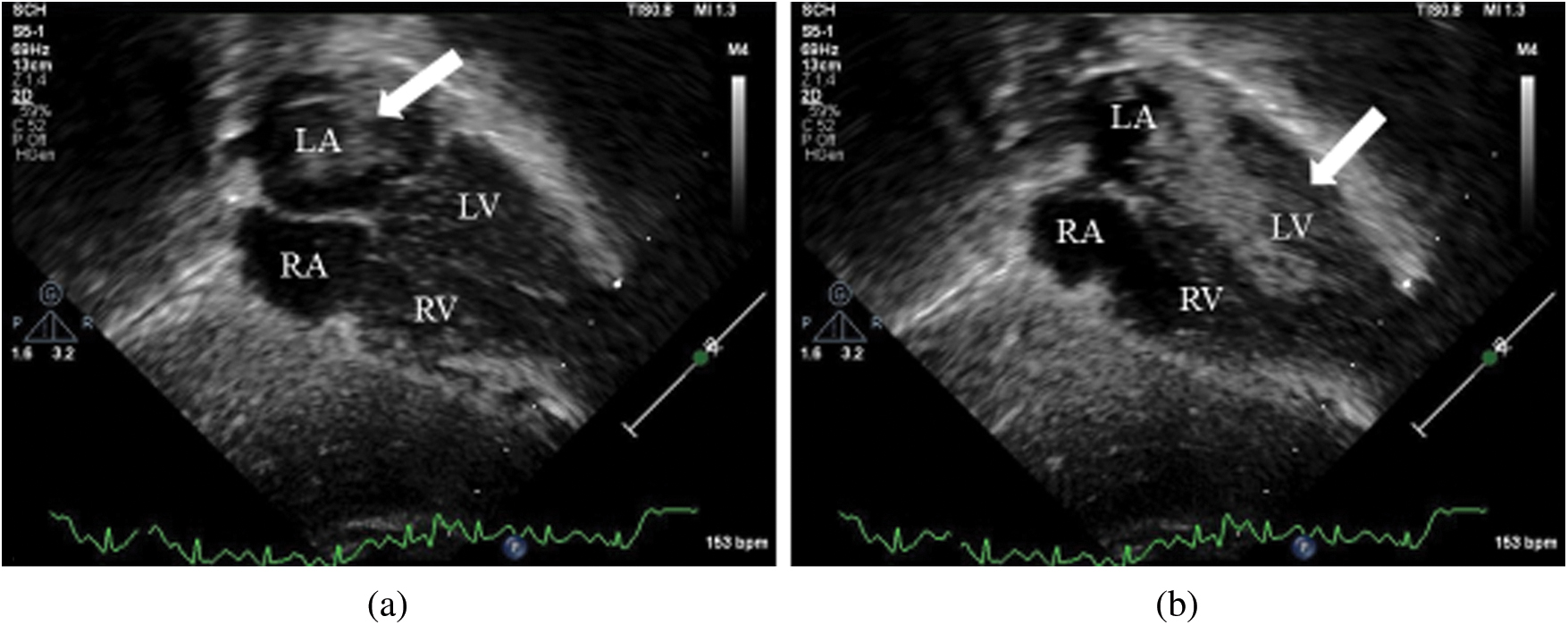
Figure 1: Subxiphoid views from contrast echocardiography with left arm injection site showing (a) contrast in the left atrium (arrow) and (b) contrast subsequently flowing between the left atrium and the left ventricle during diastole (arrow)
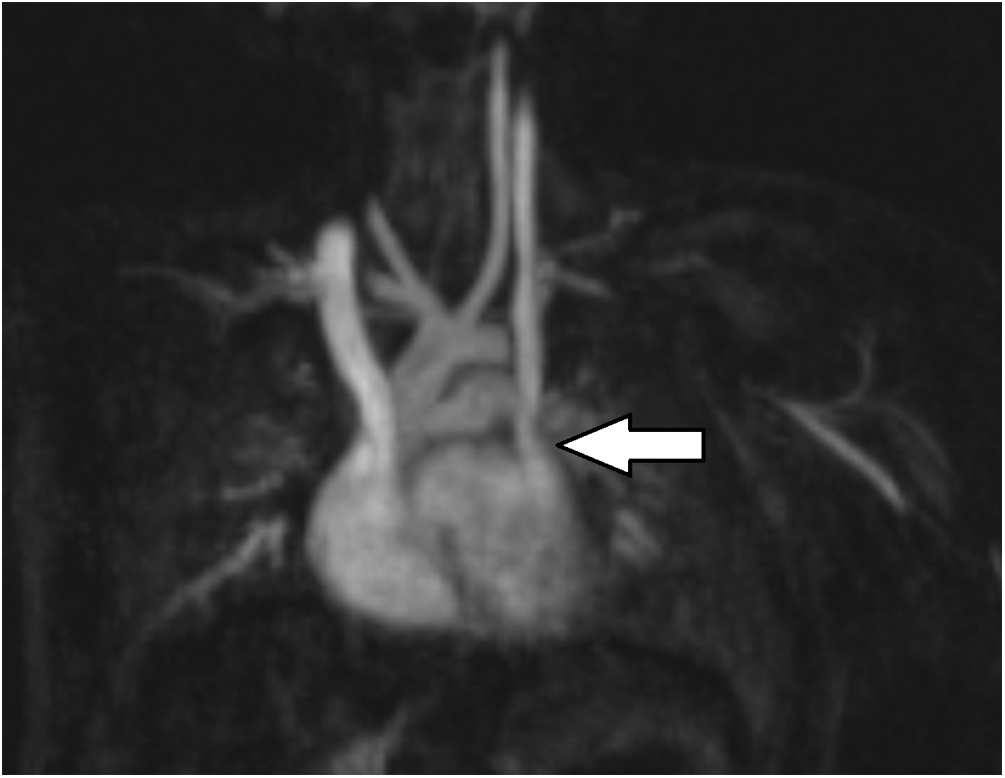
Figure 2: Oblique coronal maximum intensity projection image from a cardiac MR angiogram showing normal right SVC and a PLSVC draining to the left atrium (arrow)
The patient subsequently underwent cardiac catheterization. Angiography confirmed earlier imaging findings (Fig. 3), and the PLSVC was successfully occluded with a 10 mm Amplatzer Vascular Plug II distal to the bridging vein (Fig. 4). Following the procedure, the patient’s positional hypoxemic episodes resolved. The patient has weaned off mechanical ventilation during the day, and is currently weaning from respiratory support during sleep.
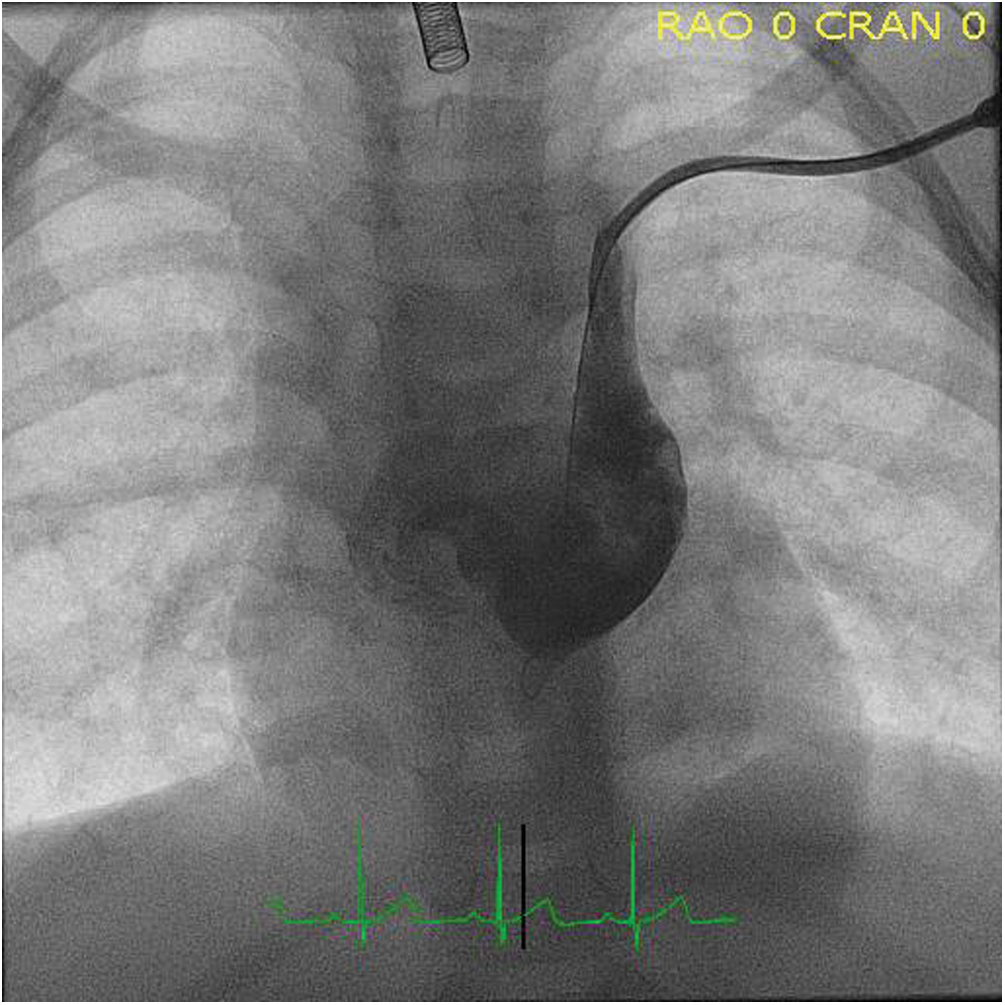
Figure 3: Angiography with contrast injection in the PLSVC demonstrating drainage into the left atrium
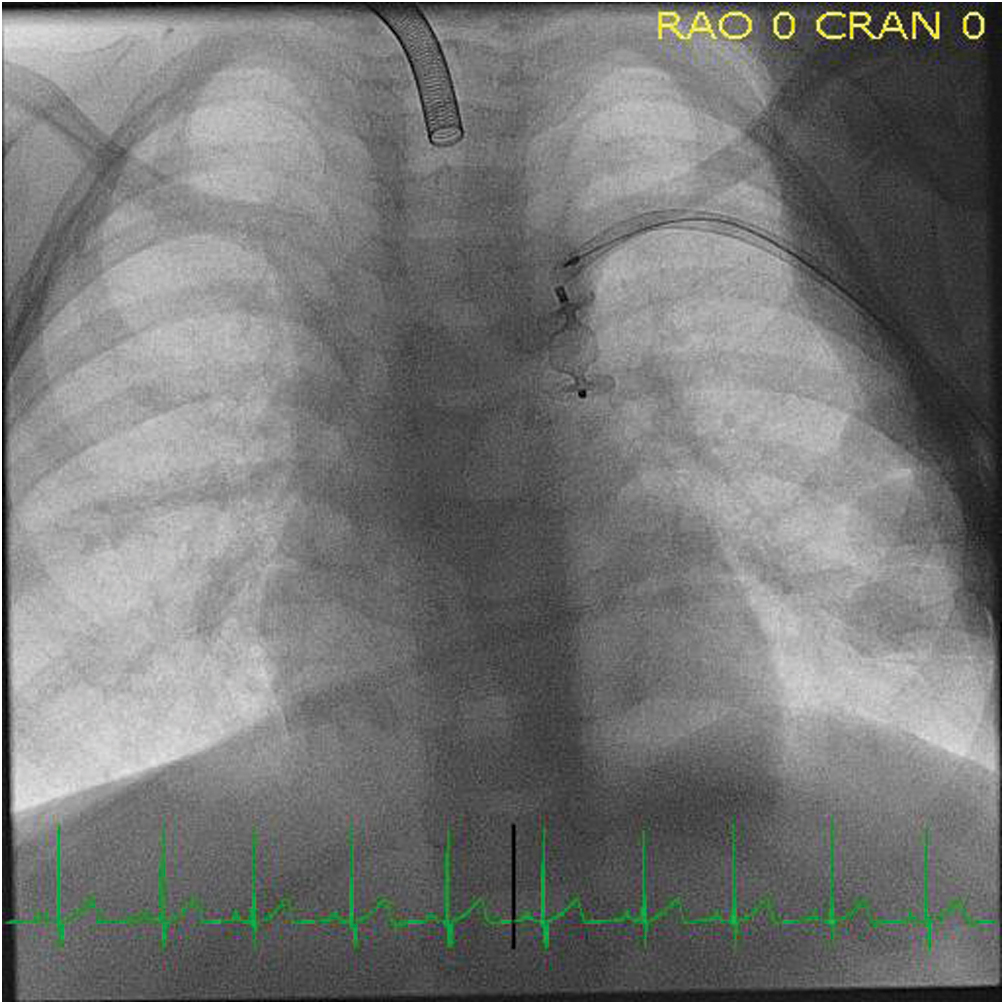
Figure 4: Fluoroscopic image during cardiac catheterization confirming correct placement of vascular plug in the PLSVC
This case presents a patient with position-dependent right-to-left shunt physiology from a PLSVC draining directly to the left atrium, a previously unreported presentation of this common venous anomaly. The case extends available reports of PLSVC to left atrial connections, emphasizing the importance of injection site in contrast echocardiography while assessing the broad differential of hypoxemia.
PLSVC has an estimated prevalence of 0.3%–0.5% in the general population and up to 10% in patients with congenital heart abnormalities [1–3]. An estimated 40% of patients with PLSVC have concurrent congenital heart disease, most commonly atrial septal defects [4,5].
PLSVC results from persistence of the left cardinal vein in embryogenesis. The vast majority (up to 90%) of PLSVC drain into the coronary sinus without hemodynamic consequence [6]. In these cases, the anomaly is typically incidentally discovered and considered a normal venous variant. Even when hemodynamically insignificant, a PLSVC draining to the coronary sinus can complicate central venous catheter placement, pacemaker or cardiac device implantation, and retrograde cardioplegia. Conversely, in a minority of cases, a PLSVC drains into the left atrium, resulting in a right-to-left shunt that can lead to hypoxemia or paradoxical embolism [7–9]. This hypoxemia can present from birth or infancy and is often worse with exertion. The degree of hypoxemia depends on the presence and size of an innominate bridging vein. In this case, the hypoxemia was exacerbated by position-dependent venous flow with a small bridging vein.
Contrast echocardiogram with right arm injection was performed during the initial hospitalization to evaluate this patient’s intermittent hypoxemic episodes, with no right-to-left shunt identified. When injection occurs in the right arm, a contrast echocardiogram can identify intracardiac and intrapulmonary shunts. However, in order to identify shunting from a PLSVC to the left atrium, contrast must be injected in the left arm. Left arm injection on the initial contrast echocardiogram would have allowed for earlier shunt identification and intervention, and may have impacted the patient’s ventilator wean progression.
Finally, this case serves as a reminder of the broad differential for hypoxemia and the importance of the history and physical exam to direct diagnostic evaluation. A careful history identified the symptom of head-position-dependent cyanosis. Subsequent clinical examination reproduced positional hypoxemia consistent with shunting physiology. For example, the hypoxemia did not improve with supplemental oxygen and was not associated with any changes in ventilation, an important distinction to make in a patient with severe underlying pulmonary disease. In addition to a venous anomaly such as a PLSVC, other relevant causes of positional right-to-left shunting to consider are pulmonary arteriovenous malformations and inter-atrial connections (e.g., patent foramen ovale) that may experience dynamic right-to-left shunting, as is the case in platypnea-orthodeoxia syndrome [10]. For this patient, a previous contrast echocardiogram had ruled out an intracardiac or intrapulmonary shunt. Finally, the dependence of the symptoms on head position suggested the hypoxemia was likely related to the head and neck vasculature.
PLSVC is a venous anomaly that, in the majority of cases, drains into the coronary sinus and is hemodynamically insignificant. However, when a PLSVC drains directly to the left atrium, it can result in right-to-left shunting leading to hypoxemia. This patient’s hypoxemic episodes were ultimately due to position-dependent right-to-left shunt through a PLSVC draining into the left atrium. The differential diagnoses for hypoxemia is broad; thus, a detailed history and physical is critical in directing diagnostic evaluation. The gold standard to identify such a shunt is contrast echocardiography with injection in the left arm, as right arm injection limits identification of shunting to the intracardiac and intrapulmonary level.
Funding Statement: The authors received no specific funding for this study.
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
1. Cha, E. M., Khoury, G. H. (1972). Persistent left superior vena cava: radiologic and clinical significance. Radiology, 103(2), 375–381. DOI 10.1148/103.2.375.
2. Geva, T. (2016). Abnormal systemic venous connections. Moss and Adams’ heart disease in infants, children, and adolescents, including the fetus and young adult. Philadelphia: Wolters Kluwer.
3. Huhta, J. C. (2011). Echocardiography and noninvasive diagnosis. Pediatric Critical Care. Philadelphia: Elsevier.
4. Sarodia, B. D., Stoller, J. K. (2000). Persistent left superior vena cava: case report and literature review. Respiratory Care, 45(4), 411–416.
5. Winter, F. (1954). Persistent left superior vena cava; survey of world literature and report of thirty additional cases. Angiology, 5(2), 90–132. DOI 10.1177/000331975400500207.
6. Goyal, S. K., Punnam, S. R., Verma, G., Ruberg, F. L. (2008). Persistent left superior vena cava: a case report and review of literature. Cardiovascular Ultrasound, 6(1), 50. DOI 10.1186/1476-7120-6-50.
7. Gupta, R., Pearson, A. (2013). Diagnosis of persistent left superior vena cava draining directly into the left atrium. North American Journal of Medical Sciences, 5(8), 496–497. DOI 10.4103/1947-2714.117328.
8. Thaiyananthan, N. N., Jacono, F. J.III, Patel, S. R., Kern, J. A., Stoller, J. K. (2009). Right-to-left anatomic shunt associated with a persistent left superior vena cava: the importance of injection site in demonstrating the shunt. Chest, 136(2), 617–620. DOI 10.1378/chest.08-2641.
9. Hutyra, M., Skala, T., Sanak, D., Novotny, J., Köcher, M. et al. (2010). Persistent left superior vena cava connected through the left upper pulmonary vein to the left atrium: an unusual pathway for paradoxical embolization and a rare cause of recurrent transient ischaemic attack. European Journal of Echocardiography, 11(9), E35.
10. Agrawal, A., Palkar, A., Talwar, A. (2017). The multiple dimensions of platypnea-orthodeoxia syndrome: a review. Respiratory Medicine, 129, 31–38. DOI 10.1016/j.rmed.2017.05.016.
 | This work is licensed under a Creative Commons Attribution 4.0 International License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. |