
 | Congenital Heart Disease |  |
DOI: 10.32604/CHD.2020.011671
ARTICLE
A Single Institution’s Experience with Later Extracardiac Fontan Procedure Off Bypass
1Division of Critical Care Medicine, Department of Pediatrics, University of Washington, Seattle Children’s Hospital, Seattle, 98105, USA
2Division of Pediatric Cardiology, UCSF Benioff Children’s Hospital Oakland, Oakland, 94609, USA
3Department of Cardiothoracic Surgery—Pediatric Cardiac Surgery, Stanford University, Stanford, 94305, USA
4Children’s Hospital Oakland Research Institute, Oakland, 94609, USA
5Division of Pediatric Critical Care Medicine, UCSF Benioff Children’s Hospital Oakland, Oakland, 94609, USA
*Corresponding Author: Carter Biewen. Email: carter.biewen@seattlechildrens.org
Received: 25 May 2020; Accepted: 11 August 2020
Abstract: Purpose: To summarize Fontan procedure data from our institution, UCSF Benioff Children’s Hospital Oakland, in order to better understand outcomes of our surgical and post-operative care. Basic Procedures: This is a retrospective cross-sectional chart review summarizing characteristics and outcomes of patients who underwent the Fontan procedure at our institution between 2005 and 2016. Main Findings: Sixty-five Fontan procedures were performed at our institution between 2005 and 2016, all of which were extracardiac Fontan procedures performed by the same surgical team. At the time of Fontan procedure, the mean patient age was 56.4 ± 18.7 months and mean weight was 16.6 ± 2.7 kg. There was no significant correlation appreciated between patient age/weight and outcomes. Six (9%) Fontan conduits were fenestrated. Thirty-eight (58%) Fontan procedures were performed off cardiopulmonary bypass. Fontan procedures performed off bypass and of shorter duration were associated with fewer days to extubation and pressor discontinuation post-operatively, as well as higher discharge SpO2. Two patients (3%) required Fontan conduit takedown during their post-operative ICU stays. The most common complications were pleural effusion, chylothorax, arrhythmia and infection. There was no early or late mortality. Principle Conclusions: Delayed extracardiac Fontan procedure off cardiopulmonary bypass appears to be a safe and effective approach. The strategy may provide benefit when considering certain outcomes, however more studies are needed to further elucidate these findings.
Keywords: Fontan; single ventricle; extracardiac; cardiopulmonary bypass
The Fontan operation, first described by Dr. Fontan in 1971, establishes pulmonary blood flow in hearts with single ventricle physiology [1], which comprise 9–12% of all congenital cardiac anomalies [2]. There is no consensus on ideal timing of the Fontan procedure; some institutions perform surgery earlier, often by age two to three years to avoid cyanosis, development of collaterals and valve dysfunction [3], while others wait for physiologic surgical indications such as low oxygen saturation or cyanosis to develop, typically around age three to five years [4]. A common approach has been to perform the procedure between eighteen months and six years with patients on cardiopulmonary bypass (CPB) [2]. While advances in CPB technique have made the procedure safer, there remain significant risks. Complications associated with CPB include an inflammatory response and capillary leak; fluid, electrolyte and acid-base imbalance; myocardial damage and dysfunction leading to low cardiac output and multiorgan dysfunction syndrome including acute kidney injury [5]. In many institutions, the extracardiac conduit has gained preference over the intra-atrial conduit, as it facilitates off-CPB Fontan procedures [3,6]. Additionally, early studies demonstrated that extracardiac conduits can lower risk of atrial arrhythmias and shorten ICU stays and time to extubation [7].
At our institution over the past 15 years, we have aimed to perform Fontan procedures using extracardiac conduits off CPB when patients are older and larger. We have found that patients generally tolerate this protocol well. We hypothesize that later (i.e., at a weight of 14.5 kg or greater) extracardiac Fontan procedure off bypass is associated with no need for fenestration, decreased pleural effusions, no need for re-intervention, fewer long-term complications and overall better outcomes. Here, we delve into and summarize patient data from Fontan procedures performed at our institution from 2005 to 2016.
In this IRB-approved retrospective cross-sectional case series, we reviewed the medical records of patients who underwent the Fontan procedure at our institution between 2005 and 2016. Patients were candidates for Fontan procedure without CPB as long as they did not require extensive operation on their central pulmonary artery, though limited pulmonary artery modifications can be performed off-CPB. We generally avoid combining the Fontan procedure with intracardiac work such as valve repair, which requires cross clamping. Our preference is to stage these cases. Details of the off-CPB procedure technique have been described previously [8]. The same surgical team performed Fontan procedures during this period, and post-operatively patients were hospitalized in the pediatric intensive care unit (PICU) at Children’s Hospital Oakland. Patients were identified using the cardiovascular surgical database records. Individual patient data was obtained from paper charts for records prior to 2012–2013, and from electronic medical records thereafter. A standardized data collection form was completed for each patient and included:
1. Patient characteristics: age, gender, weight, cardiac anatomy, NYHA class, factors associated with procedural risk (pre-operative mean PA pressure, ventricular end diastolic pressure, degree of PA stenosis or hypoplasia, type of single ventricle, and presence of moderate-severe AV valve insufficiency), presence of ventricular dysfunction, pre-operative hemoglobin and hematocrit, systemic blood oxygen saturation and any other comorbidities.
2. Fontan characteristics: prior stages of single ventricle palliation, type of Fontan conduit (e.g., extracardiac), conduit size, presence and duration of CPB, procedure duration, presence of fenestration.
3. Outcomes: mortality, length of hospital and PICU stays, time to extubation, time to discontinuation of inotropes, chest tube output, time to discontinuation of chest tubes, oxygen saturation at discharge, diuretics prescribed at the time of discharge, duration of diuretic therapy, presence and type of complication, presence and type of re-intervention.
Data analyses were performed using SAS version 9.4. The value of p = 0.05 was used as the cut-off for statistical significance. Descriptive statistics (frequency distributions or means and standard deviations, as appropriate) were computed for each independent variable. We examined the data for associations and statistical significance across the above categories (patient characteristics, Fontan characteristics, outcomes). Correlations were assessed using Pearson correlation coefficients. Additionally, we performed comparisons between select groups, specifically comparing outcomes for groups of patients based on presence of CPB, weight (<14.5 kg vs. ≥14.5 kg), and age (<5 years vs. ≥5 years). Null hypotheses were tested using Student’s t-test for continuous outcomes and Fisher’s exact test for categorical data. Data reported includes all 65 Fontan operations, and two patients who underwent Fontan conduit takedown on post-operative day 2 and post-operative day 5.
Between 2005 and 2016, there were 65 Fontan procedures performed on 64 patients (one female patient had repeat Fontan procedure after takedown). There were 37 male and 27 female patients. At time of Fontan procedure, the mean patient age was 56.4 ± 18.7 months (range 15–138) and mean weight was 16.6 ± 2.7 kg (range 10–25). Mean pre-operative pulmonary artery pressure was 10.6 ± 1.6 mmHg. Mean ventricular end diastolic pressure was 7.8 ± 2.0 mmHg. Mean pre-operative hemoglobin was 16.4 ± 1.9 g/dL and mean blood oxygen saturation was 84.2 ± 4.4%. Patient characteristics of the on- and off-bypass groups are displayed in Tab. 1.
Table 1: Patient characteristics

Cardiac anatomy categories included unbalanced AV canal (n = 20), tricuspid atresia (n = 14), double inlet left ventricle (n = 9), hypoplastic left heart (n = 8), double outlet right ventricle (n = 6), pulmonary atresia with intact ventricular septum (n = 5), and double inlet right ventricle (n = 2). Heterotaxy was present in 18 patients. All patients had previously undergone a bidirectional Glenn procedure with the exception of one who instead underwent a Kawashima-type staging procedure.
All Fontan procedures utilized extracardiac conduits. The mean total procedure duration was 229.2 ± 67.6 min. Fifty-eight percent (n = 38) of Fontan procedures were performed off CPB; patient cardiac diagnoses in this group are displayed in Tab. 2. For procedures performed on CPB, the mean bypass time was 40.1 ± 30.7 min with a range of 4 to 121 min. Median conduit size was 20 mm and ranged from 16 to 22 mm (16 mm in three patients, 18 mm in 19 patients, 20 mm in 40 patients, 22 mm in three patients). Six patients (9%) underwent fenestration of their Fontan conduit; five out of six patients with fenestrations were placed on CPB at some point during their procedure. Two patients (3%) required Fontan conduit takedown in the days following the procedure (post-operative days two and five). Procedure characteristics of the on- and off-bypass groups are displayed in Tab. 3.
Table 2: Cardiac diagnoses, off-CPB group

Table 3: Procedure characteristics. Interquartile ranges provided in parentheses

There has been no known early or late mortality during follow-up (range 2–13 years post-operatively). The mean PICU duration of stay was 14.7 ± 9.7 days, and the mean total hospital duration of stay was 15.9 ± 11.8 days. No patient or procedure characteristics including age, weight and conduit size were found to correlate with duration of ICU or hospital stay. Seventy-seven percent (n = 50) of patients were extubated on post-operative day zero and eighteen percent (n = 12) were extubated on post-operative day one. On average, vasopressors were discontinued on post-operative day 2.6 ± 1.8, and chest tubes were discontinued on post-operative day 9.4 ± 5.7. Mean blood oxygen saturation at the time of discharge was 93.7 ± 7.3%. Median duration that patients remained on diuretic therapy post-operatively was 126 days. Twenty-eight patients (44%) have required re-admission; this includes admissions for Fontan-related procedures including chest tube placement for pleural effusions. Seventeen patients (27%) have required re-intervention, which we defined as Fontan-related open or catheterization procedures including fenestration closures. Five patients have been lost to follow-up.
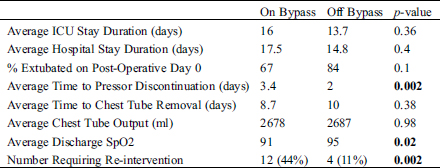
3.3.1 Fontan Procedure Off Cardiopulmonary Bypass
When comparing patients that underwent Fontan procedure off CPB (n = 38) with those who were placed on CPB, there was no difference in mean duration of stay in the ICU (13.7 vs. 16 days, p = 0.36) or hospital (14.8 vs. 17.5 days, p = 0.4). Furthermore, there was no significant difference in days to chest tube removal between patients off and on CPB (10 ± 7.8 vs. 8.7 ± 7.1, p = 0.38).
The off-CPB group, however, did seem to have improved outcomes in other areas. Patients who underwent Fontan procedure off CPB were extubated sooner than those who went on CPB (post-operative day 0.16 vs. 0.74, p = 0.03). Additionally, on average vasopressors were discontinued sooner in off-CPB patients (post-operative day 2 ± 1.5 vs. post-operative day 3.4 ± 2.6, p = 0.002). Following Fontan procedure, off-CPB patients had higher discharge SpO2 when compared to the on-CPB cohort (95 vs. 91%, p = 0.02), while pre-Fontan SpO2 was similar between groups (84.4 vs. 84%). Few patients in both groups had pulmonary AVMs.
Only four (11%) of the 38 patients who underwent Fontan procedure off bypass required re-intervention. One of these patients had their fenestration closed, one underwent elective ballooning of PA stenosis, one required Fontan conduit takedown and one underwent left hepatic vein closure and heart transplant. Twelve (44%) of the 27 patients who underwent Fontan procedure on bypass required re-intervention. Re-interventions in this group included fenestration closure (n = 5), lymphatics embolization (n = 2), debridement and rewiring of sternotomy site, epicardial pacemaker placement (n = 2), coil occlusion of persistent left superior vena cava, and Fontan conduit takedown. While the sample size is small, this increased frequency of re-intervention in the on-CPB group appears to be statistically significant (p = 0.002). Post-operative comparisons of the on- and off-bypass groups are displayed in Tab. 4.
Table 4: Post-operative comparison
At our institution, the standard weight goal for patients at time of Fontan procedure is 14.5 kg. In this analysis, there were seven patients (11%) who weighed less than 14.5 kg at the time of Fontan procedure. Their weights ranged from 10 to 14 kg. These patients overall had lower pre-operative SpO2 (80.9 ± 8.4% vs. 84.7 ± 3.6%, p = 0.03), and three had documented AVMs, likely contributing to the decision to proceed with earlier Fontan procedures. These smaller patients were no more likely to have the procedure performed on CPB; however the three patients who did remained on CPB for longer than their heavier counterparts (81 ± 43 min vs. 35 ± 26 min, p = 0.01). The prolonged CPB time in this group does not appear to be due to extra procedures, as only one of these three patients underwent additional procedure of LPA augmentation at the time of Fontan procedure. Interpretation of these results is clearly limited by the small sample size. When not limited by patient size and anatomy, the surgical team attempted to place a 20 mm conduit, which is believed to be a reasonably sized vessel for an adult. As expected, there was a positive correlation between patient weight and Fontan conduit size (r = 0.28, p = 0.02). Accordingly, a smaller Fontan conduit was used in the group of patients weighing less than 14.5 kg (18.3 ± 1.8 mm vs. 19.4 ± 1.2 mm, p = 0.023). There was no significant difference between weight groups in duration of hospitalization and PICU stay, post-operative days intubated, days on vasopressors, days with chest tubes or chest tube output.
We compared characteristics and outcomes of patients less than five years old at time of surgery with patients five years or older. Twenty-three (35%) patients were at least five years old at the time of Fontan procedure. There was no significant difference between age groups in duration of hospitalization and PICU stay, post-operative days intubated, days on vasopressors, days with chest tubes or chest tube output. Generally, age in years was positively correlated with post-operative days on vasopressors (r = 0.26, p = 0.037), however the association was only borderline significant (p = 0.055) when the more precise age in months was used.
Procedure duration seemed to have significant implications in a few outcome areas. Shorter procedure was correlated with shorter time to extubation (r = 0.58, p ≤ 0.0001), shorter time on vasopressors (r = 0.39, p = 0.0014), less chest tube output (r = 0.35, p = 0.004), and higher discharge blood oxygen saturation (r = –0.41, p = 0.0007). On the other hand, a higher pre-operative pulmonary artery pressure was correlated with a longer Fontan procedure (r = 0.30, p = 0.016) and longer time on vasopressors (r = 0.31, p = 0.012).
The most common complications were pleural effusions and chylothorax, which required repeat hospital admission in 21 patients (33%). Frequency of readmission with effusions was not associated with Fontan procedure being performed on- or off-CPB. Two patients (3%) underwent lymphatic embolization for ongoing lymphatic leaks; one patient had plastic bronchitis and the other had heterotaxy and chylous ascites secondary to complications of gastrostomy tube placement in the setting of prior Fontan procedure.
Arrhythmias occurred both intra- and post-operatively. Arrhythmias in the intra-operative and immediate post-operative period were mostly narrow-complex and included unspecified supraventricular tachycardia, ectopic atrial tachycardia, junctional ectopic tachycardia, and orthodromic re-entrant tachycardia. One patient required defibrillation for ventricular tachycardia. Nine patients (14%) were managed with single or combination therapies including cardioversion, defibrillation, pacing, and anti-arrhythmic medications. Two patients went on to develop sinus node dysfunction and two patients developed 2nd degree heart block. Two of these patients required epicardial pacemaker placement. One has an automatic implantable cardioverter-defibrillator. Another, due to heart failure, was bridged with a ventricular assist device and underwent successful heart transplant four years following Fontan procedure.
Eight patients (12.5%) were treated for hospital-acquired infections, including five (8%) who were diagnosed with mediastinitis. Two patients (3%) have been diagnosed with protein-losing enteropathy.
The Fontan procedure is ever-evolving as we strive to optimize patient outcomes. Here in this retrospective cross-sectional study, we have summarized characteristics and outcomes of children who underwent extracardiac Fontan procedure at a single institution from 2005 to 2016. We hypothesize that later extracardiac Fontan procedure off CPB is associated with decreased need for fenestration and re-intervention, decreased pleural effusions, fewer long-term complications and overall better outcomes. A strength of this review is consistency in surgical technique as all Fontan procedures were extracardiac and performed by the same surgical team.
We aim to perform Fontan procedures when patients are older and larger. The mean age and weight of our patients at time of surgery were 56.4 months and 16.6 kg. This approach is supported by the idea that matching conduit size with vascular structure size reduces the need for reoperation and conduit upsizing [9]. Our study did not reveal any disadvantage to performing Fontan procedures after age 5 years or at weight above 14.5 kg in asymptomatic patients, though symptomatic patients may benefit from earlier Fontan procedure. At this point in our analysis 2–13 years post-Fontan procedures, no known patients have required upsizing of their conduits, however longer follow-up is needed to see if this trend continues.
We hypothesize that extracardiac Fontan procedure off CPB decreases the need for repeat procedural intervention by reducing risk of myocardial damage and dysfunction. While unclear if the finding is statistically significant, in our study patients who underwent surgery off CPB had a lower rate of repeat interventions. It is difficult to attribute this finding to CPB status, however, as there are many potential confounding variables. For example, it is possible that the on-bypass group had more complex cardiac anatomy or intra-operative complications, thus putting them at higher baseline risk. Regardless, it appears that extracardiac Fontan procedures can safely be performed off CPB.
An Indian study of older children (mean age 15 years at time of surgery) found no need for post-operative vasopressors in the setting of extracardiac Fontan procedure off CPB [2]. At our institution, while all patients were on vasopressors post-operatively, there do appear to be benefits in performing Fontan procedures off CPB and with shorter procedure duration; patients demonstrated shorter times to extubation and pressor discontinuation, and were discharged with a higher SpO2. Interpretation of discharge SpO2 is challenging given that a higher proportion of patients in the on-CPB group underwent fenestration compared with the off-CPB group (19% vs. 3%). Further potential benefits to performing the Fontan procedure off CPB include avoiding exposure to packed red blood cells [6], and reduced pleural and peritoneal effusions [10]. We did not assess blood product exposure and our patients on and off CPB did not have a significant difference in effusions.
The decision to perform fenestration varies by institution. Some institutions perform fenestration regularly in as many as 90% of patients undergoing Fontan procedures [11], and this is supported by early studies demonstrating improved outcomes [12]. Other institutions perform fenestration only when necessary in high-risk patients as it comes with additional risks, decreased systemic SpO2 and requires another procedure to close the fenestration [13]. At our institution, we aim to avoid fenestration when possible during the extracardiac Fontan procedure. Of our patients, six (9%) required fenestration for elevated Fontan conduit pressures, all of whom have subsequently undergone successful fenestration closure. We did not draw conclusions about characteristics contributing to and outcomes resulting from fenestration.
Pleural effusions and chylothorax were the most common complication in our patient population. We hypothesize based on prior studies [10] that our off-CPB Fontan strategy promotes decreased pleural fluid accumulation. In fact, we observed no apparent benefit in regards to chest tube output or time to chest tube discontinuation in patients who underwent Fontan procedure off CPB or at older age/greater weight. While we did not formally compare our chest tube output data to other institutions’, our mean time to chest tube discontinuation of nine days fell within the range of means (4–11 days) from several other studies [6,7,11–14].
Because extracardiac Fontan technique does not involve an atrial incision, many institutions favor this method in order to decrease atrial inflammation, fibrosis and arrhythmias. The arrhythmia benefit however has not been supported by multiple recent studies, with extracardiac Fontan procedures even being noted to have higher rates of early post-operative bradyarrhythmias [15,16]. Correspondingly, arrhythmias remained a significant complication in our patient population despite all procedures being extracardiac. The explanations for this remains elusive, but concomitant heterotaxy or affected sinus node blood supply have been proposed as possible etiologies [17]. While there remain other potential benefits to off-CPB Fontan procedures as discussed above, arrhythmia prevention may not be one of them.
While there is a theoretical higher risk of thrombosis in extracardiac conduits compared with intra-atrial procedures, multiple studies have found no difference in rates of thrombosis or thromboembolism [18,19]. Thrombotic risk in our patient-population seemed to be low, though not insignificant, with three patients experiencing thrombotic events; one patient had a right internal jugular vein thrombus, one patient had a hepatic vein thrombus, and another experienced a left middle cerebral artery thrombotic stroke six months after surgery. There were no other reported thromboembolic events.
Previous studies have demonstrated improved mortality rates after extracardiac Fontan procedure compared with other types of Fontan procedures [20]. Of our patients, all of whom received extracardiac Fontan conduits, there has been no mortality during 2–13 years of follow-up.
First and foremost, this retrospective study simply summarizes our data. It does not thoroughly compare our approach and outcomes with those of other institutions. This study is inherently limited by its retrospective nature. While we performed analyses between groups within our patient population based on single variables (e.g., age, size, presence of CPB), findings are limited by our inability to control for other factors. Despite the same surgical and ICU teams caring for all patients, there was not a standardized care plan. There were no exclusion criteria, and not surprisingly many patients in our patient population had significant co-morbidities such as pulmonary hypertension, arrhythmias, pacemakers, pulmonary AVMs, and history of cardiac arrest requiring ECMO (one patient).
Our institution’s current approach of delaying extracardiac Fontan procedures in asymptomatic patients and performing them off CPB appears to be safe and effective. Furthermore, Fontan procedures performed off CPB may provide benefit in terms of time to extubation, pressor discontinuation and post-operative SpO2. As outcomes continue to improve following the Fontan procedure, ongoing surveillance is necessary to assess outcomes. In this manner, we can continue to modify our approach and strive to optimize patient survival and quality of life.
Author Contributions: CB was involved in project design; IRB approval application; data collection, analysis and interpretation; drafting, critical revision and approval of article. HP was involved in project concept and design, data collection and interpretation, critical revision and approval of article. OR was involved in data collection and interpretation, critical revision and approval of article. GG was involved in statistical data analysis and interpretation, critical revision and approval of article. NC was involved in project concept and design, data collection and interpretation, critical revision and approval of article.
Data Sharing: The authors do not intend to share data beyond this manuscript.
Funding Statement: The authors received no specific funding for this study.
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
1. Fontan, F., Baudet, E. (1971). Surgical repair of tricuspid atresia. Thorax, 26(3), 240–248. DOI 10.1136/thx.26.3.240.
2. Talwar, S., Singh, S., Sreenivas, V., Singh Kapoor, K., Kumar Gupta, S. et al. (2017). Outcomes of patients undergoing primary Fontan operation beyond first decade of life. World Journal for Pediatric and Congenital Heart Surgery, 8(4), 487–494. DOI 10.1177/2150135117713696.
3. Malec, E., Schmidt, C., Lehner, A., Januszewska, K. (2017). Results of the Fontan operation with no early mortality in 248 consecutive patients. Kardiologia Polska, 75(3), 255–260.
4. Feinstein, J., Woodrow Benson, D., Dubin, A., Cohen, M., Maxey, D. et al. (2012). Hypoplastic left heart syndrome: current considerations and expectations. Journal of the American College of Cardiology, 59(1), S1–S42. DOI 10.1016/j.jacc.2011.09.022.
5. Rajasekaran, S., Ring, J. C. (2012). Post-operative cardiac care, pediatric critical care study guide, pp, 607–642. London: Springer.
6. Mainwaring, R. D., Reddy, V. M., Hanley, F. L. (2014). Completion of the three-stage Fontan pathway without cardiopulmonary bypass. World Journal for Pediatric and Congenital Heart Surgery, 5(3), 427–433. DOI 10.1177/2150135114536908.
7. Azakie, A., McCrindle, B. W., Van Arsdell, G., Benson, L. N., Coles, J. et al. (2001). Extracardiac conduit versus lateral tunnel cavopulmonary connections at a single institution: impact on outcomes. Journal of Thoracic and Cardiovascular Surgery, 122(6), 1219–1228. DOI 10.1067/mtc.2001.116947.
8. McElhinney, D. B., Petrossian, E., Reddy, V. M., Hanley, F. L. (1998). Extracardiac conduit Fontan procedure without cardiopulmonary bypass. Annals of Thoracic Surgery, 66(5), 1826–1828. DOI 10.1016/S0003-4975(98)00928-X.
9. Iyengar, A. J., Winlaw, D. S., Galati, J. C., Celermajer, D. S., Wheaton, G. R. et al. (2014). Trends in Fontan surgery and risk factors for early adverse outcomes after Fontan surgery: the Australia and New Zealand Fontan registry experience. Journal of Thoracic and Cardiovascular Surgery, 148(2), 566–575. DOI 10.1016/j.jtcvs.2013.09.074.
10. Shikata, F., Yagihara, T., Kagisaki, K., Hagino, I., Shiraishi, S. et al. (2007). Does the off-pump Fontan procedure ameliorate the volume and duration of pleural and peritoneal effusions?. European Journal of Cardio-Thoracic Surgery: Official Journal of the European Association for Cardio-Thoracic Surgery, 34(3), 570–575. DOI 10.1016/j.ejcts.2008.04.053.
11. Rogers, L. S., Glatz, A. C., Ravishankar, C., Spray, T. L., Nicolson, S. C. et al. (2012). 18 years of the Fontan operation at a single institution: results from 771 consecutive patients. Journal of the American College of Cardiology, 60(11), 1018–1025. DOI 10.1016/j.jacc.2012.05.010.
12. Lemler, M. S., Scott, W. A., Leonard, S. R., Stromberg, D., Ramaciotti, C. (2002). Fenestration improves clinical outcome of the Fontan procedure: a prospective, randomized study. Circulation, 105(2), 207–212. DOI 10.1161/hc0202.102237.
13. Fan, F., Liu, Z., Li, S., Yi, T., Yan, J. et al. (2017). Effect of fenestration on early postoperative outcome in extracardiac Fontan patients with different risk levels. Pediatric Cardiology, 38(4), 643–649. DOI 10.1007/s00246-016-1561-x.
14. Ovroutski, S., Sohn, C., Miera, O., Peters, B., Alexi-Meskishvili, V. et al. (2012). Improved early postoperative outcome for extracardiac Fontan operation without cardiopulmonary bypass: a single-centre experience. European Journal of Cardio-Thoracic Surgery: Official Journal of the European Association for Cardio-Thoracic Surgery, 43(5), 952–957. DOI 10.1093/ejcts/ezs535.
15. Balaji, S., Daga, A., Bradley, D. J., Etheridge, S. P., Law, I. H. et al. (2014). An international multicenter study comparing arrhythmia prevalence between the intracardiac lateral tunnel and the extracardiac conduit type of Fontan operations. Journal of Thoracic and Cardiovascular Surgery, 148(2), 576–581. DOI 10.1016/j.jtcvs.2013.08.070.
16. Stephenson, E. A., Lu, M., Berul, C. I., Etheridge, S. P., Idriss, S. F. et al. (2010). Arrhythmias in a contemporary Fontan cohort: prevalence and clinical associations in a multicenter cross-sectional study. Journal of the American College of Cardiology, 56(11), 890–896. DOI 10.1016/j.jacc.2010.03.079.
17. Rajanbabu, B. B. (2015). Arrhythmia prevalence after extra cardiac conduit Fontan: a viewpoint. Journal of Thoracic and Cardiovascular Surgery, 149(4), 1223–1224. DOI 10.1016/j.jtcvs.2014.08.013.
18. Firdouse, M., Agarwal, A., Chan, A. K., Mondal, T. (2014). Thrombosis and thromboembolic complications in Fontan patients: a literature review. Clinical and Applied Thrombosis/Hemostasis: Official Journal of the International Academy of Clinical and Applied Thrombosis/Hemostasis, 20(5), 484–492. DOI 10.1177/1076029613520464.
19. Robbers-Visser, D., Miedema, M., Nijveld, A., Boersma, E., Bogers, A. J. et al. (2010). Results of staged total cavopulmonary connection for functionally univentricular hearts; comparison of intra-atrial lateral tunnel and extracardiac conduit. European Journal of Cardio-Thoracic Surgery: Official Journal of the European Association for Cardio-Thoracic Surgery, 37(4), 934–941. DOI 10.1016/j.ejcts.2009.10.016.
20. Pundi, K. N., Johnson, J. N., Dearani, J. A., Pundi, K. N., Li, Z. et al. (2015). 40-year follow-up after the Fontan operation: long-term outcomes of 1,052 patients. Journal of the American College of Cardiology, 66(15), 1700–1710. DOI 10.1016/j.jacc.2015.07.065.
 | This work is licensed under a Creative Commons Attribution 4.0 International License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. |