 Open Access
Open Access
ARTICLE
Placenta-derived mesenchymal stem cells attenuate secondary brain injury after controlled cortical impact in rats by inhibiting matrix metalloproteinases
1 Department of Neurosurgery, School of Clinical Medicine, Ningxia Medical University, Yinchuan, China
2 Key Laboratory of Ningxia Stem Cell and Regenerative Medicine, General Hospital of Ningxia Medical University, Yinchuan, China
3 Department of Neurosurgery, Xi’an International Medical Center Hospital, Xi’an, China
* Corresponding Author: HECHUN XIA. Email:
BIOCELL 2024, 48(1), 149-162. https://doi.org/10.32604/biocell.2023.042367
Received 27 May 2023; Accepted 03 November 2023; Issue published 30 January 2024
Abstract
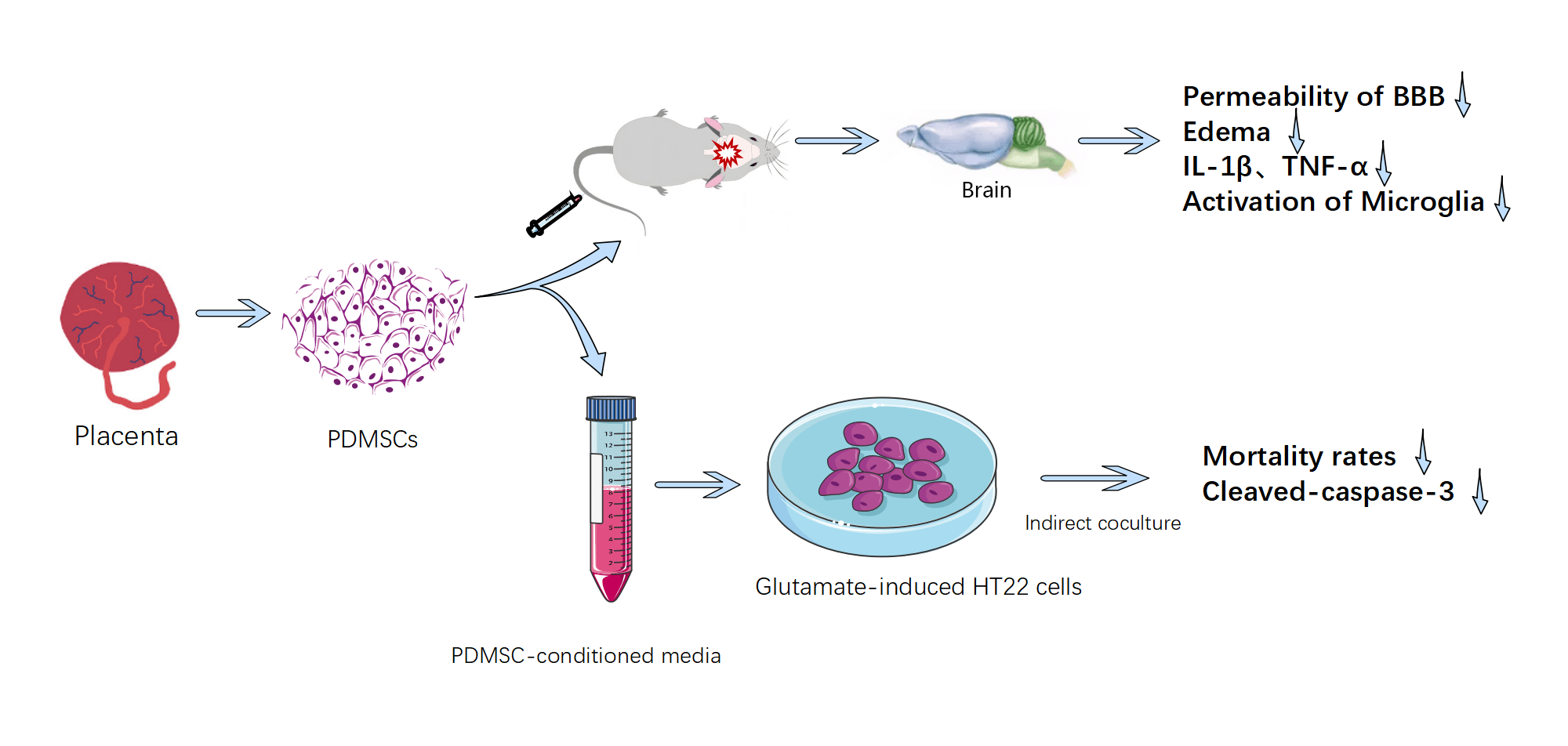
Background: As a form of biological therapy, placenta-derived mesenchymal stem cells (PDMSCs) exhibit considerable promise in addressing the complex pathological processes of traumaticbrain injury (TBI) due to their multi-target and multi-pathway mode of action. Material & Methods: This study investigates the protective mechanisms and benefits of PDMSCs in mitigating the effects of controlled cortical impact (CCI) in rats and glutamate-induced oxidative stress injury in HT22 cells in vitro. Our primary objective is to provide evidence supporting the clinical application of PDMSCs. Results: In the in vivo arm of our investigation, we observed a swift elevation of matrix metalloproteinase-9 (MMP-9) in the proximal cortex of injured brain tissues after CCI. PDMSCs, distinguished by their heightened expression of metalloproteinase tissue inhibitors-1 and -2 (TIMP-1 and TIMP-2): were intravenously administered via the caudal vein. This intervention yielded significant reductions in the permeability of the blood-brain barrier (BBB): the extent of brain edema, the levels of inflammatory cytokines IL-1β and TNF-α in damaged brain tissue, and the activation status of microglia in CCI-afflicted rats. In the realm of in vitro experiments, PDMSC-conditioned media demonstrated substantial reductions in mortality rates and cleaved caspase-3 levels in glutamate-induced HT22 cells compared with conventional media. Notably, this advantage was negated upon the introduction of neutralizing antibodies targeting TIMP-1 and TIMP-2. Conclusion: Collectively, our findings underscore the potential of PDMSCs in alleviating oxidative stress injury and secondary brain injury in the pathological process of TBI.Graphic Abstract
Keywords
Cite This Article
 Copyright © 2024 The Author(s). Published by Tech Science Press.
Copyright © 2024 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools