 Open Access
Open Access
REVIEW
Indian medicinal plants are effective in the treatment and management of COVID-19
1 Department of Pharmaceutical Chemistry, SGRR University, Uttarakhand, 248001, India
2 Department of Pharmaceutical Chemistry, HNB Garhwal University, Srinagar, 246174, India
3 Department of Veterinary Pharmacology & Toxicology, College of Veterinary Science and Animal Husbandry, Bhubaneswar, 751003, India
4 CECAPE—College of Dentistry, Juazeiro do Norte, 63050-203, Brazil
5 Department of Biological Chemistry, Regional University of Cariri, Crato, 63105-000, Brazil
6 Department of Biomedical, Surgical and Dental Sciences, Università degli Studi di Milano, Milan, 20133, Italy
7 National Interuniversity Consortium of Materials Science and Technology, Florence, 50121, Italy
* Corresponding Authors: MARCELLO IRITI. Email: ; HENRIQUE DOUGLAS MELO-COUTINHO. Email:
BIOCELL 2023, 47(4), 677-695. https://doi.org/10.32604/biocell.2023.026081
Received 15 August 2022; Accepted 23 November 2022; Issue published 08 March 2023
Abstract
Indian medicinal plants are referred to as the “nectar of life” owing to their phytochemicals and bioactive complexes that are beneficial in treating diseases. Coronavirus disease 2019 (COVID-19) is a global health issue without any proper medication. The indigenous plants of India can be exploited to control the precise signs of SARS-CoV-2. The Ministry of AYUSH (Ayurveda, Yoga and Naturopathy, Unani, Siddha, and Homeopathy) has advised routine usage of medicinal plants for COVID-19. Medicinal plants like Zingiber officinalis, Azadirachta indica, Ocimum sanctum, Nigella sativa, Withania somnifera, Curcuma longa, Piper nigrum, Allium sativum, Tinospora cordifolia, etc. have immunity-boosting, antiviral, antibacterial, antioxidant and anti-inflammatory actions that can suppress and treat symptoms of COVID-19. In vitro, in vivo as well as in silico validation, these phytochemicals can help us to manage and treat COVID-19 disease. This integration of traditional knowledge in the prophylaxis of corona infection and current skills validating it for the development of precise and powerful therapeutic approaches will more efficiently resolve different clinical aspects of COVID-19. The review focuses on both traditional and emergent methods to prevent and treat COVID-19 with various Indian medicinal plants along with their phytochemicals.Keywords
The ancient system of Indian Medicines is one of the world’s oldest medicinal practices. Sushruta Samhita, Atharvaveda, Charak Samhita, and Rigveda are some of the ancient Indian writings that mention using medicinal plants to treat illnesses. Worldwide, different medicinal herbs and plants from India are used for their curative qualities. In India, there are roughly 16,000–17,000 flowering species, of which 6,000 have medicinal qualities. Approximately 80% of the world’s population’s medical needs are satisfied by herbal medicine. The acceptance of herbal drugs was aided by factors such as antimicrobial resistance, a lack of an efficient drug regimen, the unavailability of conventional drugs, etc. (Parasuraman et al., 2014). For centuries, Indians have used medicinal plants to treat wounds and inflammation. In the colonial era, Indian medicinal plants were also used to treat epidemic diseases like smallpox, cholera, and malaria, as well as illnesses like pneumonia, tuberculosis, diarrhea, malaria, and asthma. These conventional plants are still employed in the treatment of various conditions, including diabetes, piles, parasitic infections, skin disorders, neurological, gastrointestinal, and skeletal problems, viral infections, etc. (Prasathkumar et al., 2021).
There was a spike in research after the coronavirus disease 2019 (COVID-19) pandemic broke out in an effort to develop cures or medications for it. The current COVID-19 global pandemic triggered by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) might be controlled with the aid of Indian medicinal plants and their phytochemicals. Numerous Indian medicinal plants with powerful pharmacological properties can be repurposed for COVID-19 therapy and prevention (Fig. 1, Suppl. Tables S1–S4). To understand the efficacy of these medicinal plants and their phytochemicals, studies are being done to establish their anti-inflammatory, immunomodulatory, and antiviral actions against Sars-CoV-2 symptoms. Concomitantly, many researchers tried molecular docking of phytochemicals to find in silico evidence for the use of traditional plants in the treatment and management of COVID-19 (Fuzimoto, 2021).
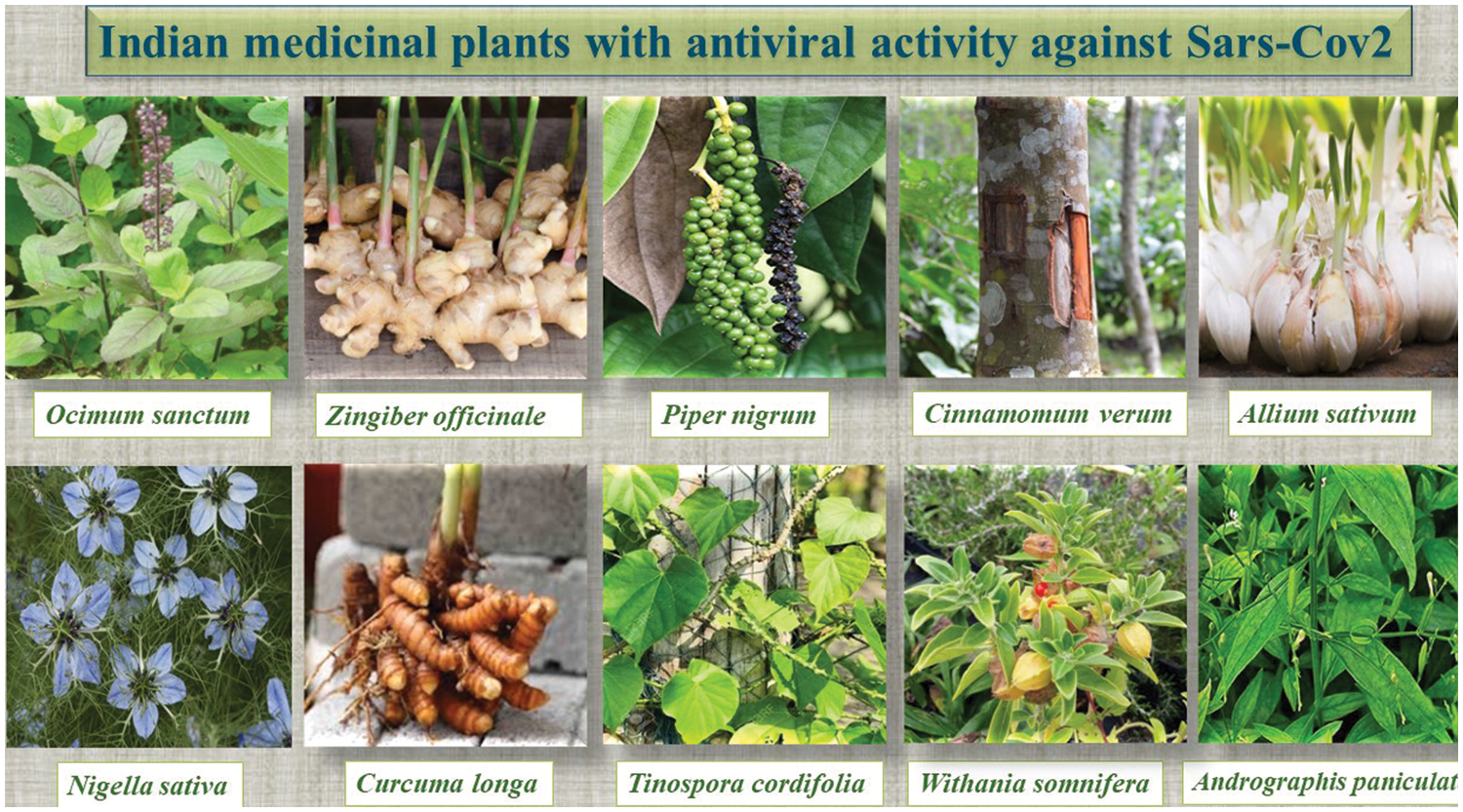
Figure 1: Some Indian Medicinal plants are effective against severe acute respiratory syndrome coronavirus 2.
A comprehensive understanding of plants and their phytochemicals effective in can SARS-CoV-2 lead to obtaining promising drug leads for COVID-19. The objective of this review is to understand the efficacy of Indian medicinal plants and their phytoconstituents in suppressing the symptoms of COVID-19. This review will help students and scientists to develop and discovers novel drugs effective in COVID-19 from conventional Indian medicinal plants.
Coronavirus disease 2019 (COVID-19)
Coronaviruses are composed of long RNA polymers bound by nucleocapsids. Coronavirus spreads via several routes, including aerosolized transmission, fecal-oral transmission, droplets, and surface transmission. COVID-19 affects multiple organs like the lungs, heart, etc. The symptoms of COVID-19 range from slight to severe respiratory distress with fever, cough, headache, sore throat, myalgia, headache, fatigue, and breath shortness. Infections can develop into respiratory failure, pneumonia, and also even death. Acute lung and renal injury and shock are common. This evolution is caused by inflammatory cytokines like granulocyte colony-stimulating factor, interferon γ-induced protein-10, macrophage Inflammatory Proteins1A, Monocyte chemoattractant protein-1, interleukin (IL)2, IL7, IL10, and tumor necrosis factor (TNF)-α (Chen et al., 2020). The angiotensin converting enzyme-2 (ACE-2) receptor in the nasal and oral mucosa allows the coronavirus ‘S’ protein to bind to host cells. The virus binds to ACE-2 receptor protein-positive organs. Other cytokines include IL-1B, IL-6, interferon (IFN)-α, IFN-γ, IL-18, IL-33, TNF-α, etc. Cell-mediated immunity becomes vigorous during this stage, and numerous proinflammatory cytokines are released (Abdulamir and Hafidh, 2020; Xu et al., 2020).
COVID-19 is diagnosed by identifying SARS-CoV-2 through PCR testing from nasopharyngeal swabs (Kumar, 2020a). As the virus and illness caused are not well-studied, no actual treatment is yet established for COVID-19. Only symptomatic treatment is possible in the absence of a specific treatment (Kesh and Palai, 2022). The use of anti-inflammatory medications (preferably non-steroids) for inflammatory conditions, anti-histamine medications for allergic conditions, paracetamol for high fevers, and antibiotics for secondary bacterial infections are required for symptomatic treatment. Improvements can be made by taking steps to lessen the specific symptoms of SARS-CoV-2, which include immunomodulation, homeostasis, and protecting the function of the heart, kidneys, and gastrointestinal system during inflammatory responses (Chen et al., 2022).
The Ministry of AYUSH (Ayurveda, Yoga and Naturopathy, Unani, Siddha, and Homeopathy) suggests various COVID-19 treatment modalities based on symptoms and stage. It suggests using basil, cinnamon, black pepper, raisins, and jaggery or lemon juice decoction to boost immunity. Turmeric in milk is also recommended. Some simple ayurvedic procedures recommended include nasal application of sesame oil/coconut oil and swill in the mouth as oil-pulling therapy. Steam inhalation of fresh mint leaves or caraway seeds is recommended during a dry cough or sore throat. Cough/throat irritation can also be relieved by combining clove with natural sugar or honey (Radhika and Malik, 2021). For asymptomatic COVID, Ayush 64, Kabasura Kudineer, and Ayush Kwath are prescribed; for symptomatic COVID-19, Ayush 64, Kabasura Kudineer, and Ayush Kwath are prescribed. Sudharsan Ghanvati can help with severe fever and body aches. Vyosadi Vati can help with coughs, common colds, and sore throats (Singh et al., 2021).
It is a poly-herbal formulation established by CCRAS, Ministry of AYUSH, Government of India. The preparation contains four ingredients with antiviral, antipyretic, antioxidant, anti-inflammatory, and immunomodulatory properties. It halts the life-threatening inflammatory retorts in COVID-19, leading to substantial morbidity. AYUSH-64 is included in the National COVID supervision procedure, Government of India, built on Ayurveda and Yoga for asymptomatic and mild cases of COVID-19 (Panda et al., 2022).
Ayush recommends the second formalization. Some of the ingredients include Guduchi, ginger, Ajwain, clove, Dusparsha, Malabar nut, Kusta, Piper longum, Bharangi, Kalamegha, Raja pata, Kokilaksha, Musta, and Neer. Kabasura Kudineer pointedly condenses SARS-CoV-2 viral load in asymptomatic COVID-19 cases with a significant decrease in the neutrophil/lymphocyte ratio and length of hospital stay, and time required to alleviate COVID-19 symptoms. Furthermore, numerous molecular docking studies revealed that the bioactive phytochemicals of Kabasura Kudineer, like andrographolide, apigenin, vasicine, cordiofoliside B, and pyrethrin, had a high affinity for the Spike(S) glycoprotein of SARSCoV-2, preventing host receptor binding. Similarly, another molecular docking study revealed that the bioactive phytochemicals of Kabasura Kudineer, like chrysoeriol and luteolin, have good binding affinity and binding interactions with the spike glycoprotein of SARS-CoV-2 to prevent the binding of host receptors. Acetoside, rutin, luteolin 7-rutinoside, chebulagic acid, violanthin, acanthoside, andrographidine C, syrigaresinol, and myricetin were found to have high binding affinity for the three Chymotrysin-like protease (3CLpro) enzyme, which plays an important role in SARSCoV-2 replication (Natarajan et al., 2021).
In comparison to synthetic drugs like ivermectin, lopinavir, ritonavir, oseltamivir, hydroxychloroquine, and azithromycin, these phytocompounds demonstrate a higher binding affinity for 3CLpro. Another molecular docking study of Kabasura Kudineer bioactive phytoconstituents demonstrated that phytocompounds such as clerodane 6,7 dione, β-amyrin, furanolactone, berberine, piperlongumine, sesamine, lupeol, piperine, and β-sitosterol have a more binding affinity for the main protease enzyme of SARS-CoV-2 and the phytocompounds like clerodanedione, β-sitosterol, beta amyrin, Piper longumine, sesamine, piperine, furanolactone, lupeol, and berberine show more binding affinity towards RNA dependent RNA polymerase (RdRP) (Maideen, 2021).
This ayurvedic formulation was mentioned in a Ministry of AYUSH advisory to combat COVID-19 and is being used as a therapeutic option for patients with COVID-19. AYUSH Kwath may be the drug of choice in the treatment of COVID-19, implying its role in prophylactic, curative, and therapeutic care. It is made up of Tulsi, Dalchini, Sunthi, and Krishna Marich. Sacred Orchid. TNF, cytokines storm, i.e., upregulation of proinflammatory cytokines in the blood like interleukin IL-1, IL-6, and TNF, was inhibited by Cinnamomum zeylanicum bark extract in severe COVID-19. The presence of linoleic acid in fixed oil has the ability to block both the cyclooxygenase and lipoxygenase pathways of arachidonate metabolism, contributing to its anti-inflammatory action. Because of its immune stimulatory properties, C. zeylanicum essential oil and powder have angiotensin-converting enzyme inhibitory and antiviral activity (Abdulamir and Hafidh, 2020). Shogaol and Gingerol compounds in Zingiber officinale inhibit the synthesis of prostaglandins and leukotrienes. These also inhibit the production of proinflammatory cytokines such as TNF-α, IL-8, and IL-1. Shogaol also reduced the expression of the COX-2 gene. Piperine inhibited not only IgM antibody secretion but also CD86 cluster of differentiation expression. The anti-inflammatory activity of piperine is mediated by the inhibition of the inducible nitric oxide synthase (i-NOS) and cyclooxygenase-2 (COX-2). In moderate clinical cases of COVID-19, Ayush Kwath is used as a preventive, curative, and restorative intervention with the goal of resolving symptoms, arresting pathogenesis, and shortening the recovery phase. Nonetheless, more preclinical and clinical trials are needed to assess the protection of this polyherbal formulation (Gautam et al., 2020).
Sudarshan Ghanvati is a highly recommended formula for the prevention of mild to moderate fevers caused by coughing, colds, allergies, indigestion, and diarrhea. It stimulates the liver, aids in blood detoxification, and improves digestion. It is used for the treatment of fever caused by dyspepsia, anorexia, fatigue, and nausea It increases immunity to fight allergens and infections. It contains Chitrak, Ashwagandha, Turmeric, Clove, Black Pepper, Nut Grass, and Ginger, and it aids in the development of immunity. It relieves body aches and combats fatigue, stress, and anxiety. It helps treat respiratory infections and alleviates tuberculosis symptoms. It reduces inflammation or swelling caused by an injury, improves digestion, and reduces stomach acidity. Sudarshan Ghanvati contains antibiotic, anti-inflammatory, and expectorant properties; therefore, this herbal proprietary preparation is useful in treating the common cold, persistent cough, and flu, and can thus help with COVID-19 symptoms. The bio-active mechanisms of the perfumed herbs help to boost immunity and prevent bacterial infestation (Ritesh and Roushan, 2021).
It is a traditional and proprietary ayurvedic medication designed specifically to treat and manage respiratory and digestive disorders. In Ayurveda, Talispatra, Chitrak, Jeera, Chavya, Tintidika, Tejpata, Dalchini, Elaichi, and jaggery are used to treat the common cold virus and are very helpful for releasing nasal discharge, congestion, irritation, and inflammation. This preparation is also beneficial for sneezing, cough, sore throat, breathing troubles, and allergic rhinitis. It is also extremely beneficial in the treatment of bronchitis, asthma, sinusitis, and other respiratory ailments. With potent antimicrobial, antibacterial, and antiseptic properties, this incredible herbal concoction plays a critical role in preventing various infections. It also decreases the risk of dengue, fever, tuberculosis, and bacterial and fungal infections (Sahoo et al., 2022).
Thus, these Indian medicinal plants have a holistic approach to combat the COVID-19 pandemic. Global research on Indian medicinal herbs for COVID-19 has found the efficacy of its active phytoconstituents (Suppl. Table S1). Medicinal plants like Glycyrrhiza glabra, Andrographis paniculata, Withania somnifera, Tinospora cordifolia, herbs used in cooking like Z. officinale, Allium sativum, Moringa oleifera, Piper nigrum, Cinnamomum verum, Curcuma longa, and essential oil-bearing plants like Ocimum sanctum, Azadirachta indica, Syzygium arromaticum, Eucalyptus globulus (Palai and Kesh, 2021) possesses phytochemicals having antioxidant, antiviral, and immunomodulatory properties (Fig. 1, Suppl. Tables S1–S4).
Some Indian Medicinal Plants with Antiviral Activity against Severe Acute Respiratory Syndrome Coronavirus 2
Ocimum sanctum Linn (Tulsi/basil/Holy basil)
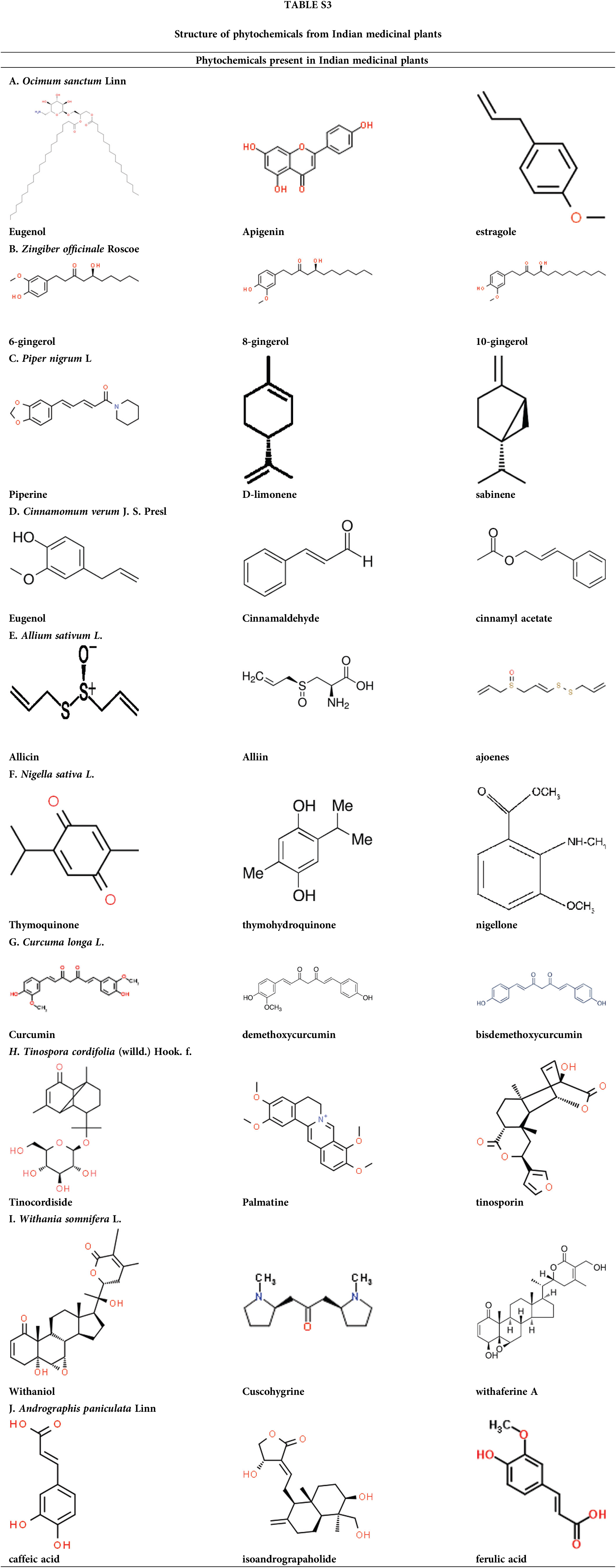
O. sanctum (Tulsi) is known as the ‘Elixir of Life’ in Ayurveda. It’s a nerve tonic and stress reliever. It is beneficial in conditions like asthma, rheumatism, digestive and liver disorders, bronchitis, and microbial contamination. Natural essential oils such as camphene, cineole, and eugenol found in O. sanctum relieve colds and chest congestion. Eugenol has pain-relieving properties and can help with body aches, colds, coughs, and other symptoms. It contains oleanolic acid, estragole, carvacrol, ursolic acid, and terpenes (Padalia and Verma, 2011; Sundaram et al., 2012). O. sanctum contains camphene, cineole, and eugenol, which aid in the relief of colds and chest congestion. Ocimumosides A and B reduce stress and help the neurotransmitters serotonin and dopamine balance in the brain. O. sanctum has anti-inflammatory properties that reduce inflammation and blood pressure. It contains phytochemicals with powerful antioxidant properties that aid in the therapy and prophylaxis of liver malignancy, cardiovascular disease, skin malignancy, oral cancer, and lung cancer. It contains high vitamin C and zinc and works as a natural immune booster. Terpenoids and polyphenols in O. sanctum methanolic extract have antiviral properties against DENV1 and H9N2 (Ghoke et al., 2018). Tulsi contains Tulsinols (A-G) and dihydrodieugenol-B, which inhibit COVID-19 main protease and papain-like protease exhibiting immune-modulatory properties (Varshney et al., 2020).
Zingiber officinale Roscoe (Saunth/dried ginger)
For thousands of years, Z. officinale (ginger) has been used in numerous ailments like migraines, arthritis, colds, nausea, and hypertension. The primary polyphenols in fresh ginger are gingerols such as 6-gingerol, 8-gingerol, and 10-gingerol. Among the phenolic compounds found in Z. officinale are quercetin, zingerone, gingerenome-A, and 6-dehydrogingerdione (Chakotiya et al., 2017). Gingerols can be converted to shogaols through heat treatment or long-term storage (Stoner, 2013). A key ginger compound, 6-Shogaol, aids the patient in resolving respiratory issues (Logeswari et al., 2020). 6-gingerol is a gifted candidate drug for COVID-19, as it has the strongest binding affinity with manifold SARS-CoV-2 targets like RNA binding proteins and viral proteases (Rathinavel et al., 2020). Z. officinale inhibited the development of a multidrug-resistant bacterial strain of Pseudomonas aeruginosa by altering membrane integrity and decreasing biofilm formation (Chakotiya et al., 2017). Owing to its phenolic compounds, Z. officinale has exceptional antimicrobial effects and effectively controls viral, Gram positive and negative bacterial, and fungal disease. Z. officinale has high antioxidant activity due to its oil, which protects against DNA damage. Z. officinale inhibits PG synthesis and interferes with cytokine signaling, thereby reducing inflammation (Al-Awwadi, 2017). Ginger stimulates IFN-secretion, which aids in the fight against viral infection (Yamprasert et al., 2020). In silico research has revealed the inhibitory potential of ginger phytocompounds in two important coronavirus targets, 6LU7 and 7JTL. Gingeronone A exhibits substantial inhibitory potential against some coronavirus targets. Thus, phytocompounds derived from ginger could be extremely beneficial against COVID-19 (Pandey et al., 2020).
Piper nigrum L (Krishna Marich/black pepper)
It is also popular as the “King of Spices” because it contains numerous bioactive constituents like flavonoids, terpenes, phenolics, and sterols with therapeutic properties like analgesic, antiplatelet, antihypertensive, anticancer, antioxidant, and so on. The essential oil profile of seeds of black pepper contains a high amount of caryophyllene, sabinene, α-pinene, limonene, β-bisabolene, etc. Pepper leaves possess a high amount of nerolidol, α-pinene, and nerolidol. Piperine, being the main bioactive component, augments the beneficial effects of several nutrients, vaccines, and drugs through the increase in bioavailability by inhibiting numerous digestive enzymes. It inhibits the exudation of hepatitis B virus surface antigen (HBsAg) and hepatitis B virus e antigen with remarkable HBV activity (HBeAg) (Jiang et al., 2013). Piperine may be effective against viral particle proliferation because it inhibits RNA packaging within the capsid protein (Choudhary et al., 2020). Piper nigrum phenolic compounds can inhibit the main protease of COVID-19 (Davella et al., 2021). In silico studies have revealed the inhibitory potential of selected phytocompound ligands on the coronavirus targets 6LU7 and 7JTL. The significant inhibitory potential against selected coronavirus targets can be very useful in combating COVID-19 (Pandey et al., 2020). Piperine can be a gifted entrant for inhibiting RNA packaging in the nucleocapsid, and thus, viral replication. Also, black pepper can combat SARS-CoV-2 directly through immunomodulatory and antiviral effects (Choudhary et al., 2020).
Cinnamomum verum J. S. Presl (Dalchini/cinnamon)
C. verum is a well-known medicinal herb with antioxidant, anti-inflammatory, antimicrobial, wound healing, and immunostimulant properties that have been shown to be beneficial in cancer, diabetes, Parkinson’s disease, AIDS, and anxiety. Volatile oils found in the plant include eugenol, cinnamaldehyde, cinnamyl acetate, copane, cinnamic acid, cinnamate, cinnamaldehyde, and camphor (Pathak and Sharma, 2021). Cinnamomum bark is active against HIV-1 and HIV-2-like rapidly spreading viruses, as evidenced by virus-induced pathogenicity in MT-4 cells (Premanathan et al., 2000). C. verum inhibits the replication of the Newcastle disease virus in chickens primarily by moderating total protein, globulin, lysozyme activity, and total antioxidant action, as well as meaningfully increasing phagocytic actions (Islam et al., 2021). When combined with other essential oils, C. zeylanicum essential oil demonstrated effective antiviral activity against HSV1 and H1N1 viruses (Ahmad et al., 2021). The extract of C. verum bark acts as an immunomodulator, significantly increasing neutrophil adhesion antibody titer, phagocytic index, and serum immunoglobulins (Balekar et al., 2014). Pphytoconstituents like procyanidine exhibits anti-inflammatory properties in carrageenan-induced edema (Qadir et al., 2018). It can alleviate the symptoms of COVID-19, being an immunomodulatory, anti-inflammatory agent effective against viruses.
A. sativum (garlic) is the most widely cultivated Allium species. Hundreds of phytochemicals are found in the bulb of A. sativum, including sulfur-containing complexes such as allicin, alliin, ajoenes, and vinyl dithiins (Al-Sanfi, 2013). Garlic’s chemical constituents are primarily sulfur-based like ajoene, alliin, S-allyl cysteine, vinyldithiin, diallylpolysulfides, etc. (Sánchez-Sánchez et al., 2020; Arreola et al., 2015). Garlic’s antibacterial activity is linked to allicin activity, which exhibits wide spectrum action against Gram-positive and Gram-negative bacteria like Shigella species and Escherichia coli (Ross et al., 2001). Garlic extracts inhibit the replication of parainfluenza virus type 3, influenza B, human rhinovirus type 2, herpes simplex type 1, human cytomegalovirus vaccinia virus, and vesicular stomatitis virus (Jang et al., 2018). Because garlic contains immune-boosting chemicals, it can be used to prevent COVID-19 infection by strengthening the immune system and suppressing the production and release of proinflammatory adipose-derived hormone leptin and cytokines. The A. sativum can reduce proinflammatory cytokine expression and reverse immunological abnormalities. Thus, A. sativum has been recommended as a useful preventative medication for SARS-CoV-2 virus infection (Percival, 2016; Bathia et al., 2020).
N. sativa (Black cumin) is the “curative black seed”. Terpenes like thymol, carvacrol, dithymoquinone, thymohydroquinone, α-pinene, d-citronellol, p-cymene, and d-limonene are among phytoconstituents found in black cumin. Its volatile oil contains t-anethole, carvacrol, 4-terpineol, longifolene, P-cymene, etc. N. sativa contains vitamins, fats, carbohydrates, minerals, and proteins with essential amino acids. Thymoquinone is antinociceptive and anti-inflammatory. These protective properties are accredited to its repeatable radical scavenging effect and collaboration with many molecular targets involved in inflammation, like cytokines and proinflammatory enzymes (Amin and Hosseinzadeh, 2016). Thymoquinone prevents viral infection and causes cell death at high concentrations indicating cytotoxic effects. N. sativa extracts combined with Z. officinale enhanced liver function and reduced viral load in the hepatitis C virus. Thymoquinone inhibits SARS-CoV-2 protease and has clear antagonistic activity against ACE 2 receptors. In silico studies demonstrated moderate to high affinity of N. sativa compounds for SARS-CoV-2 proteins and enzymes (Badary et al., 2021) N. sativa may successfully inhibit SARS-CoV-2 spike recognition and fixation by tightly binding to cell-surface HSPA5 (host cell receptors recognized by the viral spike protein). Thymoquinone has an anti-inflammatory effect and acts against the Coronavirus by preventing viral entry (Abdelrahim et al., 2022).
Tumeric (C. longa) is a yellow spice made from cooked, dried, and ground rhizomes or roots. Curcumin is the active ingredient in turmeric, accounting for 2 to 8% of the spice (Arun and Nalini, 2002). Curcumin has antioxidant and anti-inflammatory effects and influences cellular enzymes and angiogenesis (Chainani-Wu, 2003; Hua and Cheng, 2007). C. longa contains phenolic compounds and terpenoids like diarylheptanoids, sesquiterpenes, diterpenes, monoterpenes, triterpenoids, alkaloids, and sterols (Lv and She, 2010). Curcuminoids, diarylheptanoids, diphenylheptanoids, and curcumin or di-feruloyl methane are active ingredients (Jayaprakasha et al., 2006). C. longa is shown to be effective against respiratory viruses like the respiratory syncytial virus, and influenza A causing acute respiratory infections (Dai et al., 2018). Curcumin prevents influenza A virus (IAV) hemagglutinins, a homotrimer membrane glycoprotein, from binding to the host cell receptor. It can also inhibit pulmonary edema and fibrosis-related paths of COVID-19 pathogenesis (Zahedipour et al., 2020). It inhibits inflammatory cytokines, toll-like receptors, bradykinin, and chemokines via several molecular mechanisms (Babaei et al., 2020). SARS-CoV-2 viral protein access can be prevented by curcumin isolated from turmeric. In an in-silico analysis, curcumin was found to bind to the receptor-binding domain (RBD) site of the viral S protein as well as the viral attachment sites of the ACE 2 receptor (Das et al., 2021). Curcumin can act as a defensive herb in the controlling of COVID-19 spread.
Tinospora cordifolia (willd.) Hook. f.
T. cordifolia (Guduchi) is a remedial herb used for treating various diseases, including gonorrhea. The root has a strong emetic effect and is used to treat intestinal blockage. A wide range of chemicals are isolated from aerial parts, roots, entire plant of T. cordifolia. It has immunomodulatory properties due to the presence of berberine, tinosporin, palmatine, tembetarine, choline, isocolumbin, etc., like compounds (Sharma et al., 2019). T. cordifolia improves the immune protective response to the Infectious Bursal Disease vaccine in chicks (Sachan et al., 2019). In a humanized zebrafish model of SARS-CoV-2, spike-protein-induced disease confirmed behavioral fever indicated by increased body temperature, which was inverted after treatment with T. cordifolia and Thomson aqueous extracts as Giloy Ghanvati (GG) tablets test formulation. It upturned the proinflammatory cell infiltration in the swim bladder and also saved the kidney from tubular injury and necrosis. The cytological, behavioral, and morphological changes of SARS-CoV-2 spike-protein induction were restored after using Giloy Ghanvati (Balkrishna et al., 2021). Natural components isolated from T. cordifolia, such as isocolumbin, magnoflorine, berberine, and tinocordiside, were tested using in silico methods against 4 SARS-CoV-2 targets like receptor binding domain (6M0J), RNA-dependent RNA polymerase (6M71), surface glycoprotein (6VSB), and main protease (6M71) (6Y84). Giloy is a potentially useful herb in the therapy of COVID-19 infection because all four compounds demonstrated strong binding efficacy against a total of four targets (Sagar and Kumar, 2020).
The common name of W. somnifera L. (Ashwagandha) comes from the phrase “the smell and strength of a horse,” denoting its aphrodisiacal actions. W. somnifera roots are used as a sedative for swellings and tumors. Withanine, withanolides, psuedowithanine, somnine, somniferinine, and withaferin A are among the alkaloids found in the root. Withaferin A can treat the common cold, infertility, and other gynecological ailments. They improve immune homeostasis by increasing macrophage NOS activity. They have anti-inflammatory and antioxidant properties and can decrease IL-1, IL-6, and TNF. Withanolides have antiviral properties against influenza and herpes simplex viruses (Kalra et al., 2021). Withanolides are also effective immune boosters. It can be helpful in SARS-CoV-2 infection by modulating host Th-1/Th-2 immunity (Mehrotra, 2020). In-silico studies have revealed that it has a strong affinity for the ACE2-RBD interface, potentially preventing SARS-COV-2 from infecting cells (Parihar, 2022). According to the results of in silico docking and molecular dynamics, Withanoside X and Quercetin glucoside from W. somnifera have favorable exchanges at the binding sites of selected proteins, 6W01 and 6M0J, and can be used as SARS-COV-2 protein inhibitors (Chikhale et al., 2021). Ashwagandha can be used to treat SARS-CoV-2 because it prevents cytokine storms and viral infections.
Traditionally, the herb A. paniculate (Kalmegh) is termed as “King of bitter” as every component of the plant is extremely bitter. It has antiviral and antibacterial properties that reduce fever as well as muscle and bodily discomfort. It has both hepatoprotective and hepatostimulative properties (Kishore et al., 2003). The leaf, entire plant, and stem of A. aniculate yielded over 22 diterpenoids and 10 flavonoids after ethanolic or methanolic extraction (Li et al., 2007). Several isolated compounds from A. paniculate, like isoandrograpaholide inhibited tumors and proinflammatory intermediaries (NO, IL-1, and IL-6) as well as allergic intermediaries (Chandrasekaran et al., 2011). Andrographolide protects against deoxyribonucleic acid viruses (herpes simplex virus 1 and Epstein-Barr virus) and ribonucleic acid viruses (HIV, IAV, hepatitis C, dengue virus, and Japanese encephalitis virus) (Gupta et al., 2017). Andrographolide and its analogs can potentially be used in the treatment of various virus infections, including SARS-CoV-2. Andrographolide is made up of the cytotoxic gamma-butyrolactone moiety, an alpha-alkylidyne moiety, and three hydroxyls at C-3, C-19, and C-14 can be an effective chemotherapeutic agent having pharmacological properties (Verma et al., 2011). An in-silico analysis revealed that andrographolide contains likely SARS-CoV-2’s main protease inhibitors (Enmozhi et al., 2020).
Various Mechanisms of Phytochemicals against Coronaviruses (Especially Severe Acute Respiratory Syndrome Coronavirus 2)
Through in vitro and in vivo testing of phytochemicals against coronaviruses (especially SARS-CoV-2), as well as computer docking model studies that predict the anti-SARS-CoV-2 effects of these compounds against the coronavirus specifically, SARS-CoV-2, the use of natural compounds for the treatment of related complications of COVID-19, is being investigated. According to those studies, natural polyphenol compounds with prominent anti-coronavirus properties include quercetin, ocimumosides, kaempferol, myricetin, cinnamaldehyde, apigenin, allicin, piperine, and nimbin. Considering the aforementioned, it can be concluded that phytochemicals are potential sources for the development of potent anti-coronavirus medications, particularly anti-SARS-CoV-2 medications (Majnooni et al., 2020).
Inhibiting the SARS-COV-2 infection is accomplished through numerous mechanisms, including the antiviral effect regulating the stage of viral entry, gene replication, and formation of mature functional proteins. It may be an effective triple target receptor inhibitor to halt the launch of SARs-COV-2, ACE-2, host cell TMPRSS2 receptors, and virus Spike protein. The use of W. somnifera, Piper retrofractum, Plumbago zeylanica decreases oxidative factors like ROS and free radicals extending the antioxidant effect. The therapeutic plants inhibited neutrophil and cell infiltration in BALF, downregulated the extracellular signal-regulated kinase/mitogen-activated protein kinase (ERK/MAPK) pathway and increased antioxidant activities to reduce lipopolysaccharide (LPS)-induced lung injury complications. The plant O. sanctum extends anti-inflammatory effect by improving hemoglobin concentration and inhibiting the NF-Kb classical pathway. Also, P. nigrum, A. sativum, N. sativa, T. cordifolia reduces the symptoms of pulmonary infections through p38 MAPK pathways. The immunomodulatory effect of Z. officinale, C. longa, Azadirachta indica, etc. boosts antiviral immune responses, have direct anti-SARS-CoV-2 effects, and inhibits macrophage and inflammasome-mediated inflammatory actions (Mukherjee et al., 2022).
In-silico trials of active phytoconstituents of Indian medicinal plants like T. cordifolia, W. somnifera, O. sanctum, etc. predicted significant inhibition of SARS-CoV-2 main protease (Mpro or 3Clpro). Through molecular docking and molecular dynamic simulation, phytochemicals like somniferine, vicenin, withanoside V, ursolic acid, tinocordiside, and isorientin 4′-o-glucoside 2′′-O-p-hydroxybenzoagte inhibited SARS-CoV-2 Mpro action. The better-docked compounds are safe compounds with no toxicity based on their drug-likeness and the absorption, distribution, metabolism, excretion, and toxicity (ADMET) profile (Shree et al., 2022).
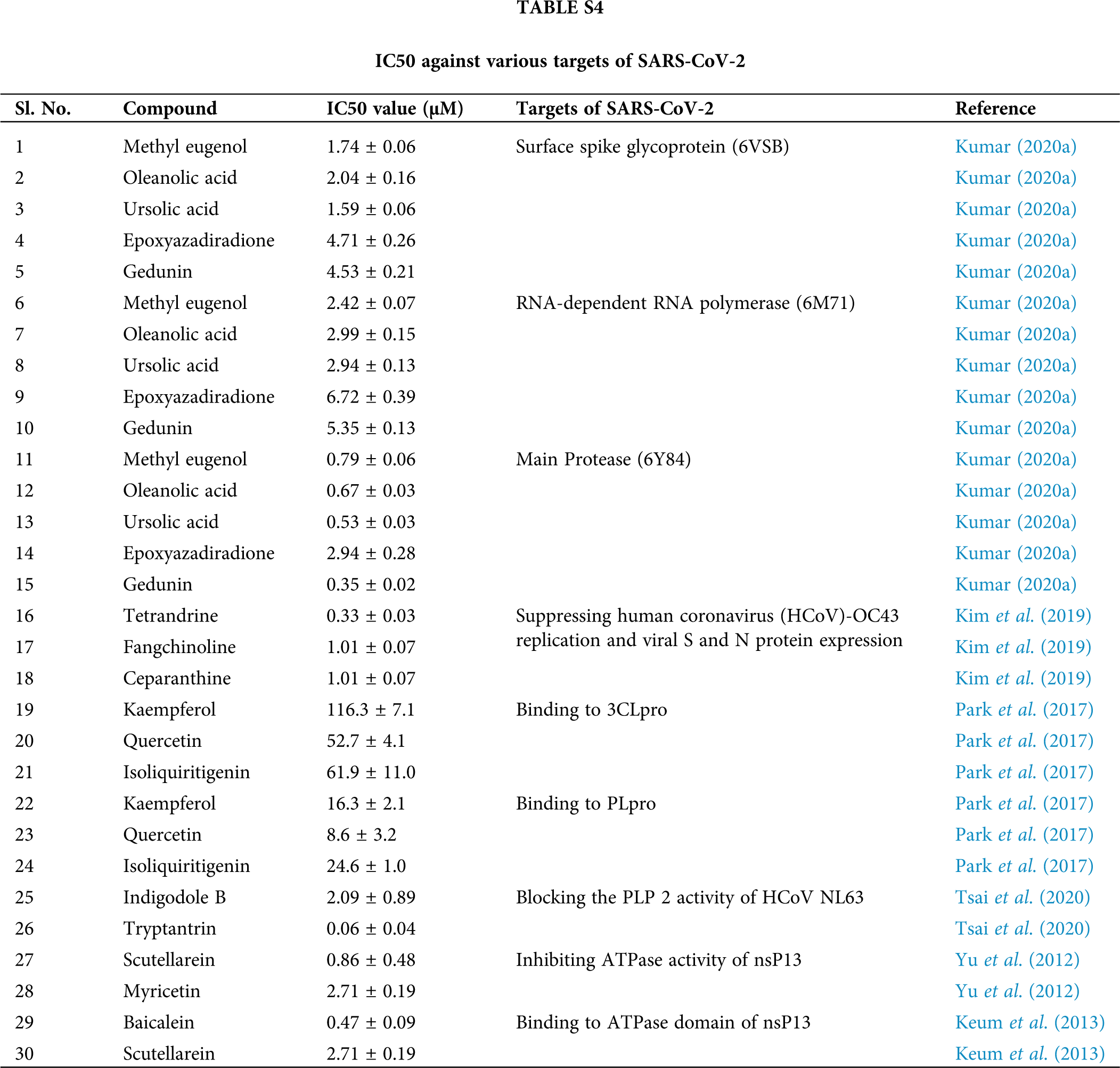
Anti-coronavirus effect of phytochemicals
Natural phytochemical components are of particular interest among the many inhibitory substances introduced against coronaviruses via the. Plant secondary and primary metabolites are being investigated as possible coronavirus inhibitory medicaments. The IC50 value (the concentration at which 50% of enzyme activity is lost), molecular docking score, and binding energy are all parameters used to determine a metabolite’s ability to inhibit a specific virus. Polyphenols, alkaloids, terpenoids, organosulfur compounds, saponins, essential oil, saikosaponins, lectins, nicotianamine, etc., are examples of secondary plant metabolites (Farshi et al., 2022). Usual compounds derived from tulsi and neem possess more binding efficacy against SARS-CoV-2 targets tangled in viral attachment and replication for the treatment of SARS-CoV-2 infections (Shrestha et al., 2022). The high binding efficacy is observed against SARS-CoV-2 surface spike glycoprotein, RNA polymerase, and the major protease. Furthermore, natural chemicals are capable of suppressing human coronavirus OC43 replication and viral S and N protein expression, binding to 3CLpro and PLpro, blocking PLP 2 activity of HCoV NL63, inhibiting ATPase activity of nsP13, and binding to the ATPase domain of nsP13 (Suppl. Table S4).
Anti-inflammatory effect of phytochemicals against acute lung injury
Many animal models demonstrated a defensive effect against acute lung injury. O. Sanctum alcoholic extracts, for example, demonstrated anti-asthmatic potential via an inflammatory mechanism by inhibiting leukotriene C4, leukotriene A4, and COX-2 in HL-60 cell lines and reducing inflammation in a mouse model for asthma (Soni et al., 2015). The aqueous extract of leaves inhibited histamine fusion in both rat peritoneal and mast cells (Negi and Dave, 2010). GA could suppress caveolin-1/NF-B expression by activating ACE2. GA activated the ACE2 and caveolin-1 pathways, alleviating LPS-induced ALI and providing a novel prospect of GA-ameliorated ALI by inducing ACE2. Thus, ACE2 and caveolin-1/NF-B signaling may be associated with the mechanism of the protective effect of GA in LPS-induced ALI (Chen et al., 2021).
Also, the anti-inflammatory effect of Nymphaea alba flower in Swiss albino mice (RS et al., 2013), Datura metel linn amelioration of asthma symptoms in BALB/c mice (Rifa’i et al., 2014), garlic protection in allergen-induced airway inflammation in mouse (Hsieh et al., 2019), and aid of Ocimum basilicum in tracheal reaction, lung inflammatory cells and antioxidant (Eftekhar et al., 2019).
These selected flavonoids have a better absorption rate. Their volume of distribution at steady-state, skin permeability, central nervous system permeability, and blood-brain barrier permeability were also examined because they have an important role in drug distribution. Among the various cytochromes P450 (CYPs) enzymes, cytochrome P450 3A4 (CYP3A4) was discovered to be inhibited by flavonoids, implying that these flavonoids may be metabolized in the liver (Shrestha et al., 2022).
ProTox-II, which calculates median lethal dose (LD50) values and toxicity classes, was also used to predict the toxicity of the selected flavonoids. The LD50 values and toxicity classes of 37 flavonoids predicted by ProTox-II are mentioned in Suppl. Table S4. In terms of acute oral toxicity, flavonoids in the toxicity class have LD50 values ranging from 2000 to 5000 and LD50 values greater than 5000. The flavonoids are also toxic class III (50 LD50 300) and toxicity class 300 LD50 2000. Malvidin and cyanidin have LD50s of 5000, tomentin E of 10,000, 4′-O-methyldiplacol and mimulone of 2000, and neobavaisoavone of 2500. Lipinski’s criteria were mostly met by the flavonoids, indicating that they can be used as drugs (Shrestha et al., 2022).
The relationship between docking score and IC50 value was investigated, and for the majority of molecules, the docking score was negative, indicating that they have better druggability (Sherin and Manojkumar, 2022). Active plant phytoconstituents T. cordifolia, W. somnifera, and O. sanctum have been projected to interact with SARS-CoV-2 Mpro or 3CLpro protease. These phytochemicals were found to be safe in ADMET studies using molecular docking (Shree et al., 2022). This implies that compounds derived from plants may be useful in developing strategies for managing COVID-19 because they have fewer side effects and significant functional capability (Ullah et al., 2022).
The traditional medicinal plants of India are a highly advantageous alternative herbal remedy for COVID-19. According to general AYUSH recommendations, medicinal plants with anti-inflammatory, antioxidant, immunomodulatory, and antiviral properties are useful for both the prevention and supportive treatment of COVID-19. The current review lists several important Indian medicinal plants that have been tested experimentally against COVID-19 and details the claimed plants’ active phytochemicals in addition to the antiviral research that has been conducted on them globally. The antiviral properties of these herbal remedies can be clarified with the aid of bioinformatics databases and tools. The effectiveness of the phytoconstituents in Indian medicinal plants is also demonstrated by the safety factors and inhibitory concentrations. Combining them all, the literature review contends that COVID-19 disease can be beaten by combining traditional and modern sciences.
Funding Statement: The authors received no specific funding for this study.
Author Contributions: The authors confirm contribution to the paper as follows: study conception and design: S.C., M.I., H.D.M.C. and S.P.; data collection: E.F.F.M.; analysis and interpretation of results: I.C.P.N.; C.L.G.R. and E.M.d.A.; draft manuscript preparation: R.S.d.A. and H.D.M.C. All authors reviewed the results and approved the final version of the manuscript.
Availability of Data and Materials: The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Ethics Approval: Not applicable.
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
References
Abdelli I, Hassani F, Bekkel Brikci S, Ghalem S (2021). In silico study the inhibition of angiotensin converting enzyme 2 receptor of COVID-19 by Ammoides verticillata components harvested from Western Algeria. Journal of Biomolecular Structure and Dynamics 39: 3263–3276. https://doi.org/10.1080/07391102.2020.1763199 [Google Scholar] [PubMed] [CrossRef]
Abdelrahim M, Esmail A, Al Saadi N, Zsigmond E, Al Najjar E, Bugazia D, Al-Rawi H, Alsaadi A, Kaseb AO (2022). Thymoquinone’s antiviral effects: It is time to be proven in the COVID-19 pandemic era and its omicron variant surge. Frontiers in Pharmacology 13: 89. https://doi.org/10.3389/fphar.2022.848676 [Google Scholar] [PubMed] [CrossRef]
Abdulamir AS, Hafidh RR (2020). The possible immunological pathways for the variable immunopathogenesis of COVID-19 infections among healthy adults, elderly and children. Electronic Journal of General Medicine 17: em202. https://doi.org/10.29333/ejgm/7850 [Google Scholar] [CrossRef]
Ahmad A, Husain A, Mujeeb M, Khan SA, Najmi AK, et al. (2013). A review on therapeutic potential of Nigella sativa: A miracle herb. Asian Pacific journal of tropical biomedicine 3: 337–352. https://doi.org/10.1016/S2221-1691(13)60075-1 [Google Scholar] [PubMed] [CrossRef]
Ahmad S, Zahiruddin S, Parveen B, Basist P, Parveen A, Gaurav, Parveen R, Ahmad M (2021). Indian medicinal plants and formulations and their potential against COVID-19–preclinical and clinical research. Frontiers in Pharmacology 11: 2470. https://doi.org/10.3389/fphar.2020.578970 [Google Scholar] [PubMed] [CrossRef]
Al-Awwadi NA (2017). Potential health benefits and scientific review of ginger. Journal of Pharmacognosy and Phytotherapy 9: 111–116. https://doi.org/10.5897/JPP2017.0459 [Google Scholar] [CrossRef]
Al-Sanfi AE (2013). Pharmacological effects of Allium species grown in Iraq. An overview. International Journal of Pharmaceuticals and Health Care Research 1: 132–147. [Google Scholar]
Amin B, Hosseinzadeh H (2016). Black cumin (Nigella sativa) and its active constituent, thymoquinone: An overview on the analgesic and anti-inflammatory effects. Planta Medica 1: 8–16. https://doi.org/10.1055/s-0035-1557838 [Google Scholar] [PubMed] [CrossRef]
Arreola R, Quintero-Fabián S, López-Roa RI, Flores-Gutiérrez EO, Reyes-Grajeda JP, Carrera-Quintanar L, Ortuño-Sahagún D (2015). Immunomodulation and anti-inflammatory effects of garlic compound. Journal of Immunology Research 2015: 401630. https://doi.org/10.1155/2015/401630 [Google Scholar] [PubMed] [CrossRef]
Arun N, Nalini N (2002). Efficacy of turmeric on blood sugar and polyol pathway in diabetic albino rats. Plant foods for Human Nutrition 57: 41–52. https://doi.org/10.1023/A:1013106527829 [Google Scholar] [PubMed] [CrossRef]
Ashokkumar K, Murugan M, Dhanya MK, Pandian A, Warkentin TD (2021). Phytochemistry and therapeutic potential of black pepper [Piper nigrum (L.)] essential oil and piperine: A review. Clinical Phytoscience 7: 52. https://doi.org/10.1186/s40816-021-00292-2 [Google Scholar] [CrossRef]
Babaei F, Nassiri-Asl M, Hosseinzadeh H (2020). Curcumin (a constituent of turmericNew treatment option against COVID-19. Food Science & Nutrition 8: 5215–5227. https://doi.org/10.1002/fsn3.1858 [Google Scholar] [PubMed] [CrossRef]
Badary OA, Hamza MS, Tikamdas R (2021). Thymoquinone: A promising natural compound with potential benefits for COVID-19 prevention and cure. Drug Design, Development and Therapy 15: 1819–1833. https://doi.org/10.2147/DDDT.S308863 [Google Scholar] [PubMed] [CrossRef]
Balekar N, Bodhankar S, Mohan V, Thakurdesai PA (2014). Modulatory activity of a polyphenolic fraction of Cinnamomum zeylanicum L. bark on multiple arms of immunity in normal and immunocompromised mice. Journal of Applied Pharmaceutical Science 4: 114–122. https://doi.org/10.7324/JAPS.2014.40720 [Google Scholar] [CrossRef]
Baliga MS, Jimmy R, Thilakchand KR, Sunitha V, Bhat NR, Saldanha E, Rao S, Rao P, Arora R, Palatty PL (2013). Ocimum sanctum L (Holy Basil or Tulsi) and its phytochemicals in the prevention and treatment of cancer. Nutrition and Cancer 65: 26–35. https://doi.org/10.1080/01635581.2013.785010 [Google Scholar] [PubMed] [CrossRef]
Balkrishna A, Khandrika L, Varshney A (2021). Giloy Ghanvati (Tinospora cordifolia (Willd.) Hook. f. and Thomson) reversed SARS-CoV-2 viral spike-protein induced disease phenotype in the xenotransplant model of humanized zebrafish. Frontiers in Pharmacology 12: 635510. https://doi.org/10.3389/fphar.2021.635510 [Google Scholar] [PubMed] [CrossRef]
Bathia GES, Beshbishy AM, Wasef LG (2020). Chemical constituents and pharmacological activities-of garlic (Allium sativum L.A review. Nutrients 12: 872. https://doi.org/10.3390/nu12030872 [Google Scholar] [PubMed] [CrossRef]
Chainani-Wu N (2003). Safety and anti-inflammatory activity of curcumin: A component of turmeric (Curcuma longa). Journal of Alternative and Complementary Medicine 9: 161–168. https://doi.org/10.1089/107555303321223035 [Google Scholar] [PubMed] [CrossRef]
Chakotiya AS, Tanwar A, Narula A, Sharma RK (2017). Zingerber officinale, its antibacterial activity on Pseudomonads aeruginosa and mode of action evaluated by flow cytometry. Microbial Pathogenesis 107: 254–260. https://doi.org/10.1016/jmicpath2017.03.029 [Google Scholar] [CrossRef]
Chandrasekaran CV, Thiyagarajan P, Deepak HB, Agarwal A (2011). In vitro modulation of LPS/calcimycin induced inflammatory and allergic mediators by pure compounds of Andrographis paniculata (King of bitters) extract. International 11: 79–84. https://doi.org/10.1016/j.intimp.2010.10.009 [Google Scholar] [PubMed] [CrossRef]
Chen TH, Hsu MT, Lee MY, Chou CK (2022). Gastrointestinal involvement in SARS-CoV-2 infection. Viruses 4: 1188. https://doi.org/10.3390/v14061188 [Google Scholar] [PubMed] [CrossRef]
Chen Y, Qu L, Li Y, Chen C, He W, Shen L, Zhang R (2021). Glycyrrhizic acid alleviates lipopolysaccharide (LPS)-induced acute lung injury by regulating Angiotensin-Converting Enzyme-2 (ACE2) and Caveolin-1 signaling pathway. Inflammation 45: 253–266. https://doi.org/10.1007/s10753-021-01542-8 [Google Scholar] [PubMed] [CrossRef]
Chen N, Zhou M, Dong X, Qu J, Gong F et al. (2020). Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: A descriptive study. The Lancet 395: 507–513. https://doi.org/10.1016/S0140-6736(20)30211-7 [Google Scholar] [PubMed] [CrossRef]
Chikhale RV, Gurav SS, Patil RB, Sinha SK, Prasad SK, Shakya A, Shrivastava SK, Gurav NS, Prasad RS (2021). sars-cov-2 host entry and replication inhibitors from Indian ginseng: An in-silico approach. Journal of Biomolecular Structure & Dynamics 39: 4510–4521. https://doi.org/10.1080/07391102.2020.1778539 [Google Scholar] [PubMed] [CrossRef]
Choudhary P, Chakdar H, Singh D, Selvaraj C, Singh SK, Kumar S, Saxena AK (2020). Computational studies reveal piperine, the predominant oleoresin of black pepper (Piper nigrum) as a potential inhibitor of SARS-CoV-2 (COVID-19). Current Science 119: 1333–1342. https://doi.org/10.18520/cs/v119/i8/1333-1342 [Google Scholar] [CrossRef]
Cárdenas Garza GR, Elizondo Luévano JH, Bazaldúa Rodríguez AF, Chávez Montes A, Pérez Hernández RA et al. (2021). Benefits of cardamom (Elettaria cardamomum (L.) Maton) and turmeric (Curcuma longa L.) extracts for their applications as natural anti-inflammatory adjuvants. Plants 10: 1908. https://doi.org/10.3390/plants10091908 [Google Scholar] [PubMed] [CrossRef]
Dai J, Gu L, Su Y, Wang Q, Zhao Y, Chen X, Deng H, Li W, Wang G, Li K (2018). Inhibition of Curcuma on influenzas A virus infection and influenzas pneumonia via oxidative stress, TLR2/4, p38/JNK MAPK and NF-κB pathways. International Immunopharmacology 54: 177–187. https://doi.org/10.1016/j.intimp.2017.11.009 [Google Scholar] [PubMed] [CrossRef]
Das S, Sarmah S, Lyndem S, Roy AS (2021). An investigation into the identification of potential inhibitors of SARS-CoV-2 main protease using molecular docking study. Journal of Biomolecular Structure and Dynamics 39: 3347–3357. https://doi.org/10.1080/07391102.2020.1763201 [Google Scholar] [PubMed] [CrossRef]
Davella R, Gurrapu S, Mamidala E (2021). Phenolic compounds as promising drug candidates against COVID-19—An integrated molecular docking and dynamics simulation study. Materials Today: Proceedings 51: 522–527. https://doi.org/10.1016/j.matpr.2021.05.595 [Google Scholar] [PubMed] [CrossRef]
Donma MM, Donma O (2020). The effects of Allium sativum on immunity within the scope of COVID-19 infection. Medical Hypotheses 144: 109934. https://doi.org/10.1016/j.mehy.2020.109934 [Google Scholar] [PubMed] [CrossRef]
Eftekhar N, Moghimi A, Hossein Boskabady M, Kaveh M, Shakeri F (2019). Ocimum basilicum affects tracheal responsiveness, lung inflammatory cells and oxidant-antioxidant biomarkers in sensitized rats. Drug and Chemical Toxicology 42: 286–294. https://doi.org/10.1080/01480545.2018.1459672 [Google Scholar] [PubMed] [CrossRef]
Enmozhi SK, Raja K, Sebastine I, Joseph J (2020). Andrographolide as a potential inhibitor of SARS-CoV-2 main protease: An in-silico approach. Journal of Biomolecular Structure and Dynamics 39: 1–7. https://doi.org/10.1080/07391102.2020.1760136 [Google Scholar] [PubMed] [CrossRef]
Farshi P, Kaya EC, Hashempour-Baltork F, Khosravi-Drani K (2022). The effect of plant metabolites on coronaviruses: A comprehensive review focusing on their IC50 values and molecular docking scores. Mini Reviews in Medicinal Chemistry 22: 457–483. https://doi.org/10.2174/1389557521666210831152511 [Google Scholar] [PubMed] [CrossRef]
Fuloria S, Mehta J, Chandel A, Sekar M, Rani NN et al. (2022). A comprehensive review on the therapeutic potential of Curcuma longa Linn. in relation to its major active constituent curcumin. Frontiers in Pharmacology 13: 820806. https://doi.org/10.3389/fphar.2022.820806 [Google Scholar] [PubMed] [CrossRef]
Fuzimoto AD (2021). An overview of the anti-SARS-CoV-2 properties of Artemisia annua, its antiviral action, protein-associated mechanisms, and repurposing for COVID-19 treatment. Journal of Integrative Medicine 19: 375–388. https://doi.org/10.1016/j.joim.2021.07.003 [Google Scholar] [PubMed] [CrossRef]
Gautam S, Gautam A, Chhetri S, Bhattarai U (2020). Immunity against COVID-19: Potential role of Ayush Kwath. Journal of Ayurveda and Integrative Medicine 17: 100350. https://doi.org/10.1016/j.jaim.2020.08.003 [Google Scholar] [PubMed] [CrossRef]
Ghoke SS, Sood R, Kumar N, Pateriya AK, Bhatia S et al. (2018). Evaluation of antiviral activity of Ocimum sanctum and Acacia arabica leaves extracts against H9N2 virus using embryonated chicken egg model. BMC Complementary and Alternative Medicine 18: 174. https://doi.org/10.1186/s12906-018-2238-1 [Google Scholar] [PubMed] [CrossRef]
Gupta S, Mishra KP, Ganju L (2017). Broad-spectrum antiviral properties of andrographolide. Archives of Virology 162: 611–623. https://doi.org/10.1007/s00705-016-3166-3 [Google Scholar] [PubMed] [CrossRef]
Hsieh CC, Peng WH, Tseng HH, Liang SY, Chen LJ, Tsai JC (2019). The protective role of garlic on allergen-induced airway inflammation in mice. American Journal of Chinese Medicine 47: 1099–1112. https://doi.org/10.1142/S0192415X19500563 [Google Scholar] [PubMed] [CrossRef]
Hua CH, Cheng AL (2007). Clinical studies with curcumin. Advances in Experimental Medicine and Biology 595: 471–480. https://doi.org/10.1007/978-0-387-46401-5 [Google Scholar] [CrossRef]
Islam AR, Ferdousi J, Shahinozzaman M (2021). Previously published ethno-pharmacological reports reveal the potentiality of plants and plant-derived products used as traditional home remedies by Bangladeshi COVID-19 patients to combat SARS-CoV-2. Saudi Journal of Biological Sciences 28: 6653–6673. https://doi.org/10.1016/j.sjbs.2021.07.036 [Google Scholar] [PubMed] [CrossRef]
RS JJ, Jagadeesh S, Ganesan S, Eerike M (2013). Anti inflammatory activity of ethanolic extract of Nymphaea alba flower in swiss albino mice. International Journal of Medical Research & Health Sciences 2: 474–478. https://doi.org/10.5958/j.2319-5886.2.3.082 [Google Scholar] [CrossRef]
Jafarzadeh A, Jafarzadeh S, Nemati M (2021). Therapeutic potential of ginger against COVID-19: Is there enough evidence? Journal of Traditional Chinese Medical Sciences 8: 267–279. https://doi.org/10.1016/j.jtcms.2021.10.001 [Google Scholar] [CrossRef]
Jang HJ, Lee HJ, Yoon DK, Ji DS, Kim JH, Lee CH (2018). Antioxidant and antimicrobial activities of fresh garlic and aged garlic by-products extracted with different solvents. Food Science and Biotechnology 27: 219–225. https://doi.org/10.1007/s10068-017-0246-4 [Google Scholar] [PubMed] [CrossRef]
Jayaprakasha GK, Roa LJM, Sakariah KK (2006). Anti-oxidant activities of Curcuma, dimethoxy curcumin and bisdemethoxycurcumin. Food Chemistry 98: 720–724. https://doi.org/10.1016/j.foodchem.2005.06.037 [Google Scholar] [CrossRef]
Jiang ZY, Liu WF, Zhang XM, Luo J, Ma YB, Chen JJ (2013). Anti-HBV active constituents from Piper longum. Bioorganic & Medicinal Chemistry Letters 23: 2123–2127. https://doi.org/10.1016/j.bmcl.2013.01.118 [Google Scholar] [PubMed] [CrossRef]
Joshi DR, Shrestha AC, Adhikari N (2018). A review on diversified use of the king of spices: Piper nigrum (Black Paper). International Journal of Pharmaceutical Sciences and Research 9: 4089–4101. https://doi.org/10.13040/IJPSR.0975-8232.9(10).4089-01 [Google Scholar] [CrossRef]
Kalra RS, Kumar V, Dhanjal JK, Garg S, Li X, Kaul SC, Sundar D, Wadhwa R (2021). COVID19-inhibitory activity of withanolides involves targeting of the host cell surface receptor ACE2: Insights from computational and biochemical assays. Journal of Biomolecular Structure and Dynamics 17: 1–4. https://doi.org/10.1080/07391102.2021.1902858 [Google Scholar] [PubMed] [CrossRef]
Kesh SS, Palai S (2022). Herbs and drugs in clinical trials for coronavirus treatments. In: Coronavirus drug discovery, vol. 2, pp. 55–70. Amsterdam, Netherlands: Elsevier. [Google Scholar]
Keum YS, Lee JM, Yu MS, Chin YW, Jeong YJ (2013). Inhibition of SARS coronavirus helicase by Baicalein. Bulletin of the Korean Chemical Society 34: 3187–3188. https://doi.org/10.5012/bkcs.2013.34.11.3187 [Google Scholar] [CrossRef]
Khan MM, dul Haque MS, Chowdhury MS (2016). Medicinal use of the unique plant Tinospora cordifolia: Evidence from the traditional medicine and recent research. Asian Journal of Medical and Biological Research 2: 508–512. https://doi.org/10.3329/ajmbr.v2i4.30989 [Google Scholar] [CrossRef]
Khazdair MR, Ghafari S, Sadeghi M (2021). Possible therapeutic effects of Nigella sativa and its thymoquinone on COVID-19. Pharmaceutical Biology 59: 694–701. https://doi.org/10.1080/13880209.2021.1931353 [Google Scholar] [PubMed] [CrossRef]
Kim DE, Min JS, Jang MS, Lee JY, Shin YS et al. (2019). Natural bis-benzylisoquinoline alkaloids-tetrandrine, fangchinoline, and cepharanthine, inhibit human coronavirus OC43 infection of MRC-5 human lung cells. Biomolecules 9: 696. https://doi.org/10.3390/biom9110696 [Google Scholar] [PubMed] [CrossRef]
Kishore PH, Reddy MV, Reddy MK, Gunasekar D, Caux C, Bodo B (2003). Flavonoids from Andrographis lineata. Phytochemistry 63: 457–461. https://doi.org/10.1016/S0031-9422(02)00702-1 [Google Scholar] [PubMed] [CrossRef]
Kumar AH (2020a). Molecular docking of natural compounds from tulsi (Ocimum sanctum) and neem (Azadirachta indica) against SARS-CoV-2 protein targets. Biology, Engineering, Medicine and Science Reports 6: 11–13. https://doi.org/10.5530/bems.6.1.4 [Google Scholar] [CrossRef]
Kumar S (2020b). Immunity boosting role of medicinal plant and Pranayama, an alternative way to fight against COVID-19. International Journal of Contemporary Medical Research 7: 11–15. https://doi.org/10.21276/ijcmr.2020.7.9.22 [Google Scholar] [CrossRef]
Kumar G, Kumar D, Singh NP (2021). Therapeutic approach against 2019-nCoV by inhibition of ACE-2 receptor. Drug Research 71: 213–218. https://doi.org/10.1055/a-1275-0228 [Google Scholar] [PubMed] [CrossRef]
Kumar RS, Narasingappa RB, Joshi CG, Girish TK, Danagoudar A (2017). Caesalpinia Crista Linn. Induces protection against DNA and membrane damage. Pharmacognosy Magazine 13: 250–257. https://doi.org/10.4103/pm.pm_557_16 [Google Scholar] [PubMed] [CrossRef]
Kumar V, van Staden J (2016). A review of Swertia chirayita (Gentianaceae) as a traditional medicinal plant. Frontiers in pharmacology 6: 308. https://doi.org/10.3389/fphar.2015.00308 [Google Scholar] [PubMed] [CrossRef]
Li J, Huang W, Zhang H, Wang X, Zhou H (2007). Synthesis of andrographolide derivatives and their TNF-α and IL-6 expression inhibitory activities. Bioorganic & Medicinal Chemistry Letters 17: 6891–6894. https://doi.org/10.1016/j.bmcl.2007.10.009 [Google Scholar] [PubMed] [CrossRef]
Logeswari J, Shankar S, Biswas PG, Muninathan N (2020). Role of medicinal plants in the prevention of COVID-19 pandemic. Medico-Legal Update 20: 2305–2308. [Google Scholar]
Lv H, She G (2010). Naturally occur diarylheptanoids. Natural Products Communications: 1687–1708. https://doi.org/10.1177/1934578X1000501035 [Google Scholar] [CrossRef]
Maideen NM (2021). Therapeutic efficacy of Kabasura Kudineer (siddha formulationin COVID-19–A review of clinical and molecular docking studies. Asian Journal of Advances in Research 14: 68–75. https://mbimph.com/index.php/AJOAIR/article/view/2362. [Google Scholar]
Majnooni MB, Fakhri S, Shokoohinia Y, Kiyani N, Stage K, Mohammadi P, Gravandi MM, Farzaei MH, Echeverría J (2020). Phytochemicals: Potential therapeutic interventions against coronavirus-associated lung injury. Frontiers in Pharmacology 11: 588467. https://doi.org/10.3389/fphar.2020.588467 [Google Scholar] [PubMed] [CrossRef]
Mao QQ, Xu XY, Cao SY, Gan RY, Corke H, Li HB (2019). Bioactive compounds and bioactivities of ginger (Zingiber officinale Roscoe). Foods 8: 185. https://doi.org/10.3390/foods8060185 [Google Scholar] [PubMed] [CrossRef]
Mehrotra N (2020). Medicinal plants, aromatic herbs and spices as potent immunity defenders: Antiviral (COVID-19) perspectives. Annals of Phytomedicine 9: 30–49. https://doi.org/10.21276/ap.2020.9.2.4 [Google Scholar] [CrossRef]
Mir SR, Ali M, Kapoor R (2004). Chemical composition of essential oil of Cinnamomum tamala Nees et Eberm. leaves. Flavour and Fragrance Journal 19: 112–114. https://doi.org/10.1002/ffj.1236 [Google Scholar] [CrossRef]
Mukherjee PK, Efferth T, Das B, Kar A, Ghosh S, Singha S, Debnath P, Sharma N, Bhardwaj PK, Haldar PK (2022). Role of medicinal plants in inhibiting SARS-CoV-2 and in the management of post-COVID-19 complications. Phytomedicine 98: 153930. https://doi.org/10.1016/j.phymed.2022.153930 [Google Scholar] [PubMed] [CrossRef]
Nadhan R, Patra D, Krishnan N, Rajan A, Gopala S, Ravi D, Srinivas P (2021). Perspectives on mechanistic implications of ROS inducers for targeting viral infections. The European Journal of Pharmacology 890: 173621. https://doi.org/10.1016/j.ejphar.2020.173621 [Google Scholar] [PubMed] [CrossRef]
Natarajan S, Anbarasi C, Sathiyarajeswaran P, Manickam P, Geetha S, et al. (2021). Kabasura Kudineer (KSKa poly-herbal Siddha medicine, reduced SARS-CoV-2 viral load in asymptomatic COVID-19 individuals as compared to vitamin C and zinc supplementation: Findings from a prospective, exploratory, open-labeled, comparative, randomized controlled trial, Tamil Nadu, India. Trials 22: 623. https://doi.org/10.1186/s13063-021-05583-0 [Google Scholar] [PubMed] [CrossRef]
Negi BS, Dave BP (2010). In vitro antimicrobial activity of Acacia catechu and its phytochemical analysis. Indian Journal of Microbiology 50: 369–374. https://doi.org/10.1007/s12088-011-0061-1 [Google Scholar] [PubMed] [CrossRef]
Nema NK, Mamdapur GM, Sarojam S, Khamborkar SD, Sajan LC, Sabu S, Chacko BK, Jacob V (2021). Preventive medicinal plants and their phytoconstituents against SARS-CoV-2/COVID-19. Pharmacognosy Reviews 13: 173–191. https://doi.org/10.5530/pres.13.4.10 [Google Scholar] [CrossRef]
Okhuarobo A, Falodun JE, Erharuyi O, Imieje V, Falodun A, Langer P (2014). Harnessing the medicinal properties of Andrographis paniculata for diseases and beyond: A review of its phytochemistry and pharmacology. Asian Pacific Journal of Tropical Disease 4: 213–222. https://doi.org/10.1016/S2222-1808(14)60509-0 [Google Scholar] [CrossRef]
Padalia RC, Verma RS (2011). Comparative volatile oil composition of four Ocimum species from Northern India. Natural Product Research 25: 569–575. https://doi.org/10.1080/14786419.2010.482936 [Google Scholar] [PubMed] [CrossRef]
Palai S, Kesh SS (2021). Essential oils: An effective therapeutic strategy against SARS-CoV-2. International Journal of Bio-Resource & Stress Management 12: 719–724. https://doi.org/10.23910/1.2021.2656a [Google Scholar] [CrossRef]
Panda AK, Kar S, Rai AK, Rao BC, Srikanth N (2022). AYUSH-64: A potential therapeutic agent in COVID-19. Journal of Ayurveda and Integrative Medicine 4: 100538. https://doi.org/10.1016/j.jaim.2021.100538 [Google Scholar] [PubMed] [CrossRef]
Pandey P, Singhal D, Khan F, Arif M (2020). An in silico screening on Piper nigrum, Syzygium aromaticum and Zingiber officinale roscoe derived compounds against SARS-CoV-2: A drug repurposing approach. Biointerface Research in Applied Chemistry 11: 11122–11134. https://doi.org/10.33263/BRIAC [Google Scholar] [CrossRef]
Parasuraman S, Thing GS, Dhanaraj SA (2014). Polyherbal formulation: Concept of ayurveda. Pharmacognosy Reviews 8: 73–80. https://doi.org/10.4103/0973-7847.134229 [Google Scholar] [PubMed] [CrossRef]
Parihar S (2022). Anti-viral activity of Withania somnifera phytoconstituents against corona virus (SARS-COV-2). Journal of Pharmacovigilance and Drug Research 3: 22–26. https://doi.org/10.53411/jpadr.2022.3.2.5 [Google Scholar] [CrossRef]
Park JY, Yuk HJ, Ryu HW, Lim SH, Kim KS, Park KH, Ryu YB, Lee WS (2017). Evaluation of polyphenols from Broussonetia papyrifera as coronavirus protease inhibitors. Journal of enzyme inhibition and medicinal chemistry 32: 504–512. https://doi.org/10.1080/14756366.2016.1265519 [Google Scholar] [PubMed] [CrossRef]
Pathak R, Sharma H (2021). A review on medicinal uses of Cinnamomum verum (Cinnamon). Journal of Drug Delivery and Therapeutics 11: 161–166. https://doi.org/10.22270/jddt.v11i6-S.5145 [Google Scholar] [CrossRef]
Percival SS (2016). Aged garlic extract modifies human immunity. The Journal of Nutrition 146: 433S–436S. https://doi.org/10.3945/jn.115.210427 [Google Scholar] [PubMed] [CrossRef]
Prasathkumar M, Anisha S, Dhrisya C, Becky R, Sadhasivam S (2021). Therapeutic and pharmacological efficacy of selective Indian medicinal plants—A review. Phytomedicine Plus 1: 100029. https://doi.org/10.1016/j.phyplu.2021.100029 [Google Scholar] [CrossRef]
Premanathan M, Rajendran S, Ramanathan T, Kathiresan K (2000). A survey of some Indian medicinal plants for anti-human immunodeficiency virus (HIV) activity. Indian Journal of Medical Research 112: 73–77. [Google Scholar] [PubMed]
Qadir MM, Bhatti A, Ashraf MU, Sandhu MA, Anjum S, John P (2018). Immunomodulatory and therapeutic role of Cinnamomum verum extracts in collagen-induced arthritic BALB/c mice. Inflammopharmacology 26: 157–170. https://doi.org/10.1007/s10787-017-0349-9 [Google Scholar] [PubMed] [CrossRef]
Radhika AG, Malik H (2021). Fight against COVID-19: Survey of Spices & Herbs used in North India. Open Journal of Epidemiology 11: 256–266. https://doi.org/10.4236/ojepi.2021.113022 [Google Scholar] [CrossRef]
Raina D, Raina S, Singh B (2021). Katuki Picrorhiza Kurroa–A promising Ayurvedic Herb. Biomedical Journal of Scientific & Technical 36: 28238–28242. https://doi.org/10.26717/BJSTR.2021.36.005805 [Google Scholar] [CrossRef]
Rathinavel T, Palanisamy M, Srinivasan P, Subramanian A, Thangaswamy S (2020). Phytochemical 6-Gingerol–A promising drug of choice for COVID-19. International Journal on Advanced Science, Engineering and Information Technology 6: 1482–1489. https://doi.org/10.29294/IJASE.6.4.2020.1482-1489 [Google Scholar] [CrossRef]
Ravi Kumar V, Garg R, Kumar M, Kumar D, Hussain T et al. (2020). Queen of herbs tulsi (Ocimum Sanctum) immunomodulatory activities and systemic symptomatic treatment of novel coronavirus (COVID-19). Clinical Pharmacology and Biopharmaceutics 9: 1000208. [Google Scholar]
Rifa’i M, Satwika D, Aulanni AM (2014). Datura metel linn ameliorates asthma symptoms in BALB/c mice. Journal of Bio-Science 22: 1–8. https://doi.org/10.3329/jbs.v22i0.30002 [Google Scholar] [CrossRef]
Ritesh MA, Roushan R (2021). Amalgamation of ayurveda with allopathy: A synergistic approach for COVID-19 treatment. IJCMCR 17: 4. https://doi.org/10.46998/IJCMCR.2021.17.000419 [Google Scholar] [CrossRef]
Rizvi ZA, Tripathy MR, Sharma N, Goswami S, Srikanth N, et al. (2021). Effect of prophylactic use of intranasal oil formulations in the hamster model of COVID-19. Frontiers in Pharmacology 12: 102884. https://doi.org/10.3389/fphar.2021.746729 [Google Scholar] [PubMed] [CrossRef]
Ross ZM, O’Gara EA, Hill DJ, Sleightholme HV, Maslin DJ (2001). Antimicrobial properties of garlic oil against human enteric bacteria: Evaluation of methodologies and comparisons with garlic oil sulfides and garlic powder. Applied and Environmental Microbiology 67: 475–480. https://doi.org/10.1128/AEM.67.1.475-480.2001 [Google Scholar] [PubMed] [CrossRef]
Sa-Ngiamsuntorn K, Suksatu A, Pewkliang Y, Thongsri P, Kanjanasirirat P et al. (2021). Anti-SARS-CoV-2 activity of Andrographis paniculata extract and its major component Andrographolide in human lung epithelial cells and cytotoxicity evaluation in major organ cell representatives. Journal of Natural Products 84: 1261–1270. https://doi.org/10.1021/acs.jnatprod.0c01324 [Google Scholar] [PubMed] [CrossRef]
Sachan S, Dhama K, Latheef SK, Samad HA, Mariappan AK et al. (2019). Immunomodulatory potential of Tinospora cordifolia and CpG ODN (TLR21 agonist) against the very virulent, infectious bursal disease virus in SPF chicks. Vaccines 7: 106. https://doi.org/10.3390/vaccines7030106 [Google Scholar] [PubMed] [CrossRef]
Sagar V, Kumar AH (2020). Efficacy of natural compounds from Tinospora cordifolia against SARS-CoV-2 protease, surface glycoprotein and RNA polymerase. BEMS Reports 6: 6–8. https://doi.org/10.5530/bems.6.1.2 [Google Scholar] [CrossRef]
Saggam A, Limgaokar K, Borse S, Chavan-Gautam P, Dixit S, Tillu G, Patwardhan B (2021). Withania somnifera (L.) Dunal: Opportunity for clinical repurposing in COVID-19 management. Frontiers in Pharmacology 12: 27. https://doi.org/10.3389/fphar.2021.623795 [Google Scholar] [PubMed] [CrossRef]
Sahoo MR, Srinivasan UM, Varier RR (2022). Development and evaluation of Talisapatradi and Vyoshadi choorna lozenges: An ayurvedic traditional formulation. Journal of Reports in Pharmaceutical Sciences 11: 110–117. https://doi.org/10.4103/jrptps.JRPTPS_80_21 [Google Scholar] [CrossRef]
Sarkar L, Oko L, Gupta S, Bubak AN, Das B et al. (2022). Azadirachta indica A. Juss bark extract and its Nimbin isomers restrict β-coronaviral infection and replication. Virology 569: 13–28. https://doi.org/10.1016/j.virol.2022.01.002 [Google Scholar] [PubMed] [CrossRef]
Shang A, Cao SY, Xu XY, Gan RY, Tang GY, Corke H, Mavumengwana V, Li HB (2019). Bioactive compounds and biological functions of garlic (Allium sativum L.). Foods 8: 246. https://doi.org/10.3390/foods8070246 [Google Scholar] [PubMed] [CrossRef]
Sharma P, Dwivedee BP, Bisht D, Dash AK, Kumar D (2019). The chemical constituents and diverse pharmacological importance of Tinospora cordifolia. Heliyon 5: e02437. https://doi.org/10.1016/j.heliyon.2019.e02437 [Google Scholar] [PubMed] [CrossRef]
Sherin DR, Manojkumar TK (2022). Potential drug leads for SARS-CoV2 from phytochemicals of Aerva lanata: An in silico approach. Authorea Preprints 1: 1–18. https://doi.org/10.22541/au.164865036.63209674/v1 [Google Scholar] [CrossRef]
Shree P, Mishra P, Selvaraj C, Singh SK, Chaube R et al. (2022). Targeting COVID-19 (SARS-CoV-2) main protease through active phytochemicals of ayurvedic medicinal plants-Withania somnifera (AshwagandhaTinospora cordifolia (Giloy) and Ocimum sanctum (Tulsi)–a molecular docking study. Journal of Biomolecular Structure and Dynamics 40: 190–203. https://doi.org/10.1080/07391102.2020.1810778 [Google Scholar] [PubMed] [CrossRef]
Shrestha A, Marahatha R, Regmi B, Dahal SR, Basnyat RC et al. (2022). Molecular docking and dynamics simulation of several flavonoids predict Cyanidin as an effective drug candidate against SARS-CoV-2 spike protein. Advances in Pharmacological and Pharmaceutical Sciences 2022: 1–13. https://doi.org/10.1155/2022/3742318 [Google Scholar] [PubMed] [CrossRef]
Singh RS, Singh A, Kaur H, Batra G, Sarma P et al. (2021). Promising traditional Indian medicinal plants for the management of novel Coronavirus disease: A systematic review. Phytotherapy Research 35: 4456–4484. https://doi.org/10.1002/ptr.7150 [Google Scholar] [PubMed] [CrossRef]
Soni KK, Lawal T, Wicks S, Patel U, Mahady GB (2015). Boswellia serrata and Ocimum sanctum extracts reduce inflammation in an ova-induced asthma model of BALB/c mice. Planta Medica 81: PB4. https://doi.org/10.1055/s-00000058 [Google Scholar] [CrossRef]
Stoner GD (2013). Ginger: Is it ready for prime time? Cancer Prevention Research 6: 257–262. https://doi.org/10.1158/1940-6207.CAPR-13-0055 [Google Scholar] [PubMed] [CrossRef]
Subapriya R, Nagini S (2005). Medicinal properties of neem leaves: A review. Current Medicinal Chemistry-Anti-Cancer Agents 5: 149–156. https://doi.org/10.2174/1568011053174828 [Google Scholar] [PubMed] [CrossRef]
Sundaram R, Ramanathan SM, Rajesh R, Satheesh B, Saravanan D (2012). LC-MS quantification of rosmarinic acid and ursolic acid in Therocimum sanc Linn. leaf extract (Holy Basal, Tulsi). Journal of Liquid Chromatography & Related Technologies 35: 634–650. https://doi.org/10.1080/10826076.2011.606583 [Google Scholar] [CrossRef]
Sánchez-Sánchez MA, Zepeda-Morales AS, Carrera-Quintanar L, Viveros-Paredes JM, Franco-Arroyo NN, Godínez-Rubí M, Ortuño-Sahagun D, López-Roa RD (2020). Alliin, an Allium sativum nutraceutical, reduces metaflammation markers in DIO mice. Nutrients 12: 624. https://doi.org/10.3390/nu12030624 [Google Scholar] [PubMed] [CrossRef]
Tsai YC, Lee CL, Yen HR, Chang YS, Lin YP, Huang SH, Lin CW (2020). Antiviral action of tryptanthrin isolated from strobilanthes cusia leaf against human coronavirus NL63. Biomolecules 10: 366. https://doi.org/10.3390/biom10030366 [Google Scholar] [PubMed] [CrossRef]
Ullah S, Munir B, Al-Sehemi AG, Muhammad S, Haq IU, Aziz A, Ahmed B, Ghaffar A (2022). Identification of phytochemical inhibitors of SARS-CoV-2 protease 3CLpro from selected medicinal plants as per molecular docking, bond energies and amino acid binding energies. Saudi Journal of Biological Sciences 29: 103274. https://doi.org/10.1016/j.sjbs.2022.03.024 [Google Scholar] [PubMed] [CrossRef]
Varshney KK, Varshney M, Nath B (2020). Molecular modeling of isolated phytochemicals from Ocimum sanctum towards exploring potential inhibitors of SARS coronavirus main protease and papain-like protease to treat COVID-19.https://ssrn.com/abstract=3554371. [Google Scholar]
Verma SK, Kumar A (2011). Therapeutic uses of Withania somnifera (Ashwagandha) with a note on withanolides and its pharmacological actions. Asian Journal of Pharmaceutical and Clinical Research 4: 1–4. [Google Scholar]
Xu H, Zhong L, Deng J, Peng J, Dan H, Zeng X, Li T, Chen Q (2020). High expression of ACE2 receptor of 2019-nCoV on the epithelial cells of oral mucosa. International Journal of Oral Science 12: 8. https://doi.org/10.1038/s41368-020-0074-x [Google Scholar] [PubMed] [CrossRef]
Yakhchali M, Taghipour Z, Mirabzadeh Ardakani M, Alizadeh Vaghasloo M, Vazirian M, Sadrai S (2021). Cinnamon and its possible impact on COVID-19: The viewpoint of traditional and conventional medicine. Biomedicine & Pharmacotherapy 143: 112221. https://doi.org/10.1016/j.biopha.2021.112221 [Google Scholar] [PubMed] [CrossRef]
Yamprasert R, Chanvimalueng W, Mukkasombut N, Itharat A (2020). Ginger extract versus Loratadine in the treatment of allergic rhinitis: A randomized controlled trial. BMC Complementary Medicine and Therapies 20: 119. https://doi.org/10.1186/s12906-020-2875-z [Google Scholar] [PubMed] [CrossRef]
Yu MS, Lee J, Lee JM, Kim Y, Chin YW, Jee JG, Keum YS, Jeong YJ (2012). Identification of myricetin and scutellarein as novel chemical inhibitors of the SARS coronavirus helicase, nsP13. Bioorganic and Medicinal Chemistry Letters 22: 4049–4054. https://doi.org/10.1016/j.bmcl.2012.04.081 [Google Scholar] [PubMed] [CrossRef]
Zahedipour F, Hosseini SA, Sathyapalan T, Majeed M, Jamialahmadi T, Al‐Rasadi K, Banach M, Sahebkar A (2020). Potential effects of curcumin in the treatment of COVID-19 infection. Phytotherapy Research 34: 2911–2920. https://doi.org/10.1002/ptr.6738 [Google Scholar] [PubMed] [CrossRef]
Cite This Article
 Copyright © 2023 The Author(s). Published by Tech Science Press.
Copyright © 2023 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF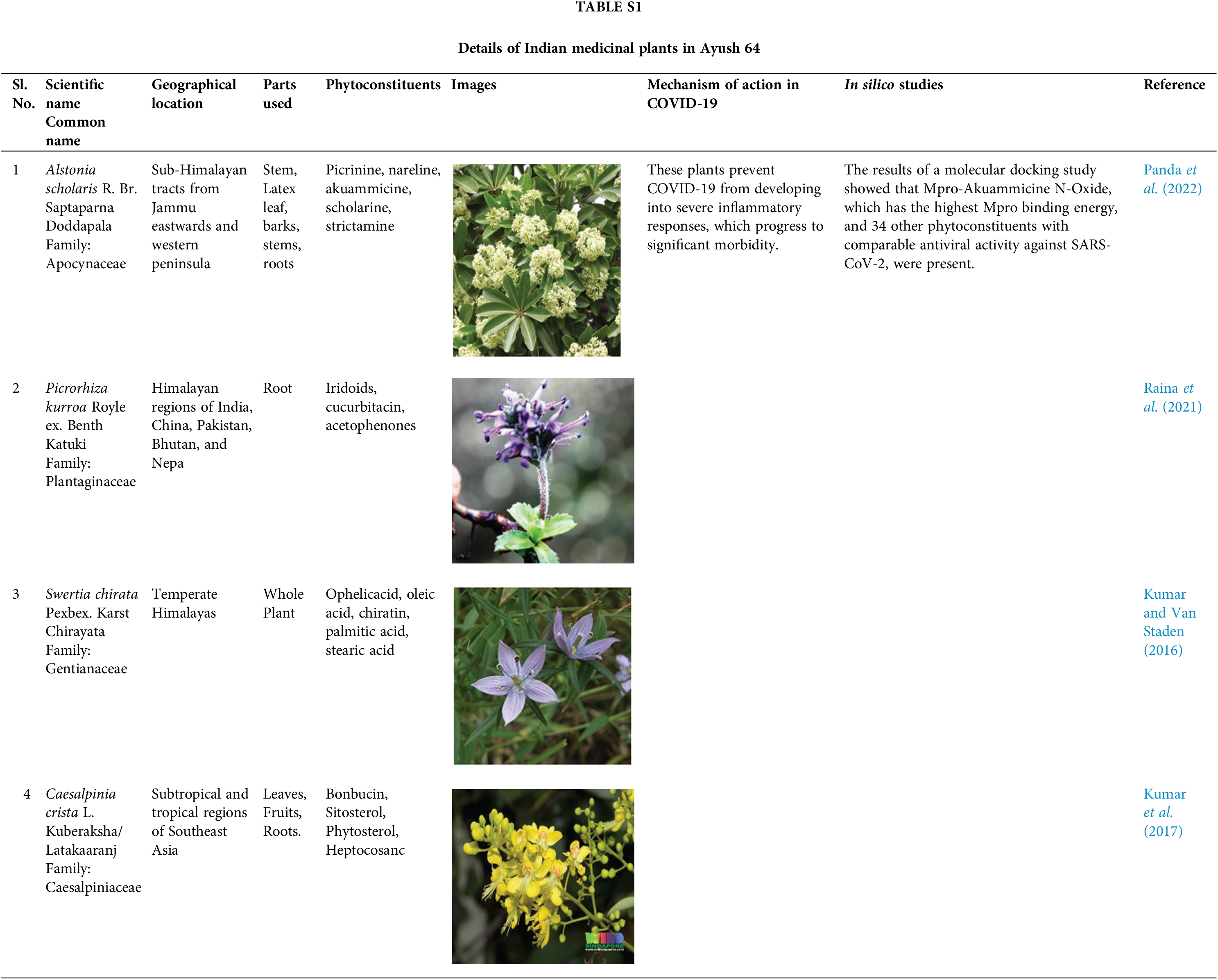

 Downloads
Downloads
 Citation Tools
Citation Tools