 Open Access
Open Access
ARTICLE
The Correlation between Psychological Resilience and Professional Quality of Life in Saudi Psychiatric Nurses: A Cross-Sectional Study
Community and Psychiatric Mental Health Nursing Department, College of Nursing, King Saud University, Riyadh, 12371, Saudi Arabia
* Corresponding Author: Ahmad M. Rayani. Email:
Psycho-Oncologie 2024, 18(4), 271-280. https://doi.org/10.32604/po.2024.056045
Received 12 July 2024; Accepted 02 September 2024; Issue published 04 December 2024
Abstract
In recent years, significant focus has been placed on resilience, with ongoing studies aiming to identify strategies for reducing the negative effects of job stress and protecting nurses from negative psychosocial outcomes. Nevertheless, as far as this topic is concerned, no research has yet been conducted in the context of Saudi psychiatric nurses. The aim of this research, therefore, is to determine how Saudi Arabian psychiatric nurses’ professional quality of life and psychological resilience relate to one another. To this aim, a cross-sectional study has been performed in Saudi Arabia incorporating a population of 167 (a 66.4% response rate) mental health nurses taken from the largest psychiatric hospital in the capital city Riyadh. Data collection was performed using the popular Arabic version of the Connor–Davidson Resilience and the Arabic version of the Professional Quality of Life Scales. To assess the variables related to both Professional Quality of Life and psychological resilience levels, statistical analyses such as Pearson correlation, ANOVA, t-tests, and linear regression were utilized. The findings show compassion satisfaction and burnout to have a moderate inverse relationship (r = −0.502), while compassion satisfaction (CS) and resilience have a moderate positive correlation (r = 0.594). Compared to their morning-shift counterparts, nurses working night shifts reported higher mean scores for resilience (72.70), CS (40.20), burnout (24.52), and compassion fatigue (CF) (28.11). Participants with less than five years’ experience in a psychiatric clinic had the highest mean resilience score (72.96). Finally, a positive relationship between resilience and compassion satisfaction (CS) was revealed using linear regression analysis (β = 0.536, t = 7.080, p = 0.000). The study reveals significant differences in the scores assigned to resilience and work-life quality based on educational qualifications, shift-work type, and experiences. Burnout and compassion satisfaction (CS) are found to be significantly correlated, as are compassion satisfaction (CS) and resilience, and burnout and compassion fatigue (CF).Keywords
As nurses’ duties involve unsociable working hours, dealing with difficult patients, and stressful encounters, the conditions in which they work are often suboptimal. Indeed, these working conditions are known to promote psychological vulnerability. The existing literature highlights how common stressors–including interpersonal conflict or tension, hostile patients, a high workload, and low income–influence nurses’ well-being and job satisfaction [1–3]. Due to the psychiatric problems their patients experience, psychiatric nurses deal with especially challenging situations when at work, such as confinement, verbal and physical abuse, and suicide attempts [4]. Moreover, a dangerous work environment manifests in situations where patients can act violently and aggressively toward nurses [5,6]. For organizations looking to retain talent in the mental health field, it is essential to focus on the professional life quality of psychiatric nurses to gain a deeper understanding of associated factors [4–6].
Professional quality of life relates to how employees feel about their working lives and their satisfaction with their job roles [7]. Burnout, compassion fatigue (CF), and compassion satisfaction (CS) all contribute to the professional quality of life of healthcare practitioners [8]. Individuals who care for traumatized patients often experience secondary traumatic stress brought about by the physical and psychological impact of the act of caring–known as CF [8]. Unlike the fatigue and stress one experiences with CF, burnout differs in its manifestation as emotional weariness, resulting from a diminished sense of accomplishment due to work-related stress and depersonalization [8].
CF has been reported as having the following effects on professionals: Job dissatisfaction, poor decision-making, feeling overworked, diminished ability to assist, lack of empathy, nonobjectivity, difficulties in maintaining a balance between empathy and objectivity, a lack of tolerance toward patients, and feelings of anxiety or aversion toward work [9–11]. In contrast, CS–the satisfaction of being able to assist others in need–is the outcome of a high professional quality of life. CS serves as a self-defense mechanism against CF and burnout [12]. According to studies on the impact of CS on nurses’ health, this factor offers considerable protection from the negative effects of chronic association with traumatized patients and exposure to occupational stressors [13].
Quality of work life is significantly impacted by several factors, including organizational, external, and personal aspects. In contrast, the behaviors and attitudes of an individual are a result of personal variables [14]. Resilience has received significant worldwide attention in recent years, becoming the focus of ongoing research into the identification of strategies for reducing the negative impacts of job stress and shielding nurses from negative psychosocial outcomes [15,16].
The term ‘resilience’ refers to the ability to quickly recover from any disaster by adapting to changing circumstances. It is seen as essential for overcoming the many stressors individuals may experience in their lives, such as threats, financial crises, catastrophes, substantial health concerns, interpersonal grief, etc. [17]. A person’s resilience is influenced by the potential risks they encounter in a workplace as well as their self-defense mechanisms. The importance of psychological health has been demonstrated and found to be particularly important for nursing, as the profession requires carrying out crucial care services for vulnerable patients who can pose numerous risk factors [17,18].
A study conducted in Saudi Arabia found 35.7% of its 213 participating nurses to be suffering from work-related stress [19]. Another study involving 160 psychiatric nurses working in two psychiatric hospitals reported higher levels of work-related stress when compared to nurses working in other departments [20]. Furthermore, work-related stressors and challenges may have a cumulative negative effect on the mental health of nurses in Saudi Arabia, which could result in states of chronic stress, emotional exhaustion, and probably patient stigmatization, post-traumatic stress disorder, and depression [1,21,22]. Continuous exposure to traumatic conditions, caused by various patient dynamics, may decrease the quality of nurses’ professional career trajectories and lead to undesirable patient outcomes [23]. It is, therefore, imperative to measure the professional quality of life of mental health nurses so that some proactive strategies can be formulated to help diminish any adverse effects of work-related stress.
In a previous open-label Saudi Arabian study, a significant correlation was identified between burnout and the factors of employment location, nursing department, and age. Notably, the presence of secondary traumatic stress was significantly associated with employment location and nursing department. In another previous study, high levels of CS and moderate levels of both burnout and secondary traumatic stress (STS) were noted among Saudi nurses [24]. Plus, a further study conducted on primary healthcare nurses found a high correlation between a high level of burnout and factors such as job stressors, age, educational level, and causes of workplace stress [25]. In a Turkish study, a significant correlation between mental health nurses’ professional ideals, compassion, fulfillment, and burnout was confirmed. Professional values, educational level, and time devoted to social activities turned out to be good predictors for burnout, as measured by the ProQOL [26]. A clear relationship between CS and burnout was also found in a similar study and, likewise, psychological resilience and burnout with CF [27]. A South African example showed that, when compared with other nursing specialties, mental health nurses experienced higher degrees of burnout and STS, together with lower degrees of CS [28]. Hence, it may prove quite discerning to conduct routine assessments for nurses regarding resilience, burnout, and ProQOL. Consequently, the design of educational programs aimed at enhancing the resilience and CS of nurses to reduce the extent of burnout is strongly recommended.
Psychiatric hospitals in Saudi Arabia provide mental health treatments as a fundamental component of a hospital-based healthcare model. In 2013, the hospital-community paradigm was adopted and a mental health action plan came into effect. Specifically, general hospitals and university hospitals provide inpatient care and polyclinic services. As of 2013, there were 21 psychiatric hospitals active and there are now 5 community mental health centers too, although full coverage across the country is still yet to be established [29]. Moreover, there are 12 psychiatric beds, 0.19 psychiatrists, and 0.39 psychiatric nurses per 100,000 individuals nationwide [29]. Compared to European nations, these rates are lower than average [30].
Psychiatric nurses’ responsibilities have changed in the 21st century both globally and in Saudi Arabia [31]. In contrast to affluent nations, Saudi Arabia has not made notable progress in the psychiatric nursing profession. There are three types of nurses in Saudi Arabia: enrolled nurses who have completed a vocational nursing program, registered nurses who have finished a general nursing undergraduate degree, and psychiatric nurses who have advanced certification or a graduate degree in psychiatric and mental health nursing. At present, 1176 nurses work in the field of mental health in Saudi Arabia [29].
The workload of psychiatric nurses has increased, yet even with this increase, there are still typically just five or six nurses working in each psychiatric clinic [29]. A recent study of the nursing practices of psychiatric nurses found that these nurses primarily focused on the physical needs of their patients by carrying out interventions, such as giving intravenous and oral medication. However, they were seldom involved in activities such as therapy, and milieu treatment was not carried out. This gap in provision can be attributed to a lack of qualified nurses, the large number of patients, and the amount of paperwork nurses must complete that falls outside the scope of nursing practice [32]. Also, because there are so few psychiatric nurses with graduate or doctoral degrees or certifications, those who work in psychiatric clinics tend to focus on meeting the physical requirements of patients rather than using more sophisticated therapies such as counseling and psychoeducation.
This study investigates the psychological resilience–ProQOL relationship present in mental health nurses–a relationship that has not been substantially explored. As mental health nursing is considered one of the most demanding and stressful professions, researching the factors contributing to nurses’ well-being has clear importance. Furthermore, this will be the first study of its kind to examine predictors for the different aspects of Professional Quality of Life. Such information can help in designing interventions and support systems to promote the mental well-being and job satisfaction of nurses. This study intends to fill this knowledge gap by assessing the relationship between psychological resilience and ProQOL among the population of mental health nurses working in the Central Region of Saudi Arabia. It also aims to determine the degree of psychological resiliency and the extent of ProQOL domains, as well as examine their associations.
Research design and participants
This cross-sectional, correlated, and descriptive study was carried out between July and August 2023. Psychiatric nurses employed by the largest psychiatric hospital in Saudi Arabia’s capital city were recruited using purposive sampling. The largest psychiatric hospital works to treat and heal addiction patients, treat mental disorders, and provide therapeutic counseling to patients’ families [33]. All participants were registered nurses over 18 years of age who were employed in inpatient services. Nurses who worked in outpatient services, such as treatment centers and rehabilitation centers, were excluded from the study.
Potential participants were informed of the study’s objectives, and consenting nurses working in the hospital’s acute, long-term psychiatric clinics and substance abuse treatment programs were asked to complete a questionnaire. The questionnaire was completed by 167 nurses out of 250, resulting in a response rate of 66.4. Fifty-five nurses were excused for not being present during the data-collecting process owing to summer break, and 28 opted to drop out for other reasons. When considering the possibility of multiple regressions, a 121 sample size was required based on the previously described effect size of 0.39 [34]. Small, medium, and large effect sizes were set at 0.15, 0.39, and 0.59, respectively. To achieve the minimum level of 0.8 statistical power, the model included 11 variables and a 0.05 significance level.
The Professional Quality of life Scale Version 5 (ProQOL 5)
An Arabic version of the Professional Quality of Life Scale Version 5 (ProQOL 5), which was first introduced by Stamm [8] was used to assess the nurses’ professional quality of life [35]. The questionnaire consisted of 3 sets of 10 items, which were designed to assess specific measures on the ProQOL subscales of CS, CF, and burnout. Participants were asked to rate each measure on a five-point Likert scale ranging from 1 (never) to 5 (always/too often), with five items reverse-scored. Each subscale’s overall score was classified as either high (≥41), moderate (23–41), or low (≤22). The Cronbach’s α for the Arabic version of ProQOL 5 were as follows: 0.74 for the overall scale, 0.88 for the CS subscale, 0.67 for the CF subscale, and 0.79 for the burnout subscale.
The Connor-Davidson Resilience Scale (CD-RISC)
The study uses Connor-Davidson Resilience Scale (CD-RISC) standardized into Arabic language by Toma and was originally introduced by Connor ad Davidson, was used to evaluate the nurses’ psychological resilience [36]. The participants are asked to respond using a five-point Likert scale on a set of 25 items and choosing the rating between 0 (non true at all) to 4 (true nearly all the time). The scale consisted of three subscales: personal competence, tolerance for negative emotions, and spiritual inclinations. The total CD-RISC scores ranged from 0 to 100. In the current study, the 25 items were assessed holistically to obtain a single score. Higher resilience is represented by high scores on the CD-RISC. The CD-RISC’s Cronbach’s alpha in this study was 0.91.
Survey data was analyzed using the IBM Statistical Package for Social Sciences Version 28.0. The tool developer’s and adapter’s recommendations were used to calculate the scores for all scales and subscales. Descriptive statistics were employed to glean insights into the participants’ demographic data, CF, CS, burnout, and psychological resilience level. Using Pearson correlation analysis and linear regression, the strength of the correlations between CF, burnout, CS, and psychological resilience was determined. To identify the demographic differences in the participant characteristics, ProQOL 5 scores, and CD-RISC scores, an analysis of variance (ANOVA) and t-tests were used. The level of statistical significance was set at p < 0.05.
The King Saud University Institutional Review Board approved the study (Ref. No. 23/0330/IRB). All participants signed an electronic informed consent form before taking part in the study.
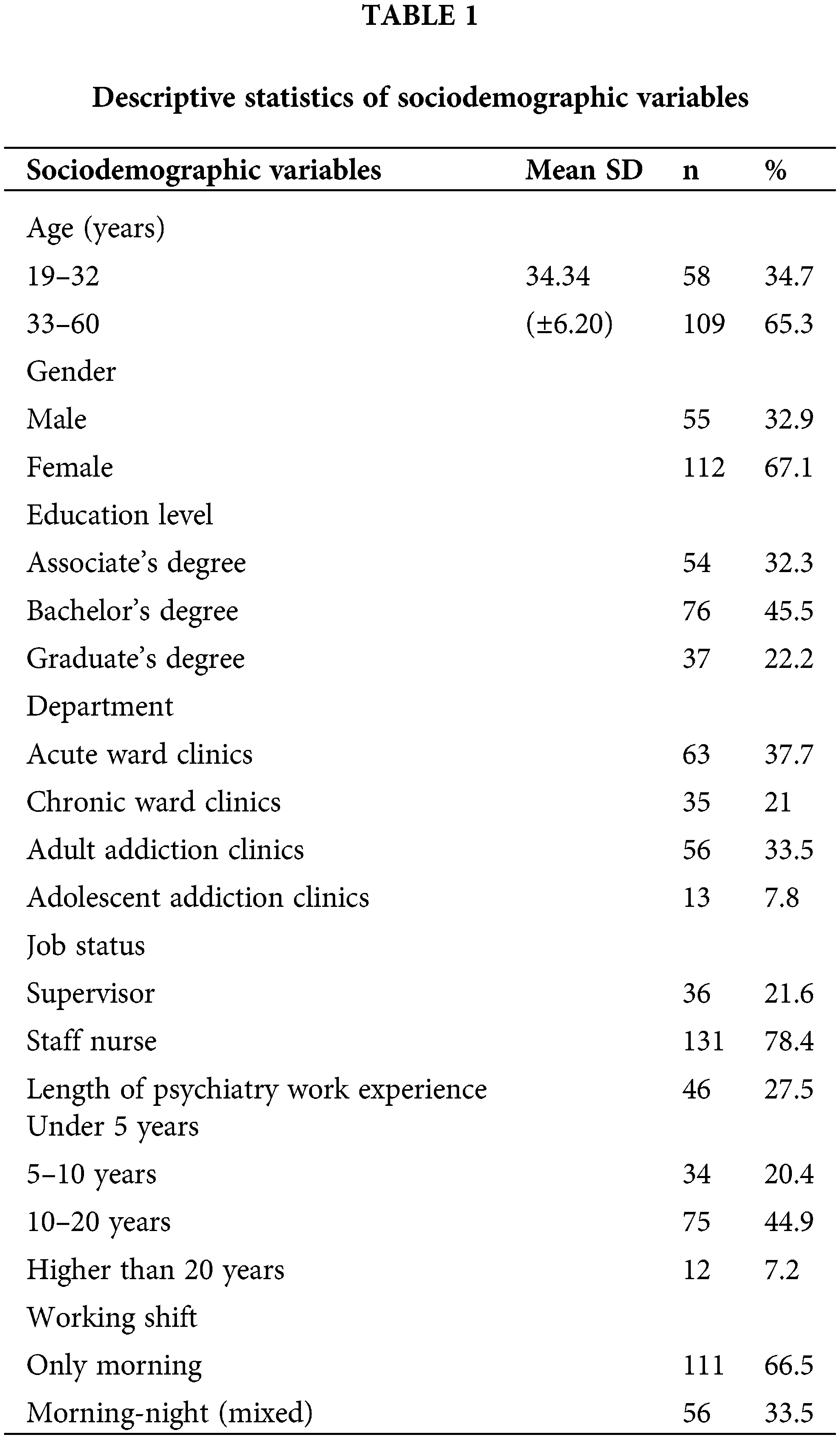
The surveys were completed by 167 psychiatric nurses whose demographic profile revealed an average age of 34.34 ± 6.20 years with an overall age range spanning from 19 to 60 years. The majority of participants were female (67.1%, n = 112), and nearly half (45.5%, n = 76) held a bachelor’s degree. The largest proportion worked as staff nurses (78.4%) in acute ward clinics (37.7%) with approximately two-thirds (66.5%) exclusively assigned to morning shifts (see Table 1).
Resilience and professional quality of life scores
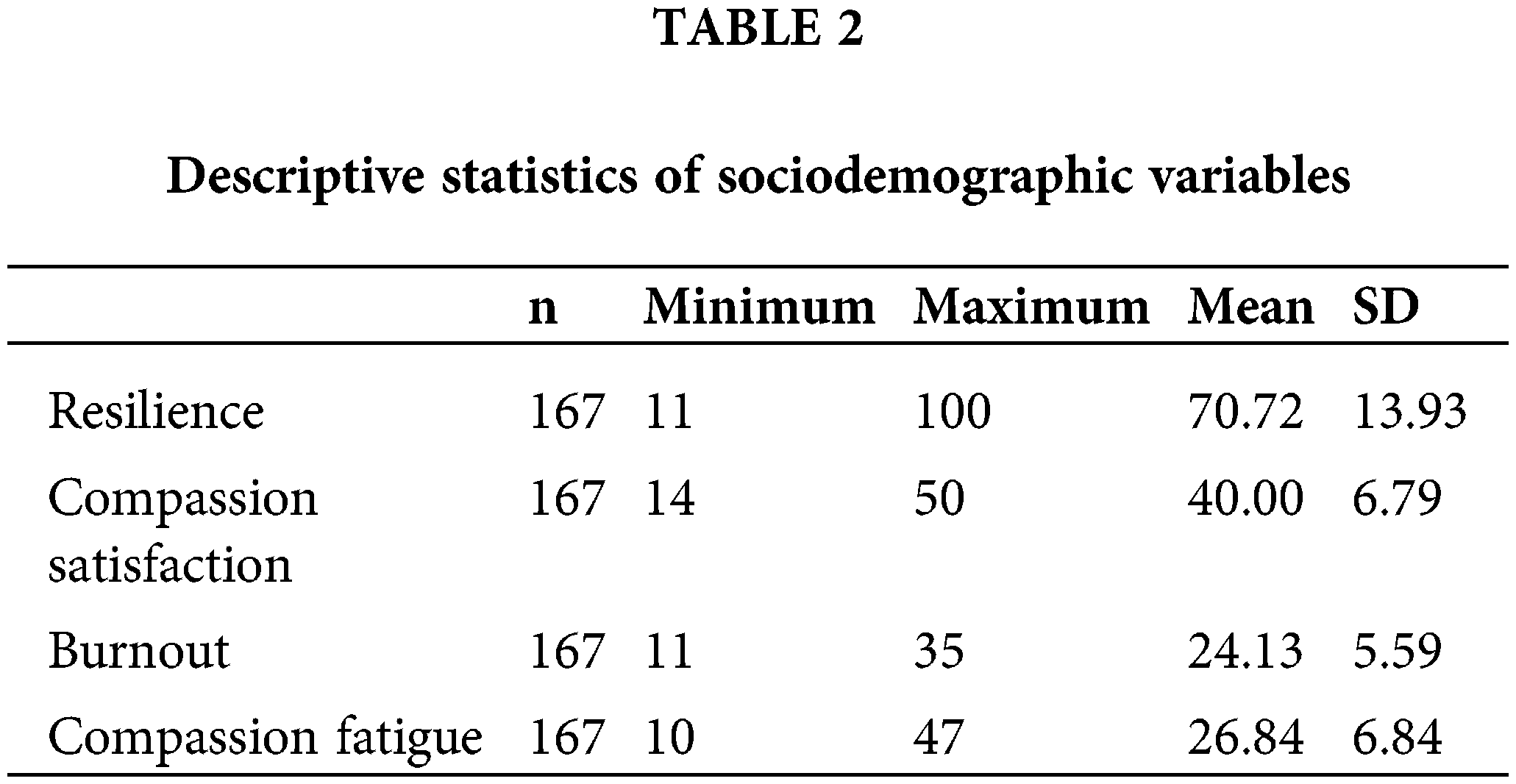
Table 2 displays the mean scores for professional quality of life and resilience, together with the corresponding subscales. The resilience scale utilizes a Likert-type rating system ranging from 0 to 4, which resulted in cumulative scores out of 100. The average resilience score of the participants was 70.72 ± 13.93 (range = 11–100). The Professional Quality of Life Scale comprised three subscales: CS with a mean score of 40 ± 6.79 (range = 14–50), burnout with a mean score of 24.13 ± 5.59 (range = 11–35), and CF/secondary trauma with a mean score of 26.84 ± 6.84 (range = 10–47).
The association between resilience, professional quality of life, and sociodemographic factors
The interaction of the scales with sociodemographic factors like age, hospital department, gender, education, job status, amount of work experience, and shift was examined (Table 3).
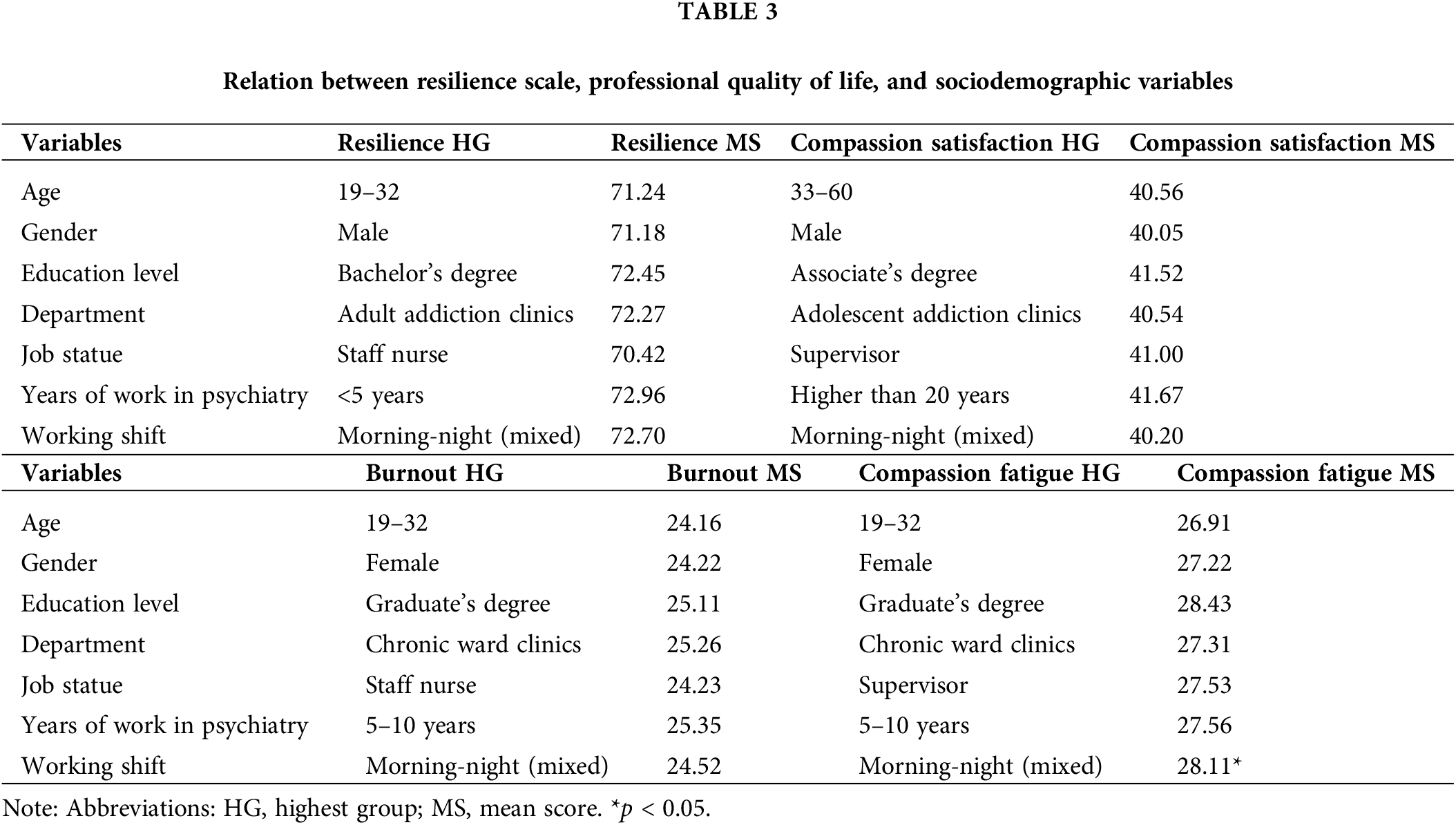
For age, the scales didn’t appear to be significantly correlated. Insignificant differences were found when participants were sub-grouped based on the reference mean age, with the scores remaining remarkably similar.
Compared to females, males psychiatric nurses scored high on resilience (71.18) and CS (40.05). Conversely, female psychiatric nurses reported higher scores for the burnout and CF scales. No statistically significant differences between genders across the scales were detected.
The psychiatric nurses educated to bachelor’s degree level attained the highest mean resilience scores (72.45). Graduate participants’ scores were the highest for burnout (25.11) and CF (28.43), while associate degree holders recorded the highest CS scores (41.52). Notably, there were no statistically significant variations between education levels.
The scores from all hospital departments revealed that, as per expectations regarding chronically stressed environments, psychiatric nurses exhibit the lowest resilience scores, alongside relatively high scores of CF and burnout. Conversely, psychiatric nurses assigned to chronic ward clinics recorded the lowest CS scores. However, no statistically significant inter-departmental variations were identified.
For both CS (40.00) and CF (27.53), supervisory nurses–which included department directors and administrators–received higher scores than staff nurses. Ward nurses had higher burnout (24.23) and resilience (70.42) scores, yet no statistically significant differences across the subscales were observed.
Working experience in psychiatric clinics
Burnout (25.35) and CF (27.56) were highest in psychiatric nurses with 5–10 years of clinic-based experience. Participants with less than five years of psychiatric clinic experience achieved the highest mean resilience score (72.96). Nonetheless, no statistically significant differences or correlations were detected between work experience and the scales.
Nurses working night shifts reported higher mean scores for resilience, CS, burnout, and CF when compared to their morning-shift counterparts. Mixed-shift nurses experienced the highest burnout mean scores during morning-night shift rotations. Statistically significant differences were apparent in the participants’ CF scores (p = 0.045).
The resilience scale and professional quality of life correlation
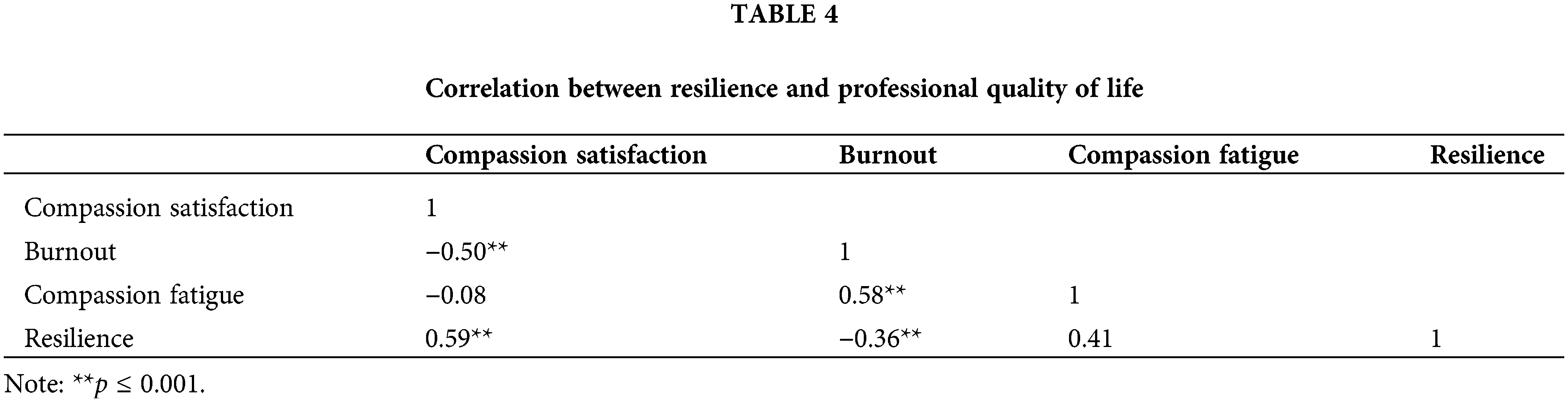
The relationships shared between resilience and professional quality of life are listed in Table 4. The results reveal that CS and burnout share a moderate inverse relationship (r = −0.502), while CS and resilience share moderate positive correlations (r = 0.594), and burnout and CF (r = 0.580). Furthermore, burnout and resilience were found to have a marginally negative relationship (r = −0.362).
The resilience scale and professional quality of life relationship
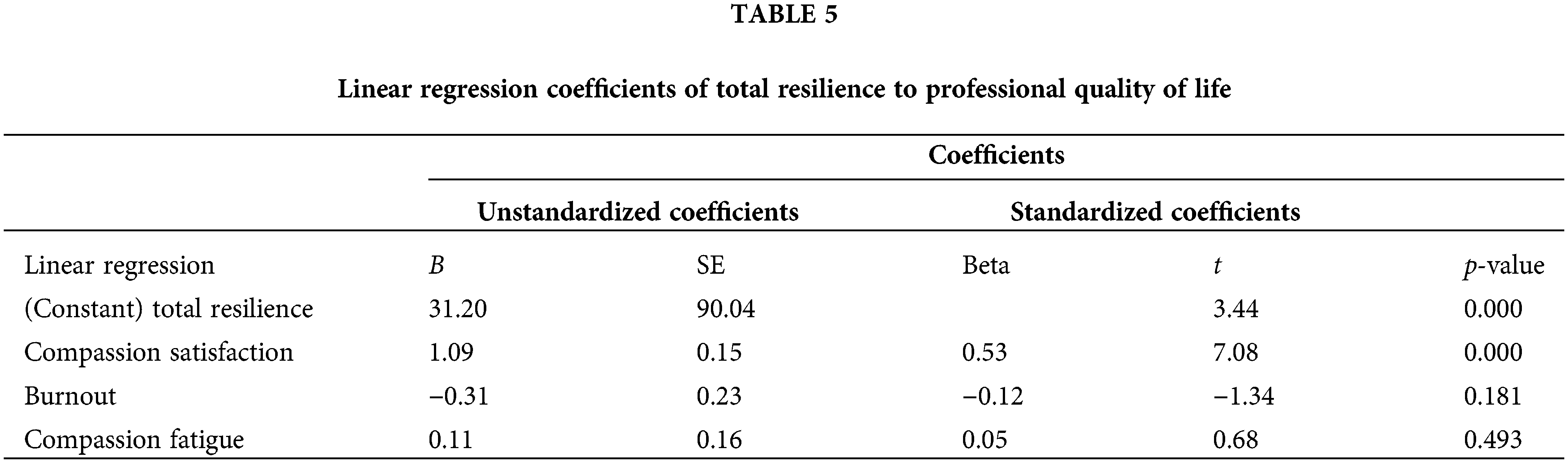
The use of linear regression analysis revealed a positive relationship between resilience and CS (β = 0.536, t = 7.080, p = 0.000). This suggests that CS increases along with resilience levels (further details are presented in Table 5).
The primary goal of this research is to examine the links between professional quality of life and psychological resilience. In doing so, the results have substantiated the anticipated inverse association between participants’ burnout levels and both CS and resilience. In essence, nurses demonstrating elevated psychological resilience and higher CS levels reported lower burnout experiences. Notably, a moderate positive correlation was observed between CF and burnout. Up to this point, few studies have examined the psychological resilience and quality of life of psychiatric nurses. Similarly, nursing research links the variables of psychological resilience and professional quality of life (burnout and CS) [13,37]. Thus, it is postulated that, by bolstering CS, interventions targeting the enhancement of psychological resilience among nurses could alleviate burnout.
The average score for the psychological resilience of study participants was 70.72 ± 13.93, which is similar to previous studies conducted among psychiatric nurses in Iran [38], psychiatric nurses in Turkey [27], mental healthcare nurses in the United States [39], and mental health nurses in Saudi Arabia [21]. Moreover, in the current work, CS, burnout, and CF had computed mean scores of 40.00 ± 6.79, 24.13 ± 5.59, and 26.84 ± 6.84, respectively. In a study involving 160 psychiatric nurses, Tirgari et al. [11] reported the mean CS, burnout, and CF scores as 23.40 ± 6.20, 27.17 ± 4.63, and 22.95 ± 6.32, respectively. Mangoulia et al. [40] found similar patterns in their study of 174 psychiatric nurses. Our results indicate that psychiatric nurses in Saudi Arabia tend to exhibit moderate levels of CS, burnout, and CF. It is crucial to note, however, that the ratio of qualified nursing staff per 100,000 individuals in Saudi Arabia is notably lower than in European countries [41]. Consequently, the workloads faced by psychiatric nurses in this study are considerably higher.
Nurses in psychiatric clinics face an array of challenges, including caring for mentally disordered individuals at risk of self-harm and experiencing verbal and physical aggression. The multifaceted responsibilities in restrictive settings, coupled with feelings of fear and guilt and the need to maintain communication with patients’ caregivers, can exact a significant emotional toll [17,42,43]. Additionally, the need to manage interpersonal conflicts and bullying among colleagues within psychiatric clinics contributes to psychosocial distress [17,44]. Organizational issues such as inadequate support, limited resources, deficient management, a surge in acute patients, and overwhelming workloads also exacerbate stress among psychiatric nurses [45–47]. Collectively, these factors can drive emotional exhaustion and burnout, triggering both physical and mental health issues [48]. Burnout can pave the way for insomnia, headaches, reduced focus, chronic fatigue, and irritability. In turn, these factors may compromise the quality of care the nurse can deliver, together with the associated patient satisfaction. All of which has the potential to result in a number of errors, at the same time causing higher morbidity and mortality rates [48].
Excessive workloads, work-related stress, being female, marital status, and workplace aggression are all reported to significantly contribute to burnout among mental health nurses [12]. Crucially, key aspects of psychological resilience can become negatively correlated with burnout and psychological health issues [49]. In response, this study underscores that fostering psychological resilience in nurses, particularly those in clinical roles, not only safeguards against emotional exhaustion but also boosts effectiveness. It is also recognized that nurses in clinical settings often overlook their own emotional needs, resulting in CF [12]. A meta-analysis has revealed a positive correlation between stress and CF, while positive emotions and socialization are identified as linked with increased CS [50].
The current study results also support the findings that CF has a positive relationship with burnout, while CS has an inverse relationship [50]. Furthermore, computer science has emerged as a significant predictor of psychological resilience. Hence, the promotion and development of psychological resilience will help to decrease the harmful effects of burnout and compassion fatigue, as well as enhance computer science skills. In light of this, the introduction of strategies aimed at increasing psychological resilience levels among nurses is suggested to decrease burnout by furthering cognitive abilities. A study conducted in Turkey, consisting of results taken from 100 psychiatric nurses, reported a positive correlation between CS and resilience and a negative correlation between CS and burnout [27]. The same results were replicated among mental health nurses in Saudi Arabia [21].
Mirroring previous research, our study’s female psychiatric nurses recorded notably higher CF and burnout scores than their male counterparts [48,51]. In contrast, male nurses reported elevated CS levels compared with their female peers and lower CF scores [52]. However, given that the nursing workforce in Saudi Arabia predominantly comprises women, the findings could be influenced by these dynamics. Furthermore, women tend to display heightened emotional responsiveness and form stronger empathic relationships, which possibly contributes to increased CF [53]. Additionally, evolutionarily speaking, women are inherently more nurturing–a trait that aligns with enhanced CS. Also, cultural gender roles may play a part in shaping these results too.
Exploring these dynamics further shows that, contrary to what is currently known in the literature, nurses who attended vocational nursing schools did not significantly outperform those from other types of educational backgrounds in terms of psychological resilience scores [54]. The prevailing literature does suggest a positive relationship between education level and psychological resilience, associating higher levels of education with greater capability in this respect [54]. This relationship could be attributed to diverse factors, including greater autonomy, better problem-solving skills, and improved coping mechanisms being present among more highly educated nurses [55]. Thus, nursing managers could consider tailored interventions to boost psychological resilience in nurses, particularly for those with undergraduate educations.
Moreover, this study has identified another element of influence: shift work–also supported by Tucker et al. [56]. Indeed, shift work may lead to physical and psychological fatigue among nurses; lowering ProQoL as a consequence, i.e., the Professional Quality of Life of nurses [57]. Clinically, this implies that nursing managers should be fully aware of the moderate degree of CF that exists among psychiatric ward nursing staff [58]. Results show that the introduction of shift-work schedules improves nurse performance. For the sake of ProQoL, therefore, necessary measures should be taken to strengthen a nursing team set-up by increasing the number of psychiatric nurses. Last but not least, this research presents critical details of the difficulties that psychiatric nurses in Saudi Arabia face with heavy workloads, workplace violence, and multiple other telling stressors.
In conclusion, this study offers vital insights into the challenges faced by psychiatric nurses in Saudi Arabia who grapple with heavy workloads, workplace violence, and numerous other stressors. The findings underscore the significance of promoting psychological resilience to mitigate the detrimental effects of burnout and CF while augmenting CS. There is evidence that teaching strategies such as self-hypnosis, social and peer support, and positive self-affirmation can actually increase the resilience of nurses, helping them cope with adversity and symptomatically reducing compassion fatigue and burnout [59,60]. In response, by enhancing nurses’ psychological well-being, healthcare institutions can enhance the quality of patient care and overall nursing outcomes.
This research is not without its limitations. Firstly, due to the adoption of a cross-sectional design, the insights are exclusively limited to the sample participants surveyed during the data collection period. Secondly, the study’s focus on a single setting impairs the generalizability of the findings, meaning they might not prove as applicable to psychiatric nurses in other healthcare institutions and hospitals. Additionally, the study uses purposive sampling, which may introduce sampling bias and affect sample representativeness. Nevertheless, it is noteworthy that the hospital selected for this research–located in Saudi Arabia’s capital city Riyadh–represents a significant nexus for psychiatric nurses and patients nationwide. As such, a cautious generalization of the results can be considered. In Saudi culture, participation in research is generally hampered by concerns regarding time (i.e., how time-consuming participation may be) and anonymity issues. Despite assurances of anonymity, professionals like nurses might choose to abstain from participation due to workload pressures or apprehensions surrounding anonymous result reporting. These factors may have collectively constrained our participant count to 167. Furthermore, one of the significant limitations of this study may be the potential for response bias, as nursing professionals may be inclined to provide more socially acceptable responses than is actually the case.
Significant differences have been revealed in the scores assigned to resilience and quality of work life based on educational qualifications, shift-work type, experiences, employment status, and hospital department. Burnout and CS were found to be significantly correlated, as were CS and resilience, and burnout and CF.
Guided by the insights garnered from this study, future research should encompass larger and more diverse sample populations drawn from a range of hospitals to develop a more comprehensive overview of psychiatric nurses’ perceptions. The current data requires more research carried out with the aim of enhancing the resilience of the psychiatric nursing population and overall work-life quality.
In psychiatric clinics, medical and nursing directors are critical for promoting resilience, encouraging CF limitations, and combating nurse burnout. Prior research has discovered and made available various workplace resources to support nursing professionals in this manner [61]. It is imperative that psychiatric nurses be equipped with consultative tools that encompass strategies to cope with stress, a means of effectively communicating with patients and families, conflict resolution, ethical quandary management, quality self-care, and psychological resilience enhancement–all strategies focused on maintaining nurses’ physical and mental well-being [61]. Plus, in addition to consulting sessions, the establishment of support forums may be advantageous [61]. Also, to maintain psychological resilience and professional quality of life in a sustainable manner, it is crucial to ensure proper follow-up of interventions in support of psychiatric nurses.
Executive interventions spotlighting the fulfillment of psychiatric nurses’ needs, fostering a positive organizational culture, and nurturing nurses’ psychological resilience will ultimately elevate both general and professional quality of life among these nurses. This, in turn, will elevate nursing care standards and heighten patient and family satisfaction.
Acknowledgement: The author of this study extends his appreciation to the Researchers Supporting Project Number (RSPD2024R1032), King Saud University, Riyadh, Saudi Arabia.
Funding Statement: The author received no financial support for the research, authorship, and/or publication of this article.
Availability of Data and Materials: The data that support the findings of this study are available from the corresponding author, upon reasonable request.
Ethics Approval: The Institutional Review Board of King Saud University approved the research project (Ref. No. 23/0330/IRB). All participants signed an electronic informed consent form before taking part in the study.
Conflicts of Interest: The author declares that they have no conflicts of interest to report regarding the present study.
References
1. Paiva-Salisbury ML, Schwanz KA. Building compassion fatigue resilience: awareness, prevention, and intervention for pre-professionals and current practitioners. J Health Serv Psychol. 2022;48(1):39–46. doi:10.1007/s42843-022-00054-9. [Google Scholar] [PubMed] [CrossRef]
2. Paskarini I, Dwiyanti E, Syaiful DA, Syanindita D. Burnout among nurses: examining psychosocial work environment causes. J Public Health Res. 2023;12(1):22799036221147812. [Google Scholar] [PubMed]
3. Staempfli S, Lamarche K. Top ten: a model of dominating factors influencing job satisfaction of emergency nurses. Int Emerg Nurs. 2020;49:100814. doi:10.1016/j.ienj.2019.100814. [Google Scholar] [PubMed] [CrossRef]
4. Itzhaki M, Bluvstein I, Peles Bortz A, Kostistky H, Bar Noy D, Filshtinsky V, et al. Mental health nurse’s exposure to workplace violence leads to job stress, which leads to reduced professional quality of life. Front Psychiatr. 2018;9:59. doi:10.3389/fpsyt.2018.00059. [Google Scholar] [PubMed] [CrossRef]
5. Liu J, Gan Y, Jiang H, Li L, Dwyer R, Lu K, et al. Prevalence of workplace violence against healthcare workers: a systematic review and meta-analysis. Occup Environ Med. 2019;76(12):927–37. doi:10.1136/oemed-2019-105849. [Google Scholar] [PubMed] [CrossRef]
6. Sun L, Gao Y, Yang J, Zang X-Y, Wang Y-G. The impact of professional identity on role stress in nursing students: a cross-sectional study. Int J Nurs Stud. 2016;63:1–8. doi:10.1016/j.ijnurstu.2016.08.010. [Google Scholar] [PubMed] [CrossRef]
7. Stamm BH. The ProQOL manual: the professional quality of life scale: compassion satisfaction, burnout & compassion fatigue/secondary trauma scales. Baltimore, MD: Sidran; 2005. [Google Scholar]
8. Stamm B. The concise manual for the professional quality of life scale: the center for victims of torture. Available from: https://proqol.org/proqol-manual. [Accessed 2010]. [Google Scholar]
9. Ledoux K. Understanding compassion fatigue: understanding compassion. J Adv Nurs. 2015;71(9):2041–50. doi:10.1111/jan.2015.71.issue-9. [Google Scholar] [CrossRef]
10. Sorenson C, Bolick B, Wright K, Hamilton R. Understanding compassion fatigue in healthcare providers: a review of current literature. J Nurs Scholarsh. 2016;48(5):456–65. doi:10.1111/jnu.2016.48.issue-5. [Google Scholar] [CrossRef]
11. Tirgari B, Azizzadeh FM, Ebrahimpour M. Relationship between posttraumatic stress disorder and compassion satisfaction, compassion fatigue, and burnout in Iranian psychiatric nurses. J Psychosoc Nurs Mental Health Serv. 2019;57(3):39–47. doi:10.3928/02793695-20181023-02. [Google Scholar] [PubMed] [CrossRef]
12. López-López IM, Gómez-Urquiza JL, Cañadas GR, De la Fuente EI, Albendín-García L, Cañadas-De la Fuente GA. Prevalence of burnout in mental health nurses and related factors: a systematic review and meta-analysis. Int J Ment Health Nurs. 2019;28(5):1035–44. doi:10.1111/inm.v28.5. [Google Scholar] [CrossRef]
13. Hegney DG, Rees CS, Eley R, Osseiran-Moisson R, Francis K. The contribution of individual psychological resilience in determining the professional quality of life of Australian nurses. Front Psychol. 2015;6:1613. [Google Scholar] [PubMed]
14. Polat FN, Erdem R. Merhamet Yorgunluğu Düzeyinin Çalişma Yaşam Kalitesi İle İlişkisi: sağlik Profesyonelleri Örneği. Süleyman Demirel Üniv Sos Bilim Enstit Derg. 2017;26:291–312. [Google Scholar]
15. Badu E, O’Brien AP, Mitchell R, Rubin M, James C, McNeil K, et al. Workplace stress and resilience in the Australian nursing workforce: a comprehensive integrative review. Int J Ment Health Nurs. 2020;29(1):5–34. doi:10.1111/inm.v29.1. [Google Scholar] [CrossRef]
16. Delgado C, Upton D, Ranse K, Furness T, Foster K. Nurses’ resilience and the emotional labour of nursing work: an integrative review of empirical literature. Int J Nurs Stud. 2017;70:71–88. doi:10.1016/j.ijnurstu.2017.02.008. [Google Scholar] [PubMed] [CrossRef]
17. Foster K, Roche M, Delgado C, Cuzzillo C, Giandinoto JA, Furness T. Resilience and mental health nursing: an integrative review of international literature. Int J Ment Health Nurs. 2019;28(1):71–85. doi:10.1111/inm.2019.28.issue-1. [Google Scholar] [CrossRef]
18. Vanhove AJ, Herian MN, Perez AL, Harms PD, Lester PB. Can resilience be developed at work? A meta-analytic review of resilience-building programme effectiveness. J Occup Organ Psychol. 2016;89(2):278–307. doi:10.1111/joop.2016.89.issue-2. [Google Scholar] [CrossRef]
19. Batran A. Work related stress among Saudi Nurses working in intensive care units. Open J Nurs. 2019;9(11):1143–52. doi:10.4236/ojn.2019.911084. [Google Scholar] [CrossRef]
20. Khobrani AA, Alosaimi AK, Abbas KS, Alsheikhi SIA, Krdy FA. Professional quality of life among psychiatric and non-psychiatric nurses in Jeddah. Med Sci. 2023;27:e40ms2720. [Google Scholar]
21. Alonazi O, Alshowkan A, Shdaifat E. The relationship between psychological resilience and professional quality of life among mental health nurses: a cross-sectional study. BMC Nurs. 2023;22(1):184. doi:10.1186/s12912-023-01346-1. [Google Scholar] [PubMed] [CrossRef]
22. AlSalem M, Alamri R, Hejazi S. Nonpsychiatric healthcare professionals’ attitudes toward patients with mental illnesses in Makkah City, Saudi Arabia: a cross-sectional study. Neuropsych Dis Treat. 2020;16:341–8. doi:10.2147/NDT. [Google Scholar] [CrossRef]
23. Nejad NG, Hosseini M, Mirzaei SM, Moghaddam ZG. Association between resilience and professional quality of life among nurses working in intensive care units. Iran J Nurs. 2019;31:49–60. doi:10.29252/ijn.31.116.49. [Google Scholar] [CrossRef]
24. Algamdi M. The professional quality of life among nurses in Saudi Arabia: a multi-centre study. Nurs Res Rev. 2022;12:29–37. doi:10.2147/NRR.S333544. [Google Scholar] [CrossRef]
25. Shahin MA, Al-Dubai SAR, Abdoh DS, Alahmadi AS, Ali AK, Hifnawy T. Burnout among nurses working in the primary health care centers in Saudi Arabia, a multicenter study. AIMS Public Health. 2020;7(4):844–53. doi:10.3934/publichealth.2020065. [Google Scholar] [PubMed] [CrossRef]
26. Başoğul C, Arabaci BL, Satıl ME, Aslan BA. Professional values and professional quality of life among mental health nurses: a cross-sectional study. Nurs Health Sci. 2021;23(2):362–71. doi:10.1111/nhs.v23.2. [Google Scholar] [CrossRef]
27. Sukut O, Sahin-Bayindir G, Ayhan-Balik CH, Albal E. Professional quality of life and psychological resilience among psychiatric nurses. Perspect Psychiatr Care. 2022;58(1):330–8. doi:10.1111/ppc.v58.1. [Google Scholar] [CrossRef]
28. Maila S, Martin PD, Chipps J. Professional quality of life amongst nurses in psychiatric observation units. S Afr J Psychiatr. 2020;26:1553. [Google Scholar] [PubMed]
29. Qureshi NA, Al-Habeeb AA, Koenig HG. Mental health system in Saudi Arabia: an overview. Neuropsychiatr Dis Treat. 2013;9:1121–35. [Google Scholar] [PubMed]
30. World Health Organization. Mental Health Atlas 2014: France: World Health Organization; 2015. [Google Scholar]
31. Delaney KR, Vanderhoef D. The psychiatric mental health advanced practice registered nurse workforce: charting the future. J Am Psychiatr Nurs Assoc. 2019;25(1):11–8. doi:10.1177/1078390318806571. [Google Scholar] [PubMed] [CrossRef]
32. Uluman O, Sukut O, Kaya F, C.H. A. Ideals and realities in psychiatric nursing practıce. In: Proceeding of IV International VIII National Psychiatric Nursing Congress-Ideals and Realities: What We Couldn’t Achieve, 2016; Manisa, Turkey. [Google Scholar]
33. Guide S. Al-Amal mental health complex 2021. Available from: https://sehaguide.com/en/Item/9320/Al-Amal-Mental-Health-Complex. [Accessed 2024]. [Google Scholar]
34. Kingdom S. Regression and ANOVA-sample size calculator Melbourne, Australia 2017. Available from: https://www.statskingdom.com/410multi_linear_regression.html. [Accessed 2024]. [Google Scholar]
35. Center for Victims of Torture. ProQOL measure 2018. Available from: https://www.ProQOL.org. [Accessed 2024]. [Google Scholar]
36. Toma G, Guetterman TC, Yaqub T, Talaat N, Fetters MD. A systematic approach for accurate translation of instruments: experience with translating the Connor-Davidson Resilience Scale into Arabic. Methodol Innov. 2017;10(3):2059799117741406. [Google Scholar]
37. Ang SY, Hemsworth D, Uthaman T, Ayre TC, Mordiffi SZ, Ang E, et al. Understanding the influence of resilience on psychological outcomes—comparing results from acute care nurses in Canada and Singapore. Appl Nurs Res. 2018;43:105–13. doi:10.1016/j.apnr.2018.07.007. [Google Scholar] [PubMed] [CrossRef]
38. Dehvan F, Kamangar P, Baiezeedy S, Roshani D, Gheshlagh RG. The relationship of mental health with resilience among psychiatric nurses. Nurs Pract Today. 2018;5(4):368–74. [Google Scholar]
39. Hernandez SH, Morgan BJ, Parshall MB. Resilience, stress, stigma, and barriers to mental healthcare in US Air Force nursing personnel. Nurs Res. 2016;65(6):481. doi:10.1097/NNR.0000000000000182. [Google Scholar] [PubMed] [CrossRef]
40. Mangoulia P, Koukia E, Alevizopoulos G, Fildissis G, Katostaras T. Prevalence of secondary traumatic stress among psychiatric nurses in Greece. Arch Psychiatr Nurs. 2015;29(5):333–8. doi:10.1016/j.apnu.2015.06.001. [Google Scholar] [PubMed] [CrossRef]
41. World Health Organization. Mental health workers data by country 2017. Available from: https://apps.who.int/gho/data/view.main.HWF11v. [Accessed 2024]. [Google Scholar]
42. Jalil R, Huber JW, Sixsmith J, Dickens GL. Mental health nurses’ emotions, exposure to patient aggression, attitudes to and use of coercive measures: cross sectional questionnaire survey. Int J Nurs Stud. 2017;75:130–8. doi:10.1016/j.ijnurstu.2017.07.018. [Google Scholar] [PubMed] [CrossRef]
43. Muir-Cochrane E, O’Kane D, Oster C. Fear and blame in mental health nurses’ accounts of restrictive practices: implications for the elimination of seclusion and restraint. Int J Ment Health Nurs. 2018;27(5):1511–21. doi:10.1111/inm.2018.27.issue-5. [Google Scholar] [CrossRef]
44. Tonso MA, Prematunga RK, Norris SJ, Williams L, Sands N, Elsom SJ. Workplace violence in mental health: a Victorian mental health workforce survey. Int J Ment Health Nurs. 2016;25(5):444–51. doi:10.1111/inm.2016.25.issue-5. [Google Scholar] [CrossRef]
45. Edward KI, Hercelinskyj G, Giandinoto JA. Emotional labour in mental health nursing: an integrative systematic review. Int J Ment Health Nurs. 2017;26(3):215–25. doi:10.1111/inm.2017.26.issue-3. [Google Scholar] [CrossRef]
46. Gabrielsson S, Sävenstedt S, Olsson M. Taking personal responsibility: nurses’ and assistant nurses’ experiences of good nursing practice in psychiatric inpatient care. Int J Ment Health Nurs. 2016;25(5):434–43. doi:10.1111/inm.2016.25.issue-5. [Google Scholar] [CrossRef]
47. Yanchus NJ, Periard D, Osatuke K. Further examination of predictors of turnover intention among mental health professionals. J Psychiatr Ment Health Nurs. 2017;24(1):41–56. doi:10.1111/jpm.2017.24.issue-1. [Google Scholar] [CrossRef]
48. Ruiz-Fernández MD, Pérez-García E, Ortega-Galán ÁM. Quality of life in nursing professionals: burnout, fatigue, and compassion satisfaction. Int J Environ Res Public Health. 2020;17(4):1253. doi:10.3390/ijerph17041253. [Google Scholar] [PubMed] [CrossRef]
49. Rushton CH, Batcheller J, Schroeder K, Donohue P. Burnout and resilience among nurses practicing in high-intensity settings. Am J Crit Care. 2015;24(5):412–20. doi:10.4037/ajcc2015291. [Google Scholar] [PubMed] [CrossRef]
50. Zhang YY, Zhang C, Han X-R, Li W, Wang YL. Determinants of compassion satisfaction, compassion fatigue and burn out in nursing: a correlative meta-analysis. Medical. 2018;97(26). [Google Scholar]
51. Roney LN, Acri MC. The cost of caring: an exploration of compassion fatigue, compassion satisfaction, and job satisfaction in pediatric nurses. J Pediatr Nurs. 2018;40:74–80. doi:10.1016/j.pedn.2018.01.016. [Google Scholar] [PubMed] [CrossRef]
52. Mooney C, Fetter K, Gross BW, Rinehart C, Lynch C, Rogers FB. A preliminary analysis of compassion satisfaction and compassion fatigue with considerations for nursing unit specialization and demographic factors. J Trauma Nurs. 2017;24(3):158–63. doi:10.1097/JTN.0000000000000284. [Google Scholar] [PubMed] [CrossRef]
53. Hojat M, Gonnella JS. What matters more about the Interpersonal Reactivity Index and the Jefferson Scale of Empathy? Their underlying constructs or their relationships with pertinent measures of clinical competence and patient outcomes? Acad Med. 2017;92(6):743–5. doi:10.1097/ACM.0000000000001424. [Google Scholar] [PubMed] [CrossRef]
54. Guo YF, Cross W, Plummer V, Lam L, Luo YH, Zhang JP. Exploring resilience in Chinese nurses: a cross-sectional study. J Nurs Management. 2017;25(3):223–30. doi:10.1111/jonm.2017.25.issue-3. [Google Scholar] [CrossRef]
55. Manomenidis G, Panagopoulou E, Montgomery A. Resilience in nursing: the role of internal and external factors. J Nurs Manage. 2019;27(1):172–8. doi:10.1111/jonm.2019.27.issue-1. [Google Scholar] [CrossRef]
56. Tucker SJ, Gallagher-Ford L, Baker M, Vottero BA. Promoting nurse retention through career development planning. Am J Nurs. 2019;119(6):62–6. doi:10.1097/01.NAJ.0000559823.73262.d2. [Google Scholar] [PubMed] [CrossRef]
57. Javanmardnejad S, Bandari R, Heravi-Karimooi M, Rejeh N, Nia SH, Montazeri A. Happiness, quality of working life, and job satisfaction among nurses working in emergency departments in Iran. Health Qual Life Outcomes. 2021;19(1):112. doi:10.1186/s12955-021-01755-3. [Google Scholar] [PubMed] [CrossRef]
58. Ni W, Xia M, Jing M, Zhu S, Li L. The relationship between professional quality of life and work environment among ICU nurses in Chinese: a cross-sectional study. Front Publ Health. 2023;11:1104853. doi:10.3389/fpubh.2023.1104853. [Google Scholar] [PubMed] [CrossRef]
59. Boselli E, Cuna J, Bernard F, Delaunay L, Virot C. Effects of a training program in medical hypnosis on burnout in anesthesiologists and other healthcare providers: a survey study. Complement Ther Clin Pract. 2021;44:101431. doi:10.1016/j.ctcp.2021.101431. [Google Scholar] [PubMed] [CrossRef]
60. Cohen C, Pignata S, Bezak E, Tie M, Childs J. Workplace interventions to improve well-being and reduce burnout for nurses, physicians and allied healthcare professionals: a systematic review. BMJ Open. 2023;13(6):e071203. doi:10.1136/bmjopen-2022-071203. [Google Scholar] [PubMed] [CrossRef]
61. Boyle DA. Compassion fatigue: the cost of caring. Nursing. 2015;45(7):48–51. doi:10.1097/01.NURSE.0000461857.48809.a1. [Google Scholar] [PubMed] [CrossRef]
Cite This Article
 Copyright © 2024 The Author(s). Published by Tech Science Press.
Copyright © 2024 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools