 Open Access
Open Access
ARTICLE
Advancement of Nursing Education in Psychosocial Oncology Care: Perspectives and Experiences of Nurses
1 College of Nursing, King Khalid University, Abha, 62217, Saudi Arabia
2 Prince Sultan Military College of Health Sciences, Dhahran, 32227, Saudi Arabia
3 College of Nursing, University of Hail, Hail, 55211, Saudi Arabia
4 College of Nursing, Shaqra University, Riyadh, 15551, Saudi Arabia
* Corresponding Authors: Eddieson Pasay-an. Email: ; Lizy Sonia Benjamin. Email:
(This article belongs to the Special Issue: Multidisciplinary Clinical Health Psychology for Cancer Experience
Psychologie clinique multidisciplinaire de la santé pour l'expérience du cancer)
Psycho-Oncologie 2024, 18(4), 281-289. https://doi.org/10.32604/po.2024.054599
Received 02 June 2024; Accepted 08 August 2024; Issue published 04 December 2024
Abstract
Introduction: The main objective of this study was to fill the gap between the knowledge nurses have about psychosocial care and what they do about cancer patients’ needs. It also aimed to devise ways to improve nursing education for nurses who could provide enhanced psychosocial support in such areas. Methods: This qualitative study relied on 18 in-depth interviews with nurses, with a focus on the difference between their understanding of psychosocial care and its application in helping cancer patients. This involved analyzing the transcribed interviews using thematic analysis. Data were collected from February to March 2024. Results: The verbal accounts of 18 participants were analyzed. These include theme 1 “holistic approach to cancer care” with the subtheme “navigating resource constraints:” theme 2 “nurses well-being and emotional input” with the subtheme “positive impact of psychosocial care:” theme 3 “Care for patients’ well-being” with subtheme “resourcefulness and resilience in psychosocial care:” theme 4 “adapting care and building connections:” theme 5 “ideal and reality in psychosocial care” with subtheme “challenges in delivering comprehensive cancer care:” and theme 6 “empowering nurses for effective psychosocial care” with subtheme “building a strong foundation for psychosocial care.” Conclusion: From the nurses’ perspective, this study indicates a need for more inclusive cancer treatment. Therefore, in addition to physical interventions, emotions and social welfare must also be addressed. Although emotionally invested, health workers may offer assistance along psychosocial lines, thus aiding both patients and caretakers. Although individualized care with personal connections is crucial for effective services, this approach can make it difficult to ensure that all clients receive adequate psychological assistance. Hence, there has been a call to enhance the training to produce nurses who offer high-quality services. This study emphasizes a more holistic approach toward the emotional needs of patients while supporting those responsible for them in their sickness journey.Keywords
Cancer is a complex, multifaceted disease. Its management needs to be holistic to address patients’ physical, emotional, and psychological requirements, including the implementation of a systematic psychosocial care plan in collaboration with other healthcare professionals [1]. Nurses are essential in this field, and it is important for them to understand that their supportive role goes across the spectrum of cancer care [2]. Therefore, nurses need access to relevant knowledge and skills if they are to perform this role effectively [3]. According to Pehrson et al. [4], people with cancer require both informational and emotional support. However, nurses do not always hear about these concerns directly from patients; hence, there is a need to identify verbal and non-verbal cues [4]. The significance of not promptly addressing an unexposed spiritual need may lead to significant distress [5]. As they act as primary caretakers and confidants in most cases, nurses have a distinct ability to provide psychosocial care and emotional support for cancer patients.
Several studies have explored the importance of health care providers’ psychosocial skills in cancer care and prevention [6–8]. Lyu et al. [6] found that nurses with higher cognitive empathy and communication abilities were more likely to provide emotional support to cancer patients. According to Connolly et al. [7], nurses who underwent psychosocial skills training reported increased confidence in providing emotional support for patients. Gabriel et al. [8] showed that counseling and support groups, such as psychosocial interventions, can enhance mental health and quality of life among patients with cancer. Numerous previous studies have identified many factors resulting in the theory-practice gap, such as system inadequacy, resource restriction, lack of experience, poor working conditions, and lack of collaboration between clinical settings and educational institutions [9,10]. These factors emphasize the need for more effective support and training for nurses to offer better psychosocial care to patients [11]. In cancer care, nurses play a crucial role in identifying and addressing psychosocial needs; however, a collaborative approach involving therapists and other mental health professionals is essential for optimal patient care.
The importance of psychosocial care in managing various emotional and social problems is gaining recognition in caring for cancer patients [12,13]. However, many nurses lack a knowledge base or feel unprepared to respond to this need [12]. This situation has resulted in a gap between theory and practice, which affects the quality of care provided to patients and their outcomes [12,13]. Psychosocial needs include the desire for connection with others, sense of purpose, stress management, and the ability to cope with intense emotions, all of which are fundamental aspects of well-being among cancer patients. Nevertheless, nurses are better positioned as primary providers; therefore, improved communication skills and psychosocial support may result in enhanced healthcare. Effective communication allows nurses to construct an environment conducive for patients and personalize assistance meant to address these core psychosocial needs. When health institutions invest in education programs, this can result in good patient outcomes and a more supportive healthcare experience [14,15]. Nonetheless, there is little research on what this significant role entails because of issues such as differences in how nurses perceive their roles rather than their actual practices concerning supportive activities for cancer patients. Reviewing the efficacy of diverse nursing training programs towards closing this theory-practice gap beyond education itself is also lacking.
This study is essential for producing a deep understanding of the psychosocial skills that nurses need to take care of patients with cancer. It is critical for policymakers, politicians, and practitioners, since it may be used to shape policies and inform interventions that would enhance psychosocial competence among nurses, thus improving nursing practice. According to previous studies [16,17]. Research on enhancing caregivers’ abilities to deliver psychosocial care during cancer treatment can benefit both the patients and the medical field. The benefits for patients include improved emotional well-being, better adherence to therapy, and reduced healthcare resource use. This would translate into reduced burnout levels in nurses, increased confidence levels, and closer relationships with patients and colleagues through simplified communication channels [18]. Furthermore, it points out cost-effective measures that are required for comprehensive practices and collaboration between healthcare and learning institutions, leading to an all-inclusive and compassionate health system at large. This study aimed to explore nurses’ perspectives on their information needs regarding psychosocial care, and what they do about cancer patients’ needs in their practice. This study also pursued strategies to equip local nurses with better psychosocial skills for hospital users. The study was conducted in one of the government hospitals located in the Aseer region (coded for privacy), a tertiary main hospital that seeks referrals from neighboring towns. Our purpose was to pursue strategies to equip local nurses with better psychosocial skills for hospital users.
This study employed a qualitative phenomenological approach to explore the gap between nurses’ knowledge of psychosocial care and their current practices in supporting cancer patients’ emotional and social needs. The Consolidated Criteria for Reporting Qualitative Research (COREQ) report comprehensively and transparently.
The study participants were 18 nurses (three males and 15 female nurses) who had cared for cancer patients. These nurses were recruited using snowball and purposive sampling, following the inclusion criteria: (a) had direct contact and continuous care for patients with cancer, (b) had no signs and symptoms of psychological burden, (c) had cared for at least two patients with cancer, and (d) participated voluntarily.
Data collection commenced after clearance from the ethics review board and directors of the participating hospital. A personalized letter was sent to 20 prospective nurses, inviting them to participate in the study. The letter indicates that no incentives were given to the participants to participate in the interviews. Of the candidates, 18 replied, indicating their ability to participate. The researchers and participants agreed on the date, time, and mode of the interview, which was conducted using Zoom meeting software, with the understanding that only the researcher and participants would be present in the meeting room. The one-on-one interview lasted 60–70 min and was recorded with the permission of the participants, as discussed in the written informed consent section, and reiterated before the meeting. Field notes were used by the researchers. Unstructured interviews and/or interactive dialog were used for data collection. Sample questions included, “Can you describe your understanding of psychosocial care in the context of cancer treatment?” “How comfortable do you feel addressing the emotional and social needs of your cancer patients? Sample probing questions included, ‘Can you further explain or clarify what you mean by that?’ Can you give an example?” Given the repetitive nature of data, researchers must determine the point at which saturation is observed. In this study, data saturation was achieved for the 16th participant. Two others were also included to ensure data saturation. No further interviews were conducted during this period. This study was conducted between February and March 2024. Ten researchers (seven women) were professors at the College of Nursing, and three were staff nurses in different hospitals. They were well-trained during the interview process. The researchers’ reasons for and interest in this topic are propelled by their purpose of improving nursing education and training programs to equip nurses with the necessary skills and knowledge to provide better psychosocial support.
Participants’ stories provide a lens through which to view evolving perspectives on caring for patients with cancer. We had to be careful as a researcher to distinguish between lived experiences and described experiences, and to prevent the wrong idea of causality. Participants may face different scenarios, but their underlying identities may remain unchanged. This core identity, shaped by their backgrounds and values, can influence their approach to problems. In some cases, it can provide a strong foundation for challenges in a way that makes people feel authentic. Participants’ challenges may enlarge, improve, or affect them in ways that may not be visible to others but may be included in their story. Comparing some of the story examples helped us understand how participants were affected by caring for patients with cancer. Researchers recognize the value of narratives when exploring ideas. However, they caution against relying solely on a single story. A deeper understanding often emerges when examining a collection of narratives, allowing for a more comprehensive picture of the idea in question.
In this study, the researchers performed member checking to ensure credibility. The participants were asked to read verbatim transcripts from their respective interviews and provide feedback on the content. A detailed description of their experiences in caring for cancer patients was used to establish transferability. An inquiry audit or an external audit was used to ensure dependability. This study aimed to evaluate the accuracy and whether the data supported the findings, interpretations, and conclusions. Finally, to ensure rigor, a phenomenological study should have confirmability, obtained using audit trials to provide rationale and describe the thought processes behind data collection, analysis, and interpretation.
The thematic analysis was performed using NVIVO software (QSR International Pty Ltd., Burlington, MA, USA). Data analysis began immediately after the completion of the first transcription. Each researcher worked independently on the initial data analysis procedures following predetermined steps. First, the researchers read the transcriptions and field notes for each interview numerous times to ensure clear understanding. Phrases and expressions that described the experiences of nurses caring for cancer patients were then chosen. Finally, meanings related to participants’ experiences were generated. The researchers collaborated in groups and organized the themes, and any discrepancies were resolved by re-evaluating the transcriptions and field notes until an agreement was reached. Subsequently, the transcriptions were compared and analyzed for phrases that reflected similar theme descriptions. These themes were revised and described in greater depth. Statements from the participants who reflected on each topic were chosen and rewritten. Since not all participants were available, we requested the nine participants who were available at that time to examine only the findings (themes and descriptions) to ensure that they matched the information they had provided. The validation process did not reveal any discrepancies in the information provided.
Based on the accounts of the 18 participants, six themes and five subthemes emerged. This includes, theme 1 “holistic approach to cancer care” with subtheme “navigating resource constraints:” theme 2 “nurses well-being and emotional input” with subtheme “positive impact of psychosocial care:” theme 3 “Care for patients’ well-being” with subtheme “resourcefulness and resilience in psychosocial care:” theme 4 “adapting care and building connections:” theme 5 “ideal and reality in psychosocial care” with subtheme “challenges in delivering comprehensive cancer care:” and theme 6 “empowering nurses for effective psychosocial care” with subtheme “building a strong foundation for psychosocial care.”
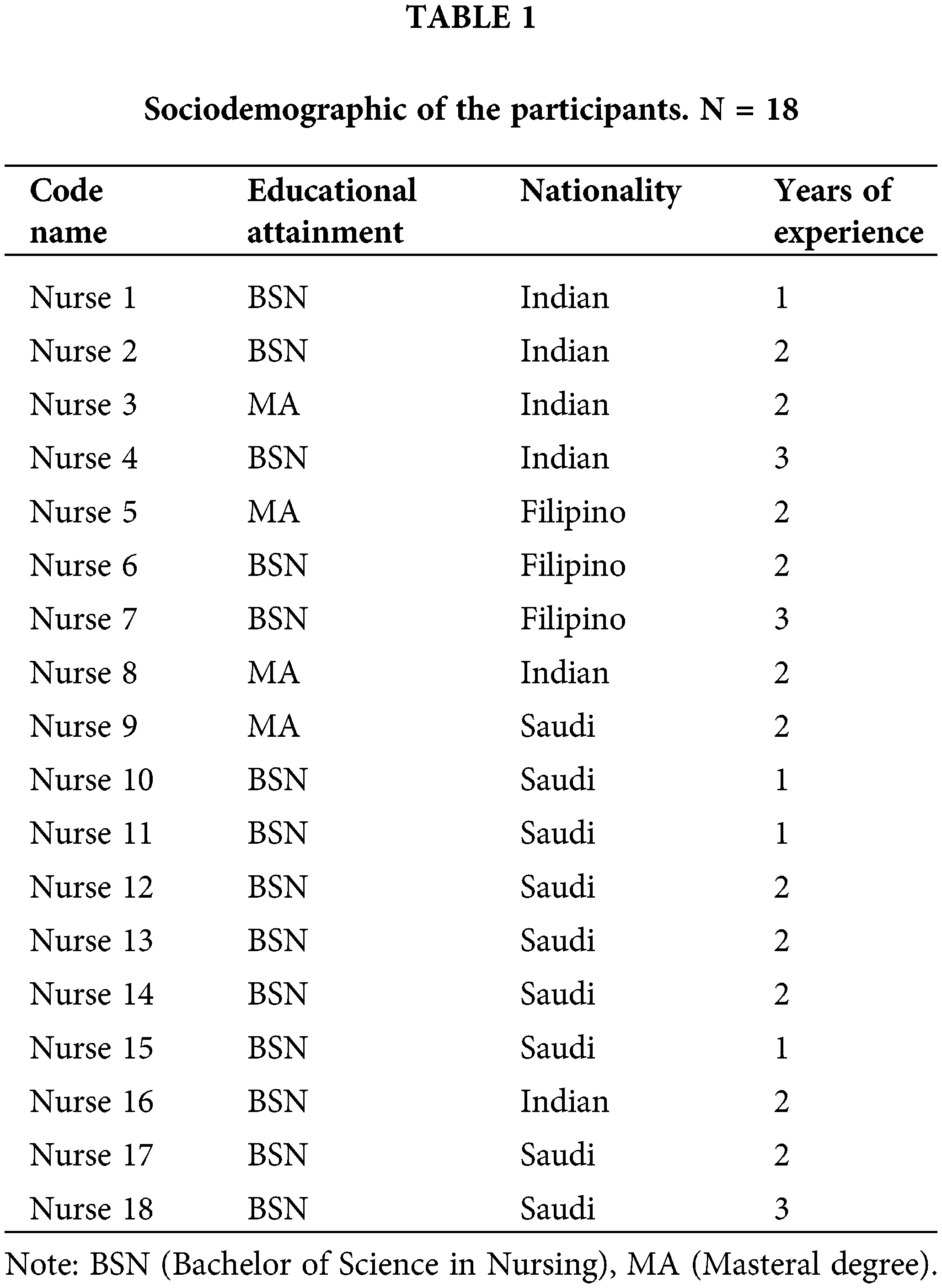
Table 1 presents the sociodemographics of the 18 participants. The participants were Bachelor of Science in Nursing (BSN) holders, and a few had a master’s degree (MA). They came from diverse nationalities and had at least 1–2 years of experience.
Theme 1: Holistic Approach to Cancer Care
This theme translates into a multifaceted treatment plan that addresses the various ways that cancer can affect a person’s life. It goes beyond just treating physical diseases and acknowledges the emotional and social toll it takes. As a result, psychosocial care has become an essential part of comprehensive cancer treatment, integrated with physical interventions to ensure that patients receive well-rounded support throughout their entire journey. In a one-to-one interview with nurses, some specifically mentioned the following:
Nurse 2: What I understand about psychosocial care is that it focuses on recognizing and addressing the emotional, social, and spiritual needs of patients throughout their cancer journey.
Nurse 4: Still clear to my mind about the seminar that I attended, when we talk about psychosocial care, it should involve respecting patients’ spiritual beliefs and practices and, if needed, connecting them with their religious leaders for support.
Nurse 5: Psychosocial care for me is about enhancing the patients’ quality of life over the course of their cancer journey. This can involve tackling body image issues arising from treatment and sexual health and helping them maintain a sense of normalcy and purpose despite the challenges they endure.
In Saudi Arabia, religious leaders hold immense trust and influence. This cultural value aligns perfectly with incorporating spiritual beliefs and practices into psychosocial care. When appropriate, connecting patients to their religious leaders for support can be a powerful tool for healing and well-being. However, when it comes to psychosocial care provision, which can be better understood by nurses who understand that cancer is a holistic approach to taking care of someone, the two do not always match. Despite positive intentions, logistical problems are experienced during delivery by nurses trying to take care of such cases.
Subtheme 1: Navigating Resource Constraints
This theme focused on the practical limitations faced by nurses, including the lack of social workers and the contribution of limited resources to emotional strain.
Nurse 12: I feel overwhelmed by the lack of support staff. For instance, having a social worker in hand could help manage some of the emotional and social challenges faced by patients, thereby reducing the burden on nurses.
Nurse 3: I cannot help but compare my previous job with my lack of social workers. Having a social worker on the floor can help ease the emotional burden.
Theme 2: Nurse Well-Being and Emotional Impact
This theme focuses on the emotional toll that caring for cancer patients takes on nurses. This highlights the challenges that this emotional burden presents in terms of providing ideal psychosocial care. The concept of burnout is emphasized along with the importance of self-care for nurses to maintain their well-being and continue providing optimal care to patients.
The nurses’ accounts directly expressed the emotional burden of their work and the need for self-care to avoid burnout.
Nurse 14: I for one, being constantly exposed to the suffering of my patients can lead me to emotional burnout... just saying...
Nurse 10: I would like to express my concern that it is as important for nurses caring for our patients, especially in the oncology ward, to avoid burnout and maintain our own well-being so that we can continue to provide optimal care for their patients.
Subtheme 2: Positive Impact of Psychosocial Care.
This subtheme refers to the positive impact of psychosocial care, extending beyond the patients that nurses care for. It can contribute to nurses’ well-being by fostering a sense of purpose and job satisfaction and potentially reducing burnout. The nurses lamented:
The idea of a holistic approach to cancer care is important, as shown by the nurses’ understanding of psychosocial care. However, dedicated nurses face numerous challenges in the delivery of comprehensive care.
Nurse 11: Part of my job that I found satisfying was providing psychosocial support, which can significantly improve the quality of life of patients and their families during very difficult times.
Nurse 2: There are many challenges, such as not being trained under this condition. As such, limited time exists mainly because of overcrowding while attending to individual patients’ needs in terms of psychosocial matters, and accessibility to other experts in social work or therapy may be inconvenient, especially in low-income settings.
Nurse 3: The pain that comes from seeing your patients suffering constantly takes an emotional toll on you. It is necessary for me to take good care of myself so that I do not end up getting burned. Nevertheless, providing psychosocial care amidst these difficulties is integral to becoming an excellent oncology nurse. Such services can improve the quality of life of both my patients and their relatives during such trial times.
Theme 3. Care for Patients’ Well-being
These obstacles can hinder effective nursing, but they do not make them less committed individuals. In fact, they portray a high level of resourcefulness and resilience in the quotes given. Even though there are limitations, they strive to find solutions in areas where they do exist, and the fact that they do so shows how dedicated they are towards enhancing the welfare of their clients.
Nurse 14: I feel like I am constantly on edge, never able to truly relax because I am worried about my patients.
Nurse 13: Can you imagine seeing them every day, especially when they are admitted? It’s hard to see someone you care about suffering so much.
Nurse 18: The feelings of helplessness were the worst. I want to do more, but I do not have much.
Subtheme 3: Resourcefulness and Resilience in Psychosocial Care
This subtheme explains how some proactive nurses try to bridge the gap between an ideal situation and reality through self-reliance, commitment, and determination while delivering psychosocial therapies, even if resources are few. Interviews showed that during this exercise, some qualities included resourcefulness, dedication, and resilience, among others. They provide examples of extraordinary initiatives to fill gaps in psychosocial care despite challenges within the health system, such as:
Nurse 1: I’ll incorporate short mindfulness exercises into my patient interactions when I feel stressed even if we don’t have a dedicated therapist.
Nurse 18: Local support groups could be held when social workers are not available.
Nurse 5: We cannot change our constraints, but we can change our own attitudes around them such as building therapeutic relationship based on trust and empathy characterized by good rapport with patients.
Theme 4. Adapting Care and Building Connections
This theme is adaptable to approaches, formation of relationships, and psychological support. Some narratives indicate that technical duties do not make up for nursing alone, thus defining boundaries.
Thus, it portrays how they modify their approach to things that leverage what is available creatively and connect with patients as a strategy for bridging the gap between what should appear essentially different from the technical limitations; however, effective psychosocial care is still provided. As stated:
Nurse 4: Since it is difficult to get time for individual counseling, I collaborate with professionals such as social workers from other units to ensure holistic patient care that addresses varying needs.
Nurse 6: At times, the most crucial measure is mere presence. Whenever I can, I make an effort to free up more time just to stay with patients and hear their problems even if it means going over after my duty.
Theme 5. Ideal and Reality in Psychosocial Care
This theme highlights the discrepancy between the theoretical knowledge psychosocial care nurses acquire in school and the practical realities they face when implementing it with patients.
Nurse 4: What do we learn about psychosocial care in nursing schools and how can we implement it with patients daily? Ideally, we have ample time to provide in-depth emotional support; however, the reality is different.
Nurse 10: One of the gaps I can see is that workloads are often overwhelming. With so many patients to care for, dedicating significant time to in-depth psychosocial support has become a luxury.
Nurse 11: For me, it can provide access to specialists, such as social workers or therapists, especially in understaffed facilities. This places an emotional burden on us, even when we lack expertise in complex situations.
Subtheme 5: Challenges in Delivering Comprehensive Cancer Care
This subtheme emphasizes the difficulties nurses face in providing complete care for their patients, acknowledging the emotional and social aspects alongside physical ones.
Nurse 15: By equipping nurses with tools and resources to effectively deliver psychosocial care, patient well-being can be significantly improved. Knowing that we are making a difference in both the physical and emotional fronts is incredibly rewarding and makes challenges more manageable.
Nurse 14: Learning time-management techniques for prioritizing psychosocial care within our existing workload could be highly beneficial.
Nurse 10: In the fast-paced environment of a cancer ward, there is definitely a gap between what we learn about psychosocial care and how much we can implement it. We understand the importance of addressing emotional needs, but reality often falls short of this.
Nurse 12: Sometimes, clear communication with doctors or other team members regarding a patient’s psychosocial needs is lacking. This makes it more difficult to ensure that patients receive holistic care. To address this, instead of just theory, training should include practical communication and coping mechanism tools that can be readily used during busy shifts.
Theme 6. Empowering Nurses for Effective Psychosocial Care:
This theme highlights suggestions made by nurses to improve themselves and provide better psychosocial care. This emphasizes the need for communication skills, self-care, and emotional resilience as well as education and training for impactful care.
Nurse 16: Being able to effectively communicate with patients from different cultural backgrounds is essential for building trust and rapport.
Nurse 8: Having a strong support system outside of work is crucial to prevent burnout.
Nurse 14: We will be able to provide full treatment. Imagine when you can confidently address things such as cancer’s fear of returning or bereaving families. All of these are scenarios where we want to make an impact but presently have no idea how or what should be done; hence, they remain impossible to attain.
Subtheme 6: Building a Strong Foundation for Psychosocial Care
This subtheme is characterized by an emphasis on communication skills, self-care practices, and educational opportunities for nurses. Self-care methods are vital in stress management and emotional wellness, allowing nurses to provide sympathy (compassionate care). Finally, nurses advocate education and training to further their competence levels and provide them with the foundations of psychosocial care.
Nurse 10: Since I started practicing mindfulness meditation, I feel better equipped to manage stress and provide compassionate care.
Nurse 18: I’ve found that actively listening and validating patients’ feelings helps them feel more supported and understood and understanding the communication helped me better understand nonverbal cues and tailor my approach to each patient.
Nurse 9: It would have been good if I had learned more about motivational interviewing in nursing school, so as to assist patients positively.
The nurses’ perspective unveils intricate “psycho-social” issues tied with oncology. For example, an ideal approach would be a holistic one that considers emotional therapy and social needs; however, there are still unresolved problems within the system. Nonetheless, they also pointed out some strategies for fighting cancer, including resilience and ways to improve training and resource access. By providing nurses with the tools they need, effective empowerment of healthcare institutions can bridge the theory practice gap towards a comprehensive and efficient cancer cure.
This study aimed to explore nurses’ perspectives on their information needs regarding psychosocial care, and what they do about cancer patients’ needs in their practice. This study also pursued strategies to equip local nurses with better psychosocial skills for hospital users. The holistic approach to cancer care recognizes the importance of psychosocial care for the complete support of cancer patients. However, the challenges encountered by the interviewed nurses in providing optimal psychosocial care can hinder this goal. Focusing on these challenges and equipping nurses with the necessary resources and training is crucial for enhancing the quality of healthcare and emotional backing within cancer-related areas. This study investigates how the constant need to manage patients’ pain caused by cancer can undermine nurses’ ability to provide comprehensive psychosocial care. This aligns with previous research by Zimmermann et al. [19] who explored the impact of emotional exhaustion on nurses, highlighting the potential for cynicism or numbing as a result of constant exposure to patient suffering. Their research aimed to improve psychosocial screening for a more targeted allocation of psycho-oncological support, reflecting the need to address these challenges [19]. This study highlights the challenges that interviewed nurses face in providing ideal psychosocial care, aligning with the importance of improved screening for better support among cancer patients. Moreover, Ernstmann et al.’s [20] research on psycho-oncology services in breast centers contained important information [20]. In this way, their national survey lays bare how psycho-oncology is practiced across various breast centers, showing why integration of psychosocial supportive elements into the milieu, creating availability and accessibility for psychogenic processes, is necessary in any type of oncologic center setting. Frisch et al. [21] also shared the challenges of providing holistic nursing practice, which aims to offer better psychosocial care to cancer patients. In addition, acknowledging the significance of psycho-oncology and having a positive therapeutic relationship among healthcare providers can enhance the delivery of comprehensive care that meets all these needs or other dimensions in which cancer patients exist.
Nurses’ well-being and emotional contribution to their patients, especially the positive impact of psychosocial care, are important elements in the delivery of healthcare. Psychosocial care refers to attending to patients’ emotional, social, and psychological needs, which can significantly affect their general health and recovery processes. Many studies have demonstrated the significance of psychosocial care in various health care settings. Such areas include the communication abilities required for nurses to provide effective psychosocial care among cancer patients, how they identify psychosocial health requirements, and eventually develop comprehensive plans for such cases [13]. This serves as a reminder that nurses are essential in dealing with patients’ psychosocial dimensions. Nevertheless, previous research cited problems impeding nurses from offering psychosocial care, including work overload and time limitation [22,23]. This would remove these obstacles so that nurses could competently provide support, which would greatly aid their proper discharge of duties. In all healthcare settings, psychosocial assistance had an affirmative effect on nurses’ well-being and emotional involvement. Consequently, recognizing the importance of providing a psychosocial support system and addressing its barriers to healthcare systems would help patients recover optimally by facilitating good health outcomes for both them and their medics.
The emotional toll and limitations in relation to cancer care experienced by nurses look at how healthcare providers, especially nurses, face emotional challenges in caring for patients suffering from cancer. This theme implies the need to deal with the emotional burden imposed on medical professionals when offering psychosocial care to people living with cancer. In addition, one study was conducted by Clover et al. [24], who sought to determine why oncology outpatients who reported being emotionally distressed may refuse help. The complexity of emotional distress among cancer patients and the barriers that hinder people from seeking assistance are reflected in this study, giving us an idea of what it means when psychologists say, “cancer medicine is a stressful job.” Additionally, the current research highlights the significance of working together as a team in different medical fields such as breast cancer and shows how emotional stress caused by care provision is taken care of [25]. Consequently, for healthcare providers to meet quality service delivery through teamwork and other holistic needs aspects, this will also minimize pressure among practitioners who often have high psychological load due to tension experienced during interactions with patients with chronic diseases such as cancer. Therefore, taking these challenges and encouraging multidisciplinary approaches will go a long way to enhancing patient care and support for those affected by cancer, thereby building resilience in psychosocial support systems.
Healthcare is a very important field where the theme of “Adapting care and building connections” needs to be addressed. Making good relationships with patients and changing the way care is provided can help improve the quality of health care. Some studies have provided information on relevant topics that substantiate the significance of this theme. For instance, Shapiro et al. [26] conducted research on Mindfulness-Based Stress Reduction for healthcare practitioners and showed that stress management programs had positive impacts on practitioners’ mental well-being. This demonstrates the importance of interventions focused on emotional well-being to enable nurses to manage stress and emotionality at work. Additionally, Kinman et al. [27] examined emotional labor and well-being among nurses, demonstrating how they establish emotional boundaries while forming empathic connections with patients that may impact them in the long-term [27]. This highlights the need to understand the affective dimension of nursing care as a whole and its impact on nurses’ welfare. In addition, there are positive effects of caring work in general on occupationally related motivation and well-being, which shows how working emotional regulation capacity can boost energy in the workplace [28]. According to this study, having emotional resources such as motivation or wellness determines the quality of provision of nursing services. These findings indicate that, in healthcare settings, it is important to adapt care strategies to build relationships and make better connections with respect to nurses’ emotional well-being requirements. To develop feelings of self-efficiency and empowerment among nurses, this study considered the following approaches: mindfulness-based interventions, understanding emotional labor, and promoting emotional regulation, but not limited to other things.
“Challenges in providing comprehensive cancer care” is a theme under “ideal and reality in psychosocial care” that examines the intricacies experienced by healthcare providers when attempting to align psychosocial care with the ideal standards. Uwayezu et al. [13] maintained that nurses who deliver psychosocial care to patients with cancer and their families need several basic competencies. Nurses, as this study shows, must be taught the knowledge, skills, and abilities necessary to address the psychosocial needs of patients with cancer, which suggests a gap between what ideal competencies should be and actuality when it comes to complex health delivery systems. In a rural Australian setting, Kenny et al. [29] explored some limitations that confront nurse specialists while offering psychological assistance to mentally ill individuals. This study describes some realistic problems faced by medical practitioners as they provide wide psychological support to prostate cancer patients, but also distinguishes general responsibilities from best practice obligations vis-à-vis emotional distress among oncology nursing professionals functioning in real clinical settings. Media coverage has reported many instances in which caregivers become stressed by taking care of or providing counseling services, such as in the work of Kenny et al. [29]. Therefore, this research paper exposes some practical hurdles that medical personnel face while trying to provide holistic psychological support, hence showing inconsistency between anticipated practices such as models of support offered based on idealistic views vs. nurses experiencing devastating emotional conditions when working with a patient with prostate problems. Ensuring these standards will help other systems overcome these challenges, including exhaustion due to emotional drain, because they may attempt to strike a balance between clinical realities and what is expected ideally in counseling someone living with different types of cancers.
“Empowering nurses for effective psychosocial care” and “building a strong foundation for psychosocial care” showed that it is important for health workers dealing with cancer patients to be trained on how to provide all-round psychological help. The most relevant part of this theme seems to be the concept that these nurses respond emotionally, socially, and psychologically to patients with cancer [30]. Through this study, it was observed that such an attitudinal shift accompanied by enhanced clinical skills and confidence in recognizing emotional symptoms leads to an improvement in the quality of healthcare [31]. This finding implies that empowering nurses with efficient communication skills is significant for establishing a solid base for the provision of psychosocial care. Steinhauser et al. [32] conveyed a similar message in their research on end-of-life care. Thus, this study explains why open communication should be encouraged among caregivers and patients regarding serious illnesses or impending deaths. Therefore, it can be concluded that a sound base for psychosocial support encompasses open dialogue and consideration of emotional well-being when people’s lives become challenging. Health systems could enhance their treatment approaches towards cancer patients, leading to improved patient outcomes and better overall health if they offer nurses the right capabilities and tools they require.
The findings of this study cannot necessarily be applied to a larger population of nurses or to cancer care settings. First, the small sample size of only 18 participants limits the generalizability of the results to nurses who take care of patients with cancer. Second, selection bias could have been introduced through snowball and purposive sampling, which were used to recruit the participants. Nurses who had a lot of interest in or information on psychosocial care were more likely to participate than others. Third, the interview reports are autobiographical accounts that may be impaired by memory bias or covered by reticence, which avoids expressing negativity. In addition, the stories may have been affected by our function as interviewers because we sought details or elaboration. We encountered participants who had synthesized their history, present, and future. Participants presented themselves in a specific way while sharing their stories and revealing or hiding their own aspects. Furthermore, we did not contain anonymized transcripts because of limited resources. Additional personnel or resources that were not available for this project would have been needed to transcribe and anonymizes the interviews. Lastly, while we did not include nurses’ perceptions in the context of nationality and educational status, we recommend that future research should specifically examine how cultural background and educational status influence nurses’ views on incorporating spiritual beliefs into psychosocial care. To provide more comprehensive insights into how best to deliver psychosocial care for cancer treatment, future research should use larger samples comprising different levels of experience in nursing and patient inputs.
Nurses interviewed in this study recognized the importance of psychosocial care, addressing the emotional and social needs of cancer patients alongside physical treatment. However, there is a gap between theory and practice. While acknowledging its value, providing this care can be challenging owing to limitations, such as workload and lack of resources. Nurses delivering it can also experience an emotional toll and compassion fatigue. Despite these obstacles, nurses demonstrate resilience and resourcefulness in finding ways to connect with their patients and offer psychosocial care. This study suggests that improved nursing education with training in communication skills, self-care practices, and psychosocial interventions can empower nurses to provide better care. Overall, this study underscores the importance of addressing patients’ psychosocial needs and the challenges that nurses face. This emphasizes the need for improved training and support to bridge this gap and deliver holistic cancer care. In the context of nursing education, a stronger emphasis should be placed on equipping nursing students with psychosocial care skills and knowledge within the nursing education system.
This study highlights the necessity for a more comprehensive approach to cancer care. As such, this is beyond just physical treatment and addresses the emotional and social aspects of patients’ well-being, which is similarly said in the subtheme “limitations of care.” Even so, nurses still have emotions that are influenced by their work with these patients, as evidenced in the subtheme “positive impact on psychosocial care” which also shows that it has benefits for both patients and caregivers. That is why cancer care in general must acknowledge how much emotion is involved in it, hence reflected through “resourcefulness and resilience in psychosocial care”; this makes it important for nurses to be well prepared. This draws on the theme “adapting care and building connections” since effective nursing involves providing personalized services to individual patients while developing bonds with these clients. However, there is a difference between what we would like things to be like, as suggested by the sub-theme “challenges in delivering comprehensive cancer care” and how they are during the provision of psychosocial support services. Finally, there is an issue about training or preparing nurses to deliver psychosocial care; this is examined through “building a strong foundation for psychosocial care.” Overall, this study suggests that holistic approaches should be taken into consideration while handling cancer cases to meet the emotional needs that come along with them, alongside supporting nurses who provide such medical aids.
Acknowledgement: The authors would like to acknowledge the full participation of the nurses during the interview process.
Funding Statement: The authors extend their appreciation to the Deanship of Research and Graduate Studies of King Khalid University for funding this work through grant number RGP1/194/45.
Author Contributions: Conceptualized the study and developed the research design: Aida Sanad Alqarni, Fatmah Ahmed Alamoudi, Eddieson Pasay-an; conducted the interviews, transcribed the data, and assisted in data analysis: Lizy Sonia Benjamin, Kawther Elthayeb Ahmed, Petelyne Pangket; performed thematic analysis and contributed to data interpretation: Richard Maestrado, Lailani Sacgaca, Ferdinand Gonzales, Benito Areola Jr. All authors reviewed the results and approved the final version of the manuscript.
Availability of Data and Materials: The data that support the findings of this study will be available upon reasonable request. Restrictions apply to the availability of these data due to the sensitive nature of the information contained within the interview transcripts.
Ethics Approval: Ethical approval was obtained from the Institutional Ethical and Review Board of King Khalid University, Abha (ECM # 2023-904). Participation in the study was voluntary and anonymous. Informed consent was obtained from all subjects involved in the study.
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
References
1. Yassine F, Kharfan-Dabaja MA. Patient resources in a cancer center. In: Aljurf M, Majhail NS, Koh MB, Kharfan-Dabaja MA, Chao NJ, editors. The comprehensive cancer center. Cham: Springer; 2022. doi:10.1007/978-3-030-82052-7_15. [Google Scholar] [CrossRef]
2. Nsiah C, Siakwa M, Ninnoni J. Registered nurses’ description of patient advocacy in the clinical setting. Nurs Open. 2019;6(3):1124–32. doi:10.1002/nop2.307. [Google Scholar] [PubMed] [CrossRef]
3. Peek GJ. Two approaches to bridging the knowledge-practice gap in oncology nursing. Oncol Nurs Forum. 2014;42(1):94–5. doi:10.1188/15.onf.94-95. [Google Scholar] [PubMed] [CrossRef]
4. Pehrson C, Banerjee SC, Manna R, Shen MJ, Hammonds S, Coyle N, et al. Responding empathically to patients: development, implementation, and evaluation of a communication skills training module for oncology nurses. Patient Educ Couns. 2016;99(4):610–6. doi:10.1016/j.pec.2015.11.021. [Google Scholar] [PubMed] [CrossRef]
5. Muzzatti B, Agostinelli G, Bomben F, Busato S, Flaiban C, Gipponi KM, et al. Intensity and prevalence of psychological distress in cancer inpatients: cross-sectional study using new case-finding criteria for the hospital anxiety and depression scale. Front Psychol. 2022;13:3921. doi:10.3389/fpsyg.2022.875410. [Google Scholar] [PubMed] [CrossRef]
6. Lyu XC, Jiang H, Lee LH, Yang CI, Sun X. Oncology nurses’ experiences of providing emotional support for cancer patients: a qualitative study. BMC Nurs. 2024;23(1):2631. doi:10.1186/s12912-024-01718-1. [Google Scholar] [PubMed] [CrossRef]
7. Connolly M, Perryman J, McKenna Y, Orford J, Thomson L, Shuttleworth J, et al. SAGE & THYMETM: a model for training health and social care professionals in patient-focused support. Patient Educ Couns. 2010;79(1):87–93. doi:10.1016/j.pec.2009.06.004. [Google Scholar] [PubMed] [CrossRef]
8. Gabriel I, Creedy D, Coyne E. A systematic review of psychosocial interventions to improve quality of life of people with cancer and their family caregivers. Nurs Open. 2020;7(5):1299–312. doi:10.1002/nop2.543. [Google Scholar] [PubMed] [CrossRef]
9. Salifu DA, Gross J, Salifu MA, Ninnoni JP. Experiences and perceptions of the theory-practice gap in nursing in a resource-constrained setting: a qualitative description study. Nurs Open. 2018;6(1):72–83. doi:10.1002/nop2.188. [Google Scholar] [PubMed] [CrossRef]
10. Ousey K, Gallagher P. The theory-practice relationship in nursing: a debate. Nurs Educ Pract. 2007;7(4):199–205. doi:10.1016/j.nepr.2007.02.001. [Google Scholar] [PubMed] [CrossRef]
11. Chan EA, Tsang PL, Ching SSY, Wong FY, Lam W. Nurses’ perspectives on their communication with patients in busy oncology wards: a qualitative study. PLoS One. 2019;14(10):e0224178. doi:10.1371/journal.pone.0224178. [Google Scholar] [PubMed] [CrossRef]
12. Nazmiye Y, Perihan G, Figen İ. The level of psychosocial skills of nurses caring for cancer patients and affecting factors: results of a multicenter study. Psycho-Oncol. 2023:1–10. doi:10.32604/po.2023.045294. [Google Scholar] [CrossRef]
13. Uwayezu M, Nikuze B, Maree J, Buswell L, Fitch M. Competencies for nurses regarding psychosocial care of patients with cancer in africa: an imperative for action. JCO Global Oncol. 2022;86(8):348. doi:10.1200/go.21.00240. [Google Scholar] [PubMed] [CrossRef]
14. Crawford T, Candlin S, Roger P. New perspectives on understanding cultural diversity in nurse-patient communication. Collegian. 2017;24(1):63–9. [Google Scholar] [PubMed]
15. Madula P, Kalembo FW, Yu H, Kaminga AC. Healthcare provider-patient communication: a qualitative study of women’s perceptions during childbirth. Reprod Health. 2018;15(1):122. doi:10.1186/s12978-018-0580-x. [Google Scholar] [PubMed] [CrossRef]
16. Northouse L, Williams AL, Given B, McCorkle R. Psychosocial care for family caregivers of patients with cancer. J Clin Oncol. 2012;30(11):1227–34. doi:10.1200/JCO.2011.39.5798. [Google Scholar] [PubMed] [CrossRef]
17. Lee M, Cha C. Interventions to reduce burnout among clinical nurses: systematic review and meta-analysis. Sci Rep. 2023;13(1):10971. doi:10.1038/s41598-023-38169-8. [Google Scholar] [PubMed] [CrossRef]
18. Smith A, Roberts J. The impact of psychosocial care on emotional well-being and treatment adherence in patients with chronic illnesses. J Health Psychol. 2020;25(3):432–45. doi:10.1177/1359105318796472. [Google Scholar] [CrossRef]
19. Zimmermann T, Dreismann L, Ginger V, Wenzel M, Hornemann B, Dietzsch F, et al. Study protocol: the optiscreen-study: optimized psycho-oncological care–from screening to intervention. J Cancer Res Clin Oncol. 2022. doi:10.21203/rs.3.rs-1633029/v1. [Google Scholar] [CrossRef]
20. Ernstmann N, Enders A, Halbach S, Nakata H, Kehrer C, Pfaff H, et al. Psycho-oncology care in breast cancer centres: a nationwide survey. BMJ Support Palliat Care. 2019;10(4):e36. doi:10.1136/bmjspcare-2018-001704. [Google Scholar] [PubMed] [CrossRef]
21. Frisch NC, Rabinovitch D. What’s in a definition? holistic nursing, integrative health care, and integrative nursing: report of an integrated literature review. J Holist Nurs. 2019;37(3):260–72. doi:10.1177/0898010119860685. [Google Scholar] [PubMed] [CrossRef]
22. Karimi Z, Fereidouni Z, Behnammoghadam M, Alimohammadi N, Mousavizadeh A, Salehi T, et al. The lived experience of nurses caring for patients with COVID-19 in Iran: a phenomenological study. Risk Manag Healthc Policy. 2020;13:1271–8. doi:10.2147/rmhp.s258785. [Google Scholar] [PubMed] [CrossRef]
23. Sheldon L, Harris D, Arcieri C. Psychosocial concerns in cancer care: the role of the oncology nurse. Clin J Oncol Nurs. 2012;16(3):316–9. doi:10.1188/12.cjon.316-319. [Google Scholar] [PubMed] [CrossRef]
24. Clover KA, Mitchell AJ, Britton B, Carter G. Why do oncology outpatients who report emotional distress decline help? Psychooncology. 2014;24(7):812–8. doi:10.1002/pon.3729. [Google Scholar] [PubMed] [CrossRef]
25. Taylor C, Shewbridge A, Harris J, Green J. Benefits of multidisciplinary teamwork in the management of breast cancer. Breast Cancer Target Ther. 2013:79. doi:10.2147/bctt.s35581. [Google Scholar] [PubMed] [CrossRef]
26. Shapiro SL, Astin JA, Bishop SR, Cordova M. Mindfulness-based stress reduction for health care professionals: results from a randomized trial. Int J Stress Manag. 2005;12(2):164–76. doi:10.1037/1072-5245.12.2.164. [Google Scholar] [CrossRef]
27. Kinman G, Leggetter S. Emotional labour and wellbeing: what protects nurses? Healthcare. 2016;4(4):89. doi:10.3390/healthcare4040089. [Google Scholar] [PubMed] [CrossRef]
28. Donoso LMB, Demerouti E, Garrosa Hernández E, Moreno-Jiménez B, Carmona Cobo I. Positive benefits of caring on nurses’ motivation and well-being: a diary study about the role of emotional regulation abilities at work. Int J Nurs Stud. 2015;52(4):804–16. doi:10.1016/j.ijnurstu.2015.01.002. [Google Scholar] [PubMed] [CrossRef]
29. Kenny A, Allenby A. Barriers to nurses providing psychosocial care in the Australian rural context. Nurs Health Sci Res J. 2012;15(2):194–200. doi:10.1111/nhs.12014. [Google Scholar] [PubMed] [CrossRef]
30. Chan EA, Wong F, Cheung MY, Lam W. Patients’ perceptions of their experiences with nurse-patient communication in oncology settings: a focused ethnographic study. PLoS One. 2018;13(6):e0199183. doi:10.1371/journal.pone.0199183. [Google Scholar] [PubMed] [CrossRef]
31. Molina-Mula J, Gallo-Estrada J. Impact of nurse-patient relationship on quality of care and patient autonomy in decision-making. Int J Environ Res Public Health. 2020;17(3):835. doi:10.3390/ijerph17030835. [Google Scholar] [PubMed] [CrossRef]
32. Steinhauser KE, Clipp EC, McNeilly M, Christakis NA, McIntyre LM, Tulsky JA. In search of a good death: observations of patients, families, and providers. Ann Intern Med. 2000;132(10):825. doi:10.7326/0003-4819-132-10-200005160-00011. [Google Scholar] [PubMed] [CrossRef]
Cite This Article
 Copyright © 2024 The Author(s). Published by Tech Science Press.
Copyright © 2024 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools