 Open Access
Open Access
ARTICLE
The Impact of Nursing Staff’s Work Attitude on the Fear of Patients Recovering from Benign Tumors: Family Support as a Mediating Variable
1 Department of Education, Beijing Normal University, Beijing, 100091, China
2 International College, Krirk University, Bangkok, 10210, Thailand
3 Organization Personnel Department, Jiangxi Justice Police Vocational College, Nanchang, 330013, China
* Corresponding Author: Aihua Cheng. Email:
Psycho-Oncologie 2024, 18(4), 291-303. https://doi.org/10.32604/po.2024.054446
Received 28 May 2024; Accepted 14 September 2024; Issue published 04 December 2024
Abstract
The perception of nursing staff’s attitude influences patient fear. Understanding this dynamic is crucial for fostering a supportive environment conducive to patient well-being and effective healthcare practices. The purpose of this research is to investigate how the attitudes and behaviours of nursing staff influence the fear and anxiety levels of patients recovering from benign tumors, aiming to improve patient care and recovery outcomes. Data was collected from a sample of 100 participants, comprising 20 nursing staff and 80 patients recovering from benign tumors. Surveys were administered to gather quantitative data on attitudes and fear levels. Participants were selected randomly from hospital records and outpatient clinics. Our analysis encompassed nursing staff attitude, patient fear levels, the influence of family support, progression of tumor recovery, patient-reported satisfaction, and the quality of healthcare services provided. The quantitative aspect utilized PLS-SEM software to perform regression analysis, evaluating both direct and indirect effects. Statistical analysis assessed the relationships between nursing staff attitudes, patient fear during benign tumor recovery, and the mediating role of family support. The findings of the study demonstrate that better nurse attitudes (Hypothesis 1, and stronger family support (Hypothesis 2, are linked to lower levels of patient fear. Partially mediating the relationship between nurse attitudes and patient fear, according to Hypothesis 3 , is family support. Patients’ perceptions of family support are highly influenced by nursing behaviour, as demonstrated by Hypothesis 4 . Our research showed a strong relationship between the attitudes of nursing personnel and patient fear levels. Family support demonstrated a strong mediating effect on patient fear. Patient-reported satisfaction is positively correlated with family support. However, no significant relationship was found between healthcare service quality and patient fear.Keywords
Recovering from benign tumors is not an easy task since patients have to undergo several operations that can be very unpleasant, which brings fear and anxiety towards the whole process of healing [1]. In the course of this journey, it is revealed that how the nursing staff approach the patients may help in a positive way to shape the patient’s perception towards the recovery process and/or emotional health. This discourse seeks to examine a relationship between the negativity of nursing staff work attitude toward patients recovering from benign tumors and the fear factor as a moderating variable via family support [2].
Being the primary interactants with the patients, nursing staff has a direct, significant impact on the experience that patients have in the course of treatment [3]. Since patients are vulnerable, their fears can be alleviated or heightened by the attitude, courtesy, and professionalism of the nursing staff. Positive work attitudes involving kindness, observation, and professionalism of employees have an impact on reducing patients’ anxieties and increasing their confidence to be cured, hence availing a suitable environment [4].
However, negative or indifferent attitudes from nursing staff may contribute to the exacerbation of patients’ anxieties, making them feel lonely, distrustful, and vulnerable. The preliminary study indicated that patient oncological reconditioning after benign tumor surgery may lead to uncertainty about their health. Here, the ‘healing’ attitude of the healthcare personnel who deal with such patients plays a central role in the recovery and building of the patients’ psychological coping strategies [5]. This form of vulnerability is underpinned by family support as a moderating factor. It remains an obvious truth that the family provides comfort and support for an array of patients, as they need motivation, love, and encouragement in their rehabilitation process [6].
When nursing staff shows a positive work attitude, then family members may be placed in a position to participate in the care of the patient to minimize the aspect of fear while at the same time enhancing the health of the entire being [7]. However, if the patient requires close and attentive nursing care, the pressure that is placed on the family may increase, thereby heaping more worries on the patient and hindering a healthy recovery [8].
The difficulty in confirming the relationship between nurse work attitude, patient’s fear, and the moderating effect of family support indicates the complexities involved in developing an effective patient-centered empathic communication model that demands healthcare institutions seriously consider the importance of efficient, comprehensive, and humane patient care [9]. Hospitals should actively encourage the culture of compassionate care in patients as well as caregivers by strengthening the support from families and healthcare personnel to ensure that they provide encouragement and hope to the patient going for benign tumor surgery or any other related treatment [10].
Inability to create a direct causal relationship between nursing staff attitude and benign tumor patients’ fear, mediated using family support due to methodological constraints. This study aims to determine how the nursing staff attitudes impact the fear level in benign tumor-suffering people with family support as a mediator. Recognizing these dynamics informs methods for reinforcement of patient care and therapeutic effects utilizing the PLS-SEM and quantitative analysis.
For convenience, we summarize below some of the frequently used acronyms in this paper:
TQM- Total Quality Management
HDAS- Hospital Depression and Anxiety Scale
PTG- Post-traumatic growth
VR- Virtual reality
MT- Music therapy
APAIS-A- Amsterdam Preoperative Anxiety & Information Scale–Anxiety
PONV- Postoperative nausea and vomiting
PROMIS- Patient-Reported Outcomes Measurement Information System
• Study highlights the significant impact of nursing staff attitudes on patient fear levels during benign tumor recovery, emphasizing the importance of positive nurse-patient interactions.
• The study underscores the crucial mediating role of family support in alleviating patient fear, suggesting that involving family members in the recovery process can enhance patient well-being.
• The quantitative aspect utilized PLS-SEM software to perform regression analysis, evaluating both direct and indirect effects.
• Statistical analysis assessed the relationships between nursing staff attitudes, patient fear during benign tumor recovery, and the mediating role of family support.
To examine how patient participation affects job satisfaction, helping behaviours, and work engagement in nurses, as well as patient satisfaction as recommended by Ding et al. [11], it also examined the moderating effects of length of stay, first inpatient stay, and nurses’ socio-demographic characteristics. Utilizing survey information from 522 inpatients and 282 nurses in a Chinese government medical facility, the study determined that patient engagement had a favourable impact on every result. Nurse Job satisfaction was impacted by age and organizational duration, but work engagement was unaffected or helpful behaviours, the effects on patient satisfaction were influenced by the length of stay and the initial inpatient admission.
Cole et al. [12] suggested investigating workplace elements that influence the propensity of registered nurses (RNs) to report unsafe behaviours and to advocate for their patients. Following Black’s study, which found that 34% of RNs were aware of potential patient damage but did not report it because of fear of reprisal and uncertainty about the efficacy of reporting, data were gathered from RNs working in acute care hospitals. The findings show that a proactive safety culture and a supportive work environment greatly increase RNs’ readiness to disclose problems, even while fear of reprisals indeed exists. To promote an encouraging atmosphere, education, professional associations, and protective legislation were essential.
Wang et al. [13] suggested to investigate how clinical nurses viewed the culture of patient safety were affected by total quality management (TQM), with a particular emphasis on relationships with work values and employee happiness. Data were gathered from 30 inpatient and 12 critical care unit surveys out of 700 valid ones that were distributed between 25 June and 05 July, 2015, across five regional teaching hospitals in Taiwan. Serial mediation analysis and structural equation modelling were used to examine a cross-sectional survey that included anonymous, self-administered questionnaires. Findings illustrated the importance of Total Quality Management (TQM) in creating a good work environment and enhancing safety culture among nurses by demonstrating how TQM both directly and indirectly improves attitudes toward patient safety culture through work values and employee happiness.
To find out how doctors and nurses felt about patient safety and to look at correlations between these attitudes, experience with adverse occurrences, and workload. Al-Mugheed et al. [14] recommended a descriptive cross-sectional design and involved 73 physicians and 246 nurses from two private hospitals in Northern Cyprus. The safety attitudes questionnaire’s Turkish version was used to collect the data. The findings showed that all patient safety domains were perceived negatively, with the least favourable perception being of the safety climate, while the most favourable perspective is of the working conditions. There were statistically significant variations in experiences, workloads, unfavourable incidents, and safety attitudes.
Hinz et al. [15] recommended assessing the measurement invariance of the Hospital Anxiety and Depression Scale (HADS), comparing depression and anxiety levels between cancer patients and the general population, and looking into disparities in age and gender. The HADS was used to evaluate these characteristics using information from 2747 members of the general community and 3785 cancer patients in Germany. The findings indicated that in comparison to age- and gender-matched members of the general population, cancer patients experienced slightly lower levels of depression but higher levels of anxiety. Notably, anxiety disproportionately affected young cancer patients. The study identified no significant interaction effects with clinical factors and validated measurement invariance across age and gender.
Li et al. [16] suggested examining how resilience relates to the impacts of anxiety and depression on PTG in breast cancer patients receiving chemotherapy. It involved 260 patients from a Shanxi hospital and was conducted between November 2017 and January 2019, using basic slope tests for moderation effects and hierarchical regression combined with structural equation modelling to evaluate mediation effects. Resilience strongly mediated and moderated the association between anxiety, depression, and PTG, according to the results, which were obtained using scales for anxiety, depression, resilience, and PTG. The highlights of the study were how psychological therapies were necessary to improve PTG by utilizing resilience.
The effectiveness of music therapy (MT) with immersive and interactive virtual reality (VR) in easing patients’ psychological discomfort during chemotherapy for breast cancer was recommended by Chirico et al. [17]. Thirty patients from the VR group, thirty from the MT group, and thirty-four from the control group getting normal care were involved. During treatment, the techniques included measuring anxiety, mood, and weariness. The findings showed that while both VR and MT reduced anxiety and elevated mood, VR was more successful than MT in lowering anxiety, despair, and exhaustion.
Kim et al. [18] suggested evaluating how a five-minute educational film on the Internet affected patients with colorectal cancer anxiety before surgery. Anxiety was assessed before and after watching the movie using the Hospital Anxiety and Depression Scale (HADS) and the Amsterdam Preoperative Anxiety and Information Scale-Anxiety (APAIS-A) in a prospective, single-arm observational trial with 32 patients. The APAIS-A (from 10.8 to 8.2,
Majumdar et al. [19] recommended assessing PA prevalence and effects on postoperative outcomes in patients undergoing outpatient cancer surgery [19]. 16.7% of patients in the retrospective cohort research, which examined 10,048 surgeries involving 8683 patients between January 2016 and April 2018, reported having preoperative anxiety. Increased rates of unplanned overnight admissions, urgent care visits, and postoperative nausea and vomiting (PONV) were associated with this worry. Treating 30 individuals for anxiety was necessary to avoid one case of PONV; even more patients were required to prevent other unfavourable outcomes. Subsequent investigations ought to examine the causal connection between worry before surgery and difficulties following it.
Mariani et al. [20] recommended looking into how coping mechanisms and the perception of social support affected symptoms of anxiety and depression during the COVID-19 lockdown. 96 healthy individuals (mean age = 39.3), 46 of whom were male, answered several questionnaires, such as the Multidimensional Scale of Perceived Social Support (MSPSS), the Symptom Checklist-90-Revised (SCL-90-R), and the Coping Inventory for Stressful Situations (CISS). The findings indicated that family support (FS) had a negative correlation with depressive symptoms, while emotion-focused coping had a positive correlation with both anxious and depressed symptoms. The results of multiple regression models showed that FS specifically reduced depressive symptoms, while emotion-focused coping strongly predicted both anxious and depressed symptoms. The results highlight the need to preserve family ties and employ efficient emotional regulation techniques to manage mental health throughout significant crises.
The relationship between anxiety, coping mechanisms, and family support in cancer patients receiving chemotherapy at the Dr. Pirngadi General Hospital in Medan was recommended by Sari et al. [21]. A correlational descriptive strategy was employed in the investigation, and 102 patients were chosen via purposive sampling. Questionnaires on anxiety, coping mechanisms, and family support were used to gather data. Significant negative correlations with Emotion Focused Coping (EFC) (r = −0.462) and anxiety (r = −0.646) and positive correlations (r = 0.612) between FS and Problem Focused Coping (PFC) were found in the bivariate analysis. FS was found to have a strong association with PFC (OR = 12.2) and a negative association with anxiety (OR = 0.039) and EFC (OR = 0.142) in multivariate analysis.
Psychosocial impact on cancer patients
Dorman-Ilan et al. [22] suggested assessing depression and anxiety in COVID-19 patients and their family members during the first hospital stay, with a particular emphasis on stress variables associated with socio-demographics and the pandemic. Telephone interviews were conducted with 90 hospitalized patients and 125 adult and paediatric relatives between 25- and 72-h following admission to gather data. In addition to qualitative questions about anxieties, melancholy, and coping mechanisms, the approaches included quantitative assessments utilizing the PROMIS Anxiety and Depression modules. The findings showed that both groups had elevated anxiety levels and fewer depression symptoms. Anxiety was higher in adults than in youngsters, it was higher in females, and it was lower among participants who were ultra-orthodox. Feeling alone was linked to anxiety in patients, but anxiety among relatives was associated with feeling unprotected by the hospital.
The impact of control locus, coping versatility (CV), and family resilience (FR) on the mental health of breast cancer patients during the COVID-19 pandemic was recommended by Brivio et al. [23]. The study finds that FR and an internal control locus significantly enhance positive affect and mitigate negative emotions. Data from 154 patients were analyzed using Walsh’s FR questionnaire, the mini control locus scale, the perceived ability to cope with trauma scale, and the positive-negative affect schedules. To increase patient adaptation and stress management, it is recommended that programs supporting FR and CV be developed by clinical psychologists.
Previous studies have explored numerous aspects of the nursing staff attitudes, including patient engagement, quality management, and workspace characteristics, but there is a gap in understanding how these attitudes especially impact the fear and anxiety levels of the patient recovering from benign tumors. This gap suggests a requirement to focus on the interactions and behaviours of the nursing staff that could improve the patient’s anxiety, potentially improving the overall patient care and recovery outcomes. To enhance the patient care and recovery results, this study examined how nursing staff attitudes and behaviours affect the patient’s levels of fear and anxiety while they recover from benign tumors.
Hypothesis 1 (H1): There is a negative correlation between the nursing staff’s positive work attitude (NSPWA) and the level of fear experienced by patients (LFEP) recovering from benign tumors.
This hypothesis proposes that there is a negative relationship between the nursing staff’s good work attitudes and the degree of fear experienced by patients recuperating from benign tumors. It refers to the nursing staff’s constructive behaviours that enhance the patient’s level of fear. This hypothesis claims that nursing staff’s voice and behaviour affect the patient’s recovery from emotional illness.
Hypothesis 2 (H2): The higher levels of family support (LFS) are associated with LFEP improvement from benign tumors.
This hypothesis implies a negative association between nursing staff professionalism and the level of fear indicated by patients recuperating from benign tumors. If the nursing staff’s positive attitude increases, patients’ dread decreases, and vice versa. This hypothesis posits that the nursing staff’s style and conduct may influence patients’ emotional states during rehabilitation.
Hypothesis 3 (H3): The LFS mediates the link between NSPWA and LFEP recovering from benign tumors.
This hypothesis, which also necessitates taking into account the function of mediation, holds that family support mediates the relationship between the work attitude of nursing staff and patients’ levels of dread in cases of benign tumors. Stated differently, this implies that the degree of family support plays a role in mediating or perpetuating the link between the fear of the patient and the good work attitude of the nursing staff. The relationship between nursing staff attitudes and patient outcomes is discussed in this theory as being mediated by family support.
Hypothesis 4 (H4): NSPWA has a rapid effect on the level of family support perceived by patients (LFSP).
This hypothesis proposes that nursing staff’s work attitude is connected to patients’ perceived family support. This implies that nursing personnel’s behaviour can influence patients’ perceptions of family support. In other words, it indicates that when the nursing staffs offer a positive attitude at work, patients might indicate greater support from family or parents. On the contrary, if the nursing staffs exhibit a negative attitude toward work, the rise may create poor reporting of family support.
Fig. 1 shows the basic model, which is composed of primary independent variables, such as NSPWA. LFS is the mediated variable. The dependent variables are LFEP and LFSP that results from the interplay of these elements will be the primary focus of the study.
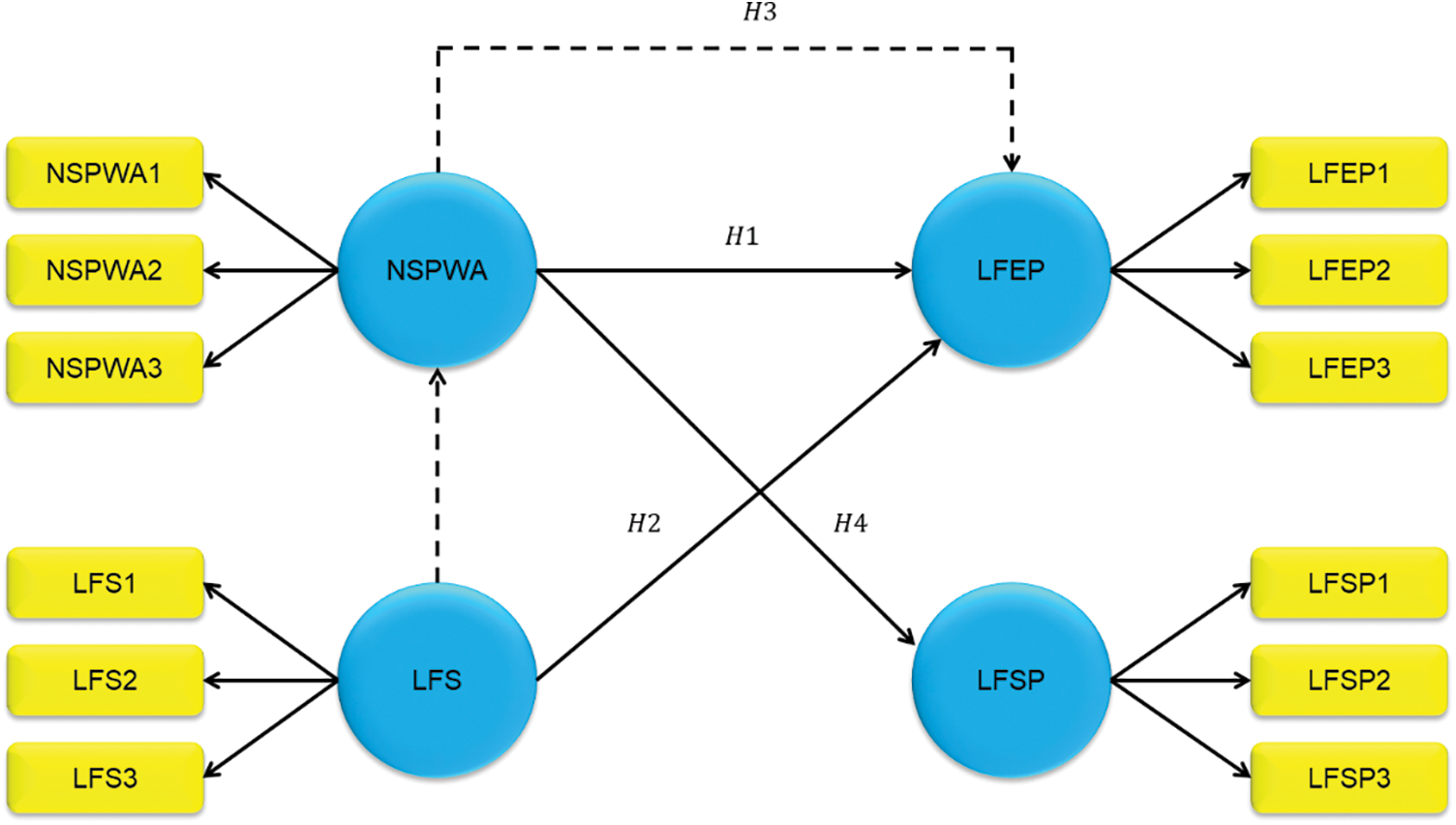
Figure 1: Conceptual model
The research was carried out in an extensive regional hospital in China that specialized in tumor treatment. This location was selected due to its varied patient population and highly skilled nursing staff. This arrangement offers abundant chances to investigate the effects of nursing attitudes and family support on patient outcomes.
250 adult patients (18 years of age and older) with benign tumors undergoing varying stages of treatment data were included in the study. They were chosen between 2022 and 2023 from the oncology wards. The study has 100 patients’ data who were receiving therapy for benign tumors and fulfilled the inclusion criteria. 150 people in the exclusion criteria had severe cognitive impairment or comprehension-impairing linguistic obstacles. The confidentiality of the data used in the study is of paramount importance, and as such, it cannot be shared due to privacy and ethical considerations. The data contains sensitive information about patients and healthcare providers and sharing it could pose significant privacy risks. Furthermore, the hospital where the data was collected has strict ethical and legal regulations in place that explicitly prevent the release of such confidential data. Therefore, in compliance with these regulations and to uphold the highest standards of ethical conduct, the data cannot be made publicly available.
This study, approved by the ethical committee of Krirk University (approval number IRB2022-1234-ABCD), used participant data from individuals receiving therapy for benign tumors. Researchers ensured confidentiality and privacy protection for participants, following ethical guidelines. Explicit consent was obtained from all participants, and data integrity is maintained throughout and after the study.
To choose participants for this study from the intended population, we used a random selection technique. To give each eligible patient in the oncology wards an equal chance of being included in the trial, random sampling was adopted. Results from this method may be trusted and generalized since it reduces selection bias and improves sample representativeness.
The variables used in this study consist of three types, such as dependent variable, mediating variable, and independent variable.
Independent Variable: Nursing Staff’s Positive Work Attitude (NSPWA);
Mediating Variable: Levels of Family Support (LFS);
Dependent Variable: Level of Fear Experienced by Patients (LFEP), level of family support perceived by patients (LFSP).
The data collection of 100 different patients from various hospitals consists of components such as diagnosis, family support, age, gender, and educational level of healthcare providers. It also has survey data collected from several levels, including the nursing staff’s positive work attitude (NSPWA), the level of fear experienced by patients (LFEP), the level of family support (LFS), and the level of family support perceived by patients (LFSP). Tables 1 and 2 represent the hospital’s patient and nursing staff demographics. Figs. 2 and 3 show the characteristics of demographics.
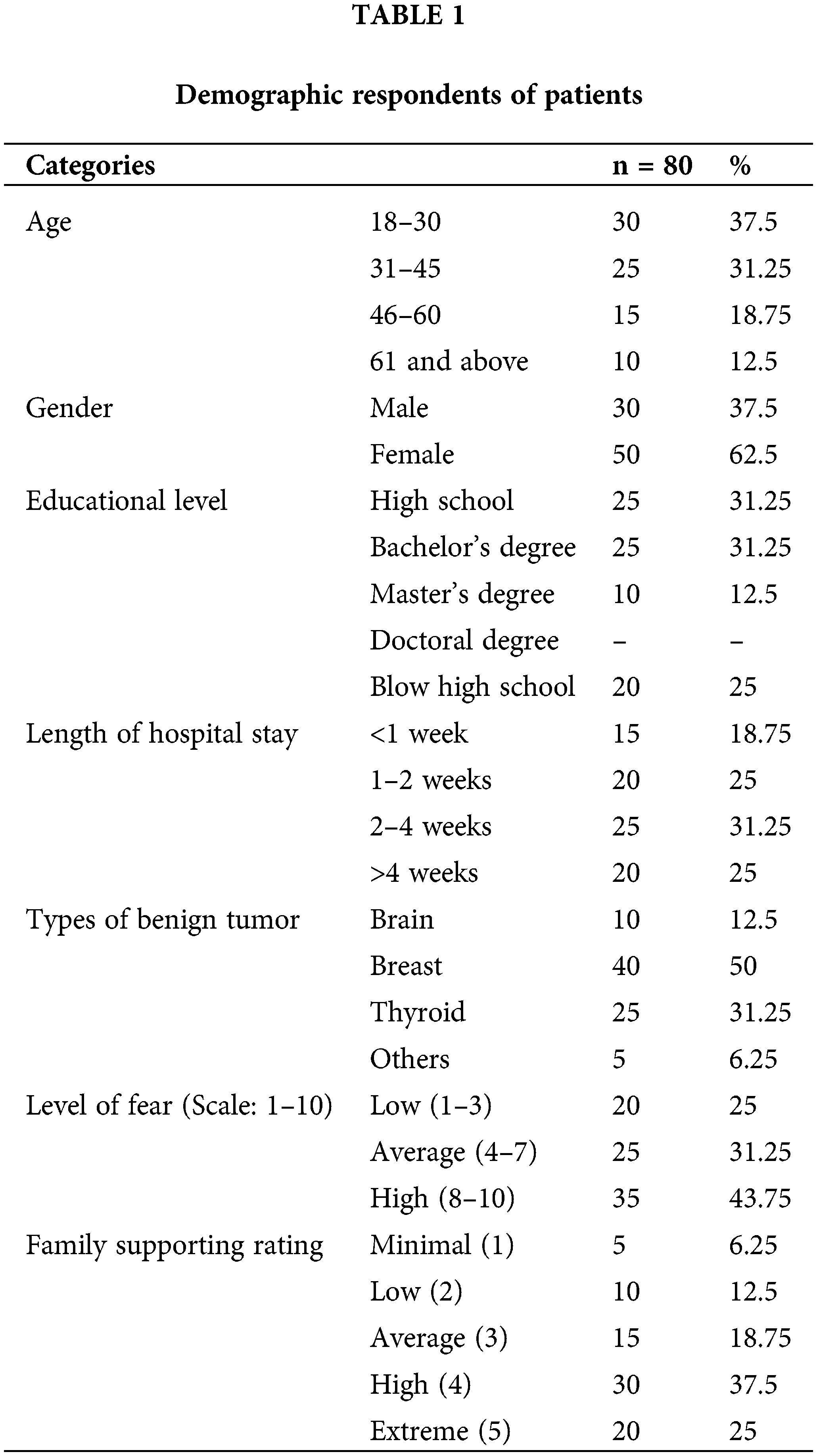
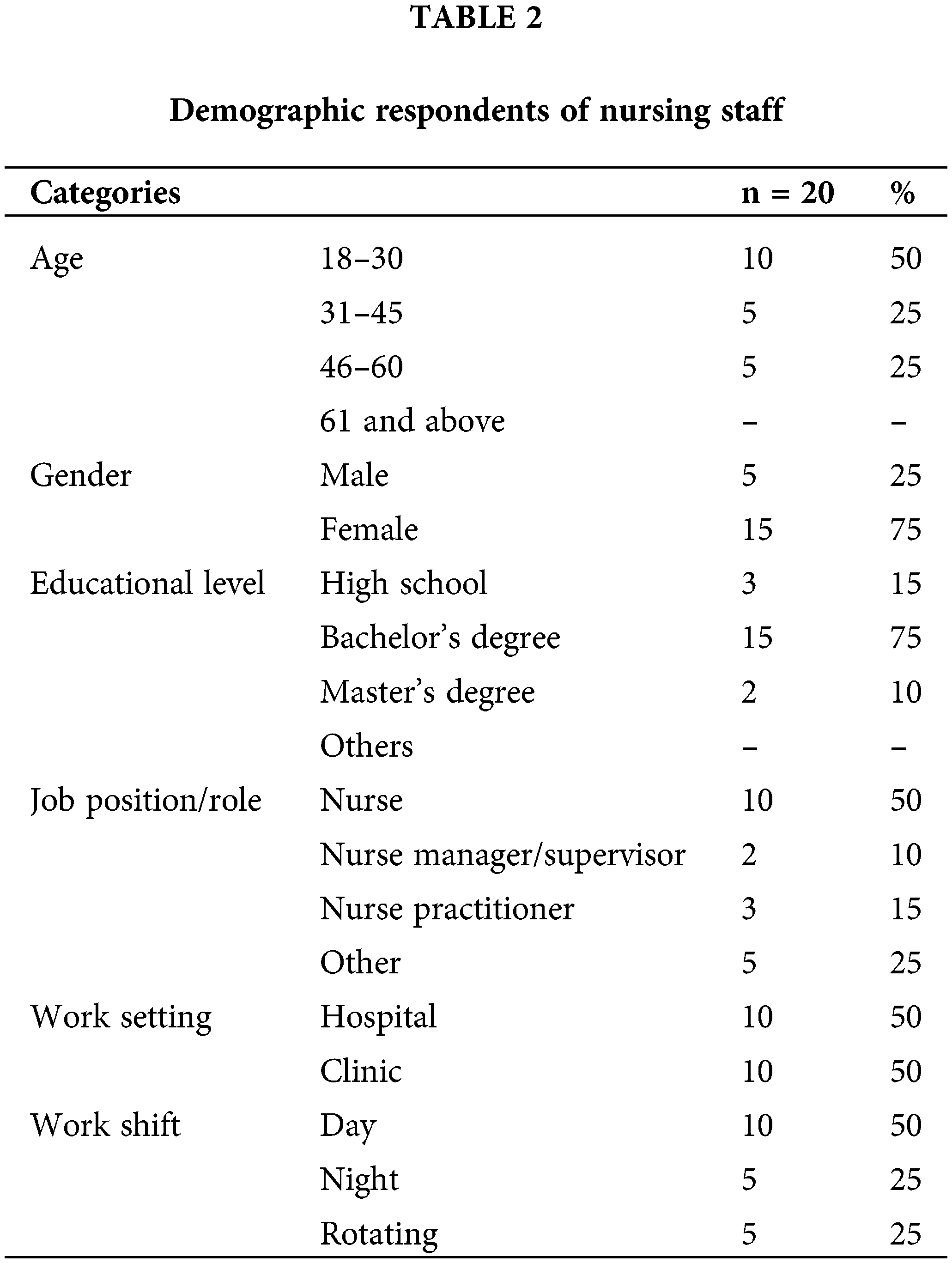
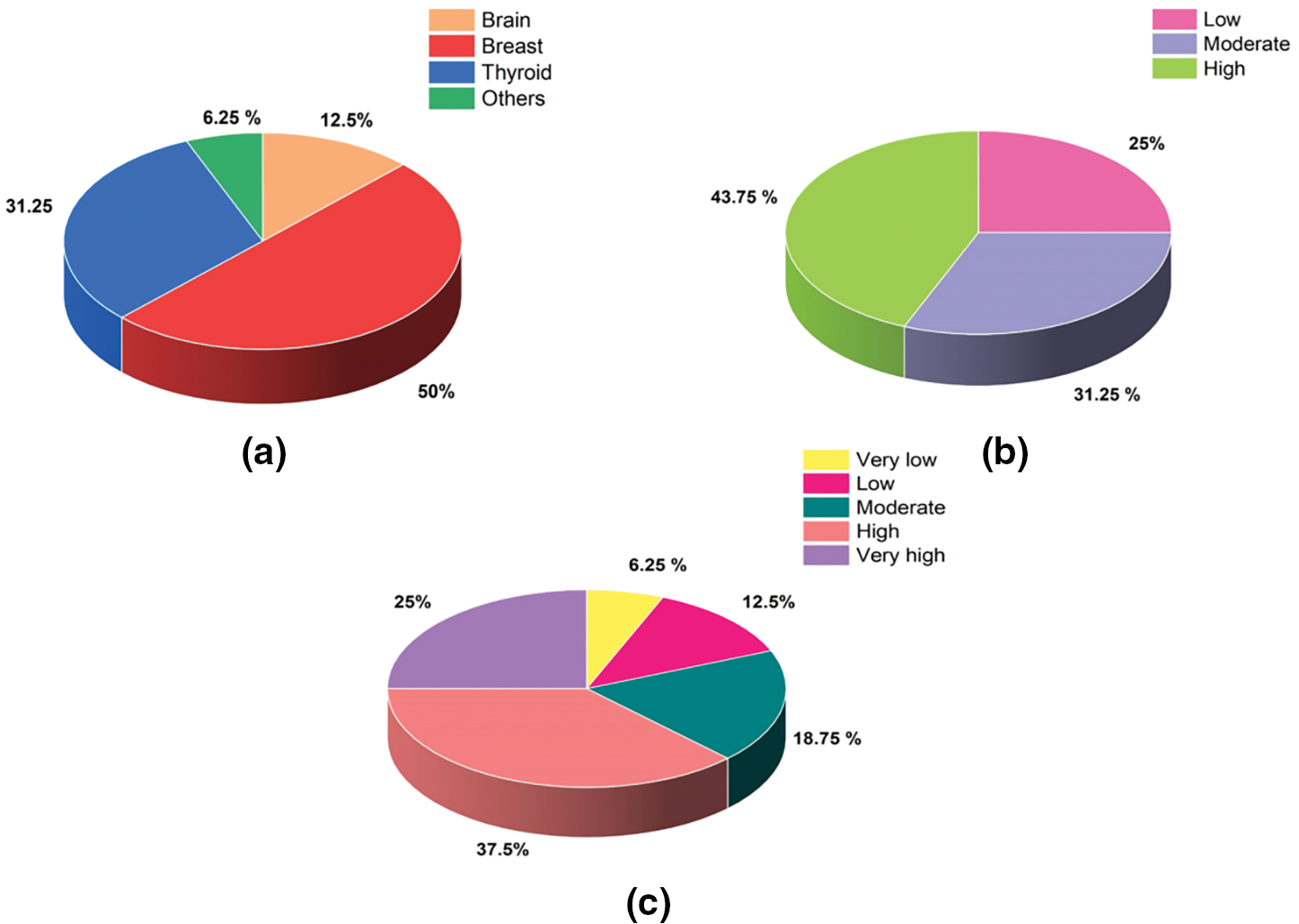
Figure 2: Patients (a) Types of benign tumor (b) Level of fear (c) Family supporting rating
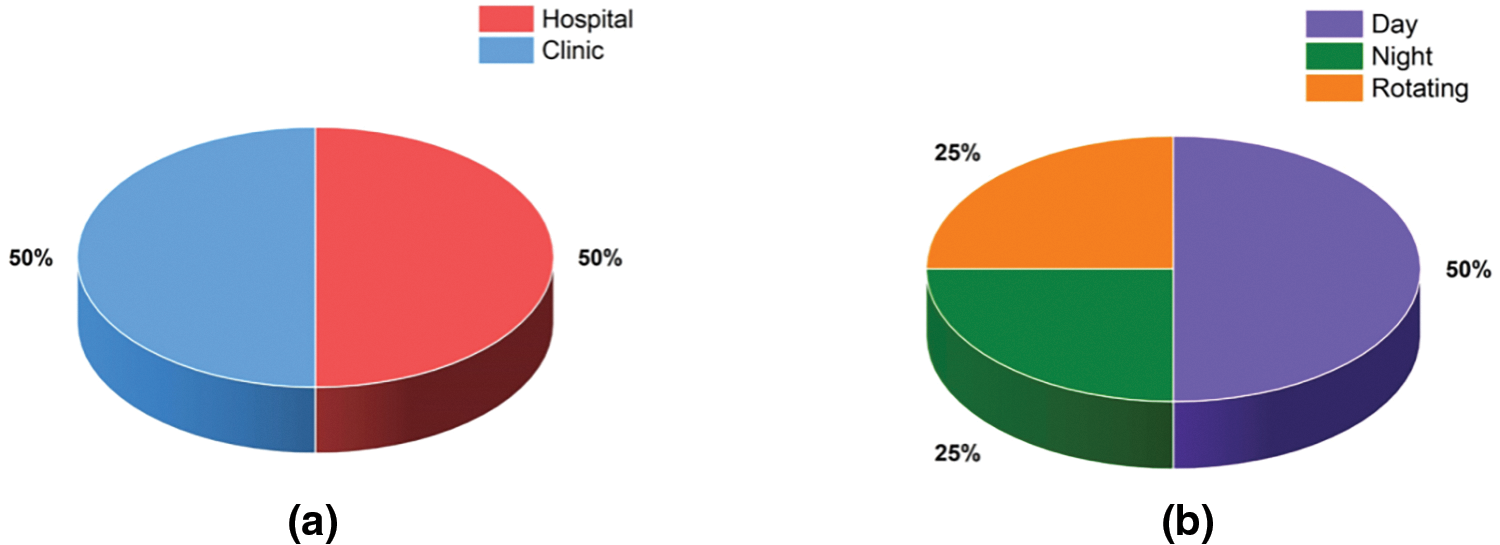
Figure 3: Nurse staff (a) Work setting (b) Work shift
A questionnaire design was created after an extensive evaluation of the research on the effect of nursing staff’s work attitudes on patients’ fear of recovering from benign tumors. The first stage in this procedure is to design a questionnaire that includes five crucial components. Appendix A displays the variables in the questionnaires.
1. Demographic Information: Surprisingly, ten questions were asked about the respondents of patients and nursing staff.
2. Nursing Staff’s Positive Work Attitude (NSPWA): These three questions were in this area and focused on nursing staff attitudes.
3. Level of Fear Experienced by Patients (LFEP): This section has three questions that relate to the degree of fear exhibited by a patient.
4. Levels of Family Support (LFS): Three questions in this part revolved around the effects of the level of family support.
5. Level of Family Support Perceived by Patients (LFSP): The last part was comprised of three questions aiming at capturing the patients’ perception of the family support level.
6. The questionnaire of the variables is ranged by using a 5-point Likert scale. The point such as strongly disagree (1) to strongly agree, (5) very poor, (1) to excellent (5), not confident at all (1) to very confident (5), no fear (1) to extreme fear, (5) not concerned (1) to extremely concerned (5), not at all (1) to extremely (5), not at all (1) to completely (5), never (1) to always (5), none (1) to extensive (5), and none (1) to a great deal (5).
Partial least squares structural equation modelling (PLS-SEM) is a statistical method for examining difficult relationships between latent variables in structural equation models. Unlike classic covariance-based SEM, PLS-SEM is ideal for exploratory research or for analyzing small numbers of samples, non-normal data, or complicated models with several variables. The model is estimated using PLS-SEM by repeatedly maximizing the explained variance in the variables of dependence while minimizing the residuals. The framework model and the evaluation model are its two main methods for doing this. The measurement model looks into the relationships between observable variables and implicit presumptions to assess the validity and reliability of the measuring tools. This entails evaluating factor loadings, composite reliability (CR), and the average variance extracted (AVE). The structural model examines the links between latent components to test hypotheses and determine the intensity and importance of both direct and indirect impacts. PLS-SEM calculates the coefficients using bootstrapping approaches to determine their significance and offer confidence intervals.
Evaluation of measurement model
The measurement tools were created using accepted theoretical frameworks that were pertinent to the concepts under evaluation. This framework aided in the creation and selection of items by offering a detailed conceptual grasp of the constructs. If a measurement tool is particular to the group under study and yields consistent results after multiple administrations, it is said to be reliable. When assessing measuring tools, several types of reliability are crucial. Test-retest reliability, for example, measures the consistency of the tools over time, whereas internal consistency gauges the degree of relationship between a group of items or questions. Internal consistency is typically measured using Cronbach’s alpha, also known as coefficient alpha. Nevertheless, this statistic assumes tau equivalency, which may not hold in practical applications. Coefficient omega offers alternate scale reliability metrics to overcome this.
Tests for validity and reliability were performed and results showed that the measures were error-free and reliable because the AVE, CR values and Cronbach’s alpha were higher than the minimal allowed values. Convergent validity analysis also confirmed that there was no cross-loading onto other component factors and that each item was loaded onto a single component factor. To assess statistical significance and bolster the convergent validity of the two measurement models’ components, the critical ratio (CR) was employed. The findings also provided support for discriminant validity, which holds that a single item should only assess one latent construct at a time and not several latent constructs. Each latent variable’s AVE was greater than the squared correlation for the same pair, suggesting that each construct was unique and distinct from the others.
Table 3 summarizes the measurement model assessment, which assessed the validity and reliability of constructs such as LFSP, NSPWA, LFS, and LFEP. Each construct’s loading values, Cronbach’s alpha (α), AVE, and CR are presented. Values above 0.70 for loading, α, and CR, as well as above 0.50 for AVE, indicate high reliability and validity. In this scenario, all constructions meet or surpass the criteria, indicating strong measurement model performance. As a result, the items accurately assess their target structures, having high validity convergence and internal dependability.
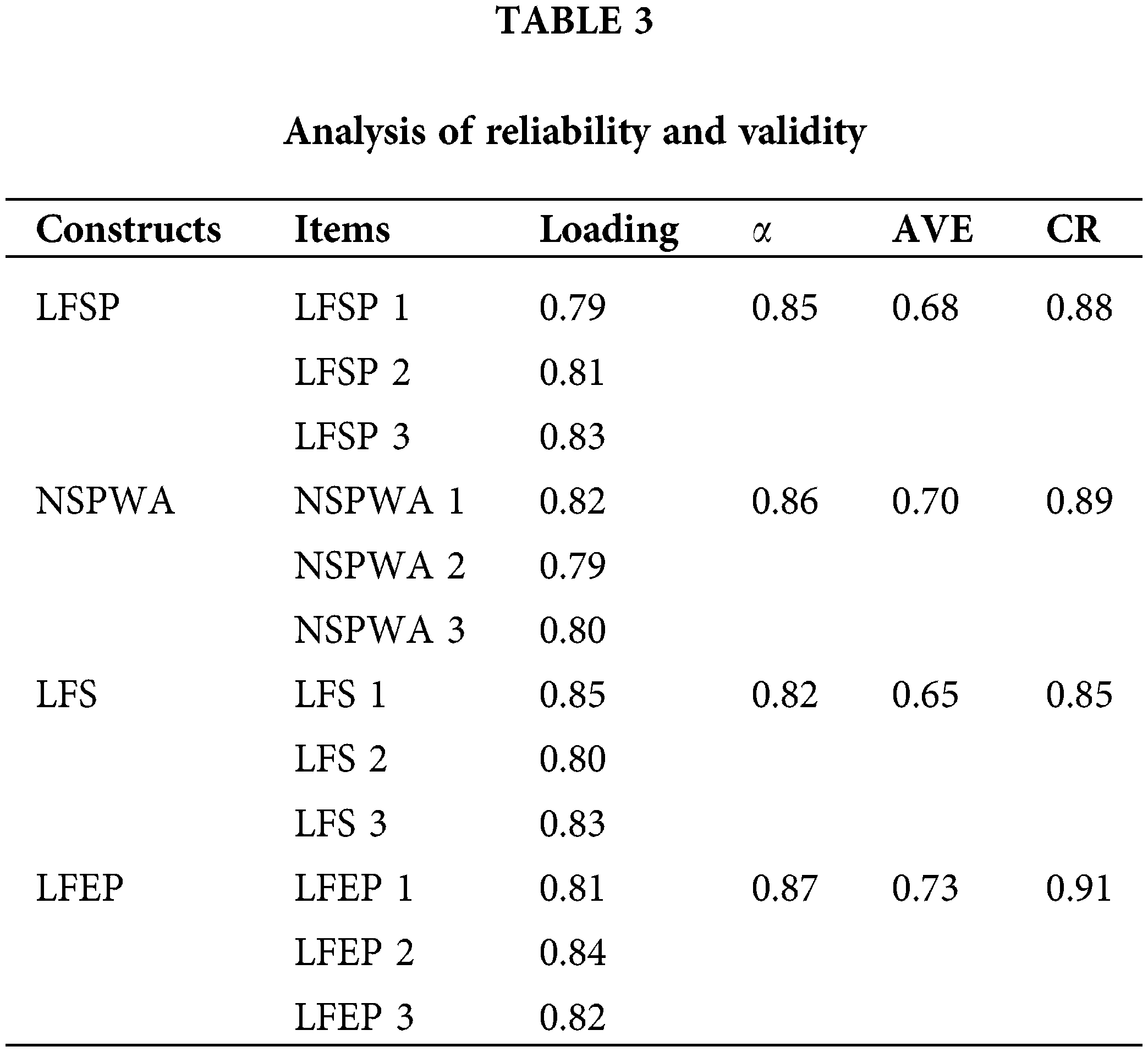
Table 4 shows that the square root of each construct’s AVE (diagonal components) is larger than its association with other constructs (off-diagonal components). This verifies the constructs’ discriminant validity, demonstrating that each construct is separate and assesses a unique idea when compared to others.
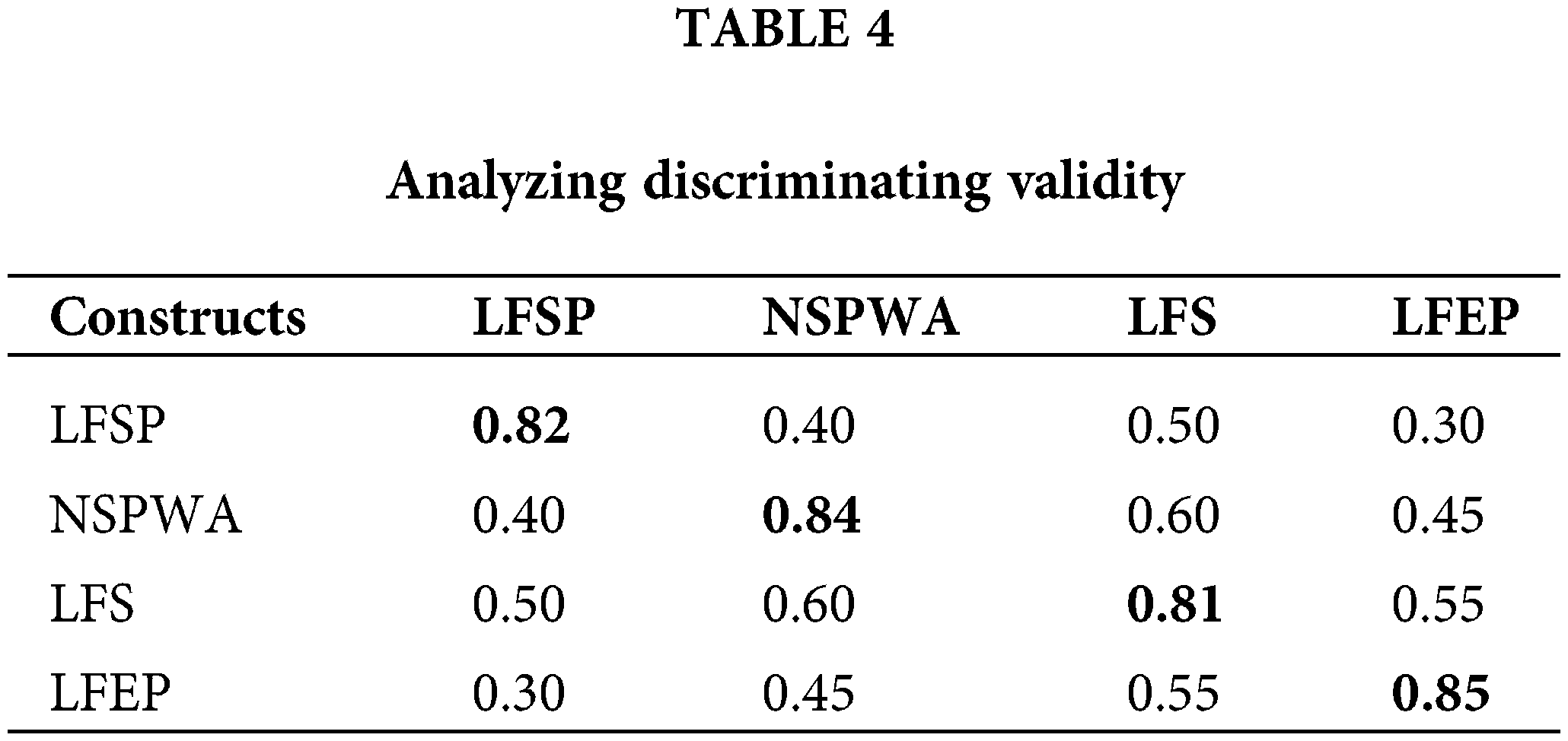
Table 5 shows the variance influencing variables (VIF) for each construct in the context of a study hypothesis. Variation influence variables assess how much each component adds to the total variation in the study model. In this situation, the constructions denote factors. Table 5 shows the numerical influence factor for each construct, which represents its relative relevance in explaining the changes reported in the study model. For example, a higher influence factor indicates that the construct contributes more to the total variability in the model. This information aids in understanding the relative relevance of various components within their study framework, allowing for more informed interpretations and implications for future investigations. Fig. 4 shows the outcome of the assessment model.
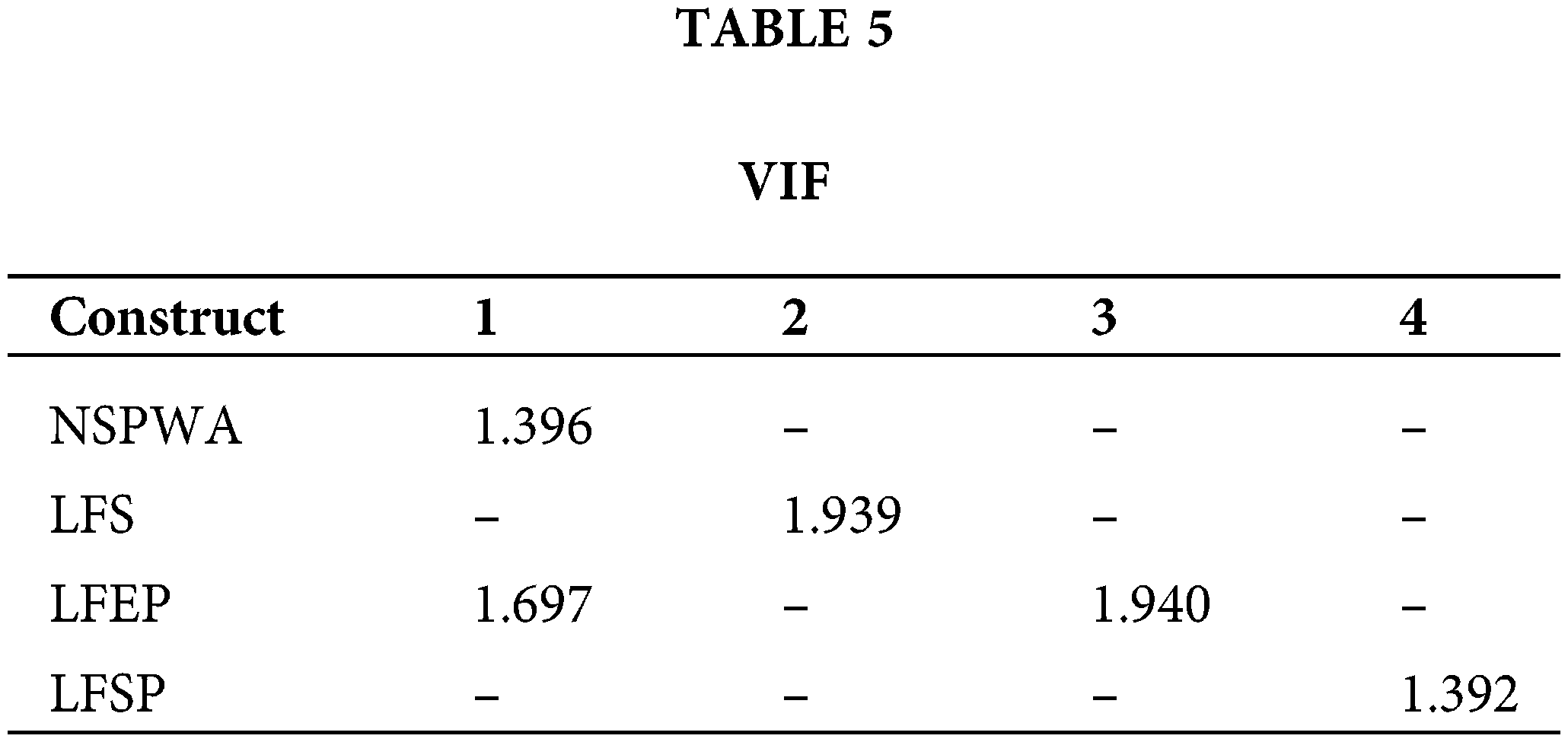
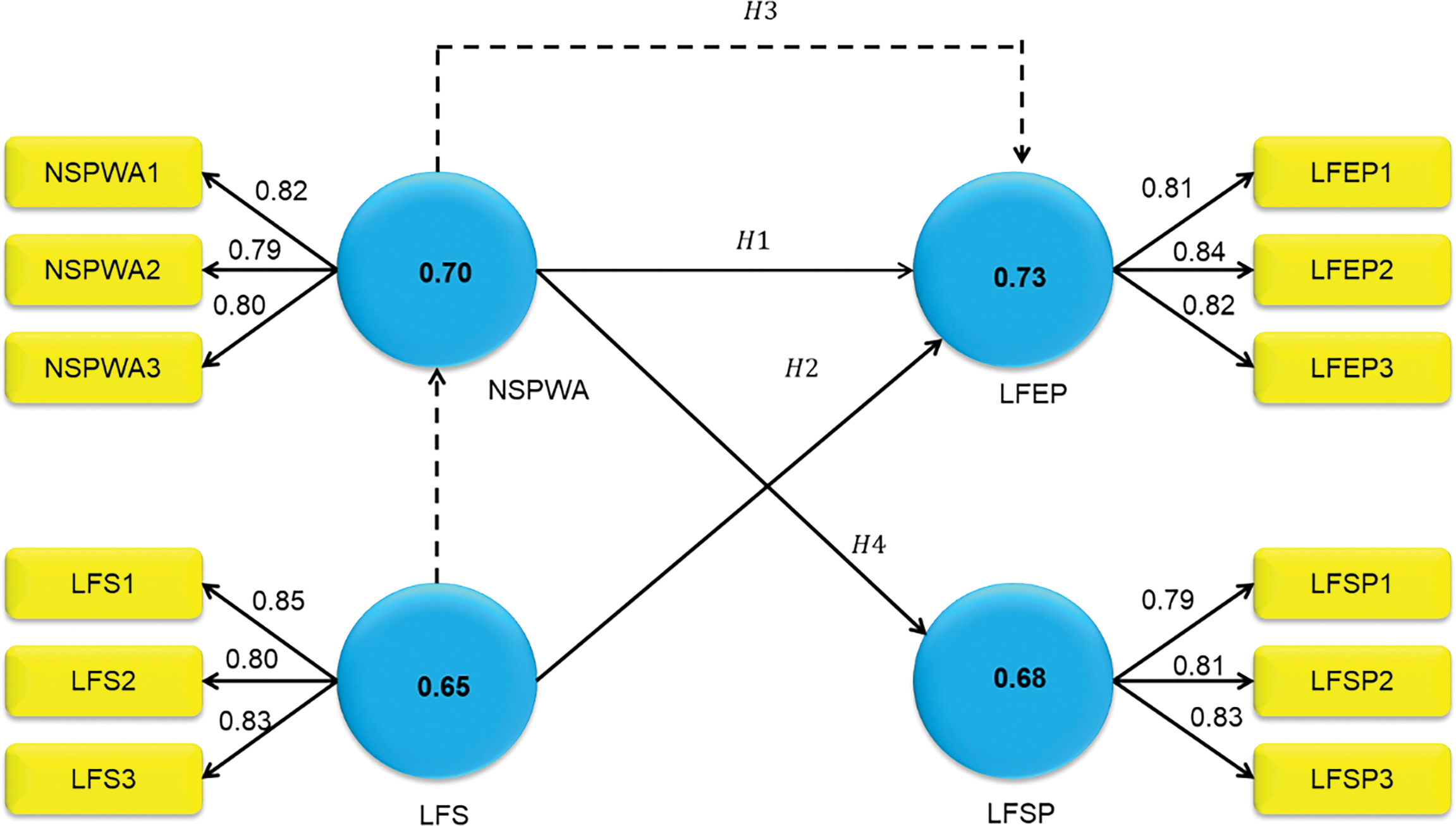
Figure 4: Outcome of measurement model
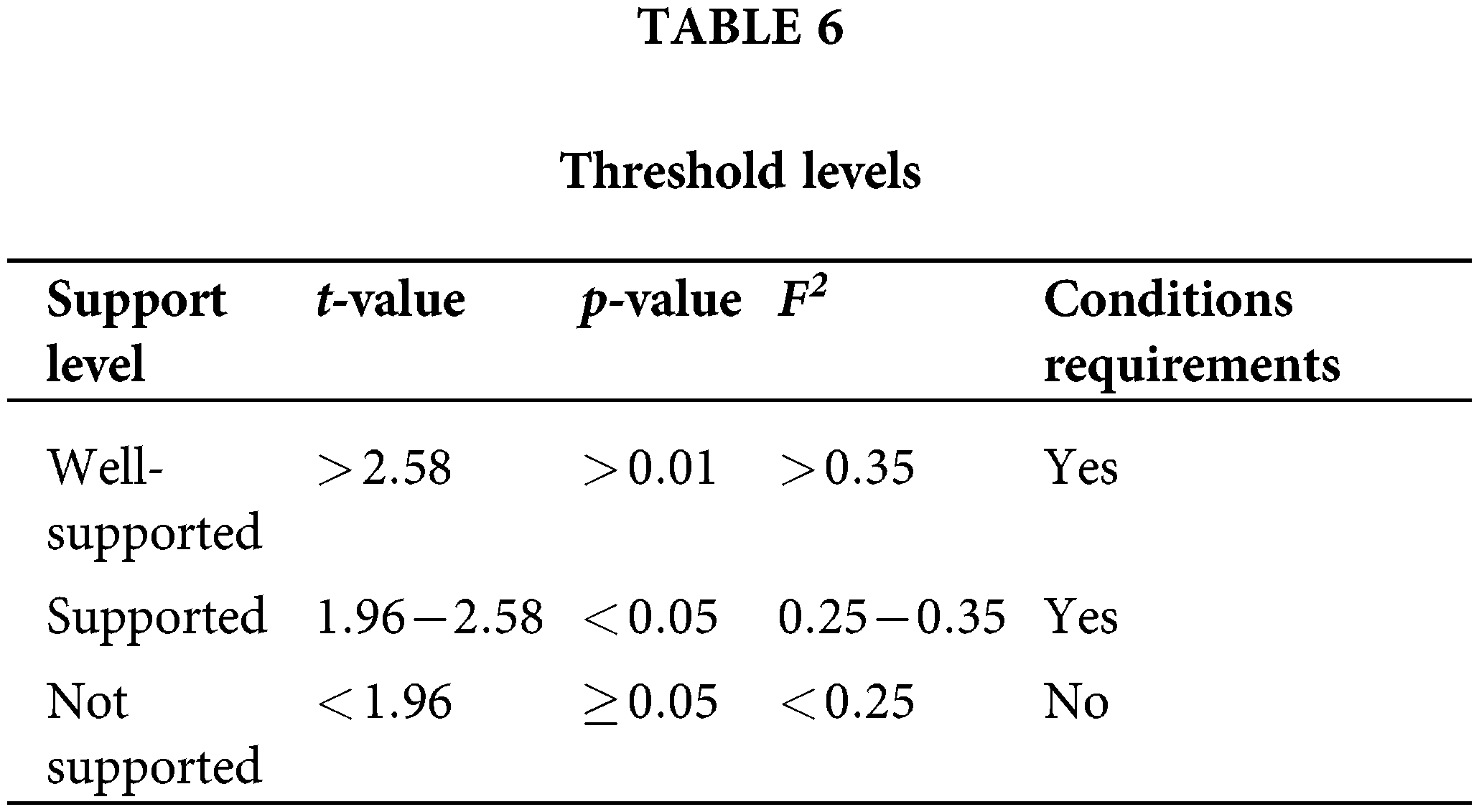
Table 6 shows an exhaustive overview of the hypothesis explored within the study framework. The directional associations between predictor and outcome variables are examined for each hypothesis using path
When
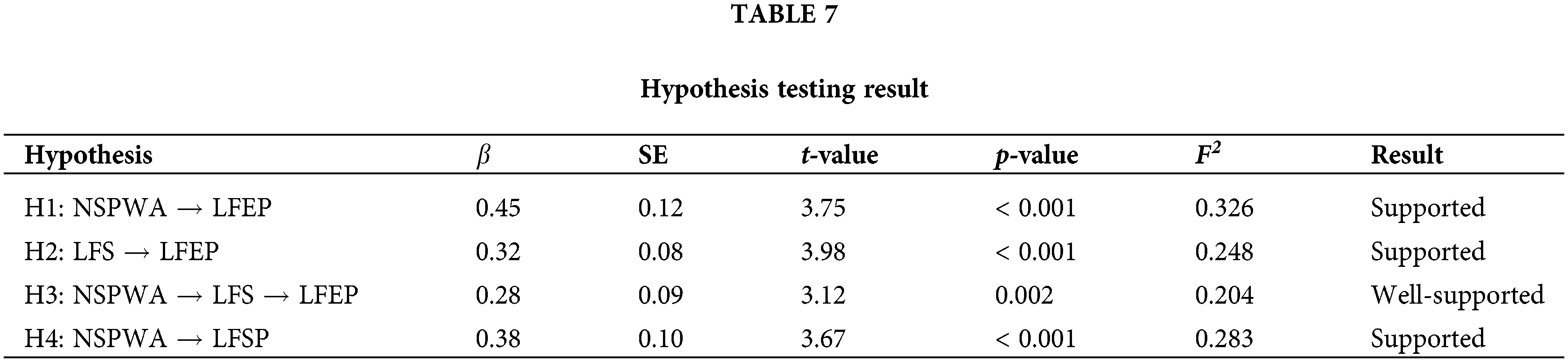
Fig. 5 depicts the results of the structural model.
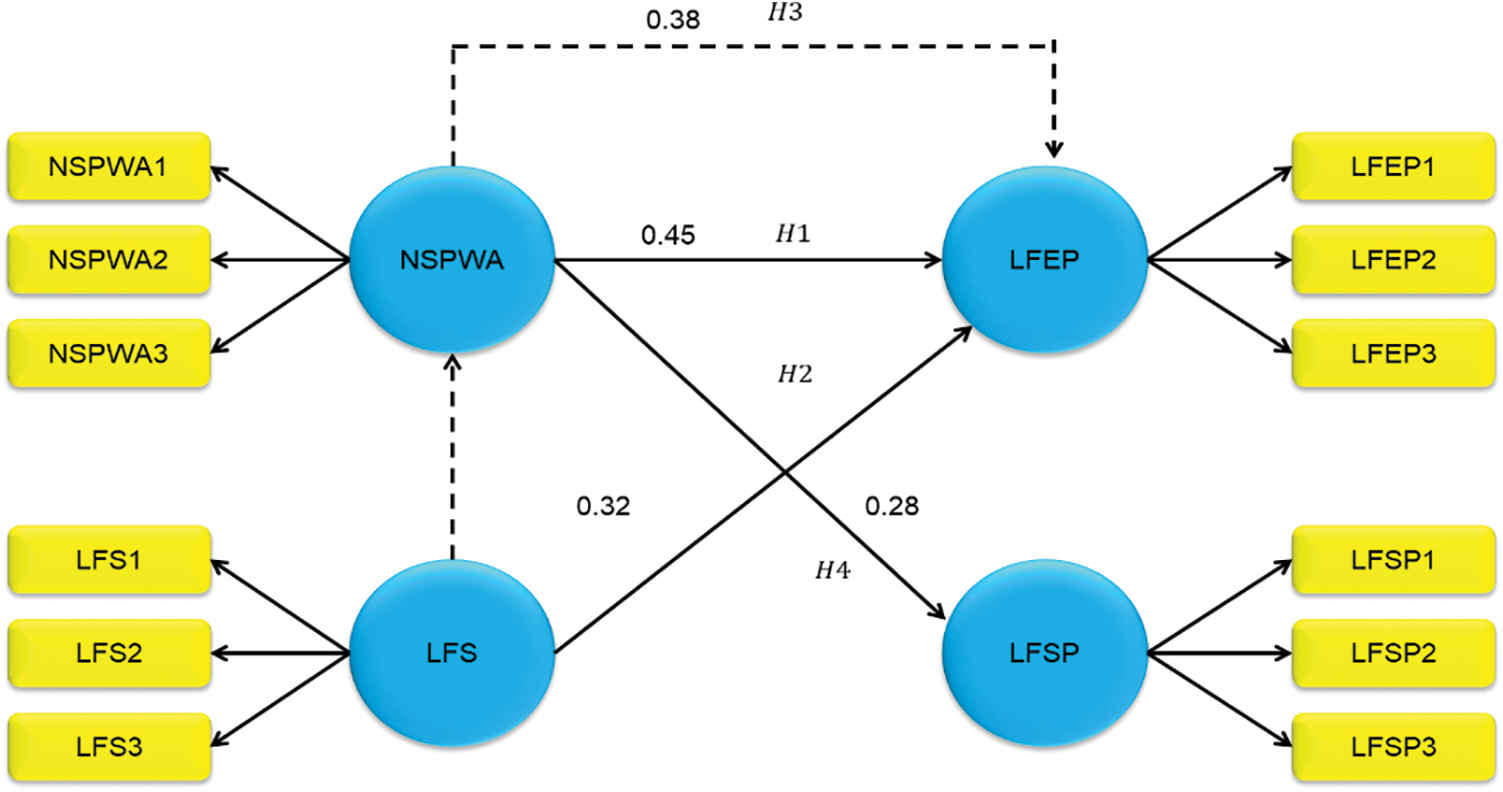
Figure 5: Result of structural model
The patients receiving spinal intramedullary tumor resection experienced significantly fewer problems, higher quality of life, lower anxiety and sadness, and increased nursing satisfaction following surgery (p < 0.05) due to postoperative refined nursing [24].
The 310 participants ranged in age from 17 to 62 years old. Of them, 48.1% were nurses and midwives, 13.9% were technicians and laboratory workers, 16.5% were doctors, 16.5% were secretaries, and 5.2% were students. In terms of screening for breast cancer, 63.5% regularly performed breast self-examinations (BSEs). Among the subjects, 58.4% had never had a Pap smear test, 27.7% had never had a gynecological checkup, and 60.3% had never undergone mammography (MMG) or ultrasonography (USG) [25].
Out of 148 individuals with lung tumors, 45 did not experience any anxiety or sadness, whereas 103 did. Income, sleep quality, and psychological state within the family were important factors influencing psychological state. Income, mental state of the family, anxiety about sleep quality, and type of tumor were found to be risk variables by multivariate analysis. Compared to the control group, the study group had better medication and life behaviours at discharge, as well as lower HAD scores [26].
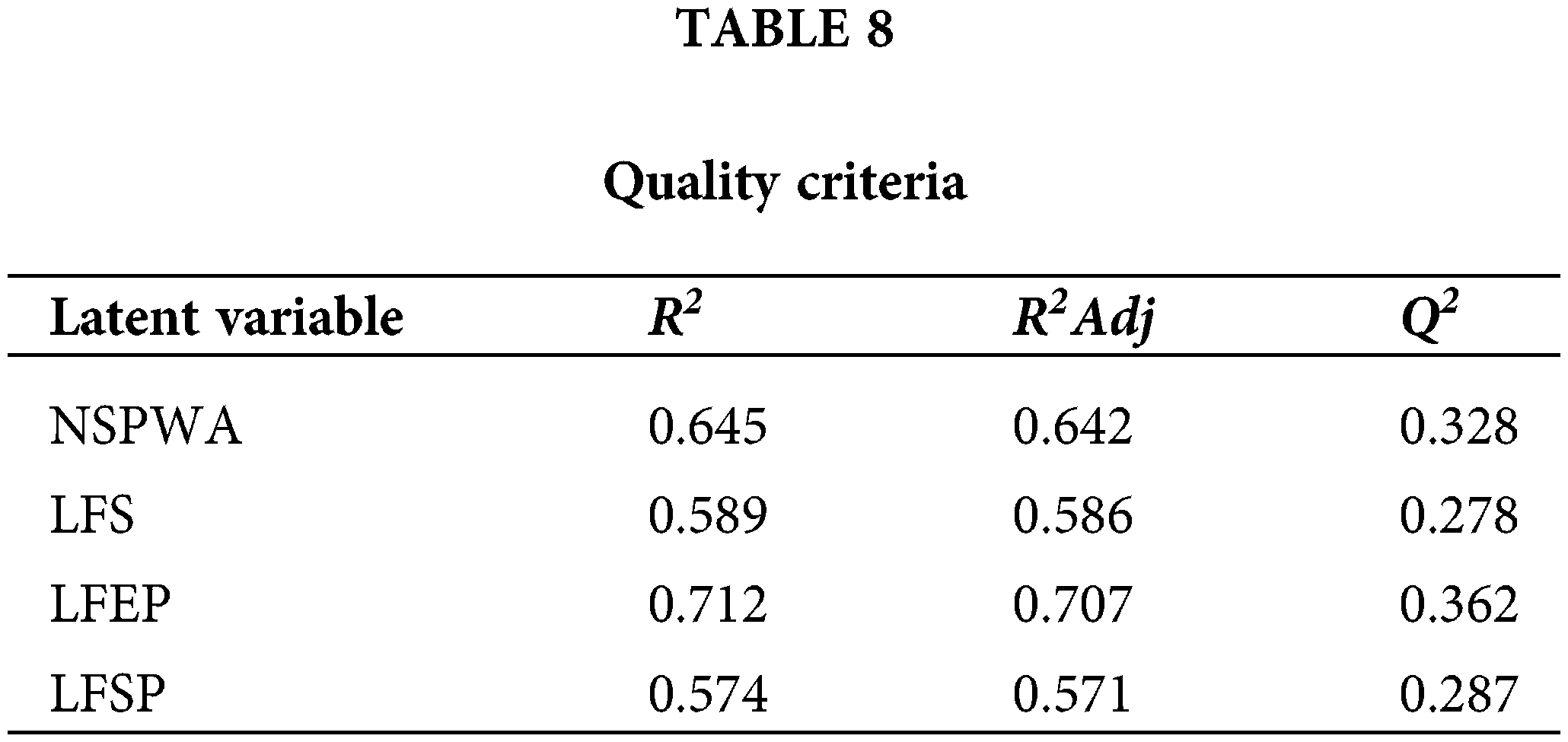
This section provides significant support for the research’s hypotheses, highlighting the role of support from families as a mediator in reducing patient worry. Hypotheses examining the effect of nursing staff’s positive attitude and amount of familial support on patient dread were shown to be significant, with p-values showing statistical significance. Table 6 displays the findings of studies on NSPWA, LFS, and LFEP in the recovery from benign tumors. Better nurse attitudes and more family support are correlated with lower patient dread, according to the results of Hypothesis 1 and Hypothesis 2, which both showed significant positive relationships (β = 0.45 and 0.32, respectively, p < 0.001). A partial mediation of the association between nursing attitudes and patient dread is suggested by the strong support for Hypothesis 3, which tested mediation (β = 0.28, p < 0.002). According to Hypothesis 4 (β = 0.38, p < 0.001), the study demonstrates that patients’ perceptions of family support are significantly influenced by nursing behaviour. Notably, Hypothesis 3 proved to be particularly solid, revealing a well-supported link in which nursing staff’s good work attitude increases patient dread via the impact on family support. This study emphasizes the significant function of family support in reducing patient worry during recovery, emphasizing its significance in healthcare settings. Overall, the findings provide realistic evidence for the significance of encouraging satisfying relationships among the nursing staff and patients, underscoring the tremendous authority that a supportive environment has on patient well-being.
The limited sample size of 100 people selected from hospital and outpatient clinic records could limit the generalizability of the study’s conclusions. It is important to exercise caution when interpreting the findings of larger studies because potential biases in sampling techniques can affect how representative the patient and nursing staff groups under investigation are as a result. The future scope can encompass investigating longitudinal effects to evaluate long-term implications, integrating varied healthcare settings to make findings more broadly applicable, and integrating nursing staff attitudes and family support treatments into practice to enhance patient outcomes.
The perception of the nursing workforce’s attitudes substantially affects affected person fear levels, underscoring the importance of fostering a supportive environment for patient well-being and powerful healthcare practices. This study investigated the effect of nursing staff attitudes and behaviours on fear and tension stages amongst sufferers improving from benign tumors, aiming to enhance affected person care and restoration effects. Data from 100 participants, which included 20 nursing personnel and 80 patients, was gathered through surveys administered randomly from hospital information and outpatient clinics. Analysis, using the PLS-SEM software program, targeted statistical evaluation to evaluate direct and indirect consequences. Results discovered an enormous correlation between the nursing body of workers’ attitudes and patient worry degrees, with a circle of relative aid performing as a strong mediator. Patient-reported pride undoubtedly correlated with own family help, whilst no huge courting was found between healthcare provider greatness and affected person fear. Understanding those dynamics is essential for growing a supportive environment conducive to affected persons’ well-being and improving healthcare practices for people getting better from benign tumors. A small sample size may additionally restrict generalizability. Future studies could explore various patient populations and healthcare settings. Investigate interventions to improve nursing workforce attitudes and beautify own family aid for better-affected person outcomes.
Acknowledgement: All the authors have contributed equally to the research, manuscript preparation and writing. All the details have been listed under the author contributions statement.
Funding Statement: The authors received no specific funding for this study.
Author Contributions: The authors confirm their contributions to the paper as follows: study conception and design: Chengzhe Guo; data collection: Aihua Cheng and Jian Chen; analysis and interpretation of results: Chengzhe Guo; draft manuscript preparation: Chengzhe Guo and Aihua Cheng; data collection, review and editing: Gaojie Cheng. All authors reviewed the results and approved the final version of the manuscript.
Availability of Data and Materials: The data used for the study is collected from a hospital. Due to the data policies of the hospital and ethical guidelines, the collected data cannot be publicly shared. This statement has been clarified on the manuscript as well. Primary health care corporation (PHCC) is the data set owner. PHCC organisational policies allow for the release of data for research purposes only and do not permit publication of the raw data.
Ethics Approval: This study was approved by the Ethical Committee of Krirk University (approval number IRB2022-1234-ABCD), explicit consent was obtained from all participants, and data integrity is maintained throughout and after the study.
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
References
1. Gillis C, Gill M, Gramlich L, Culos-Reed SN, Nelson G, Ljungqvist O, et al. Patients’ perspectives of prehabilitation as an extension of Enhanced Recovery After Surgery protocols. CanJ Surg. 2021;64(6):E578. doi:10.1503/cjs.014420. [Google Scholar] [PubMed] [CrossRef]
2. Shao M, Yang H, Du R, Zhang M, Zhu J, Zhang H, et al. Family resilience in cancer treatment and key influence factors: a systematic review. Eur J Oncol Nurs. 2023;66:102403. doi:10.1016/j.ejon.2023.102403. [Google Scholar] [PubMed] [CrossRef]
3. Kwame A, Petrucka PM. A literature-based xref of patient-centered care and communication in nurse-patient interactions: barriers, facilitators, and the way forward. BMC Nurs. 2021;20(1):158. doi:10.1186/s12912-021-00684-2. [Google Scholar] [PubMed] [CrossRef]
4. Benbassat J. Teaching professional attitudes and basic clinical skills to medical students: a practical guide. Berlin, Germany: Springer Nature; 2023. [Google Scholar]
5. Chu KH, Tung HH, Clinciu DL, Hs HI, Wu YC, Hsu CI, et al. A preliminary study on self-healing and self-health management in older adults: perspectives from healthcare professionals and older adults in Taiwan. Gerontol Geriatr Med. 2022;8:23337214221077788. doi:10.1177/23337214221077788. [Google Scholar] [PubMed] [CrossRef]
6. Bunce AE. “What we’re saying makes sense so I’ve subscribed to it and I try to live by it.”: a qualitative exploration of prisoners’ motivation to participate in an innovative rehabilitation program through the lens of self-determination theory (Ph.D. Thesis). University of Surrey: Guildford; 2020. [Google Scholar]
7. Billings J, Ching BCF, Gkofa V, Greene T, Bloomfield M. Experiences of frontline healthcare workers and their views about support during COVID-19 and previous pandemics: a systematic review and qualitative meta-synthesis. BMC Health Ser Res. 2021;21:1–17. [Google Scholar]
8. Abraham LK. Mama might be better off dead: the failure of health care in urban America. Chicago, USA: University of Chicago Press; 2019. [Google Scholar]
9. Finstad GL, Giorgi G, Lulli LG, Pandolfi C, Foti G, León-Perez JM, et al. Resilience, coping strategies and posttraumatic growth in the workplace following COVID-19: a narrative review on the positive aspects of trauma. Int J Environ Res Public Health. 2021;18(18):9453. doi:10.3390/ijerph18189453. [Google Scholar] [PubMed] [CrossRef]
10. Lin B, Gutman T, Hanson CS, Ju A, Manera K, Butow P, et al. Communication during childhood cancer: systematic review of patient perspectives. Cancer. 2020;26(4):701–16. [Google Scholar]
11. Ding B, Liu W, Tsai SB, Gu D, Bian F, Shao X. Effect of patient participation on nurse and patient outcomes in inpatient healthcare. Int J Environ Res Public Health. 2019;16(8):1344. doi:10.3390/ijerph16081344. [Google Scholar] [PubMed] [CrossRef]
12. Cole DA, Bersick E, Skarbek A, Cummins K, Dugan K, Grantoza R. The courage to speak out: a study describing nurses’ attitudes to report unsafe practices in patient care. J Nurs Manag. 2019;27(6):1176–81. doi:10.1111/jonm.v27.6. [Google Scholar] [CrossRef]
13. Wang KY, Chou CC, Lai JCY. A structural model of total quality management, work values, job satisfaction, and patient-safety-culture attitude among nurses. J Nurs Manag. 2019;27(2):225–32. doi:10.1111/jonm.2019.27.issue-2. [Google Scholar] [CrossRef]
14. Al-Mugheed K, Bayraktar N, Al-Bsheish M, AlSyouf A, Jarrar MT, AlBaker W, et al. Patient safety attitudes among doctors and nurses: associations with workload, adverse events experience. Healthcare. 2022;10:631. doi:10.3390/healthcare10040631. [Google Scholar] [PubMed] [CrossRef]
15. Hinz A, Herzberg PY, Lordick F, Weis J, Faller H, Brähler E, et al. Age and gender differences in anxiety and depression in cancer patients compared with the general population. Europ J Cancer Care. 2019;28(5):e13129. doi:10.1111/ecc.13129. [Google Scholar] [PubMed] [CrossRef]
16. Li L, Hou Y, Kang F, Wei X. The mediating and moderating roles of resilience in the relationship between anxiety, depression, and post-traumatic growth among breast cancer patients based on structural equation modeling: an observational study. Medicine. 2020;99(50):e23273. doi:10.1097/MD.0000000000023273. [Google Scholar] [PubMed] [CrossRef]
17. Chirico A, Maiorano P, Indovina P, Milanese C, Giordano GG, Alivernini F, et al. Virtual reality and music therapy as distraction interventions to alleviate anxiety and improve mood states in breast cancer patients during chemotherapy. J Cell Physiol. 2020;235(6):5353–62. doi:10.1002/jcp.29422. [Google Scholar] [PubMed] [CrossRef]
18. Kim MJ, Oh HK, Lee KC, Yang HH, Koo BW, Lee J, et al. Effects of an internet-based informational video on preoperative anxiety in patients with colorectal cancer. Ann Surg Treat Res. 2019;96(6):290. doi:10.4174/astr.2019.96.6.290. [Google Scholar] [PubMed] [CrossRef]
19. Majumdar JR, Vertosick EA, Cohen B, Assel M, Levine M, Barton-Burke M. Preoperative anxiety in patients undergoing outpatient cancer surgery. Asia-Pac J Oncol Nurs. 2019;6(4):440–5. doi:10.4103/apjon.apjon_16_19. [Google Scholar] [PubMed] [CrossRef]
20. Mariani R, Renzi A, Di Trani M, Trabucchi G, Danskin K, Tambelli R. The impact of coping strategies and perceived family support on depressive and anxious symptomatology during the coronavirus pandemic (COVID-19) lockdown. Front Psychiat. 2020;11:587724. doi:10.3389/fpsyt.2020.587724. [Google Scholar] [PubMed] [CrossRef]
21. Sari DK, Dewi R, Daulay W. Association between family support, coping strategies and anxiety in cancer patients undergoing chemotherapy at General Hospital in Medan, North Sumatera. Indones Asian Pac J Cancer Prev. 2019;20(10):3015–9. doi:10.31557/APJCP.2019.20.10.3015. [Google Scholar] [PubMed] [CrossRef]
22. Dorman-Ilan S, Hertz-Palmor N, Brand-Gothelf A, Hasson-Ohayon I, Matalon N, Gross R, et al. Anxiety and depression symptoms in COVID-19 isolated patients and their relatives. Front Psychiatry. 2020;11:581598. doi:10.3389/fpsyt.2020.581598. [Google Scholar] [PubMed] [CrossRef]
23. Brivio E, Guiddi P, Scotto L, Giudice AV, Pettini G, Busacchio D, et al. Patients living with breast cancer during the coronavirus pandemic: the role of family resilience, coping flexibility, and locus of control on affective responses. Front Psychol. 2021;11:567230. doi:10.3389/fpsyg.2020.567230. [Google Scholar] [PubMed] [CrossRef]
24. Ma X, He Z, Zhou S, Huang G, Zhu R, Wang Q. Analysis of postoperative nursing effect of patients with spinal intramedullary tumor resection under microscope. Acta Microsc. 2020;29(5):2617. [Google Scholar]
25. Duymuş ME, Aydın HA. Evaluation of awareness, behaviour, and knowledge levels of female healthcare professionals about breast and cervical cancer in Southern Turkey. Acta Oncol Turc. 2023;56(1):13–26. doi:10.5505/aot.2023.60376. [Google Scholar] [CrossRef]
26. Feng J, Ge L, Jin F, Jiang L. Application of narrative nursing combined with focused solution model to anxiety and depression in patients with lung tumors during the perioperative period. Front Surg. 2022;9:858506. doi:10.3389/fsurg.2022.858506. [Google Scholar] [PubMed] [CrossRef]
Nursing Staff’s Positive Work Attitude (NSPWA):
1. How much do you agree with the subsequent statement: “I respect the emotions of my patients in the recovery process”?
• Strongly Disagree
• Disagree
• Neutral
• Agree
• Strongly Agree
2. On the same scale please evaluate your level of professionalism in dealing with patients and their families.
• Very Poor
• Poor
• Fair
• Good
• Excellent
3. What level of confidence can respondents express while communicating the correct information to the patient for their concern/Information Need?
• Not Confident at All
• Somewhat Confident
• Moderately Confident
• Confident
• Very Confident
Level of Fear Experienced by Patients (LFEP):
1. Please rate your current level of fear about your chances of recovery from a benign tumor starting from 1 to 10 where 1 is no fear and 9–10 is extreme fear.
• No fear (1)
• Middle Fear (2–4)
• Moderate Fear (5–7)
• High Fear (8)
• Extreme fear (9–10)
2. Kindly highlight any particular concern or fear you have about your recovery from the benign tumor.
• Not Concerned
• Slightly Concerned
• Moderately Concerned
• Quite Concerned
• Extremely Concerned
3. How much do you feel you want additional support or guidance to address your fears throughout the recovery procedure?
• Not at All
• A Little
• Moderately
• Quite a Bit
• Extremely
Levels of Family Support (LFS):
1. To what extent do you feel your family members understand your fears and concerns about your recovery from the benign tumor?
• Not at All
• A Little
• Moderately
• Quite a Bit
• Completely
2. How often do your family members provide you with emotional support and reassurance during your recovery process?
• Never
• Rarely
• Sometimes
• Often
• Always
3. Rate the level of practical assistance your family members offer you in managing daily tasks or medical appointments during your recovery.
• None
• Minimal
• Some
• Substantial
• Extensive
Level of Family Support Perceived by Patients (LFSP)
1. How much do you feel that your family members understand what scares and worries you about recovering from the benign tumor?
• Not at All
• A Little
• Moderately
• Quite a Bit
• Completely
2. How much do you feel that your family members give you the love and care you need to help you recover?
• None
• Very Little
• Some
• A Lot
• A Great Deal
3. Estimate the degree of practical help you think your family members provide when dealing with routine duties or medical check-ups during your recovery period.
• None
• Minimal
• Some
• Substantial
Cite This Article
 Copyright © 2024 The Author(s). Published by Tech Science Press.
Copyright © 2024 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools