 Open Access
Open Access
ARTICLE
Network Structure and Variability of Recurrence Fear in Early-Stage Non-Small Cell Lung Cancer: A Symptom Network Analysis
Department of Thoracic Surgery, National Cancer Center/National Clinical Research Center for Cancer/Cancer Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, 100021, China
* Corresponding Authors: Yan Liu. Email: " />; Man Liu. Email:
" />
# These authors contributed equally to this work
Psycho-Oncologie 2024, 18(4), 317-328. https://doi.org/10.32604/po.2024.053678
Received 07 May 2024; Accepted 08 August 2024; Issue published 04 December 2024
Abstract
Background: Lung cancer, one of the most prevalent and deadly malignancies worldwide, not only poses a significant physical burden but also a profound psychological challenge to patients. Among these psychological challenges, the fear of recurrence stands out as a particularly distressing issue. This fear, often rooted in the patients’ past experiences with the disease and its treatment, can significantly impact their quality of life, mental health, and even compliance with follow-up care. Moreover, this fear can be exacerbated by the lack of understanding and support from healthcare professionals and family members, further isolating patients and compounding their psychological burden. Therefore, understanding and addressing the fear of recurrence in lung cancer patients is crucial for improving their overall well-being and outcomes. Aims: This study aims to develop a symptom network model for fear of recurrence in early-stage lung cancer patients, analyzing symptom correlations to enhance healthcare providers’ understanding and management of these symptoms, thereby improving patient outcomes and quality of life. Design: A cross-sectional study design was used. Method: We employed convenience sampling to recruit 551 lung cancer patients from the Thoracic Surgery Department of a tertiary hospital in Beijing between January 2023 and December 2023. A cross-sectional study was conducted using the General Information Questionnaire, Fear of Disease Progression Scale, and Level of Hope Scale. Network analysis was performed with JASP 0.18.3.0 using the EBICglasso method, and centrality metrics including Betweenness, Closeness, Degree centrality, and Expected influence were calculated. Results: Symptom network analysis identified fear of family impact and future work disruption as central to recurrence fear in these patients. Gender-based analysis revealed ‘fear of being unable to continue work’ as central in males, while ‘fear of affecting family members’ was central in females. Among adolescents, concerns about future work, medication side effects, and family impact showed the highest expected influence. In contrast, older patients predominantly feared major treatment implications. One-way ANOVA indicated that older age correlated with reduced recurrence fear, and higher hope levels significantly mitigated this fear. Conclusion: This study broadens understanding of fear of recurrence across demographic variables like gender and age, elucidating symptom interrelations and impacts. Future strategies should focus on patient-specific differences in recurrence fear to formulate targeted interventions. Relevance to Clinical Practice: Through in-depth analysis of the symptom network, healthcare professionals can more comprehensively understand the psychological responses of lung cancer patients when they face the risk of recurrence, and then formulate more precise and personalized treatment plans. At the same time, doctors and nurses can adjust treatment strategies in a timely manner according to the changes in the patient’s symptom network and provide more comprehensive psychological support, thus enhancing the patient’s treatment adherence and outcome. Patient Contribution: People who were invited to participate voluntarily completed a range of questionnaires.Keywords
Supplementary Material
Supplementary Material FileCancer continues to be a significant global public health challenge and a key driver of the worldwide economic burden. According to the most recent statistics from the International Agency for Research on Cancer (IARC) of the World Health Organization (WHO), released on 02 February 2024, lung cancer accounted for 1.8 million deaths globally. This represents 18.7% of all cancer fatalities, placing lung cancer at the forefront of the cancer mortality spectrum [1]. As scientific research progresses and clinical evidence accumulates, the survival and prognosis for patients with early-stage non-small cell lung cancer have significantly improved, changing public perception from a fear of cancer to viewing it as a manageable condition. However, the completion of treatment marks not an end but the beginning of a new phase, often overshadowed by the fear of recurrence—a persistent concern that can unexpectedly unsettle patients. This fear, known as Fear of Cancer Recurrence (FCR), is a prevalent and distressing emotional experience during the protracted, uncertain journey of treatment and recovery, driving worries about recurrence and metastasis. FCR encapsulates the deep-seated anxiety of the unknown, confronting patients with an ongoing psychological challenge [2]. The psychological state of fear and worry persists across the treatment and survival trajectory for lung cancer patients. Research indicates that up to 97% of these patients experience fear of recurrence at some point during their illness journey [3]. During this phase, lung cancer patients frequently encounter emotional fluctuations that can lead to feelings of helplessness and confusion. The pervasive fear of the disease often results in anxiety, depression, and other psychological issues, markedly diminishing their quality of life [4]. Simultaneously, research has revealed that fear of recurrence may drive some patients to avoid follow-up and screening appointments. This avoidance behavior increases the risk of late detection of recurrence, subsequently reducing survival rates [5]. Conversely, some patients, driven by fear of recurrence, may engage in excessive health monitoring and frequent doctor consultations, leading to over-testing and over-treatment. This not only wastes healthcare resources but also heightens the risks of medical radiation exposure. Moreover, it perpetuates and intensifies anxiety, potentially undermining the effectiveness of their treatment [6]. Furthermore, the FCR extends beyond the individual patient, impacting families and society. Research indicates that family caregivers often exhibit higher levels of FCR than the patients themselves, leading to social isolation for both the patient and the family. This not only diminishes the caregivers’ capacity to provide effective care but also adversely affects the patient’s quality of survival [7].
FCR, as a form of mental distress, is increasingly recognized as the sixth vital sign in assessing a cancer patient’s health status, complementing the traditional five signs: temperature, respiration, heart rate, blood pressure, and pain. Recent studies have demonstrated the utility of FCR in clinical practice. For example, Simard et al. highlighted FCR as a significant predictor of psychological well-being in cancer survivors. Additionally, Lebel et al. showed that incorporating FCR assessments into routine care improved patient outcomes by facilitating timely psychological interventions. Such evidence underscores the importance of FCR in comprehensive cancer care [8–10]. Accurate identification and assessment of a patient’s fear of relapse are imperative. Research indicates that FCR is a unique, independent, and multidimensional construct, distinct from anxiety, depression, and distress, characterized by its specific features and underlying mechanisms [11]. Presently, FCR assessment in clinical settings primarily relies on standardized scales. These tools are valued for their simplicity, time efficiency, clear results, and scientific reliability, allowing for quantitative scoring across various scenarios and severity grading. The 12-item Fear of Disease Progression Simplified Scale stands out as a universally acknowledged instrument that has been effectively employed to evaluate FCR [12]. Previous uses of the scale to explore and evaluate the diagnostic significance of patients’ fear of relapse thresholds have overlooked the interactions and impacts among the scale’s individual items. Symptom management is paramount in contemporary healthcare, necessitating the identification, comprehension, and management of a broad spectrum of patient symptoms. Research advocates for a more precise assessment of patients’ conditions and needs, leading to the creation of tailored care plans.
With the advent of precision medicine, the Nursing Science Precision Health (NSPH) model has gained prominence. From a precision health perspective, symptom science is increasingly directed towards creating personalized strategies for diagnosing, treating, and preventing the adverse symptoms of disease across diverse populations and settings [13]. Precise measurements are crucial in elucidating why individuals with the same clinical diagnosis exhibit varied symptoms, severity levels, triggers, and impacts on daily life, and why they respond differently to pharmacological and non-pharmacological therapies [14]. Against this backdrop, the concept of the symptom network has gained prominence, referring to the interconnected and mutually influential symptoms experienced by patients throughout their illness trajectory [15]. Currently, scholars internationally have conducted extensive research across various medical fields, including cancer, diabetes, AIDS, heart disease, and perioperative care, to investigate the application of symptom management theory in nursing practice [16]. The development of a symptom network model enables healthcare professionals to obtain a comprehensive and nuanced understanding of patients’ symptomatic profiles, thereby enhancing symptom management. Symptom management theory advocates for an approach grounded in the individuality of symptoms, promoting the formulation of hypotheses, their validation, and the subsequent development of tailored symptom management strategies to ameliorate patients’ health issues, enhance treatment outcomes, and improve quality of life. Accordingly, this study aims to employ symptom network analysis to systematically examine the core elements and distinct characteristics of the Fear of Cancer Recurrence (FCR) scale. The goal is to pinpoint the central symptoms of recurrence fear in patients with early-stage non-small cell lung cancer and to elucidate their interconnections. This analysis will inform the creation of personalized psychological intervention plans, aiming to improve intervention efficacy, support recovery and survival quality, and aid in clinical decision-making.
An anonymous cross-sectional survey.
This study employed a cross-sectional survey method, targeting lung cancer patients from the Department of Thoracic Surgery at a tertiary hospital in Beijing between January 2023 and December 2023. Inclusion criteria were as follows: (1) non-small cell lung cancer confirmed by postoperative pathology with a pathological stage of 1–2; (2) age over 18 years; (3) awareness of their diagnosis; and (4) clear consciousness and no communication barriers. Exclusion criteria included: (1) serious cardiac, hepatic, renal, or other functional disorders; (2) cognitive or psychosomatic disorders; and (3) impaired hearing and language expression, preventing study cooperation. Participants provided informed consent and voluntarily joined the study, which received ethical approval from the Ethics Committee of the Cancer Hospital of the Chinese Academy of Medical Sciences (Approval No. 23/179-3921).
For sample size determination, we used the PASS software for a cross-sectional survey with continuous variables, assuming a two-sided test, alpha of 0.05, Based on previous studies a mean recurrence fear score of 31.98, a standard deviation of 8.98 [17], and an allowable error of 1. The calculated sample size was 310 cases, adjusted for a 20% non-response rate, resulting in a required sample of 372 cases. To enhance scientific validity, this study ultimately included 596 participants, exceeding the calculated sample size requirement.
General information collection form
We developed a bespoke general information questionnaire, informed by relevant literature. This questionnaire gathered socio-demographic details, including age, gender, education level, and monthly income, as well as disease-related information, such as pathological type, staging, family history of cancer, comorbidities, and the receipt of radiotherapy and chemotherapy.
Revised fear of progression scale (FoP-Q-SF)
The scale, developed by Mehnert et al. in Germany, builds on the Fear of Progression Questionnaire (FoP-Q). Initially crafted to measure anxiety and fear in patients with chronic diseases requiring ongoing medication, such as hypertension, it was later adapted for use among cancer patients. The scale comprises two dimensions—physical health and social/family life—each with six assessment items, totaling 12 items. Patients self-report their responses using a Likert scale ranging from 1 (‘never’) to 5 (‘always’), leading to a possible total score between 12 and 60, where higher scores indicate greater FCR. The scale’s reliability is evidenced by a Cronbach’s alpha of 0.87, while in this study, it achieved a Cronbach’s alpha of 0.913 [18].
Hope levels were measured using the Herth Hope Inventory (HHI), a scale comprising three dimensions: positive attitudes toward reality and the future (4 items), positive behavior adoption (4 items), and sustaining close relationships (4 items), totaling 12 items. Responses are scored on a 4-point scale, with higher scores indicating greater hope. The HHI has demonstrated reliability, with a Cronbach’s alpha of 0.767; in this study, it achieved a Cronbach’s alpha of 0.807 [19].
To facilitate data collection, we utilized ‘Questionnaire Star’ to create an electronic questionnaire, generating a QR code distributed via the research team’s WeChat. Patients were invited to scan the code and complete the survey. The questionnaire’s opening page provided a standard introduction, outlining the study’s purpose and significance, completion instructions, and assurances of anonymity, voluntary participation, and data privacy. It was configured to allow only one response per IP, with a flip-page question format and mandatory answer requirements. After rigorous verification, data were exported to an Excel sheet. The survey, initiated on 04 January 2023, concluded on 08 December 2023, after gathering data from 596 participants. Post-data cleansing, which involved removing 24 responses due to excessively short completion times (under 180 s) and 21 for patterns indicating non-valid responses (like uniform or contradictory answering), yielded 551 valid questionnaires, representing a 92.44% response rate.
Statistical analyses of baseline characteristics were conducted using SPSS 25.0. Categorical variables were presented as frequency and percentage, while continuous variables were described using mean ± standard deviation. Differences in continuous variables across groups were evaluated using one-way ANOVA, with Harman’s one-way test applied to assess common method bias. A p-value of < 0.05 was considered statistically significant. Network analyses were conducted with JASP 0.18.3.0; individual fear network analysis utilized the EBIC glasso method, and influence factor network analysis employed the mgm method. Centrality metrics, including Betweenness, Closeness, Degree centrality, and Expected influence, were calculated to assess the network’s properties.
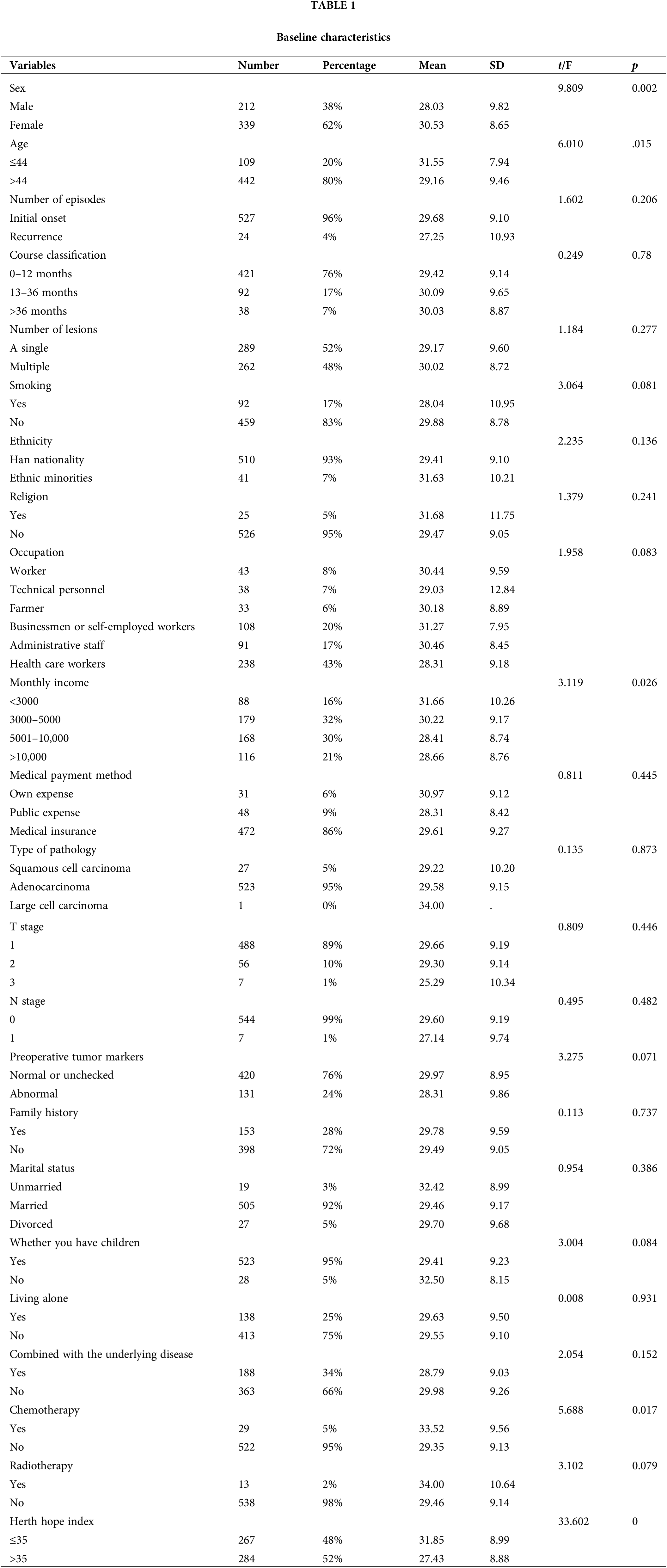
A total of 596 questionnaires were distributed in this study, and 551 postoperative patients with early-stage lung cancer were formally included. Among them, 212 cases were male and 339 cases were female, and the recurrence fear index of male (28.0 ± 9.8) was significantly lower than that of female (30.5 ± 8.7) (p = 0.002), as shown in Table 1.
Symptom network analysis of fear of recurrence in early stage lung cancer patients
Network analysis results, depicted in Fig. 1A and detailed in Tables S1 and S2, revealed significant connections within the Fear of Recurrence Scale. Notably, the strongest linkage was between item 1 (fear of progress) and item 2 (fear of examination), and between item 7 (fear of relying on strangers) and item 8 (fear of discontinuing hobbies), each with a connection weight of 0.278 (Table S3). Centrality analysis, shown in Fig. 1B, identified item 11 (fear of family repercussions) as having the highest Expected Influence (EI) index, indicating it as a central symptom with a strong positive correlation to other symptoms. Additionally, item 4 (fear of affecting future work) exhibited the highest scores in closeness and betweenness centrality, along with a high EI index, underscoring its pivotal role in the symptom network.
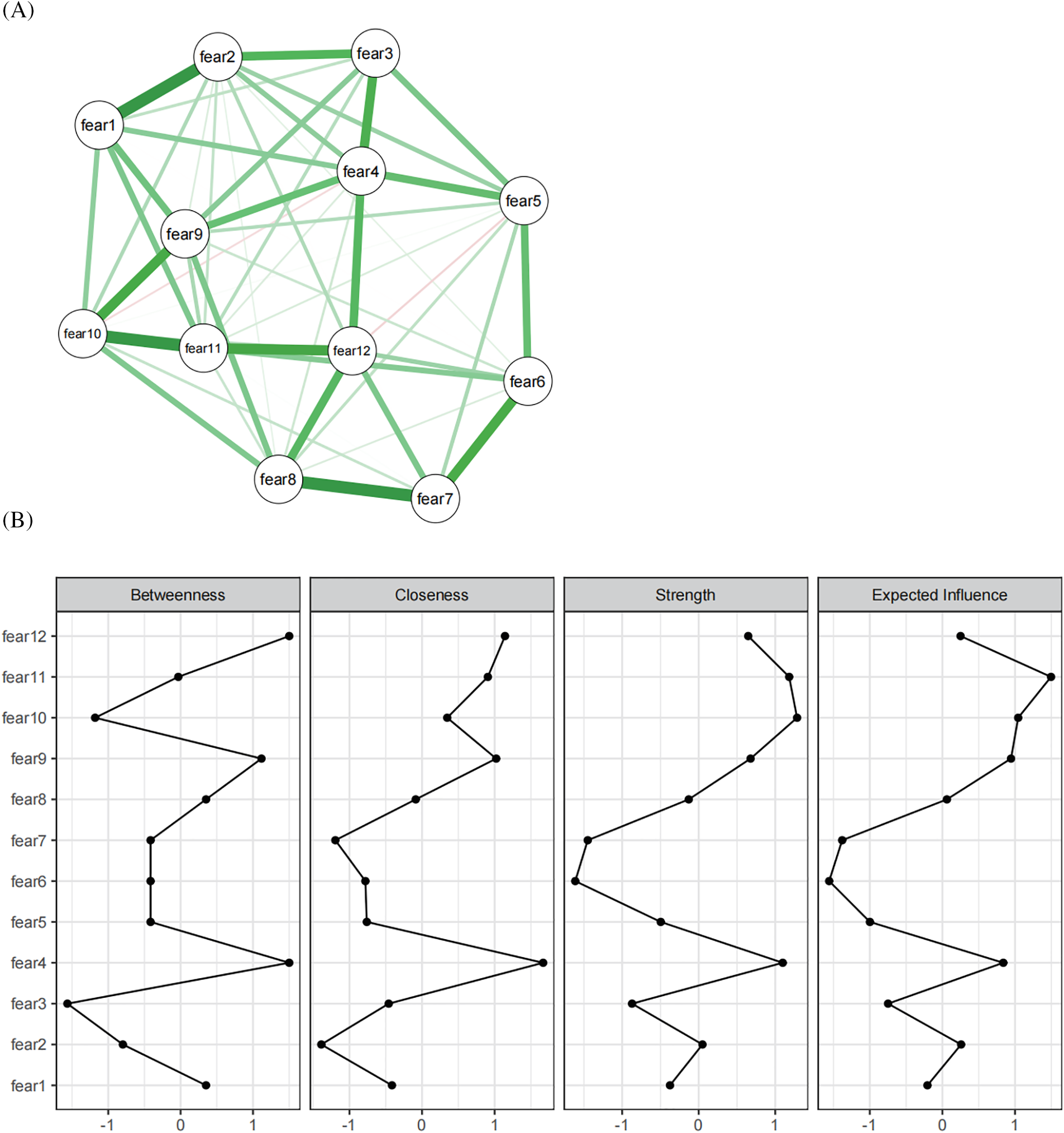
Figure 1: Fear of recurrence network analysis: overall characteristics and associations ((A): Results of the network analysis of the relapse fear scale; (B): Results of centrality analysis).
Gender differences in the recurrence fear symptom network of early stage lung cancer
Comparative analysis of the recurrence fear symptom networks between genders revealed distinct patterns, illustrated in Fig. 2A,B. In males, the strongest network connection was between items 6 and 7 of the recurrence fear scale (0.294), with the next highest between items 11 (worry about family) and 12 (worry about work continuity) at 0.236. For females, the highest linkage weight was found between items 7 (relying on strangers) and 8 (continuing hobbies) at 0.462, with item 1 (fear of progress) and item 2 (fear of examination) also showing significant connectivity at 0.315 (detailed in Table S4).
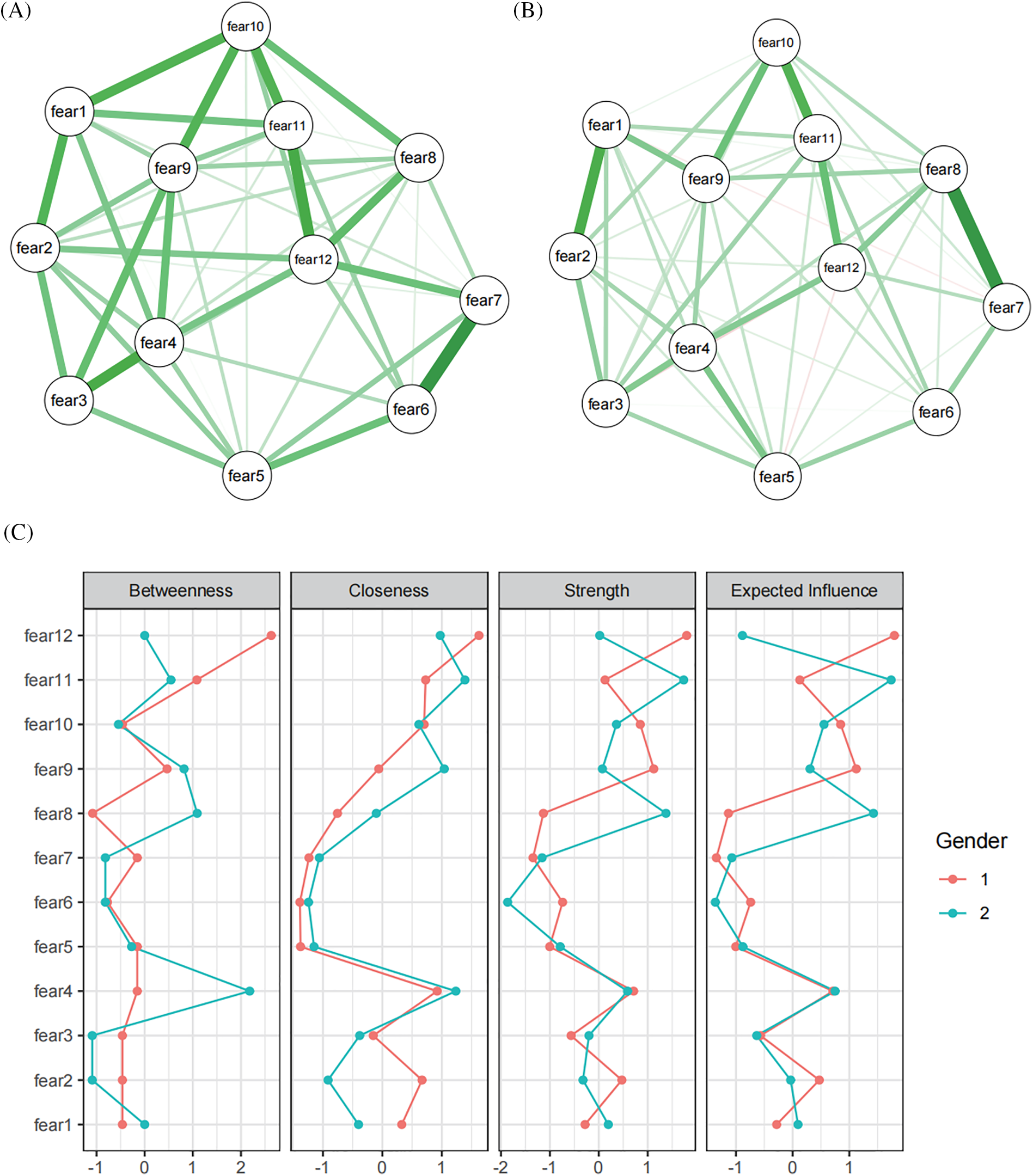
Figure 2: Fear of recurrence network analysis: the influence of the gender factor (This figure illustrates the fear of recurrence network among different gender groups. The nodes represent various factors contributing to the fear of recurrence, and the edges represent the relationships between these factors. (A): Network for male patients, highlighting the most salient connections and nodes. (B): Network for female patients, with emphasis on distinct patterns compared to males. (C): Centrality analysis).
Centrality analysis, shown in Fig. 2C, identified item 12 (fear of not being able to continue working) as the central symptom in the male network, exhibiting the highest expected impact index, closeness, and betweenness centrality. In females, item 11 (fear of affecting family) emerged as the central symptom, with the highest values in expected impact, closeness, and betweenness centrality. These findings indicate that men primarily fear the loss of work capability, whereas women are more concerned about the disease’s impact on their families.
Age differences in recurrence fear symptom networks in early stage lung cancer
Comparative analysis was conducted on the recurrence fear symptom networks across different age groups, with findings presented in Fig. 3A,B. For adolescents, the strongest connection was between item 7 (fear of relying on strangers) and item 8 (fear of discontinuing hobbies) with a weight of 0.407, followed by item 3 (fear of pain) and item 4 (fear of impacting future work) at 0.313. In the middle-aged and elderly group, the most significant links were between item 1 (fear of disease progression) and item 2 (fear of regular checkups) at 0.335, and between item 10 (fear of treatment side effects) and item 11 (fear of family impact) at 0.28 (detailed in Table S5).
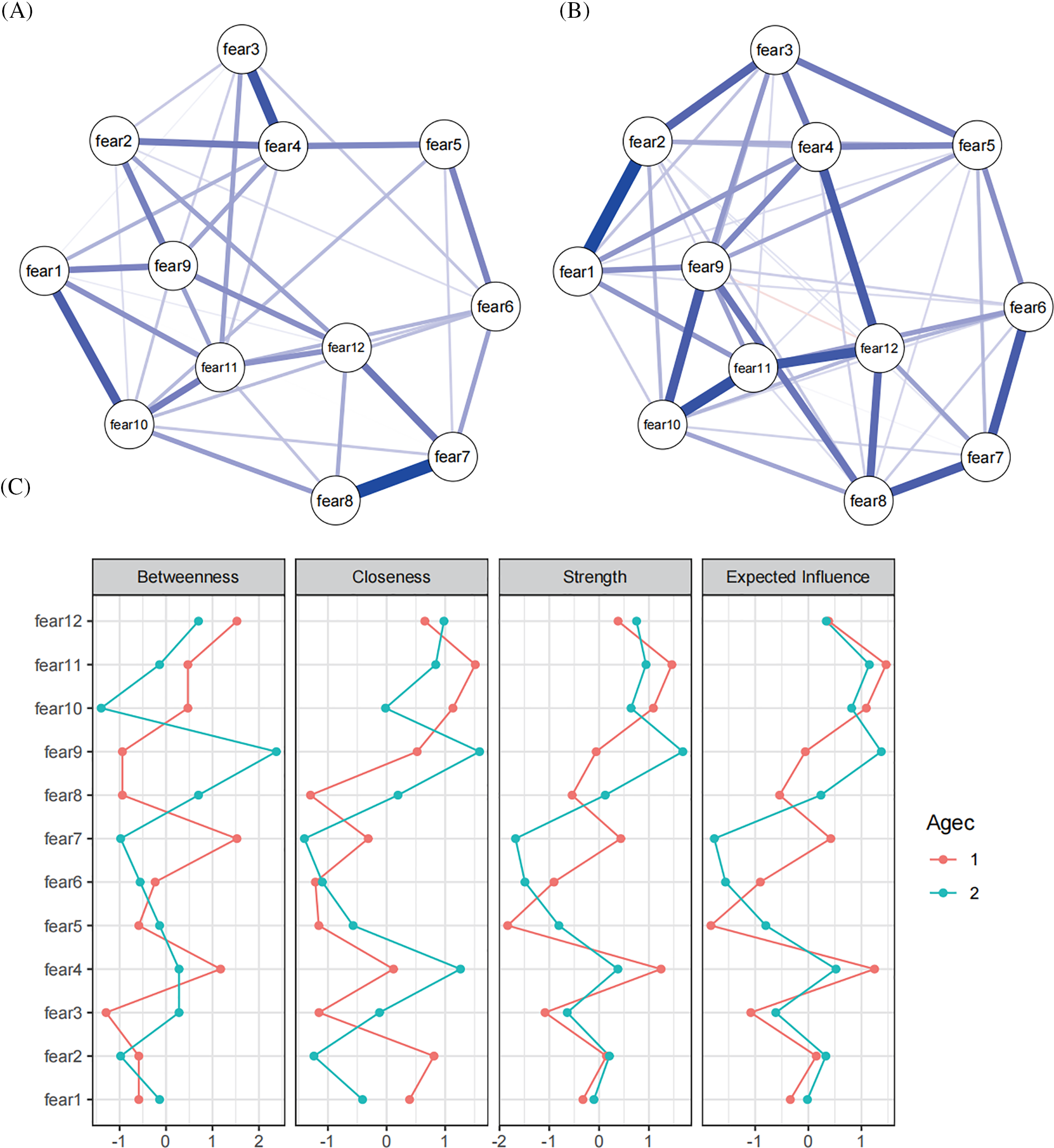
Figure 3: Fear of recurrence network analysis: the influence of the age factor (This figure depicts the fear of recurrence network stratified by age groups. It shows how factors influencing fear of recurrence vary across different age categories. (A): Network for adolescents patients. (B): Network formiddle-aged and elderly; (C): Centrality analysis).
Centrality analysis, depicted in Fig. 3C, indicated that in adolescents, items 4 (fear of affecting future work), 10 (fear of treatment harming the body), and 11 (fear of family impact) had the highest expected influence indices, identifying them as central symptoms. Among middle-aged and elderly patients, item 9 (fear of major treatments) emerged as the central symptom, exhibiting the highest values in expected influence, closeness, and betweenness centrality.
Network analysis of factors influencing recurrent fear
In the analysis, baseline characteristics significantly related to recurrence fear were integrated with fear-related symptoms using mgm network analysis, as shown in Fig. 4A. Age emerged as a pivotal factor, with older individuals exhibiting less fear of recurrence. Notably, the reduction in relapse fear with increasing age was primarily mediated by a decrease in item 12 (fear of not being able to continue working).
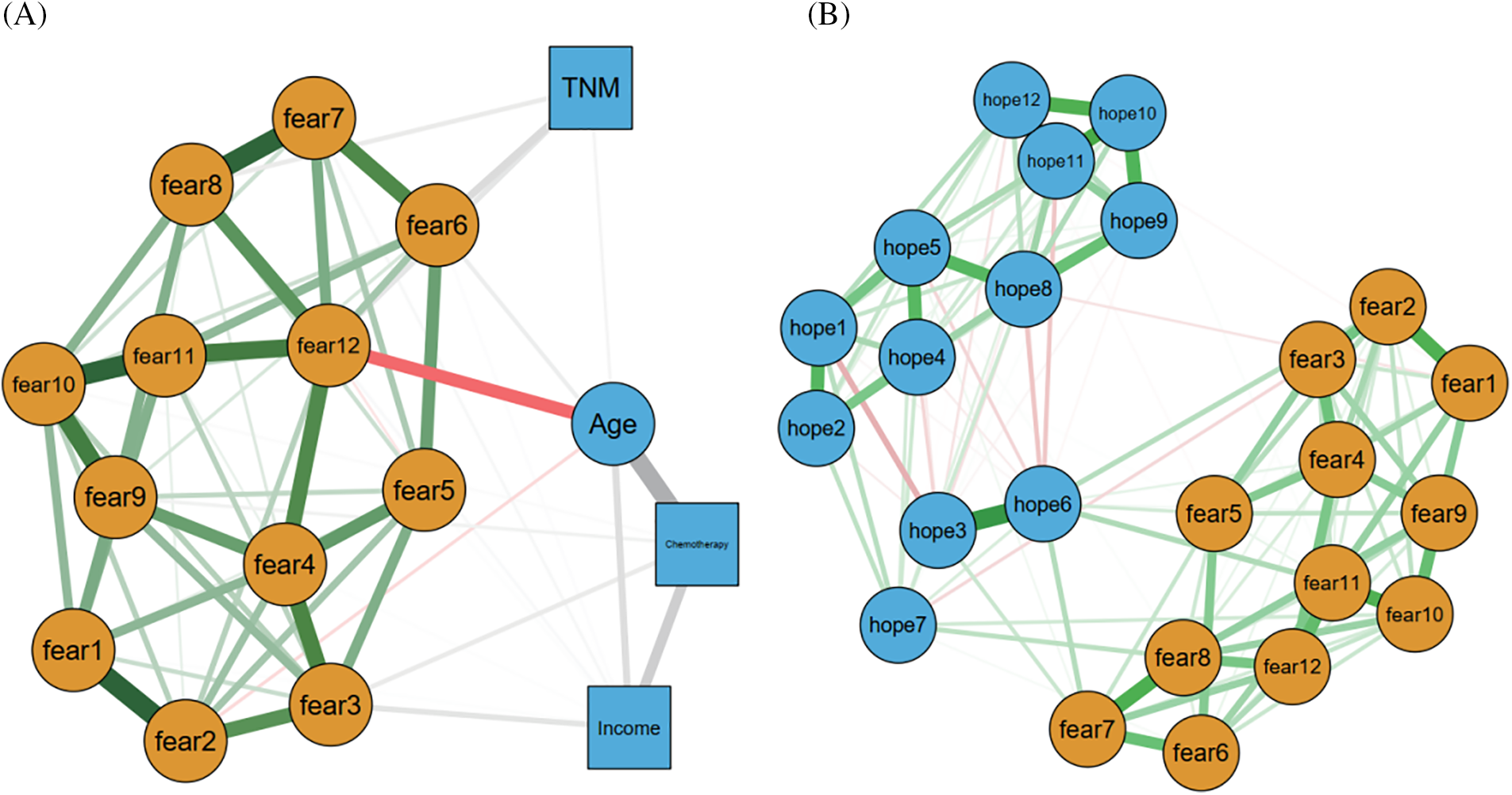
Figure 4: FCR-factors co-network ((A): results of mgm network analysis of baseline characteristics and fear-related symptoms; (B): Comprehensive symptom network analysis of relapse fear and the hope index, showing Item 6 of the hope index (fear of the future) as a key bridge).
Harman’s one-way ANOVA indicated that the first factor accounted for 37.6% of the variance in relapse fear and the hope index, which is below the 50% threshold, suggesting minimal common method bias. The combined symptom network analysis of relapse fear and the hope index, depicted in Fig. 4B, revealed that item 6 from the hope index (fear of the future) acts as a critical bridge. Specifically, the amelioration of relapse fear due to an increased hope index is predominantly achieved through the alleviation of future-related fears (Table S6).
Diverse network structures among patients underscore the potential for personalized medicine, enabling healthcare professionals to create individualized treatment plans and symptom management strategies [20]. This study investigated the network structure of recurrence fear in early-stage lung cancer patients, where the edge weight in the symptom network signifies the correlation strength between different symptoms. Understanding these edge weights assists clinical staff in comprehending the interactions and influences among symptoms. This knowledge unveils crucial symptom correlation patterns, thereby enabling more precise diagnostic and treatment recommendations [21]. The study revealed that the strongest connections within the network were between fear of disease progression and fear of examination, and between fear of relying on strangers and fear of losing the ability to continue hobbies, each with a significant weight of 0.278. This observation aligns well with the relapse fear model proposed by Lee-Jones et al., offering a robust explanation for these relationships [22], Lee-Jones posited that internal and external cues are crucial in triggering cognitive, emotional, and behavioral responses associated with FCR. Patients with heightened FCR levels tend to engage in behaviors like excessive self-examination, frequent seeking of advice, and restricted future planning, which temporarily alleviate anxiety and provide comfort. In the network analysis, central symptoms included fear of family impact and fear of hindering future work. Thus, it is advisable that psychological interventions and health guidance increasingly address the disease’s effects on social roles and functions. Clinical practice guidelines suggest integrating cognitive-behavioral therapy (CBT) and mindfulness-based stress reduction (MBSR) to help patients manage FCR effectively [23]. Additionally, supportive-expressive group therapy has shown promise in alleviating FCR by fostering a sense of community and shared experience among patients [24]. These therapeutic approaches can be tailored to address the specific fears identified in the network analysis, providing targeted and effective interventions.
Additionally, fears and hopes are often influenced by social and cultural circumstances. The national health and welfare system plays a pivotal role in the treatment process over time. In our country, the health system provides comprehensive coverage for cancer diagnosis and treatment, which can alleviate some of the financial and logistical burdens on patients. This support may reduce anxiety related to treatment costs and accessibility, potentially influencing the levels of FCR and overall psychological well-being. Furthermore, cultural attitudes towards cancer and health can shape patients’ experiences and expectations, impacting their emotional responses and coping mechanisms. Future research should explore the interplay between these social, cultural, and systemic factors and their effects on patient outcomes. Understanding these dynamics can help tailor interventions that address both the medical and psychosocial needs of cancer patients, leading to more holistic and effective care.
In examining gender disparities in recurrence fear among early-stage lung cancer patients, we noted significant differences in the centrality rankings and local connectivity of symptoms between genders. Males showed the highest expected impact index for fear of work discontinuation, making it central in their network. Females, conversely, had the highest expected impact index for fear of affecting family members, positioning it at the network’s core. These findings likely reflect the varied social divisions of labor, roles, cognitive schemas, and coping strategies between genders [25]. Traditionally, societal expectations have positioned women primarily in caregiving roles, involving household and childcare responsibilities. Consequently, women may express heightened concern over how illness impairs their capacity to fulfill these roles. Additionally, as key providers of emotional support within families, women worry about the emotional and life impacts of their illness on family members, heightening anxiety about family dynamics. Moreover, following significant traumatic events, women are more inclined to perceive the world as perilous, self-blame, and form negative self-perceptions, leading to feelings of failure and guilt [25]. Traditional societal roles often cast men as the primary financial providers, responsible for maintaining stable family income. Consequently, men may harbor increased concerns about how illness could impair their work performance and financial stability, thereby heightening work-related anxiety and worry. Furthermore, societal recognition and self-esteem issues mean that men are often more aware of their societal and workplace status, leading to fears that illness might tarnish their image and standing among peers and supervisors [26]. We recommend that individuals, during illness, consider redistributing roles and responsibilities within the family, allowing others to share tasks typically undertaken by them. Setting realistic expectations and accepting potential limitations in fulfilling usual responsibilities, while maintaining a positive outlook and seeking professional assistance, can help manage fear. Medical professionals should promote symptom self-reporting among patients to improve nurse-patient communication. However, it is important to recognize the variability in patient self-reporting. Patients, regardless of gender, should be guided to accurately report their symptoms, detailing their nature, severity, and frequency, to enhance symptom management and the accuracy of nursing decisions.
This study’s comparative network analysis across different age groups revealed that in adolescents, fears related to work impact, treatment side effects, and family concerns were central in the recurrence fear network. Adolescents, who are in a pivotal phase of identity and self-worth development, may thus perceive illness as a threat to their body image and self-esteem. In contrast, middle-aged and elderly patients primarily feared the prospect of major treatments, indicating a shift in concern towards health outcomes over time [27]. Adolescents may fear that illness will alter their appearance and diminish their physical abilities, affecting their roles in work and family life. Additionally, they face multiple expectations and pressures from family, school, and society. Illness can exacerbate concerns about failing to meet these expectations, impacting their future career and family dynamics [28]. Consequently, parents, physicians, and mental health professionals should focus on and support the post-treatment fears of adolescent lung cancer patients, aiding them in understanding and managing these fears to enhance their overall health and recovery. Moreover, this study found that concerns about major treatments were central in the symptom network of elderly patients, aligning with findings from previous studies [29]. The analysis suggests that physical and psychological adaptability may wane with age, leading middle-aged and elderly patients to be particularly concerned about the pain, discomfort, and side effects of treatments. Additionally, they might fear the treatments’ impact on their bodily functions and long-term quality of life, including concerns about physical rehabilitation and functional recovery [30]. Family members and healthcare providers should offer information and emotional support to assist older individuals in managing their treatment-related fears, thereby fostering their physical and mental well-being and recovery. Our network analysis revealed that fear of recurrence decreases with age in early-stage lung cancer patients. Specifically, reducing work-related fears can alleviate overall recurrence fear, presenting a new focus for future interventions. Notably, adolescents rank tenth globally in cancer burden, highlighting the significance of addressing this issue [31]. Adolescents, as a distinct patient group within the cancer population, face unique challenges. They are navigating critical stages of physical, emotional, and psychosocial development, including career progression, higher education, relationships, and childbearing. They also face a higher risk of long-term and late-stage quality of life deterioration. Additionally, this age group has specific biological, social, familial, and economic needs. Cancer in adolescents can lead to decreased productivity and alter the social fabric, incurring significant societal costs. It is crucial to focus more on the psychological aspect of recurrence fear among young early-stage lung cancer patients. Our findings indicate that an elevated hope index can mitigate recurrence fear, primarily by diminishing future-related fears. This insight offers a new direction for research, suggesting that enhancing patients’ hope levels may overall reduce their fear of recurrence. Increasing patients’ hope and confidence about the future can be achieved by providing detailed information on the disease, treatment, and recovery, bolstering social support, fostering psychological resilience, and educating them about the disease’s progression, treatment efficacy, and recovery prospects [32–34]. Collaborating with patients to establish realistic and attainable recovery goals can provide them with a clear future direction and a sense of the value of their efforts, enhancing their hope and reducing fear of the disease. This approach can facilitate better disease and recovery process management [6].
Our study has several limitations that should be acknowledged. Firstly, the focus of our research was exclusively on early-stage non-small cell lung cancer (NSCLC) patients. While this allowed us to address the specific needs and challenges faced by this group, it limits the generalizability of our findings to patients at other stages of lung cancer or those with different types of tumors. Future studies should include a broader spectrum of patients, encompassing various stages of lung cancer and other tumor types, to enhance the effectiveness of treatment approaches and provide more comprehensive educational insights for young colleagues. Secondly, in our analysis, we found that patients who received adjuvant chemotherapy exhibited higher levels of fear of recurrence (FCR). Due to the small number of these patients, conducting a separate network analysis would not provide robust results or sufficient statistical power. However, we adjusted the network diagram in Fig. 4A for clinical baseline characteristics significantly impacting FCR, showing that adjuvant chemotherapy influences the FCR symptom network primarily through fear of major treatment (fear9) and fear of pain (fear3). Future studies should focus more on the adjuvant treatment group with larger sample sizes to accurately delineate the symptom network for this population, as this would provide more comprehensive insights and enhance the effectiveness of treatment approaches.
In this study, extensive clinical data from early-stage lung cancer patients were analyzed using machine learning and deep learning techniques to quantitatively assess recurrence fear symptoms, enhancing the study’s reliability and applicability. Network analysis of these symptoms elucidated their interrelations, offering clinicians valuable insights for refining patient assessments, treatment plans, and prognostic evaluations, thus facilitating personalized care and risk management. Future research should aim to develop and evaluate targeted psychological support and intervention strategies, further investigating the mechanisms and determinants of recurrence fear and its impacts on quality of life and mental health. Given that this study’s sample was confined to early-stage lung cancer patients in China, future research could broaden its scope to other countries or regions to enhance the study’s generalizability.
Relevance to Clinical Practice
The investigation into symptom network analysis of recurrence fear in lung cancer patients holds significant importance, as it contributes to a more profound understanding of the complexity and multidimensionality of recurrence fear. Through analyzing the relationships among various symptoms reported by patients, it unveils the interactions and potential causal links between these symptoms. This analysis not only aids healthcare professionals in gaining a better insight into their patients’ psychological state but also furnishes crucial insights for developing more effective interventions.
Furthermore, symptom network analysis holds far-reaching implications for research in related fields. Firstly, it offers novel methodologies and perspectives for research within the realms of psychology, psychiatry, and clinical psychology. By delving into the symptom networks associated with patients’ relapse fears, researchers can attain a more comprehensive understanding of the intricacies of patients’ mental health and provide a theoretical underpinning for devising more potent mental health interventions.
Secondly, symptom network analysis provides valuable insights for healthcare policymakers and clinical practitioners. Understanding the symptom network of recurrence fear in lung cancer patients enables healthcare policymakers to better comprehend patients’ needs and formulate appropriate policies to enhance patients’ mental health. For clinical practitioners and nurses, such analyses serve as guiding principles to more accurately assess and manage patients’ mental health concerns, enabling the provision of tailored treatment plans.
In conclusion, investigating the symptom network analysis of fear of relapse in lung cancer patients is pivotal for advancing mental health research and clinical practice. It fosters a deeper understanding of the nature of fear of relapse, provides guidance for developing more effective interventions, and opens up new research avenues and theoretical foundations for related fields.
Acknowledgement: We extend our heartfelt gratitude to all researchers and patients who participated in this study.
Funding Statement: This research was supported by Beijing Hope Run Special Fund of Cancer Foundation of China (LC2022C05).
Author Contributions: Conceptualization, investigation, writing—original draft: Lu Liu; methodology, conceptualization, investigation, writing—original draft: Man Liu; validation, data curation, visualization, writing—original draft: Zhuoheng Lv; project administration: Yousheng Mao; writing—review & editing, project administration, funding acquisition: Yan Liu. All authors reviewed the results and approved the final version of the manuscript.
Availability of Data and Materials: Please contact the corresponding author via email to request access to the de-identified data.
Ethics Approval: The study was independently approved by the Ethics Committee of Cancer Hospital Chinese Academy of Medical Sciences (Approval No. 23/179-3921). All procedures performed in this study were conducted following the Declaration of Helsinki.
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
Supplementary Materials: The supplementary material is available online at https://doi.org/10.32604/po.2024.053678.
References
1. Tan DJH, Ng CH, Muthiah M, Yong JN, Chee D, Teng M, et al. Rising global burden of cancer attributable to high BMI from 2010 to 2019. Metabolism. 2024;152:155744. doi:10.1016/j.metabol.2023.155744. [Google Scholar] [PubMed] [CrossRef]
2. Luo X, Li W, Chen Y, Sun HW, Humphris G, Liu T, et al. Fear of recurrence in Chinese cancer patients: prevalence, correlates, and network analysis. Front Psychiatr. 2022;13:803543. doi:10.3389/fpsyt.2022.803543. [Google Scholar] [PubMed] [CrossRef]
3. Hao X, Li H, Zhan T. Research status on fear of cancer recurrence. Chin J Modern Nurs. 2022;17:2376–80 (In Chinese). [Google Scholar]
4. Luo X, Li W, Yang Y, Humphris G, Zeng L, Zhang Z, et al. High fear of cancer recurrence in Chinese newly diagnosed cancer patients. Front Psychol. 2020;11:1287. doi:10.3389/fpsyg.2020.01287. [Google Scholar] [PubMed] [CrossRef]
5. Rha SY, Park JS, Choi YY, Hong B, Lee J. Fear of cancer recurrence and its predictors and outcomes among cancer survivors: a descriptive correlational study. Eur J Oncol Nurs. 2022;58:102138. doi:10.1016/j.ejon.2022.102138. [Google Scholar] [PubMed] [CrossRef]
6. Bergerot CD, Philip EJ, Bergerot PG, Siddiq N, Tinianov S, Lustberg M, et al. Fear of cancer recurrence or progression: what is it and what can we do about it? Am Soc Clin Oncol Educ Book. 2022;42:1–10. [Google Scholar] [PubMed]
7. Lin CR, Chen SC, Simard S, Chang JTC, Lai YH. Psychometric testing of the fear of cancer recurrence inventory-caregiver Chinese version in cancer family caregivers in Taiwan. Psychooncology. 2018;27(6):1580–8. doi:10.1002/pon.v27.6. [Google Scholar] [CrossRef]
8. Bultz BD, Carlson LE. Emotional distress: the sixth vital sign in cancer care. J Clin Oncol. 2005;23(26):6440–1. doi:10.1200/JCO.2005.02.3259. [Google Scholar] [PubMed] [CrossRef]
9. Simard S, Savard J. Fear of cancer recurrence inventory: development and validation of a multidimensional measure of fear of cancer recurrence. Support Care Cancer. 2013;21(2):461–70. [Google Scholar]
10. Lebel S, Ozakinci G, Humphris G, Mutsaers B, Thewes B, Prins J, et al. From normal response to clinical problem: definition and clinical features of fear of cancer recurrence. Support Care Cancer. 2016;24(8):3265–8. doi:10.1007/s00520-016-3272-5. [Google Scholar] [PubMed] [CrossRef]
11. Simard S, Savard J, Ivers H. Fear of cancer recurrence: specific profiles and nature of intrusive thoughts. J Cancer Surviv. 2010;4(4):361–71. doi:10.1007/s11764-010-0136-8. [Google Scholar] [PubMed] [CrossRef]
12. Fardell JE, Jones G, Smith AB, Lebel S, Thewes B, Costa D, et al. Exploring the screening capacity of the fear of cancer recurrence inventory-short form for clinical levels of fear of cancer recurrence. Psychooncology. 2018;27(2):492–9. doi:10.1002/pon.v27.2. [Google Scholar] [CrossRef]
13. Dorsey SG, Pickler RH. Precision science in nursing research. Nurs Res. 2019;68(2):85. doi:10.1097/NNR.0000000000000333. [Google Scholar] [PubMed] [CrossRef]
14. Hickey KT, Bakken S, Byrne MW, Demiris G, Docherty SL, Dorsey SG, et al. Precision health: advancing symptom and self-management science. Nurs Outlook. 2019;67(4):462–75. doi:10.1016/j.outlook.2019.01.003. [Google Scholar] [PubMed] [CrossRef]
15. Yang Z, Zhu Z, Hu Y. Advances in the application of symptom networks in symptom management. J Nurs. 2022;37(5):91–4 (In Chinese). [Google Scholar]
16. Zhu Z, Sun Y, Kuang Y, Yuan X, Gu H, Zhu J, et al. Contemporaneous symptom networks of multidimensional symptom experiences in cancer survivors: a network analysis. Cancer Med. 2023;12(1):663–73. doi:10.1002/cam4.v12.1. [Google Scholar] [CrossRef]
17. Guo HT, Wang SS, Zhang CF, Zhang HJ, Wei MX, Wu Y, et al. Investigation of factors influencing the fear of cancer recurrence in breast cancer patients using structural equation modeling: a cross-sectional study. Int J Clin Pract. 2022;2022:279440. [Google Scholar]
18. Zhao T, Zhou X, Liang H. Research on the detection and application of cancer recurrence fear scale in colorectal cancer patients. Chongqing Med. 2020;49(16):4 (In Chinese). [Google Scholar]
19. Yu J, Dong H, Song Y, Zhu. Influencing factors of hope among Chinese patients with hematological malignancies from the perspective of positive psychology: a cross-sectional study. Cancer Nurs. 2022;45(6):465–72. doi:10.1097/NCC.0000000000001035. [Google Scholar] [PubMed] [CrossRef]
20. Zhu Z, Xing W, Hu Y, Wu B, So KWW. Paradigm shift: moving from symptom clusters to symptom networks. Asia Pac J Oncol Nurs. 2022;9(1):5–6. doi:10.1016/j.apjon.2021.12.001. [Google Scholar] [PubMed] [CrossRef]
21. Zhu Z, Guo M, Dong T, Han S, Hu Y, Wu B. Assessing psychological symptom networks related to HIV-positive duration among people living with HIV: a network analysis. AIDS Care. 2022;34(6):725–33. doi:10.1080/09540121.2021.1929815. [Google Scholar] [PubMed] [CrossRef]
22. Lee-Jones C, Humphris G, Dixon R, Hatcher MB. Fear of cancer recurrence--a literature review and proposed cognitive formulation to explain exacerbation of recurrence fears. Psychooncology. 1997;6(2):95–105. doi:10.1002/(ISSN)1099-1611. [Google Scholar] [CrossRef]
23. Mehnert A, Koch U. Psychological comorbidity and health-related quality of life and its association with awareness, utilization, and need for psychosocial support in a cancer register-based sample of long-term breast cancer survivors. J Psychosom Res. 2008;64(4):383–91. doi:10.1016/j.jpsychores.2007.12.005. [Google Scholar] [PubMed] [CrossRef]
24. Custers JA, Van den Berg SW, Van Laarhoven HW, Bleiker EM, Gielissen MF, Prins JB. The cancer worry scale: detecting fear of recurrence in breast cancer survivors. Cancer Nurs. 2014;37(1):E44–50. doi:10.1097/NCC.0b013e3182813a17. [Google Scholar] [PubMed] [CrossRef]
25. Li X, Wu H, Shi Y. Gender role perception and household consumption structure: a study based on data from the Chinese household panel survey. J Cent Univ Financ Econ. 2023;8:73–90. [Google Scholar]
26. Zhu H, Lu J. Work or family: a theoretical discussion on the release of gender dividends from the perspective of multiple roles. J Sun Yat-Sen Univ (Soc Sci Ed). 2021;61(5):161–70 (In Chinese). [Google Scholar]
27. Tong X. Obedience and resistance: adolescent self-identity and its integration: social work’s advocacy practice for affirmative parent-child relationships. Xuehai Mag. 2022;1:117–26 (In Chinese). [Google Scholar]
28. Li F, Cui Y, Li Y, Guo L, Ke X, Liu J, et al. Prevalence of mental disorders in school children and adolescents in China: diagnostic data from detailed clinical assessments of 17,524 individuals. J Child Psychol Psychiatry. 2022;63(1):34–46. doi:10.1111/jcpp.v63.1. [Google Scholar] [CrossRef]
29. Venuta F, Diso D, Onorati I, Anile M, Mantovani S, Rendina EA. Lung cancer in elderly patients. J Thorac Dis. 2016;8(11):S908–14. [Google Scholar] [PubMed]
30. Chong RC, Ong MW, Tan KY. Managing elderly with colorectal cancer. J Gastrointest Oncol. 2019;10(6):1266–73. doi:10.21037/jgo. [Google Scholar] [CrossRef]
31. Alvarez EM, Force LM, Xu R. The global burden of adolescent and young adult cancer in 2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Oncol. 2022;23(1):27–52. doi:10.1016/S1470-2045(21)00581-7. [Google Scholar] [PubMed] [CrossRef]
32. Zhang L. Effect of positive psychology intervention strategies under the PERMA model on the fear and hope level of cancer recurrence in lung cancer chemotherapy patients. Chin Sch Dr. 2023;10:758–60+66 (In Chinese). [Google Scholar]
33. Tauber NM, O’Toole MS, Dinkel A, Galica G, Humphris G, Lebel S, et al. Effect of psychological intervention on fear of cancer recurrence: a systematic review and meta-analysis. J Clin Oncol. 2019;37(31):2899–915. doi:10.1200/JCO.19.00572. [Google Scholar] [PubMed] [CrossRef]
34. Tu M, Wang F, Shen S. Influences of psychological intervention on negative emotion, cancer-related fatigue and level of hope in lung cancer chemotherapy patients based on the PERMA framework. Iran J Public Health. 2021;50(4):728–36. [Google Scholar] [PubMed]
Cite This Article
 Copyright © 2024 The Author(s). Published by Tech Science Press.
Copyright © 2024 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools