 Open Access
Open Access
ARTICLE
Clinical Effect Observation of Constructing PERMA Model in Psychological Intervention for Patients with Chronic Cancer Pain
Integrated Traditional Chinese and Western Medicine Department, Nantong Tumor Hospital, Nantong, 226361, China
* Corresponding Author: Dong-Li Ji. Email:
Psycho-Oncologie 2024, 18(4), 329-336. https://doi.org/10.32604/po.2024.053098
Received 24 April 2024; Accepted 07 September 2024; Issue published 04 December 2024
Abstract
Background: The constructing PERMA model in psychological intervention was applied to patients with chronic cancer pain to provide data reference for reducing pain, fear of cancer recurrence, and improving the level of psychological capital. Aim: To explore the clinical effects of constructing PERMA model in psychological intervention for patients with chronic cancer pain. Methods: A total of 98 patients with chronic cancer pain admitted to our hospital from March 2021 to March 2023 were randomly divided into two groups, 49 cases in each group. The control group received routine intervention, while the research group constructed PERMA model based on the routine intervention for psychological intervention. The pain severity, fear of cancer recurrence, psychological capital and quality of life before and after intervention were compared between the two groups. Results: After two months of intervention, the pain in the research group was milder than that in the control group (p < 0.05). The scores and total scores of all dimensions of fear of cancer recurrence in the research group were lower than those in the control group (p < 0.05). The scores and total scores of each dimension of psychological capital in the research group were higher than those in the control group (p < 0.05). The scores of all dimensions of quality of life in the research group were higher than those in the control group (p < 0.05). Conclusion: The PERMA model constructed in psychological interventions for patients with chronic cancer pain can assist analgesic medications to reduce pain and alleviate the fear of cancer recurrence, increase the level of psychological capital, and thus improve quality of life.Keywords
Cancer pain is cancer-induced pain that is one of the main causes of body pain in patients with end-stage cancer [1]. The pathological mechanism of cancer pain is extremely complex, including the growth and compression of tumor tissue, and stimulation to nerve tissue. Patients usually cannot endure the pain and it will aggravate with the progression of the disease, not only seriously affecting their quality of life, but also causing serious psychological damage [2,3]. At present, pain has been listed as another important vital indicator besides vital signs such as body temperature, respiration, and blood pressure [4]. Psychological intervention is a short self-management training, which is more acceptable than previous symptom-centered interventions [5,6]. The PERMA model is a happiness model proposed based on psychology, which improves the happiness and alleviates the negative psychological emotions by improving the individual positive emotions, participating in active activities, helping to obtain the “sense of achievement”, correctly defining and finding meaning, and improving the relationship with others [7,8]. The PERMA model enhances individual well-being by promoting positive emotions, building positive relationships, realising self-worth and participating in family and social activities, etc. The PERMA model is a theoretical framework for well-being based on positive psychology, and realizes that the concept of “well-being” is measurable, developable and sustainable. The whole theoretical framework has five dimensions. There are five dimensions in the theoretical framework: positive emotions (P), engagement (E), positive relationships (R), meaning (M) and achievement (A). An individual’s feelings constitute positive emotions, such as happiness, satisfaction, gratitude, self-esteem, and aspiration; Engagement refers to total immersion in something attractive, where the individual forgets about self and the world, and all of his or her attention and energy is focused on what is happening in the present moment; Positive relationships refer to healthy and positive relationships with family, friends, close friends, co-workers, classmates, and loved ones, where the individual feels accompanied and helped; Meaning is different from subjective judgement, but rather an objective perspective on committing to something that the individual recognizes and is interested in: Achievement is the individual’s success and sense of self-identity in accomplishing or focusing on something. Subjective elements are present in all five dimensions, with positive relationships, meaning and achievement having more objective components than the other two. Seligman also noted that three attributes are present in all five dimensions: firstly, individuals do not seek to acquire all dimensions, but rather gravitate towards a particular one; secondly, each dimension exists independently of each other and has a well-defined conceptualization and assessment methodology; and thirdly, the attainment of each dimension is in the context of promoting well-being. In this study, the PERMA model was constructed in the psychological intervention for the patients with chronic cancer pain admitted to Integrated Traditional Chinese and Western Medicine Department of Nantong Cancer Hospital, Jiangsu Province. The results were as follows.
Inclusion criteria: age ≥ 18 years old; They were all diagnosed with cancer by combining imaging examinations such as CT and MRI with histopathological examination results; Numeric Rating Scale (NRS) score ≥4 points; Estimated survival >3 months.
Exclusion criteria: Combined with severe cardiovascular and cerebrovascular diseases; Combined with severe liver, kidney, lung and other organ dysfunction; Combined language communication disorders; Previous mental history; Poor treatment compliance. There was no significant difference in general data between the two groups (p > 0.05).
The procedures for both T1 and T2 surveys adhered to the (i) declaration of Helsinki, and (ii) ethical principles for medical, psychological, and sociological research involving human participants. The Nantong Cancer Hospital Research Ethics Committeeapproved the study protocol (Approval No. Tongzhonglun Review (Research) 2023-065). All participants signed the informed consent in this study.
Routine intervention was performed in the control group. Interveners were instructed to give patients analgesics according to doctor’s advice and asked to take conscious and comfortable posture. Interveners were closely observed on various vital signs indicators. In addition, they were guided to learn the correct methods to relieve bad emotions. They could be distracted from pain by listening to music and communicating with relatives.
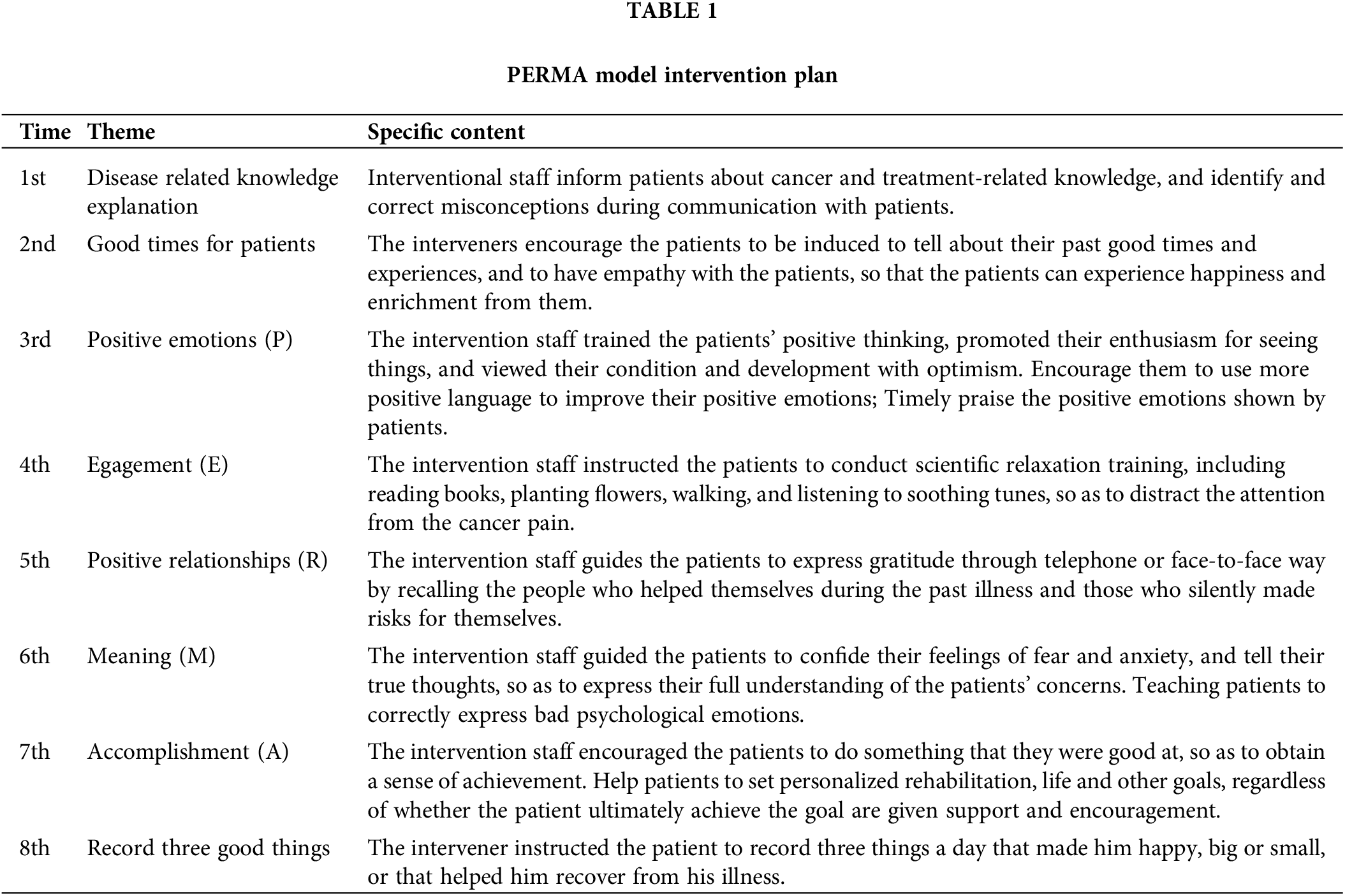
The research group constructed PERMA model in psychological intervention. Specific as follows: (1) Preparation stage: The intervention group was established, and its members included specialist nurses, department head nurses and psychological counselors. All the members of the group had more than 5 years of clinical work experience. The team reviewed the literature on “cancer pain”, “positive psychology”, and “PERMA model” on platforms such as Wanfang, CNKI and NCBI, and formulated the specific preliminary intervention plan after discussion. The psychological experts and specialists were invited for review and revision, and the formal intervention content was finally determined. The team members were guided and supervised by the experts throughout the intervention process. (2) Intervention stage: The intervention was divided into eight times, with one theme for each intervention, 20–30 min/time, and one time per week (Table 1). Before the formal start of the intervention, the researcher actively communicated with the two nurse practitioners in charge and the patients, explaining to the patients the concept of the PERMA-based positive psychological intervention and the purpose of the intervention, and obtaining the patients’ understanding and co-operation, and the participating patients voluntarily took part in the PERMA-based positive psychological intervention and signed an informed consent form to ensure their participation in the whole process. Patients in the intervention group were continuously interviewed with the PERMA-based positive psychological intervention for 20–60 min each time, twice a week for a total of eight times, and were urged to complete the exercises for a total of four weeks. If patients needed to be discharged before the end of the intervention, the interviews were conducted through electronic media, establishment of a WeChat group, or by telephone. The intervention programme developed in this study was based on the therapeutic concept of positive psychological intervention, aimed at improving the level of family resilience in patients with liver cancer, and there was logic and feasibility between the content of the eight intervention interviews.
Patients were assessed using Pain severity, Fear of cancer recurrence, Psychological capital and Quality of life scales, all of which were evaluated from previous literature.
1. Pain severity: The NRS was used to evaluate the pain severity of the two groups. The total scores were 0–10 points and 0 point was painless, 1–3 points: mild pain; 4–6 points: moderate pain; 7–10 points: Severe pain. The higher the score was, the more severe the pain would be [9].
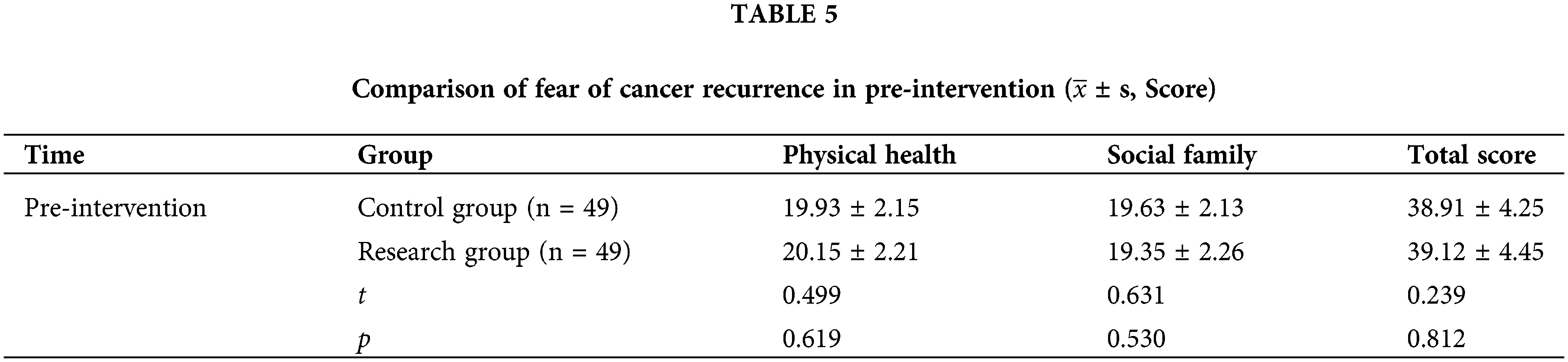
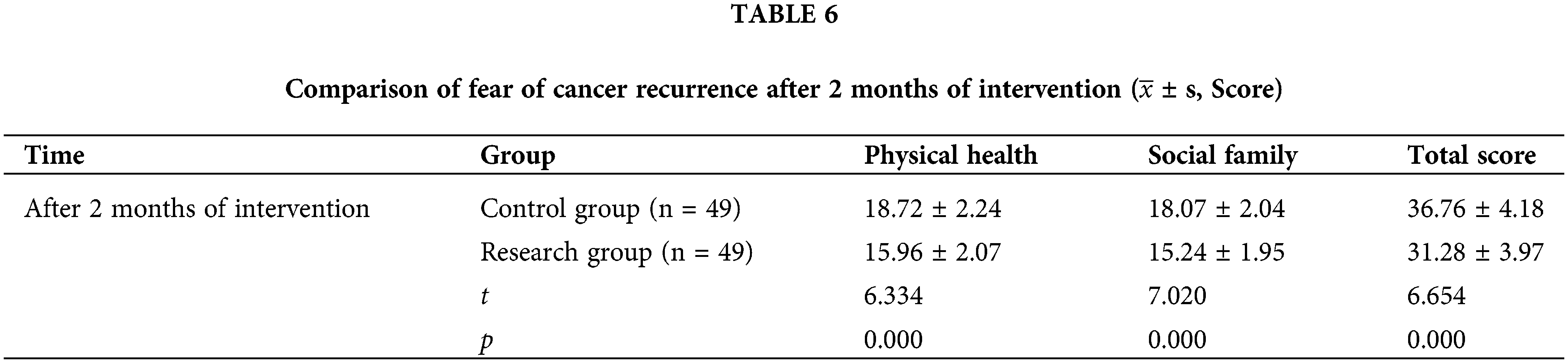
2. Fear of cancer recurrence: The fear of cancer recurrence inventory was used to evaluate the fear of cancer recurrence in two groups, with 12 items in 2 dimensions, 1–5 points for each item and 12–60 points in total. The higher the score was, the more serious the fear of cancer recurrence would be [10].
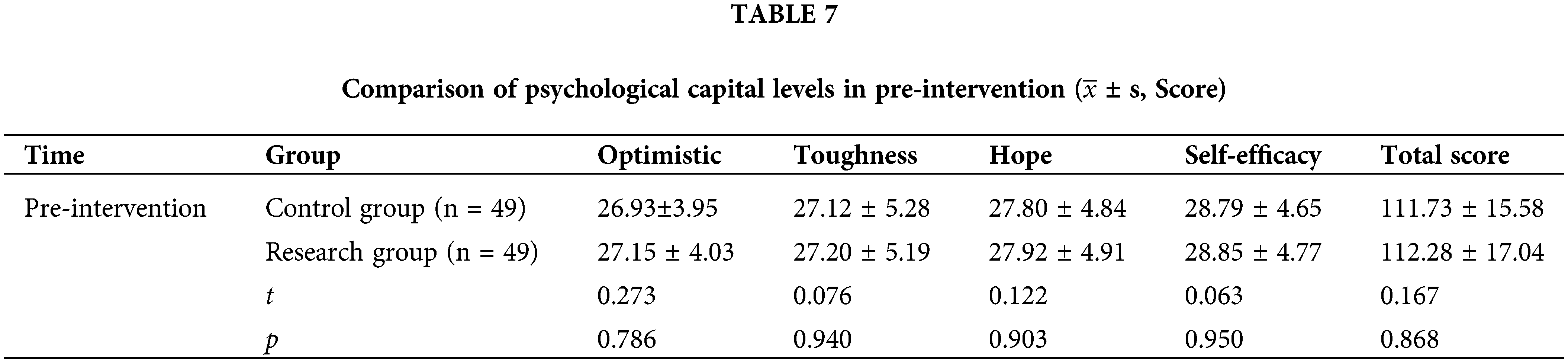
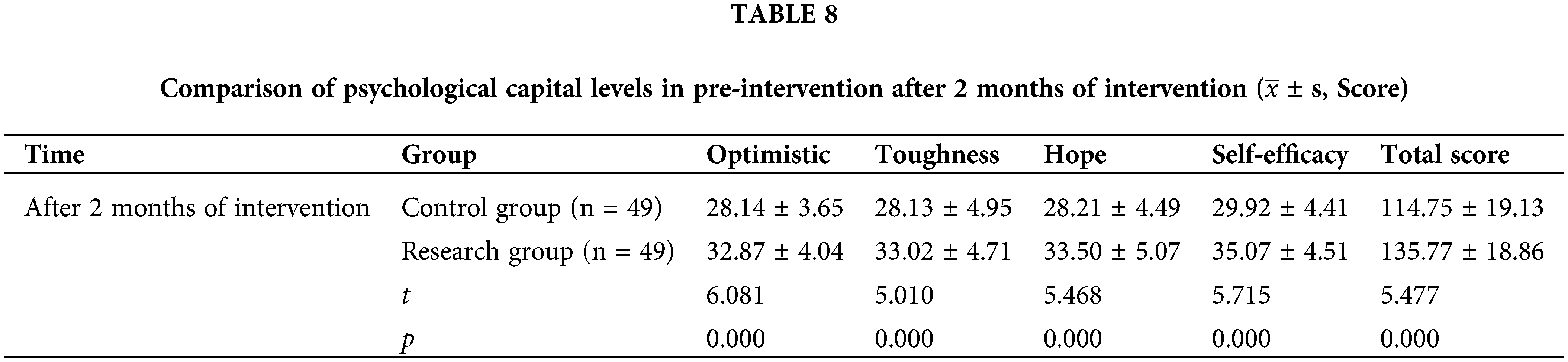
3. Psychological capital: The psychological capital questionnaire was used to evaluate the psychological capital level of the two groups, with a total of 4 dimensions and 26 items, each with 1–7 points. The higher the score was, the higher the psychological capital level was [11].
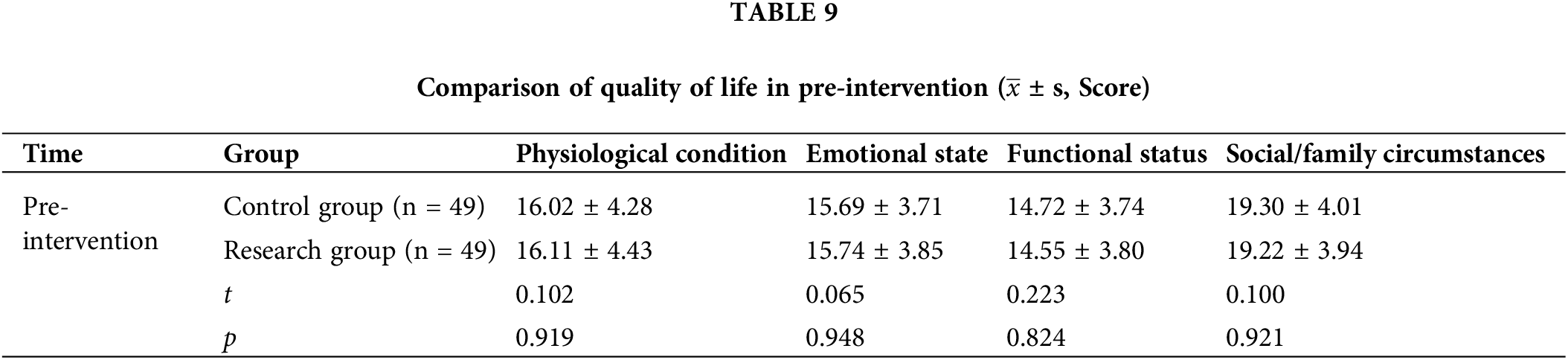
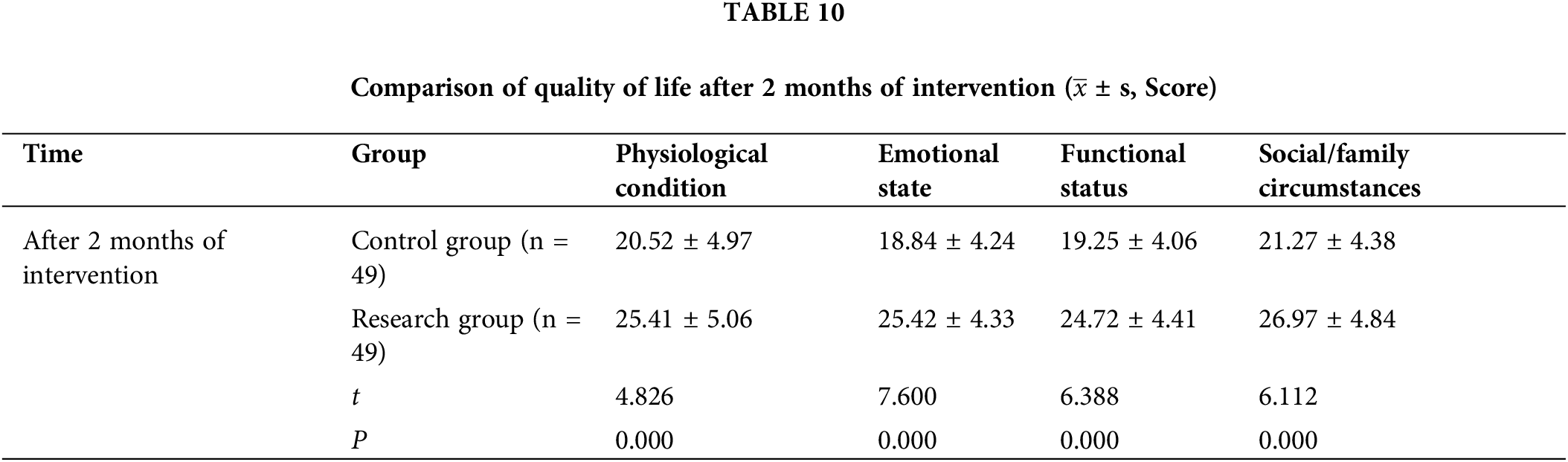
4. Quality of life: The functional assessment of cancer therapy-general (FACT-G) was used to evaluate the quality of life of the two groups, with 27 items in four dimensions, with 0–4 points for each item. The higher the score was, the higher the quality of life was [12].
The collected data were entered into EpiData 3.1 database in the form of double checking and double entry, and the data were analysed by applying IBM SPSS 25.0 statistical software. Measurement data were described by mean ± standard deviation (
Basic information of particpants
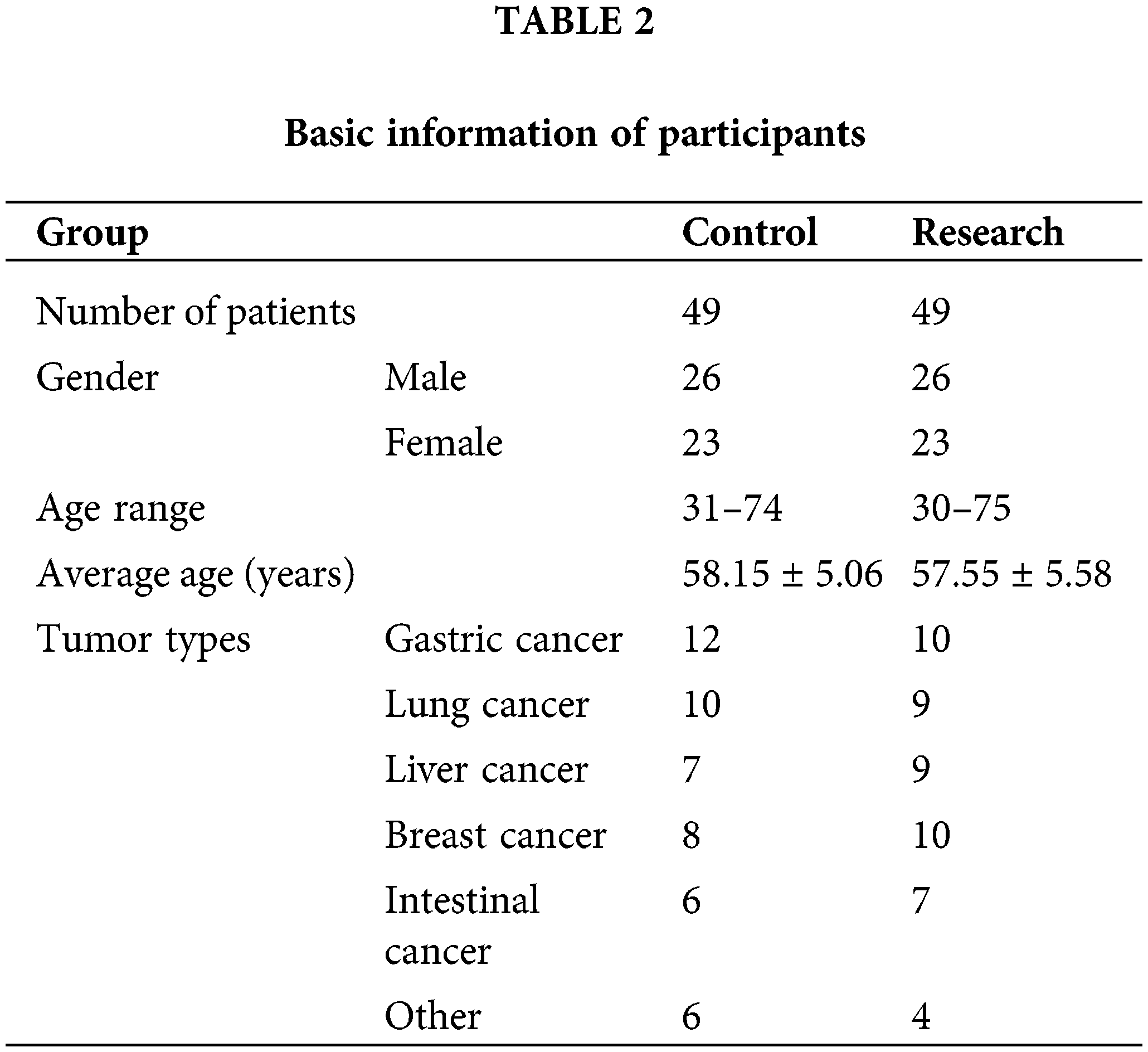
A total of 98 patients with chronic cancer pain who were admitted to Integrated Traditional Chinese and Western Medicine Department of Nantong Cancer Hospital, Jiangsu Provincel from March 2021 to March 2023 were randomly divided into two groups, 49 cases in each group. There were 26 males and 23 females in the control group; The age ranged from 31 to 74 years, with an average of (58.15 ± 5.06) years; Tumor types: gastric cancer 12 cases, lung cancer 10 cases, liver cancer 7 cases, breast cancer 8 cases, intestinal cancer 6 cases, other 6 cases. There were 26 males and 23 females in the research group; The age ranged from 30 to 75 years, with an average of (57.55 ± 5.58) years; Tumor types: gastric cancer 10 cases, lung cancer 9 cases, liver cancer 9 cases, breast cancer 10 cases, intestinal cancer 7 cases, others 4 cases (Table 2).
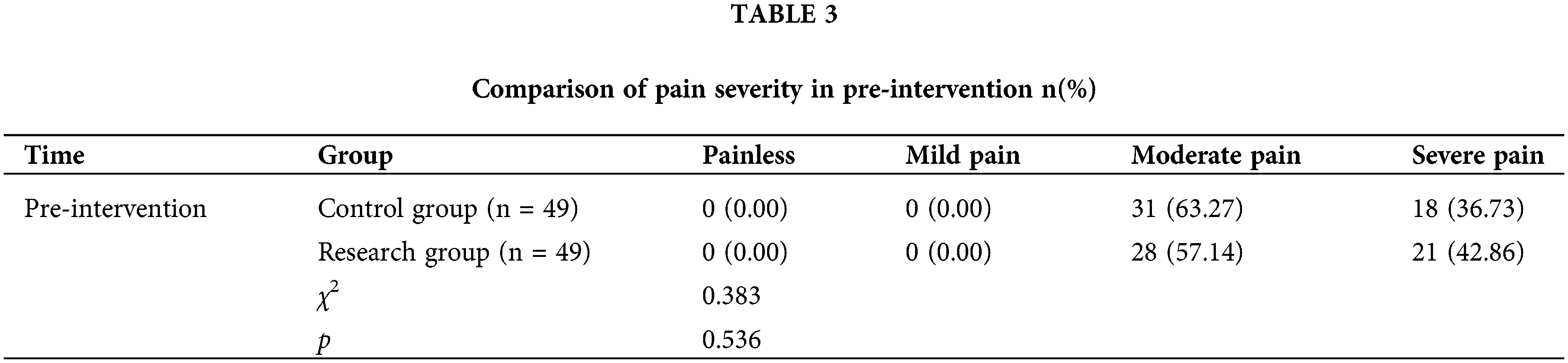
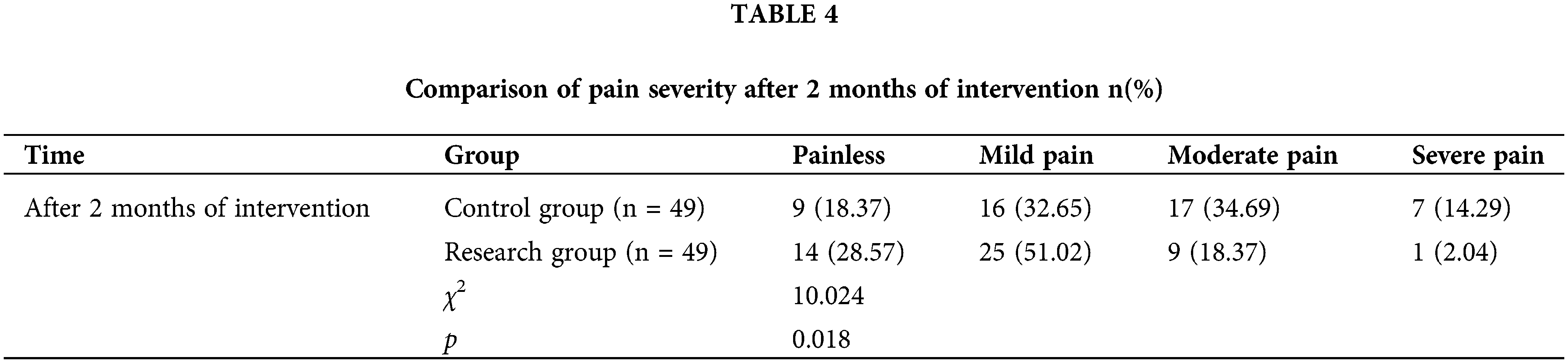
After two months of intervention, the pain severity in the research group was milder than that in the control group (p < 0.05) (Tables 3 and 4).
After two months of intervention, the scores and total scores of all dimensions of fear of cancer recurrence in the research group were lower than those in the control group (p < 0.05) (Tables 5 and 6).
After two months of intervention, the scores and total scores of each dimension of psychological capital in the research group were higher than those in the control group (p < 0.05) (Tables 7 and 8).
After two months of intervention, the scores of each dimension of quality of life in the research group were higher than those in the control group (p < 0.05) (Tables 9 and 10).
With the changes in people’s lifestyle and habits, the increase in work and life pressure, and poor diet and living habits, the incidence of cancer is significantly increased, which has a huge impact on the physiology and psychology of patients and significantly reduces their quality of life [13,14]. Pain is not only a physiological activity, but also can cause significant impact on the psychology of patients, becoming a high incidence symptom of cancer patients [15]. Cancerous pain has a great impact on the quality of life of patients and also causes great distress to the psychological, physiological and mental status of patients [16]. Persistent carcinomatous pain has caused great damage to the patient’s body, resulting in partial loss of confidence in treatment and life, or even suicidal ideation in severe cases [17]. In addition, bad psychological emotions can also negatively affect the endocrine, neurological, and immune regulatory functions of the body, causing disorders of the immune regulatory system and eventually leading to the growth and spread of tumor cells [18,19]. Therefore, effective psychological intervention measures should be taken for such patients to alleviate their bad emotions and promote the improvement of their quality of life [20]. In this study, we constructed the PERMA model in the psychological intervention for patients with chronic cancer pain and achieved significant results.
In this study, it was observed that the pain in the research group was milder than that in the control group after two months of intervention (p < 0.05). These results indicated that the PERMA model constructed in the psychological intervention for patients with chronic cancer could effectively relieve the pain. The reason for this analysis is that positive psychology believes that by using its potential strength, it can gradually help patients to change bad psychological emotions and promote the rise of happiness. The PERMA model was integrated into the positive psychological intervention, and effective targeted psychological intervention measures were formulated through the five elements that affect happiness, positive emotion (P), engagement (E), positive relationships (R), meaning (M) and accomplishment (A) [21,22]. As a result, patients can focus on the beautiful things and people in life, and actively view their own condition at the same time. In order to face difficulties and pain symptoms with an optimistic attitude, and cooperate with the analgesic drug intervention, they can finally effectively adjust their pain perception and response, increase the pain threshold, and thus relieve pain [23,24]. The results of this study showed that the scores and total scores of all dimensions of fear of cancer recurrence in the research group were lower than those in the control group (p < 0.05). These results indicated that the PERMA model constructed in the psychological intervention for chronic cancer patients could effectively alleviate the fear of cancer recurrence. The reason was analyzed as follows: Intervention staff conducted positive disease cognition guidance for patients, encouraged them to pay attention to the positive side of daily life, and helped patients to alleviate concerns about cancer recurrence and metastasis through active communication and relaxation training [25,26]. In this study, the scores and total scores of each dimension of psychological capital in the research group were higher than those in the control group (p < 0.05). It indicated that the construction of PERMA model in psychological intervention for patients with chronic cancer could effectively improve the level of psychological capital. The reason for the analysis is that psychological capital refers to the emotions, psychological attitudes and potentials exhibited by individuals in their growth and development. These factors together affect individual mental health and emotional adaptability. A higher level of psychological capital enables them to better cope with various difficulties in life [27,28]. During the intervention for patients with chronic cancer pain, we should encourage them to actively express their inner feelings, so as to increase their confidence in accepting their own diseases and overcoming them. By encouraging patients to do what they are good at and setting personalized goals for them, they can obtain a sense of achievement, gradually form a positive and optimistic thinking, and finally gradually improve the level of psychological capital [29]. In this study, it was observed that the scores of all dimensions of quality of life in the research group were higher than those in the control group (p < 0.05). The main analysis reason is that by constructing PERMA model in psychological intervention, patients with chronic cancer pain can be promoted to actively cope with the pain, psychological resilience is improved, and the happiness and satisfaction of life are promoted. It helps patients to find a meaningful direction in life, relieves adverse psychological emotions, and ultimately significantly improves the quality of life [30].
Despite the promising results demonstrated in this study on the clinical effects of applying the PERMA model in psychological intervention for patients with chronic cancer pain, there are several limitations that should be acknowledged. Firstly, the study had a relatively small sample size of 98 patients, which may limit the generalizability of the findings to a broader population. Larger sample sizes would allow for more robust analysis and conclusions. Secondly, the study was conducted over a short duration of two months, limiting the ability to assess the long-term sustainability of the intervention’s effects. Follow-up studies with extended intervention periods would provide valuable insights into the durability of the PERMA model. Thirdly, the study design was a randomized controlled trial, but it did not include a placebo group. The inclusion of a placebo group would have allowed for a more rigorous assessment of the specific effects of the PERMA model intervention, as opposed to potential placebo effects. Lastly, the study focused primarily on quantitative measures of pain, fear of cancer recurrence, psychological capital, and quality of life. Incorporating qualitative methods, such as interviews or focus groups, could provide a deeper understanding of the patients’ experiences and perceptions of the PERMA model intervention. In summary, while the study offers valuable insights into the potential benefits of the PERMA model in psychological intervention for chronic cancer pain, future research with larger sample sizes, longer intervention periods, inclusion of placebo groups, and integration of qualitative methods would help address these limitations and further strengthen the evidence base for this intervention approach.
Innovation Points and Clinical Significance of the Study. The innovation Points is application of the PERMA Model in Cancer Pain Management: This study innovatively applies the PERMA model, which stands for Positive Emotion, Engagement, Relationships, Meaning, and Achievement, in the psychological intervention for patients with chronic cancer pain. This approach represents a departure from traditional pain management strategies, focusing on the psychological aspects of pain and its impact on patients’ overall well-being. The clinical Significance is improving Quality of Life for Cancer Patients: By reducing pain severity and fear of cancer recurrence, the PERMA model intervention has the potential to significantly improve the quality of life for patients with chronic cancer pain. This is crucial for cancer patients, who often face not only physical pain but also emotional and social challenges.
In summary, the PERMA model constructed in psychological interventions for patients with chronic cancer pain can assist analgesic medications to reduce pain and alleviate the fear of cancer recurrence, increase the level of psychological capital, and thus improve quality of life.
Acknowledgement: The authors are grateful to Dong-Li Ji for her help with the preparation of figures in this paper.
Funding Statement: The authors extend their appreciation to the Deanship of Research and Graduate Studies of King Khalid University for funding this work through grant number RGP1/194/45; Research Project Funded by Nantong Municipal Health Commission (QNZ2023058).
Author Contributions: Yu-Feng Ren designed the research study; Yu-Feng Ren, Dong-Li Ji, Yu Wu, Ru-Qin Ben and Hai-Xia Wei performed the primary literature review and data extraction; Yu-Feng Ren, Dong-Li Ji, Yu Wu, Ru-Qin Ben and Hai-Xia Wei analyzed the data and wrote the manuscript; Yu-Feng Ren was responsible for revising the manuscript for important intellectual content. All authors reviewed the results and approved the final version of the manuscript.
Availability of Data and Materials: The data of this study will be provided as required.
Ethics Approval: The procedures for both T1 and T2 surveys adhered to the (i) declaration of Helsinki, and (ii) ethical principles for medical, psychological, and sociological research involving human participants. The Nantong Cancer Hospital Research Ethics Committee approved the study protocol (Approval No. Tongzhonglun Review (Research) 2023-065). All participants signed theinformed consent in this study.
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
References
1. Fink RM, Gallagher E. Cancer pain assessment and measurement. Semin Oncol Nurs. 2019;35(3):229–34. doi:10.1016/j.soncn.2019.04.003. [Google Scholar] [PubMed] [CrossRef]
2. Liu XL, Zhu GY. Effect of standardized cancer pain intervention on cancer pain degree, psychological state and quality of life in patients with advanced lung cancer. Oncol Prog. 2023;21(4):435–8+450. [Google Scholar]
3. Eaton LH, Brant JM, McLeod K, Yeh C. Nonpharmacologic pain interventions: a review of evidence-based practices for reducing chronic cancer pain. Clin J Oncol Nurs. 2017;21(3):54–70. doi:10.1188/17.CJON.S3.54-70. [Google Scholar] [PubMed] [CrossRef]
4. Knoerl R, Lavoie Smith EM, Weisberg J. Chronic pain and cognitive behavioral therapy: an integrative review. West J Nurs Res. 2016;38(5):596–628. doi:10.1177/0193945915615869. [Google Scholar] [PubMed] [CrossRef]
5. Hu TT, Ren HY, Xu XX, Wang MX, Goa YN, Zhang G, et al. Effects of standardized pain assessment and peer education in cancer pain patients. Chin J Mod Nurs. 2021;27(6):799–803 (In Chinese). [Google Scholar]
6. Wu XL, Liang MB, Zhuang XQ, Qin HY, Qin XF, Jia DM, et al. Establishment of quality evaluation criteria for out-patient medical records of cancer pain and assessment of its application effect. Natl Med J China. 2022;102(39):3115–20 (In Chinese). [Google Scholar]
7. Meng YJ, Chen JY, Zhang Q, Li J, Li JC. Application of pharmaceutical care model in pain management of cancer patients. Hainan Med J. 2022;33(18):2410–12 (In Chinese). [Google Scholar]
8. Eaton LH, Jang MK, Jensen MP, Pike KC, Heitkemper MM, Doorenbos AZ. Hypnosis and relaxation interventions for chronic pain management in cancer survivors: a randomized controlled trial. Support Care Cancer. 2022;31:50. doi:10.1007/s00520-022-07498-1. [Google Scholar] [PubMed] [CrossRef]
9. Yang HL, Zhao JW, Jiang JY, Lu YL. Intervention effect of dignity therapy on psychological distress and dignity level of patients with moderate and severe cancer pain. J Nurse Train. 2023;38(1):69–72+80 (In Chinese). [Google Scholar]
10. Lovell MR, Phillips JL, Luckett T, Lam L, Boyle FM, Davidson PM, et al. Effect of cancer pain guideline implementation on pain outcomes among adult outpatients with cancer-related pain: a stepped wedge cluster randomized trial. JAMA Netw Open. 2022;5(2):e220060. doi:10.1001/jamanetworkopen.2022.0060. [Google Scholar] [PubMed] [CrossRef]
11. Paice JA, Mulvey M, Bennett M, Dougherty PM, Farrar JT, Mantyh PW, et al. AAPT diagnostic criteria for chronic cancer pain conditions. J Pain. 2017;18(3):233–46. doi:10.1016/j.jpain.2016.10.020. [Google Scholar] [PubMed] [CrossRef]
12. Zhang J, Yang XY, Ren JW. Effect of external application of self-made aitong powder on pain relief and treatment compliance for patientswith bone metastases. J Sichuan Tradit Chin Med. 2021;39(1):205–8 (In Chinese). [Google Scholar]
13. Gao PP, Xu JJ, Gong JR, Lu HP. Effect of whole-process management for outpatients with cancer pain based on medication therapy management. Fudan Univers J Med Sci. 2022;49(5):649–55 (In Chinese). [Google Scholar]
14. Brant JM. The assessment and management of acute and chronic cancer pain syndromes. Semin Oncol Nurs. 2022;38(1):151248. doi:10.1016/j.soncn.2022.151248. [Google Scholar] [PubMed] [CrossRef]
15. Huang AM, Yang J, Wang XL, Shang MM, Liu QK, Tang N, et al. Study on the application of emotion function exercise in negative psychology and quality of life of patients with cancer pain in digestive tract (with video). Chin J Cancer Prev Treat. 2022;29(14):1074–9 (In Chinese). [Google Scholar]
16. Eaton LH, Hulett JM. Mind-body interventions in the management of chronic cancer pain. Semin Oncol Nurs. 2019;35(3):241–52. doi:10.1016/j.soncn.2019.04.005. [Google Scholar] [PubMed] [CrossRef]
17. Park S, Sato Y, Takita Y, Tamura N, Ninomiya A, Kosugi T, et al. Mindfulness-based cognitive therapy for psychological distress, fear of cancer recurrence, fatigue, spiritual well-being, and quality of life in patients with breast cancer–a randomized controlled trial. J Pain Symptom Manag. 2020;60(2):381–9. doi:10.1016/j.jpainsymman.2020.02.017. [Google Scholar] [PubMed] [CrossRef]
18. Ran JB, Liu L, Deng MY. Efficacy of FOCUS PDCA in reducing the incidence of breakthrough pain in inpatients with cancer pain. Chin J Clin Oncol Rehabil. 2021;28(11):1364–6 (In Chinese). [Google Scholar]
19. Peng DD, Zhou J, Shi YX, Cheng J. Effects of behavioral change combined with deep breathing and rest training on quality of life and compliance in patients with cancer pain. Chin J Health Care Med. 2022;24(6):492–4 (In Chinese). [Google Scholar]
20. Bao T, Seidman A, Li Q, Seluzicki C, Blinder V, Meghani SH, et al. Living with chronic pain: perceptions of breast cancer survivors. Breast Cancer Res Treat. 2018;169(1):133–40. doi:10.1007/s10549-018-4670-9. [Google Scholar] [PubMed] [CrossRef]
21. Gao M. The effect of hope intervention combined with WeChat platform health education on cancer pain in elderly patients with advanced lung cancer. Shanxi Med J. 2022;51(23):2743–6 (In Chinese). [Google Scholar]
22. Wang J, Li LM. Effects of pain education combined with three-step analgesic ladder on medication compliance and quality of life of patients with advanced cancer pain. J Clin Res. 2022;39(6):929–31 (In Chinese). [Google Scholar]
23. Fernández-Castillo RJ, Gil-García E, Vázquez-Santiago MS, Barrientos-Trigo S. Chronic non-cancer pain management by nurses in specialist pain clinics. Br J Nurs. 2020;29(16):954–9. doi:10.12968/bjon.2020.29.16.954. [Google Scholar] [PubMed] [CrossRef]
24. Ling GZ, Li MY, Wei RQ, Huang JL. Management effect of health education based on behavioral change wheel theory combined with clinical pharmacists-participated multidisciplinary team model on cancerous pain patients administrating opioid drugs. Guangxi Med J. 2022;44(23):2744–8 (In Chinese). [Google Scholar]
25. Costeira C, Paiva-Santos F, Pais N, Sousa AF, Paiva I, Carvalho DH, et al. Cancer patients with chronic pain and their caregivers during COVID-19: a descriptive study. Nurs Rep. 2023;13(3):934–45. doi:10.3390/nursrep13030082. [Google Scholar] [PubMed] [CrossRef]
26. Xu X, Cheng Q, Ou M, Li S, Xie C, Chen Y. Pain acceptance in cancer patients with chronic pain in Hunan, China: a qualitative study. Int J Nurs Sci. 2019;6(4):385–91. [Google Scholar] [PubMed]
27. Luo ZB, Luo BL, Chen QS, Wang PR, Guo ZJ, Lin YJ, et al. Qualitative study on self-management experience of patients with cancer pain. J Nurs Sci. 2021;36(11):21–4. [Google Scholar]
28. Deng TT, Zheng JJ. Effects of human based health education combined with standardized management on the treatment wish, rehabilitation belief and life quality of patientts with cancer pain. Hebei Med J. 2021;43(6):952–5 (In Chinese). [Google Scholar]
29. Check DK, Jones KF, Fish LJ, Dinan MA, Dunbar TK, Farley S, et al. Clinician perspectives on managing chronic pain after curative-intent cancer treatment. JCO Oncol Pract. 2023;19(4):e484–91. doi:10.1200/OP.22.00410. [Google Scholar] [PubMed] [CrossRef]
30. Zhang H, Zhang S, Song F, Sun Q. Effects of self-care management guided by empowerment theory in cancer pain patients. Chin J Mod Nurs. 2022;28(5):660–2 (In Chinese). [Google Scholar]
Cite This Article
 Copyright © 2024 The Author(s). Published by Tech Science Press.
Copyright © 2024 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools