 Open Access
Open Access
ARTICLE
The Mediating and Moderating Effects of Family Resilience on the Relationship between Individual Resilience and Depression in Patients with Breast Cancer
1 School of Psychology, Nanjing Normal University, Nanjing, 210000, China
2 Department of Nursing, Jiangsu Cancer Hospital & Jiangsu Institute of Cancer Research & The Affiliated Cancer Hospital of Nanjing Medical University, Nanjing, 210000, China
3 Jiangsu Province Key Laboratory of Anesthesiology, Xuzhou Medical University, Xuzhou, 221000, China
4 Department of Anesthesiology, Jiangsu Cancer Hospital & Jiangsu Institute of Cancer Research & The Affiliated Cancer Hospital of Nanjing Medical University, Nanjing, 210000, China
* Corresponding Authors: Qin Zhou. Email: ; Aiji Jiang. Email:
# These authors contributed equally to this work
Psycho-Oncologie 2024, 18(3), 191-200. https://doi.org/10.32604/po.2024.053942
Received 14 May 2024; Accepted 05 August 2024; Issue published 12 September 2024
Abstract
Objective: This study evaluated the effect of resilience on depression among patients with breast cancer from individual and familial perspectives by exploring the mediating and moderating effects of family resilience between individual resilience and depression. Methods: A questionnaire survey was conducted among 337 patients with breast cancer who were admitted to the Oncology Department of Jiangsu Province Hospital. The survey included demographic information, the Connor–Davidson Resilience Scale (CD-RISC), the Family Resilience Assessment Scale (FRAS), and the Chinese version of the Patient Health Questionnaire-9 (PHQ-9) for Depression. The relationship among individual resilience, family resilience, and depression was analyzed using hierarchical regression and bootstrap test to assess the mediating and moderating effects of family resilience. Results: The depression scores were (13.50 ± 5.16), the individual resilience scores were (48.62 ± 17.50), and the family resilience scores were (105.98 ± 24.35). Significant differences in depression scores were observed in terms of family monthly income, average weekly exercise before diagnosis, post-diagnosis interpersonal relationship quality, and overall sleep quality in the past month (p < 0.05). Patients with lower individual resilience had significantly higher depression scores than those with higher resilience (F = 24.314, p < 0.001), and similarly, patients with lower family resilience had higher depression scores than those with higher family resilience (F = 41.660, p < 0.001). Individual resilience and family resilience were significantly negatively correlated with depression (r = −0.447 and −0.441, respectively, p < 0.001). Hierarchical regression analysis and bootstrap test showed that family resilience (β = −0.310, p < 0.001) had a partial mediating effect between individual resilience (β = −0.321, p < 0.001) and depression. The indirect effect size was −0.038, the 95% CI was (−0.056, −0.020), and the direct effect ratio was 71.43%. The interaction of family resilience and individual resilience had a moderating effect on depression (B = 0.166, p < 0.001). Family resilience negatively moderated the relationship between individual resilience and depressive symptoms and enhanced the protective effect of individual resilience against depression with increasing family resilience. Conclusion: Family resilience has mediating and moderating effects between individual resilience and depression in patients with breast cancer.Keywords
Breast cancer is a malignant tumor that originates from the epithelial cells of the ducts or lobules of the breast [1]. According to the statistics from the International Agency for Research on Cancer of the World Health Organization in 2020, breast cancer had approximately 2.26 million new cases worldwide, and it is the most common and remarkable threat to women’s health globally [2–4]. Despite clinical breakthroughs in the treatment of breast cancer, including surgery, chemotherapy, radiotherapy, targeted therapy, and immunotherapy [5], the effect of psychological factors on malignancies has not received sufficient attention. Psychological stress can significantly affect the treatment outcomes and quality of life of patients with breast cancer by weakening the immune function, reducing treatment adherence, interfering with drug metabolism, and lowering the overall quality of life [6–8]. Depression is a common psychological health issue among patients with cancer. Research has shown that the prevalence of depression among patients with breast cancer is significantly higher (32.2%) than among healthy population (6.4%), with a notably higher proportion of severe depression cases [9]. Therefore, psychological interventions play a crucial role in enhancing the quality of life and potentially extending the survival of patients with breast cancer.
Individual resilience refers to a trait that enables a person to successfully adapt to and transform adversity into a positive force, helping to alleviate depression and anxiety in patients [10,11]. It serves as a protective factor in coping with cancer. Researching and strengthening individual resilience can enhance patients’ adaption to adversity, thus enhancing their confidence and ability to handle challenges and reducing the risk of psychological health issues [12]. It also lays the foundation for further exploring the role of family in the disease coping process.
Relying on the strength of the patient alone is not sufficient to deal with cancer as a major negative life event; social support is needed. Family plays a crucial protective role in the psychological health of patients with cancer and serves as a vital source of support in adapting to the challenges of the disease. Families vary in their capacity to adapt to stress and, consequently, in the level of psychological support they provide. Researchers have indicated that family resilience plays an important role in this context [13]. Family resilience refers to a family’s ability to flexibly rebound from adversity and demonstrate positive endurance, challenge-response capabilities, and self-recovery [14]. Robust family resilience not only alleviates the caregiving burden on family members but also enhances the protective effects on the psychological health of patients and caregivers. It helps families return to normal life trajectories and promotes post-traumatic growth in patients [15]. Therefore, recognizing the protective role of family resilience in addressing the psychological health issues of patients with breast cancer is vital.
Previous studies have confirmed that individual resilience and family resilience play a synergistic role, the improvement of both can improve individual mental health, and the two may interact. Tao et al. [16] pointed out that individual resilience plays a mediating role in family resilience and psychological distress in young patients with breast cancer. Li et al. [17] found that individual resilience can directly alleviate the fear of cancer recurrence in patients with breast cancer, whereas family resilience can indirectly alleviate the fear of cancer recurrence through individual resilience. In summary, family resilience may significantly influence on individual resilience and thus have an influence on the mental health of patients with breast cancer. However, whether family resilience has an effect on the intensity or direction of individual resilience on depression and how family resilience changes the intensity or direction of individual resilience on depression have been rarely researched. Therefore, the present study aimed to assess whether the two variables, family resilience and individual resilience, affect depression in patients with breast cancer, test whether family resilience is a mediating and moderating variable between individual resilience and depression, and determine how the moderating effect changes.
This study adopted a cross-sectional study and was designed to be conducted in December 2022. Nurses from the Milk and Gland Department of Jiangsu Cancer Hospital asked patients with breast cancer admitted to the department about their willingness to participate in the study in person or by phone from 01 January 2023 to 12 December 2023, emphasizing the voluntary nature of the test and the confidentiality of the study, and then the patients signed an informed consent form. Considering the physical and mental health status of patients with cancer, along with their age and educational level, scales with few questions and accurate and easy-to-understand language expression were adopted as much as possible to avoid discomfort and a negative effect on patients during the filling process. The questionnaire survey was conducted by answering questions on the spot or filling out the questionnaire star (distributed through WeChat), and the time allotted for participants to complete the whole questionnaire was about 5–10 min. Data collection was completed in January 2024, the analysis was ready, and the results were obtained. Data identifying personal information were deleted, and the manuscript was finally completed in April 2024.
Convenience sampling was performed, and patients with breast cancer who were admitted to the breast Department of Jiangsu Cancer Hospital from August 2023 to November 2023 were selected as the research objects. In structural equation research, the required sample size is 15–20 times the number of independent variables. This study had 18 independent variables, and the sample size was determined to be 270–360. A total of 354 questionnaires were issued in this study, and 337 effective questionnaires were finally included in the analysis, with an effective rate of 95.20%. The inclusion criteria were as follows: (1) confirmed diagnosis of breast cancer; (2) age ≥18 years, with awareness of the condition and diagnosis; (3) clear consciousness, without cognitive nor communication barriers; and (4) informed consent provided and voluntary participation in the study. The exclusion criteria were as follows: (1) concurrent severe diseases; (2) with other types of cancer; and (3) incomplete data or withdrawal from the study partway through. The study was approved by the Ethical Committee of Jiangsu Province Cancer Hospital (No. 2023009). All participants provided informed consent in this study.
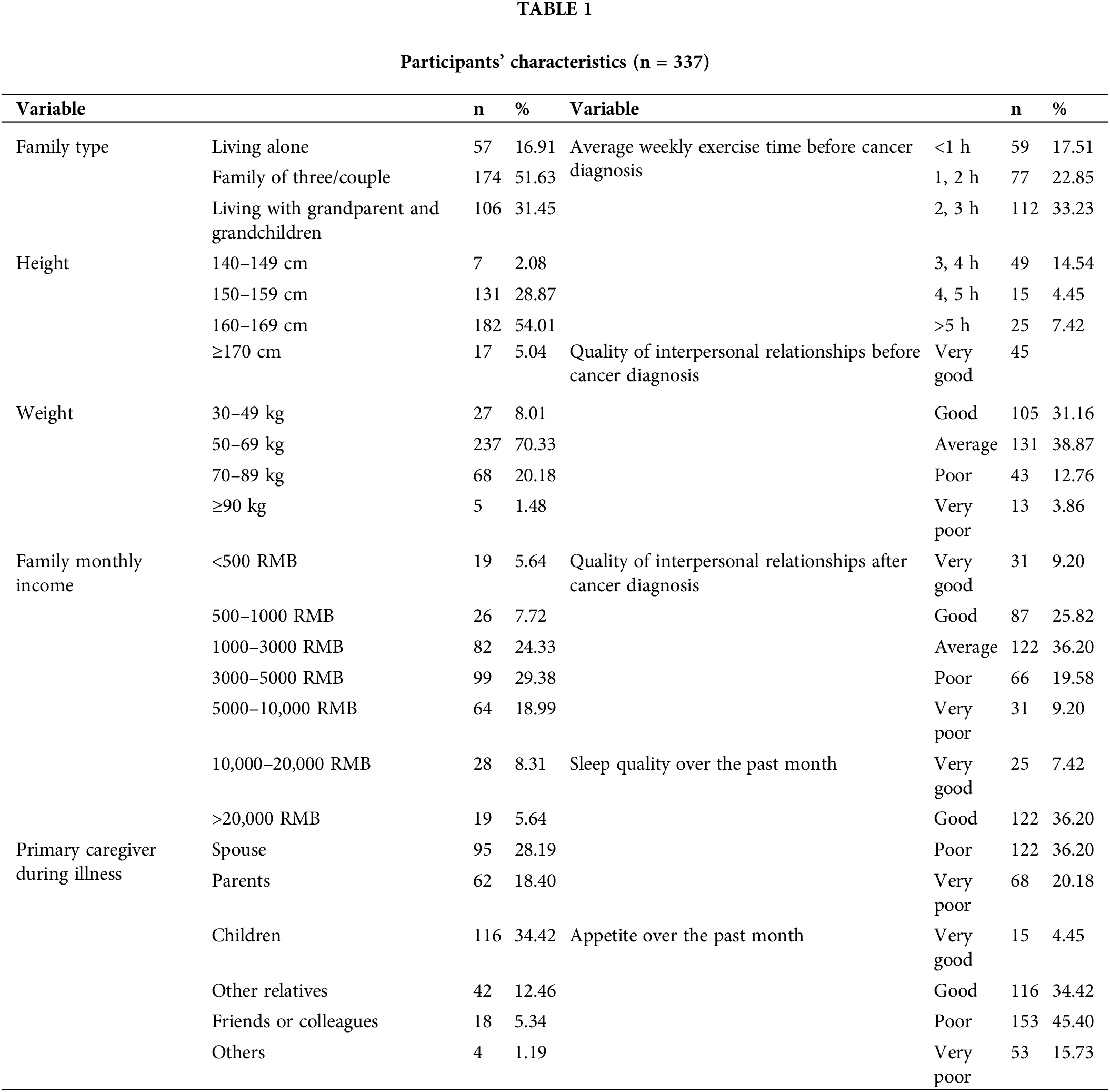
A custom-designed survey questionnaire was used to collect basic information, including height, weight, type of family, family monthly income, primary caregiver during the illness, average weekly exercise time before cancer diagnosis, quality of interpersonal relationships before and after the diagnosis, sleep quality over the past month, and appetite over the past month, from the patients.
Connor–Davidson resilience scale (CD-RISC)
CD-RISC was utilized to assess the resilience levels of patients with breast cancer and their caregivers, and this scale is widely used in China [18]. This scale comprises 25 items covering three dimensions: tenacity, strength, and optimism. It employs a 5-point Likert scale for scoring, where 0–4 correspond to “never,” “seldom,” “sometimes,” “often,” and “always,” respectively. The total score ranges from 0 to 100, with higher scores indicating higher levels of individual resilience. The scale categorizes resilience scores into low (0–25), moderate, (26–75), and high (76–100) resilience levels. The Cronbach ‘α coefficient of this scale was 0.963 (KMO = 0.949, p < 0.001).
Family resilience assessment scale (FRAS)
FRAS is used to evaluate a family’s capacity to resiliently rebound when faced with adverse circumstances, It is the most commonly used scale in China to measure an individual’s family resilience [19]. The scale consists of 40 items divided into four dimensions: family communication and problem-solving, which includes 19 items; maintaining a positive outlook, which includes 10 items; family connection, which includes five items; and utilization of social and economic resources, which includes six items. Each item is scored on a 4-point Likert scale, ranging from 1 (strongly disagree) to 4 (strongly agree). The total score ranges from 40 to 160, with higher scores indicating greater family resilience. The Cronbach’α coefficient of this scale was 0.982 (KMO = 0.972, p < 0.001).
Chinese version of patient health questionnaire (PHQ-9)
PHQ-9 is primarily used to assess the symptoms and severity of depression, and it is widely used in China to evaluate patients’ psychological state regarding depression [20]. It comprises nine items, each rated on a 4-point Likert scale, with scores ranging from 0 (not at all) to 3 (nearly every day). The total score can range from 0 to 27, with higher scores indicating more severe symptoms of depression. The Cronbach’s α coefficient of this scale was 0.877 (KMO = 0.897, p < 0.001).
SPSS (version 26.0) software was used for statistical analysis. Univariate analyses were used to assess differences in depression scores across demographic variables. Differences in depression scores between groups with varying levels of individual resilience and family resilience were evaluated, with post-hoc pairwise comparisons were conducted for any significant differences. Pearson’s or Spearman’s correlation analyses were applied to examine the relationships among individual resilience, family resilience (total and by dimension), and depression status. Finally, hierarchical regression and bootstrap test were used to determine whether family mental resilience plays a mediating role between individual mental resilience and depression, and the PROCESS plugin of SPSS was used to analyze the moderating effect. A significance level of p < 0.05 was considered statistically significant.
A total of 337 patients with breast cancer completed the survey. Among them, 16.91% lived alone (57 cases), and those with family monthly income of 3000–5000 RMB (n = 99, 29.38%) and whose primary caregiver were children during illness (n = 116, 34.42%) were the most (Table 1).
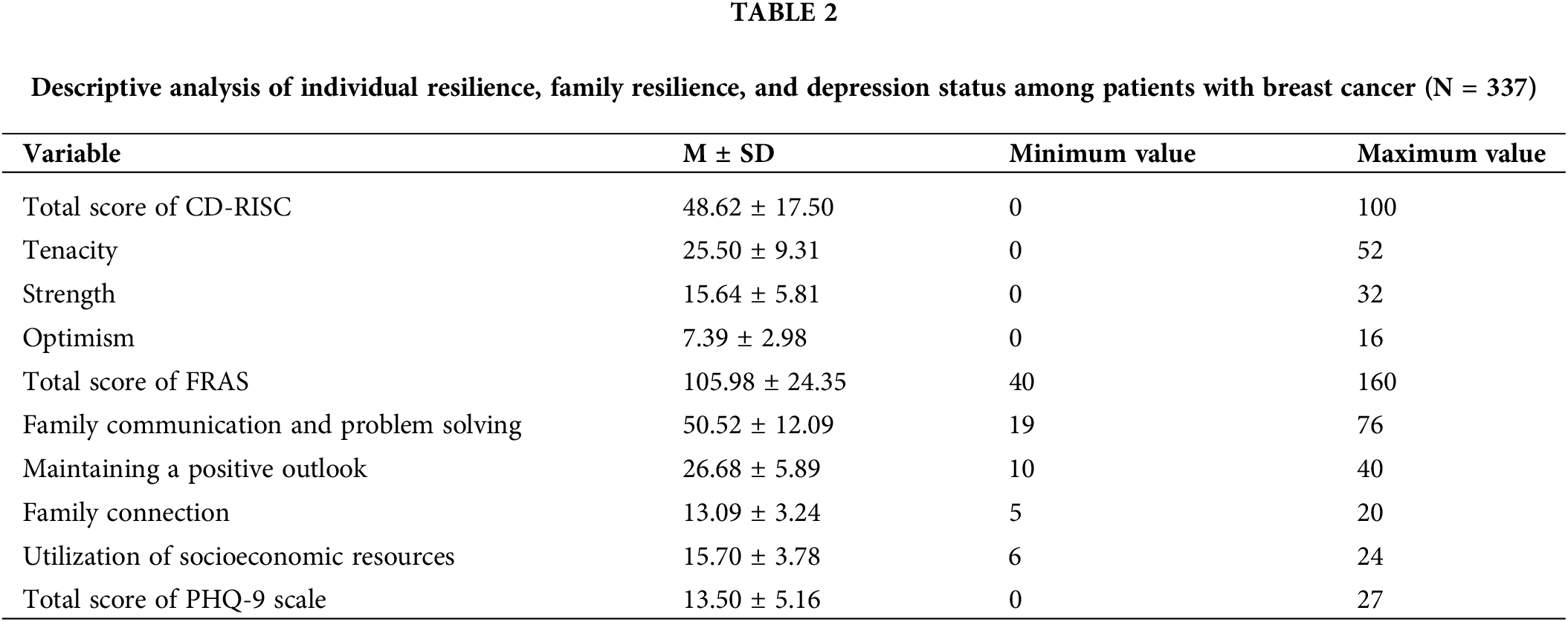
Descriptive statistical analysis of individual resilience, family resilience, and depression
Table 2 presents the scores for individual resilience, family resilience, and depression among patients with breast cancer. The results showed the following average scores: total CD-RISC score of 48.62 ± 17.50, total FRAS score of 105.98 ± 24.35, and total PHQ-9 score of 13.50 ± 5.16.
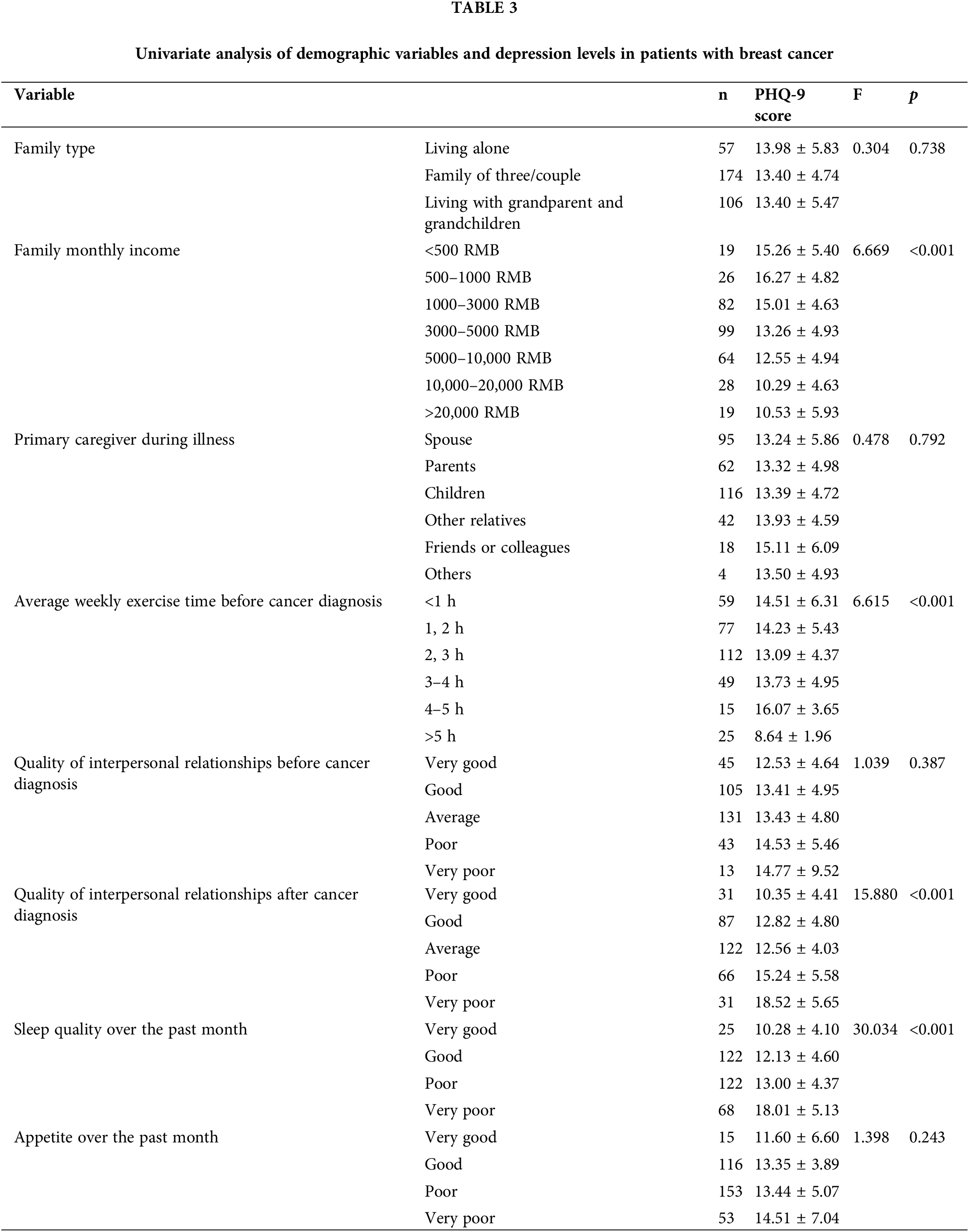
Univariate analysis of demographic variables and depression levels in patients with breast cancer
Univariate analysis of variance was conducted, with depression levels as the dependent variable and demographic variables as the independent variables. The results indicated significant differences in depression scores among patients with different levels of family monthly income (F = 6.669, p = 0.000), average weekly exercise time before cancer diagnosis (F = 6.615, p = 0.000), interpersonal relationship quality after diagnosis (F = 15.880, p = 0.000), and overall sleep quality in the past month (F = 30.034, p = 0.000). However, no significant differences in depression scores were found among patients with different types of families, primary caregivers during illness, interpersonal relationship quality before cancer diagnosis, and appetite over the past month (p > 0.05, Table 3).
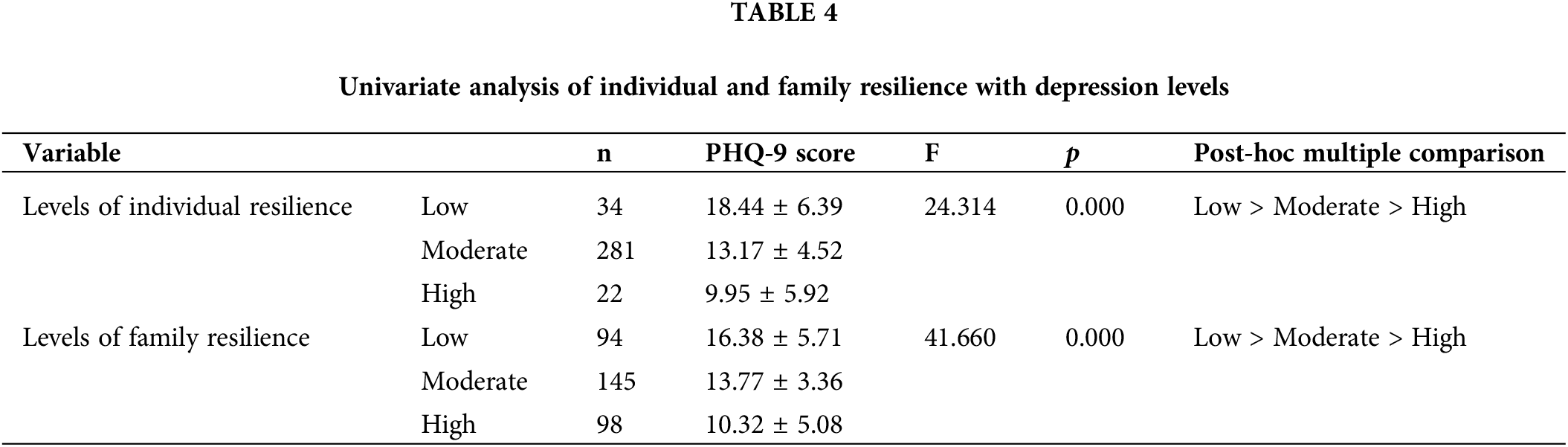
Univariate analysis of individual and family resilience with depression levels
The individual resilience scores were categorized as follows: scores of 0–25 was classified into the low individual resilience group, consisting of 34 individuals; scores of 26–75 was placed in the moderate individual resilience group, consisting of 281 individuals; and scores of 76–100 were categorized into the high individual resilience group, comprising 22 individuals. By using extreme grouping, the top 27% highest scorers on FRAS were classified into the high group (98 individuals), the lowest 27% were categorized into the low group (94 individuals), and those scoring between the 27th and 46th percentiles were placed in the moderate group (145 individuals).
The univariate analysis showed significant differences in PHQ-9 depression scores among patients with different levels of individual resilience (F = 23.314, p = 0.000). Post-hoc multiple comparison results indicated that patients with low individual resilience had significantly higher PHQ-9 scores than those with moderate resilience, and those with moderate resilience had higher scores than those with high resilience. Similar significant differences were observed in PHQ-9 scores among patients with different levels of family resilience (F = 41.660, p = 0.000). Post-hoc comparisons revealed that patients with low family resilience had significantly higher PHQ-9 scores than those with moderate resilience, and those with moderate resilience scored higher than those with high resilience (Table 4).
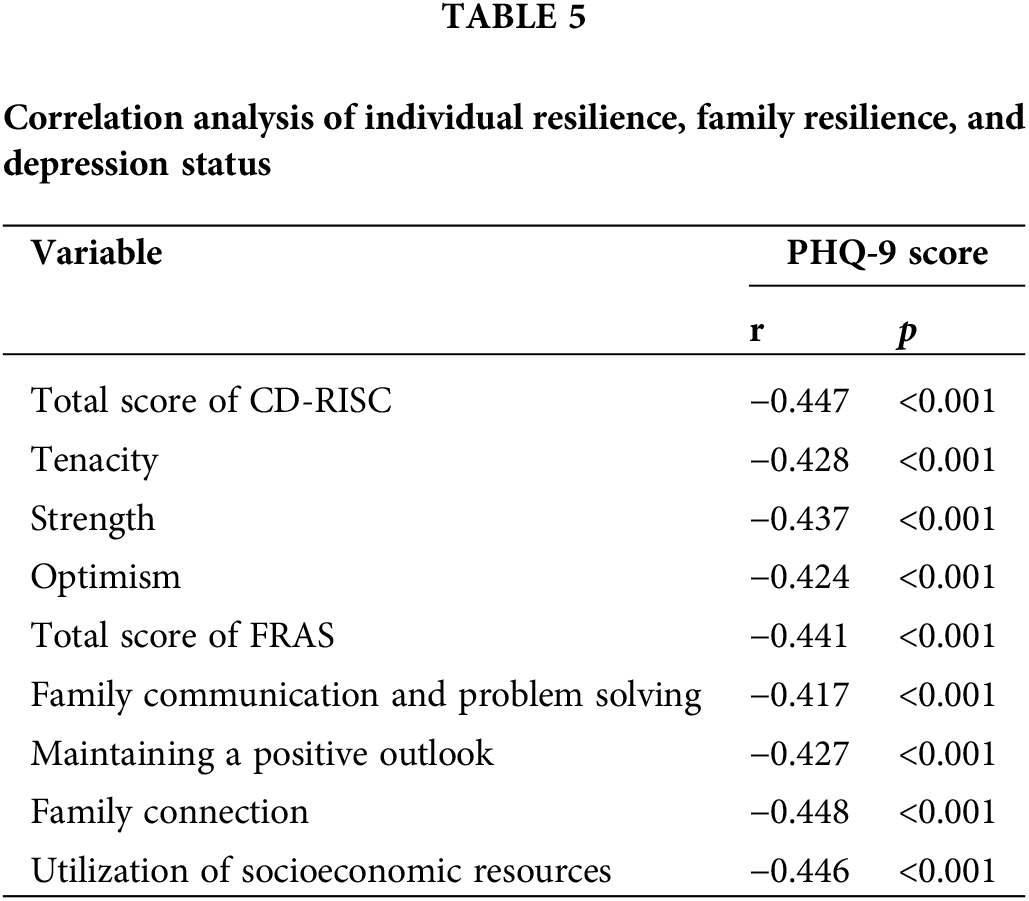
Correlation analysis of individual resilience, family resilience, and depression status
The correlation analysis results indicated that the total score of CD-RISC and its individual dimensions were significantly negatively correlated with the total PHQ-9 score among patients with breast cancer (p = 0.000). Similarly, the total score of FRAS and its dimensions were significantly negatively correlated with the total PHQ-9 score (p = 0.000, Table 5).
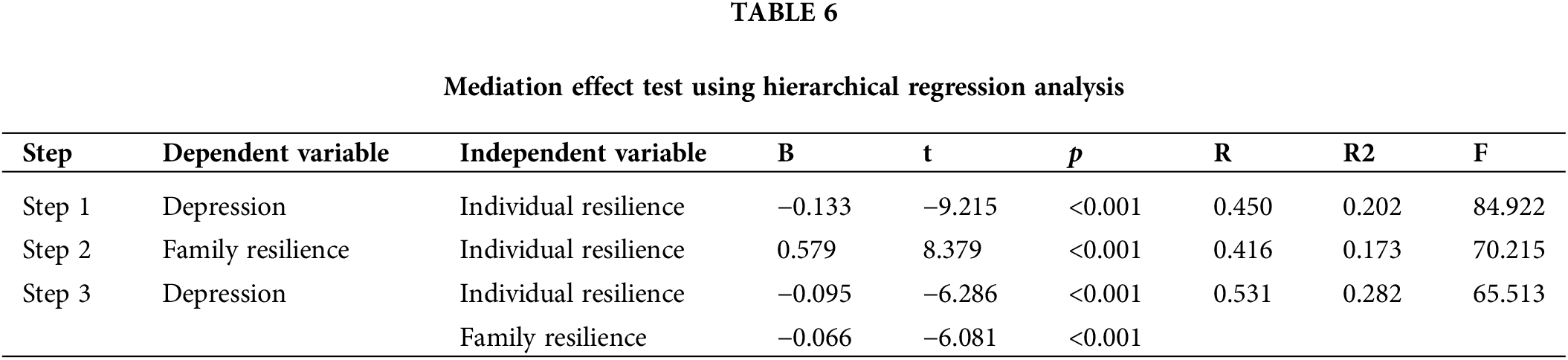
Mediating role of family resilience between individual resilience and depression
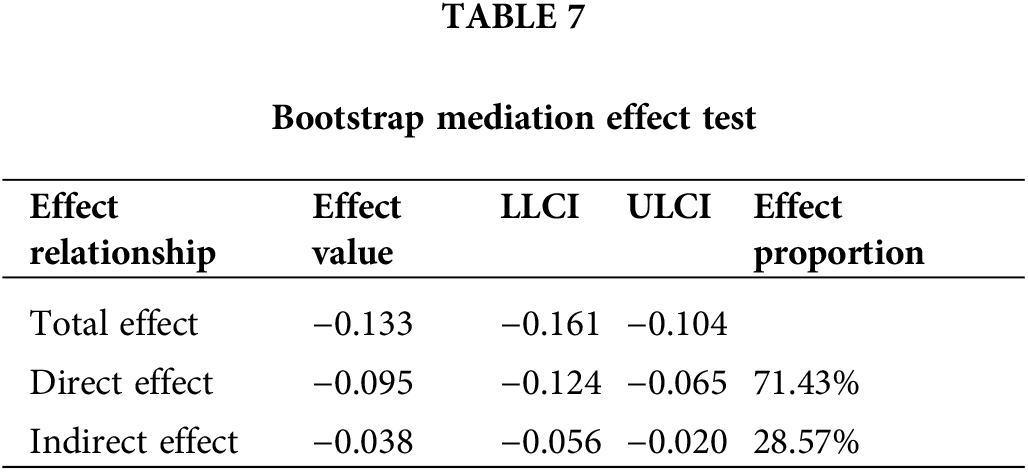
The mediating effect was tested using hierarchical regression analysis. In the first step, individual resilience was used as the independent variable and depression as the dependent variable to examine the predictive effect of individual resilience on depression. In the second step, individual resilience was used as the independent variable and family resilience as the dependent variable to examine the predictive effect of individual resilience on family resilience. In the third step, individual resilience and family resilience were used as independent variables, and depression was used as the dependent variable to examine the predictive effects of individual resilience and family resilience on depression. The results showed that individual resilience had a significant negative predictive effect on depression (β = −0.450, p < 0.001) and a significant positive predictive effect on family resilience (β = 0.416, p < 0.001). After the mediating variable was included, ndividual resilience (β = −0.321, p < 0.001) and family resilience (β = −0.310, p < 0.001) remained significant predictors of depression, indicating that family resilience has a significant partial mediating effect between individual resilience and depression (Table 6). The bootstrap mediation effect test results showed an indirect effect value of −0.038, with a 95% CI of (−0.056, −0.020), and the direct effect accounted for 71.43% (Table 7).
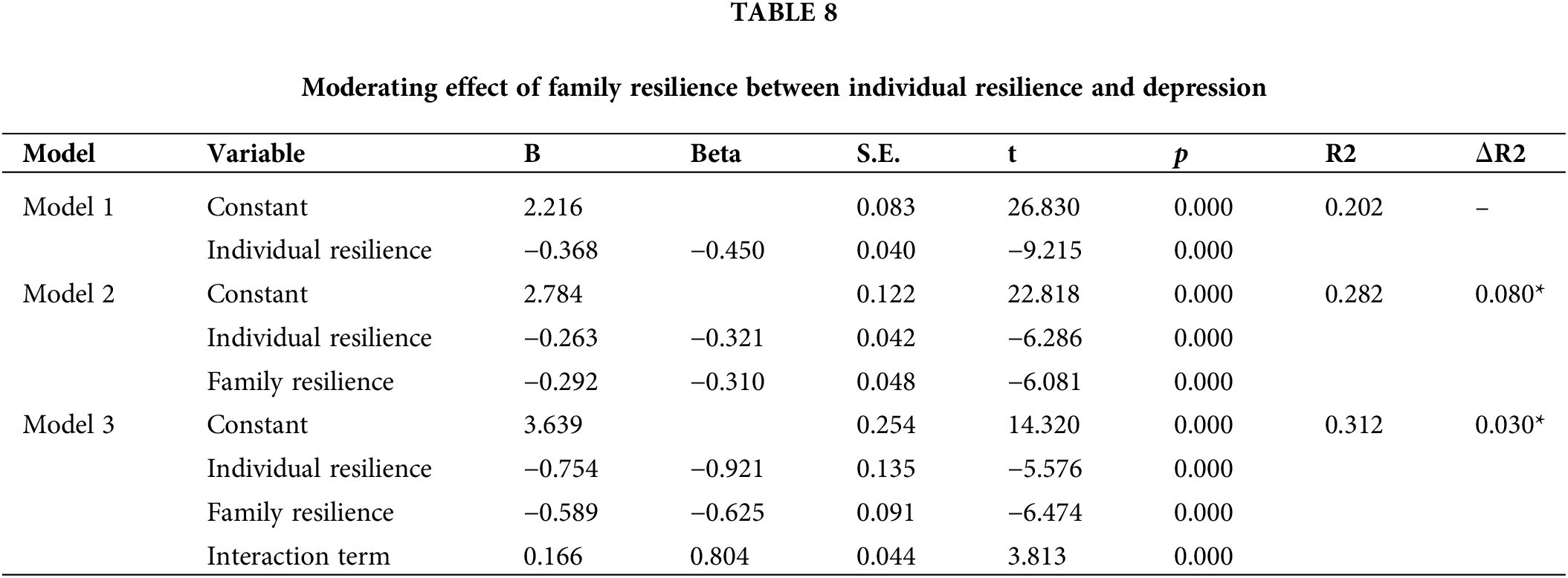
Moderating role of family resilience between individual resilience and depression
This study examined how individual resilience, as an independent variable, influences depressive symptoms, with family resilience acting as a moderating variable to test whether it affects (either strengthens or weakens) the effect of individual resilience on depression. The results indicated that individual resilience (B = −0.368, p = 0.000 and family resilience (B = −0.292, p = 0.000) significantly negatively predict depression. The interaction effect between individual and family resilience was statistically significant (B = 0.166, p = 0.000), with the positive value indicating that as family resilience increases, so does the protective effect of individual resilience against depression (Table 8).
Analysis using the PROCESS plugin showed that as the FRAS score increased, the moderating effect decreased (negative change), indicating that family resilience significantly negatively moderates the relationship between individual resilience and depressive symptoms (Fig. 1A). Further analysis of the patterns between individual resilience and depression scores at low and high levels of family resilience (low and high FRAS scores) revealed that the relationship between individual resilience and depression scores was more negative at lower levels of family resilience. This finding indicated that higher individual resilience scores were associated with lower PHQ-9 scores. However, at higher levels of family resilience, this relationship was less pronounced (Fig. 1B).
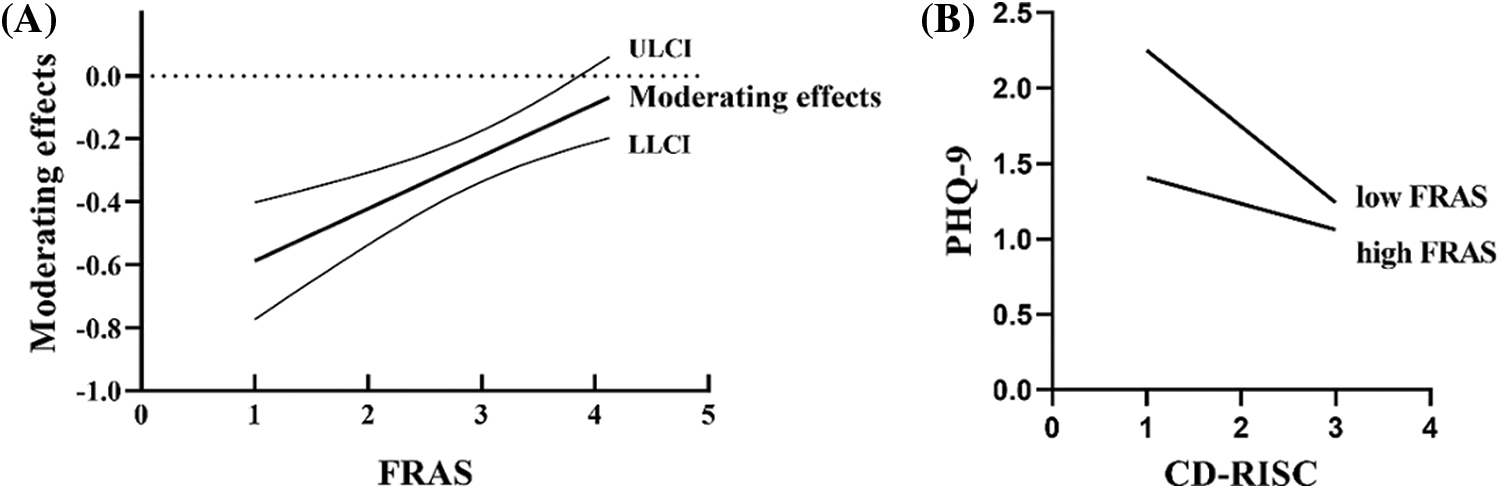
Figure 1: Diagram of the moderating effect of family resilience between individual resilience and depression. (A) Moderating role of family resilience between individual resilience and depression. ULCI, upper-level confidence interval; LLCI, lower-level confidence interval. (B) Moderating effects between individual resilience and depression at high and low levels of family resilience.
This study analyzed the factors contributing to depressive moods in patients with breast cancer. The results identified several key factors affecting depression among patients with breast cancer, including family monthly income, average weekly exercise time before cancer diagnosis, quality of interpersonal relationships after diagnosis, and overall sleep quality in the past month. Cancer imposes a significant economic burden on families, and a high family income serves as a robust support resource. It allows patients to undergo cancer treatment without the worry of financial constraints and thus could alleviate levels of depression; conversely, a low family income tends to have increased depression levels [21]. Moreover, exercise influences depression, as demonstrated by findings that subjects who engaged in more than 5 h of exercise per week had the lowest depression scores. This finding suggests that physical activity is beneficial for maintaining the psychological health of patients with cancer [22]. Álvarez-Pardo et al. [23] indicated that patients with breast cancer who receive socioemotional and material support exhibited a significant negative correlation with depressive symptoms. During periods of high stress, these patients need to express their feelings to family and friends to gain emotional support. The higher the quality of interpersonal relationships, the greater the perceived social support, which helps alleviate negative emotions. In the present study, patients with better interpersonal relationships after diagnosis had significantly lower depression scores than those with poorer relationships. Moreover, sleep disorders are prevalent among patients with breast cancer, and it can critically affect their quality of life [24]. A study assessing sleep quality among patients with breast cancer found a significant correlation between poor sleep quality and high levels of depression and low quality of life [25]. This finding aligns with the findings of the present study. The insomnia in patients may not be only related to the diagnosis and management of cancer but also directly affected by drugs and chemotherapy; insomnia affects depression, which, in turn, could aggravate insomnia, and how to improve patients’ sleep to reduce the degree of depression is a worthy direction of future research [26].
This study found that CD-RISC and FRAS scores were significantly negatively correlated with depression levels, suggesting that lower levels of either individual resilience or family resilience are associated with more severe depression. Individual resilience may directly influence psychological health by enhancing self-efficacy and positive emotional regulation, whereas family resilience might indirectly affect patients’ psychological states by providing social support and reducing daily stress. Further analysis identified the strength dimension of individual resilience as a significant negative predictor of depression levels. This dimension includes traits such as self-efficacy, goal orientation, and problem-solving abilities. Individuals with a higher strength dimension can more effectively mobilize internal resources and adopt proactive coping strategies when faced with difficulties, thereby reducing the occurrence of depressive moods [27,28]. The dimension of utilizing socioeconomic resources within family resilience significantly negatively predicted individual depression levels. This dimension involves how a family utilizes available economic and social resources to support its members during illness, indicating that families that can effectively manage and mobilize resources, such as financial aid, social connections, and access to information, to help alleviate psychological stress and reduce depression in patients [29,30]. The present study extends the application of resilience theory in the research of psychological health in breast cancer, clarifying the dual mechanisms of influence that individual and family resilience have on depressive symptoms. It emphasizes that enhancing the resilience of the individual and the family is a crucial goal of psychological interventions for patients with breast cancer.
The results of the mediation effect test in this study showed that family resilience played a partial mediating role between individual resilience and depression in patients with breast cancer, indicating that individual resilience not only directly affects depression in patients with breast cancer but also indirectly affects the degree of depression through family resilience. Meanwhile, family mental resilience exhibited a significant negative adjustment effect between individual mental resilience and depressive symptoms. This finding showed that higher family resilience enhances the protective effect of individual resilience against depression, the stronger the individual resilience, the fewer the symptoms of depression. These results emphasize that an individual’s psychological health is influenced by factors across multiple levels. As part of an individual’s social support system, the level of family resilience significantly affects the efficacy of individual resilience and, consequently, individual emotions [31,32]. Therefore, in clinical practice and psychological health interventions, attention should not only be focused on the patient’s personal treatment but also on how to enhance the resilience of the entire family. Additionally, this study found that as family resilience increased, its moderating effect on individual resilience and depression slowed down. This finding suggests that the protective effect of family resilience on depression reaches a “threshold” at higher levels, beyond which further strengthening of individual resilience has a limited effect on improving depressive moods, possibly because family support has a greater effect during an individual’s lowest emotional periods. As family support increases, its effectiveness gradually plateaus, necessitating the exploration of other factors to further alleviate depressive symptoms.
The results showed that enhancing individual resilience and family resilience is beneficial to relieve the depression of patients with breast cancer. Improving an individual’s family resilience can help enhance the effect of individual resilience on relieving depression. Clinical nursing staff should pay attention not only to the mental health of patients but also to the help from patients’ families.
This study has certain limitations. First, it was conducted in a single hospital, which has strong regional characteristics and cannot avoid the variations caused by developmental differences between different areas. Second, the data collection in this study primarily relied on questionnaire surveys, which may be affected by the respondents’ comprehension biases, the authenticity of their responses, and other subjective factors. Future research should expand the scope of the survey, increase the sample size, and consider using various data collection methods to overcome these limitations and verify the broader applicability and universality of the study results.
Family resilience plays a partial mediating and moderating role in the relationship between individual resilience and depression in patients with breast cancer. When family resistance is high and individual resilience is low, family resilience can be utilized to alleviate the negative impact of low individual resilience. It can reduce the psychological health of the patient and reduce the occurrence of depression. This study provides insights for future research on the mechanisms affecting patients with cancer and their families, suggesting the exploration of the relationships between individual and family resilience and other mental health factors, cognitive functions, or quality of life.
Acknowledgement: The authors thank research participants for their participation in this study.
Funding Statement: This study was supported by the National Natural Science Foundation of China (No. 82203171) and the Jiangsu Province Science and Technology Coordination Research Project (No. JSKXKT2023040).
Author Contributions: Conception and design: Youqi Jiang, Bing Wu and Aiji Jiang; Provision of study materials or patients: Jiahui Chen and Guangshan Jin; Collection and assembly of data: Ruyi Jin and Minhao Zhang; Data analysis and interpretation: Qin Zhou; Manuscript writing: All authors; Final approval of manuscript: All authors. All authors reviewed the results and approved the final version of the manuscript.
Availability of Data and Materials: The data will be provided upon request to the corresponding author.
Ethics Approval: The study was approved by the Ethical Committee of Jiangsu Province Cancer Hospital (No. 2023009). All participants provided informed consent in this study.
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
References
1. Chirico A, Vizza D, Valente M, Iacono ML, Campagna MR, Palombi T, et al. Assessing the fear of recurrence using the Cancer Worry Scale in a sample of Italian breast cancer survivors. Support Care Cancer. 2022;30(3):2829–37. doi:10.1007/s00520-021-06718-4. [Google Scholar] [PubMed] [CrossRef]
2. Park SY, Lim JW. Cognitive behavioral therapy for reducing fear of cancer recurrence (FCR) among breast cancer survivors: a systematic review of the literature. BMC Cancer. 2022;22(1):217. doi:10.1186/s12885-021-08909-y. [Google Scholar] [PubMed] [CrossRef]
3. Bártolo A, Santos IM, Guimarães R, Reis S, Monteiro S. Attentional bias toward reproduction-related stimuli and fertility concerns among breast cancer survivors. Behav Med. 2022;48(4):273–83. doi:10.1080/08964289.2021.1879725. [Google Scholar] [PubMed] [CrossRef]
4. International Agency for Research on Cancer. Latest global cancer data: cancer burden rises to 19.3 million new cases and 10.0 million cancer deaths in 2020. Available from: https://www.iarc.who.int/news-events/latest-global-cancer-data-cancer-burden-rises-to-19-3-million-new-cases-and-10-0-million-cancer-deaths-in-2020/. [Accessed 2021]. [Google Scholar]
5. El Masri J, Phadke S. Breast cancer epidemiology and contemporary breast cancer care: a review of the literature and clinical applications. Clin Obstet Gynecol. 2022;65(3):461–81. doi:10.1097/GRF.0000000000000721. [Google Scholar] [PubMed] [CrossRef]
6. Phoosuwan N, Lundberg PC. Psychological distress and health-related quality of life among women with breast cancer: a descriptive cross-sectional study. Support Care Cancer. 2022;30(4):3177–86. doi:10.1007/s00520-021-06763-z. [Google Scholar] [PubMed] [CrossRef]
7. Liu W, Liu J, Ma L, Chen J. Efect of mindfulness yoga on anxiety and depression in early breast cancer patients received adjuvant chemotherapy: a randomized clinical trial. J Cancer Res Clin Oncol. 2022;148(9):2549–60. doi:10.1007/s00432-022-04167-y. [Google Scholar] [PubMed] [CrossRef]
8. Yang Y, Sun H, Luo X, Li W, Yang F, Xu W, et al. Network connectivity between fear of cancer recurrence, anxiety, and depression in breast cancer patients. J Affect Disord. 2022;309:358–67. doi:10.1016/j.jad.2022.04.119. [Google Scholar] [PubMed] [CrossRef]
9. Yu S, Li W, Tang L, Fan X, Yao S, Zhang X, et al. Depression in breast cancer patients: immunopathogenesis and immunotherapy. Cancer Lett. 2022;536:215648. doi:10.1016/j.canlet.2022.215648. [Google Scholar] [PubMed] [CrossRef]
10. Simancas Fernández M, Zapata Rueda C, Galván Patrignani G, Celedón Rivero JC, Hernández Padilla J. Adaptation to the disease, resilience and optimism in woman with breast cancer. Rev Colomb Psiquiatr. 2023;52(4):280–6. [Google Scholar]
11. Ostadi-Sefidan H, Faroughi F, Fathnezhad-Kazemi A. Resilience and its related factors among women with breast cancer. Eur J Cancer Prev. 2024;33(2):129–35. [Google Scholar] [PubMed]
12. Wan X, Huang H, Peng Q, Yu NX, Zhang Y, Ding Y, et al. A meta-analysis on the relationship between posttraumatic growth and resilience in people with breast cancer. Nurs Open. 2023;10(5):2734–45. doi:10.1002/nop2.1540. [Google Scholar] [PubMed] [CrossRef]
13. Tao L, Hu X, Chen H, Xiao S, Zhang X. Factors influencing the burden on spousal caregivers of breast cancer survivors. Support Care Cancer. 2022;30(9):7789–99. doi:10.1007/s00520-022-07130-2. [Google Scholar] [PubMed] [CrossRef]
14. Tao L, Ma X, Yang Y, Hu X, Fu L, Li J. Investigating fear of cancer recurrence among female breast cancer survivors and their spouses in southwest China: a cross-sectional study. BMJ Open. 2024;14(2):e077964. doi:10.1136/bmjopen-2023-077964. [Google Scholar] [PubMed] [CrossRef]
15. Almeida S, Rodrigues da Silva D, Frasquilho D, Costa B, Sousa B, Mourinho Baptista T, et al. Cross-cultural adaptation and psychometric evaluation of the Portuguese version of the family resilience questionnaire–short form (FaRE-SF-P) in women with breast cancer. Front Psychol. 2023;13:1022399. doi:10.3389/fpsyg.2022.1022399. [Google Scholar] [PubMed] [CrossRef]
16. Tao L, Zhong T, Hu X, Fu L, Li J. Higher family and individual resilience and lower perceived stress alleviate psychological distress in female breast cancer survivors with fertility intention: a cross-sectional study. Support Care Cancer. 2023;31(7):408. doi:10.1007/s00520-023-07853-w. [Google Scholar] [PubMed] [CrossRef]
17. Li Y, Li N, Wang J, Shang Q, Zhang B, Cao M. Effects of social support, family resilience, and individual resilience on fear of cancer recurrence among persons with breast cancer: a cross-sectional study. West J Nurs Res. 2023;45(11):993–1000. doi:10.1177/01939459231200772. [Google Scholar] [PubMed] [CrossRef]
18. Liu S, Huang R, Li A, Yu S, Yao S, Xu J, et al. Effects of the CALM intervention on resilience in Chinese patients with early breast cancer: a randomized trial. J Cancer Res Clin Oncol. 2023;149(20):18005–21. doi:10.1007/s00432-023-05498-0. [Google Scholar] [PubMed] [CrossRef]
19. Chang L, Zhang S, Yan Z, Li C, Zhang Q, Li Y. Symptom burden, family resilience, and functional exercise adherence among postoperative breast cancer patients. Asia Pac J Oncol Nurs. 2022;9(11):100129. doi:10.1016/j.apjon.2022.100129. [Google Scholar] [PubMed] [CrossRef]
20. Yang Y, Qi H, Li W, Liu T, Xu W, Zhao S, et al. Predictors and trajectories of fear of cancer recurrence in Chinese breast cancer patients. J Psychosom Res. 2023;166:111177. doi:10.1016/j.jpsychores.2023.111177. [Google Scholar] [PubMed] [CrossRef]
21. Guo YQ, Ju QM, You M, Liu Y, Yusuf A, Soon LK. Depression, anxiety and stress among metastatic breast cancer patients on chemotherapy in China. BMC Nurs. 2023;22(1):33. doi:10.1186/s12912-023-01184-1. [Google Scholar] [PubMed] [CrossRef]
22. Fresno-Alba S, Denche-Zamorano Á., Pastor-Cisneros R, Pereira-Payo D, Franco-García JM, Jiménez-Castuera R. Breast cancer and physical activity: a bibliometric analysis. Front Oncol. 2023;12:1051482. doi:10.3389/fonc.2022.1051482. [Google Scholar] [PubMed] [CrossRef]
23. Álvarez-Pardo S, de Paz JA, Romero-Pérez EM, Tánori-Tapia JM, Rendón-Delcid PA, González-Bernal JJ, et al. Related factors with depression and anxiety in mastectomized women breast cancer survivors. Int J Environ Res Public Health. 2023;20(4):2881. doi:10.3390/ijerph20042881. [Google Scholar] [PubMed] [CrossRef]
24. Zhu W, Gao J, Guo J, Wang L, Li W. Anxiety, depression, and sleep quality among breast cancer patients in North China: mediating roles of hope and medical social support. Support Care Cancer. 2023;31(9):514. doi:10.1007/s00520-023-07972-4. [Google Scholar] [PubMed] [CrossRef]
25. Mete Civelek G, Akinci MG, Dalyan M. Evaluation of sleep quality, depression, and quality of life in patients with breast cancer related Lymphedema. Lymphat Res Biol. 2023;21(3):289–95. [Google Scholar] [PubMed]
26. Zhang J, Qin Z, So TH, Chang TY, Yang S, Chen H, et al. Acupuncture for chemotherapy-associated insomnia in breast cancer patients: an assessor-participant blinded, randomized, sham-controlled trial. Breast Cancer Res. 2023;25(1):49. doi:10.1186/s13058-023-01645-0. [Google Scholar] [PubMed] [CrossRef]
27. Lau WKW. The role of resilience in depression and anxiety symptoms: a three-wave cross-lagged study. Stress Health. 2022;38(4):804–12. doi:10.1002/smi.v38.4. [Google Scholar] [CrossRef]
28. Mungase M, Chaudhury S, Patil AA, Jagtap B, Jain V. Stress, anxiety, depression, and resilience in cancer patients on radiotherapy. Ind Psychiatry J. 2021;30(2):346–52. doi:10.4103/ipj.ipj_78_20. [Google Scholar] [PubMed] [CrossRef]
29. Park M, Choi EK, Lyu CJ, Han JW, Hahn SM. Family resilience factors affecting family adaptation of children with cancer: a cross-sectional study. Eur J Oncol Nurs. 2022;56:102078. doi:10.1016/j.ejon.2021.102078. [Google Scholar] [PubMed] [CrossRef]
30. Chen X, Yan Q, Tang Y, Zhu J, Zhang W, Zhang J. Financial toxicity, family resilience and negative emotions among young and middle-aged breast cancer patients: a multicentre cross-sectional study. Breast. 2024;75:103735. doi:10.1016/j.breast.2024.103735. [Google Scholar] [PubMed] [CrossRef]
31. Chen JJ, Wang QL, Li HP, Zhang T, Zhang SS, Zhou MK. Family resilience, perceived social support, and individual resilience in cancer couples: analysis using the actor-partner interdependence mediation model. Eur J Oncol Nurs. 2021;52:101932. doi:10.1016/j.ejon.2021.101932. [Google Scholar] [PubMed] [CrossRef]
32. Hu X, Wang W, Wang Y, Liu K. Fear of cancer recurrence in patients with multiple myeloma: prevalence and predictors based on a family model analysis. Psychooncology. 2021;30(2):176–84. doi:10.1002/pon.5546. [Google Scholar] [PubMed] [CrossRef]
Cite This Article
 Copyright © 2024 The Author(s). Published by Tech Science Press.
Copyright © 2024 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools