 Open Access
Open Access
ARTICLE
The Coping Styles and Perception of Illness in Patients with Breast Cancer—Relation to Body Image and Type of Surgery
1 Faculty of Medical Sciences, University of Kragujevac, Kragujevac, 34000, Serbia
2 Faculty of Sciences & Faculty of Philology and Arts, University of Kragujevac, Kragujevac, 34000, Serbia
* Corresponding Author: Darko Hinić. Email:
Psycho-Oncologie 2024, 18(3), 159-168. https://doi.org/10.32604/po.2024.050122
Received 28 January 2024; Accepted 26 March 2024; Issue published 12 September 2024
Abstract
Breast cancer is considered one of the most frequent causes of morbidity and death in women. Individuals’ response to information regarding health threats and illness can influence the adjustment of the treatment to existing conditions including the issues of non-completion of treatment or non-attendance at medical appointments. The study aimed to examine the relationship between illness perception, body image dissatisfaction and (mal)adaptive coping styles in breast cancer patients. A sample of 197 patients with diagnosed breast cancer hospitalized at the Center for Oncology and Radiology, Kragujevac, Serbia, was surveyed. The instruments included sociodemographic questionnaire, a Brief Illness Perception Questionnaire (BIPQ), a Body Image Scale (BIS), and a Mini-Mental Adjustment to Cancer Scale (Mini-MAС). Results showed that 52% of the variance of maladaptive coping style in women who underwent mastectomy was explained by the negative illness perception, while body image dissatisfaction reflected through this connection (CFI > .95, GFI > .95, RMSEA = .01, SRMR = .08). Similar results were found in patients with breast-conserving surgery but with lower percentage (36%) of variance explained (CFI > .95, GFI > .95, RMSEA < .02, SRMR < .05). If confirmed by further studies, these results would suggest that patients who underwent mastectomy tend to be more dissatisfied with their body image, have tendency to perceive illness as threatening and resort to maladaptive coping styles. However, any form of appearance modification, including breast-conserving surgery, carries the risk of body image dissatisfaction, and consequently the risk of maladaptive coping behaviors. Our results suggest that health professionals and public policies should put an additional focus on the assessment of the patient’s body image dissatisfaction, to improve the health and wellbeing of the affected women.Keywords
Breast cancer is the most frequent cancer and the second cause of death by cancer in women worldwide [1]. Every fourth woman suffering from cancer had breast cancer in 2020, while in Serbia during the same year, there were 6724 women with the same diagnosis [2].
The treatment for illnesses is increasingly dependent on patients’ capacity to regulate their own prevention/treatment regimens, so individuals’ response to information regarding health threats and illness can influence early detection of illness, adjustment of treatment to existing conditions, and the issue of non-completion of treatment or non-attendance at medical appointments [3]. Therefore, crucial questions in oncology nowadays are not only related to the treatment but also to the emotional and psychological well-being of patients [4].
The Common Sense Model suggests that patients form a system of beliefs or representations of illness, which further regulates their reactions toward illness, and treatment [5]. It is the dynamic process by which individuals perceive, interpret, and respond to illness-related information [3]. Illness perceptions are comprised of perceptions and cognitive representations of causes of illness, timeline of the illness, potential consequences of it, the degree of control over the illness, and emotional reactions to it [6]. These beliefs may influence threat responses that may lead to failure to engage in treatment-seeking behavior or actions that are ineffective in addressing the threat, such as denial or minimization of the threat [3]. There is evidence that psychological factors can have a modulating effect on the state of patients in the period after chemotherapy, e.g., results showed that psychological distress had a great impact on quality of life in the prechemotherapy period and 6 months after the completion of chemotherapy [7].
There is an ongoing debate on the stability of these beliefs. Previous studies claimed that illness perceptions are open to change and that they can be successfully altered by short interventions in chronically ill patients [6]. However, other studies conducted among people with cancer found that these perceptions are relatively stable, especially without directed intervention aimed specifically at modifying them [8].
Although the potential role of coping styles of patients suffering from cancer has been the subject of many studies, still there is no decisive evidence of its’ prediction role in cancer survival rate [9]. When dealing with various stressful situations, including illness, affected persons may show different reactions, and it was shown that the style of coping with illness, i.e., how a person tries to overcome the illness and its consequences, can significantly affect the outcome of the treatment [10]. Individuals’ coping strategies and responses to illness are guided by perception, cognitive representations of, and emotional responses to the illness. For instance, in a sample of patients with different types of cancer illness perception acted as a framework for the coping strategies [6]. In breast cancer patients a weak relationship between illness representations and coping strategies was found [11]. However, some previous research failed to confirm a mediating role of coping in the relationship between illness perceptions and psychological distress [8]. Therefore, one of the issues we will deal with in this paper is a closer examination of the relationship between coping strategies and illness perceptions.
Coping strategies for overcoming illness are usually divided into adaptive and maladaptive [12,13]. The styles of coping with an illness that is considered maladaptive are avoidance, helplessness, anxious preoccupation, fatalism, blaming others, etc., therefore this approach is considered avoidant-oriented [3,9]. The adaptive styles most frequently include active coping, perseverance, seeking social support, etc. so authors label it as approach-oriented. In line with this categorization, the research found that individuals show a better quality of life if they score higher on the fighting spirit and lower on the helpless-hopeless and anxious preoccupation subscales [12]. Also, the impact of therapy, hospitalization, and recurrence of the illness on the impairment of the quality of life is smaller if the affected woman uses more active coping styles [14]. Other studies found mixed results, with the possible influence of disease progression, the impact of therapy, hospitalization, life circumstances, etc. [13].
Coping with cancer is a long-term process, and the choice of coping strategies depends both on individual features (personality traits, perceived support) and temporal variability (the stage of the disease and its course) [15]. Coping responses are also dynamic processes since individuals monitor the effects of their responses related to illness progression or the impact of therapy. In this study, we will rely on an extended Common-sense model suggesting that the individual may opt to adapt or modify the coping procedure according to the individual’s beliefs about the accessibility, effectiveness, and costs of the selected treatment [3]. Therefore, we will examine if the (mal)adaptive strategies are connected to illness perceptions and other factors significant to patients with breast cancer, such as illness characteristics (treatment length, metastases, type of applied surgery or post-surgery treatment), socio-demographic characteristics (age, education, marital, and employment status, number of children). Authors of the model emphasize that research to date has not extensively tested potential interaction effects within the model, such as individual differences or personality traits [3]. We have not studied personality traits in our study either, however, we studied body image perception as an important factor that has not been studied a lot in the context of illness perception, but that could have a large impact on the illness response of patients with this type of cancer.
Body image perception and satisfaction
Diagnosing and treatment of breast cancer leave long-term consequences on women’s physical health and lead to various changes in their physical appearance, as it results in hair loss, the appearance of lymphedema, weight problems, scarring or the removal of one or both breasts [16–18]. This is the reason why investigating the perception of one’s physical appearance became important. Furthermore, body image perception implies the way in which people perceive their body, but also the way they experience the perception of their body image by others [18]. This image is modified by our affective and motivational mental processes, which results in an evaluation that is not always an objective assessment of one’s appearance [19]. A gap between the body image and the ideal image is associated with impaired quality of life, feelings of body incompleteness, sexual difficulties, problems in the relationship with partner and other social relations [20]. However, research indicates that some of these concerns are not addressed within the patient-physician relationship, which primarily focuses on illness treatment and recovery [20].
In breast cancer, women often undergo breast surgical treatment either through mastectomy or breast-conserving surgery (BCS), with both techniques showing similar overall survival rates [21]. These surgical treatments are related to how patients perceive their body image. In a mastectomy, the entire breast is removed, therefore, a woman experiences a permanent change in her appearance with more concerns with body image and sexual functioning [22]. However, in a BCS the location of the scar may be the reason for the dissatisfaction of a large number of patients [23]. The female patients recruited for our study underwent surgical intervention during treatment (BCS or mastectomy), which may have influenced their body image and illness perception. Therefore, body image satisfaction is one of the key constructs assessed in the study.
The aim of the study was to examine how women with breast cancer perceived their illness and their body image after the treatment, as well as to examine the potential relation and predictive power of illness perception and body image satisfaction on adaptive and maladaptive styles of coping with illness. Sociodemographic variables, characteristics and treatment of the illness were examined as control variables. The research was conducted with the goal of better understanding the factors influencing the choice of coping strategies, in particular understanding the way that body image dissatisfaction may influence these choices through illness perceptions and regarding different types of surgical interventions.
The research was conducted at the Center for Oncology and Radiology, Clinical Center in Kragujevac. Based on the inclusion (adult, female patients hospitalized with a diagnosis of breast cancer, who underwent surgical intervention, and who gave informed consent) and exclusion criteria (psychiatric disorder or other form of malignant disease), 197 female patients were invited to participate in the study during their inpatient treatment. In the study group, oncologists used criteria of the International Classification of Diseases–10 (ICD-10) [24] to conclude a diagnosis of breast cancer. The authors of the study evaluated other psychiatric and somatic comorbidities of patients based on the ICD-10 criteria using personal history and medical history records and in the final study only patients without other malignancies or psychiatric disorders were included. Since a surgical intervention was an inclusion criterion, patients were divided into two groups regarding the type of surgical intervention (breast-conserving surgery vs. mastectomy). Moreover, since a large number of changes in physical appearance was expected in patients undergoing chemotherapy, for example, an increase in body weight [25], one group included patients that underwent either chemotherapy or chemotherapy with other types of treatment, and the other group consisted of patients that received no chemotherapy.
The study was approved by the Ethical Committee of the Clinical Centre of Kragujevac (No. 01/20-659) and conducted in accordance with the Declaration of Helsinki. The goal and nature of the research was explained to the participants, who provided written informed consent. Participants completed the study measures in a single assessment session.
The sociodemographic and clinical characteristics of the study group are shown in Table 1.
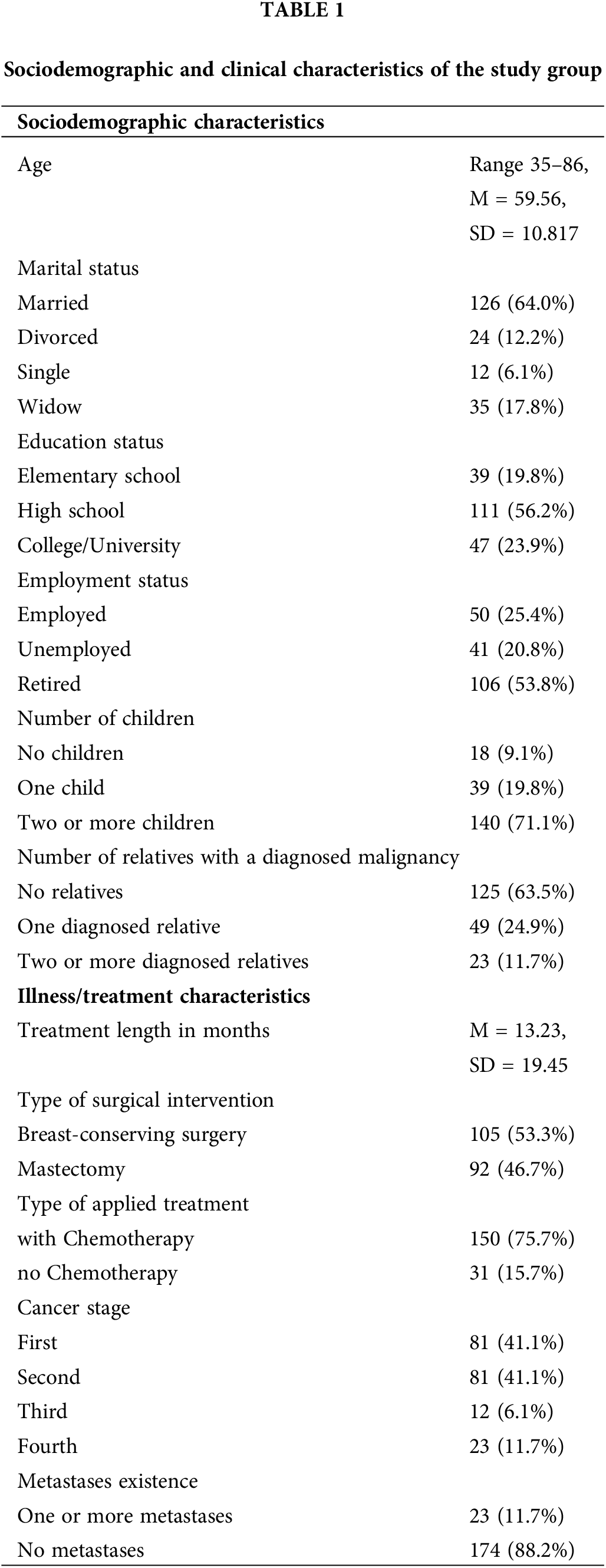
A short-structured interview and medical records were used to obtain data on socio-demographic characteristics (see Table 1), the length of treatment expressed in months, the type of surgical intervention (breast-conserving surgery vs. mastectomy), the type of postoperative treatment (chemotherapy, radiotherapy, etc.), the stage in which the illness was diagnosed, metastases and lymphedema existence.
Brief Illness Perception Questionnaire—BIPQ assesses the degree to which the illness was perceived as threatening or benign [26]. The questionnaire consists of eight items (0–10 range) regarding the consequences, length, and degree of control the examinees had over their illness, the evaluation of treatment success, emotional consequences and the points to which they understand the illness (e.g., How much do you think your treatment can help your illness?). The total score range is from 0 to 80, and a lower score indicates the perception of the illness as less threatening [26]. Previous results showed acceptable reliability of this scale, and the reliability in our research was α = .80.
The Mini-Mental Adjustment to Cancer—Mini-MAС [27], consists of 29 items assessing psychological adjustment in cancer patients on a scale of Likert’s type (1 to 4 range). The scale shows acceptable psychometric properties and convergent validity with several psychosocial outcomes (e.g., anxiety, depression, quality of life) at various stages of the illness [28]. However, the factor structure showed some inconsistency ranging from the original five to three or even two dimensions of coping with the illness. A review of the literature showed commonly used division into adaptive or constructive and maladaptive or negative styles of coping with illness [12], which we also used in our research (e.g., I try to fight the illness, or I feel completely at a loss about what to do). The original questionnaire showed acceptable reliability α = .87 which was confirmed in our study (α = .86).
The Body Image Scale—BIS is a questionnaire of 10 items that aims to examine the affective, behavioral and cognitive components of the perceived changes in the body image after applied surgical intervention, precisely the degree to which women feel discouraged and worried about the perceived physical changes [29]. The questionnaire consists of questions on a four-degree Likert’s type of scale, from 0–not at all, to 3–very much (e.g., Have you been feeling less feminine as a result of your disease or treatment?). The overall summary score ranges from 0 to 30, where higher scores represent increased body dissatisfaction or distress. The original questionnaire was validated among breast cancer patients and showed acceptable reliability of α = .93, which was confirmed in our study (α = .78).
The data were analyzed in IBM SPSS 21 using standard descriptive statistics (i.e., frequencies, percentages, mean values, standard deviation). t-test or one-way analysis of variance (ANOVA) was used for calculating differences, while the Spearman’s or Pearson’s correlation coefficients were calculated to estimate the association between measured variables. Finally, structural equation modeling analysis was used to test the prediction models (Maximum likelihood estimation procedures) in AMOS version 21.
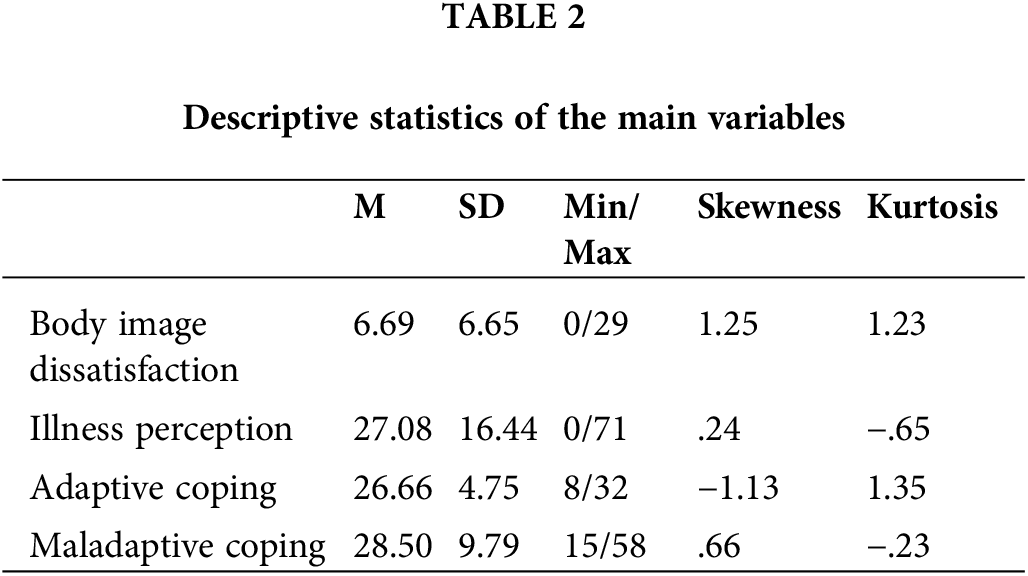
Descriptive statistics of the main variables are shown in Table 2.
Although values for Skewness and Kurtosis are between ±1, the adaptive coping scores were grouped toward higher values (see Fig. 1A), while the scores for maladaptive coping were grouped toward lower values (see Fig. 1B). The participants reported low levels of distress associated with body image changes.
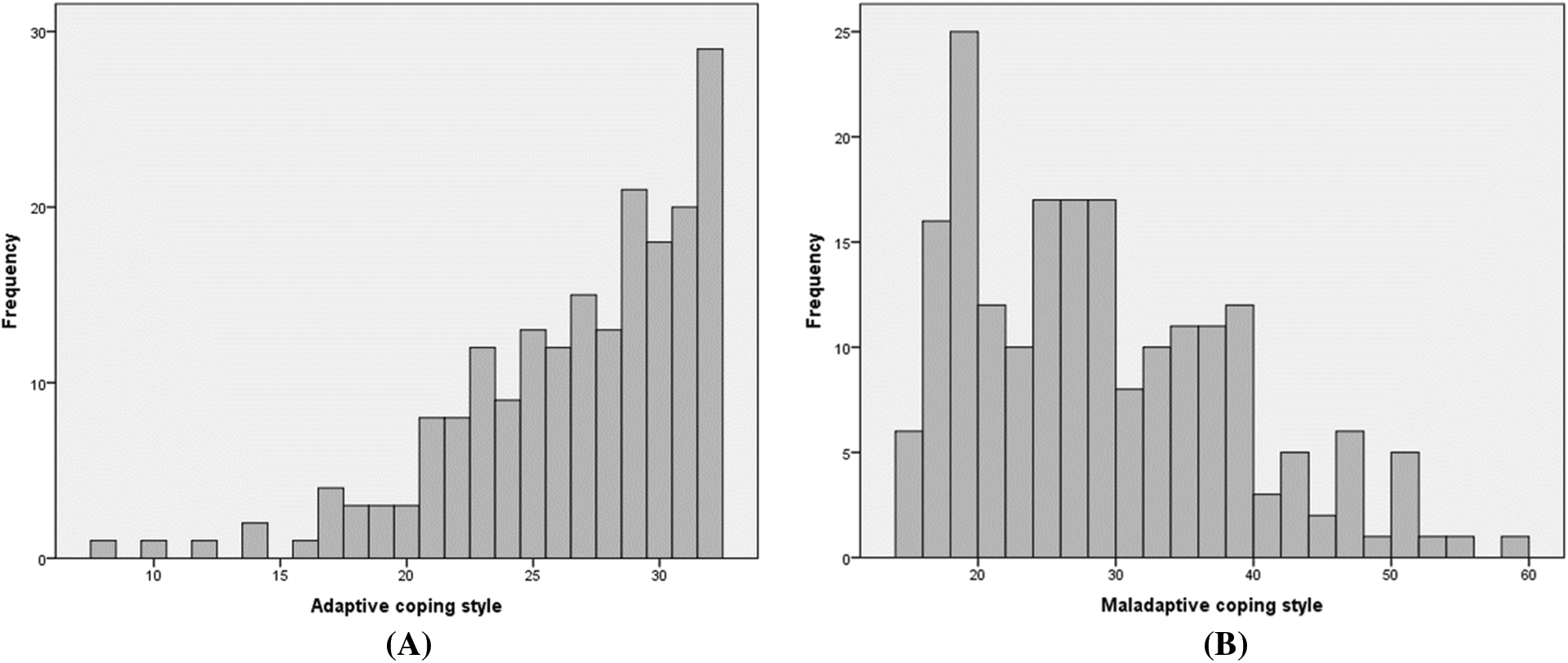
Figure 1: (A) Distribution of adaptive coping styles scores. (B) Distribution of maladaptive coping styles scores.
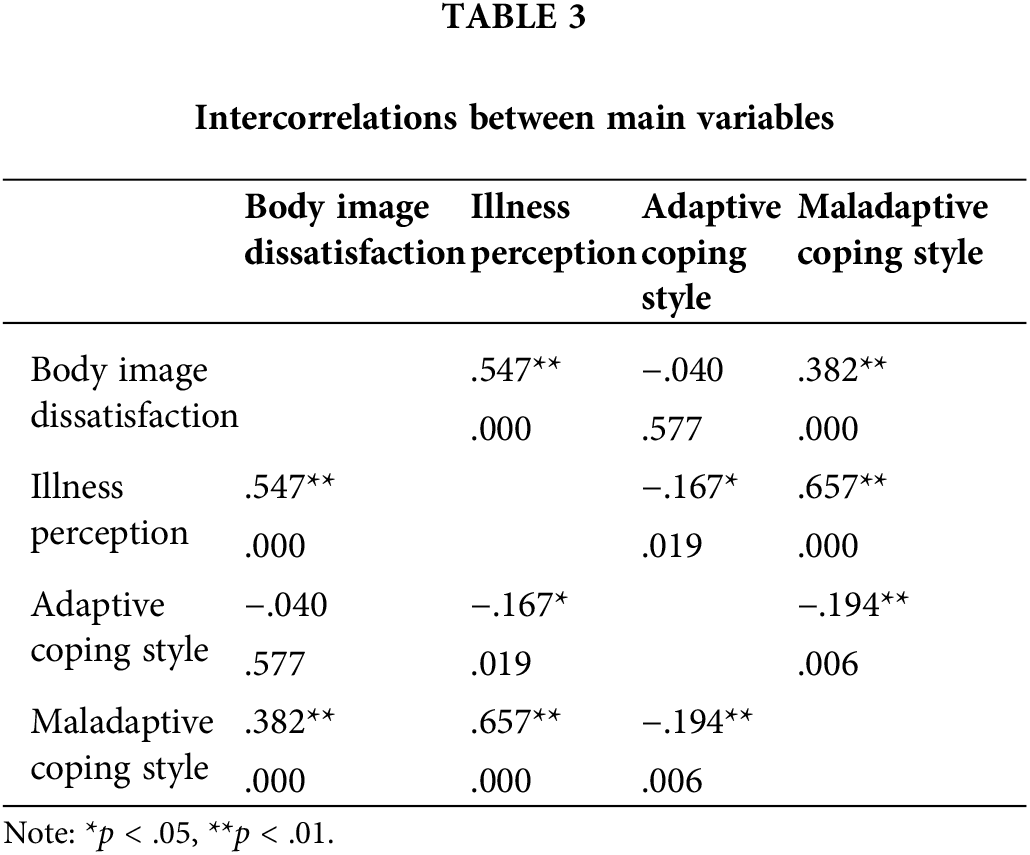
Intercorrelation matrix shows high correlations both between Illness perception and Body image dissatisfaction, and between Illness perception and Maladaptive coping style (Table 3).
Furthermore, we tested if any of control (continuous) variables showed correlation with main variables and if there were differences in control (categoric) variables. Only Length of treatment showed moderate correlation with Adaptive coping style (r = −.328, p < .01). Patients with metastases used less Adaptive strategies (t(195) = −3.011, p < .001, d = .67). Women who received chemotherapy used Maladaptive strategy more often (t(195) = 2.198, p < .05, d = .35).
Patients in the first and second illness stages and younger than 59 years of age showed more Body image dissatisfaction than patients in third and fourth illness stages (t(195) = 2.178, p = .03, d = .38), and older than 60 years of age (t(195) = 2.274, p = .02, d = .33). Patients with lymphedema perceived body image more negatively (t(195) = 2.030, p = .04, d =.34), similar to patients on chemotherapy (t(195) = 2.951, p < .01, d = .58), and patients with mastectomy (t(195) = 2.626, p < .01, d = .45).
Based on theoretical assumptions, we tested a structural model according to which Body image dissatisfaction and Illness perception were hypothesized to predict Adaptive and Maladaptive styles of coping. From other tested variables (sociodemographic, clinical/treatment data), according to the obtained significant correlations/differences with the criterion (coping styles) or predictor variables, we included the connection between Length of treatment and Metastases with the Adaptive, and Treatment type with Maladaptive coping style. Finally, with Body image dissatisfaction being in relation with Age groups, Cancer stage, Treatment type and Lymphedema, these variables were also included in the initial model (see Fig. 2A). Since we wanted to explore the importance of surgical intervention type, we tested two separate models, one in BCS group and the other in mastectomy group.
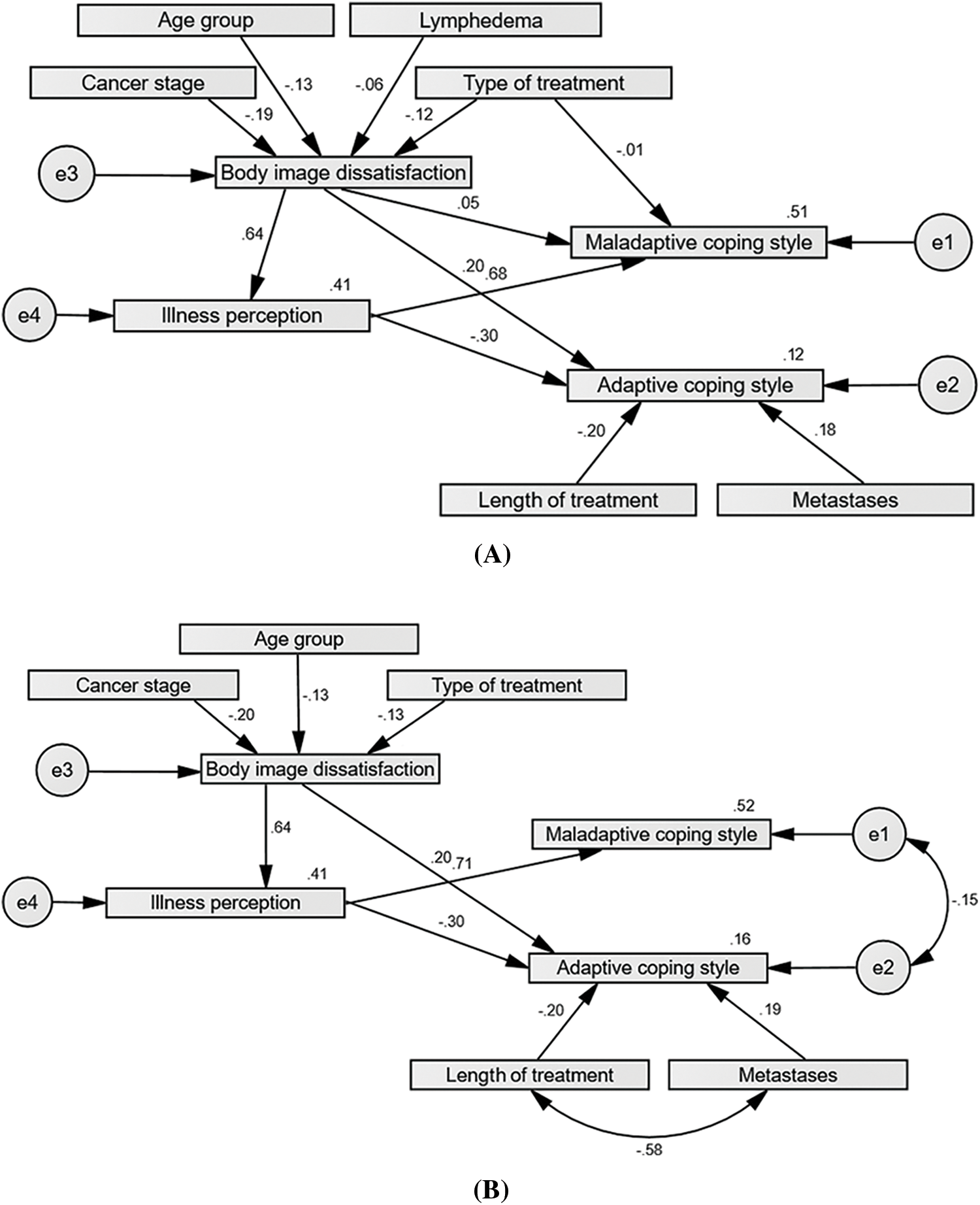
Figure 2: (A) Initial predictive model for coping styles (mastectomy group). (B) Final predictive model for coping styles (mastectomy group).
Initial analysis of Modification indices showed that in the mastectomy group Length of treatment and Metastases existence, the Type of treatment and Lymphedema, as well as coping styles residuals should be correlated (the second model in Table 4). In further analysis, some paths were not statistically significant. The type of treatment did not directly predict Maladaptive style, while Lymphedema did not significantly predict Body image dissatisfaction, therefore we excluded mentioned connections and variable Lymphedema. Moreover, Body image dissatisfaction did not add anything to the prediction of coping style values directly, so the final model included only the effect of Body image dissatisfaction on Illness perception (see Fig. 2B).
In the final model, the Maladaptive coping style was directly predicted by Illness perception, while Body image dissatisfaction had a role through Illness perception (with age, cancer stage, and chemotherapy treatment in relation to Body image). Adaptive coping style was directly predicted by Illness perception and Body image dissatisfaction, while Length of treatment and Metastases existence were seen as important control variables. This model was able to explain 52% of the Maladaptive coping style variance and 16% of the Adaptive coping style variance (see Fig. 3A).
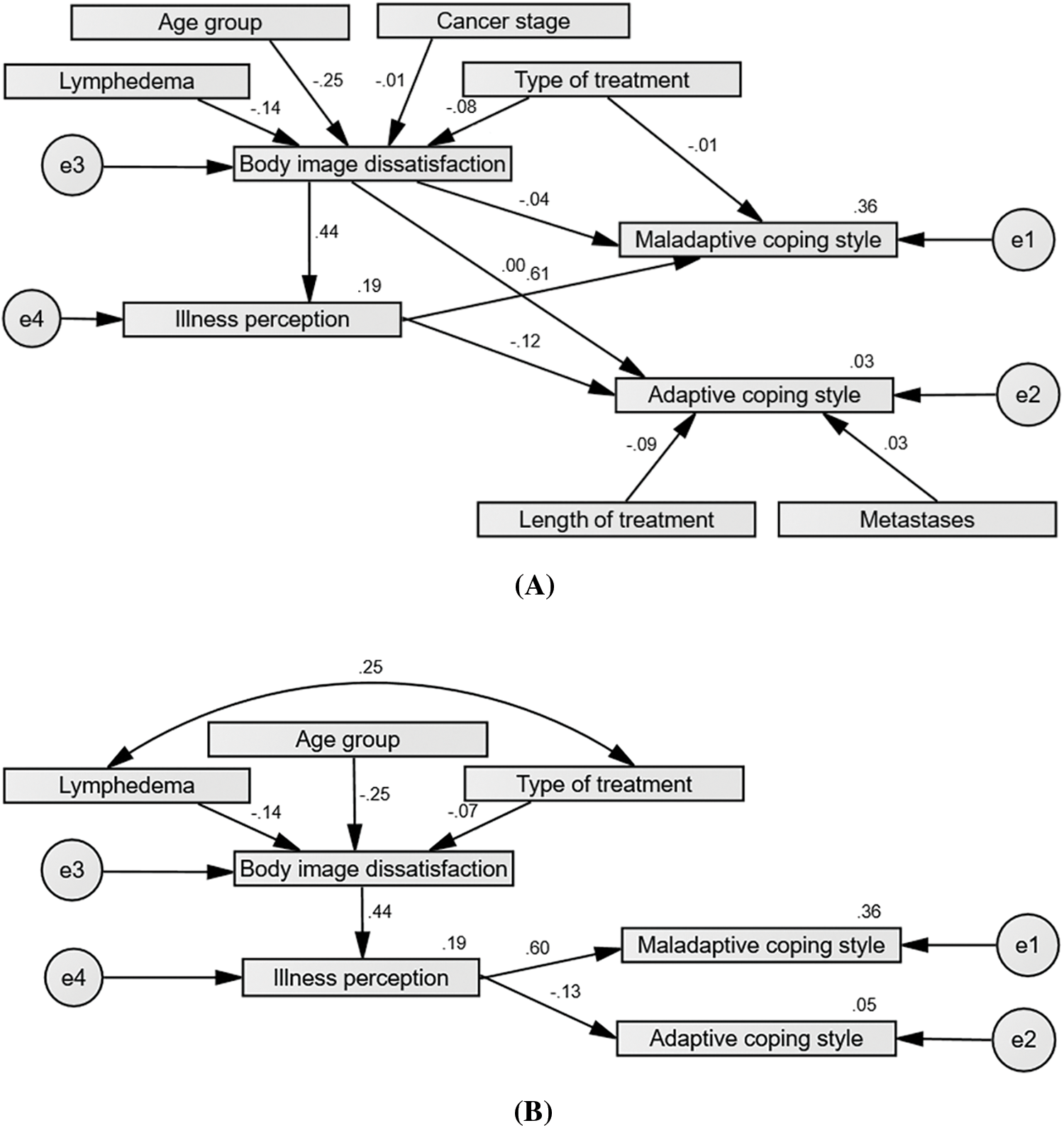
Figure 3: (A) Initial predictive model for coping styles (breast-conserving surgery group). (B) Final predictive model for coping styles (breast-conserving surgery group).
Initial analysis of Modification indices showed that in the BCS group Length of treatment and Metastases, as well as Type of treatment and Lymphedema existence should be correlated. Furthermore, Body image dissatisfaction did not predict additional values of coping styles, therefore our second model included only its effect on Illness perception, and similar results were obtained with the Type of treatment that did not directly predict Maladaptive style (Table 5).
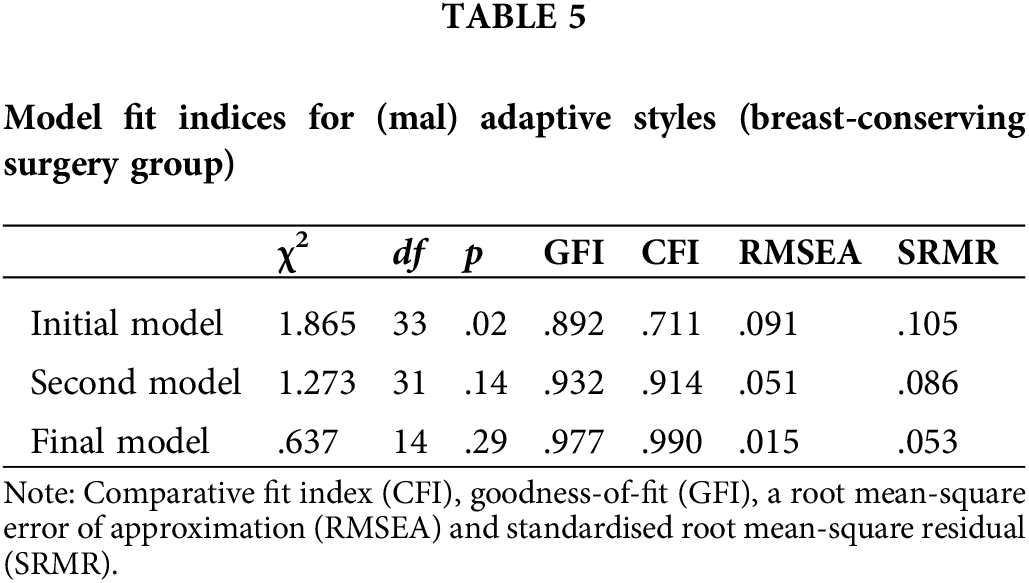
In further analysis, the Length of treatment and Metastases did not additionally contribute to the prediction of Adaptive styles nor did the Cancer stage contribute to the prediction of Body image dissatisfaction, so these variables were excluded from the final model (see Figs. 3A, 3B).
In the final model coping styles were directly predicted by Illness perception, and Body image dissatisfaction has a role through Illness perception (with age, chemotherapy treatment and lymphedema in relation to Body image). This model was able to explain 36% of the Maladaptive and only 5% of Adaptive coping style variance.
Although breast cancer is frequently linked to body image dissatisfaction, in our study women showed a lower level of dissatisfaction with their body image. On average, they use adaptive styles of coping with illness more than maladaptive ones. The data showed that women who perceive their illness as threatening tend to be more dissatisfied with their body image and that they tend to resort to maladaptive coping styles. Adaptive coping styles are used less by women whose treatment lasts a long time as well as by those with metastases. Women with illnesses diagnosed in stage 1 and 2, as well as those with lymphedema and receiving chemotherapy, show greater body image dissatisfaction.
The focus of this research was the evaluation of the predictive model according to which Body image dissatisfaction and Illness perception were hypothesized to predict Adaptive and Maladaptive styles of coping with the illness. We tested two models, one in patients with breast-conserving surgery and one with mastectomy. We also tested the potential effects of sociodemographic variables, clinical characteristics, and treatment of the illness as control variables.
Studies seem to indicate that illness threat perceptions tend to be positively related to avoidant and negatively related to adaptive coping procedures and linked to maladaptive outcomes such as higher negative emotional responses, lower quality of life, and reduced likelihood of treatment-seeking behaviour [3]. In contrast, control-related perceptions and more coherent beliefs regarding the illness are linked to approach coping behaviours, as well as better functioning, increased treatment seeking, and reduced distress. We also confirmed the results claiming that the connection between negative illness perception and maladaptive coping styles was especially strong. Other authors also stated that reactions to illness were altered through modulation of the illness perception: more avoidance induces underestimation of the threat and minimization of difficulties, whereas more anxiety induces passivity, overestimation of threat, and emphasizes the inability to cope with a threatening situation [31]. In our final models in both groups of patients, Maladaptive coping style was directly predicted by Illness perception, while Body image dissatisfaction has a role through illness perceptions (with age, chemotherapy treatment, cancer stage, or lymphedema in relation to Body image). Adaptive coping style was also predicted by Illness perception and Body image dissatisfaction, while Length of treatment and Metastases existence were important control variables. These results imply that women who evaluate their illness as more threatening show greater body image dissatisfaction too, similar to results in a recently conducted study [32].
Although the two models are similar, the prediction model explained a larger percentage of the variance of coping styles in the sample of women who underwent mastectomy. The type of surgical intervention has a great influence on the illness perception, body image, and consequently on reactions to illness. As in previous studies [22,29], women who underwent mastectomy scored significantly higher on Body image dissatisfaction than those who underwent BCS. Losing a breast can remain a source of distress over time and a source that undermines women’s body image [33]. Mastectomy was found to lead to anxiety and problems related to the experience of sexuality and femininity in previous studies too [34]. In this regard, it is necessary to pay extra attention to psychosocial interventions intended for women who have undergone mastectomy.
As stated, the results of our research showed that patients with metastases used adaptive coping mechanisms to a lesser extent. However, the direction of this relation is unknown, i.e., could the tendency to maladaptive style have influenced the deterioration of the patient’s health and occurrence of metastases, or did the metastatic changes contribute to resorting to maladaptive style? Previous research showed that some maladaptive mechanisms, such as restraint, can lead to the progression of cancer to advanced stage and metastasis [35]. It was also shown that patients whose treatment lasted longer use adaptive coping styles to a lesser extent, which may be the result of discouragement and hopelessness that occurs in these women, i.e., less use of fighting spirit as a way of coping with the illness as previous studies shown [13]. Moreover, it may be stated that patients with incurable forms employ different coping mechanisms than those with oncological conditions presenting a favorable prognosis [36].
Furthermore, we must comment on the factors in relation to body image satisfaction since this construct has an important indirect effect on coping styles through illness perception. A review of the literature shows that younger patients evaluate their body image more negatively than older women suffering from breast cancer [37]. Our results confirm these findings regardless of surgery type. The perception of body image has two components: one reflecting self-perception (how women see their bodies), and the other reflecting how they think other people see their bodies [33]. It may be possible that the second component is not that important in the latter stages of life, or there is a greater tolerance to dissatisfaction. Some authors claim that women who considered themselves older felt better equipped to manage changes in body image since they had stopped connecting their self-worth to their appearance [33]. Moreover, body image perception is more negative among working women than among housewives and retired women [38].
Patients in the first and second illness stages showed more body image dissatisfaction than patients in later stages. Given that the symptoms of the illness diagnosed in advanced stages are usually more serious, women with stage III/IV cancer are probably more focused on various somatic and psychological consequences of the illness than on their physical appearance and body image.
Patients on chemotherapy perceived body image more negatively which is expected since a large number of changes in physical appearance is related to chemotherapy [25]. Chemotherapy and comorbidity were found to be predictors of maladaptive coping even 5 years postdiagnosis [9]. Finally, a review of the literature shows that women with breast cancer who develop lymphedema show a higher degree of frustration, symptoms of depression and significantly impaired body image perception [17]. We have found similar results in the group with breast-conserving surgery. Lymphedema does not limit women only in everyday physical functioning but may create an additional feeling of discomfort while looking at the reflection in the mirror and getting dressed.
Limitations and future directions
This research was conducted using self-evaluation questionnaires. Thus, it is recommended to conduct a study where coping styles will be evaluated based on the data obtained by patients’ significant others. Also, since this is cross-sectional research, the data about predictive values are statistical and do not necessarily confirm the cause-effect relation.
The state of health of the subjects at the time of the examination was not known, so there remains the possibility that the results were affected by some current complaints (dizziness, weakness, nausea, etc.).
What would be the recommendations for future research? Our research did not include the examination of personality traits and psychosocial functioning of the affected women, which may be a task for future studies. Authors of the extended Common sense model also emphasize that research to date has not extensively tested individual differences or personality traits as mediators or predictors [3]. In some of these studies, psychological adjustment to cancer was linked to attachment tendencies, where coping skills were lower in insecure patients often resulting in nonadherence to medical treatment and lower trust in physicians [31]. A study showed that two main constructs of Type-D personality, namely social inhibition (SI) and negative affectivity (NA), were related to maladaptive coping [39]. Therefore, it is desirable to conduct research aimed at examining the relation between different personality traits and certain coping mechanisms in order to choose the appropriate psychological techniques at the very beginning of the treatment which will try to reduce the use of maladaptive coping styles.
One of the factors that can have a great influence on the tendency towards certain coping mechanisms, and thus influence the connection between coping mechanisms and dissatisfaction with body image is the perception of social support. One study showed that support from family, friends, and partners is associated with a greater fighting spirit [40], which indicates the need to conduct a study that would include measurement of the social support as a mediating factor in the connection between the variables used in our research.
Cross-cultural studies have demonstrated that cultural factors can influence patients’ reports about their health, illness, or treatment. For instance, Japanese breast cancer patients were more reluctant to report problems associated with the illness and medical treatment than Dutch patients [41]. Lower levels of reported body image dissatisfaction in our sample, regardless of all changes in physical appearance, may be the result of the stigmatization of those suffering from some form of malignancy that is still present in our culture. Due to the poor psychoeducation of the population affected individuals may encounter avoidance from others, which may lead to denying obvious changes in their physical appearance in order to additionally protect themselves. Moreover, it is important to notice that positive and negative feelings toward the body can coexist (especially when considering both appearance and functionality), and a woman may experience generally positive feelings toward her body, but at the same time, have a particular negative image of the appearance of the scars [33].
Given that perception of illness as threatening is related to avoiding some forms of treatment [42], our results suggest the need to put an additional focus on the assessment of the patient’s body image dissatisfaction, in order to improve the health and well-being of the affected women.
Regarding health care and therapeutic planning, health professionals and public policies should take into consideration the impact of surgery on the body image of the patients and possible changes in that image [21], since this is related to patients’ illness perception and therefore to coping strategies as well. In the mentioned systematic review mastectomy was a major impact factor in the body image perception and sexuality of women with breast cancer in almost half of the analysed studies [21]. Considering these results, it is advised that a psychologist be involved from the beginning of the treatment and perform adequate psychological preparation of patients for all possible physical and psychological changes that the disease brings with it. If there is impaired sexual functioning, as a result of dissatisfaction with physical appearance, it is advisable to start couples counselling and involve the partner in the process of healing to help the woman accept herself and her body. At every stage of treatment, it is necessary to encourage women to focus on their strengths and use their healthy resources. Whenever there is a possibility, it is desirable to offer women reconstructive breast surgery to reduce the potential distortion of their physical appearance image. Finally, women who show certain personality characteristics and a tendency to apply adaptive coping mechanisms can organize self-support groups with psychologists and help other, more vulnerable women.
Acknowledgement: None.
Funding Statement: The authors received no specific funding for this study.
Author Contributions: The authors confirm contribution to the paper as follows: study conception and design: N. Stojadinović, D. Hinić, G. Mihajlović, M. Spasić; data collection: N. Stojadinović, M. Spasić; analysis and interpretation of results: N. Stojadinović, D. Hinić, M. Mladenović; draft manuscript preparation: N. Stojadinović, D. Hinić. All authors reviewed the results and approved the final version of the manuscript.
Availability of Data and Materials: Since data may include some confidential information, it cannot be released due to ethical and privacy considerations of patients involved in the study.
Ethics Approval: The study was approved by the Ethical Committee of the Clinical Centre of Kragujevac (No. 01/20-659) and conducted in accordance with the Declaration of Helsinki. The goal and nature of the research was explained to the participants, who provided written informed consent. Participants completed the study measures in a single assessment session.
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
References
1. Burguin A, Diorio C, Durocher F. Breast cancer treatments: updates and new challenges. J Pers Med. 2021;11(8):808. doi:10.3390/jpm11080808. [Google Scholar] [PubMed] [CrossRef]
2. Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–49. doi:10.3322/caac.21660. [Google Scholar] [PubMed] [CrossRef]
3. Hagger MS, Orbell S. The common sense model of illness self-regulation: a conceptual review and proposed extended model. Health Psychol Rev. 2022;16(3):347–77. doi:10.1080/17437199.2021.1878050. [Google Scholar] [PubMed] [CrossRef]
4. Novakov I, Popović Petrović S, Ilinčić Zlatar S, Tatić M, Ševo M. What contributes the most to the breast cancer patients’ quality of life during therapy: clinical factors, functional and affective state, or social support?. Vojnosanit Pregl. 2021;78(4):445–55. doi:10.2298/VSP190501024N. [Google Scholar] [CrossRef]
5. Leventhal H, Nerenz DR, Steele DJ. Illness representations and coping with health threats. In: Baum A, Taylor SE, Singer JE, editors. Handbook of psychology and health. Oxfordshire, UK: Routledge; 2020. p. 219–52. [Google Scholar]
6. Hopman P, Rijken M. Illness perceptions of cancer patients: relationships with illness characteristics and coping. Psycho-Oncol. 2015;24(1):11–8. doi:10.1002/pon.3591. [Google Scholar] [PubMed] [CrossRef]
7. Oh PJ, Cho JR. Changes in fatigue, psychological distress, and quality of life after chemotherapy in women with breast cancer: a prospective study. Cancer Nurs. 2020;43(1):E54–60. doi:10.1097/NCC.0000000000000689. [Google Scholar] [PubMed] [CrossRef]
8. McCorry NK, Dempster M, Quinn J, Hogg A, Newell J, Moore M, et al. Illness perception clusters at diagnosis predict psychological distress among women with breast cancer at 6 months post diagnosis. Psycho-Oncol. 2013;22(3):692–8. doi:10.1002/pon.3054. [Google Scholar] [PubMed] [CrossRef]
9. Schou-Bredal I, Ekeberg Ø, Kåresen R. Variability and stability of coping styles among breast cancer survivors: a prospective study. Psychooncol. 2021;30(3):369–77. doi:10.1002/pon.5587. [Google Scholar] [PubMed] [CrossRef]
10. Khalili N, Farajzadegan Z, Mokarian F, Bahrami F. Coping strategies, quality of life and pain in women with breast cancer. Iran J Nurs Midwifery Res. 2013;18(2):105–11. [Google Scholar] [PubMed]
11. Rozema H, Völlink T, Lechner L. The role of illness representations in coping and health of patients treated for breast cancer. Psychooncol. 2009;18(8):849–57. doi:10.1002/pon.1488. [Google Scholar] [PubMed] [CrossRef]
12. Cho YU, Lee BG, Kim SH. Coping style at diagnosis and its association with subsequent health-related quality of life in women with breast cancer: a 3-year follow-up study. Eur J Oncol Nurs. 2020;45:101726. doi:10.1016/j.ejon.2020.101726. [Google Scholar] [PubMed] [CrossRef]
13. Igrutinović N, Hinić D, Mihajlović G, Spasić M, Dodić S. Hopelessness and fighting spirit relation with illness perception in female breast cancer patients. Psicooncol. 2022;19:215–28. doi:10.5209/psic.84036. [Google Scholar] [CrossRef]
14. Ahadzadeh AS, Sharif SP. Uncertainty and quality of life in women with breast cancer: moderating role of coping styles. Cancer Nurs. 2018;41(6):484–90. doi:10.1097/NCC.0000000000000552. [Google Scholar] [PubMed] [CrossRef]
15. Ragala MEA, El Hilaly J, Amaadour L, Omari M, Asril AEL, Atassi M, et al. Validation of mini-mental adjustment to cancer scale in a Moroccan sample of breast cancer women. BMC Cancer. 2021;21(1):1042. doi:10.1186/s12885-021-08755-y. [Google Scholar] [PubMed] [CrossRef]
16. Lovelace DL, McDaniel LR, Golden D. Long-term effects of breast cancer surgery, treatment, and survivor care. J Midwifery Women’s Health. 2019;64(6):713–24. doi:10.1111/jmwh.13012. [Google Scholar] [PubMed] [CrossRef]
17. Eaton LH, Narkthong N, Hulett JM. Psychosocial issues associated with breast cancer-related lymphedema: a literature review. Curr Breast Cancer Rep. 2020;12(4):216–24. doi:10.1007/s12609-020-00376-x. [Google Scholar] [PubMed] [CrossRef]
18. Davis C, Tami P, Ramsay D, Melanson L, MacLean L, Nersesian S, et al. Body image in older breast cancer survivors: a systematic review. Psycho-Oncol. 2020;29(5):823–32. doi:10.1002/pon.5359. [Google Scholar] [PubMed] [CrossRef]
19. Stolić M, Ignjatović-Ristić D, Jović M, Jeremić J, Hinić D, Jovanović M, et al. Body image dissatisfaction, temperament traits, and self-esteem in patients with multiple minimally invasive cosmetic procedures. Srp Arh Celok Lek. 2019;147(1–2):61–6. doi:10.18848/2156-8960/CGP/v08i03/21-29. [Google Scholar] [CrossRef]
20. Joseph E, Beranek M. The psychosocial impact of mastectomies on body image in women with breast cancer. Int J Health Wellness Soc. 2018;8(3):21–9. [Google Scholar]
21. Martins Faria B, Martins Rodrigues I, Verri Marquez L, da Silva Pires U, Vilges de Oliveira S. The impact of mastectomy on body image and sexuality in women with breast cancer: a systematic review. Psicooncología. 2021;18:91–115. doi:10.5209/psic.74534. [Google Scholar] [CrossRef]
22. Moreira H, Silva S, Marques A, Canavarro MC. The Portuguese version of the body image scale (BIS)—psychometric properties in a sample of breast cancer patients. Eur J Oncol Nurs. 2010;14(2):111–18. doi:10.1016/j.ejon.2009.09.007. [Google Scholar] [PubMed] [CrossRef]
23. Gass J, Mitchell S, Hanna M. How do breast cancer surgery scars impact survivorship? Findings from a nationwide survey in the United States. BMC Cancer. 2019;19(1):342. doi:10.1186/s12885-019-5553-0. [Google Scholar] [PubMed] [CrossRef]
24. World Health Organization. The ICD-10 classification of mental and behavioural disorders: clinical descriptions and diagnostic guidelines. Geneva: World Health Organization; 1992. [Google Scholar]
25. de Kruif AJ, Westerman MJ, Winkels RM, Koster MS, van Der Staaij IM, van den Berg MM, et al. Exploring changes in dietary intake, physical activity and body weight during chemotherapy in women with breast cancer: a mixed-methods study. J Hum Nutr Diet. 2021;34(3):550–61. doi:10.1111/jhn.12843. [Google Scholar] [PubMed] [CrossRef]
26. Broadbent E, Petrie KJ, Main J, Weinman J. The brief illness perception questionnaire. J Psychosom Res. 2006;60(6):631–7. doi:10.1016/j.jpsychores.2005.10.020. [Google Scholar] [PubMed] [CrossRef]
27. Watson M, Law M, Santos M, Greer S, Baruch J, Bliss J. The mini-MAC: further development of the mental adjustment to cancer scale. J Psychosoc Oncol. 1994;12(3):33–46. doi:10.1300/J077V12N03_03. [Google Scholar] [CrossRef]
28. Hulbert-Williams NJ, Hulbert-Williams L, Morrison V, Neal RD, Wilkinson C. The mini-mental adjustment to cancer scale: re-analysis of its psychometric properties in a sample of 160 mixed cancer patients. Psycho-Oncol. 2012;21(7):792–7. doi:10.1002/pon.1994. [Google Scholar] [PubMed] [CrossRef]
29. Hopwood P, Fletcher I, Lee A, Al Ghazal S. A body image scale for use with cancer patients. Eur J Cancer. 2001;37(2):189–97. doi:10.1016/s0959-8049(00)00353-1. [Google Scholar] [PubMed] [CrossRef]
30. Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Model. 1999;6(1):1–55. doi:10.1080/10705519909540118. [Google Scholar] [CrossRef]
31. Favez N, Cairo Notari S. Body image, sexual activity, and side effects of treatments across the first year after surgery in women facing breast cancer: the influence of attachment insecurity. J Psychosoc Oncol. 2021;39(6):749–64. doi:10.1080/07347332.2021.1890306. [Google Scholar] [PubMed] [CrossRef]
32. Liu Y, Liu W, Ma Y, Yang X, Zhou H, Zhang T, et al. Research on body image cognition, social support and illness perception in breast cancer patients with different surgical methods. Front Psychol. 2022;13:931679. doi:10.3389/fpsyg.2022.931679. [Google Scholar] [PubMed] [CrossRef]
33. Brunet J, Price J, Harris C. Body image in women diagnosed with breast cancer: a grounded theory study. Body Image. 2022;41:417–31. [Google Scholar] [PubMed]
34. Zhang N, Fielding R, Soong I, Chan KK, Tsang J, Lee V, et al. Illness perceptions among cancer survivors. Support Care Cancer. 2016;24(3):1295–304. doi:10.1007/s00520-015-2914-3. [Google Scholar] [PubMed] [CrossRef]
35. Reiche EM, Nunes SO, Morimoto HK. Stress, depression, the immune system, and cancer. Lancet Oncol. 2004;5(10):617–25. doi:10.1016/S1470-2045(04)01597-9. [Google Scholar] [PubMed] [CrossRef]
36. Nipp RD, El-Jawahri A, Fishbein JN, Eusebio J, Stagl JM, Gallagher ER, et al. The relationship between coping strategies, quality of life, and mood in patients with incurable cancer. Cancer. 2016;122(13):2110–6. doi:10.1002/cncr.30025. [Google Scholar] [PubMed] [CrossRef]
37. Paterson CL, Lengacher CA, Donovan KA, Kip KE, Tofthagen CS. Body image in younger breast cancer survivors: a systematic review. Cancer Nurs. 2016;39(1):39–58. doi:10.1097/NCC.0000000000000251. [Google Scholar] [PubMed] [CrossRef]
38. Chang O, Choi EK, Kim IR, Nam SJ, Lee JE, Lee SK, et al. Association between socioeconomic status and altered appearance distress, body image, and quality of life among breast cancer patients. Asian Pac J Cancer Prev. 2014;15(20):8607–12. doi:10.7314/apjcp.2014.15.20.8607. [Google Scholar] [PubMed] [CrossRef]
39. Grassi L, Caruso R, Murri MB, Fielding R, Lam W, Sabato S, et al. Association between Type-D personality and affective (anxiety, depression, post-traumatic stress) symptoms and maladaptive coping in breast cancer patients: a longitudinal study. Clin Pract Epidemiol Ment Health. 2021;17(1):271–9. doi:10.2174/1745017902117010271. [Google Scholar] [PubMed] [CrossRef]
40. Calderon C, Gomez D, Carmona-Bayonas A, Hernandez R, Ghanem I, Gil Raga M, et al. Social support, coping strategies and sociodemographic factors in women with breast cancer. Clin Transl Oncol. 2021;23(9):1955–60. doi:10.1007/s12094-021-02592-y. [Google Scholar] [PubMed] [CrossRef]
41. Lugtenberg RT, Kaptein A, Matsuda A, Inoue K, Murray M, Kobayashi K, et al. Perceptions of Japanese and Dutch women with early breast cancer about monitoring their quality of life. J Psychosoc Oncol. 2022;40(4):527–40. doi:10.1080/07347332.2021.1936741. [Google Scholar] [PubMed] [CrossRef]
42. Iskandarsyah A, de Klerk C, Suardi DR, Sadarjoen SS, Passchier J. Consulting a traditional healer and negative illness perceptions are associated with non-adherence to treatment in Indonesian women with breast cancer. Psycho–Oncology. 2014;23(10):1118–24. doi:10.1002/pon.3534. [Google Scholar] [PubMed] [CrossRef]
Cite This Article
 Copyright © 2024 The Author(s). Published by Tech Science Press.
Copyright © 2024 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper View Full Text
View Full Text Download PDF
Download PDF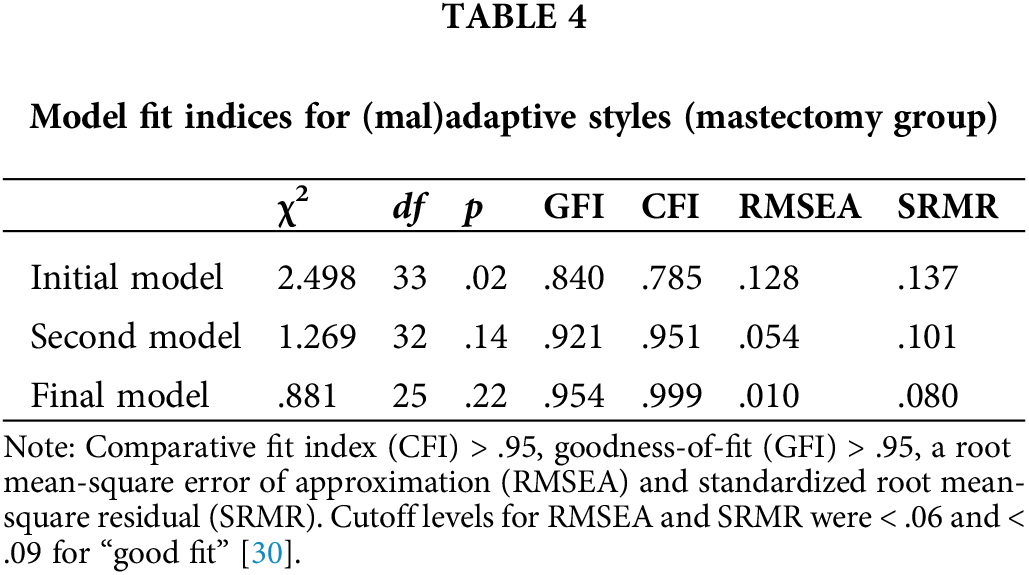
 Downloads
Downloads
 Citation Tools
Citation Tools