 Open Access
Open Access
REVIEW
Fear of Cancer Recurrence in Women with Gynecological Cancer: A Systematic Review
1 Afyonkarahisar Health Sciences University, Atatürk Health Services Vocational School, Patient Care, Afyonkarahisar, 03030, Turkey
2 Faculty of Nursing, Akdeniz University, Antalya, 07000, Turkey
* Corresponding Author: Öznur Körükcü. Email:
Psycho-Oncologie 2024, 18(3), 147-158. https://doi.org/10.32604/po.2024.046627
Received 09 October 2023; Accepted 18 February 2024; Issue published 12 September 2024
Abstract
Although some types of gynecological cancer have a poor prognosis and high recurrence rate, less is known about the fear of cancer recurrence (FCR) in gynecological cancer patients than in other cancer populations. Psychosocial problems may be experienced more in gender-specific cancers. In order to prevent future health problems related to FCR, it is critical to identify the factors affecting FCR in different subgroups and to develop various interventions. The aim of this study was to review the literature on the factors affecting the FCR in women diagnosed with gynecological cancer and interventions to reduce the FCR. The protocol of this review was registered with PROSPERO (Registration number: CRD42023452570). A total of 18 studies from 10 different countries were included in the systematic review by searching on the PubMed, ScienceDirect, Ovid, Sage, Scopus, Taylor & Francis, Web of Science, CINAHL Complete, and Cochrane databases were searched in English between July-August 2023 without year limitation to identify studies on FCR in women with gynecological cancer. Data from eligible articles were extracted and appraised for quality by two independent reviewers. In addition, bibliometric analysis method was used to visually map the studies on FCR in women with gynecological cancer according to the most frequently repeated keyword, number of citations, most cited author and publication year. The findings of the study are categorized and interpreted under two headings, “Interventions affecting FCR” and “Factors influencing FCR”. Sociodemographic characteristics such as age, economic status, social support, family history of cancer, psychological characteristics, quality of life and symptoms affect FCR. Deterioration in mental health and emotional weakness predict higher FCR, increase in positive emotional expression reduces FCR. The negative effects of cancer on sexuality and relationships, concerns about future treatments and emotional problems, and anxiety about not being able to fulfill their roles at home/work are the underlying reasons for the FCR. Therefore, professional psychosocial support should be provided to cancer survivors. Further studies are needed to identify the factors that trigger FCR and to plan interventions accordingly. This study is expected to encourage health professionals to plan interventions and research for gynecological cancer survivors.Keywords
Supplementary Material
Supplementary Material FileGynecological cancer includes malignancies occurring in the female reproductive system and is the type of cancer with the highest morbidity and mortality after breast cancer in women [1]. Unlike other organ cancers, gynecological cancers, which include malignant tumors of the vulva, vagina, cervix, uterus, ovaries and fallopian tubes, cause changes in the perception of sexual identity and sexuality, the inability to talk openly and share feelings during diagnosis and treatment, embarrassment, failure to ensure the continuity of reproduction, and some psychosexual problems [2,3].
Cancer diagnosis, advanced cancer, diagnosis at a young age, interpersonal stressors, and physical changes related to cancer treatment affect mental health and quality of life and pave the way for anxiety and depression [4]. In addition, a common source of anxiety seen in most patients is the FCR [5].
Fear, which is a subjective experience, is a basic emotion that emerges when a threat is perceived, and has a multidimensional structure characterized by cognitive, biological, emotional, and behavioral factors [6]. While cancer recurrence is defined as the recurrence of cancer after completing treatment, there is no universal definition of the FCR, but it is generally defined as the fear that the cancer will reappear in the same place or in a different part of the body, will progress, or will be diagnosed as a different cancer [7]. It is normal to experience some degree of FCR [8]. Transient or low-level FCR may be adaptive, alerting the patient to signs of new or recurrent cancer, and encouraging positive health behaviors, but persistent and excessive fear has negative psychosocial effects [9].
Various systematic reviews and meta-analyses have identified potential risk factors for FCR. These include younger age, female gender, a greater number of physical symptoms, lower income, and lower education level. All of these factors are significantly associated with a higher incidence of FCR [10–12]. Regarding the prevalence of FCR, a systematic literature review reported that 49% of cancer survivors experienced “moderate-to-high” levels of FCR [13]. High levels of FCR are difficult to manage, and the FCR tends to increase over time, leading to anxiety and depression [7]. Approximately 80% of patients diagnosed with ovarian epithelial cancer will relapse after standard first-line treatment and endometrial cancer recurrence reach as high as 50% in advanced stages or in patients with aggressive histologic condition [14,15].
FCR is becoming an increasing problem in people with different types of cancer and in various populations, including vulnerable groups [10]. In order to prevent future health problems related to FCR, it is necessary to know the prevalence and causes of FCR for the general cancer population and different subgroups. Thus, the burden of FCR in different groups can be predicted and interventions can be planned for those in need. Most research on FCR focuses on breast cancer patients and the type of surgery, and the degree of FCR may vary according to the type of cancer [13]. Although some types of gynecological cancer have a poor prognosis and high recurrence rate, less is known about the FCR in gynecological cancer patients than in other cancer populations [16]. Gender-specific cancers, such as breast and genital tract cancers, can lead to additional mental health problems. Women may experience more FCR than men [12]. This study aims to examine the factors that influence FCR and planned interventions in women with gynecological cancer or survivors of gynecological cancer.
The aims and research questions of this study include:
(1) What are the factors affecting the level of FCR in women with gynecological cancer or a history of gynecological cancer?
(2) What are the interventions to reduce the FCR in women with gynecological cancer or a history of gynecological cancer?
The systematic review was carried out in accordance with the PRISMA guidelines (Suppl. Table S1) by retrospectively scanning the research articles on the subject [17]. Key terms are “gynecologic cancer” OR “ovarian cancer” OR “endometrial cancer” OR “cervical cancer” OR “gynecologic neoplasm” AND “fear of cancer recurrence (FCR)” OR “fear of cancer relapse” OR “fear of recurrence” in various combinations. The PubMed, ScienceDirect, Ovid, Sage, Scopus, Taylor & Francis, Web of Science, CINAHL Complete, and Cochrane electronic databases were searched in English between July-August 2023 without year limitation. The protocol was registered at PROSPERO under number CRD42023452570.
After the duplicate records were removed using the EndNote 20.4 program, 1130 results were scanned according to the title and abstract, and after the irrelevant studies were excluded, the remaining 64 studies were examined according to the inclusion and exclusion criteria. A total of 18 studies were reviewed, the main theme or one theme of which was the FCR of gynecological cancers. The details of article selection are shown in Fig. 1.
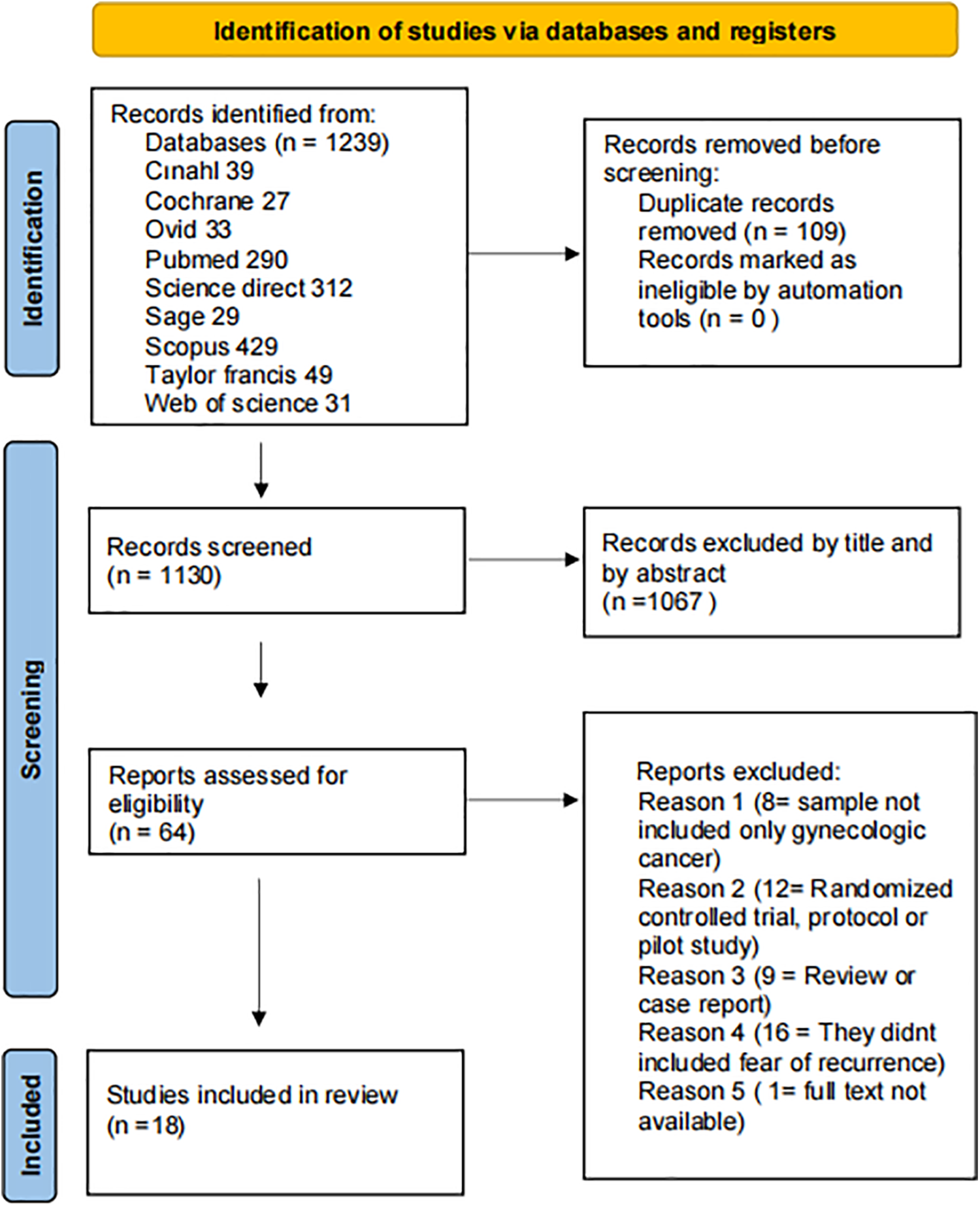
Figure 1: Selection process of the study.
Bibliometric analysis method was used to visual mapping studies on FCR in women with gynecological cancer by most frequently repeated keyword, number of citations, most cited author, and year of publication. Web of Science database and VOSviewer (version 1.6.18) was used to analyze. The information for the documents that meet the requirements contained source, title, author, keywords, document type, abstract and counts of citation, publication year which were exported into Excel format. The date of the retrieval was 27th Nov 2023.
Determining the research questions and keywords [18,19]:
P: Those diagnosed with gynecological cancer (endometrium, ovary, cervix, fallopian tube) or survivors of gynecological cancer
I: Interventions to identify or reduce factors affecting FCR
C: Standard or conventional treatment group
O: Factors affecting FCR
S: Randomized controlled, quasi-experimental, cross-sectional, qualitative, and descriptive studies.
Inclusion criteria:
The sample consisted of women with gynecological cancer or a history of gynecological cancer.
One of the main themes is the evaluation of the FCR.
Exclusion criteria:
Review studies, feasibility studies, study protocols, unpublished thesis studies, conference abstracts, articles for which the original text is not available, studies that are not in the English language, and studies that do not include FCR recurrence in gynecological cancer patients were excluded from the scope of the review. Whether the studies met the inclusion criteria was determined by a review of the records by two independent reviewers. The full-text reviews of the articles that were determined to be suitable were made by the research team.
The first and second authors independently identified studies that met the inclusion criteria for systematic review. After the title, abstract, and full text were examined in detail, the studies to be included were determined by both authors by comparing the studies When differences of opinion occurred about any study, consensus was achieved through discussion.
The data extraction instrument devised by the researchers can be seen in Table 1. The data extracted from each relevant article included the authors, publication year, study population, number of participants, type of research, and data collection/measurement tool. To reduce the possible risk of bias in our study, the literature scan, and article selection were carried out independently by the first and second authors.
Methodological quality assessment of the studies
The articles included in this systematic review were assessed for their methodological quality by the primary investigator and checked by the secondary investigator. The JIB Critical Appraisal Checklist for Randomized Controlled Trials, Analytical Cross-sectional, Quasi-Experimental Studies, and Qualitative Studies published by the Joanna Briggs Institute was used in the quality assessment [19]. This control lists 13 items for randomized controlled trials, 8 items for cross-sectional studies, 9 items for quasi-experimental studies, and 10 items for qualitative studies each item is evaluated as yes, no, unclear, and not applicable. The methodological quality evaluation of the studies is given in Table 1. Quality evaluation results of the articles can be obtained from the first author upon request.
In this study, 18 articles were examined. The findings obtained from the studies are presented by grouping them under the headings of “Author, year and country”, “type of research”, “aim”, “sample”, “data collection/measurement tool”, “results” and “quality score” (Table 1).
When the studies that met the inclusion criteria were examined, there were 18 studies in total, including 2 randomized controlled, 1 quasi-experimental, 7 cross-sectional, and 8 qualitative studies. Studies were conducted in various countries such as Denmark, the USA, Canada, Thailand, Indonesia, Taiwan, Turkey, Israel, China, and Australia. When the reporting qualities of the randomized controlled studies were evaluated over 13 points, the mean score was found as 9 (range, 8–10); the quasi-experimental study was evaluated over 9 points, the quality score was found as 7; cross-sectional studies were evaluated over 8 points, the mean score was found as 5,8 (range, 4–8) and qualitative studies were evaluated over 10 points, the mean score was found as 8,5 (range, 7–10).
When the included studies were visualized with the bibliometric analysis method, it was seen that the most repeated keyword was “fear of cancer recurrence”, the most cited study was Myers et al. [16], and the most cited author was Sharon Manne (Figs. 2–4).
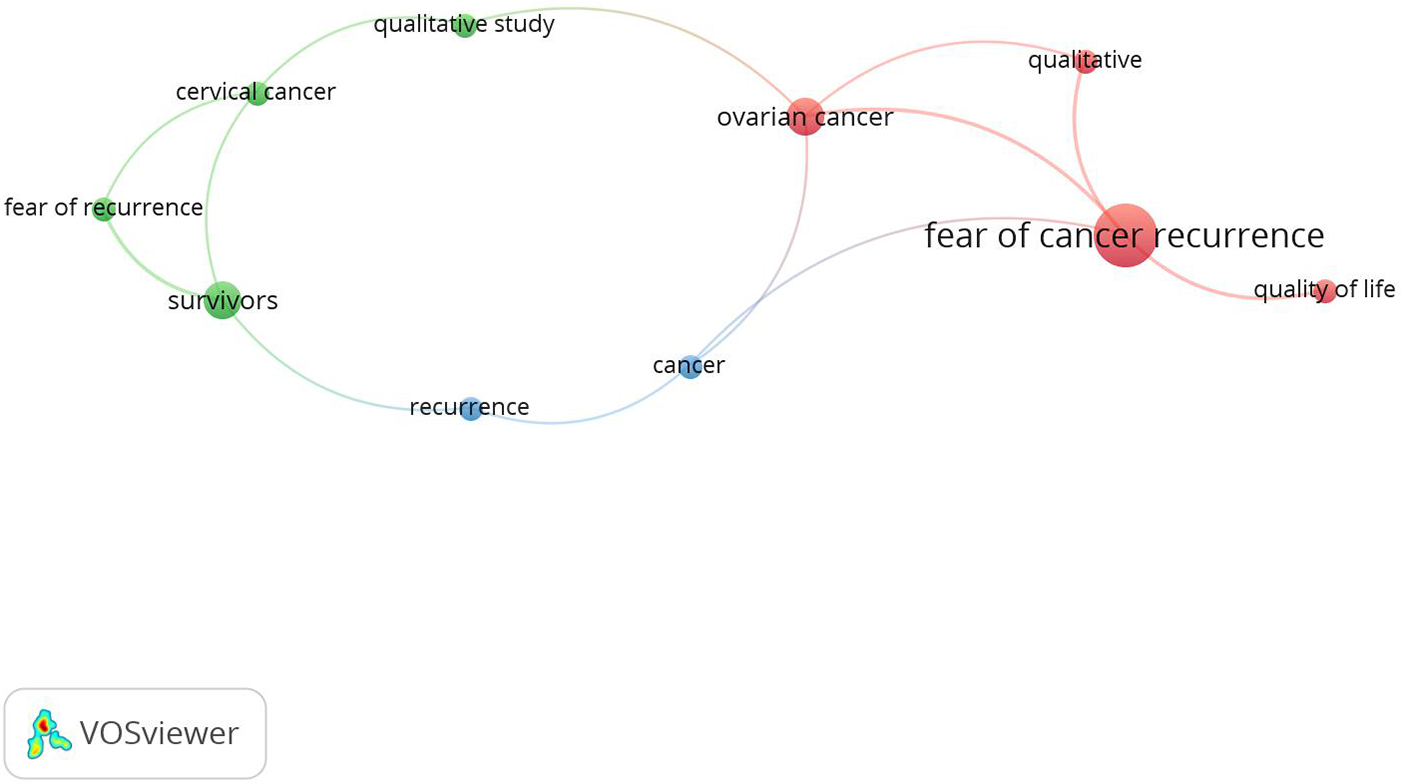
Figure 2: Most frequently repeated keyword.
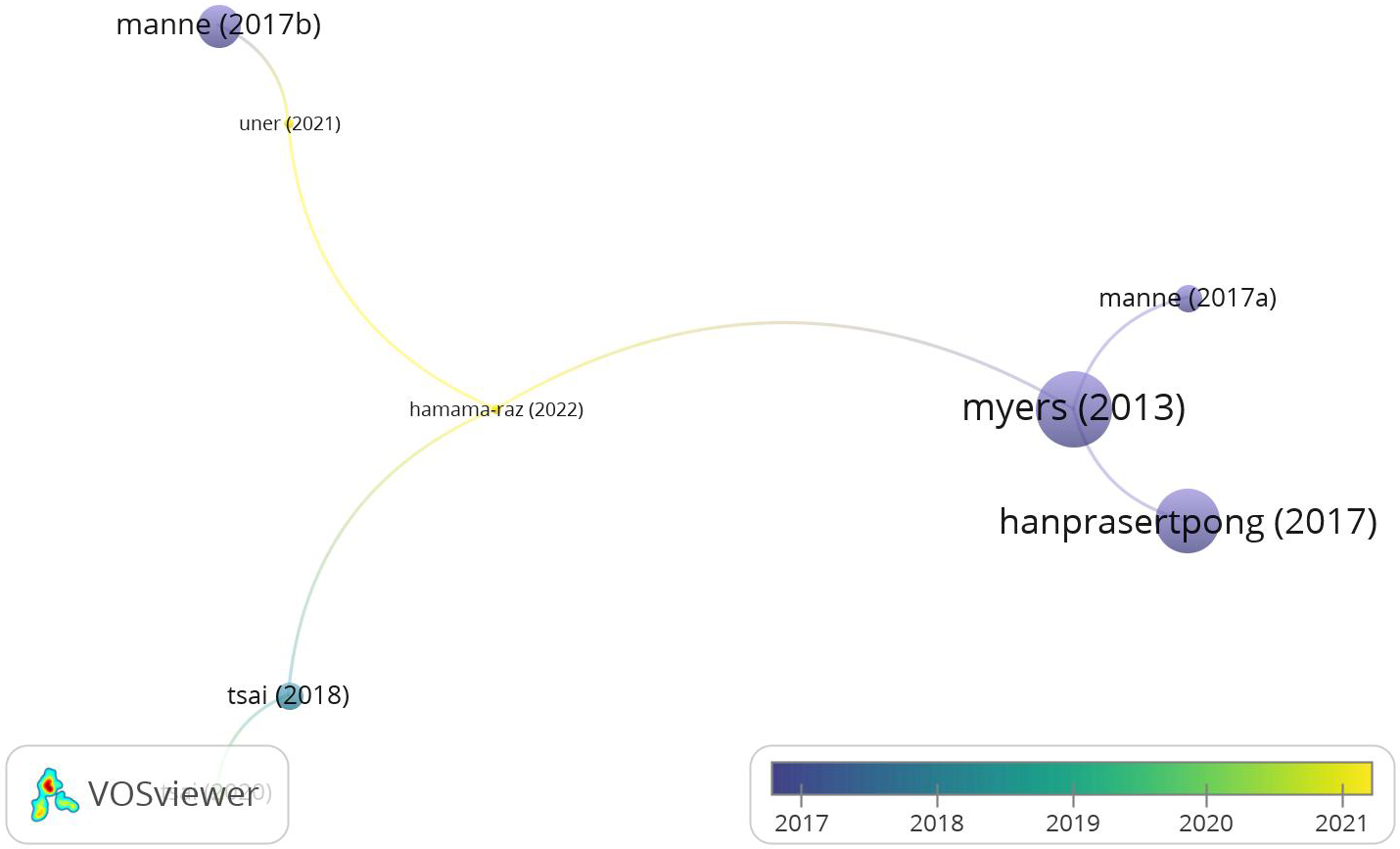
Figure 3: Most cited study.
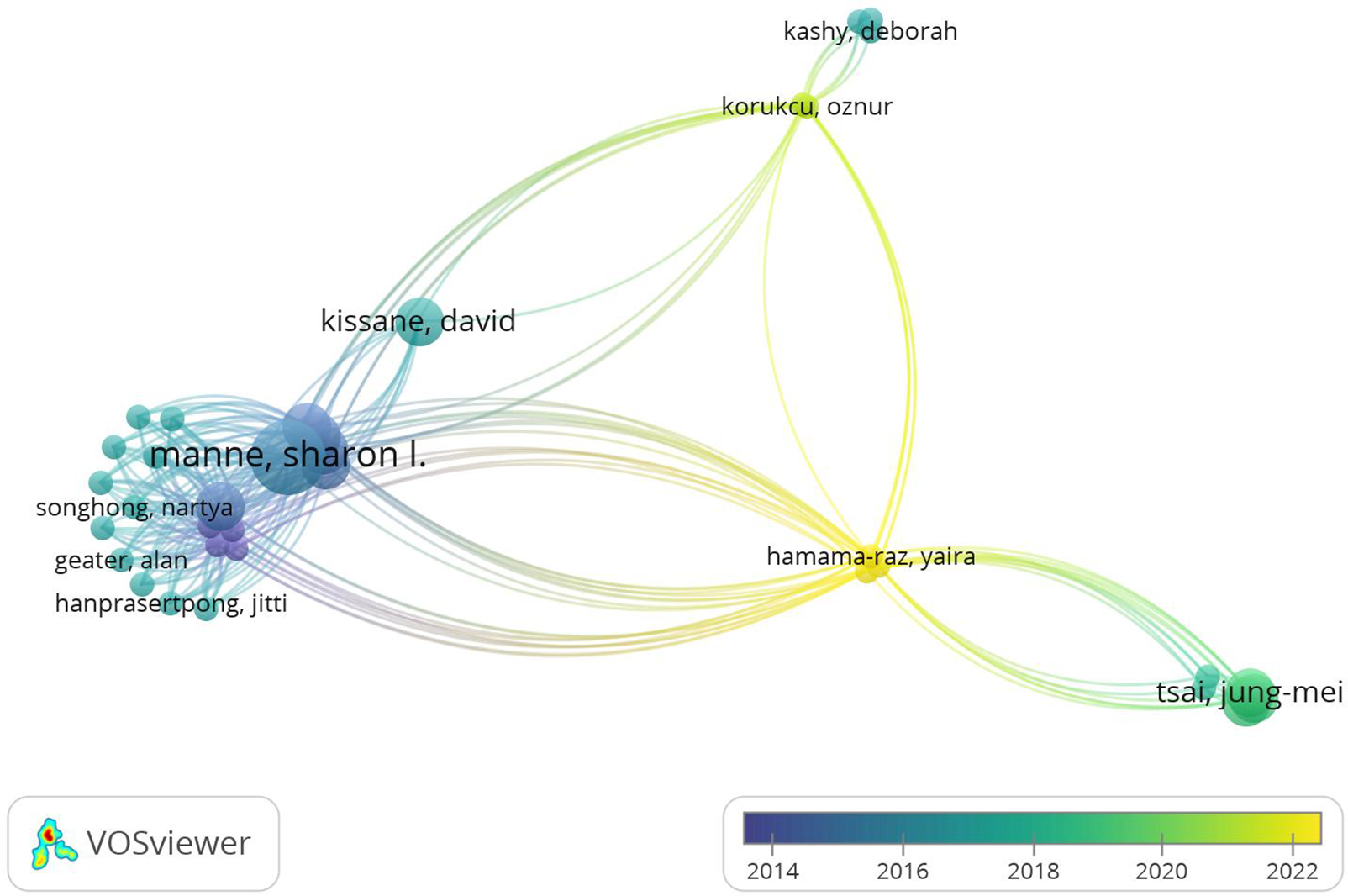
Figure 4: Most cited author.
The aims of the studies differ, but the common denominator is to investigate the relationship of FCR with quality of life and psychological distress and to identify situations that increase and decrease FCR. As a result, interventions and recommendations were made in the studies to determine the factors affecting FCR and to reduce the FOR.
Jeppesen et al. [20] tested the hypothesis that routine gynecological examinations and controls may remind women of cancer and may cause delayed detection of relapse symptoms and that therefore, follow-up under patient control will reduce FCR.
Manne et al. [21] examined structured coping intervention (CCI) with techniques in cognitive-behavioral interventions that focus on improving coping and seeking support skills, self-care, assessing and changing life priorities, managing FOR, identifying emotional responses to cancer, and promoting expression of emotions. It was concluded that supportive counseling (SC) interventions that support strengths and increase self-esteem did not significantly affect FCR. In order to achieve an effective result on the FCR and cancer-specific anxiety, it was stated that intensive intervention sessions focusing on cancer concerns and fears given after the initial treatment should be completed or that these intensive sessions should be added to the CCI.
Pradhan et al. [22] measured the cancer fear of women with ovarian cancer by completing the FoP-Q-SF scale before and after reading an online booklet created specifically for ovarian cancer. As a result, it was determined that women were satisfied with the booklet and would recommend it to others, but that it had little role in reducing the FCR and progression, and that women’s fear of cancer did not change significantly during the week after reading the booklet.
Hanprasertpong et al. [23] found that the 3 items with the highest fear score among the 12 items of the Cancer Progress Scale were worrying about what would happen to their family, fear of pain, and fear of the progression of the disease. Anxiety disorder and poor quality of life were associated with higher FCR, whereas sociodemographic characteristics were not significantly associated with FCR.
Manne et al. [24] aimed to analyze whether the evolution of cancer fear occurs in different patterns, i.e., increasing, decreasing, or stable over time, with group-based trajectory modeling. The secondary aim was to describe the association of FOR subgroups with demographic, medical, and psychological characteristics. When the characteristics of the subgroup that experienced stable and high levels of FOR were examined, it was determined that it was associated with features such as younger age, having metastatic cancer, depression, cancer anxiety, and less coping.
Sukyati et al. [25] examined FCR and its relationship with social support in women with gynecological cancer and stated that there was a positive significant relationship between age and FCR and that sociodemographic characteristics such as occupational status, monthly income, and cancer history were associated with FCR. It was stated that those with high social support experienced a lower FOR and that more studies were needed in this area.
Myers et al. [16] conducted a study to explain how the physical, emotional, and role changes associated with the diagnosis affect psychological adjustment and FOR. It was determined that social and cognitive variables (social variables such as positive reappraisal, coping efficiency, and self-esteem, and cognitive variables such as avoidance of negative reactions from family and friends) mediated approximately 66% of the relationship between fear of repetition and depression.
Ayu et al. [26] stated that FCR was negatively correlated with quality of life and that reducing FOR was an important theme in improving care and improving quality of life. It was also emphasized that sufficient knowledge and education in nurses play an important role in reducing FCR.
Disease representation refers to beliefs and expectations about the disease. Self-regulation was defined as meeting one’s own needs and achieving physical, psychological, and spiritual well-being through one’s actions, and it was concluded that other factors such as FCR, disease representation, self-regulation strategies, age, social support, and treatment method (surgery, chemotherapy) were associated with quality of life. FCR and negative disease representation were negatively correlated with quality-of-life subscales [27].
In the study by Sam [28], which aimed to reveal the similarities and differences in FCR experienced by cervical, ovarian, and uterine cancer survivors, survivors were grouped and evaluated according to age, disease-free time, and ethnicity. The mean FCR score was found to be similar, and the FCR was found to be higher in the Caucasian group, the younger age group, and the group with a disease-free period of less than 5 years.
Tsai et al. [29] in their qualitative study, revealed 3 themes, namely experiencing a depressive state as if facing a fierce enemy, feeling oneself in the shadow of cancer recurrence, and changing the mindset and perspective for positive progress. It was revealed that patients’ FOR fluctuated while they waited for the results of follow-up and control tests such as CA-125, and it was suggested that the actual situation be disclosed in advance so that patients have enough strength to face the disease.
Uner et al. [30] in their qualitative study, stated that the fears of women who had colposcopy during this process were grouped under three main themes: fear of colposcopy, feelings related to FCR and experience, and fear of getting cervical cancer. It was found that women with a history of cancer who underwent colposcopy due to abnormal cervical cytology during routine oncology controls had a significant FCR. Suggestions were made to healthcare professionals to be aware of the emotional needs of women in coping with the FCR during the colposcopy process and to support these patients by determining their social care needs.
In a qualitative study aimed at exploring and expanding the meaning of FCR among cervical cancer survivors, some patients experienced greater FCR in the first years, while others described taking antidepressants as a way of coping to overcome their FCR [31]. In addition to the participants who stated that an optimistic perspective in their spouse or partners alleviated the FOR, there were also participants who could not share their fears with their spouses and felt lonely. In this study, it was stated that FCR is a phenomenon that encompasses three factors: uncertainty, social-cognitive processing, and death anxiety, which are suggested to be addressed to improve the well-being of cervical cancer survivors.
Han et al. [32] examined the relationship of uncertainty in prognosis with FCR in individuals with ovarian cancer and stated that uncertainty not only triggers but can also improve FCR as a result of their qualitative interview. It was concluded that when an effective individual coping mechanism is developed, prognostic uncertainty can have a positive effect as it includes the possibility of non-relapse, and a two-way uncertainty process can develop with negative effects such as catastrophizing and ineffective coping, and increasing FRC in people who are prone to negative thoughts.
Ji et al. [33] conducted a qualitative study to determine the negative moods and coping styles experienced by patients with cervical cancer during the rehabilitation period, and it was found that the negative emotions observed in the period until they regained their former health after cancer diagnosis and treatment consisted of FCR, concerns about gender perception, and feelings of inferiority due to deterioration in body image. During this period, patients thought that their current health information was insufficient and stated that they needed a strong rehabilitation.
Galica et al. [34] conducted a qualitative study to determine how ovarian cancer survivors living in small towns or rural areas coped with FCR, and themes such as self-awareness, trust, self-prioritization, and positive orientation of thoughts and actions emerged as internal coping resources, while themes such as health personnel support emerged as external coping resources. Most women had high levels of FCR, and it was suggested that oncology nurses should be active in identifying and directing the internal and external resources available to survivors of this cancer to deal with FCR.
In a qualitative study using the Cancer Fear of Relapse Model to elicit women’s responses regarding their feelings, thoughts, and beliefs about FCR, four main themes related to women’s experiences of FCR emerged: uncertainty surrounding recurrence, varied beliefs and sources of worry, perceived risk of recurrence, and management of FCR. In this study, the uncertainty of cancer recurrence was found to be a major concern, and the inability to distinguish between natural symptoms and recurrence symptoms increased the FCR. It was stated that medical treatment and follow-up may be insufficient to meet psychosocial needs and that nurse-led follow-ups are needed to provide appropriate support [35].
Dewi et al. [36] concluded that the information obtained from television, the internet, social media, and cancer-surviving friends’ conversations about relapse, and the lack of family support triggered the FOR. Responses to the FOR consisted of four themes: firstly, anxiety for treatment such as radiation, chemotherapy, and surgery, secondly, fear of spreading the disease to other organs, thirdly, when going for screening after treatment, and fourthly, the feeling of discomfort reflected in watching television, having a relationship, or sleeping. These fears can arise at any time and affect daily life both emotionally and psychologically. Participants in the study hoped to receive information from healthcare professionals about the future status of the disease and treatments after their treatment was completed.
Fear of cancer recurrence and progression is one of the most frequently reported problems and one of the most common areas of unmet need for cancer survivors and caregivers [13]. This review aims to identify the factors associated with FCR in cancer patients and provide a theoretical framework.
Relationship between sociodemographic characteristics and FCR
When the relationship between age and FCR is examined in studies, it is stated that being at a younger age increases the probability of experiencing more FCR [16,21,28]. Because of their normative life expectancy, young women may place greater emphasis on their roles in body image, sexuality, child-rearing, and employment, and therefore may be more fearful of the threat of cancer recurrence. Contrary to these data, there are also studies stating that there is a positive correlation between age and FCR [25] or that age does not significantly affect FCR [23].
The literature suggests no clear correlation between marital status and the FCR [37]. Two studies investigating the association between marital status and FCR among women with gynecological cancer indicated no significant difference, aligning with the current literature [23,25]. In a study with a sample of ten people, it was stated that those who were single had a higher level of FOR than those who were married [36]. The fact that married people have social support such as spouses and children can reduce the FOR [27]. However, women’s focus on the people and relationships within their social circle instead of themselves may lead to a higher level of FOR compared to single individuals.
Those with fewer financial problems described less FOR [38], It has been stated that triggers from the FCR subdomains are most associated with low-income levels [25]. While there is no significant relationship between working in a paid job and FCR [23,39], there is also a study stating that FCR increases significantly as income level increases [39].
When examined in terms of gynecological cancer types, the FCR did not differ according to the cancer type [16,28,38,39]. Metastatic cancer, BRCA gene mutation, and family history of cancer in the participants were associated with FCR, while a family history of cancer was associated with higher psychosocial distress and functional impairment [21,25,35]. A family history of cancer or a genetic predisposition may trigger fear in women due to exposure to a certain risk factor and the feeling of not being able to control it.
It has been reported that Caucasian women experience more FCR [21] and that women who do not receive chemotherapy, have a lower body mass index, and have better physical functioning have a lower FCR [38]. Social support resources can prevent the occurrence of stressful life events; when stressful life events occur, they can change the way the event is perceived alleviate the stressful effect of the event and positively affect the adaptation of the person [25]. It is stated that one of the underlying reasons for the FCR is that cancer affects patients’ relationships [24,33], one of their biggest fears is worrying about what will happen to their families, and social relationships and social support are important factors affecting FCR [23,30]. Family is the most used social support group to cope with FCR, and patients with high social support have lower FCR levels [25,34,36,38].
Effectiveness of psychosocial characteristics and interventions on FCR
It is reported that deterioration in mental health and emotional weakness predict higher FCR [23], increase in positive emotional expression reduces FOR [21], when the effect of metacognitions on FCR is examined, negative thoughts about FOR are stronger than positive thoughts and trigger FCR [39], and FRC is more likely to increase in individuals who are prone to catastrophic and negative thinking and are unable to cope with prognostic uncertainty [31,32,35]. Self-awareness, confidence, self-prioritization, and positive orientation of thoughts and actions emerged as available internal coping resources for rural women in coping with FCR, while it was determined that they had needs such as health personnel support as external coping resources, and depending on this result, it can be said that those living in rural areas or smaller cities should be supported more when their access to health services is taken into account [34].
There are also results such as the finding that structured coping interventions and supportive counseling interventions with techniques in cognitive-behavioral interventions reduce cancer anxiety but do not significantly affect the FCR [21], and that an online resource created in terms of providing information on cancer does not make any difference in FCR [22]. It is stated that cognitive-behavioral intervention as well as cognitive-existential interventions reduce the FCR in women with breast and gynecological cancer and provide improvement in the scores which are sub-dimensions of FCR of coping, cognitive avoidance, need for reassurance from physicians, quality of life, and triggers [40]. These results suggest that more robust interventions should be developed to reduce FCR in the gynecological cancer population.
In a qualitative interview, undetected symptoms of relapse and uncertainty about the likelihood of relapse were sub-themes of the FCR experience [35], and perceived risk of relapse and disease uncertainty triggered FCR, while there are also results stating that women with anxiety and intolerance of uncertainty showed more negative coping behaviors [39], and that uncertainty of prognosis not only triggers the disease but also has a positive effect because this uncertainty includes the possibility of non-relapse [32].
The negative effects of cancer on sexuality and relationships, concerns about future treatments and emotional problems, and anxiety about not being able to fulfill their roles at home and work are the underlying reasons for the FOR [24,33]. Another trigger is accessing information about cancer from media such as TV programs, social media, and the internet [36]. Knowledge of cancer statistics and recurrence rates is one of the factors affecting the perception and FCR [35]. Tsai et al. [29] reported that while waiting for the results of follow-up and control tests such as CA-125, the FOR fluctuated during this uncertainty period. It was reported that women with a history of cancer who underwent colposcopy due to abnormal cervical cytology in routine oncology controls had a significant FCR and that their anxiety increased during gynecological examination [30]. It is stated that as the quality-of-life decreases, FCR increases and there is a negative relationship between the sub-dimensions of the quality-of-life scale and FCR [23,26,27]. For this reason, interventions should be planned to reduce the FCR and increase the quality of life among cancer survivors.
Due to the limited number of studies in the field of FCR in women with gynecological cancer, the findings were visualized to encourage researchers and to provide general information about the studies conducted in this field. The most used keywords in this field may be helpful when searching databases. And again, in the visuals presented with VOSviewer, the most cited author and study according to years are included. Although the study by Myers et al. [16] is the most cited publication in this field, when analyzed by year, it is seen that the current studies belong to Hamama-Raz et al. [31], Uner et al. [30]. While Manne was the most cited author in the past, it is seen that Hamama-Raz et al. [31] and Tsai et al. [29] are the most frequently cited authors in 2022.
Health personnel should be provided with knowledge and awareness in this area, and as well as the feelings and experiences of patients with FCR, those of caregivers should not be ignored. In addition to routine medical care, patients’ anxiety and fears should be reduced with various interventions by integrating a psychosocial and holistic approach to oncology. In intervention studies concerning FCR, it may be advisable to create group counseling programs based on the factors that trigger patients’ FCR, the coping strategies they employ, and their expectations of the healthcare system and social support resources for managing this fear. If FCR is at a high level, female patients should be referred to a psycho-oncologist. Psychoeducation with individuals about the possibility of recurrence of the disease, attempts to reduce this possibility and management of this fear may help to reduce fear.
The study’s strength lies in its systematic presentation of research on the factors that influence FCR in a specific group, namely women with gynecological cancer, in a quality-assessed manner. However, this study has limitations that should be considered. The FCR measurement methods, sample size, and study types varied among the included studies, which prevented the necessary conditions for conducting a meta-analysis from being met. Therefore, only descriptive data were analyzed and interpreted. It is noteworthy that the majority of the studies were conducted in the USA. As cultural and disease perceptions of women may vary across different countries, it is important to conduct research in other regions to obtain more global and generalizable results. The second limitation, which slightly reduces generalizability, is the exclusion of non-English articles. The limited number of interventions aimed at reducing FCR in women with gynecological cancer in the literature has resulted in limited recommendations for clinical practice. Therefore, it is hoped that this study will encourage further experimental and intervention studies on the FCR.
Sociodemographic factors affecting the FCR difference between studies, are elements such as age, marital status, economic status, gynecological cancer type. Negative thoughts and emotionally weak people should be supported by various interventions by considering the psychosocial features, considering factors that trigger FCR, it was concluded that women experiencing fear and FCR should reduce their anxiety. When the existing literature is examined, it is thought that more studies should be done on this subject.
Acknowledgement: The authors express their gratitude to all the authors of the publications used in the preparation of the systematic review.
Funding Statement: The authors received no specific funding for this study.
Author Contributions: Conception and design: Öznur Körükcü. Material preparation, data collection and analysis were performed by Şerife Büyükokudan and Öznur Körükcü. Manuscript writing and revision: Şerife Büyükokudan and Öznur Körükcü Final approval of manuscript: Şerife Büyükokudan and Öznur Körükcü. Study quality ratings: Şerife Büyükokudan and Öznur Körükcü.
Availability of Data and Materials: The datasets used and/or analyzed during the current study are available from the corresponding author on a reasonable request.
Ethics Approval: The present study does not involve human participants or animal subjects. The protocol was registered at PROSPERO under number CRD42023452570.
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
Supplementary Materials: The supplementary material is available online at https://doi.org/10.32604/po.2024.046627.
References
1. Papade A, Reddy GS, Pravalika N, Kumar BS. Risk factors of female reproductive cancers in Indian inhabitants. Medico Res Chron. 2020;7(3):112–8. [Google Scholar]
2. La Rosa VL, Shah M, Kahramanoglu I, Cerentini TM, Ciebiera M, Lin LT, et al. Quality of life and fertility preservation counseling for women with gynecological cancer: an integrated psychological and clinical perspective. J Psychosom Obstet Gynecol. 2020;41(2):86–92. [Google Scholar] [PubMed]
3. Warren N, Melrose DM, Brooker JE, Burney S. Psychosocial distress in women diagnosed with gynecological cancer. J Health Psychol. 2018;23(7):893–904. [Google Scholar] [PubMed]
4. Niedzwiedz CL, Knifton L, Robb KA, Katikireddi SV, Smith DJ. Depression and anxiety among people living with and beyond cancer: a growing clinical and research priority. BMC Cancer. 2019;19(1):1–8. [Google Scholar]
5. Zhang X, Sun D, Qin N, Liu M, Jiang N, Li X. Factors correlated with fear of cancer recurrence in cancer survivors: a meta-analysis. Cancer Nurs. 2022;45(5):406–15. [Google Scholar] [PubMed]
6. Mazzocco K, Masiero M, Carriero MC, Pravettoni G. The role of emotions in cancer patients’ decision-making. Ecancermedicalscience. 2019;13:914. [Google Scholar] [PubMed]
7. Mutsaers B, Butow P, Dinkel A, Humphris G, Maheu C, Ozakinci G, et al. Identifying the key characteristics of clinical fear of cancer recurrence: an international Delphi study. Psycho-Oncol. 2020;29(2):430–6. [Google Scholar]
8. Koral L, Cirak Y. The relationships between fear of cancer recurrence, spiritual well-being and psychological resilience in non-metastatic breast cancer survivors during the COVID-19 outbreak. Psycho-Oncol. 2021;30(10):1765–72. [Google Scholar]
9. Tauber NM, O’Toole MS, Dinkel A, Galica J, Humphris G, Lebel S, et al. Effect of psychological intervention on fear of cancer recurrence: a systematic review and meta-analysis. J Clin Oncol. 2019;37(31):2899. [Google Scholar] [PubMed]
10. Anderson K, Smith A’, Diaz A, Shaw J, Butow P, Sharpe L, et al. A systematic review of fear of cancer recurrence among indigenous and minority peoples. Front Psychol. 2021;12:621850. [Google Scholar] [PubMed]
11. Luigjes-Huizer YL, Tauber NM, Humphris G, Kasparian NA, Lam WWT, Lebel S, et al. What is the prevalence of fear of cancer recurrence in cancer survivors and patients? A systematic review and individual participant data meta-analysis. Psycho-Oncol. 2022;31:879–92. [Google Scholar]
12. Pang C, Humphris G. The relationship between fears of cancer recurrence and patient gender: a systematic review and meta-analysis. Front Psychol. 2021;12:640866. [Google Scholar] [PubMed]
13. Simard S, Thewes B, Humphris G, Dixon M, Hayden C, Mireskandari S, et al. Fear of cancer recurrence in adult cancer survivors: a systematic review of quantitative studies. J Cancer Surviv. 2013;7(3):300–22. [Google Scholar] [PubMed]
14. Ozga M, Aghajanian C, Myers-Virtue S, McDonnell G, Jhanwar S, Hichenberg S, et al. A systematic review of ovarian cancer and fear of recurrence. Palliat Support Care. 2015;13(6):1771–80. [Google Scholar] [PubMed]
15. Salani R. Survivorship planning in gynecologic cancer patients. Gynecol Oncol. 2013;130(2):389–97. [Google Scholar] [PubMed]
16. Myers SB, Manne SL, Kissane DW, Ozga M, Kashy DA, Rubin S, et al. Social-cognitive processes associated with fear of recurrence among women newly diagnosed with gynecological cancers. Gynecol Oncol. 2013;128(1):120–7. [Google Scholar] [PubMed]
17. Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Reprint—preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Physical Ther. 2009;89(9):873–80. [Google Scholar]
18. Centre for Reviews and Dissemination. Systematic reviews: CRD’s guidance for undertaking reviews in health care. In: Akers J, editor. Centre for reviews and dissemination. York, UK: University of York; 2013. [Google Scholar]
19. Moola S, Munn Z, Tufanaru C, Aromataris E, Sears K, Sfetcu R, et al. Chapter 7: systematic reviews of etiology and risk. In: Joanna Briggs institute reviewer’s manual. vol. 5. Adelaide, Australia: The Joanna Briggs Institute; 2020. p. 217–69. [Google Scholar]
20. Jeppesen M, Jensen P, Hansen D, Christensen R, Mogensen O. Patient-initiated follow up affects fear of recurrence and healthcare use: a randomised trial in early-stage endometrial cancer. BJOG: Int J Obstet Gynaecol. 2018;125(13):1705–14. [Google Scholar]
21. Manne SL, Virtue SM, Ozga M, Kashy D, Heckman C, Kissane D, et al. A comparison of two psychological interventions for newly diagnosed gynecological cancer patients. Gynecol Oncol. 2017;144(2):354–62. [Google Scholar] [PubMed]
22. Pradhan P, Sharpe L, Butow PN, Smith AB, Russell H. Is a brief online booklet sufficient to reduce fear of cancer recurrence or progression in women with ovarian cancer? Front Psychol. 2021;12:634136. [Google Scholar] [PubMed]
23. Hanprasertpong J, Geater A, Jiamset I, Padungkul L, Hirunkajonpan P, Songhong N. Fear of cancer recurrence and its predictors among cervical cancer survivors. J Gynecol Oncol. 2017;28(6):1–11. [Google Scholar]
24. Manne SL, Myers-Virtue S, Kissane D, Ozga ML, Kashy DA, Rubin SC, et al. Group-based trajectory modeling of fear of disease recurrence among women recently diagnosed with gynecological cancers. Psycho-Oncol. 2017;26(11):1799–809. [Google Scholar]
25. Sukyati I, Afiyanti Y, Rahmah H, Milanti A. Fear of recurrence predictors among Indonesian gynecological cancer survivors. J Int Dent Med Res. 2019;12(1):305–9. [Google Scholar]
26. Ayu NKP, Afiyanti Y. Fear of cancer recurrence and quality of life among gynaecological cancer survivors under treatment. Enfermería Clínica. 2021;31:S276–80. [Google Scholar]
27. Tsai LY, Lee SC, Wang KL, Tsay SL, Tsai JM. A correlation study of fear of cancer recurrence, illness representation, self-regulation, and quality of life among gynecologic cancer survivors in Taiwan. Taiwan J Obstet Gynecol. 2018;57(6):846–52. [Google Scholar] [PubMed]
28. Sam A. Fear of cancer recurrence in gynecologic cancer survivors: an overview. J Oncol Navig Surviv. 2018;9(3):1–10. [Google Scholar]
29. Tsai LY, Tsai JM, Tsay SL. Life experiences and disease trajectories in women coexisting with ovarian cancer. Taiwan J Obstet Gynecol. 2020;59(1):115–9. [Google Scholar] [PubMed]
30. Uner FO, Korukcu O. A qualitative exploration of fear of cancer recurrence in Turkish cancer survivors who were referred for colposcopy. Health Soc Care Commun. 2021;29(3):729–37. [Google Scholar]
31. Hamama-Raz Y, Shinan-Altman S, Levkovich I. The intrapersonal and interpersonal processes of fear of recurrence among cervical cancer survivors: a qualitative study. Support Care Cancer. 2022;30(3):2671–8. [Google Scholar] [PubMed]
32. Han PK, Gutheil C, Hutchinson RN, LaChance JA. Cause or effect? The role of prognostic uncertainty in the fear of cancer recurrence. Front Psychol. 2021;11:626038. [Google Scholar] [PubMed]
33. Ji J, Zhu H, Zhao JZ, Yang YQ, Xu XT, Qian KY. Negative emotions and their management in Chinese convalescent cervical cancer patients: a qualitative study. J Int Med Res. 2020;48(9):0300060520948758. [Google Scholar] [PubMed]
34. Galica J, Giroux J, Francis JA, Maheu C. Coping with fear of cancer recurrence among ovarian cancer survivors living in small urban and rural settings: a qualitative descriptive study. Eur J Oncol Nurs. 2020;44:101705. [Google Scholar] [PubMed]
35. Kyriacou J, Black A, Drummond N, Power J, Maheu C. Fear of cancer recurrence: a study of the experience of survivors of ovarian cancer. Canadian Oncol Nurs J. 2017;27(3):236. [Google Scholar]
36. Dewi SK, Afiyanti Y, Rachmawati IN. Fear of recurrence among gynaecological cancer survivors: a qualitative study. Enfermería Clínica. 2021;31:S352–5. [Google Scholar]
37. Crist JV, Grunfeld EA. Factors reported to influence fear of recurrence in cancer patients: a systematic review. Psycho-Oncol. 2013;22:978–86. [Google Scholar]
38. Krok-Schoen JL, Naughton MJ, Bernardo BM, Young GS, Paskett ED. Fear of recurrence among older breast, ovarian, endometrial, and colorectal cancer survivors: findings from the WHI LILAC study. Psycho-Oncol. 2018;27(7):1810–5. [Google Scholar]
39. Lebel S, Maheu C, Tomei C, Bernstein LJ, Courbasson C, Ferguson S, et al. Towards the validation of a new, blended theoretical model of fear of cancer recurrence. Psycho-Oncol. 2018;27(11):2594–601. [Google Scholar]
40. Maheu C, Lebel S, Bernstein LJ, Courbasson C, Singh M, Ferguson SE, et al. Fear of cancer recurrence therapy (FORTa randomized controlled trial. Health Psychol. 2023;42(3):182–94. [Google Scholar] [PubMed]
Cite This Article
 Copyright © 2024 The Author(s). Published by Tech Science Press.
Copyright © 2024 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper View Full Text
View Full Text Download PDF
Download PDF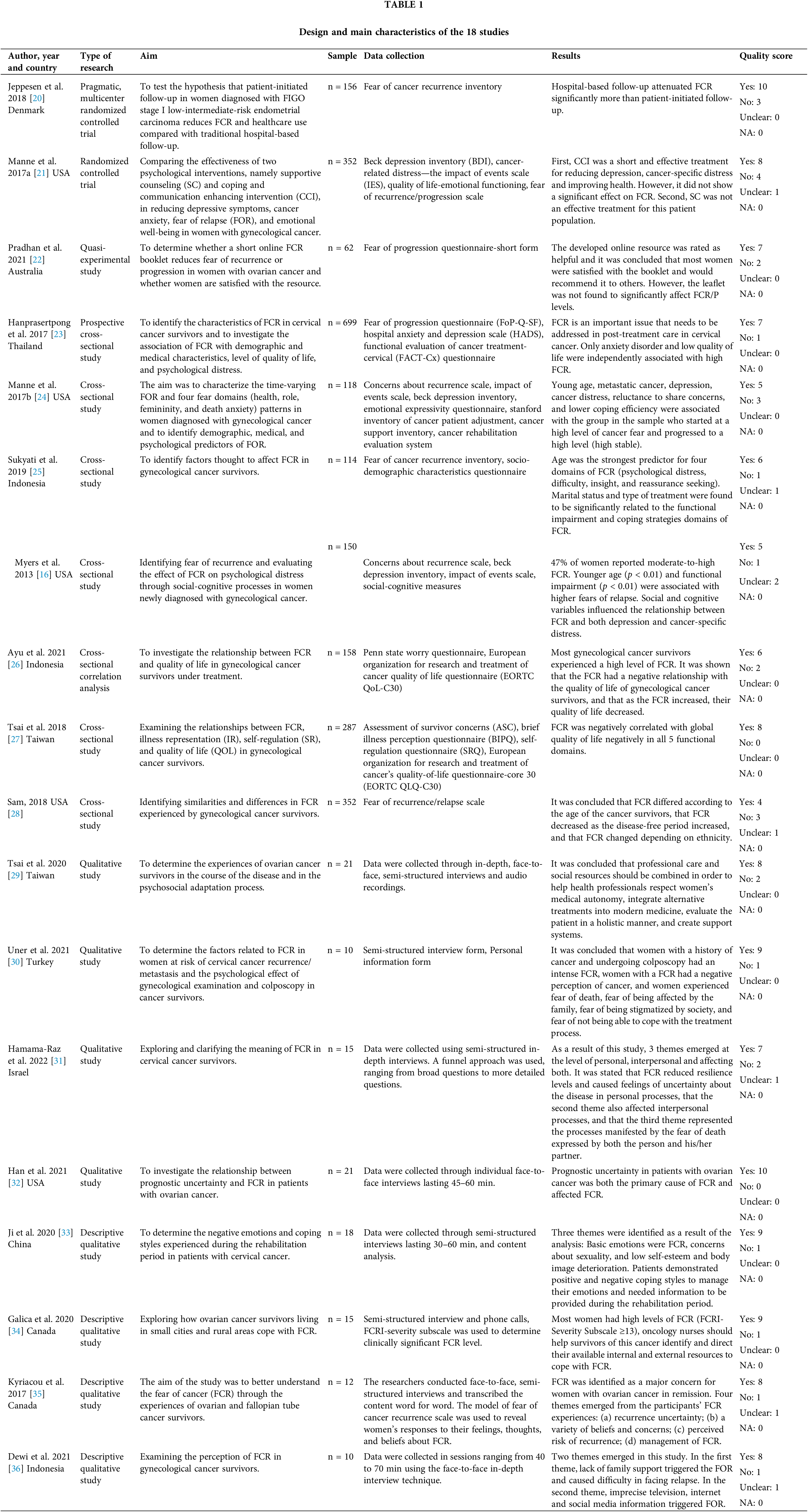
 Downloads
Downloads
 Citation Tools
Citation Tools