 Open Access
Open Access
ARTICLE
The Impact of Social Support on the Mental Health of Cancer Patients: Evidence from China
School of Public Administration and Law, Hunan Agricultural University, Changsha, 410128, China
* Corresponding Author: Wanxiu Zhu. Email:
Psycho-Oncologie 2024, 18(1), 69-77. https://doi.org/10.32604/po.2023.046593
Received 08 October 2023; Accepted 06 December 2023; Issue published 25 March 2024
Abstract
Exploring the relationship between social support and the mental health of cancer patients is a vital endeavor for enhancing mental well-being. The objective of this study was to explore the relationship between social support and psychological well-being in cancer patients and to provide new empirical evidence for psychological improvement in cancer patients. This research holds significant practical implications for optimizing China’s public health system and strengthening the development of a healthy China. Using data from the 2018 China Health and Retirement Longitudinal Study (CHARLS) database, we empirically examined the influence of social support on the mental health of cancer patients. Models such as Ordered Probit and OLogit were used to provide empirical evidence and theoretical insights for enhancing the mental health of cancer patients in a context marked by a high prevalence of cancer. The findings indicated that both formal and informal social support mechanisms were effective in improving the mental health of cancer patients. Furthermore, we utilized the propensity score matching (PSM) model to eliminate the endogeneity issue associated with sample selectivity bias. The results obtained through PSM demonstrated robustness, underscoring the importance of addressing sample selectivity bias when assessing the impact of social support on the mental health of cancer patients. Therefore, the Chinese government is recommended to prioritize the use of social support as a means to proactively enhance the mental health of cancer patients, thereby continuously elevating their overall quality of life.Keywords
The improvement of mental health among cancer patients represents a critical concern within the domains of public health and psychology worldwide [1–3]. In recent years, the incidence of cancer has surged in tandem with the rise in living standards across populations. According to data released by the World Health Organization in 2020, a staggering 9.96 million cancer-related deaths were reported globally. Thirty percent of these fatalities, equating to 3 million lives, occurred in China, which stands atop the global ranks for both cancer incidence and mortality [4]. Relevant research has shown that cancer patients frequently grapple with adverse psychological states, stemming from physical suffering and other factors [5]. This not only hampers their recovery but also exerts additional stress upon their families. In 2022, during the 20th National Congress of the Communist Party of China (CPC), President Xi Jinping proposed that safeguarding public health must assume a paramount strategic role in development. He emphasized the need to enhance health-promoting policies, with specific attention to mental health. Elevating the mental health of cancer patients has been identified as a key component in the broader endeavor to optimize China’s public health system and establish a healthier China. However, contemporary research has shown limited focus on the mental health of cancer patients. Against the backdrop of escalating cancer incidence, implementing measures that can intervene to enhance the mental health of cancer patients and alleviate their suffering is imperative. This endeavor holds profound significance not only for the physical recuperation of these patients but also for its broader societal impact in fostering increased awareness and compassion for cancer patients.
In recent years, social support has garnered increasing attention from both academics and practitioners as a vital approach to enhancing mental health. Social support encompasses the collective actions of specific social networks that employ material and emotional resources to aid socially vulnerable groups without seeking compensation [6]. It serves as a comprehensive term encompassing various forms of assistance originating externally to the individual, and it constitutes a social behavior that coexists with the presence of vulnerable groups. According to social support theory, the strength of an individual’s social support network directly correlates with their capacity to navigate a spectrum of environmental challenges [7]. Cancer patients suffer both physically and psychologically as a result of this disease. Especially in the advanced stages of the illness, psychological trauma can exacerbate the progression of the disease [8]. As a “vulnerable group” in the health field, cancer patients stand to benefit greatly from social support, aiding them in coping with the physical and psychological challenges presented by their condition. Material aid, psychological comfort, and familial companionship, all facets of social support, collectively function to improve the mental well-being of cancer patients. Therefore, we aimed to empirically analyze the impact of social support on the mental health of cancer patients, using data sourced from the 2018 China Health and Retirement Longitudinal Study (CHARLS) database. The objective of this study was to explore the relationship between social support and psychological well-being in cancer patients and to provide new empirical evidence for psychological improvement in cancer patients. This research operates in the context of the high prevalence of cancer and the advancement initiatives geared toward developing a healthy China.
Mental health of cancer patients
As society continues to evolve and the cancer incidence rates rise, the mental health of cancer patients has garnered increasing scholarly attention. Klikovac et al. studied the impact of the COVID-19 pandemic on the mental health of cancer patients in Serbia. Their findings indicated that older patients and those who perceived their socio-economic and health status more favorably experienced lower levels of anxiety, depression, and stress [9]. Macia et al. explored the relationship between emotional control, resilience, and mental health in cancer patients. They discovered that high resilience and low emotional control acted as protective factors, while elevated emotional control was identified as a risk factor for mental health issues [10]. The study by Thinh et al. assessed the prevalence and severity of depression and anxiety symptoms, impairments in access to mental health, and associations of dysfunction among cancer inpatients. The high frequency and severity of depression and anxiety symptoms highlight the importance of integrating mental health services into existing oncology treatment options [11]. In 2017–2018, Jeihooni et al. conducted a survey involving 200 cancer patients in Shiraz, Iran, to investigate the effects of an educational intervention based on the PRECEDE model. Their results demonstrated that after 6 months of intervention, the experimental group exhibited significant increases in knowledge, attitudes, health-promoting behaviors, patient hope, and mental well-being compared with the control group [12]. Becarevic et al. explored the correlation between religion and mental health in cancer patients and observed that Muslim cancer patients were more religious and spiritual than the non-cancer Muslim population. These patients also expressed a need for spiritual support to alleviate depression, anxiety, and stress [13].
Social support and mental health
Research on the link between social support and mental health has seen a steady increase, with scholars recognizing it as a pivotal tool for promoting mental health. Jennifer’s investigation involved evaluating the connection between mental health and social support among a large randomized sample of college students. The findings revealed that students with low-quality social support were at a higher risk of mental health problems, including a six-fold greater likelihood of experiencing depressive symptoms compared with students with high-quality social support [14]. Kira et al. analyzed the relationship between social support and physical and mental health in a sample of 220 TNB youth aged 14–25 years living in Quebec, Canada. The results showed a significant positive relationship between different support sources and mental health and well-being outcomes [15]. Qi et al. examined the relationship between levels of social support and mental health among Chinese adolescents during the COVID-19 outbreak. The study showed that the prevalence of mental health problems was higher among Chinese adolescents with low to moderate levels of social support during this period [16]. Muoz-Bermejo et al. explored how perceived social support impacted the mental health of older caregivers and showed that social support played a significant role in enhancing their mental well-being [17]. Hu et al. examined the relationship between social support and the mental health of Chinese college students and determined that social support positively affected the mental well-being of these students [18]. Xie et al. analyzed the impact of social support on the health of older adults using 2018 CLHLS data. The results indicated that formal social support significantly improved the health of older adults, while informal social support had a positive effect on the mental health of this demographic [19].
The existing literature comprehensively revealed that research on the mental health of cancer patients primarily focuses on identifying the influencing factors and strategies to promote mental well-being. Studies exploring the correlation between social support and mental health have predominantly concentrated on adolescents and the elderly, particularly in the context of epidemics. Research specifically addressing the relationship between social support and the mental health of cancer patients is lacking. Given the escalating incidence of cancer, enhancing the quality of life for both cancer patients and the broader public health system in China holds profound importance. This can be achieved by employing diverse approaches to improve the mental health of cancer patients. Accordingly, we utilized the highly representative CHARLS data in China to empirically examine the influence of social support on the mental health of cancer patients. Additionally, we conducted robustness tests and endogeneity analyses with the objective of providing insights that can inform the development of public health policies in China.
The data in this study was sourced from the 2018 CHARLS database. This database was established in 2011 under the auspices of the National Development Research Institute of Peking University (NDI). It was co-organized and implemented by the China Social Science Survey Center of Peking University and the Peking University Youth League Committee. The survey covers 28 provinces (municipalities and districts), 150 counties (municipalities and districts), and 450 villages (neighborhood committees) across the country. Due to its large sample size and wide coverage, it has become a recognized and authoritative source of data in the field of social sciences in China. The 2018 questionnaire survey collected information on respondents’ demographic and sociological characteristics, family backgrounds, economic statuses, health statuses, and lifestyles. For the purposes of the study, cancer patients were selected as the subjects for analysis. Control variables were then chosen in conjunction with the sample screening process, and missing values, outliers, and invalid variables were processed and removed. Finally, we obtained a total of 375 valid samples.
Dependent variable: The mental health of cancer patients was the dependent variable in this study. Currently, various measures of mental health exist in the academic world [20–22]. In this study, we assessed mental health by considering the depression status of individuals. The 2020 CHARLS database contains an item labeled “DC011—I feel emotionally drained.” This item offers the following response options: “rarely or not at all,” “not too much,” “sometimes or half the time,” and “most of the time.” We assigned values of 1–4 to these response categories. Here, 1 indicates that cancer patients seldom experience feelings of depression, signifying good mental health; 2 denotes infrequent experiences of depression, indicating fair mental health; 3 signifies occasional feelings of depression, suggesting somewhat compromised mental health; and 4 represents frequent experiences of depression, indicating poor mental health.
Independent variable: Social support was the independent variable in this study. Measurement of social support lacks a uniform consensus; for instance, some studies categorize it into formal and informal social support based on types [23], whereas others categorize it into objective and subjective support based on attributes [24]. In this study, we adopted a comprehensive approach informed by prior research, using a combination of formal and informal social support for measurement. Formal social support encompasses key components such as participation in social insurance programs and receipt of in-home medical services. In the database, specific questions pertain to these aspects: “Are you enrolled in health insurance?” and “Do you participate in basic pension insurance?” A response of “yes” to 1 to either question was assigned a value of 1, indicating enrollment in social insurance; otherwise, it was assigned a value of 0. For home health care services, the question “Have you received home health care services?” was coded as 1 for those who have accepted such services and 0 for those who have not. Informal social support includes indicators related to financial support for children and the extent of caregiving provided. A respondent was assigned a value of 1 if they received financial support for their children; otherwise, it was marked as 0. For the child care indicator, we used the frequency of meeting with their children as a measure, assigning values ranging from 1 to 10 to reflect increasing levels of engagement with their children.
Control variable: Numerous studies have demonstrated that an individual’s inherent characteristics play a key role in influencing their mental health status [25,26]. Therefore, in our model, we included the following control variables: gender, age, place of residence, literacy, and marital status. Detailed variable definitions and statistical information are presented in Table 1.

The dependent variable in this paper is the mental health status of cancer patients, which is a multicategorical variable, so we utilize the Ordered Probit regression model for analysis. In this paper, we set the following Ordered Probit regression model [27]:
In Eq. (1),
Whether or not a cancer patient receives social support can be influenced by a number of listed factors such as gender, age, literacy, marital status, and so on. Therefore, the estimation results of the model will produce selective bias. In order to control as much as possible the bias in model estimation due to sample selection bias, this paper utilizes the propensity score matching (PSM) model [28] to estimate the net effect of the impact of social support on the mental health of cancer patients. Whether to accept social support is a self-choice made by individual cancer patients according to their own conditions, so the model will appear due to sample selection bias. In this study, the PSM model was used to reduce the estimation bias and maintain the robustness of the model analysis results. The model is set up as follows:
In Eq. (2),
Descriptive statistical results
According to the results of descriptive statistics, the mean score of the mental health of the surveyed cancer patients in the sample was 2.208. Approximately 61.07% of the respondents reported having good and fair mental health, indicating that over half of the respondents were in a good psychological condition. Regarding formal social support, the highest enrollment rate, at 96.6%, was observed in social insurance participation. In contrast, only 24.8% of patients had received in-home services. In terms of informal support, 18.67% of patients reported receiving financial support from their children. Additionally, a higher-than-average number of respondents mentioned that their children provided frequent care. In terms of gender, 63.2% of the participants were male, whereas 36.8% were female. The average age of the respondents was 67.883 years, with 77.87% of them having completed primary and secondary education. As for marital status, the majority of respondents, accounting for 84.8%, were married.
Table 2 presents the results of the basic regression examining the effect of social support on the mental health of cancer patients. Models (1) and (2) assessed the influence of formal social support on the mental well-being of these patients, and models (3) and (4) focused on the effects of informal social support. The results revealed that the coefficient of model (1) was −1.119, indicating that social insurance significantly affects the mental health of cancer patients at a 5% level of significance. Moreover, compared to cancer patients who do not receive social support, those who do receive such support experience an improvement of 1.119 units in their mental health. Similarly, in models (2), (3), and (4), the effects of receiving home health care services, children’s financial support, and children’s accompaniment and care on the mental health of cancer patients were significant at 1%, 10%, and 1% significance levels, respectively. For each unit of social support added, the mental health of patients was positively influenced by 0.371, 0.276, and 0.057 units in these respective cases. Collectively, both formal and informal social support made positive contributions to the mental health of cancer patients. Additionally, the control variables indicated that patients with higher levels of literacy had better mental health, and patients who were married exhibited a propensity for better mental health. An overview of the baseline regression results is presented in Table 2.
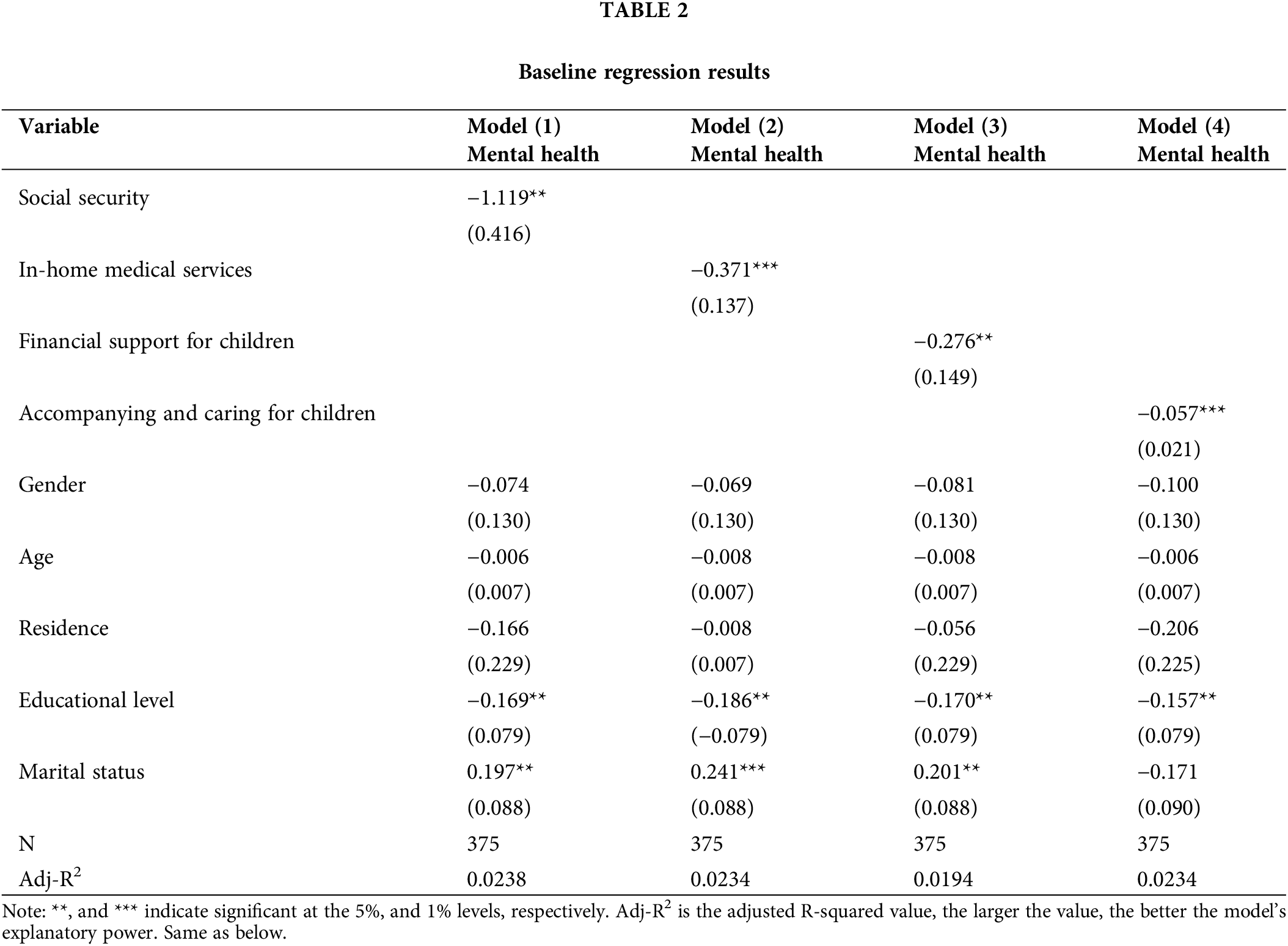
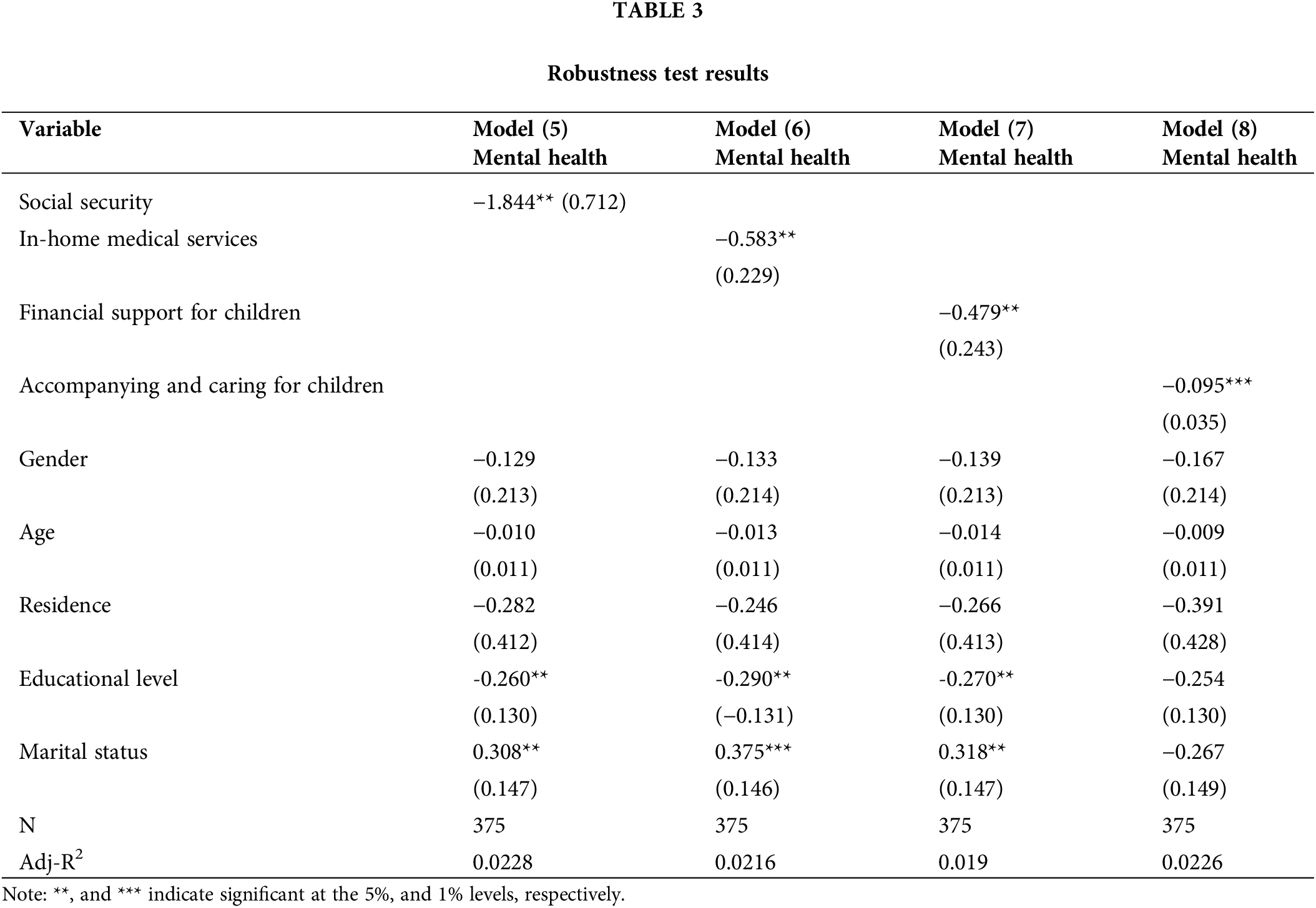
To ensure the robustness of the estimation results, we used the replacement econometric modeling approach for testing robustness. Given that the dependent variables in this study are multicategorical variables, we utilized the OLogit model for analysis. The results revealed that social insurance, in-home medical services, children’s financial support, and children’s companionship and care exhibited a significant positive impact on the mental health of cancer patients (Table 3). This finding indicated that both formal and informal social support positively improved the mental health of cancer patients. Moreover, this result was consistent with the baseline regression results, underscoring the robustness of the estimation results obtained in this study.
The receipt of social support by a cancer patient can be influenced by various factors, including gender, age, and literacy level, leading individuals to make independent choices based on self-judgment. At this point, the model encounters an endogeneity issue due to sample selectivity bias. To address this concern and obtain unbiased estimation results, we used the propensity score matching (PSM) model to conduct endogeneity tests, thus eliminating sample selectivity bias. In this study, we selected both K-nearest and radius neighbor matching for estimation [29]. Before formally executing the matching process, performing a balance test to assess the quality of sample matching is essential. Only when the matched samples passed the sample balance test could we proceed with subsequent analysis. The results of the balance test of the samples are presented in Table 4.
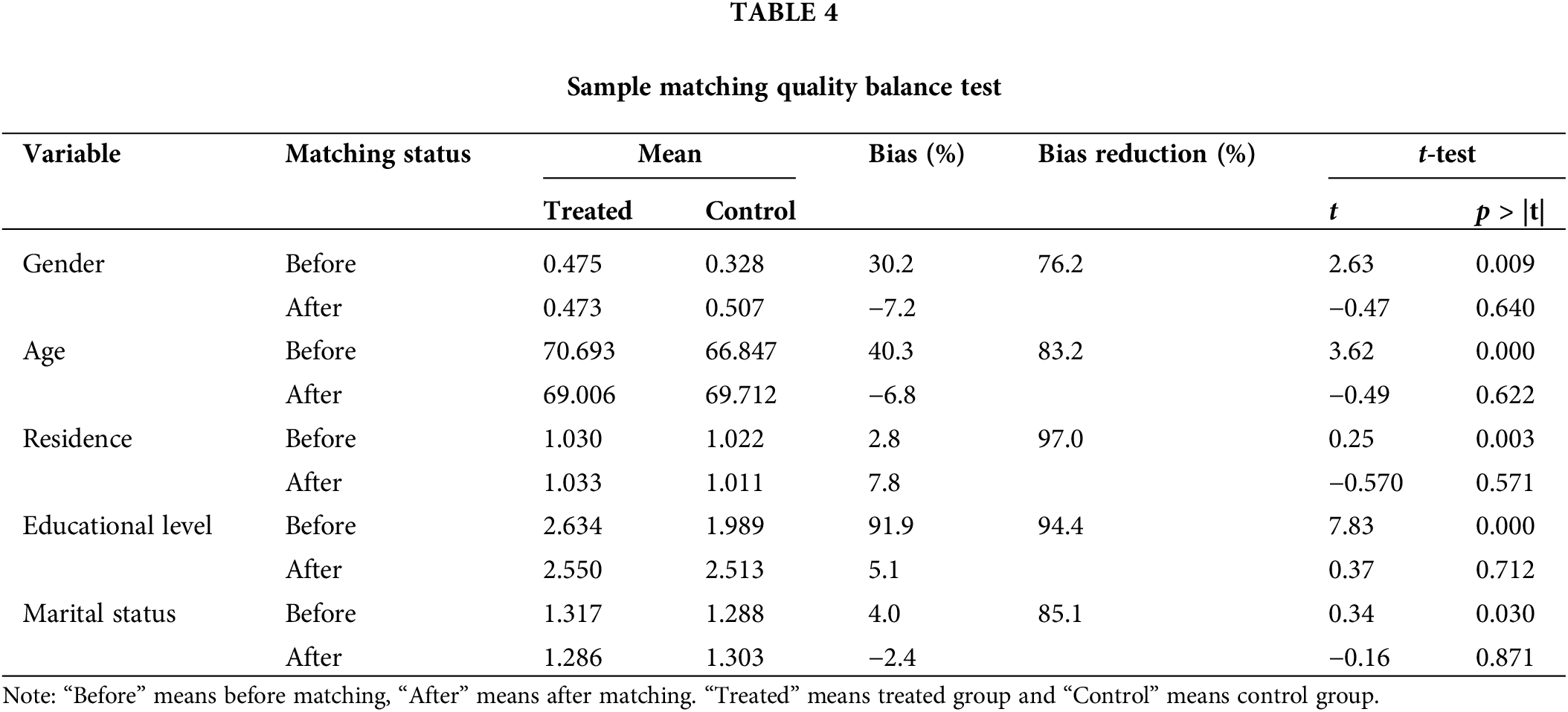
According to the results of the balance test, the absolute value of the standardized deviation for all variables after matching was less than 5%. The t-test results for the means of all variables in the treatment and control groups were significant before matching but not after matching. These findings indicated a higher quality of matching. Additionally, we included kernel density function plots before and after matching. The post-matching kernel density function plot exhibited greater consistency, further indicating improved quality of the samples and successful results in the sample balance test. The kernel density function plots before and after matching are displayed in Figs. 1 and 2, respectively.

Figure 1: Kernel density function plot before matching.

Figure 2: Kernel density function plot after matching.
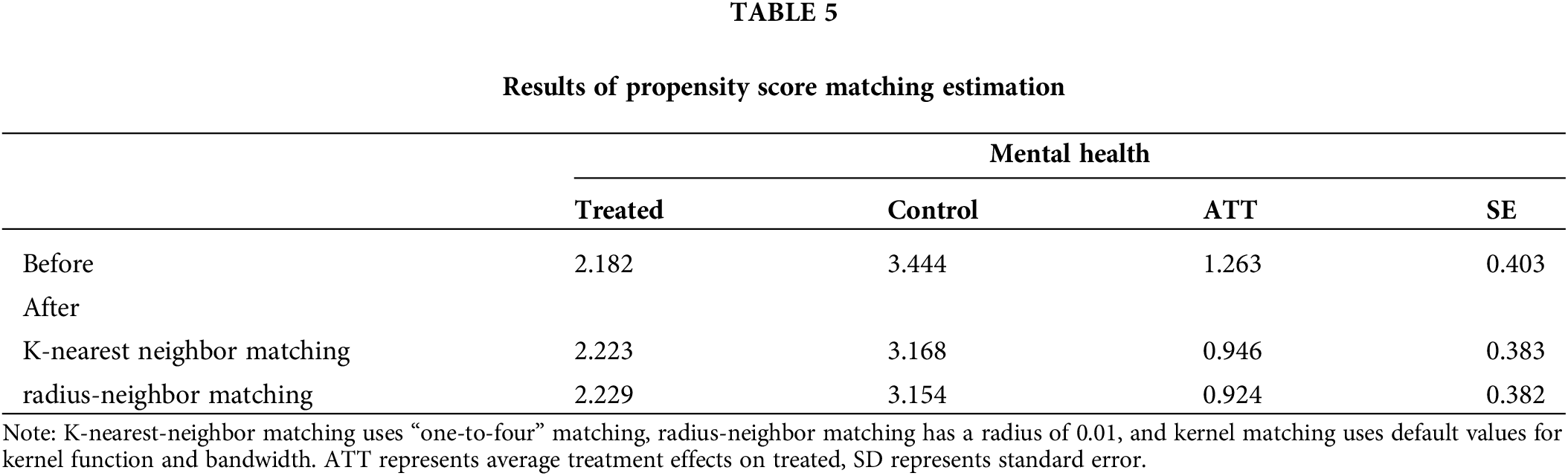
Table 5 presents the estimation results obtained after conducting PSM. According to the results, using the K-nearest neighbor matching method, the ATT value of the mental health status of cancer patients was 1.263 before matching and decreased to 0.946 after matching. This observation indicated that, following the adjustment for selection bias within the sample, the net effect of social support on the mental health of cancer patients was 94.6%. Similarly, using the radius neighbor matching method, the ATT value of the sample was 1.263 before matching and decreased to 0.924 after matching. This observation indicated that the net effect of social support on the mental health of cancer patients was 92.4%. These outcomes underscore the enhanced robustness of the results obtained through PSM analysis. Furthermore, they highlight the potential underestimation of the impact of social support on the mental health of cancer patients if sample selectivity bias remains unaddressed. Owing to space constraints, results solely pertaining to the impact of formal social support on the mental health of cancer patients are reported here. For a comprehensive overview, please refer to Table 5.
The results of this study demonstrate that both formal and informal social support can effectively enhance the mental health of cancer patients. Regarding formal social support, engaging in social insurance programs and receiving home medical services can effectively promote the psychological health of these patients. Compared to receiving home medical services, participation in social insurance exerted a significantly higher effect on the psychological health of cancer patients. This distinction can be attributed to the robust and comprehensive social security system in China, where the coverage rates for both basic social pension and basic medical insurances have reached 90%. Additionally, the participation rate in basic medical insurance is as high as 95%. On the one hand, this reflects the influence of traditional Chinese cultural values, such as the concept of “providing for the old,” wherein pension insurance plays a pivotal role in providing a safety net. Consequently, cancer patients enrolled in pension insurance programs experience a heightened sense of security, thereby positively affecting their emotional and psychological health. On the other hand, patients covered by urban and rural residents’ medical insurance typically have at least 50% coverage of their medical expenses courtesy of the state. Moreover, those participating in urban workers’ medical insurance benefit from an approximately 80% reimbursement rate. This means that the onset of cancer does not result in financially crippling expenses for the patient’s family. Therefore, this financial security positively affects the psychological well-being of individuals facing cancer diagnoses.
Informal social support, financial assistance, and spiritual companionship from family members can have a positive impact on the mental health of cancer patients. Numerous studies have consistently demonstrated that cancer patients often experience substantial mental distress, particularly those with advanced cancer who must confront both physical suffering and psychological anguish, including the fear of death [5,30]. Therefore, during this critical phase, cancer patients greatly benefit from the strong support provided by their family members, which, in turn, enhances their mental health and expedites the process of recovery. Furthermore, we conducted a robustness test using the method of substitution measurement modeling, and the results affirmed the reliability and stability of the findings presented in this study. Additionally, our analysis employing a PSM model indicated that mitigating the issue of sample self-selection yielded more refined results. Elimination of endogeneity led to a more accurate estimation of the impact of social support on the mental health of cancer patients.
For these reasons, we present several pertinent recommendations. First, the mental health of cancer patients should be prioritized. Given the unique challenges faced by cancer patients, their bodies and minds are subjected to greater stress than those of healthy individuals. Therefore, relevant authorities must place substantial emphasis on the provision of care and psychological for cancer patients. This extends to the family members of these patients, who should also have access to relevant psychological counseling services. Second, actively enhancing the function of social support in alleviating the emotional distress experienced by cancer patients is imperative. At the level of formal social support, the government should expand the scope of social insurance coverage and increase participation rates. Furthermore, it should actively guide the family members of cancer patients in providing both material and spiritual support. Community-based initiatives, such as educational and training programs focused on cancer care and support for family members, can be instrumental in leveraging the vital role that family members play in the care and recovery of cancer. Nevertheless, our study has certain limitations. Regarding the selection of indicators for measuring social support, the absence of a unified consensus within the academic community has resulted in a lack of precision and completeness in our choices. Our future endeavors will involve a more meticulous refinement of the scientific measurement related to social support indicators. The innovation of this study lies in the empirical analysis of the impact of social support on the mental health of cancer patients by using the data of China’s Health and pension tracking survey, which not only provides new empirical evidence for the formulation of health support and promotion policies for cancer patients in the new era, but also has great significance for the strategy of promoting healthy China. Moreover, due to data constraints, we did not differentiate between patients with various types of cancer. In reality, different cancer patients exhibit substantial variations in their conditions. Addressing these distinctions represents a focal point for our future in-depth research.
Improving and promoting the mental health status of cancer patients is a crucial focus in the fields of public health and psychology in various countries. Our study presents an empirical examination of the influence of social support on the mental health of cancer patients, using data from the 2018 CHARLS database. The findings indicate that both formal and informal social support can effectively improve the mental health of cancer patients. Additionally, we employed the PSM model to address potential endogeneity issues arising from sample selectivity bias. The results obtained through PSM demonstrate robustness, revealing that the impact of social support on the mental health of cancer patients may be underestimated in the absence of measures to counteract sample selectivity bias. Consequently, the Chinese government must prioritize the provision of social support as a proactive means to improve the psychological health of cancer patients, thereby continuously enhancing their quality of life. Moreover, this study provides empirical evidence and theoretical reference to further advance the establishment of a healthy China.
Acknowledgement: The authors thank research participants for their participation in this study.
Funding Statement: The author received no specific funding for this study.
Author Contributions: The idea design, first draft writing, data analysis, and interpretation of the results of the manuscript are the responsibility of the main Zhu. All authors reviewed the results and approved the final version of the manuscript.
Availability of Data and Materials: The data of 2018 China Health and Retirement Longitudinal Study (CHARLS) is publicly available at http://charls.pku.edu.cn/pages/data/2018-charls-wave4/zh-cn.html accessed on 24 September 2020.
Ethics Approval: The studies involving human participants were reviewed and approved by the approval for CHARLS data was obtained from the Biomedical Ethics Review Committee of Peking University (approval number: IRB00001052-11015). All participants signed informed consent at the time of participation.
Conflicts of Interest: The author declares that they have no conflicts of interest to report regarding the present study.
References
1. Zhang X, Xiao H, Chen Y. Effects of life review on mental health and well-being among cancer patients: a systematic review. Int J Nurs Stud. 2017;74(2):138–48 [Google Scholar] [PubMed]
2. Granek L, Nakash O, Ben-David M, Shapira S, Ariad S. Oncologists’ treatment responses to mental health distress in their cancer patients. Qual Health Res. 2018;28(11):1735–45 [Google Scholar] [PubMed]
3. Hemmington A, Huang D, Coomarasamy C, Young MJ, Consedine NS, Reynolds LM. When mental illness and cancer collide: an investigation of the predictors of outcomes for cancer patients with a history of mental health problems. Psycho-Oncol. 2020;29(3):525–31. [Google Scholar]
4. Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: A Cancer J Clin. 2021;71:209–49 [Google Scholar] [PubMed]
5. Eckerling A, Ricon-Becker I, Sorski L, Sandbank E, Ben-Eliyahu S. Stress and cancer: mechanisms, significance and future directions. Nat Rev Cancer. 2021;21(12):767–85 [Google Scholar] [PubMed]
6. Cohen S, Syme SL. Issues in the study and application of social support. Social Support and Health. 1985;3:3–22. [Google Scholar]
7. Taylor SE. Social support: a review. Oxf Handb Health Psychol. 2011;1:189–214. [Google Scholar]
8. Uchino BN, Bowen K, Carlisle M, Birmingham W. Psychological pathways linking social support to health outcomes: a visit with the “ghosts” of research past, present, and future. Soc Sci Med. 2012;74(7):949–57 [Google Scholar] [PubMed]
9. Klikovac TD, Petrović N, Šarić Đ. Assessment of cancer patients’ mental health during the coronavirus pandemic in Serbia. Int J Environ Res Public Health. 2023;20(2):1132 [Google Scholar] [PubMed]
10. Macía P, Gorbeña S, Barranco M, Alonso E, Iraurgi I. Role of resilience and emotional control in relation to mental health in people with cancer. J Health Psychol. 2022;27(1):211–22. [Google Scholar]
11. Vu TT, Lu W, Weiss M, Nguyen LTH, Ngo VK. Mental health, functional impairment, and barriers to mental health access among cancer patients in Vietnam. Psycho-Oncol. 2023;5(32):701–11. [Google Scholar]
12. Rakhshani T, Gholampour Y. Investigating the effect of an educational intervention on health promotion behaviors, hope enhancement and mental health in cancer patients. https://europepmc.org/article/PPR/PPR161231 [Accessed 2020]. [Google Scholar]
13. Becarevic N, Softic R. Religiosity and mental health among muslim cancer patients. Eur Psychiatry. 2023;66(S1):S945–6. [Google Scholar]
14. Hefner J, Eisenberg D. Social support and mental health among college students. Am J Orthopsychiatry. 2009;79(4):491–9 [Google Scholar] [PubMed]
15. London-Nadeau K, Chadi N, Taylor AB, Chan A, Pullen Sansfaçon A, Chiniara L, et al. Social support and mental health among transgender and nonbinary youth in Quebec. LGBT Health. 2023;10(4):306–14 [Google Scholar] [PubMed]
16. Qi M, Zhou SJ, Guo ZC, Zhang LG, Min HJ, Li XM, et al. The effect of social support on mental health in Chinese adolescents during the outbreak of COVID-19. J Adolesc Health. 2020;67(4):514–8 [Google Scholar] [PubMed]
17. Muñoz-Bermejo L, Adsuar JC, Postigo-Mota S, Casado-Verdejo I, de Melo-Tavares CM, Garcia-Gordillo MÁ, et al. Relationship of perceived social support with mental health in older caregivers. Int J Environ Res Public Health. 2020;17(11):3886. [Google Scholar]
18. Hu S, Cai D, Zhang XC, Margraf J. Relationship between social support and positive mental health: a three-wave longitudinal study on college students. Curr Psychol. 2022;41:6712–21. [Google Scholar]
19. Xie J, Chen Y, Huangbei Y, Xie B, Pei T. Research on the health status and social support impact of elderly people—Based on 2018 CLHLS data. Health Econ Res. 2022;39:74–8+82. [Google Scholar]
20. Usher K, Durkin J, Bhullar N. The COVID-19 pandemic and mental health impacts. Int J Ment Health Nurs. 2020;29(3):315 [Google Scholar] [PubMed]
21. Cullen W, Gulati G, Kelly BD. Mental health in the COVID-19 pandemic. QJM: An Int J Med. 2020;113(5):311–2. [Google Scholar]
22. Braghieri L, Levy RE, Makarin A. Social media and mental health. Am Econ Rev. 2022;112(11):3660–93. [Google Scholar]
23. Ye H, Li W. A study of the impact of social support on the subjective well-being of elderly veterans. Northwest Popul Mag. 2022;43:107–18. [Google Scholar]
24. Li M, Li H, Cao L, Wang Y, Cai L, Sun J, et al. Analysis of the moderating role of social support between depressed mood and quality of survival in patients undergoing chemotherapy for oncology. China Health Stat. 2021;38:384–86+390. [Google Scholar]
25. Kiely KM, Brady B, Byles J. Gender, mental health and ageing. Maturitas. 2019;129:76–84 [Google Scholar] [PubMed]
26. Blakemore SJ. Adolescence and mental health. Lancet. 2019;393(10185):2030–1 [Google Scholar] [PubMed]
27. Ai C, Norton EC. Interaction terms in logit and probit models. Econ Lett. 2003;80(1):123–9. [Google Scholar]
28. Dehejia RH, Wahba S. Propensity score-matching methods for nonexperimental causal studies. Rev Econ Stat. 2002;84(1):151–61. [Google Scholar]
29. Wang J. To use or not to use propensity score matching? Pharm Stat. 2021;20(1):15–24 [Google Scholar] [PubMed]
30. Carroll D. Health psychology: stress, behaviour and disease. London: Routledge; 2019. [Google Scholar]
Cite This Article
 Copyright © 2024 The Author(s). Published by Tech Science Press.
Copyright © 2024 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools