 Open Access
Open Access
ARTICLE
Existe-t-il un profil spécifique de perception du risque de COVID-19 chez les personnes atteintes d’un cancer ? une étude transversale
Is There a Specific Profile of COVID-19 Risk Perception among People with Cancer? A Cross-Sectional Study
1
Unit 1296 « Radiation : Defense, Health, Environment », INSERM, University Lyon 2, Bron, 69676, France
2
LPS UR849-Aix-Marseille Université, Marseille, 13284, France
3
Service de recherche clinique, Hôpital Fondation Adolphe de Rothschild, Paris, 75019, France
* Corresponding Author: Renaud Mabire-Yon. Email:
Psycho-Oncologie 2023, 17(4), 245-256. https://doi.org/10.32604/po.2023.042296
Received 25 May 2023; Accepted 10 July 2023; Issue published 28 December 2023
RÉSUMÉ
Objectifs : Cette étude visait à déterminer si les personnes atteintes d’un cancer (PAC) présentaient un profil unique de perception du risque COVID-19 et à identifier les facteurs psychosociaux caractérisant les PAC qui n’appartenaient pas au profil majoritaire de perception du risque. Procédure : Une étude transversale par auto-questionnaire en ligne a été menée en France du 25 avril au 7 mai 2020, avec un échantillon (n = 748) comprenant des PAC, des personnes ne recevant pas de traitement contre le cancer et des personnes n’ayant pas d’antécédents de cancer. Des profils latents de perception du risque COVID-19 (PLPR) ont été établis. Méthodes : Une régression logistique multinomiale multivariée a été réalisée pour évaluer l’association entre le statut de cancer et l’appartenance au PLPR. Les caractéristiques des PLPR selon les différents profils ont été comparées. Résultats : Quatre profils se sont dégagés, allant d’une perception faible du risque à une perception haute du risque. Les PAC étaient plus susceptibles d’appartenir au profil « Percepteurs à haut risque » (aOR : 3,02; p < 0,001). Les PAC ne correspondant pas à ce profil avaient un niveau socio-économique perçu plus élevé (p < 0,05). La majorité des PAC avaient un profil commun de perception du risque COVID-19, principalement influencé par les connaissances médicales désignant le cancer comme un facteur de risque d’avoir une COVID-19 grave. Le niveau socio- économique perçu était un facteur déterminant de la perception des risques parmi les PAC. Conclusion : Les interventions visant à modifier la perception du risque de COVID-19 devraient tenir compte de ces facteurs, en mettant particulièrement l’accent sur les préoccupations liées à l’infection par le SRAS-CoV-2.Abstract
Aims: This study aimed to determine if people with cancer (PWC) exhibit a unique COVID-19 risk perception profile and identify psychosocial factors characterizing PWC who do not conform to the majority risk perception profile. Procedure: A cross-sectional online self-questionnaire study was conducted in France from April 25 to May 07, 2020, with a sample (n = 748) comprising PWC, individuals not currently receiving cancer treatment, and those without a history of cancer. Latent profiles of COVID-19 risk perception (PCRP) were established. Methods: A multivariate multinomial logistic regression was performed to assess the association between cancer status and PCRP membership. Characteristics of PWC across different profiles were compared. Results: Four profiles emerged, ranging from Low-Risk to High-Risk Perceivers. PWC were more likely to belong to the High-Risk Perceivers profile (aOR: 3.02; p < 0.001). PWC not conforming to this profile had a higher perceived socioeconomic level (PSL) (p < 0.05). The majority of PWC demonstrated a specific COVID-19 risk perception profile, mainly influenced by medical knowledge linking cancer to increased COVID-19 severity. PSL was a key determinant in shaping risk perception among PWC. Conclusion: Interventions targeting COVID-19 risk perception modification should consider these factors, with particular emphasis on addressing concerns related to SARS-CoV-2 infection.MOTS CLÉS
Keywords
Supplementary Material
Supplementary Material FileIn December 2019, the world was introduced to COVID-19, a new coronavirus disease caused by Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) [1]. During the initial stages of the pandemic, there were no vaccines or antiviral treatments available, prompting countries to impose lockdowns and enforce social distancing measures. These behavioral prescriptions aimed to reduce person-to-person contact and slow down the virus’s spread. However, the virus continued to spread rapidly across the globe, leading to the largest pandemic of the 21st century. By May 2020, there were 3.86 million reported cases of SARS-CoV-2 infection and over 280,000 deaths [2]. Moreover, the pandemic placed immense pressure on health care systems worldwide. As a result, the provision of cancer care was severely disrupted, with non-urgent medical consultations and surgeries being postponed [3]. These delays in treatment resulted in increased psychological distress for people with cancer [4].
Furthermore, cancer has been identified as a significant risk factor for developing severe cases of COVID-19 and experiencing higher fatality rates [5]. As a result, people with cancer (PWC) are considered a particularly vulnerable group during the pandemic. Their risk perception has been influenced by several factors, including the anxiety-provoking media context, confinement measures, and their tendency to compare their risk to that of others [6–9].
In addition to these factors, sociodemographic and health variables play a role in shaping risk perception. For example, men generally perceive lower risks associated with COVID-19 than women [10,11], both in terms of personal vulnerability and the severity of potential consequences [12,13]. Age also influences risk perception, with younger individuals typically being less concerned about COVID-19 than older individuals [13]. However, more nuanced results emerge when differentiating between perceived vulnerability and perceived severity of the disease. While older age is positively associated with perceived severity, it is negatively associated with perceived vulnerability [12,14–16].
Furthermore, having indirect experiences with the virus, such as knowing someone infected with SARS-CoV-2, leads to heightened risk perception. Due to the widespread dissemination of warning messages emphasizing the vulnerability of immunocompromised individuals, particularly cancer patients, to COVID-19 (Haut Conseil de la Santé Publique, 2021), it is likely that individuals with pre-existing health conditions experienced a more acute perception of risk related to the virus. In line with this, research has demonstrated a higher perception of vulnerability in patients suffering from chronic diseases [17] or cancer [17,18].
To our knowledge, no study has focused on characterizing the risk perception of COVID-19 among patients with cancer compared to those who have had cancer or those who have never had cancer. This is a major gap in the scientific literature. Indeed, COVID-19 risk perception is positively associated with the adoption of preventive behaviors [19,20] (e.g., COVID-19 vaccination), cancer treatment adherence [21] and the level of worry about many aspects of life [22] (e.g., losing someone you love, the health care system being overloaded, having to face loneliness). Thus, the results of this research will allow the implementation of psychosocial interventions based on the modification of the COVID-19 risk perception promoting optimal prevention practices while preserving PWC from too high a level of worry. Thus, the main objectives of the study presented in this article were (1) to determine whether PWC, compared to people without cancer, shared a single COVID-19 risk perception profile and (2) to identify, among PWC, the psychosocial factors associated with belonging to a particular COVID-19 risk perception profile. The secondary aim of the study was to identify psychosocial and health factors associated with different profiles of COVID-19 risk perception.
The data were collected as part of the “Représentations Sociales, Adaptations, Risques: Cancer et COVID-19” study (RAR2C—Social Representations, Adaptations, Risks: Cancer and COVID-19). This was a cross-sectional study using an online self-report questionnaire available on the Seintinelles platform (https://www.seintinelles.com/) from April 25 to May 07, 2020. See Fig. 1 for a summary of the procedure.
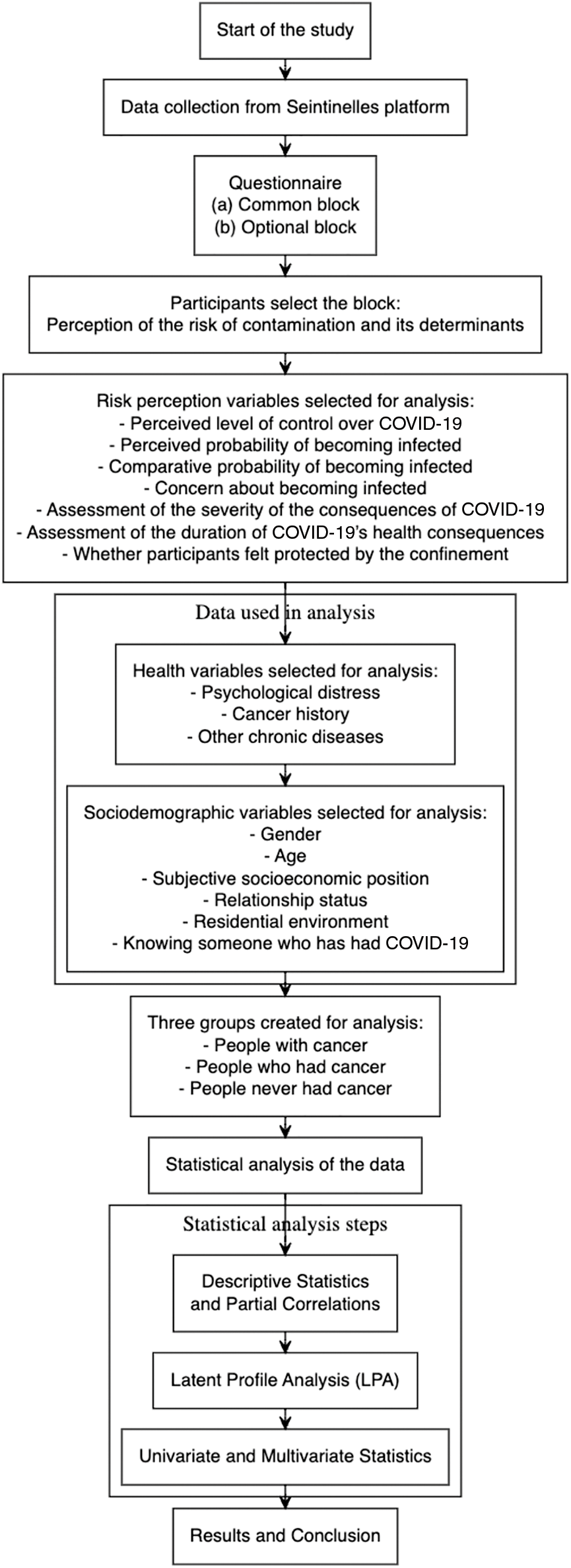
Figure 1: Flowchart of the study process.
The questionnaire was open to everyone registered on the platform (people with or without cancer). The study included only participants who were 18 years of age or older. No exclusion criteria were applied.
Only those who chose to complete the “Risk” portion of the questionnaire are included for this analysis. Details of the procedure are given in the supplementary material.
Measurements1
The following variables were used for the risk representation profiles (a) perceived level of control over COVID-19, (b) the perceived probability of becoming infected by SARS-CoV-2, (c) comparative probability of becoming infected by SARS-CoV-2, (d) concern about becoming infected by SARS-CoV-2, (e) assessment of the severity of the consequences of COVID-19 on one’s health and (f) assessment of the duration of COVID-19’s health consequences on health. Finally, participants were asked to indicate whether they felt protected by the confinement.
Psychological distress. To measure psychological distress, the French version [23] of the 12-item General Health Questionnaire was used (GHQ-12). The score on each question was dichotomized (0-0-1-1). The higher the score, the greater the psychological distress. The internal consistency of the GHQ-12 measured in our sample was good (α = 0.81 and Ω = 0.82).
Cancer. Participants were asked if they had ever had cancer in their lifetime. If so, they were asked if they were still undergoing treatment and the cancer site.
Other chronic diseases. Participants were asked if they suffered from one or more chronic diseases (other than cancer). These diseases were divided into two groups: (1) diseases that lead to a weakened condition in relation to COVID-19 and (2) diseases that do not lead to a weakened condition in relation to COVID-19. These groups were established referring to the opinion issued by France’s Haut Conseil de la Santé Publique [24].
Sociodemographic data such as gender, age, subjective socioeconomic position (on a 10-point Likert scale ranging from “the worst place in society” to “the best place in society”), relationship status and residential environment (urban, rural, or peri-urban), and knowing someone who has had COVID-19, were gathered.
The statistical analyses were carried out on R software [25]. The graphical representations have been made using the following packages: ggplot2 [26] and ggpubr [27].
Descriptive statistics and partial correlations
The descriptive statistics—for the quantitative variables—were calculated using their means, standard deviation, medians, extreme values, and the first and third quartiles using R package gtsummary [28]. Categorical variables were described by the number and percentage of each modality. Finally, partial correlations between risk perception variables were estimated using the R package ppcor [29].
To uncover potential heterogeneity in COVID-19 risk perception among cancer patients, we used Latent Profile Analysis (LPA) instead of direct group comparisons. We identified latent risk perception profiles for the entire sample and examined which profile was most common among cancer patients. LPA, using the package tidyLPA [30], was performed with six risk perception variables (see supplementary materials for details). Skewed variable distributions were normalized using the non-paranormal transformation [31] in the R package huge [32]. After estimation, latent profile models were compared via BLRT, BIC, AIC, and entropy scores to determine the best model. Profiles were plotted and compared using Kruskal-Wallis test, and Conover’s non-parametric all-pairs comparison test [33] was employed for post-hoc testing using the R package PMCMRplus [34].
Univariate and multivariate statistics
At first, on health and sociodemographic variables, univariate tests (χ2 test for qualitative variables and the Kruskal-Wallis test for quantitative variables) were performed to identify the factors associated with each profile. Then, significant variables at the threshold of p < 0.05 were included in the multinomial logistic regression model. The profile with the largest number of individuals was used as the reference profile. The model was estimated with the package nnet [35]. Finally, the model’s goodness of fit was tested with the Hosmer-Lemeshow test [36] using the package generalhoslem [37].
Personal data from the Seintinelles association relative to the constitution and management of a panel of people for research were processed by CNIL’s health care division under No. 1688474. The study received a favorable opinion from Inserm’s Comité d’Évaluation Éthique (Ethical Review Committee) No. 20-682 dated April 14, 2020.
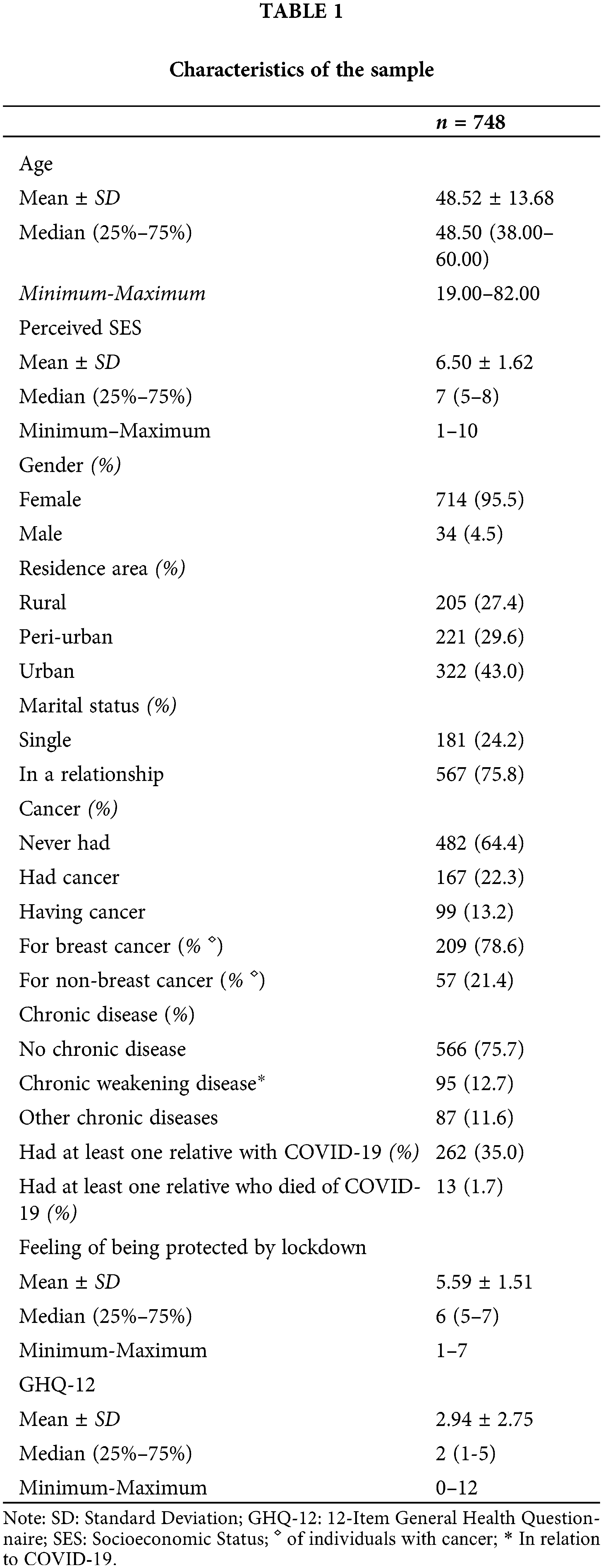
Characteristics of participants
The RAR2C study gathered answers from 2,882 individuals. Approximately 30% (n = 748) answered the questions concerning risk and comprised the sub-sample used for our analyses. These 748 respondents had an average age of 48 years. The average perceived socioeconomic level was relatively high (m = 6.50). Almost all participants were female (95.5%) and lived in couples (75.8%). 43% lived in urban areas. Most of them had not experienced a loved one’s death (98.3%), although 35% of the participants had someone close to them who had had COVID-19. 75.7% of the participants stated that they did not have any chronic disease, and 64.4% said they had never had cancer. At the time of the survey, 13% were undergoing treatment for cancer. With a mean of 5.59, individuals felt protected by the lockdown. Finally, the average GHQ-12 score (2.94) was reliable, indicating good mental health (see Table 1).
Risk perception, latent profiles, and associated factors
Perception of the risk associated with COVID-19
For all six variables (Table 2) used to characterize COVID-19 risk perception, perceived control had the lowest average score (mean [m] = 2.67), followed by the assessment of the comparative probability of becoming infected by SARS-CoV-2 (m = 4.16) and the assessment of the severity of the COVID-19’s health consequences (m = 3.31). On the other hand, the highest average scores were observed for the assessment of concern about becoming infected by SARS-CoV-2 (m = 4.71), the perceived probability of becoming infected by SARS-CoV-2 (m = 4.52), and the assessment of the duration of COVID-19’s health consequences (m = 4.36). For the participants, SARS-CoV-2 infection and the resulting disease are seen as a highly worrisome risk overall, which is uncontrollable and highly probable, with serious consequences. However, there is a remarkable dispersion of participants’ responses to the questions on the concerns raised by the disease and the perception of its consequences.
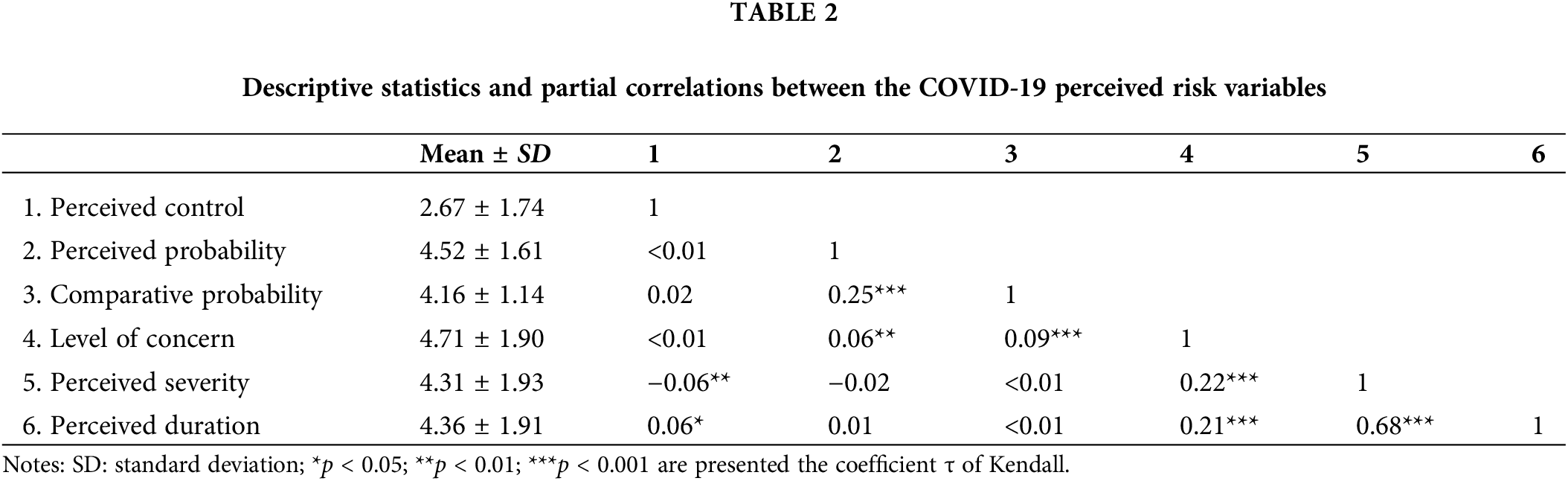
Table 2 shows the partial correlations between the COVID-19 perceived risk variables. The perceived control was significantly associated with the perceived severity and the perceived duration but not significantly associated with other variables. The perceived probability was significantly associated with the comparative probability and the level of concern. The comparative probability was also significantly associated with the level of concern. In addition, the level of concern was significantly associated with the perceived severity and the perceived duration. Finally, perceived severity and perceived duration were significantly, positively, and strongly correlated.
With a concern for parsimony in our Latent Profile Analysis (LPA), we did not explore models with more than six profiles (Table 3). Following the recommendations of the literature [38], the models containing profiles regrouping less than 5% of the sample were discarded. Taking the BIC and the BLRT (at p < 0.05) into account led us to consider the four-profile model the most relevant, whose entropy was satisfactory.
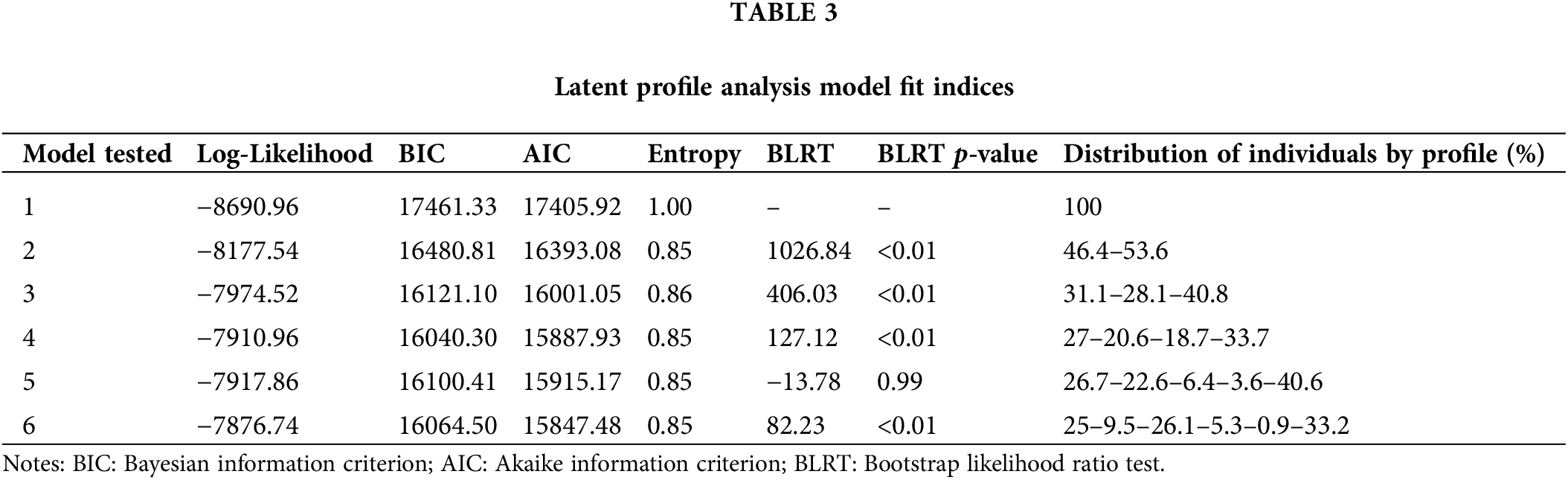
Fig. 2 presents the average score per profile on the different dimensions of risk perception. There was no significant difference in perceived control (Fig. 1A) and perceived probability (Fig. 1B). However, the comparative probability (Fig. 1C) allowed two profiles to be distinguished from each other (p < 0.05). Furthermore, all profiles differed from each other in their level of concern (Fig. 1D), level of perceived severity (Fig. 1E), and perceived duration (Fig. 1F) (each with a p < 0.0001). The four profiles are distributed from lowest to highest perceived risk. Thus, the different profiles were respectively named: low risk perceivers (20.6%; n = 154), moderately low risk perceivers (33.7%; n = 252), moderately high-risk perceivers (18.7%; n = 140), and high-risk perceivers (27%: n = 202). In the high-risk perceivers profile, the disease was considered very serious (i.e., COVID-19’s duration and health consequences) and very worrisome.
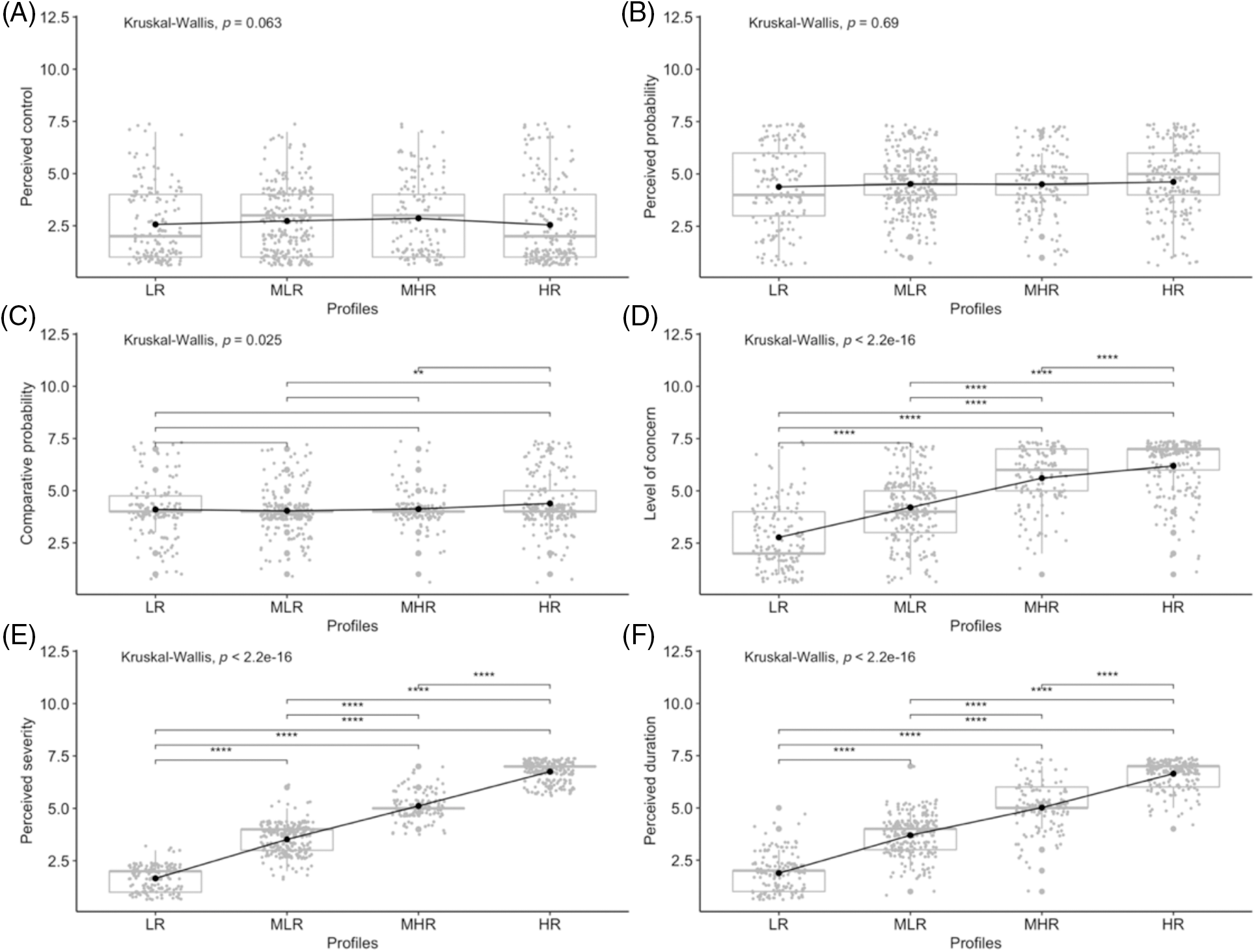
Figure 2: The plot of scores per profile on COVID-19 risk perception variables. LR: low risk perceiver; MLR: moderately low risk perceivers; MHR: moderately high risk perceiver; HR: high risk perceivers; **p < 0.01; ***p < 0.001; ****p < 0.0001; the black dots represent the means.
Conversely, in the low-risk perceivers profile, the disease was considered benign and is not really a source of concern. The other two profiles can be qualified as intermediate. The moderately high perceivers profile covers individuals who perceived the risk as moderately high. The disease was represented as being moderately serious and worrisome. The moderately low perceivers profile was the most common. The disease was considered as not being very serious and not very worrisome.
Association between cancer and risk perception profiles
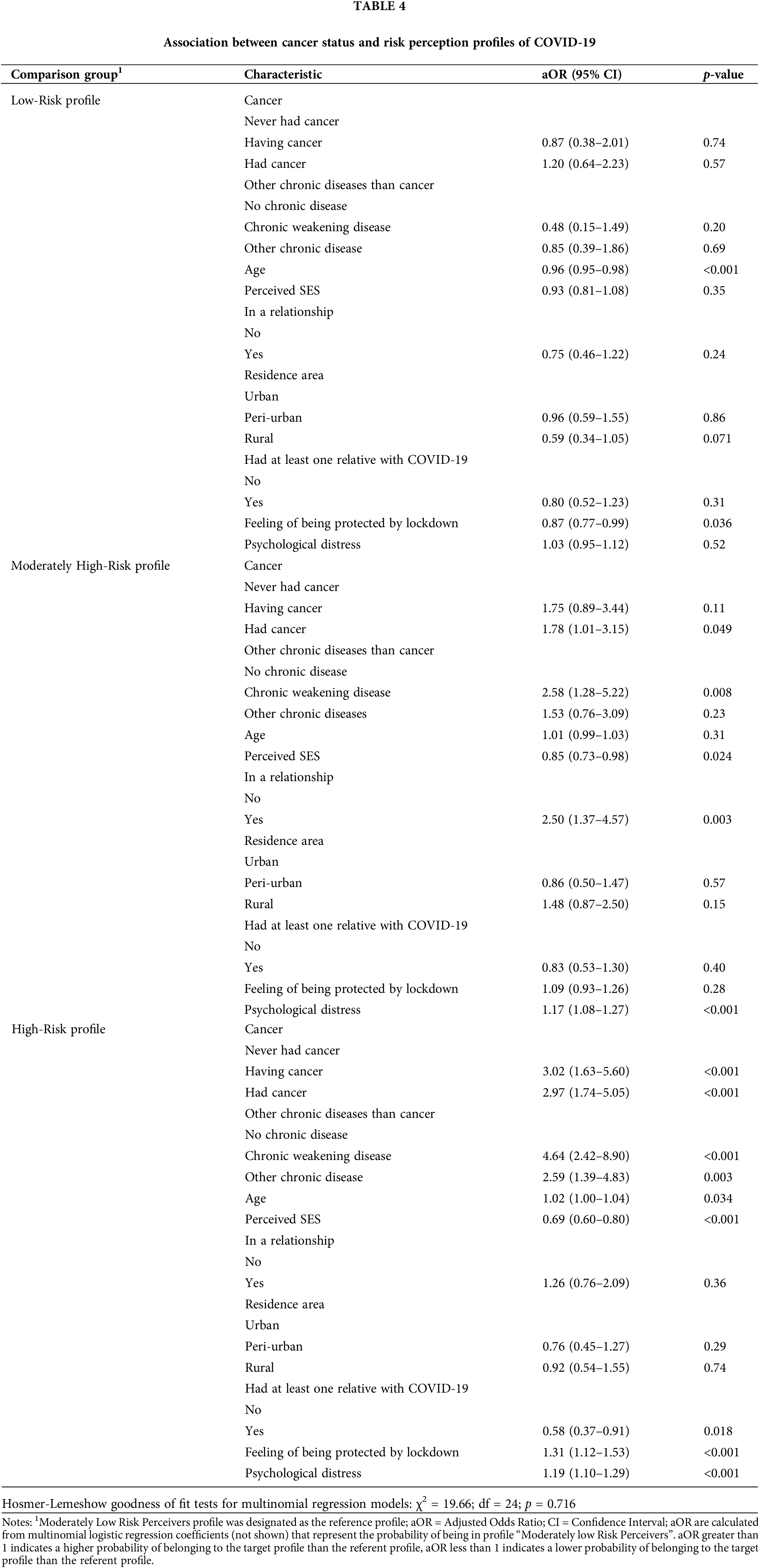
Multivariate multinomial logistic regression was performed to determine whether individuals with cancer had a specific COVID-19 risk perception profile. The model had a good adjustment quality (Hosmer-Lemeshow test’s p-value = 0.716)2.
As show in Table 4, regardless of the effect of other chronic diseases than cancer, age, subjective socioeconomic status, marital status, the area of residence, having relatives with COVID-19, perceived protection by confinement, and psychological distress: people undergoing cancer treatment were much more likely than others to belong to the high-risk profile (Adjusted Odds Ratio [aOR]: 3.02; p < 0.001). Being on cancer treatment was not associated with any other profile. However, those who had cancer were more likely to belong to the high-risk profile (aOR: 2.97; p < 0.001) and to the moderately high-risk profile (aOR: 1.78; p < 0.049). Significant associations with control variables are presented in the supplementary material.
Factors associated with perceived risk of COVID-19 among individuals with cancer
Our last objective was to identify, among people undergoing cancer treatment (n = 99), the psychosocial factors that distinguish individuals from different profiles of risk perception. Indeed, not all people undergoing cancer treatment belonged to the high-risk profile; 44% (n = 44) belonged to the high-risk profile, 21% (n = 21) belonged to the moderately high-risk profile, 25% (n = 25) belonged to the moderately low risk profile, and 9.1% (n = 9) belonged to the low-risk profile (see Fig. 3).
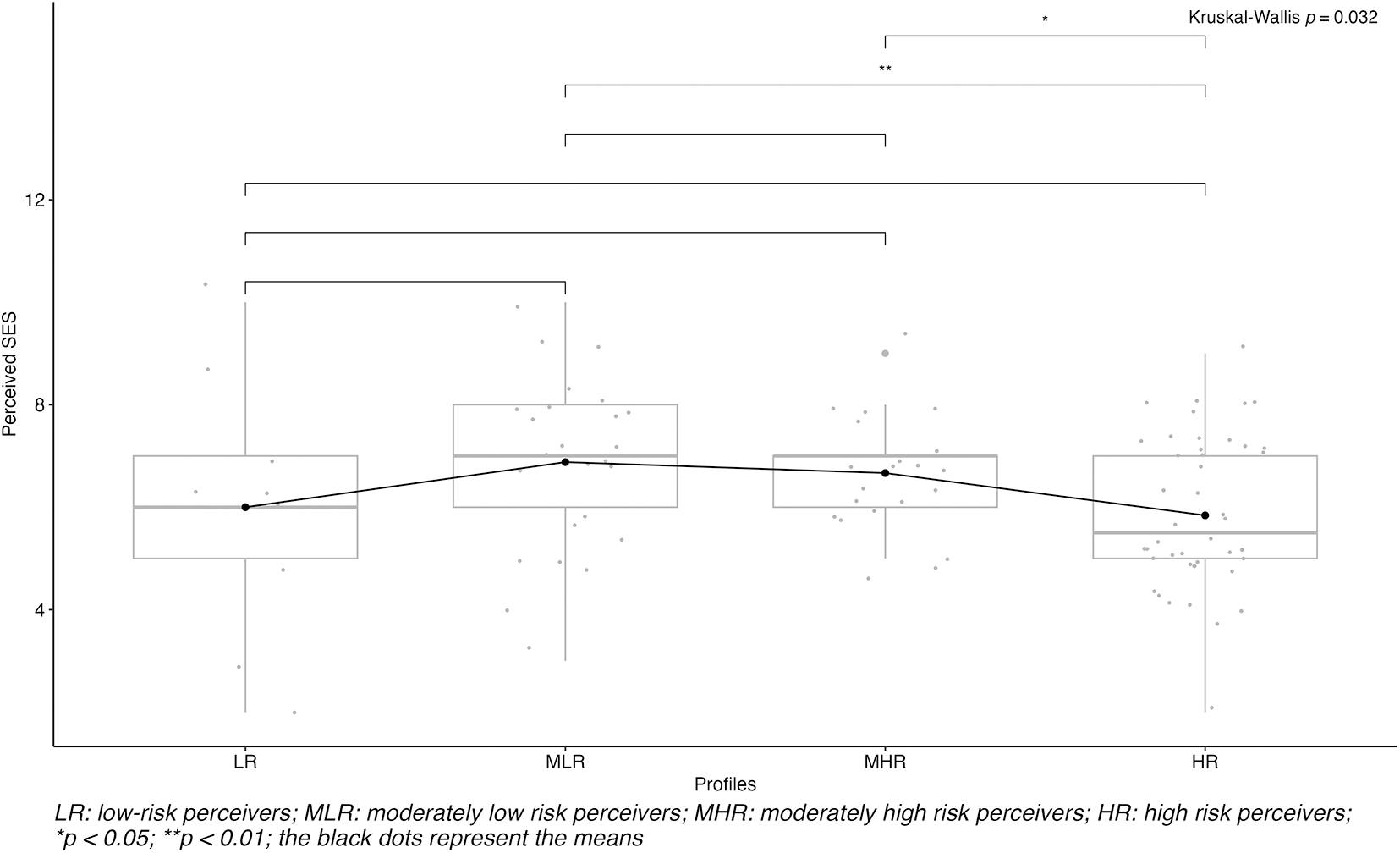
Figure 3: The plot of perceived SES scores by profile among individuals undergoing cancer treatment. LR: low risk perceiver; MLR: moderately low risk perceivers; MHR: moderately high risk perceiver; HR: high risk perceivers; *p < 0.05; **p < 0.01; the black dots represent the means.
A series of univariate tests were conducted with the health and psychosocial variables (Cf. supplementary materials). Between COVID-19’s risk perception profiles, only the perceived SES was significantly different (p = 0.032) (Fig. 2). Among those undergoing cancer treatment, those not belonging to the high-risk perceivers profile (i.e., belonging to the moderately high perceivers or moderately low perceivers profiles) had a significantly higher perceived SES level (respectively, p < 0.05 and p < 0.01).
Our analysis shows that, in a context of major health crisis due to a hitherto unknown virus, where scientific knowledge is uncertain and under construction, there was a typical organization of the representation of the risk related to COVID-19 among PWC (whatever the type or stage of cancer). Although most PWC perceive high risk, this is not the only perception observed among them. Perceived socioeconomic status was found to be involved in the variation in risk perception. Thus, the experience of somatic vulnerability appears essential but not sufficient to understand the relationship with health risks for people with cancer.
The risk associated with SARS-CoV-2 infection is consensually perceived as both uncontrollable and highly probable. This risk is also perceived as being worrisome and severe, although the participants’ perceptions on this subject are not unanimous. This perception seems relevant to an epidemic phenomenon, quickly spreading and with potentially lethal consequences. When these data were collected, little or no knowledge existed about this risk, its origin, methods of protection, or how to deal with it. The characteristics of the COVID-19 risk were close to those found by Slovic [39] to characterize catastrophic risks, assessed as feared and unknown risks, such as those related to chemical industries or biotechnologies.
The perception variables formed a group of variables that were relatively well associated, arguing for a conceptual consistency of the perceived risk as we measured it.
The partial correlation analysis between the six dimensions of risk perception tended to show a conceptual consistency of the perceived risk as we measured it. Perceived control was the variable least conditionally associated with the rest of the variables. The level of concern was conditionally associated with severity, duration, and perceived probability. Finally, individuals did not distinguish between the perceived duration and severity of the COVID-19. Thus, a severe infection would necessarily be long, and conversely, a long infection would necessarily be severe.
The latent profile analysis performed distinguished four major profiles with respect to the individual risk of being infected by COVID-19, which notably differed in terms of (1) the level of concern about becoming infected, (2) the perception of the severity of the health consequences in case of infection and (3) the perception of the duration of the health consequences.
The four profiles produce a polarized continuum ranging from a profile associated with a low level of perceived risk (Low Risk Perceivers) to a very high level of perceived risk (High-Risk Perceivers). This configuration is close to that previously identified by Yang et al. [40]. Like us, they distinguish different profiles that differ by the degree of intensity of COVID-19 risk perception (i.e., Risk Deniers, Risk Neutrals, Risk Exaggerators). Nevertheless, their results differ from ours in the number of profiles described and in the relative importance of each of these profiles. Our results enabled us to isolate four profiles instead of three for Yang et al. [40]: Low Risk/Moderately Low Risk Perceivers vs. Moderately High/High-Risk Perceivers. Also, our configuration does not include a neutral profile.
Cancer and COVID-19 risk perception. Our results show that PWC were about three times more likely to belong to the high-risk perceivers profile than those who had never had cancer. This relationship was also observed for people who have already had cancer. In addition, compared to people who have never had cancer, those who have had cancer were more likely to have a moderately high perceived risk of COVID-19. These results support the hypothesis that how individuals with cancer develop a risk perception of COVID-19 is based partly on medical knowledge widely disseminated in social communication (e.g., media) that presented cancer as a vulnerability factor for SARS-CoV-2 infection. The association between somatic vulnerabilities and COVID-19 risk perceptions, for a large part, was consistent with the literature. These results are in accordance with those found in the study by Chen et al. [41], carried out on a sample of people with cancer, which showed that the level of concern related to cancer’s progression is positively associated with the level of concern related to COVID-19. The link between a high perception of risk related to COVID-19 and having cancer is also found in a study of all (n = 171,087) COVID-19 cases diagnosed in Portugal until April 2020. Along the same lines, among cancer survivors, the farther their cure dates are in the past, the less concern they show for the health consequences of COVID-19 [18].
Nevertheless, not all individuals with cancer belonged to the high-risk perceivers profile. Thus, we sought to identify factors characteristic of individuals who do not belong to the high-risk perceivers profile among cancer patients. A higher perceived SES level characterized cancer patients who did not belong to the high-risk profile. This is consistent with studies that find a positive association between low SES and COVID-19 prevalence and mortality [42–44], and a higher level of concern among PWC [45]. Because they have a lower level of trust in institutions and governments, the most socioeconomically precarious populations are the most vulnerable during natural disasters [46]. Thus, in the context of the COVID-19 crisis, the least socioeconomically precarious individuals would have more confidence in institutions (e.g., governments, health care system, physicians) to preserve their health in the event of SARS-CoV-2 infection. However, a study dedicated to the study of risk perception of COVID-19 found results contrary to ours; individuals with high-risk perception had a higher SES [47]. The discussion of the secondary results is presented in the supplementary materials.
The level of concern: a double-edged emotion. It is beneficial for people to maintain a sufficient level of concern to ensure preventive behaviors [20,48]. However, the concern is also a factor in psychological distress and intergroup violence [49]. Thus, the concern appears to be a fundamental dimension of risk perception that should be carefully influenced and deserves special attention during the follow-up of cancer patients. Concern about SARS-CoV-2 infection can be either self-oriented3 or other-oriented4. To influence the level of concern, interventions differentiated according to the nature of the concern seem appropriate.
Recommendations, Future Direction and Conclusion
Therefore, we recommend that Health Care Providers (HCP) investigate the nature of their patients’ SARS-CoV-2-related concerns by inviting them to express themselves freely about their concerns and the contexts in which they arise. At the same time, HCPs can assess the extent to which this concern is associated with (1) psychological distress, (2) effective prevention behaviors, and (3) good knowledge about COVID-19. This information will contribute to implementing interventions that focus on COVID-19’s risk perception. Concern should be mitigated for patients with a high-risk perception profile if it causes psychological distress. For PWC with a high-risk perception who do not engage in preventive behaviors, it is appropriate to at least attenuate the level of concern and build with them easily appropriable prevention solutions considering their social and material living conditions. The prevention measures must be adapted to the constraints of life and not the opposite. For patients with a low level of concern and too little engagement in preventive behaviors, we propose to act to simultaneously increase their concern and their perception of severity. However, this type of intervention must be accompanied by (1) an excellent monitoring of psychological distress and (2) the collaborative construction of adapted prevention solutions. Collaborative construction of prevention solutions with patients is even more crucial for people of low socioeconomic status.
In any case, we recommend maintaining a high perception of severity to prevent disengagement from preventive behaviors or optimize adopting these behaviors. In addition, since the level of knowledge about COVID-19 is positively related to effective prevention behaviors [50], interventions should also include constructive and didactic exchanges that allow patients to acquire accurate knowledge about COVID-19.
Several limitations need to be considered when interpreting our results. In the non-representative sample, men were under-represented, as were single people and socioeconomically precarious individuals. The online questionnaire could only reach people with access to the Internet. This calls for caution in generalizing our results to the general population. The participants were recruited through the collaborative “Seintinelles” platform, which brings together volunteers willing to participate in cancer studies. Given the cross-sectional nature of the data, it was not possible to show causal links between variables. The associations found will have to be confirmed by a longitudinal study or by default, via more specific analyses such as Bayesian network analysis. Given the relatively small number of cancer patients in our sample, studying the differences between different cancers was impossible. Studies with a greater diversity of cancer types would show possible differences in risk perception depending on the type and severity of cancer. A single-item measure of SES does not allow an extremely fine analysis of the influence of this factor. Studies that measure SES in more detail could be very informative. Finally, the data were collected in a very singular context; that of a total lockdown imposed by the French government. A longitudinal approach would allow us to verify the robustness of the results over time and the change of context.
Future research should explore COVID-19 risk perception dynamics over time, especially as new information and treatments emerge. Longitudinal studies and larger samples with diverse cancer types can provide deeper insights into risk perception differences depending on cancer type and severity.
Acknowledgement: We, the authors, would like to express our appreciation to the researchers of the RAR2C group. We thank C. Carpentier, J. Devif, B. Douffet, M. Doumergue, D. Ferraz, M. Girodet, S. Guinguené, N. Kalampalikis, T. Leroy, S. Leveaux, X. Mabire, P. Mercier, C. Morin-Messabel, M. Pannard, S. Rouat, and E. Vayre for their contributions. We particularly want to acknowledge A. Le Bonniec and X. Mabire for their helpful comments on the initial version of this work. Additionally, we extend our thanks to the members of the “Seintinelles” association, who supported and approved this research. We particularly appreciate the assistance of Guillemette Jacob. Finally, we would like to thank all of those who took part in our study. Your participation has been integral to this research.
Financements/Funding Statement: This work was supported by the French National Research Agency and Cancéropôle CLARA—Lyon—France.
Contributions des auteurs/Author Contributions: The study was designed with the participation of all authors under the supervision of Marie Préau. Renaud Mabire-Yon, Thibaud Marmorat and Claire Della Vecchia contributed to the data collection. Data analysis was carried out by Renaud Mabire-Yon with the help of Thibaud Marmorat and Hervé Picard. All authors contributed to the interpretation of the data. The manuscript was written by Renaud Mabire-Yon, Thibaud Marmorat and Arnaud Siméone. The manuscript has been proofread, improved and then validated by all the authors.
Disponibilité des données et du matériel/Availability of Data and Materials: The data will be provided upon request to the corresponding author.
Avis éthqiues/Ethics Approval: Personal data from the Seintinelles association relative to the constitution and management of a panel of people for research were processed by CNIL’s health care division under No. 1688474. The study received a favorable opinion from Inserm’s Comité d’Évaluation Éthique (Ethical Review Committee) No. 20-682 dated April 14, 2020.
Conflits d’intérêt/Conflicts of Interest: The authors of this research certify that they do not have any affiliation with any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
Matériels supplémentaires/Supplementary Materials: The supplementary material is available online at https://doi.org/10.32604/po.2023.042296.
1The detail of the measurements is available in supplementary material.
2A nonsignificant p-value indicates no evidence that the observed and expected frequencies differ (i.e., evidence of good fit).
3e.g., worry about developing a severe form of COVID-19.
4e.g., fear of harming others (by infecting them) or fear of being stigmatized if infected.
References
1. Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708–20. doi:10.1056/NEJMoa2002032. [Google Scholar] [PubMed] [CrossRef]
2. WHO Coronavirus (COVID-19) Dashboard | WHO Coronavirus (COVID-19) Dashboard with Vaccination Data. Available from: https://covid19.who.int/table. [Accessed 2022]. [Google Scholar]
3. The Lancet Oncology. Safeguarding cancer care in a post-COVID-19 world. Lancet Oncol. 2020;21(5):603. doi:10.1016/S1470-2045(20)30243-6. [Google Scholar] [PubMed] [CrossRef]
4. Ye Y, Wang J, Cai S, Fu X, Ji Y. Psychological distress of cancer patients caused by treatment delay during the COVID-19 pandemic in China: a cross-sectional study. Psychooncology. 2022;31(9):1607–15. [Google Scholar] [PubMed]
5. Thakur B, Dubey P, Benitez J, Torres JP, Reddy S, Shokar N, et al. A systematic review and meta-analysis of geographic differences in comorbidities and associated severity and mortality among individuals with COVID-19. Sci Rep. 2021;11(1):8562. doi:10.1038/s41598-021-88130-w. [Google Scholar] [PubMed] [CrossRef]
6. Attema AE, L’Haridon O, Raude J, Seror V. Beliefs and risk perceptions about COVID-19: evidence from two successive French representative surveys during lockdown. Front Psychol. 2021 [cited 2021 May 16];12:265. doi:10.3389/fpsyg.2021.619145. [Google Scholar] [PubMed] [CrossRef]
7. de Vries M, Claassen L, te Wierik MJM, van den Hof S, Brabers AEM, de Jong JD, et al. Dynamic public perceptions of the coronavirus disease crisis, the Netherlands, 2020. Emerg Infect Dis. 2021;27(4):1098–109. doi:10.3201/eid2704.203328. [Google Scholar] [PubMed] [CrossRef]
8. Siegrist M, Luchsinger L, Bearth A. The impact of trust and risk perception on the acceptance of measures to reduce COVID-19 cases. Risk Anal. 2021;41(5):787–800. [Google Scholar] [PubMed]
9. Trifiletti E, Shamloo SE, Faccini M, Zaka A. Psychological predictors of protective behaviours during the COVID-19 pandemic: theory of planned behaviour and risk perception. J Community Appl Soc Psychol. 2021. [Google Scholar]
10. Dryhurst S, Schneider CR, Kerr J, Freeman ALJ, Recchia G, van der Bles AM, et al. Risk perceptions of COVID-19 around the world. J Risk Res. 2020;23(7–8):994–1006. doi:10.1080/13669877.2020.1758193. [Google Scholar] [CrossRef]
11. Yıldırım M, Güler A. Factor analysis of the COVID-19 perceived risk scale: a preliminary study. Death Stud. 2020;48(5):585–598. [Google Scholar]
12. Rosi A, van Vugt FT, Lecce S, Ceccato I, Vallarino M, Rapisarda F, et al. Risk perception in a real-world situation (COVID-19how it changes from 18 to 87 years old. Front Psychol. 2021;12:528. doi:10.3389/fpsyg.2021.646558. [Google Scholar] [PubMed] [CrossRef]
13. Savadori L, Lauriola M. Risk perception and protective behaviors during the rise of the COVID-19 outbreak in Italy. Front Psychol. 2021;11:3822. doi:10.3389/fpsyg.2020.577331. [Google Scholar] [PubMed] [CrossRef]
14. Bruine de Bruin W. Age differences in COVID-19 risk perceptions and mental health: evidence from a National U.S. Survey conducted in March 2020. J Gerontol Ser B. 2021;76(2):e24–9. [Google Scholar]
15. Guastafierro E, Toppo C, Magnani FG, Romano R, Facchini C, Campioni R, et al. Older adults’ risk perception during the COVID-19 pandemic in lombardy region of Italy: a cross-sectional survey. J Gerontol Soc Work. 2021;64(6):585–98. [Google Scholar] [PubMed]
16. Pasion R, Paiva TO, Fernandes C, Barbosa F. The AGE effect on protective behaviors during the COVID-19 outbreak: Sociodemographic, perceptions and psychological accounts. Front Psychol. 2020;11:561785. doi:10.3389/fpsyg.2020.561785. [Google Scholar] [PubMed] [CrossRef]
17. Laires PA, Dias S, Gama A, Moniz M, Pedro AR, Soares P, et al. The association between chronic disease and serious COVID-19 outcomes and its influence on risk perception: survey study and database analysis. JMIR Public Health Surveill. 2021;7(1):e22794. doi:10.2196/22794. [Google Scholar] [PubMed] [CrossRef]
18. Leach CR, Kirkland EG, Masters M, Sloan K, Rees-Punia E, Patel AV, et al. Cancer survivor worries about treatment disruption and detrimental health outcomes due to the COVID-19 pandemic. J Psychosoc Oncol. 2021;39(3):347–65. [Google Scholar] [PubMed]
19. Patwary MM, Alam MA, Bardhan M, Disha AS, Haque MZ, Billah SM, et al. COVID-19 vaccine acceptance among low- and lower-middle-income countries: a rapid systematic review and meta-analysis. Vaccines. 2022;10(3):427. doi:10.3390/vaccines10030427. [Google Scholar] [PubMed] [CrossRef]
20. Zancu SA, Măirean C, Diaconu-Gherasim LR. The longitudinal relation between time perspective and preventive behaviors during the COVID-19 pandemic: the mediating role of risk perception. Curr Psychol. 2022 Apr 11 [cited 2022 Jun 25];21(5):571. doi:10.1007/s12144-022-03069-z. [Google Scholar] [PubMed] [CrossRef]
21. Cheli S, Lam WWT, Estapé T, Winterling J, Bahcivan O, Andritsch E, et al. Risk perception, treatment adherence, and personality during COVID-19 pandemic: an international study on cancer patients. Psychooncology. 2022;31(1):46–53. doi:10.1002/pon.5775. [Google Scholar] [PubMed] [CrossRef]
22. Chambon M, Dalege J, Elberse JE, van Harreveld F. A psychological network approach to attitudes and preventive behaviors during pandemics: a COVID-19 study in the United Kingdom and the Netherlands. Soc Psychol Personal Sci. 2021 Mar 23 [cited 2022 Jun 14];13(1):233–45. doi:10.1177/19485506211002420. [Google Scholar] [CrossRef]
23. Lesage FX, Martens-Resende S, Deschamps F, Berjot S. Validation of the general health questionnaire (GHQ-12) adapted to a work-related context. Open J Prev Med. 2011;1(2):44–8. doi:10.4236/ojpm.2011.12007. [Google Scholar] [CrossRef]
24. Haut Conseil de la Santé Publique. Coronavirus SARS-CoV-2: barrier and physical distancing measures for the general population. 2021 [cited 2021 Apr 22]. Available from: https://www.hcsp.fr/Explore.cgi/AvisRapportsDomaine?clefr=912. [Google Scholar]
25. R Core Team. R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing. Available from: https://www.R-project.org/. [Accessed 2021]. [Google Scholar]
26. Wickham H. ggplot2: elegant graphics for data analysis. Springer; 2016. [Google Scholar]
27. Kassambara A. ggpubr: “ggplot2” based publication ready plots. Available from: https://CRAN.R-project.org/package=ggpubr. [Accessed 2020]. [Google Scholar]
28. Sjoberg DD, Curry M, Hannum M, Larmarange J, Whiting K, Zabor EC. Presentation ready data summary and analytic result tables. Available from: https://CRAN.R-project.org/package=gtsummary. [Accessed 2021]. [Google Scholar]
29. Kim S. ppcor: an R package for a fast calculation to semi-partial correlation coefficients. Commun Stat Appl Methods. 2015;22(6):665–74. doi:10.5351/CSAM.2015.22.6.665. [Google Scholar] [PubMed] [CrossRef]
30. Rosenberg JM, Beymer PN, Anderson DJ, Van Lissa CJ, Schmidt JA. tidyLPA: an R package to easily carry out latent profile analysis (LPA) using open-source or commercial software. J Open Source Softw. 2019;3(30):978. doi:10.21105/joss.00978. [Google Scholar] [CrossRef]
31. Liu H, Lafferty J, Wasserman L. The nonparanormal: semiparametric estimation of high dimensional undirected graphs. J Mach Learn Res. 2009;10(10):2295–328. [Google Scholar]
32. Jiang H, Fei X, Liu H, Roeder K, Lafferty J, Wasserman L, et al. huge: High-Dimensional Undirected Graph Estimation. Available from: https://CRAN.R-project.org/package=huge. [Accessed 2021]. [Google Scholar]
33. Conover WJ, Iman RL. Multiple-comparisons procedures. Informal report. Los Alamos National Lab. (LANLLos Alamos, NM (United States). 1979 Feb [cited 2022 Mar 5]. Report No. LA-7677-MS. Available from: https://www.osti.gov/biblio/6057803. [Google Scholar]
34. Pohlert T. PMCMRplus: Calculate Pairwise Multiple Comparisons of Mean Rank Sums Extended. 2021. Available from: https://CRAN.R-project.org/package=PMCMRplus. [Google Scholar]
35. Venables WN, Ripley BD. Modern applied statistics. 4th ed. New York: Springer; 2002. [Google Scholar]
36. Fagerland MW, Hosmer DW, Bofin AM. Multinomial goodness-of-fit tests for logistic regression models. Stat Med. 2008;27(21):4238–53. doi:10.1002/sim.3202. [Google Scholar] [PubMed] [CrossRef]
37. Jay M. generalhoslem: Goodness of Fit Tests for Logistic Regression Models. Available from: https://CRAN.R-project.org/package=generalhoslem. [Accessed 2019]. [Google Scholar]
38. Spurk D, Hirschi A, Wang M, Valero D, Kauffeld S. Latent profile analysis: a review and “how to” guide of its application within vocational behavior research. J Vocat Behav. 2020;120(1):103445. doi:10.1016/j.jvb.2020.103445. [Google Scholar] [CrossRef]
39. Slovic P. Perception of risk. Science. 1987;236(4799):280–5. doi:10.1126/science.3563507. [Google Scholar] [PubMed] [CrossRef]
40. Yang Z, Xin Z. Heterogeneous risk perception amid the outbreak of COVID-19 in China: implications for economic confidence. Appl Psychol Health Well-Being. 2020 Dec 1;12(4):1000–18. doi:10.1111/aphw.12222. [Google Scholar] [PubMed] [CrossRef]
41. Chen G, Wu Q, Jiang H, Zhang H, Peng J, Hu J, et al. Fear of disease progression and psychological stress in cancer patients under the outbreak of COVID-19. Psychooncology. 2020;29(9):1395–8. doi:10.1002/pon.5451. [Google Scholar] [PubMed] [CrossRef]
42. Hawkins RB, Charles EJ, Mehaffey JH. Socio-economic status and COVID-19-related cases and fatalities. Public Health. 2020;189(16):129–34. doi:10.1016/j.puhe.2020.09.016. [Google Scholar] [PubMed] [CrossRef]
43. Rozenfeld Y, Beam J, Maier H, Haggerson W, Boudreau K, Carlson J, et al. A model of disparities: risk factors associated with COVID-19 infection. Int J Equity Health. 2020;19(1):126. doi:10.1186/s12939-020-01242-z. [Google Scholar] [PubMed] [CrossRef]
44. Ginsburgh V, Magerman G, Natali I. COVID-19 and the role of inequality in French regional departments. Eur J Health Econ. 2021;22(2):311–27. doi:10.1007/s10198-020-01254-0. [Google Scholar] [PubMed] [CrossRef]
45. Ernst M, Beutel ME, Brähler E. Cancer as a risk factor for distress and its interactions with sociodemographic variables in the context of the first wave of the COVID-19 pandemic in Germany. Sci Rep. 2022;12(1):2021. [Google Scholar] [PubMed]
46. Rowel R, Sheikhattari P, Barber TM, Evans-Holland M. Introduction of a guide to enhance risk communication among low-income and minority populations: a grassroots community engagement approach. Health Promot Pract. 2012;13(1):124–32. doi:10.1177/1524839910390312. [Google Scholar] [PubMed] [CrossRef]
47. Reed-Thryselius S, Fuss L, Rausch D. The relationships between socioeconomic status, COVID-19 risk perceptions, and the adoption of protective measures in a Mid-Western City in the United States. J Community Health. 2022 Feb 7 [cited 2022 Mar 23];47(3):464–74. doi:10.1007/s10900-022-01070-y. [Google Scholar] [PubMed] [CrossRef]
48. Elharake JA, Shafiq M, McFadden SM, Malik AA, Omer SB. The association of COVID-19 risk perception, county death rates, and voluntary health behaviors among U.S. Adult population. J Infect Dis. 2021;225:jiab131. [Google Scholar]
49. Tei S, Fujino J. Social ties, fears and bias during the COVID-19 pandemic: fragile and flexible mindsets. Humanit Soc Sci Commun. 2022;9(1):1–7. doi:10.1057/s41599-022-01210-8. [Google Scholar] [CrossRef]
50. Siddiquea BN, Shetty A, Bhattacharya O, Afroz A, Billah B. Global epidemiology of COVID-19 knowledge, attitude and practice: a systematic review and meta-analysis. BMJ Open. 2021;11(9):e051447. doi:10.1136/bmjopen-2021-051447. [Google Scholar] [PubMed] [CrossRef]
Cite This Article
 Copyright © 2023 The Author(s). Published by Tech Science Press.
Copyright © 2023 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools